Preemptive kidney transplantation is both patient-centered and cost saving and affords the benefit of avoiding dialysis-related complications such as placement of an arteriovenous graft or fistula, catheter-related infection, and risk of cardiovascular events. Patients who ultimately receive a preemptive kidney transplant, on average, spend 1 year on the kidney transplant waiting list (1). The benefits of preemptive placement on the transplant waiting list are also significant and include initiating conversations about potential living donors, addressing modifiable contraindications to transplant early, accruing waiting time and priority under the current US kidney allocation policy to receive donor offers, and possibly improving mental health.
Median graft survival of deceased and living kidney donor transplants is 11.7 years and 19.2 years, respectively; however, 5% of patients in the United States initiating dialysis treatment for ESKD do so after a failed transplant (2–4). Repeat kidney transplantation in patients with failing kidney allografts is associated with improved survival outcomes and better quality of life than returning to dialysis (5,6). Surprisingly, even though a significant number of patients with a failing transplant are under the care of a transplant center or general nephrologist and stand to benefit from early referral, rates of preemptive waitlist placement and repeat transplantation are low (7). Furthermore, the pervasive inequities that exist for processes of care and access to primary preemptive kidney transplantation persist for access to repeat preemptive kidney transplantation (8,9).
The findings by Vinson et al. in this issue of Kidney360 provide a contemporary cohort analysis of adult recipients over an 18-year period, demonstrating that access to preemptive kidney transplantation (cases of both primary and repeat transplant) occur only in the minority of patients and are plagued with inequities by race, sex, and socioeconomic and comorbid status (10). Over the years studied, they report the cumulative incidence of preemptive repeat kidney transplant was lower than for preemptive primary transplant (15% versus 19%). The odds of repeat preemptive kidney transplant among patients who were Black, Hispanic, men, unemployed, and less educated were lower compared with those who were White, women, employed, and received graduate school education. Notably, Vinson et al. found that patients who received a preemptive primary kidney transplant were twice as likely to receive a preemptive repeat kidney transplant, suggesting individual patient characteristics are strongly associated with the likelihood of either primary or repeat preemptive transplant. The study highlighted that a majority of both preemptive primary and repeat kidney transplants were from living donors. In addition, results indicated a higher incidence of preemptive repeat kidney transplant for patients who received post-transplant care at a specialty transplant center or from a kidney physician compared with those who received primary care only (8%–12% versus 6%).
On the basis of the evidence of this study, combined with prior research that evaluated the incidence and variation of preemptive transplantation, what are the lessons learned, and how can we intervene most effectively? Of primary concern, despite robust long-standing evidence confirming the benefits of preemptive transplantation, still today only the minority of patients are waitlisted or receive a transplant before dialysis. As evidenced in this study, this includes patients with a failed kidney transplant who have already successfully navigated the process to receive an initial transplant and who often receive longitudinal care from a transplant center. Although clearly some patients with a failing transplant may not be viable candidates for repeat transplantation, these results suggest that some combination of patient and center characteristics lead to suboptimal care for a large cohort of patients. Patients with failing and failed kidney transplants represent a unique subpopulation of patients with ESKD due to the accumulation of medical comorbidities related not only to prolonged dialysis and transplant vintage, but also to long-term exposure to immunosuppression. The current results seem to suggest that the focus of care in the post-transplant setting may mimic the same downstream barriers to care that patients with native advanced chronic kidney disease face to preemptive kidney transplant.
Stable transplant recipients may often transition to community nephrology care. Therefore, the focus on longer-term needs such as repeat transplantation may become less of a priority in the day-to-day care processes for transplant centers. Some transplant centers that have a codified process for initial transplant listing may fail to develop and apply screening protocols to determine eligibility for repeat transplant candidacy, thus leading to delays in referrals and evaluations. Post-transplant care protocols may also omit continuous patient education about the potential loss of transplant function, in lieu of prolonging the life of the transplant or focusing attention on immunosuppression modification or other medical complications of advanced transplant dysfunction.
