Abstract
Introduction
Intravenous (IV) insertions are among the most performed procedures for children seeking medical care; they are often a painful and stressful experience for both children and their caregivers. Paediatric distress and pain that is inadequately treated may lead to a frightened and uncooperative child, repeated IV attempts and overall frustration with care for both the family and clinical team. We hypothesise that distraction via an immersive virtual reality (VR) experience may reduce the associated distress for children undergoing IV insertions.
Methods and analysis
This two-armed randomised controlled superiority trial will be conducted in a Canadian paediatric emergency department and will aim to enrol 80 children overall. Children will be randomised to receive either departmental standard of care alone or standard of care plus an immersive VR experience. Children 6–17 years of age who are undergoing IV insertion and have topical anaesthetic application will be considered for inclusion. Our primary objective is to compare the reduction of distress between the two study arms. The primary outcome will be the child’s observed distress score as measured by the Observational Signs of Behavioral Distress-Revised tool. Secondary outcomes include the child’s pain intensity and fear, parental anxiety, satisfaction with the IV procedure, as well as adverse events. Recruitment launched in September 2020 and is expected to end in March 2022.
Ethics and dissemination
This study has been approved by the Health Research Ethics Board (University of Alberta). Informed consent will be obtained from parents or guardians, and assent from children. Study data will be submitted for publication irrespective of results. This study is funded through a Women and Children’s Health Research Institute Innovation grant. Purchase of the VR equipment was facilitated through a Stollery Children’s Hospital Foundation small equipment grant.
Trial registration number
NCT04291404Cite Now
Keywords: ACCIDENT & EMERGENCY MEDICINE, Pain management, Paediatric A&E and ambulatory care, PAIN MANAGEMENT
Strengths and limitations of this study.
This randomised controlled trial will assess the effectiveness of immersive virtual reality-based distraction for the reduction of intravenous insertion-related distress in children.
This study measures patient-relevant and family-relevant outcomes including child distress, pain, fear and safety, as well as parental anxiety and satisfaction.
The study team includes parent and patient partners as co-investigators who will inform study methods and outcomes.
The study intervention will be compared with current standard of care; however, since there is no consistent standard of care distraction practice, this may create some heterogeneity in the comparison arm of the study.
Given the nature of the study intervention, it is not possible to blind patients, parents/caregivers, healthcare providers or outcome assessors; the statistician will be blinded to study arms.
Introduction
Needle procedures, including venipuncture and intravenous (IV) placement, are described by children as some of the most distressing and painful parts of their healthcare visit.1–4 Untreated distress and pain can lead to a scared and uncooperative child, a need for repeated IV attempts, reduced efficiency and overall dissatisfaction with care for the patient, family and the healthcare team.3 5 6 Unpleasant medical encounters in childhood can also shape an individual’s perception of healthcare and expectations of pain in adulthood.7–9 This can result in increased anticipatory anxiety and pain for future medical procedures or an avoidance of healthcare services, altogether.1 As needle procedures form a routine and necessary part of care in the emergency department (ED), it is an important responsibility of healthcare providers to adequately manage children’s distress and pain, wherever possible.10 11
The recommended and responsible approach to managing children’s procedural pain incorporates physical, psychological and pharmacological components.10–15 While pharmacological interventions such as topical anaesthetic creams are available, their effectiveness is limited to pain, as they do not address procedure-related distress and anxiety.10 Distraction therapy is a commonly employed psychological strategy which involves engaging children in a cognitive task or activity to divert attention away from nociceptive stimuli.16 An effective distractor provides sensory stimulation and is highly engaging and age appropriate to fully capture the attention of a child.12 16 Previous research has indicated that children who use distraction as an active form of coping experience reduced pain and distress during painful procedures.12 17 18 Traditional distraction techniques such as music, video, stories, imagery and focused breathing have been previously explored for children undergoing unpleasant medical procedures and demonstrated mixed results.19–24 Our team’s recently conducted systematic review of digital technologies has suggested that digital distraction techniques appear promising, but require further study to confirm their utility for painful procedures.25
Virtual reality (VR) technology is rapidly emerging as a novel distraction tool for children undergoing various medical procedures. Unlike traditional distraction techniques, VR uses a combination of visual, auditory and tactile stimuli to create the illusion of being fully immersed in an artificial three-dimensional (3D) environment.26 A head-mounted display (or ‘VR goggles’) delivers the VR video and audio to the child, and serves to block out the view and sounds of the hospital room.14 This further removes the patient from the chaos of the treatment room and diverts their attention away from surrounding painful and anxiety-evoking stimuli. To date, VR distraction therapy has shown promise for patients undergoing a range of distressing healthcare procedures, including burn wound cleaning, chest radiography, dental interventions and chemotherapy.27–32 Therapeutic VR has also led to improved health outcomes for patients with anxiety disorders, phobias, post-traumatic stress disorder and eating disorders.33–36
The ED presents unique challenges when attempting to distract a child during a painful medical procedure. Due to the chaotic, noisy and unpredictable environment, it is an ideal place to ‘stress-test’ the ability of VR technology to immerse a child into a distracting and ‘safe’ space. Rapid advances in VR technology over the last few years, and improved cost-effectiveness, offer a unique opportunity to explore its use in the ED setting. A few recently published studies from the paediatric ED setting suggest that VR has a positive impact on IV insertion-related pain and satisfaction,12 14 37–40 although outcomes such as distress and adverse effects remain poorly studied.38 Recent systematic reviews, which have mostly focused on non-ED and inpatient settings, have shown that the current evidence is inconclusive, sometimes contradictory, and have called for further research in larger study groups.41 42 Furthermore, many previous trials use proprietary software designed specifically for medical use which may limit widespread accessibility to all centres. This study will evaluate an ‘off-the-shelf’ device with a range of widely accessible software.
This study will evaluate the effectiveness of a VR intervention in reducing IV placement-related distress for children 6–17 years old presenting to the ED. We hypothesise that the use of immersive VR distraction will reduce children’s IV-related distress when compared with standard of care and will improve overall satisfaction with the procedure for the patient, family and the healthcare team.
