Abstract
Objectives
To compare gender diversity between UK surgical specialties, assess trends over time, and estimate when gender parity might be achieved.
Design
Observational study.
Setting
National Health Service, UK.
Participants
NHS Hospital & Community Health Service workforce statistics for 2011 to 2020
Main outcome measures
Logistic regression was used to compare female representation in 2020 between surgical specialties, and to examine for any significant trends between 2011 and 2020. The method of least squares was used to estimate when female representation of specialty registrars would reach 50% (‘gender parity’) for specialties with <40% female representation.
Results
In 2020, female consultant and specialty registrar representation was significantly different between surgical specialties (both p<0.001). Female representation for each specialty were as follows (from highest to lowest): Specialty Registrars—Ophthalmology 49.7%, Otolaryngology 48.2%, Paediatric Surgery 45.5%, Plastic Surgery 42.2%, General Surgery 39.8%, Urology 31.6%, Vascular Surgery 25.0%, Neurosurgery 24.7%, Cardiothoracic Surgery 21.3%, and Trauma and Orthopaedics 20.6%; Consultants—Ophthalmology 32.4%, Paediatric Surgery 31.7%, Plastic Surgery 20.9%, General Surgery 17.5%, Otolaryngology 17%, Vascular Surgery 13.7%, Urology 11.7%, Cardiothoracic Surgery 10.8%, Neurosurgery 8.2%, and Trauma and Orthopaedics 7.3%. There was a significant positive trend in female representation of specialty registrars between 2011 and 2020 for all specialties except for Paediatric Surgery (representation consistently >45%) and Vascular Surgery (representation consistently <30%). General Surgery was estimated to achieve gender parity of their specialty registrars by 2028, Urology by 2033, Neurosurgery by 2064, Trauma and Orthopaedics by 2070, and Cardiothoracic Surgery by 2082.
Conclusions
Despite improvements over the last decade, gender disparity persists in the UK surgical workforce and there are significant differences between surgical specialties. Further work is necessary to establish the reasons for these observed differences with a specific focus on Vascular Surgery, Cardiothoracic Surgery, Neurosurgery, and Trauma and Orthopaedics.
Keywords: surgery, organisation of health services, medical education & training, human resource management
Strengths and limitations of this study.
This study is the first detailed analysis of gender representation in UK surgical specialties.
NHS Hospital & Community Health Service workforce statistics adjust the values to a multiple of 5 and are subject to reporting bias from NHS organisations.
Due to the nature of the data, it was not possible to perform multivariate analysis or adjust for demographic differences between groups.
Introduction
Addressing gender disparity in surgery is not only a moral obligation but would likely lead to improvements in patient care, financial performance, innovation and risk assessment.1 2 In 2020, Baroness Helena Kennedy QC led an independent review which ultimately described a lack of diversity and inclusion within the leadership of the Royal College of Surgeons of England.1 Additionally, the report briefly commented on gender disparity within the wider surgical workforce. The review stated that in the UK, 35% of surgical trainees and 14% of surgical consultants are female whereas 57% and 37% of all other trainees and consultants, respectively, are female.3
It is important to note that over the last 25 years, female medical students have made up >50% of medical school entrants in the UK.4 5 This suggests that the primary problem lies with attracting medical school graduates to surgical specialties. However, it is possible that influences, before or during medical school, form part of the multifactorial cause for gender disparity in surgery.
Steps have been taken to increase female representation within surgery in the UK, which has increased since 1991 when only 3% of the consultant body were women.2 Notable contributions to this change have been made by Women in Surgery (WinS), formerly Women in Surgical Training, which is a national initiative that has been ‘encouraging, enabling and inspiring women to fulfil their surgical career ambitions’ for the last 30 years.3 Despite the work of WinS, and diversity and inclusion statements made by surgical organisational bodies, women are still underrepresented in surgical specialties.6–12
This is a worldwide issue, with analysis from the World Health Organization describing a global female representation in surgery similar to the UK’s.13 14 Therefore, it is no surprise that there are numerous groups like WinS aiming to tackle gender inequality in surgery, including the Association of Women in Surgery, the Royal Australasian College of Surgeons own Women in Surgery, and Women in Surgery Africa, to name but a few.
