Abstract
Introduction
Small molecule inhibitors of the terminal step in intrahepatic triglyceride synthesis (diacylglycerol acyltransferase 2 inhibitor (DGAT2i, PF-06865571, ervogastat)) and upstream blockade of de novo lipogenesis via acetyl-coenzyme A carboxylase inhibitor (ACCi, PF-05221304, clesacostat) showed promise in reducing hepatic steatosis in early clinical trials. This study assesses efficacy and safety of these metabolic interventions to resolve non-alcoholic steatohepatitis (NASH) with fibrosis.
Methods and analysis
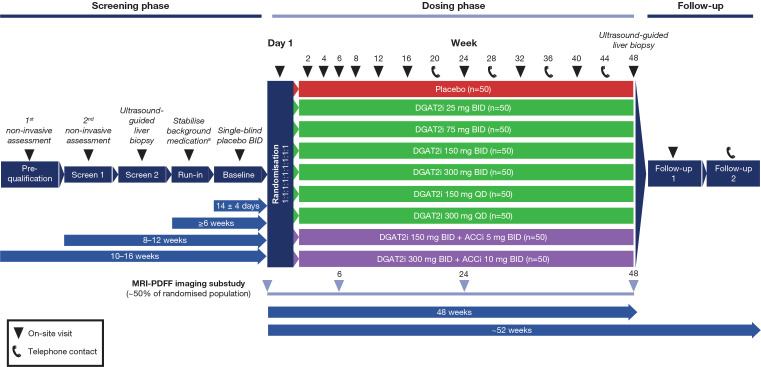
This phase II, randomised, dose-ranging, dose-finding study evaluates DGAT2i 25–300 mg two times per day (BID) or 150–300 mg once a day, DGAT2i 150–300 mg BID+ACCi 5–10 mg BID coadministration or matching placebo in a planned 450 adults with biopsy-confirmed NASH and liver fibrosis stages 2–3 from approximately 220 sites in 11 countries across North America, Europe and Asia. A triage approach including double-confirmation via non-invasive markers is included prior to screening/baseline liver biopsy. On confirmation of histological diagnosis, participants enter a ≥6-week run-in period, then a 48-week double-blind, double-dummy dosing period. The primary endpoint is the proportion of participants achieving histological NASH resolution without worsening fibrosis, ≥1 stage improvement in fibrosis without worsening NASH, or both, assessed by central pathologists. Other endpoints include assessment of hepatic steatosis (imaging substudy), overall safety and tolerability, and evaluation of blood-based biomarkers and quantitative ultrasound parameters over time.
Ethics and dissemination
Metabolic Interventions to Resolve NASH with fibrosis (MIRNA) is conducted in accordance with the Declaration of Helsinki and Council for International Organisations of Medical Sciences (CIOMS) International Ethical Guidelines, International Council on Harmonisation Good Clinical Practice guidelines, applicable laws and regulations, including privacy laws. Local independent review board/ethics committees (IRB/ECs) review/approve the protocol, any amendments, informed consent and other forms. Participants provide written informed consent. Details of all IRB/ECs, as well as results, will be published in a peer-reviewed journal and publicly disclosed through ClinicalTrials.gov, EudraCT, and/or www.pfizer.com and other public registries as per applicable local laws/regulations.
Trial registration number
Keywords: hepatology, clinical trials, magnetic resonance imaging, histopathology
Strengths and limitations of this study.
This is the first clinical study to evaluate histological endpoints after oral administration of diacylglycerol acyltransferase 2 inhibitor (DGAT2i) and DGAT2i+acetyl-coenzyme A carboxylase inhibitor in participants with biopsy-confirmed non-alcoholic steatohepatitis and fibrosis stage F2 or F3.
A triage approach (including double-confirmation via non-invasive blood and quantitative ultrasound-based markers prior to screening/baseline liver biopsy), coupled with central reading of all liver biopsies with consensus required to determine eligibility and assess drug(s) effects, is designed to improve efficiency in identifying participants likely to meet histological entry criteria and robust confidence in histological findings.
The dosing period includes a longitudinal evaluation of non-invasive imaging and blood-based biomarkers, to identify correlations between histological parameters and non-invasive imaging and/or blood-based biomarkers, in order to assess drug effects.
The Bayesian dose–response modelling methodologies employed enable an efficient and complete characterisation of dose–response, to aid phase III dose selection.
