Abstract
Introduction
Telemedicine and blood pressure (BP) self-monitoring conduces to management of hypertension. Recent hypertension guidelines highly recommended single pill combination (SPC) for the initial treatment of essential hypertension. Based on this fact, an SPC-based telemedicine titration regimen with BP self-monitoring could be a better way in managing hypertension. This trial aims to elucidate whether telemedicine combined with BP self-monitoring is superior to self-monitoring alone during hypertension management.
Methods and analysis
This study will be a multicentred, open-labelled, randomised controlled trial. A minimum sample of 358 hypertensive patients with uncontrolled BP from four centres will be included. The intervention group will include BP self-monitoring and tele-monitoring plus a free SPC-based telemedicine titration therapy for 6 months, they will be recommended to take BP measurements at least once every 7 days, in the meantime, researchers will call to give a consultation on lifestyle or titration advice once a fortnight. The control group will be required to self-monitor BP at the same time interval as intervention group, without any therapy change. Primary outcome of the trial will be the difference in systolic blood pressure at 6-month follow-up between intervention and control group, adjusted for baseline variables. Secondary outcomes such as BP control rate, major adverse cardiovascular events, medication adherence, quality of life will be investigated.
Ethics and dissemination
Ethics approval was granted by Ethical Committee of Shanghai Tenth People’s Hospital (SHSY-IEC-4.1/20-194/01). The results will be disseminated in peer-reviewed literature, and to policy-makers and healthcare partners.
Trial registration number
ChiCTR2000037217.
Keywords: hypertension, adult cardiology, epidemiology
Strengths and limitations of this study.
This trial will investigate whether single pill combination-based simplified telemedicine regimen is superior to self-monitoring alone, and advantages of clinic-free hypertension management.
Although the trial is multicentred, but all four of them are in urban area. Meanwhile, potentially eligible participants for this trial are not universal, exclusion criteria are strictly designed, this may limit the generalisation and application of the study results to a broader population.
It is possible that high frequent blood pressure (BP) measurement may result in BP elevation due to anxiety.
Mean home BP and office BP will be used as outcomes in this trial, not 24 hours ambulatory BP.
This trial may have spillover effect more or less when at the clinician or clinic level owing to the individualised randomisation plan.
Introduction
Hypertension is the leading remediable risk factor for cardiovascular disease (CVD), hypertension and its mediated organ damages are the cause of increased morbidity and mortality worldwide.1–3 The number of adult patients with hypertension increased from 594 million in 1975 to 1.13 billion in 2015 (226 million of whom in China).4 In sharp contrast with the increasing prevalence of hypertension, the well-controlled rate of hypertension is still far below expectations.4 Despite the availability of effective treatment, only 31.3% of the hypertensive patients with pharmacologic therapies have controlled blood pressure (BP) in low-income and middle-income countries (38.0% of whom in China,5 while 40.7% of the patients were well-controlled in high-income countries.6 One of the main reasons for this problem could be the poor medication adherence.7 8Another reason for the poor control rate could be the imbalance between the number of patients and physicians. Hence, it is necessary to develop an easy and effective way to improve control of BP in management of hypertension. Self-monitoring and telemedicine have been proved to reduce BP and improve adherence to antihypertensive medication.9–15 The Chinese Hypertension Guidelines16 stressed that home BP (HBP) self-monitoring can be used to improve patients’ compliance, and it is expected to become a new model of BP management in the future. Meanwhile, hypertension guidelines proposed by the International Society of Hypertension (ISH),17 National institute for Health and Care Excellence,18 in Europe19 and China16 all recommended single pill combination (SPC) for initial treatment, and the first step of antihypertensive therapy is to choose ACE inhibitors/angiotensin receptor blockers and calcium channel blocker, which can improve adherence to treatment. On the basis of the self-monitoring and telemedicine, an SPC-based simplified titration regimen according to the latest hypertension guideline16 17 19 20 was developed in this study.
This trial investigates whether SPC-based telemedicine combined with BP self-monitoring is superior to self-monitoring alone during hypertension management.
Methods and design
Study setting
The Simplified regImen for the Management of hyPertension with teLemedicine and blood pressure sElf-monitoring study will be an open-labelled, two-arm, parallel, randomised controlled trial to compare SPC-based telemedicine combined with BP self-monitoring to usual care in the management of hypertension. This trial will take place in four centres: Shanghai 10th People’s Hospital, Shanghai Xuhui Central Hospital, Shanghai Putuo People’s Hospital and Shanghai Putuo Central Hospital. Recruitment started on 21 December 2020 and this study is planned to end on 30 June 2022.