Broad stroke attempts to remove barriers to training for women in surgery have been implemented across all specialities. However, highlighting differences between surgical specialities would guide a more nuanced and paced approach, learning from specialities with a greater proportion of female trainees. A few intra-speciality studies have described a lack of gender diversity but, to the authors’ knowledge, no inter-specialty comparative study has ever been performed.11 12 This study aims to compare gender diversity between UK surgical specialties, analyse trends over time, and estimate when gender parity might be achieved.
Methods
Data
A freedom of information request was made to NHS Digital, which provided NHS Hospital & Community Health Service workforce statistics for 2011 to 2020. These data included number of employees and gender, stratified by grade and surgical specialty. Gender was provided in the binary format of male and female. The grades used in this analysis were ‘Specialty Registrar’ and ‘Consultant’. The specialties included were Cardiothoracic Surgery, General Surgery, Neurosurgery, Ophthalmology, Otolaryngology, Paediatric Surgery, Plastic Surgery, Trauma and Orthopaedics, Urology, and Vascular Surgery.
Each NHS Trust provides data to NHS Digital annually, and the accumulated totals are adjusted as follows: zeroes are unchanged, counts ending between 1 and 7 (inclusive) are displayed as 5, and all other counts are rounded to the nearest 5. There were insufficient data available for Vascular Surgery from 2011 to 2013.
Terminology
NHS digital provide data for gender using the terms ‘male’ and ‘female’. These terms are normally used to refer to a person’s sex assignment at birth; however, in demographic data collection they are often used to identify a person’s gender.
As the data we analysed, and much of the literature, use demographic data which use the terms ‘male’ and ‘female’ for gender, rather than ‘man’ and ‘woman’, we will also use these terms. When using the term ‘female’ to describe surgical consultants or registrars we will therefore mean ‘people who responded as female when asked their gender’ rather than ‘people whose sex was assigned as female at birth’.
Statistical analysis
Univariate logistic regression with robust standard errors was used to estimate the odds ratios (OR) comparing the proportion of female surgeons in 2020 at specialty registrar and consultant level between the 10 surgical specialties. Urology was used as the reference category as it is one of the larger specialties with female representation close to the median for both specialty registrars and consultants. Wald tests were used to calculate p values.
Univariate logistic regression was used to analyse the trends in female representation from 2011 to 2020 for each specialty. The likelihood ratio test was used to confirm that time (in years) could be used as a continuous variable rather than a categorical variable.
For the specialties with <40% female representation of specialty registrars, and a significant trend, the method of least squares was used to fit a trend line to estimate time to gender parity (figure 1). Gender parity was defined as 50% female representation.
Figure 1.
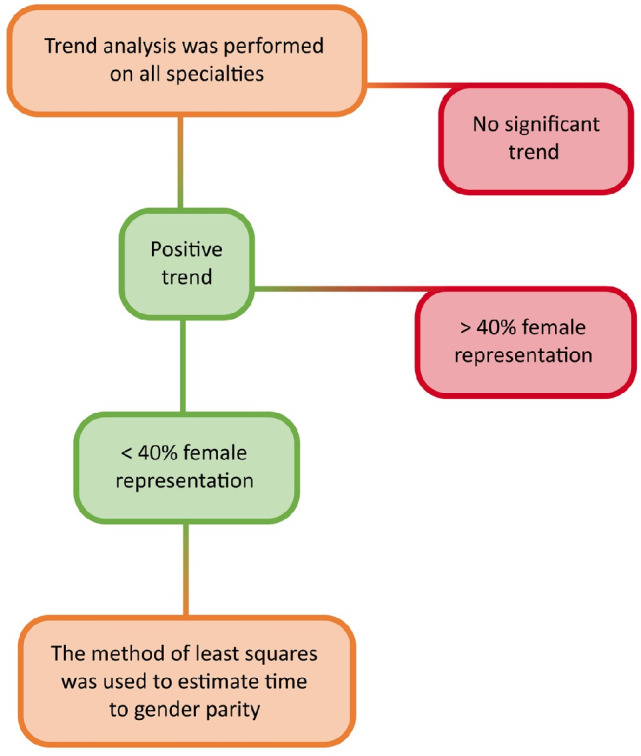
Flowchart to demonstrate selection for time-to-parity analysis for surgical registrars.