Methods and analysis
This study is a two-armed, randomised controlled superiority trial. The study protocol is reported using the Standard Protocol Items : Recommendations for Interventional Trials- Patient Reported Outcomes (SPIRIT-PRO) reporting guidelines43 (see table 1).
Table 1.
WHO trial registration dataset
| Data category | Information |
| Primary registry and trial identifying number | clinicaltrials.gov NCT04291404 |
| Date of registration in primary registry | 2 March 2020 |
| Secondary identifying numbers | University of Alberta Research Ethics Board # Pro00095418 |
| Source(s) of monetary or material support | Stollery Children’s Hospital Foundation and the Women and Children’s Health Research Institute Innovation grant |
| Primary sponsor | University of Alberta |
| Secondary sponsor(s) | – |
| Contact for public queries | Dr Samina Ali 780.248.5575 sali@ualberta.ca |
| Contact for scientific queries | Dr Samina Ali 780.248.5575 sali@ualberta.ca |
| Public title | The Virtual Reality Trial |
| Scientific title | A randomised controlled trial of virtual reality-based distraction for intravenous insertion-related distress in children |
| Countries of recruitment | Canada |
| Health condition(s) or problem(s) studied | Intravenous (IV) insertion-related distress |
| Intervention(s) | Addition of distraction via an immersive virtual reality experience to departmental standard of care during the IV insertion procedure |
| Key inclusion and exclusion criteria | To be eligible to participate in this study, an individual must meet all of the following inclusion criteria: (a) child aged 6–17 years; (b) requires IV placement; and (c) will receive topical anaesthetic cream for IV placement. Children meeting any of the following criteria will be excluded: (a) medically unstable; (b) unconscious or not fully alert; (c) visual, auditory cognitive or mental health issues precluding safe interaction with the VR intervention; (d) conditions that could be exacerbated by the VR environment, such as current symptomatic nausea/vomiting/dizziness/migraine, or a history of psychosis/hallucinations/epilepsy; (e) presence of an infection/injury which could contaminate the VR intervention equipment such as open wounds/infections of the head and neck area, or suspected/confirmed methicillin-resistant Staphylococcus aureus colonisation; (f) screens positive for ‘influenza-like illness’ as per departmental screening criteria; (g) language barrier precluding the ability to understand and complete study assessments, in the absence of a native language translator; or (h) previous enrolment in this study. |
| Study type | Randomised controlled superiority trial |
| Date of first enrolment | 5 October 2020 |
| Sample size | 80 |
| Recruitment status | Actively recruiting |
| Primary outcome(s) | The primary outcome will be the child’s total observed distress score during the IV procedure as measured on the Observational Signs of Behavioral Distress-Revised tool. |
| Key secondary outcomes | Secondary outcomes include: (a) the child’s self-reported pain score during the IV procedure, using an 11-point 0–10 verbal Numerical Rating Scale); (b) the child’s self-reported fear score during the IV insertion as measured by the Children’s Fear Scale; (c) parental/caregiver anxiety associated with the procedure, as assessed by the State Trait Anxiety Inventory–State Trait Revised Version; (d) satisfaction with the procedure for the child, their parent/caregiver and the nurse inserting the IV, as assessed by a 5-point Likert scale; and (e) the proportion of children who experience adverse events related to the study intervention. |
| Ethics review | University of Alberta Research Ethics Board # Pro00095418 |
| Completion date | – |
| Summary results | – |
| Individual Participant Data (IPD) sharing statement | De-identified data can be shared, on a case-by-case basis, upon discussion with the principal investigator. |
Setting and study period
This study will be conducted in the Stollery Children’s Hospital (SCH) ED in Edmonton, Alberta, Canada. The SCH is a tertiary care hospital whose annual ED census is typically approximately 60 000. The 2020 ED census for the SCH was reduced to 36 899 due to the COVID-19 pandemic. Recruitment launched in September 2020 and is expected to end in March 2022. Based on our team’s previous experience conducting research in this setting, and considering the ongoing pandemic-related considerations, we anticipate 18 months of recruitment to meet our overall target of 80 patients.
Eligibility and exclusion criteria
Children will be eligible if they are 6–17 years, require an IV placement during their ED visit and have received topical anaesthetic cream for their IV placement. This age group was chosen as they can reliably self-report pain and are expected to benefit from the VR study intervention, based on prior studies.44 Due to ethical and pragmatic considerations, we insisted that children must be receiving topical anaesthetic cream for IV placement to be eligible for our study, as it is effective and considered standard of care within our hospital.10 Exclusion criteria are detailed in table 1.