Eligibility criteria and recruitment
Internet-based advertising and clinic visit will be used for recruitment, participants who were previously diagnosed with essential hypertension and taking antihypertensive agents, but with uncontrolled BP (office BP >140/90 mm Hg) are considered as potentially eligible. Considering high frequent of BP measuring may lead to BP elevation caused by anxiety, it is not recommended for patients with high anxiety to self-monitor HBP.16 Detailed inclusion and exclusion criteria are listed in box 1. At first visit, potentially eligible participants will undergo a 2-week screening phase, they will be trained to record their HBP on a paper diary at least twice a day (online supplemental file 1), their previous antihypertensive drugs will be replaced with SPC-based titration regimen which is equivalent to their previous ones following specified regimen exchange plan (online supplemental file 2) and also by physicians’ experience to verify drug adherence and compliance. Participants who managed to fill at least three quarters of the whole BP diary, also without any drug side effects will be considered as fully eligible, randomisation will be performed by senior researchers, physicians will be blinded during the trial process.
Box 1. Inclusion and exclusion criteria.
Inclusion criteria
Age 18 and 75 years.
Willing to participate the study and sign informed consent.
Essential hypertension under medical treatment with uncontrolled blood pressure (systolic blood pressure (SBP) >140 mm Hg or diastolic blood pressure >90 mm Hg).
Exclusion criteria
Office SBP >180 mm Hg.
Essential hypertension.
Taking over three different antihypertensive agents.
Atrial fibrillation or other malignant arrhythmias.
Any diagnosed type I or II diabetes, renal dysfunction, coronary heart disease, heart failure or a history of stroke or myocardial infarction.
Any serious medical condition.
Participation in any other trial.
Amnesia or dementia.
Diagnosed with severe valvular heart disease.
Pregnancy or expecting to get pregnant.
Spouse already participated in the study.
Not own a mobile phone for remote communication.
Conditions determined unfit for the study by investigators.
Participants who were either not tolerated or had no response to similar antihypertensive therapies.
bmjopen-2021-049162supp001.pdf (565.7KB, pdf)
bmjopen-2021-049162supp002.pdf (153KB, pdf)
Office BP measurement
The day before office BP measurement, participants will be informed to avoid smoking and caffeine. Office measurement will be performed with automated electronic sphygmomanometer (RBP-9802, Raycome Health Technology Corporation, Shenzhen) by nurses or physicians in a quiet room, 3 measurements with at least 1 min interval, average of second and third readings will be recorded.17
HBP uploads
Participants will be trained to use the automated electronic sphygmomanometer (RBP-9802, Raycome Health Technology, Shenzhen), which will upload the HBP readings to data centre via 2G network (online supplemental file 3). The BP monitors will be given for free, participants are allowed to keep it even after the trial ended. A notification for BP measuring will be sent to the participants at 9:00 am and 21:00 pm via private message or social app. A minimum of once a 7-day measurement is recommended. All participants may review their uploaded BP history.
bmjopen-2021-049162supp003.pdf (1.3MB, pdf)
Control (self-monitoring) group
Usual care group will remain their own management plan without further intervention, HBP measurement is required but without interventional monitoring.
Intervention group
Intervention group will conclude both self-monitoring and tele-monitoring, plus telemedicine, they will take antihypertensive agents following the prespecified titration regimen based on uploaded HBP. Every 2 weeks, researchers will check patients’ uploaded HBP records, and give a consultant call under supervision of physicians (patients’ personal information censored). After the call, based on the prespecified BP titration regimen, the physician will prescribe the antihypertensive tablets for the future 2 weeks, and all the medications will be delivered within 24 hours to patients. Participants who suffered long time side effects of any drugs prescribed by this trial will be discontinued immediately. Participants who are using spironolactone will receive free blood check monthly to monitor blood potassium level.
Outcome assessment
The primary outcome of the trial will be the difference in systolic BP (SBP) (office BP, mean of second/third readings, mm Hg) at 6-month follow-up between intervention and control group, adjusted for baseline variables.