Patient and Public involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research.
Results
Data description
In 2020, there were 10 420 consultants and 6525 registrars working in one of the 10 surgical specialties in the UK, of which 1680 (16.1%) and 2230 (34.2%) were female, respectively. Trauma and Orthopaedics was the largest specialty with 2750 consultants and 1725 registrars, while Paediatric Surgery was the smallest with 205 consultants and 165 registrars. Full data for each year, 2011 to 2020, can be found in the online supplemental material.
bmjopen-2021-055516supp001.pdf (53.3KB, pdf)
Comparison of gender representation between surgical specialties in 2020
In 2020, the specialties with the highest female representation of registrars were Ophthalmology (49.7%), Otolaryngology (48.2%), and Paediatric Surgery (45.5%), followed by Plastic Surgery (42.2%), General Surgery (39.8%), Urology (31.6%), Vascular Surgery (25.0%), Neurosurgery (24.7%), Cardiothoracic Surgery (21.3%), and Trauma and Orthopaedics (20.6%). There was a significant difference observed between the surgical specialties (p<0.001). For context, Ophthalmology had a significantly higher female representation of registrars compared with Urology (49.7% vs 31.6%; OR 2.14, 95% CI 1.68 to 2.72) and Trauma and Orthopaedics had a significantly lower female representation compared with Urology (20.6% vs 31.6%; OR 0.56, 95% CI 0.45 to 0.70) (table 1).
Table 1.
Female representation by surgical specialty for 2020 and estimated odds ratios (OR) compared to Urology (green = greater OR, red = lesser OR, black = non-significant difference). Specialties listed by female representation (%) in descending order
| Surgical specialty | Total | Female | OR | 95% CI | P value | |
| Registrars | N | N | % | <0.001 | ||
| Ophthalmology | 715 | 355 | 49.7 | 2.14 | 1.68 to 2.72 | |
| Otolaryngology | 550 | 265 | 48.2 | 2.01 | 1.56 to 2.60 | |
| Paediatric Surgery | 165 | 75 | 45.5 | 1.81 | 1.26 to 2.59 | |
| Plastic Surgery | 450 | 190 | 42.2 | 1.58 | 1.21 to 2.07 | |
| General Surgery | 1645 | 655 | 39.8 | 1.43 | 1.15 to 1.78 | |
| Urology | 475 | 150 | 31.6 | 1 | ||
| Vascular Surgery | 120 | 30 | 25.0 | 0.72 | 0.46 to 1.14 | |
| Neurosurgery | 385 | 95 | 24.7 | 0.71 | 0.52 to 0.96 | |
| Cardiothoracic surgery | 305 | 65 | 21.3 | 0.59 | 0.42 to 0.82 | |
| Trauma and Orthopaedics | 1725 | 355 | 20.6 | 0.56 | 0.45 to 0.70 | |
| Consultants | N | N | % | <0.001 | ||
| Ophthalmology | 1495 | 485 | 32.4 | 3.63 | 2.91 to 4.54 | |
| Paediatric Surgery | 205 | 65 | 31.7 | 3.51 | 2.47 to 5.00 | |
| Plastic Surgery | 550 | 115 | 20.9 | 2.00 | 1.51 to 2.65 | |
| General Surgery | 2625 | 460 | 17.5 | 1.61 | 1.29 to 2.00 | |
| Otolaryngology | 795 | 135 | 17.0 | 1.55 | 1.18 to 2.02 | |
| Vascular Surgery | 255 | 35 | 13.7 | 1.20 | 0.80 to 1.81 | |
| Urology | 985 | 115 | 11.7 | 1 | ||
| Cardiothoracic surgery | 415 | 45 | 10.8 | 0.92 | 0.64 to 1.33 | |
| Neurosurgery | 365 | 30 | 8.2 | 0.68 | 0.44 to 1.03 | |
| Trauma and Orthopaedics | 2750 | 200 | 7.3 | 0.59 | 0.47 to 0.76 | |
In terms of consultants, the specialties with the highest female representation were Ophthalmology (32.4%) and Paediatric Surgery (31.7%), followed by Plastic Surgery (20.9%), General Surgery (17.5%), Otolaryngology (17.0%), Vascular Surgery (13.7%), Urology (11.7%), Cardiothoracic Surgery (10.8%), Neurosurgery (8.2%), and Trauma and Orthopaedics (7.3%). There was a significant difference observed between the surgical specialties (p<0.001). For context, Ophthalmology had a significantly higher female representation of consultants compared with Urology (32.4% vs 11.7%; OR 3.63, 95% CI 2.91 to 4.54) and Trauma and Orthopaedics had a significantly lower female representation compared with Urology (7.3% vs 11.7%; OR 0.59, 95% CI 0.47 to 0.77) (table 1).