Study intervention and comparison
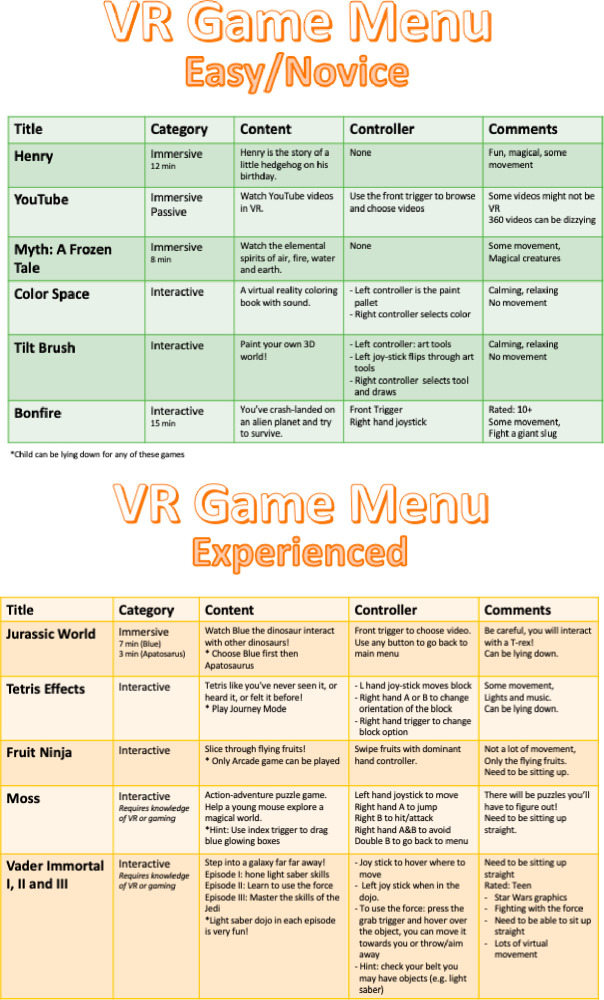
The intervention will include the use of an immersive VR application that will engage children for the duration of the IV procedure. The VR intervention will be provided in addition to standard of care. The child will wear the VR goggles (Oculus Quest, Oculus, Facebook Technologies; see figure 1) and small handheld controllers (optional) can be used to interact with the virtual environment and change settings. The VR goggles will occlude the patient’s view of the treatment room, and a pair of noise-cancelling headphones (optional) can be used to block out ambient hospital sounds. Together, this will provide the child with a unique vivid experience of being fully immersed or ‘present’ inside the 3D virtual world. The child will be presented with one of two VR menu options, one for novice users and another for more experienced users. The menus will have preselected VR applications that are suitable for use during the IV procedure and will include a combination of interactive games and immersive 3D movies designed specifically for a VR experience (see figure 2). The choice of applications was based on consultation with the SCH Youth Advisory Committee prior to commencing the study. The shortlisted applications were then tested by the principal investigators, other team members and youth. The research assistant (RA), who will be trained in proper equipment use and troubleshooting, will help the child with selecting and running the VR game/movie. Based on child and nursing preference, children may either sit up or lie in a supine position for the duration of the procedure. The chosen VR games will not require the child to move their torso or both arms, to not interfere with the IV placement. The VR goggles can be removed at any time during the procedure if the child so desires. The game/application selected by the child will be recorded on the case report form.
Figure 1.

Child using virtual reality goggles in the emergency department.
Figure 2.
Virtual reality (VR) game menus.
The control group will receive departmental standard of care which will include topical anaesthetic cream (mandatory for inclusion in the study) and may include parent/caregiver support, child life services, nursing support, and other support strategies at the discretion of the ED clinical care team and the family. Child life services include preprocedural education, distraction and coaching, intraprocedural presence, and post-procedural support and prizes. At present, there is no single established distraction therapy or routine that is consistently employed for IV procedures within our ED. Thus, for pragmatic and ethical considerations, it is felt that the new study VR intervention should be compared with what is currently already in practice (ie, standard of care). Generally, VR technology is not employed by the nursing staff for distracting the child. However, other forms of technology (ie, smart phones, tablets) will not be prohibited in the control group if the family chooses to offer them. Use of other devices and distraction techniques will be documented.
Randomisation, allocation concealment and blinding
Randomisation will be determined using an online randomisation tool hosted on the REDCap45 (Research Electronic Data Capture) platform. Following documentation of informed consent and assent, the RA will obtain the computer-generated randomised assignment for the child by clicking on the ‘Randomise’ button within the study-specific REDCap case report form. Allocation will be concealed from the research staff, ED clinical staff and the family until this point. However, due to the nature of the intervention, it is not possible to maintain blinding once the child has been randomised.
Children and their parents/caregivers will be informed that the study will evaluate and compare different forms of distraction, however they will not be made aware of the study hypothesis for the VR intervention. Furthermore, the statistician will be blinded to treatment assignment by using randomisation codes until data analysis is complete.
Recruitment and data collection
Participant recruitment will occur in the SCH ED when RAs are on-site, from approximately 15:00 to 23:00 daily. Based on our team’s previous research, this time frame corresponds with peak ED volume. RAs will screen the electronic ED track board and communicate with on-site clinical staff to identify potentially eligible patients. The RA will then further assess eligibility based on the inclusion/exclusion criteria detailed above. If the child is deemed eligible and the family is willing to participate, the RA will obtain written informed consent from the parent/ caregiver and assent from the child (see online supplemental appendix 1). One parent/caregiver for each child will be asked to provide consent and complete all relevant study questionnaires.
bmjopen-2021-057892supp001.pdf (11.9MB, pdf)
Prior to the beginning of the IV procedure, the RA will collect baseline information, including: baseline heart rate, preprocedure distress, fear and pain scores from the child, and preprocedure anxiety score from the parent/caregiver. The RA will then access the randomisation tool on REDCap to reveal the child’s group assignment (VR intervention or control).
For the VR intervention group, the RA will set up the VR equipment and spend approximately 5–10 min explaining the intervention to the child, including proper use of the goggles and controller. The RA will then help the child put on and secure the goggles and headphones, and hand them the controller. They will document the time required for equipment set-up as well as any technical challenges encountered. As per hospital infection-control policy, all VR equipment including the goggles, headphones and controller will be sanitised with disinfectant wipes between participants. A disposable one-time use cover will be placed on the goggles for each participant. For all participants (both study arms), the RA will begin video recording the child 5 min prior to the start of the procedure and continue until 5 min post-procedure, to allow for complete coding of Observational Signs of Behavioral Distress-Revised (OSBD-R) distress scores at a later time.
For all participants (both study arms), the staff nurse will insert the IV following institutional protocol. In keeping with the pragmatic design of the trial, no additional or study-specific instructions will be provided to either nurses or parents/caregivers regarding their behaviour during the procedure. For purposes of the study, the start of the IV insertion procedure will be marked by the cleaning of the IV site by the staff nurse. The end of the procedure will be defined by the last point of contact by the staff nurse (ie, taping cannula in place with or without arm board, wrapping arm with gauze and taping the gauze in place).
During the procedure, the RA will closely monitor the child for any adverse effects. The child will also be asked to let the team know immediately if they are experiencing any adverse events or discomfort related to the VR intervention (ie, dizziness, nausea, headache). The VR intervention can be discontinued (ie, the headset can be removed) at any time, at the discretion of the child or clinical team. If an adverse event were to occur, the clinical team will be notified, and details will be logged in the REDCap adverse event log. Additionally, the RA will make a note of any technical failures or issues associated with the VR equipment during enrolment.
