ABSTRACT
Insufficient vaccine coverage and dominance of the more transmissible severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants are the leading causes of the continued spread of coronavirus disease 2019 (COVID-19) worldwide. To curb the surge in infections, COVID-19 vaccination has been advocated as a priority measure, especially for frail populations and people at high risk of exposure. Patients on in-centre maintenance haemodialysis (HD) embody both conditions. They are at high risk of severe COVID-19 consequences due to their advanced age and weakened immune system and carry an increased risk of SARS-CoV-2 transmission within shared dialysis rooms and public vehicles. Vaccination of the entire HD population is therefore the most effective strategy to protect patients from the dire consequences of COVID-19. Unfortunately, a minority of patients still express COVID-19 vaccine hesitancy. The management of this group of patients, who have the full right to HD treatment, poses demanding problems from a patient safety perspective. The placement of unvaccinated patients within the dialysis room and the protection of all vaccinated patients are some of the most urgent problems the nephrologist faces during the COVID-19 pandemic. In light of these COVID-19-driven changes, an ethical reflection on the management of unvaccinated patients appears crucial to act responsibly and contribute to the health promotion of dialysis patients.
Keywords: COVID-19, dialysis, ethics, haemodialysis, screening, vaccine
‘Why do I need another nasal swab if I am asymptomatic?’ claimed a patient on maintenance dialysis before starting the dialysis session. ‘The reasons are simple enough to comprehend. You returned from a holiday dialysis centre without a recent negative COVID-19 test’, replied the doctor. ‘Furthermore, if I am not mistaken, you are also unvaccinated’, the doctor said, speaking to the patient from the other side of the dialysis bed.
This scenario represents one of the many cross-sections of daily life in a haemodialysis (HD) unit during the time of coronavirus disease 2019 (COVID-19). Testing for COVID-19 and anti-COVID vaccination have become the main interventions for the prevention of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Negative COVID-19 testing, regardless of adherence to vaccination, is a critical prerequisite when uninfected HD patients move between dialysis units. Generally, each dialysis centre demands proof of negative testing within 48–72 h before their arrival, which means tests are required on the way to and the way back from another unit. Similar regulations are applied for domestic and international travel, according to the country’s requirements. For instance, people are allowed to board an aircraft or ship if they show proof of a recent negative COVID-19 test. For residents undergoing vaccination, a ‘vaccine passport’ certificate has been issued. This ‘green pass’ allows the possessors, in the absence of symptoms, to access otherwise restricted indoor places such as restaurants, museums, gyms and hotels. The first countries that embraced this policy were Israel and Italy. In Italy, the green pass is now mandatory for all private and public sector employees to continue working unless they provide proof of negative COVID-19 test results performed within 48 (antigenic test) or 72 h (molecular test).
The proposal for the green pass evolved from the generalized desire to return to normality after a long period of social restriction while attempting to limit the spread of COVID-19 by incentivizing vaccination uptake. However, although the green pass has encouraged some hesitant individuals, not everyone is willing to be vaccinated [1]. For this group of people, entry to certain locations and benefits of a gradual easing of COVID-19 restrictions continue to be forbidden.
Likewise, many activities of unvaccinated patients on chronic HD may be further limited by the lack of a green pass. An exception is the delivery of lifesaving treatments such as in-centre HD. Given these circumstances, the question that arises is ‘How should dialysis units approach unvaccinated in-centre HD patients given that they have a right to and require regular treatment?’
Dialysis units are small communities that have been exposed to undue risk from COVID-19. Per-population cases and deaths among dialysis patients have exceeded the general population by 100-fold in some countries [2]. It is universally acknowledged that in-centre HD patients have an increased risk of SARS-CoV-2 transmission because they share dialysis, waiting and dressing rooms as well as dialysis transportation services with other patients [3]. Furthermore, these patients show increased susceptibility to severe COVID-19 due to their advanced age and weakened immune system [4]. These conditions also impact the efficacy of the vast vaccination campaign launched in high- and upper-middle-income countries, since dialysis patients might remain wholly or partially unprotected by a standard cycle of COVID-19 vaccination.