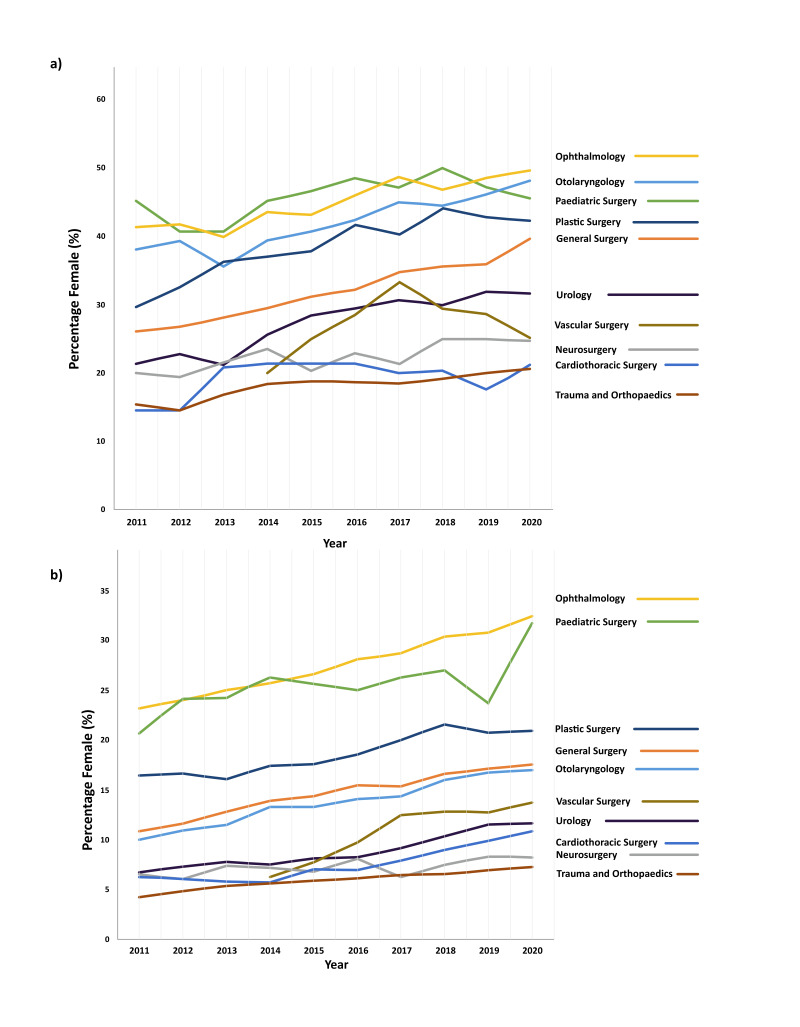
Gender representation trend between 2011 and 2020
All 10 surgical specialties had an increase in female representation in their registrar and consultant workforce between 2011 and 2020 (figure 2). Overall, the proportion of female registrars has risen from 25.3% (1550/6120) to 34.2% (2230/6525) and female consultants from 10.6% (795/7505) to 16.1% (1680/10 480).
Figure 2.
Percentage of UK surgical workforce who are female from 2011 to 2020. (A) Registrars. (B) Consultants.
There was a significant positive trend in female representation seen for both registrars and consultants in Cardiothoracic Surgery, General Surgery, Ophthalmology, Plastic Surgery, Trauma and Orthopaedics, and Urology, and only for registrars in Neurosurgery and Otolaryngology (all p<0.05).