Immediately following the first attempt at IV placement (regardless of whether it was successful), the RA will collect post-procedure distress, fear and pain scores from the child, and post-procedure anxiety score from the parent/caregiver. A few minutes after completion of the IV placement, satisfaction and acceptability questionnaires will be completed with the child, parent/caregiver as well as the staff nurse responsible for inserting the IV. Five minutes after the procedure is completed, the RA will stop the video recording. The duration of the procedure and total number of IV attempts will be documented. If the first attempt at placement is unsuccessful, any additional attempts will occur after all relevant study questionnaires/measurements have been completed.
Demographic information, history and visit details will also be collected from the family and the child’s medical chart (see figure 3 for study flow schematic).
Figure 3.
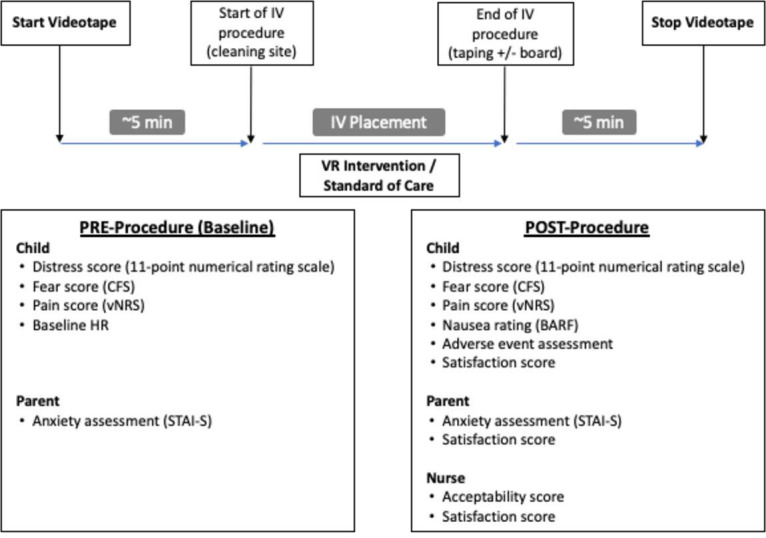
Flow diagram of study procedures. OSBD-R coding of videos will be done by RAs post-visit. BARF, Baxter Retching Faces; CFS, Children’s Fear Scale; HR, heart rate; IV, intravenous; OSBD-R, Observational Scale of Behavioral Distress-Revised; RAs, research assistants; STAI-S, State Trait Anxiety Inventory–State Scale Revised Version; vNRS, verbal Numerical Rating Scale; VR, virtual reality.
Outcome measures
Our primary outcome is distress. Our secondary outcomes are (a) pain; (b) fear; (c) the parental/caregiver anxiety; and (d) parental/caregiver and nurse satisfaction with the procedure in the intervention; and (e) safety.
Our primary outcome measure will be the child’s total distress score during the IV procedure. Distress associated with the procedure will be assessed using the OSBD-R. The OSBD-R is a validated scale that is widely used to measure pain and distress associated with various medical procedures in children.46–48 The tool assesses eight specific behaviours that are indicative of distress and are weighted according to intensity: information seeking, crying, screaming, restraint, verbal resistance, emotional support, verbal pain and flailing. Study participants will be videotaped for the duration of the IV procedure as well as for a few minutes before and after; distress will be scored preprocedure, during and post-procedure. Two RAs who are trained in the use of the tool will independently observe the videotapes and record the frequency of each of the eight behaviours during continuous 15-second intervals. To ensure high inter-rater reliability, the first 10% of coded videos will be analysed for inter-rater reliability and RAs will be provided with feedback and retraining, as needed, prior to coding the remaining videos. The mean OSBD-R scores between the two RAs will be used as the final scores. This standardised procedure for OSBD-R has been successfully used in previous research evaluating distraction.29 49–52 This scale demonstrates high inter-rater reliability as well as moderate to high correlations with other behavioural measures of distress.49 53 54
Our principal secondary outcome measure will be the child’s pain score during the IV procedure. Pain will be measured using an 11-point verbal Numerical Rating Scale ranging from 0 (no pain) to 10 (worst possible pain). This scale is a commonly used pain measurement tool in paediatric acute pain studies and is validated for use in children 6–17 years of age.55–58 Pain scores will be self-reported by children both before and immediately following the IV procedure.
Fear will be measured using the Children’s Fear Scale (CFS).4 59 This scale depicts five faces representing increasing levels of anxiety, where the leftmost face depicts ‘not scared at all’ (score=0) and the rightmost face means ‘most scared possible’ (score=4). The CFS is an adaptation of the adult Faces Anxiety Scale59 and has been validated to measure fear in children undergoing painful medical procedures.4 Children will be asked to independently rate their fear both before and immediately following the IV procedure.
Parental/caregiver anxiety will be measured with the State Trait Anxiety Inventory–State Scale Revised Version (STAI-S, Form Y), a validated and commonly used version of STAI, which has improved psychometric properties.60 Parents/caregivers will be asked to complete the STAI questionnaire both before and immediately following the IV procedure.
Parent/caregiver and nurse satisfaction with the procedure will be measured using a 5-point Likert scale, ranging from 1 ‘very dissatisfied’ to 5 ‘very satisfied’. Child satisfaction with the procedure will be measured using a 5-point Likert scale, ranging from 1 ‘not at all happy’ to 5 ‘very happy’. Satisfaction scores will be collected immediately following the IV procedure.
Safety of the VR intervention will be determined by assessing the frequency of adverse events post-intervention. Specifically, nausea will be self-rated by children immediately following the intervention, using the Baxter Retching Faces (BARF) scale.61 This scale consists of six faces depicting increasing levels of nausea, with assigned scores ranging from 0 to 10. The BARF scale is widely used in medical research, and has demonstrated construct, content and convergent validity as a tool to measure nausea in children.61 The presence of other adverse events (ie, dizziness) will also be recorded by the RA. Children who are presenting with nausea, vomiting, dizziness or migraines prior to enrolment will be excluded from the study to avoid exacerbating these conditions with the use of the VR equipment.