The comprehensive evidence to date suggests that particularly given the high morbidity and mortality for patients on return to dialysis, timely, objective, and effective interventions to initiate assessment for repeat candidacy are critically needed. These interventions are likely to both improve outcomes and be cost-effective. Importantly, the identification and processes for re-listing patients should not be particularly burdensome. Information to identity patients with eGFRs that would qualify without clear contraindications and a desire for a repeat procedure should be readily attainable. Use of objective flags or other automated notes in medical charts to identify patients who may qualify for repeat listing may be effective in expediting these processes.
The fact that similar patient groups are largely disadvantaged in access to preemptive repeat as primary kidney transplantation signals a call to action by the kidney community to understand and disrupt the systemic factors that explain these pervasive disparities. We must understand the mechanisms underlying these inequities because access to repeat kidney transplant is another critical reflection of disparities across the entire spectrum of kidney disease. From a policy perspective, preemptive referral, evaluation, and waitlisting should be measured and highly incentivized for both repeat and primary preemptive kidney transplantation. (Re)transplant needs to reach a threshold of importance, especially within a population of patients who have already successfully navigated the kidney transplant process. Unfortunately, the emphasis of quality assurance and accountability in the field of transplantation is focused primarily on transplants that occur. In contrast, “missed opportunities” to facilitate care for patients who would benefit from transplantation are largely unmeasured and unrecognized.
Importantly, rates of preemptive repeat waitlisting and repeat kidney transplant significantly vary by transplant center (7). In addition, center-level variation in rates of preemptive primary listing is not strongly correlated with rates at repeat transplantation. As displayed in Figure 1, the rates of preemptive (both primary and repeat) vary substantially among adult kidney transplant centers, suggesting that best practices may be identified by centers with higher rates. In addition, the lack of correlation between these rates may suggest that center processes of care and emphases for preemptive care for initial transplant may differ from repeat transplantation. Cumulatively, the center-level variation suggests that there are opportunities to improve care delivery to potential repeat transplant candidates and develop structured guidelines or automated referral processes for patients being closely followed within transplant centers.
Figure 1.
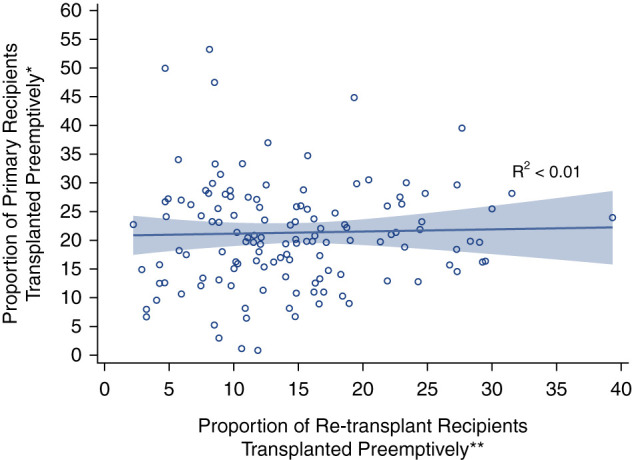
Comparison of proportion (%) of preemptive primary kidney transplant recipients and preemptive repeat kidney transplant recipients by transplant center. Each “o” represents a single transplant center). *Limited to centers with at least 30 primary transplants between 2015 and 2021; two centers with no preemptive transplants not shown. **Limited to centers with at least 30 repeat transplants between 2015 and 2021; 32 centers with no preemptive repeat transplants not shown.
Overall, the study by Vinson et al. highlights an important component of transplant care delivery that, despite the large number of patients affected, has largely been understudied (10). Efforts to improve care for potential repeat candidates can be addressed and likely must incorporate interventions at the center level and policies that focus on attenuating disparities and expediting care. A key perspective for our collective interventions and policies is to remain focused on the overall patient lifetime rather than solely the graft life of an individual transplant. With this focus, consideration of long-term care planning, preparation for potential graft failure, and early communication with patients regarding the potential for re-transplantation are important. Further research to address patient-centric care and to improve the quality of life of the ESKD population is critically needed in our field.