There was no significant trend in female representation seen for both registrars and consultants in Paediatric Surgery (p=0.152 and p=0.070, respectively), but this specialty has remained one of the specialties with the highest female representation across the study period (consistently above 45% for registrars and above 20% for consultants). Although there was a significant positive trend in female representation seen for consultants in Vascular Surgery (p=0.017), there was no such trend for the registrars where female representation has been consistently below 30%.
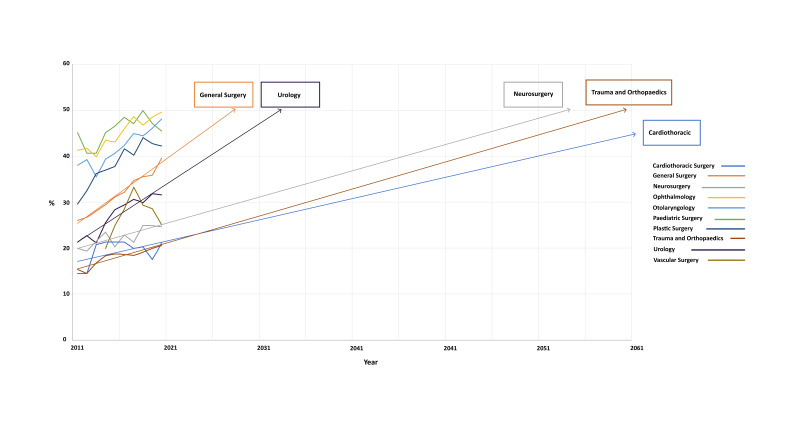
Time to gender parity
There were five specialties with a female representation of registrars below 40% and a positive trend observed between 2011 and 2020: General Surgery, Urology, Neurosurgery, Cardiothoracic Surgery, and Trauma and Orthopaedics.
General Surgery was estimated to achieve gender parity of their registrars by 2028 (1.47% per year, R2=0.98), Urology by 2033 (1.31% per year, R2=0.88), Neurosurgery by 2064 (0.58% per year, R2=0.67), Trauma and Orthopaedics by 2070 (0.59% per year, R2=0.85), and Cardiothoracic Surgery by 2082 (0.46% per year, R2=0.25) (figure 3). There was no significant trend observed for Vascular Surgery registrars and so no estimation of time to gender parity was possible.
Figure 3.
Projection of trends to estimate time to parity for female registrars in surgical specialties.
Discussion
This study demonstrates that gender disparity persists in the UK surgical workforce and that there are significant differences between surgical specialties. This disparity has decreased over the last decade, but in certain specialties this was not statistically significant. Estimations suggest that for registrars training in Neurosurgery, Trauma and Orthopaedics, and Cardiothoracic Surgery, it will take an estimated 45–60 years to reach gender parity if nothing changes. There was also no upward trend observed for Vascular registrars and female representation may remain at below 30%.
Specialties that are closer to gender parity are Ophthalmology and Paediatric Surgery followed by Otolaryngology, Plastic Surgery, and General Surgery. The specialties which have the lowest proportion of female surgeons are Trauma and Orthopaedics, Cardiothoracic Surgery, and Neurosurgery, while Vascular Surgery and Urology have only marginally greater female representation. Trauma and Orthopaedics was the only specialty that had a significantly greater gender disparity for both registrars and consultants, when compared with the reference specialty of Urology.
The data provided by NHS Digital are limited by errors made by organisations providing the data or by staff working in more than one role. In an attempt to minimise error from this the roles used were ‘Specialty Registrar’ and ‘Consultant’, since ‘Staff Grades’ and ‘Specialty Doctors’ are more likely to work in more than one role, trust or specialty. Another limitation is that gender is only supplied in the binary format of ‘male’ and ‘female’ which does not include those who identify as transgender or non-binary, which in the UK is estimated to make up 1% of the population.15
For undisclosed reasons, the values given in the data are not absolute but are adjusted to a multiple of 5, as described in the methods. These adjustments make the greatest difference to smaller specialties and for this reason data for 2013 have not been included in the trend analysis for Vascular Surgery. It was only in 2012 that Vascular Surgery was considered a separate specialty from General Surgery, which explains the relatively small number of vascular surgeons.