Secondary outcomes are as follows:
Difference in diastolic BP (DBP) (office BP, mean of second/third readings, mm Hg) at follow-up point (3 months and 6 months) between intervention and control group adjusted for baseline variables.
Difference in mean BP (uploaded HBP, mm Hg) during the trial (6 months) between intervention and control group.
Difference in mean BP (uploaded HBP, mm Hg) during the trial (3 months) between intervention and control group.
Percentage of weeks which mean HBP ≤135/85 mm Hg in total weeks by the end of third month and sixth month follow-up.
Adverse events: clinical events; the State-Trait Anxiety Inventory;21 side effects.
Medication outcomes: Medication Adherence Rating Scale,22 Beliefs about Medicine Questionnaire,23 The Stanford Expectations of Treatment Scale.24
Life habits: alcohol use disorders identification test-concise,25 diet, exercise, smoking.
Quality of life, EuroQol-5-Dimensions-5-Level (EQ-5D-5L)26 scores.
Participant timeline
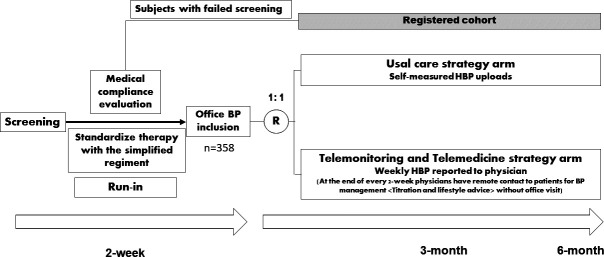
As shown in figure 1, a screening phase is set to check participants’ eligibility following the inclusion and exclusion criteria. After signing informed consent, the participants will receive a 2-week screening. Subjects who failed screening will be signed to the registered (real world) cohort, they will not be asked to self-monitor or receive any interventions, but will be invited to follow up for office BP measuring by the end of third month and sixth month, mainly to investigate how they manage their BP without any interventions, compared with control group.
Figure 1.
Schematic representation of the simple trial. During the screening phase, participants’ drug adherence will be fully evaluated. Participants who failed the screening will be directed to registered cohort. Participants who passed the screening will be stratified by centre during randomisation. There will be two office visits for all participants during run-in phase. Maximum duration of this trial will be 6 months. BP, blood pressure; HBP, home blood pressure.
During the follow-ups, participants in the intervention group will receive remote contact from physicians of each centre at the end of every 2 weeks, including medication titration plan (based on HBP uploads), lifestyle change suggestion (diet, smoke, alcohol etc.). Senior researchers will also receive feedbacks from participants during the teleconsultant. Participants in the control group will remain their own choice for clinic visit without further interventions. An office visit is required at the end of third and sixth month for both groups, trial-related information or data will be obtained as well (table 1).
Table 1.
Measurements and data collection
| Enrolment (21 December 2020) |
Screening visit | 3 months | 6 months | |
| Demographic questions | × | |||
| Office BP measurement | × | × | × | |
| Duration of hypertension and antihypertensive treatment | × | |||
| Smoking habits and alcohol intake | × | × | × | |
| Biochemical measurements | Optional* | Optional* | Optional* | |
| HBP 2-week hand-written record | × | |||
| HBP telemonitoring reports | × | × | ||
| EQ-5D-5L26 questionnaire | × | × | × | |
| SETS24 questionnaire | × | × | ||
| MARS22 questionnaire | × | × | ||
| BMQ23 questionnaire | × | × | × | |
| Lifestyle: Audit-C,25 diet, exercise, smoking | × | × | ||
| Adverse effects, anxiety (STAI)21 and side effects of medication | × | × | × | |
| Technical difficulties during trial | × | × |
*Only participants who are using spironolactone need to check blood monthly to monitor blood potassium level.
BMQ, Beliefs about Medicine Questionnaire; BP, blood pressure; EQ-5D-5L, EuroQol-5-Dimensions-5-Level; HBP, home blood pressure; MARS, Medication Adherence Rating Scale; SETS, Stanford Expectations of Treatment Scale; STAI, State-Trait Anxiety Inventory.
Sample size calculation
According to the previous studies, the intervention group lowered the average BP of patients by about 5 mm Hg compared with the control group, the SD of the patients’ BP was around 15 mm Hg.27 Based on a two-tailed test of two independent means, with a significance (α) level of 0.05% and 90% power, 155 patients were selected for each group. It was assumed that the drop-out rate of this study is no more than 15%, the study requires a total sample of 179 patients to be recruited in each group with a total of 358 patients.