Disclosures
A. Huml reports membership of Cleveland MOTTEP Advisory Board, is a chairperson for IPRO ESRD Network of the Ohio River Valley Medical Review Board, is a member of the Medical Director Advisory Council for The National Forum of ESRD Networks, and has other interests/relationships with Cleveland Kidney Precision Medicine Project (KPMP) Community Advisory Board. J. Schold reports consultancy agreements with Guidry and East, Novartis, Sanofi Corporation, and Transplant Management Group; honoraria from Novartis and Sanofi; is a Board Member of the Data Safety Monitoring Board Member—Bristol Myers Squibb and Nephrosant; and participates in a speakers’ bureau for Sanofi.
Funding
None.
Acknowledgments
The content of this article reflects the personal experience and views of the authors and should not be considered medical advice or recommendation. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the authors.
Footnotes
See related article, “Disparities in Access to Preemptive Repeat Kidney Transplant: Still Missing the Mark?,” on pages 144–152.
Author Contributions
A. Huml and J. Schold conceptualized the study, wrote the original draft of the manuscript, reviewed and edited the manuscript. J. Schold undertook the formal analysis.
References
- 1.King KL, Husain SA, Jin Z, Brennan C, Mohan S: Trends in disparities in preemptive kidney transplantation in the United States. Clin J Am Soc Nephrol 14: 1500–1511, 2019. 10.2215/CJN.03140319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poggio ED, Augustine JJ, Arrigain S, Brennan DC, Schold JD: Long-term kidney transplant graft survival—Making progress when most needed. Am J Transplant 21: 2824–2832, 2021. 10.1111/ajt.16463 [DOI] [PubMed] [Google Scholar]
- 3.Messa P, Ponticelli C, Berardinelli L: Coming back to dialysis after kidney transplant failure. Nephrol Dial Transplant 23: 2738–2742, 2008. 10.1093/ndt/gfn313 [DOI] [PubMed] [Google Scholar]
- 4.United States Renal Data System : 2013 USRDS Annual Data Report: Atlas of Chronic Kidney Disease and End-stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2013 [Google Scholar]
- 5.Rao PS, Schaubel DE, Wei G, Fenton SS: Evaluating the survival benefit of kidney retransplantation. Transplantation 82: 669–674, 2006. 10.1097/01.tp.0000235434.13327.11 [DOI] [PubMed] [Google Scholar]
- 6.Rao PS, Schaubel DE, Jia X, Li S, Port FK, Saran R: Survival on dialysis post-kidney transplant failure: Results from the Scientific Registry of Transplant Recipients. Am J Kidney Dis 49: 294–300, 2007. 10.1053/j.ajkd.2006.11.022 [DOI] [PubMed] [Google Scholar]
- 7.Schold JD, Augustine JJ, Huml AM, O’Toole J, Sedor JR, Poggio ED: Modest rates and wide variation in timely access to repeat kidney transplantation in the United States. Am J Transplant 20: 769–778, 2020. 10.1111/ajt.15646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Purnell TS, Crews DC: Persistent disparities in preemptive kidney transplantation. Clin J Am Soc Nephrol 14: 1430–1431, 2019. 10.2215/CJN.09800819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reese PP, Mohan S, King KL, Williams WW, Potluri VS, Harhay MN, Eneanya ND: Racial disparities in preemptive waitlisting and deceased donor kidney transplantation: Ethics and solutions. Am J Transplant 21: 958–967, 2021. 10.1111/ajt.16392 [DOI] [PubMed] [Google Scholar]
- 10.Vinson AJ, Kiberd BA, West K, Mannon RB, Foster BJ, Tennankore KK: Disparities in access to preemptive repeat kidney transplant: Still missing the mark? Kidney360 3: 144–152, 2022. 10.34067/KID.0003162021 [DOI] [PMC free article] [PubMed] [Google Scholar]