Another issue was that, due to the nature of the data, it was not possible to perform multivariate analysis or adjust for demographic differences between groups. A limitation of estimating time to parity was that a linear trend was assumed. With 10 data points it is difficult to predict how gender representation will change over time; however, there was no strong evidence that this would be exponential or logarithmic. A linear trend is also likely to underestimate the time to gender parity as the rate of change is unlikely to stay the same as parity is approached.
To the authors acknowledge this is the first analysis of its kind; however, a comparable study in the USA stated that, despite an increasing female representation in surgical specialties, there remained an underrepresentation of women.16
The disparity we describe is even more pronounced when we consider that female representation in medical student entrants has remained between 55% and 60% for the last 25 years in the UK.4 5 It should also be stated that since medical student gender representation is static, the trend towards gender parity is not due to an increasing proportion of female medical students. Unfortunately, we do not know why female representation in certain specialties is increasing more than others, and we have no strong evidence of which initiatives have worked or are transferable across a wide range of surgical specialities.11 We hope that specific specialties have identified barriers for women in surgery and created more equitable training, and worry that other specialties with greater degrees of implicit bias and hidden curriculums are not changing.
Previous studies have described barriers for female surgical trainees. In 2017, a systematic review from the USA demonstrated greater attrition of female general surgery trainees, most commonly to switch specialty or due to the lifestyle.17 Several qualitative studies and a systematic review have demonstrated common barriers to female trainees pursuing a career in surgery including verbal discouragement, which is disproportionally gender-based for women, sexism and discrimination, family/caring commitments, lack of mentorship, and poor work-life balance.17–21
However, several of these barriers exist for other specialties but do not lead to gender disparity. For example, UK Obstetrics and Gynaecology training has comparable shift work and skill requirements to surgical specialties, and 80% of trainees are female.22 Since technical aspects of surgical training, family/caring commitments or work-life balance are non-specific, it is possible that cultures of discrimination, gender-specific discouragement and lack of mentorship have led to the low representation of women in surgery. Variations in the prevalence of such cultures, and resultant specialty stereotypes, could cause the differences in female representation between specialties that have been demonstrated. Therefore, appreciating the lived experiences of female consultant surgeons and trainees and tackling discriminatory cultures would be an integral step to achieving gender parity; perhaps more importantly, this would likely lead to greater job satisfaction and retention of female surgeons.
The specialties with greatest time to parity already have very low female representation; perhaps the slow rate of change is due to having even fewer role models, greater implicit bias or more discriminatory cultures than the other specialties. Orthopaedics had the lowest female representation of all surgical specialties, and a recently published review on the current challenges for women in orthopaedics named many of the barriers listed above as causative.23 The review highlights the need for cultural and structural change to improve workforce diversity, specifically suggesting the need for mentors and addressing implicit bias.
Discriminatory cultures were also discussed in an independent review into the gender pay gap in medicine, led by the Department of Health and Social Care in 2020.24 The review identified surgery as having the greatest unadjusted gender pay gaps which was largely explained by differences in age, experience and grade. Cultural barriers that were raised as contributing to these differences were male-dominated specialties being ‘macho’, gender-specific discrimination, and a lack of role models.24
Encouragingly, this study shows there has been a trend towards gender parity over the last 10 years. However, for some specialties, including Paediatric Surgery and Vascular Surgery, there was no significant trend. For Paediatric Surgery, this might be because it is one of the specialties closest to gender parity, so is less likely to have large increases in female trainees; whereas the absence of a significant trend for Vascular Surgery is potentially due to the smaller cohort and greater annual variation in a newly defined specialty.
For some specialties it will take a minimum of 40 years to reach gender parity for registrars if no intervention is taken. Neurosurgery, Cardiothoracic Surgery, Trauma and Orthopaedics, and Vascular Surgery are specialties that would likely benefit from greater attention than specialties closer to gender parity. Some of these specialties have already started this process. For example, the Society for Cardiothoracic Surgery has established an equality, diversity and inclusion strategy that includes a survey of members and a Women in Cardiothoracic Surgery Mentorship Programme.25
It is encouraging to see the development of specialty specific mentorship programmes like this, which have been highlighted as important by several working groups including the Association of Surgeons of Great Britain and Ireland Women in Surgery.26 This group also identified the potential for social media to provide an easier method of finding gender-specific mentors, role models and support networks.