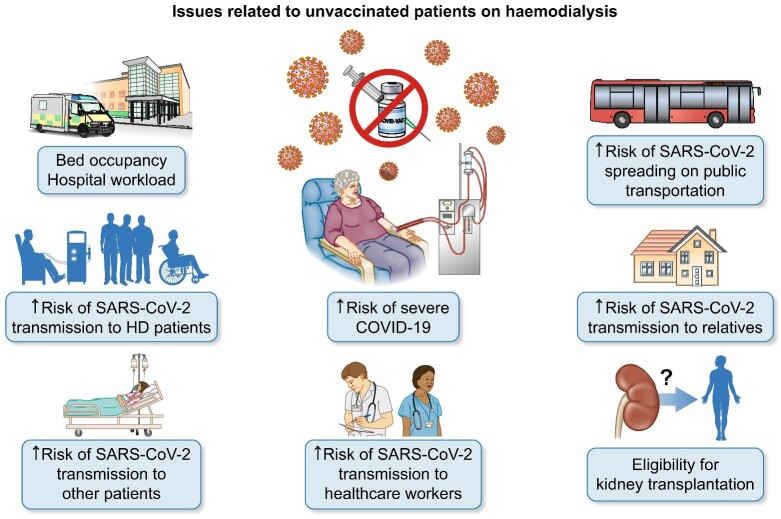
Hence, whereas some HD patients are willing to mitigate the risk of SARS-CoV-2 infection with a third booster dose [5], a minority of patients (∼3% in our centre) still express uncertainty about vaccination. This proportion, although numerically small, poses significant logistic and ethical difficulties in the management of these patients (Figure 1). On the one hand, unvaccinated patients have the full right to access healthcare, including HD. On the other hand, other patients and healthcare workers also have a right to be protected from an unvaccinated person who may pose a health risk to them. In the absence of a satisfactory solution, here we discuss various ethical considerations arising around the challenging placement of these patients within the dialysis unit, an issue that requires urgent deliberation (Table 1).
FIGURE 1:
Practical issues related to the unvaccinated patients on in-centre maintenance haemodialysis.
Table 1.
Ethical concerns in the management of in-centre HD patients with COVID-19 vaccine hesitancy
| Issues | Ethical concerns |
|---|---|
| Placement of unvaccinated patients within the dialysis unit | Discrimination |
| Isolation of unvaccinated patients | High risk of COVID-19 outbreak |
| Breaches of privacy and confidentiality | |
| Mix of unvaccinated and vaccinated patients within the same room | Unprotection of vaccinated patients |
| Miscellaneous | |
| Transportation | Unprotection of the driver and vaccinated patients |
| Access to the dialysis unit | Unprotection of healthcare workers |
| Access to health services other than dialysis | Unprotection of vaccinated patients and healthcare workers |
| Waiting list for kidney transplantation | Poor medication adherence |
One potential solution may appear to be gathering all patients who refuse vaccination in a separate room as is current practice for hepatitis B virus–positive patients. In this way, vaccinated patients would be somewhat shielded from the risk of contagion from unvaccinated patients. Although this solution appears logistically fair, it does not act in the best interest of the patient and contrasts with the principle of prioritizing patient's safety for the following reasons:
Patients who are reluctant to be vaccinated are extremely vulnerable to COVID-19. Gathering all unvaccinated patients in one room may increase the risk of SARS-CoV-2 transmission among the most vulnerable and may have disastrous consequences in case of a COVID-19 outbreak.
The lack of immunization against COVID-19 does not mean SARS-CoV-2 infection and therefore cannot be compared to a communicable infectious disease such as hepatitis B. This implies that confining measures are unnecessary for unvaccinated individuals without COVID-19.
Isolation may be perceived as unfair discrimination against people who deny vaccination. Confining unvaccinated patients could also jeopardize the confidentiality of the vaccination status, which instead should be guaranteed as much as possible, especially for unvaccinated people with personal or religious objections.