Sample size
The sample size for the study is 80 patients overall. Sample size calculations were conducted using a two-tailed, two-sample Mann-Whitney test for the primary outcome of observed behavioural distress based on data from the team’s previous trial of digital distraction. To detect a large effect size of 0.6 on the OSBD-R (which was observed in a previous trial), given a type I error of 0.05% and 80% power, the study will require 35 patients for each of the two study arms. To account for attrition and technical recording failures, the team will plan to over-recruit by 10%–15%, for an overall total of 80 patients. This will allow sufficient power to find a difference in the primary outcome if a difference truly exists.
Statistical methods
Statistical analyses will be conducted using statistical software SAS (V.9; SAS Institute). The significance level will be set at 0.05. Baseline variables will be described using appropriate summary statistics for each group. Imbalances between groups for key baseline variables will indicate the need for further adjusted analyses. For the primary outcome of observed behavioural distress, total OSBD-R scores will be compared between the two groups using independent samples t-tests if they are normally distributed or Mann-Whitney U tests if they are skewed (the Sidak correction procedure will be used to reduce the probability of a type I error). Additional model-based analyses (multiple linear regression) will be conducted, as needed, with behavioural distress as the response variable, preprocedure behavioural distress and group indicators as the explanatory variables along with some possible effect modifiers such as age, sex and parental/caregiver anxiety levels. Our primary analysis will be based on an intention-to-treat approach where all children who were randomly assigned to a study group will be included in the group to which they were randomised. Where cell sizes are small or data are sparse or missing, proxy information or appropriate imputation methods will be used as needed. Similar approaches will be used to compare the groups with respect to secondary outcomes if appropriate.
Patient and public involvement
The team’s parent advisor (KS) has provided ongoing input on the study protocol and design, and has provided valuable feedback on the content, flow and readability of the consent forms and data collection forms. The Stollery Youth Advisory Council, led by team member AP, provided input on the study design, outcomes measures, and types of VR applications that might be engaging and practical for our study population. AP also reviewed the study protocol and related documents to ensure that the outcomes and tools were patient relevant and age appropriate. Following recruitment completion, parent and youth advisors will be further engaged to discuss study results and dissemination plans in the context of patient-centred and family-centred care.
Data management and confidentiality
Data will be entered into a secure online REDCap45 database hosted by the Women and Children’s Health Research Institute (WCHRI) (see online supplemental appendix 2 for case report form). WCHRI’s REDCap installation is a validated electronic, web-based data capture system housed in a secure data centre at the University of Alberta. Data are entered into REDCap through a web-based interface using 128-bit SSL encryption. Each team member will be granted an individual username/password and will require additional two-factor authentication to log in. All datasets used for statistical analysis will be encrypted and devoid of any patient identifiers. For internal data quality control, a secure master list will be maintained to accurately link study IDs to the patient’s medical record.
Selected data elements will be validated electronically throughout the recruitment period and any discrepancies will be assigned to team members for timely resolution. REDCap includes internal quality checks, such as automatic range checks, to identify data that appear inconsistent, incomplete or inaccurate.
Study data will be entered directly into REDCap in real time via research iPads or, in some cases (ie, parent/caregiver indicates a preference to complete paper-based questionnaires), responses may be collected on paper first and then transcribed into REDCap by a trained RA. All paper documents (including study questionnaires, consent/assent forms and the master list) will be stored in a locked cabinet in a secure location that is only accessible to authorised research staff members. Study videos will be stored electronically in a secure institutional shared drive with restricted access to study staff. Videos will be saved according to their study ID only. The centrally compiled dataset will be stored on a secure server and computers at the University of Alberta. Following completion of the study, all data will continue to be kept in a secure location for 5 years as dictated by the research ethics board.
Ethics and dissemination
This study has received approval from the Health Research Ethics Board (HREB) at the University of Alberta (HREB identifier: Pro00073476). Any amendments to the study protocol or documents will be submitted for HREB review and will receive approval prior to implementation. Significant protocol amendments will also be reflected online on the clinicaltrials.gov study registration. This study has also received operational approval from the SCH ED.
All children will receive the best possible care for their presenting complaint, regardless of whether they choose to participate. It is possible that patients in the VR intervention group may experience nausea, mild motion sickness or dizziness, however these effects are rare in children and adolescents, ranging from 0% to 5%.62 63 VR applications have been selected appropriately to minimise these discomforts, and children are monitored closely throughout the study for any adverse effects. Children experiencing nausea, vomiting, dizziness or migraine headaches prior to enrolment will be excluded to avoid potential exacerbation. Study participation is unlikely to prolong the ED length of stay. For infection-control purposes, children screening positive for ‘influenza-like illness’ (as per ED screening criteria) are excluded to prevent potential contamination of the VR equipment.
Due to resource/logistical constraints, study recruitment will be limited to English-speaking families or those with their own interpreter, at a single recruiting centre, and during RA shift hours only. Critically ill children requiring immediate IV insertion will also be excluded to avoid delaying medical care. This may limit the generalisability of the study findings. We will not be controlling for the type of distraction used in the standard of care arm, but we will record what was employed. While this may create some heterogeneity in the comparison arm of the study, it will be a pragmatic reflection of clinical reality. Due to the nature of the intervention, blinding is not possible for the participants or the research personnel, though the statistician will be blinded to study group.
The study team plans to publish trial results in a high-impact, peer-reviewed journal and present results at national and international meetings; authorship eligibility will be determined by employing the International Committee of Medical Journal Editors’ recommended guidelines.64 Statistical code and dataset can be made available upon request.
Supplementary Material
Acknowledgments
The authors would like to thank the members of the Stollery Youth Advisory Council, who provided valuable input on the study design and gaming/application choices for the virtual reality headsets.