Randomisation
Eligible patients are randomly assigned to the control and intervention group using a competitive design in clinical trial sites. Randomisation will be done after screening, ensuring that the assessing occupational therapist will not be biased at this time by knowing the group assignment. A random number will be generated before the start of this study. The random number list will be kept by the third party and uploaded into a random data assigned system. When participants are recruited, they will be assigned a random number by the system sequentially. If a patient is later excluded for any reason, the participant’s position in the randomisation list will not be replaced by any new participants. Senior researchers will generate the allocation sequence online and assign participants to interventions. Physicians will be blinded to both intervention and usual care group, considering usual care participants’ clinical visit may bring contaminations to the trial.
Target BP and titration of medication
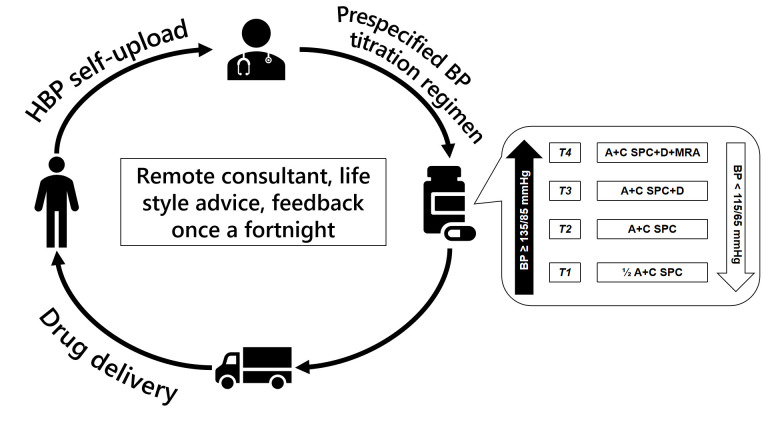
At the end of every 2-week remote follow-up, titration will be prescribed based on the 2-week average HBP in the intervention group under supervision of physicians. Antihypertensives titration regimen is shown in figure 2, referring to ISH 2020 guide.17 Three different types of anti-hypertensive drugs were used in this trial: a SPC containing perindopril arginine 10 mg and amlodipine 5 mg (COVERAM, Servier, France); a thiazide-like diuretic indapamide (NATRILIX, Servier, France) and a mineralocorticoid receptor antagonist spironolactone 20 mg (Yatai, China).
Figure 2.
Antihypertensives titration regimen of the simple trial. A+C SPC: ACEI +CCB SPC. T1: half dose of an SPC pill; T2: a full dose of SPC; T3: a full dose of SPC plus diuretic; T4: a full does of SPC plus diuretic plus MRA. ACEI, ACE inhibitor; HBP, home blood pressure; CCB, calcium channel blocker; MRA, mineralocorticoid receptor antagonist; SPC, single pill combination.
As shown in figure 2, if average HBP is below 135/85 mm Hg and above 115/65 mm Hg, the BP is in the green zone without any medication modification. Participants will keep their current medications. If average HBP is between 135/85 mm Hg and 155/105 mm Hg, antihypertensive agents will be upgraded (eg, T1→T2); if average HBP is between 155/105 mm Hg and 170/110 mm Hg, antihypertensive agents will be upgraded two level (eg, T1→T3); if average HBP is below 115/65 mm Hg, antihypertensives will be downgraded (eg, T2→T1); if average HBP is below 100/50 mm Hg or above 180/115 mm Hg, a visit to clinic will be required, event will be recorded, participants may choose whether continue or leave the trial.
Statistical analysis and data management
Statistical software R (V.4.0.2) is used for analyses. Analyses will be conducted on an intention-to-treat (ITT) and per-protocol population basis. Data for each assessment will be summarised for each treatment group and the descriptive statistics will be calculated depending on the data distribution for each assessment. Outcomes will be collected at the times defined in the study protocol. ITT analysis will be used to deal with the missing data for the primary outcome. An unpaired t-test will be used to analyse the difference between office SBP at baseline and office BP at 6-month follow-up between the intervention group and the control group. Subgroup factors include the elderly, men, smokers, patients with grade 2 hypertension and patients with poor compliance. A general linear mixed model will analyse the primary outcomes using data collected during 3-month and 6-month follow-up, adjusting for baseline variables. A p<0.05 will be considered to indicate statistical significance.