A fairer solution may therefore be to mix unvaccinated with vaccinated HD patients while all shield appropriately with masks, handwashing and distancing. In order to achieve a somewhat local herd immunity threshold, physicians may take into account the immunological response of the other patients in the room. In addition, to offer the best standard of care and reduce the risk of COVID-19 spread, unvaccinated patients would be required to undergo frequent testing. In parallel with the green pass regulation, COVID-19 testing may be performed, in a high-resource setting, every 48–72 h, which will coincide approximately with each dialysis session.
In conclusion, the management of unvaccinated patients in dialysis units imposes a series of ethical challenges that are not easy to resolve. No clear indications exist on the best way to protect vaccinated HD patients from unvaccinated ones and vice versa in terms of timing and modality (antigenic or molecular test) of anti-COVID-19 screening. Patient education should be encouraged because it has been shown to be an effective tool in increasing vaccine acceptance. However, in the meantime, as educational interventions yield positive results and herd immunity nears, frequent testing of unvaccinated patients may be a temporal solution to reduce the risk of COVID-19 transmission within dialysis units.
ACKNOWLEDGEMENTS
Special thanks are due to Prof. Valerie Luyckx for her ability to communicate the beauty of ethics.
Contributor Information
Gaetano Alfano, Nephrology, Dialysis and Transplant Unit, University Hospital of Modena, Modena, Italy; Clinical and Experimental Medicine PhD Program, University of Modena and Reggio Emilia, Modena, Italy.
Francesco Fontana, Nephrology, Dialysis and Transplant Unit, University Hospital of Modena, Modena, Italy.
Niccolò Morisi, Surgical, Medical and Dental Department of Morphological Sciences, Section of Nephrology, University of Modena and Reggio Emilia, Modena, Italy.
Giacomo Mori, Nephrology, Dialysis and Transplant Unit, University Hospital of Modena, Modena, Italy.
Gianni Cappelli, Nephrology, Dialysis and Transplant Unit, University Hospital of Modena, Modena, Italy; Surgical, Medical and Dental Department of Morphological Sciences, Section of Nephrology, University of Modena and Reggio Emilia, Modena, Italy.
Riccardo Magistroni, Nephrology, Dialysis and Transplant Unit, University Hospital of Modena, Modena, Italy; Surgical, Medical and Dental Department of Morphological Sciences, Section of Nephrology, University of Modena and Reggio Emilia, Modena, Italy.
Gabriele Donati, Nephrology, Dialysis and Transplant Unit, University Hospital of Modena, Modena, Italy; Surgical, Medical and Dental Department of Morphological Sciences, Section of Nephrology, University of Modena and Reggio Emilia, Modena, Italy.
AUTHORS’ CONTRIBUTIONS
All authors critically reviewed and approved the manuscript in its final form.
FUNDING
None.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest. This article has not been published previously in whole or part.
REFERENCES
- 1. Wilf-Miron R, Myers V, Saban M. Incentivizing vaccination uptake: the “green pass” proposal in Israel. JAMA 2021; 325: 1503–1504 [DOI] [PubMed] [Google Scholar]
- 2. Robinson BM, Guedes M, Alghonaim M et al. Worldwide early impact of COVID-19 on dialysis patients and staff and lessons learned: a DOPPS roundtable discussion. Kidney Med 2021; 3: 619–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alfano G, Ferrari A, Magistroni R et al. The frail world of haemodialysis patients in the COVID-19 pandemic era: a systematic scoping review. J Nephrol 2021; 34: 1387–1403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Combe C, Kirsch AH, Alfano G et al. At least 156 reasons to prioritize COVID-19 vaccination in patients receiving in-centre haemodialysis. Nephrol Dial Transplant 2021; 36: 571–574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dekervel M, Henry N, Torreggiani M et al. Humoral response to a third injection of BNT162b2 vaccine in patients on maintenance haemodialysis. Clin Kidney J 2021; 14: 2349–2355 [DOI] [PMC free article] [PubMed] [Google Scholar]