Footnotes
Twitter: @drsaminaali
Contributors: SA is a paediatric emergency clinician-researcher and professor of Pediatrics & Emergency Medicine at the University of Alberta. She co-developed and revised the protocol and co-drafted the protocol paper. She chose the previously validated tools for measuring the primary outcomes. MR is the programme lead for the Pediatric Emergency Medicine research programme at the University of Alberta and co-principal investigator of this study. She co-developed the study protocol, co-drafted the protocol paper and will operationalise the study. JS is the Mary Jo Haddad Nursing Chair in Child Health at the Hospital for Sick Children’s Research Institute and a nurse practitioner in the Department of Anesthesia’s chronic pain programme at the hospital. She assisted with the study design and protocol revision. KM is a pediatric trainee at the University of Calgary, with expertise in OSBD-R coding. He assisted with the study design and protocol revision. BV led the statistical analysis planning and contributed to protocol revision. BF is a child life specialist at the Stollery ED with expertise in managing children’s pain and distress in the ED setting. She assisted with the study design and protocol revision. KS is a family partner who has provided input into study outcomes to ensure family-relevant outcomes are chosen and will inform our knowledge translation efforts to the public. AP is the coordinator of the Stollery Youth Advisory Council. Together with the council, she informed programming choices for the virtual reality devices and has reviewed the protocol and related documents to ensure that the outcomes and tools are patient relevant and age appropriate. JP is the acting director for Stollery child life services with expertise in managing children’s pain and distress in the ED. She has informed study methods and will aid and support the development of our knowledge translation plan. LH is a professor in the Department of Pediatrics at the University of Alberta and director of the Alberta Research Centre for Health Evidence (Edmonton, Canada). She assisted with the study design and drafting the protocol, and provides expertise in clinical trial methodology and statistical analyses. All authors have approved this final version of the protocol. None of the authors have financial or other conflicts of interests as they pertain to this study and its involved recruitment sites.
Funding: This work is funded by the generosity of the Stollery Children’s Hospital Foundation through the Women and Children’s Health Research Institute Innovation grant. Purchase of the virtual reality goggles was facilitated through a generous small equipment grant from the Stollery Children’s Hospital Foundation. LH is supported by a Canada Research Chair in Knowledge Synthesis and Translation and is a distinguished researcher with the Stollery Science Lab supported by the Stollery Children’s Hospital Foundation.
Disclaimer: The funders do not have any role in the collection, management, analysis, or interpretation of data; writing of the report; or the decision to submit the report for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Stevens BJ, Abbott LK, Yamada J. CIHR Team in Children’s Pain. Epidemiology and management of painful procedures in children in Canadian hospitals. Can Med Assoc J 2011;183:E403–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duff AJA. Incorporating psychological approaches into routine paediatric venepuncture. Arch Dis Child 2003;88:931–7. 10.1136/adc.88.10.931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanchez Cristal N, Staab J, Chatham R, et al. Child life reduces distress and pain and improves family satisfaction in the pediatric emergency department. Clin Pediatr 2018;57:1567–75. 10.1177/0009922818798386 [DOI] [PubMed] [Google Scholar]
- 4.McMurtry CM, Noel M, Chambers CT, et al. Children's fear during procedural pain: preliminary investigation of the children's fear scale. Health Psychol 2011;30:780–8. 10.1037/a0024817 [DOI] [PubMed] [Google Scholar]
- 5.McGrath PJ, McAlpine L. Psychologic perspectives on pediatric pain. J Pediatr 1993;122:S2–8. 10.1016/s0022-3476(11)80002-8 [DOI] [PubMed] [Google Scholar]
- 6.Drendel AL, Ali S. Ten practical ways to make your ED practice less painful and more Child-Friendly. Clin Pediatr Emerg Med 2017;18:242–55. 10.1016/j.cpem.2017.09.001 [DOI] [Google Scholar]
- 7.El-Housseiny AA, Alamoudi NM, Farsi NM, et al. Characteristics of dental fear among Arabic-speaking children: a descriptive study. BMC Oral Health 2014;14:118. 10.1186/1472-6831-14-118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fields HL. How expectations influence pain. Pain 2018;159 Suppl 1:S3–10. 10.1097/j.pain.0000000000001272 [DOI] [PubMed] [Google Scholar]
- 9.Noel M, Rabbitts JA, Tai GG, et al. Remembering pain after surgery: a longitudinal examination of the role of pain catastrophizing in children's and parents' recall. Pain 2015;156:800. 10.1097/j.pain.0000000000000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trottier ED, Doré-Bergeron M-J, Chauvin-Kimoff L, et al. Managing pain and distress in children undergoing brief diagnostic and therapeutic procedures. Paediatr Child Health 2019;24:509–21. 10.1093/pch/pxz026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedrichsdorf SJ, Eull D, Weidner CA. A Children’s Comfort Promise: how can we do everything possible to prevent and treat pain in children using quality improvement strategies? Pediatric Pain Letter 2016;18:26–30. [Google Scholar]
- 12.Dumoulin S, Bouchard S, Ellis J, et al. A randomized controlled trial on the use of virtual reality for Needle-Related procedures in children and adolescents in the emergency department. Games Health J 2019;8:285–93. 10.1089/g4h.2018.0111 [DOI] [PubMed] [Google Scholar]