Clinical Research Institute of Shanghai Jiao Tong University Medicine School will be responsible as the data monitoring committee and for auditing trial conduct. The questionnaires are collected by researchers and recorded into the research electronic data collection system, which will be used as an electronic data collection (EDC) system for long-term data storage and management. Only authorised researchers can obtain these data. Data in the EDC system will be checked by built-in algorithm, monitored when some modification is required, and traceable to source data. Due to patient confidentiality and the possibility of access to EDC system, the collected clinical data will not be shared with the public.
Patient and public involvement
There was no patient or public involvement in the study design.
Ethics and dissemination
Ethics approval was granted by Ethical Committee of Shanghai Tenth People’s Hospital (SHSY-IEC-4.1/20-194/01). The results will be disseminated in peer-reviewed literature, and to policy-makers and healthcare partners. Any major modifications in protocol will be kept written record, protocol version will be updated, investigators, RECs, participants trial registries and journal regulators will be informed by email or phone call. Senior researchers will obtain and archive informed consent or assent from potential trial participants or authorised surrogates, participants may keep a copy or take photos of informed consent at their own discretion.
Discussion
This trial focuses on the feasibility of SPC-based telemedicine combined with BP self-monitoring compared with self-monitoring alone during hypertension management, also assesses whether the regimen is safe and effective for BP control of patients with uncontrolled hypertension and no other severe diseases.
The management of hypertension faced great challenge while COVID-19 pandemic28 hit the globe. During the pandemic, the number of clinical tests and consultations dramatically dropped, not only in China, but in well-developed European countries.29 Telemedicine and self-monitoring are not novel approach in hypertension management, since large randomised controlled trials proved their feasibility in control of BP, but there is still great challenge, which came from two different directions. One of them is patients’ low awareness of hypertension mediated organ damage and low compliance in taking BP measurements, for telemedicine requires patients’ higher activeness in management of hypertension. The other one comes from policy-makers, for they know little about how much benefit and the cost-effectiveness does telemedicine could bring, as a result, a systematic assessment on how to run a telemedicine procedure and how much the public can be benefited is urgently needed.
This study will investigate a simple strategy for BP managing, which may further lead to prevention of CVD and other severe complications.30 It may also help bring better quality of life by enabling better use of their time instead of spending much of it waiting in the hospitals on the premise that the technical difficulty related to telemedicine can be solved sufficiently.30 Especially in areas with large number of hypertension patients. It is always difficult for patients to visit doctors owing to the disproportion of numbers of doctors and patients in these countries.
Moreover, a clinic-free, simplified and unified telemedicine plan may help lighten the burden of public health both in cost and management of hypertension, especially during COVID-19 pandemic. Predictively speaking, with the rise of artificial intelligence, we hope that someday telemedicine and hypertension management can be greatly benefited from advanced technology, and we hope that this study can more or less contribute to this great goal.
Supplementary Material
Footnotes
YL and RM contributed equally.