This study is limited in that the design relies on assumptions around the translation of effects observed in earlier non-biopsy studies to a histological endpoint; the impact of the drug(s) on clinical outcomes will need confirmation in an adequately sample-sized phase III trial.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is characterised by excessive accumulation of intrahepatic lipids, especially triglycerides (steatosis) and estimated to affect >25% of the global population.1 2 A progressive subtype of the disease, non-alcoholic steatohepatitis (NASH), is defined by cellular injury and inflammation2 and affects 21%–25% of people with NAFLD.3 4 NASH drives fibrogenesis,5 and fibrosis stage is linked to disease outcome and mortality.6–9
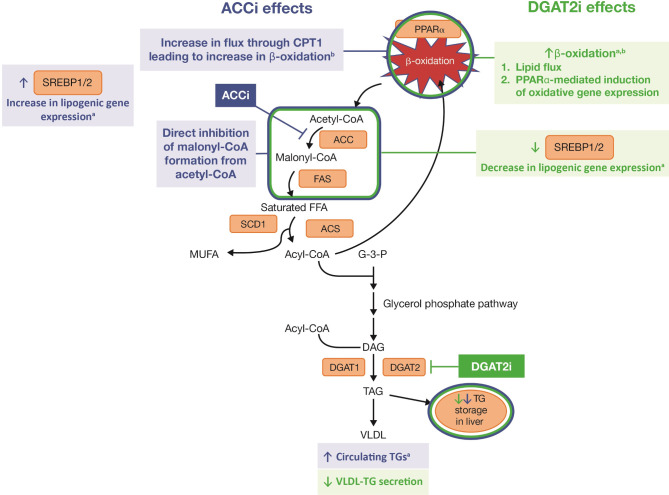
Targeting molecular pathways involved in the early pathogenesis and abnormal accumulation of hepatic steatosis could prevent inflammation, cellular injury and fibrosis, thus offering potential treatments for patients with NASH and liver fibrosis. Acetyl-coenzyme A carboxylase (ACC) and diacylglycerol acyltransferase 2 (DGAT2) each play a role in hepatic steatosis (figure 1). De novo lipogenesis (DNL) is more active in patients with NAFLD than in healthy individuals and may contribute to excess hepatic triglycerides,10 with ACC being the first committed enzyme in the hepatic DNL pathway.11 DGAT2 is highly expressed in the liver and adipose tissue12 and catalyses the terminal step of DNL, specifically the esterification of a fatty acid with diacylglycerol to form triglyceride.13 Independent inhibition of each of these steps has been shown to reduce hepatic steatosis. Sterol regulatory element-binding protein 1c (SREBP1c) is a metabolic switch that governs hepatic lipogenesis,14 15 and ACC inhibition is associated with upregulation of SREBP1c activity, but reduced steatosis in hepatocytes.11 Conversely, inhibition of DGAT2 was found to down-regulate SREBP1c activity, which in turn reduced hepatic lipogenesis;16 in addition, a small molecule inhibitor of DGAT2, PF-06427878, reduced hepatic steatosis in a rodent model and clinically after 2 weeks of dosing.17 In patients with NAFLD, oral administration of another small molecule inhibitor of DGAT2 (DGAT2i, PF-06865571, ervogastat) for 14 days resulted in dose-dependent reductions in both liver fat and serum triglycerides.18 In addition to its effects on steatosis, ACC inhibition may have direct antifibrotic effects in hepatic stellate cells, the collagen-producing fibroblast population in the liver; in rodent models, ACC inhibition abrogated a metabolic switch necessary for induction of glycolysis and oxidative phosphorylation during hepatic stellate cell activation in vitro, thereby reducing hepatic fibrosis.19
Figure 1.
Effects of ACC and DGAT2 inhibition on hepatic lipid metabolism.11 13 16 27 50 aAdaptive effects. bIn non-clinical models. ACC, acetyl-coenzyme A carboxylase; ACCi, ACC inhibitor; ACS, acyl-CoA synthetase; CoA, coenzyme A; CPT1, carnitine palmitoyl transferase 1; DAG, diacylglycerol; DGAT, diacylglycerol acyltransferase; DGAT2i, DGAT2 inhibitor; FAS, fatty acid synthase; FFA, free fatty acid; G-3-P, glycerol-3-phosphate; MUFA, monounsaturated fatty acid; PPARα, peroxisome proliferator-activated receptor α; SCD1, stearoyl-CoA desaturase 1; SREBP, sterol regulatory element-binding protein; TAG, triacylglycerol (also known as triglyceride); TG, triglyceride.