- 13.Jain S, Hegenbarth MA, Humiston SG, et al. Increasing ED use of jet injection of lidocaine for IV-related pain management. Pediatrics 2017;139:e20161697. 10.1542/peds.2016-1697 [DOI] [PubMed] [Google Scholar]
- 14.Chan E, Hovenden M, Ramage E, et al. Virtual reality for pediatric needle procedural pain: two randomized clinical trials. J Pediatr 2019;209:160-167.e4. 10.1016/j.jpeds.2019.02.034 [DOI] [PubMed] [Google Scholar]
- 15.Gaskell S. Evidence-Based guidelines for the management of invasive and/or distressing procedures with children. Br J Soc Psychol 2019. [Google Scholar]
- 16.McCaul KD, Malott JM. Distraction and coping with pain. Pain 1985;23:315. 10.1016/0304-3959(85)90138-1 [DOI] [PubMed] [Google Scholar]
- 17.Manne SL, Bakeman R, Jacobsen PB, et al. An analysis of a behavioral intervention for children undergoing venipuncture. Health Psychol 1994;13:556–66. 10.1037//0278-6133.13.6.556 [DOI] [PubMed] [Google Scholar]
- 18.Vessey JA, Carlson KL, McGill J. Use of distraction with children during an acute pain experience. Nurs Res 1994;43:369–72. [PubMed] [Google Scholar]
- 19.Klassen JA, Liang Y, Tjosvold L, et al. Music for pain and anxiety in children undergoing medical procedures: a systematic review of randomized controlled trials. Ambul Pediatr 2008;8:117–28. 10.1016/j.ambp.2007.12.005 [DOI] [PubMed] [Google Scholar]
- 20.Cohen LL, Blount RL, Panopoulos G. Nurse coaching and Cartoon distraction: an effective and practical intervention to reduce child, parent, and nurse distress during immunizations. J Pediatr Psychol 1997;22:355–70. 10.1093/jpepsy/22.3.355 [DOI] [PubMed] [Google Scholar]
- 21.Cassidy K-L, Reid GJ, McGrath PJ, et al. Watch needle, watch TV: audiovisual distraction in preschool immunization. Pain Med 2002;3:108–18. 10.1046/j.1526-4637.2002.02027.x [DOI] [PubMed] [Google Scholar]
- 22.Downey LVA, Zun LS. The impact of watching cartoons for distraction during painful procedures in the emergency department. Pediatr Emerg Care 2012;28:1033. 10.1097/PEC.0b013e31826cac1a [DOI] [PubMed] [Google Scholar]
- 23.Young T, Griffin E, Phillips E, et al. Music as distraction in a pediatric emergency department. J Emerg Nurs 2010;36:472–3. 10.1016/j.jen.2010.05.014 [DOI] [PubMed] [Google Scholar]
- 24.Ha YO, Kim HS. The effects of audiovisual distraction on children's pain during laceration repair. Int J Nurs Pract 2013;19 Suppl 3:20–7. 10.1111/ijn.12165 [DOI] [PubMed] [Google Scholar]
- 25.Gates M, Hartling L, Shulhan-Kilroy J, et al. Digital technology distraction for acute pain in children: a meta-analysis. Pediatrics 2020;145. 10.1542/peds.2019-1139. [Epub ahead of print: 22 01 2020]. [DOI] [PubMed] [Google Scholar]
- 26.Ahmadpour N, Randall H, Choksi H, et al. Virtual reality interventions for acute and chronic pain management. Int J Biochem Cell Biol 2019;114:105568. 10.1016/j.biocel.2019.105568 [DOI] [PubMed] [Google Scholar]
- 27.Sikka N, Shu L, Ritchie B, et al. Virtual Reality-Assisted pain, anxiety, and anger management in the emergency department. Telemed J E Health 2019;25:1207-1215. 10.1089/tmj.2018.0273 [DOI] [PubMed] [Google Scholar]
- 28.Hoffman HG, Doctor JN, Patterson DR. Use of virtual reality for adjunctive treatment of adolescent burn pain during wound care: a case report. Pain 2000;85:305–9. 10.1016/s0304-3959(99)00275-4 [DOI] [PubMed] [Google Scholar]
- 29.Han S-H, Park J-W, Choi SI, et al. Effect of immersive virtual reality education before chest radiography on anxiety and distress among pediatric patients: a randomized clinical trial. JAMA Pediatr 2019;173:1026-1031. 10.1001/jamapediatrics.2019.3000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shetty V, Suresh LR, Hegde AM. Effect of virtual reality distraction on pain and anxiety during dental treatment in 5 to 8 year old children. J Clin Pediatr Dent 2019;43:97–102. 10.17796/1053-4625-43.2.5 [DOI] [PubMed] [Google Scholar]
- 31.Furman E, Jasinevicius TR, Bissada NF, et al. Virtual reality distraction for pain control during periodontal scaling and root planing procedures. J Am Dent Assoc 2009;140:1508–16. 10.14219/jada.archive.2009.0102 [DOI] [PubMed] [Google Scholar]
- 32.Schneider SM, Hood LE. Virtual reality: a distraction intervention for chemotherapy. Oncol Nurs Forum 2007;34:39–46. 10.1188/07.ONF.39-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gerardi M, Rothbaum BO, Ressler K, et al. Virtual reality exposure therapy using a virtual Iraq: case report. J Trauma Stress 2008;21:209–13. 10.1002/jts.20331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parsons TD, Rizzo AA. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis. J Behav Ther Exp Psychiatry 2008;39:250–61. 10.1016/j.jbtep.2007.07.007 [DOI] [PubMed] [Google Scholar]
- 35.Botella C, Serrano B, Baños RM, et al. Virtual reality exposure-based therapy for the treatment of post-traumatic stress disorder: a review of its efficacy, the adequacy of the treatment protocol, and its acceptability. Neuropsychiatr Dis Treat 2015;11:2533–45. 10.2147/NDT.S89542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marco JH, Perpiñá C, Botella C. Effectiveness of cognitive behavioral therapy supported by virtual reality in the treatment of body image in eating disorders: one year follow-up. Psychiatry Res 2013;209:619–25. 10.1016/j.psychres.2013.02.023 [DOI] [PubMed] [Google Scholar]
- 37.Litwin SP, Nguyen C, Hundert A, et al. Virtual reality to reduce procedural pain during IV insertion in the pediatric emergency department: a pilot randomized controlled trial. Clin J Pain 2021;37:94–101. 10.1097/AJP.0000000000000894 [DOI] [PubMed] [Google Scholar]