Contributors: YL, RM, YZg, TF, YX, CJ and YZo participated in the conception and design of the study protocol; YL and RM wrote the first draft; YZg, CJ, TF and YZo reviewed the manuscript and contributed to the revision of the manuscript; RM, HY, JZ, JS, MW, FZ, JG and JH will be involved in the recruitment of participants and the acquisition of data. YL and TF will be responsible for data analysis. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Funding: This study is funded by Shanghai Tenth People’s Hospital, grant number 2021SYPDRC015, and funded by China International Medical Foundation (CIMF), grant number Z-2019-42-1908-3. This study is also funded by the CR LIFE SCIENCE TXT Healthcare and Technology (Beijing), grant number N/A. Special thanks to CR LIFE SCIENCET XT Healthcare team: Ying Zheng, Minle Wan, Wentao Zhang, Xiang Li, Yu Feng and Si Fan who made this trial possible both financially and technically.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Patel P, Ordunez P, DiPette D, et al. Improved blood pressure control to reduce cardiovascular disease morbidity and mortality: the standardized hypertension treatment and prevention project. J Clin Hypertens 2016;18:1284–94. 10.1111/jch.12861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2095–128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol 2020;76:2982-3021. 10.1016/j.jacc.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 2017;389:37–55. 10.1016/S0140-6736(16)31919-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation 2018;137:2344–56. 10.1161/CIRCULATIONAHA.117.032380 [DOI] [PubMed] [Google Scholar]
- 6.Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959–68. 10.1001/jama.2013.184182 [DOI] [PubMed] [Google Scholar]
- 7.Falaschetti E, Mindell J, Knott C, et al. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet 2014;383:1912–9. 10.1016/S0140-6736(14)60688-7 [DOI] [PubMed] [Google Scholar]
- 8.Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J 2013;34:2940–8. 10.1093/eurheartj/eht295 [DOI] [PubMed] [Google Scholar]
- 9.McManus RJ, Mant J, Franssen M, Bradley B, Lovekin C, Judge D, et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet 2018;391:949-959. 10.1016/S0140-6736(18)30309-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet 2010;376:163–72. 10.1016/S0140-6736(10)60964-6 [DOI] [PubMed] [Google Scholar]
- 11.McKinstry B, Hanley J, Wild S, et al. Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial. BMJ 2013;346:f3030. 10.1136/bmj.f3030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens 2006;8:174–80. 10.1111/j.1524-6175.2006.04872.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McManus RJ, Mant J, Haque MS, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA 2014;312:799–808. 10.1001/jama.2014.10057 [DOI] [PubMed] [Google Scholar]
- 14.Tucker KL, Sheppard JP, Stevens R, et al. Self-Monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med 2017;14:e1002389. 10.1371/journal.pmed.1002389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sheppard JP, Tucker KL, Davison WJ, et al. Self-Monitoring of blood pressure in patients with Hypertension-Related Multi-morbidity: systematic review and individual patient data meta-analysis. Am J Hypertens 2020;33:243–51. 10.1093/ajh/hpz182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CGftMo H, League CH. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med 2019;24:24–53. [Google Scholar]
- 17.Unger T, Borghi C, Charchar F, et al. 2020 International Society of hypertension global hypertension practice guidelines. Hypertension 2020;75:1334–57. 10.1161/HYPERTENSIONAHA.120.15026 [DOI] [PubMed] [Google Scholar]
- 18.Jones NR, McCormack T, Constanti M, et al. Diagnosis and management of hypertension in adults: NICE guideline update 2019. Br J Gen Pract 2020;70:90–1. 10.3399/bjgp20X708053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021–104. 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 20.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American heart association Task force on clinical practice guidelines. Hypertension 2018;71:e13–115. 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 21.Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait anxiety inventory (STAI). Br J Clin Psychol 1992;31:301–6. 10.1111/j.2044-8260.1992.tb00997.x [DOI] [PubMed] [Google Scholar]
- 22.Horne R, Weinman J,. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 1999;47:555–67. 10.1016/s0022-3999(99)00057-4 [DOI] [PubMed] [Google Scholar]
- 23.Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health 1999;14:1–24. 10.1080/08870449908407311 [DOI] [Google Scholar]
- 24.Younger J, Gandhi V, Hubbard E, et al. Development of the Stanford expectations of treatment scale (sets): a tool for measuring patient outcome expectancy in clinical trials. Clin Trials 2012;9:767–76. 10.1177/1740774512465064 [DOI] [PubMed] [Google Scholar]
- 25.Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction 1993;88:791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- 26.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maimaitiaili R, Teliewubai J, Zhao S, et al. Relationship between vascular aging and left ventricular concentric geometry in community-dwelling elderly: the Northern Shanghai study. Clin Interv Aging 2020;15:853–63. 10.2147/CIA.S248816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shah S, Diwan S, Kohan L, et al. The technological impact of COVID-19 on the future of education and health care delivery. Pain Physician 2020;23:S367–80. [PubMed] [Google Scholar]
- 29.Omboni S. Telemedicine during the COVID-19 in Italy: a missed opportunity? Telemed J E Health 2020;26:973–5. 10.1089/tmj.2020.0106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yatabe MS, Yatabe J, Asayama K, et al. The rationale and design of reduction of uncontrolled hypertension by remote monitoring and telemedicine (remote) study. Blood Press 2018;27:99–105. 10.1080/08037051.2017.1406306 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-049162supp001.pdf (565.7KB, pdf)
bmjopen-2021-049162supp002.pdf (153KB, pdf)
bmjopen-2021-049162supp003.pdf (1.3MB, pdf)