The general trend towards gender parity is promising and hopefully this study will inspire intra- and inter-specialty analyses to establish the reasons for the observed differences between surgical specialties. Analysis of surgical trainee experiences, positive and negative, would give greater insight into these differences and enable a specialty specific approach to achieving equality of opportunity.
We would suggest a follow-up of mentorship programmes and other initiatives in order to provide evidence for our efforts. We also believe that UK surgical societies should draw inspiration from the Perry Initiative in the USA, which implemented a medical student outreach programme and demonstrated a positive influence on women to choose orthopaedics.27 Policy change should be influenced by successful initiatives and look to the specialties closest to gender parity for inspiration.
Conclusion
Gender disparity persists in the UK surgical workforce and there are significant differences between surgical specialties. This disparity has decreased over the last decade, but in certain groups this is not statistically significant. We estimate that for some specialties achieving gender parity will take longer than 60 years.
The differences in gender disparity between surgical specialties have not been described previously and further work is needed to highlight the causes. We also suggest following-up mentorship programmes and diversity initiatives to provide evidence for our efforts and inform future policies aimed at improving the equality of opportunity and working experiences for women in surgery.
Supplementary Material
Footnotes
Twitter: @Thomas_H_Newman, @mparry7, @RoxannaZakeri
Contributors: THN—guarantor, joint lead with MGP, specifically initial conceptualisation, literature review, data curation, supporting analysis, administration, original drafting and revising of manuscript. MGP—joint lead with THN, specifically supporting conceptualisation and literature review. Lead for statistical analysis and equal contribution to original drafting and revising of manuscript. RZ—supported literature review and original drafting. Review and editing of manuscript. VP—supported literature review and original drafting. Review and editing of manuscript. AN—review and editing of manuscript. SV—review and editing of manuscript. FB—review and editing of manuscript. JG—supervisor, involved with supervision of all aspects of the article and heavily involved with conceptualisation, analysis, original drafting, review and editing.
Funding: The article publishing charge (APC) was kindly provided by Ms Janet Tomlinson, a private donor who has consented to the sharing of her name and story. Ms Tomlinson recently had major surgery and was struck by the lack of female surgeons in the department caring for her. Following serendipitous events, Ms Tomlinson was made aware of our work and has kindly covered the APC, allowing us to publish in an open access journal.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1. How Diversity & Inclusion Matter | McKinsey [Internet]. [cited 2021 May 20]. Available: https://www.mckinsey.com/featured-insights/diversity-and-inclusion/diversity-wins-how-inclusion-matters#
- 2. Gomez LE, Bernet P. Diversity improves performance and outcomes. J Natl Med Assoc 2019;111:383–92. 10.1016/j.jnma.2019.01.006 [DOI] [PubMed] [Google Scholar]
- 3. Royal College of Surgeons . An independent review on diversity and inclusion for the Royal College of Surgeons of England [Internet]. Royal College of Surgeons. [cited 2021 May 8]. Available: https://www.rcseng.ac.uk/about-the-rcs/about-our-mission/diversity-review-2021/
- 4. selection-alliance-2019-report.pdf [Internet]. [cited 2021 May 20]. Available: https://www.medschools.ac.uk/media/2608/selection-alliance-2019-report.pdf
- 5. 2004 UK Demography Schools Medicine.pdf [Internet]. [cited 2021 May 20]. Available: http://puntsdevista.comb.cat/edicio9/Documents/2004%20UK%20Demography%20Schools%20Medicine.pdf
- 6. BAUS . Statement on Equality [Internet]. [cited 2021 May 12]. Available: https://www.baus.org.uk/about/governance/statement_on_equality.aspx
- 7. British Association of Oral and Maxillofacial Surgeons . BAOMS President welcomes RCSEng review into diversity and reveals the specialty’s response [Internet]. [cited 2021 May 12]. Available: https://www.baoms.org.uk/about/news/145/baoms_president_welcomes_rcseng_review_into_diversity_and_reveals_the_specialtys_response
- 8. PLASTA . About PLASTA - PLASTA [Internet]. [cited 2021 May 12]. Available: https://www.plasta.org/about/default.aspx
- 9. BOA . Diversity and Inclusion [Internet]. [cited 2021 May 12]. Available: https://www.boa.ac.uk/about-us/diversity-and-inclusion.html
- 10. ENT UK . Equality and Diversity [Internet]. [cited 2021 May 12]. Available: https://www.entuk.org/equality-and-diversity
- 11. Walsh U, Meyer FJ. Awareness and impact of wins on female surgical trainees. Bulletin 2011;93:1–5. 10.1308/147363511X558155 [DOI] [Google Scholar]
- 12. Skinner H, Bhatti F. Women in surgery. Bulletin 2019;101:12–14. 10.1308/rcsbull.TB2019.12 [DOI] [Google Scholar]
- 13. Xepoleas MD, Munabi NCO, Auslander A, et al. The experiences of female surgeons around the world: a scoping review. Hum Resour Health 2020;18:80. 10.1186/s12960-020-00526-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization . Delivered by women, led by men: a gender and equity analysis of the global health and social workforce. [online] Apps.who.int, 2021. Available: https://apps.who.int/iris/handle/10665/311322 [Accessed 22 Oct 2021].