- 38.Goldman RD, Behboudi A. Virtual reality for intravenous placement in the emergency department-a randomized controlled trial. Eur J Pediatr 2021;180:725–31. 10.1007/s00431-020-03771-9 [DOI] [PubMed] [Google Scholar]
- 39.Chen Y-J, Cheng S-F, Lee P-C, et al. Distraction using virtual reality for children during intravenous injections in an emergency department: a randomised trial. J Clin Nurs 2020;29:503–10. 10.1111/jocn.15088 [DOI] [PubMed] [Google Scholar]
- 40.Osmanlliu E, Trottier ED, Bailey B, et al. Distraction in the emergency department using virtual reality for intravenous procedures in children to improve comfort (DEVINCI): a pilot pragmatic randomized controlled trial. CJEM 2021;23:94–102. 10.1007/s43678-020-00006-6 [DOI] [PubMed] [Google Scholar]
- 41.Lambert V, Boylan P, Boran L, et al. Virtual reality distraction for acute pain in children. Cochrane Database Syst Rev 2020;10:CD010686. 10.1002/14651858.CD010686.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Czech O, Wrzeciono A, Rutkowska A, et al. Virtual reality interventions for Needle-Related procedural pain, fear and Anxiety-A systematic review and meta-analysis. J Clin Med 2021;10:3248. 10.3390/jcm10153248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chan A-W, Tetzlaff JM, Altman DG, et al. Spirit 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hoffman HG, Rodriguez RA, Gonzalez M, et al. Immersive virtual reality as an adjunctive non-opioid analgesic for Pre-dominantly Latin American children with large severe burn wounds during burn wound cleaning in the intensive care unit: a pilot study. Front Hum Neurosci 2019;13:262. 10.3389/fnhum.2019.00262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jay SM, Elliott C. Observation scale of behavioral Distress-Revised. information procedures, definitions of behaviors, OSBD interval coding form, 1986. [Google Scholar]
- 47.Jay SM, Elliott C. Behavioral observation scales for measuring children's distress: the effects of increased methodological rigor. J Consult Clin Psychol 1984;52:1106–7. 10.1037//0022-006x.52.6.1106 [DOI] [PubMed] [Google Scholar]
- 48.Tucker CL, Slifer KJ, Dahlquist LM. Reliability and validity of the brief behavioral distress scale: a measure of children's distress during invasive medical procedures. J Pediatr Psychol 2001;26:513–23. 10.1093/jpepsy/26.8.513 [DOI] [PubMed] [Google Scholar]
- 49.Elliott CH, Jay SM, Woody P. An observation scale for measuring children's distress during medical procedures. J Pediatr Psychol 1987;12:543–51. 10.1093/jpepsy/12.4.543 [DOI] [PubMed] [Google Scholar]
- 50.Megel ME, Houser CW, Gleaves LS. Children's responses to immunizations: lullabies as a distraction. Issues Compr Pediatr Nurs 1998;21:129–45. 10.1080/014608698265456 [DOI] [PubMed] [Google Scholar]
- 51.Noguchi LK. The effect of music versus nonmusic on behavioral signs of distress and self-report of pain in pediatric injection patients. J Music Ther 2006;43:16–38. 10.1093/jmt/43.1.16 [DOI] [PubMed] [Google Scholar]
- 52.Hartling L, Newton AS, Liang Y, et al. Music to reduce pain and distress in the pediatric emergency department: a randomized clinical trial. JAMA Pediatr 2013;167:826–35. 10.1001/jamapediatrics.2013.200 [DOI] [PubMed] [Google Scholar]
- 53.Stevenson MD, Bivins CM, O'Brien K, et al. Child life intervention during angiocatheter insertion in the pediatric emergency department. Pediatr Emerg Care 2005;21:712. 10.1097/01.pec.0000186423.84764.5a [DOI] [PubMed] [Google Scholar]
- 54.Jay SM, Ozolins M, Elliott CH, et al. Assessment of children’s distress during painful medical procedures. Health Psychology 1983;2:133–47. 10.1037/0278-6133.2.2.133 [DOI] [Google Scholar]
- 55.von Baeyer CL. Children's self-report of pain intensity: what we know, where we are headed. Pain Res Manag 2009;14:39–45. 10.1155/2009/259759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Miró J, Castarlenas E, de la Vega R, et al. Validity of three rating scales for measuring pain intensity in youths with physical disabilities. Eur J Pain 2016;20:130–7. 10.1002/ejp.704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Castarlenas E, Jensen MP, von Baeyer CL, et al. Psychometric properties of the numerical rating scale to assess self-reported pain intensity in children and adolescents: a systematic review. Clin J Pain 2017;33:376–83. 10.1097/AJP.0000000000000406 [DOI] [PubMed] [Google Scholar]
- 58.Castarlenas E, Miró J, Sánchez-Rodríguez E. Is the verbal numerical rating scale a valid tool for assessing pain intensity in children below 8 years of age? J Pain 2013;14:297–304. 10.1016/j.jpain.2012.12.004 [DOI] [PubMed] [Google Scholar]
- 59.McKinley S, Coote K, Stein-Parbury J. Development and testing of a faces scale for the assessment of anxiety in critically ill patients. J Adv Nurs 2003;41:73–9. 10.1046/j.1365-2648.2003.02508.x [DOI] [PubMed] [Google Scholar]
- 60.Spielberger CD, Sydeman SJ. State-trait anxiety inventory and state-trait anger expression inventory. Hillsdale. NJ: Lawrence Erlbaum Associates, 1994: 292–321. [Google Scholar]
- 61.Baxter AL, Watcha MF, Baxter WV, et al. Development and validation of a pictorial nausea rating scale for children. Pediatrics 2011;127:1542. 10.1542/peds.2010-1410 [DOI] [PubMed] [Google Scholar]
- 62.Gold JI, Mahrer NE. Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. J Pediatr Psychol 2018;43:266-275. 10.1093/jpepsy/jsx129 [DOI] [PubMed] [Google Scholar]
- 63.Hoffman HG, Patterson DR, Seibel E, et al. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain 2008;24:299-304. 10.1097/AJP.0b013e318164d2cc [DOI] [PubMed] [Google Scholar]
- 64.ICMJE . International Committee of medical Journal editors, 2017. Available: http://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html [Accessed 03 Aug 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-057892supp001.pdf (11.9MB, pdf)