- 15. The truth about trans [Internet]. Stonewall. [cited 2021 May 26], 2018. Available: https://www.stonewall.org.uk/truth-about-trans
- 16. Klifto KM, Payne RM, Siotos C, et al. Women continue to be underrepresented in surgery: a study of AMA and ACGME data from 2000 to 2016. J Surg Educ 2020;77:362–8. 10.1016/j.jsurg.2019.10.001 [DOI] [PubMed] [Google Scholar]
- 17. Khoushhal Z, Hussain MA, Greco E, et al. Prevalence and causes of attrition among surgical residents: a systematic review and meta-analysis. JAMA Surg 2017;152:265–72. 10.1001/jamasurg.2016.4086 [DOI] [PubMed] [Google Scholar]
- 18. Liang R, Dornan T, Nestel D. Why do women leave surgical training? A qualitative and feminist study. Lancet 2019;393:541–9. 10.1016/S0140-6736(18)32612-6 [DOI] [PubMed] [Google Scholar]
- 19. Bellini MI, Graham Y, Hayes C, et al. A woman's place is in theatre: women's perceptions and experiences of working in surgery from the association of Surgeons of Great Britain and Ireland Women in Surgery Working Group. BMJ Open 2019;9:e024349. 10.1136/bmjopen-2018-024349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Giantini Larsen AM, Pories S, Parangi S, et al. Barriers to pursuing a career in surgery: an institutional survey of Harvard Medical School students. Ann Surg 2021;273:1120–6. 10.1097/SLA.0000000000003618 [DOI] [PubMed] [Google Scholar]
- 21. Lim WH, Wong C, Jain SR, et al. The unspoken reality of gender bias in surgery: a qualitative systematic review. PLoS One 2021;16:e0246420. 10.1371/journal.pone.0246420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. O&G Workforce Report. [cited 2021 May 26], 2018. Available: https://www.rcog.org.uk/globalassets/documents/careers-and-training/workplace-and-workforce-issues/rcog-og-workforce-report-2018.pdf
- 23. Ahmed M, Hamilton LC. Current challenges for women in orthopaedics. Bone & Joint Open 2021;2:893–9. 10.1302/2633-1462.210.BJO-2021-0089.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dacre J. Mend the Gap: The Independent Review into Gender Pay Gaps in Medicine in England. [online] Assets.publishing.service.gov.uk, 2021. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/944246/Gender_pay_gap_in_medicine_review.pdf [Accessed 27 Oct 2021].
- 25. Equality, Diversity and Inclusion [Internet]. [cited 2021 Jun 15]. Available: https://scts.org/professionals/equality_diversity_and_inclusion.aspx
- 26. Bellini MI, Adair A, Fotopoulou C, et al. Changing the norm towards gender equity in surgery: the Women in Surgery Working Group of the Association of Surgeons of Great Britain and Ireland's perspective. J R Soc Med 2019;112:325–9. 10.1177/0141076819854194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lattanza LL, Meszaros-Dearolf L, O'Connor MI, et al. The Perry Initiative’s medical student outreach program recruits women into orthopaedic residency. Clin Orthop Relat Res 2016;474:1962–6. 10.1007/s11999-016-4908-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055516supp001.pdf (53.3KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.