In clinical trials, liver-targeted ACC-inhibiting agents have been associated with potent reductions in hepatic steatosis, but with accompanying elevations in serum triglycerides.11 20 21 Doses ≥40 mg/day of a liver-targeted ACC inhibitor (ACCi; PF-05221304, clesacostat) showed near-complete DNL inhibition for 0–10 hours after 14 days of dosing in healthy adults, but these doses were accompanied with increases in serum triglycerides.22 However, doses <40 mg/day still inhibited DNL by up to 80% but without elevated serum triglycerides.22 Based on this observation in healthy adults, doses ≤50 mg/day were evaluated in a phase IIa dose-ranging trial with the ACCi in participants with NAFLD and presumed NASH.23 Reductions in liver steatosis, markers of liver inflammation (alanine aminotransferase (ALT), aspartate aminotransferase (AST)) and markers of hepatocyte cell death (cytokeratin (CK)18-M30 and CK18-M65) were observed following 16 weeks of dosing.23 However, these potentially beneficial effects were accompanied by marked elevations in fasting serum triglycerides,23 which is a known mechanistic consequence of hepatic ACC inhibition.11 20 Notably, the magnitude of this serum triglyceride increase appears to be higher in adults with NAFLD/presumed NASH than in healthy adults.22 23 It could be hypothesised that the increased SREBP1c tone in patients with NAFLD, potentially due to hyperinsulinaemia, makes patients more sensitive to ACCi and resultant SREBP activation, compared with healthy adults.24–26
While independent inhibition of either upstream (ACC) or downstream (DGAT2) pathways may have limited efficacy for pharmacological treatment of NASH, based on the scientific evidence (figure 1), evaluation of DGAT2i and ACCi together is intriguing given the opposing effects on SREBP1c. Indeed, in rodent models, DGAT2i+ACCi reduced steatosis as well as inflammation and fibrosis markers without the expected ACCi-associated increases in serum triglycerides.27 In a 6-week, phase IIa trial in patients with NAFLD, DGAT2i 300 mg two times per day (BID)+ACCi 15 mg BID reduced hepatic steatosis to a similar degree as ACCi alone and to a greater degree than DGAT2i alone, as assessed by magnetic resonance imaging-proton density fat fraction (MRI-PDFF).23 The nadir for effect on liver fat was observed at 12–16 weeks with ACCi alone and was not determined for DGAT2i+ACCi.23 Notably, ACCi-induced elevations in triglycerides (47% increase relative to placebo) were effectively mitigated by DGAT2i+ACCi.23
Metabolic Interventions to Resolve NASH with fibrosis (MIRNA, NCT04321031) is a phase II, randomised, placebo-controlled, dose-ranging, dose-finding study that assesses the efficacy and safety of an investigational, orally administered DGAT2i and DGAT2i+ACCi in adults with biopsy-confirmed NASH and liver fibrosis stage 2 or 3, as defined using NASH-Clinical Research Network (NASH-CRN) criteria.28 MIRNA is envisioned to add to the body of scientific evidence by assessing histological endpoints, such as NAFLD Activity Score (NAS) and liver fibrosis. MIRNA is supplemented by a concurrent, short-term (6-week dosing), phase IIa trial of DGAT2i+ACCi (NCT04399538) that aims to identify the lowest dose of DGAT2i that can mitigate ACCi-induced adverse effects on serum lipids, to further aid in the optimal selection of dose(s) of DGAT2i+ACCi for subsequent pivotal studies.
Methods and analysis
Study design
MIRNA is a randomised, double-blind, double-dummy, placebo-controlled, dose-ranging, dose-finding, 9-arm, parallel-group study conducted across approximately 220 planned sites in Bulgaria, Canada, China, Hong Kong, India, Japan, South Korea, Poland, Slovakia, Taiwan and the USA (including Puerto Rico). Recruitment initiated in June 2020 in the USA and is ongoing. Randomisation is estimated to be completed in December 2022. This study includes a total of 22 on-site visits and telephone contacts, and each participant’s time in the study ranges from 62 to 68 weeks (figure 2). Given the prior clinical experience of ≤6 weeks with DGAT2i and DGAT2i+ACCi,23 frequent post-randomisation visits have been planned to permit close monitoring of safety. Procedures throughout MIRNA are summarised in online supplemental table 1. A blinded Steering Committee comprising both external and internal medical/clinical representatives from each country/region of study operations will oversee recruitment, retention and quality issues within the country/region.
Figure 2.
MIRNA study design. The intervals depict the maximum time between the various periods in the study. aIn addition, metformin dose reduced if dose is >1 g/day. ACCi, acetyl-CoA carboxylase inhibitor; BID, two times per day; DGAT2i, diacylglycerol acyltransferase 2 inhibitor; MIRNA, Metabolic Interventions to Resolve NASH with fibrosis; MRI-PDFF, magnetic resonance imaging-proton density fat fraction; n, target number of participants; QD, once a day.
bmjopen-2021-056159supp001.pdf (191.4KB, pdf)
Eligibility is determined in a three-step process
Guidance from the European Association for the Study of the Liver and American Association for the Study of Liver Disease recognises the significant interest in non-invasive biomarkers for identifying NASH;29 30 as such, MIRNA aims to reduce the burden of liver biopsies by using non-invasive techniques to identify eligible participants that are most likely to exhibit NASH, thus increasing selection efficiency. Medical history review, medication use and blood-derived assessments are used to exclude other causes of NAFLD and other liver diseases. Stability of liver function measurements is confirmed during the pre-qualification and first screening visits. Double-confirmation of liver fat and stiffness using quantitative ultrasound (FibroScan®, EchoSens, Paris, France), along with AST to derive FASTTM scores,31 are used to identify participants qualifying for a screening/baseline liver biopsy. In a prospective derivation and global validation study, FAST score cut-offs for sensitivity (≥0.90) of 0.35 and for specificity (≥0.90) of 0.67 were reported, leading to a positive predictive value of 0.83 (84/101) and a negative predictive value of 0.85 (93/110).31 A slightly lower cut-off of ≥0.30 is used in MIRNA since this threshold needs to be met twice, with an expected missed case rate (participants with NASH and F2 or F3 who do not undergo biopsy based on FAST score) of 9.7% and expected screen fail rate (participants undergoing biopsy based on FAST but fail on biopsy) of 49.5%, indicating that two participants would need to be biopsied to detect one eligible participant.31
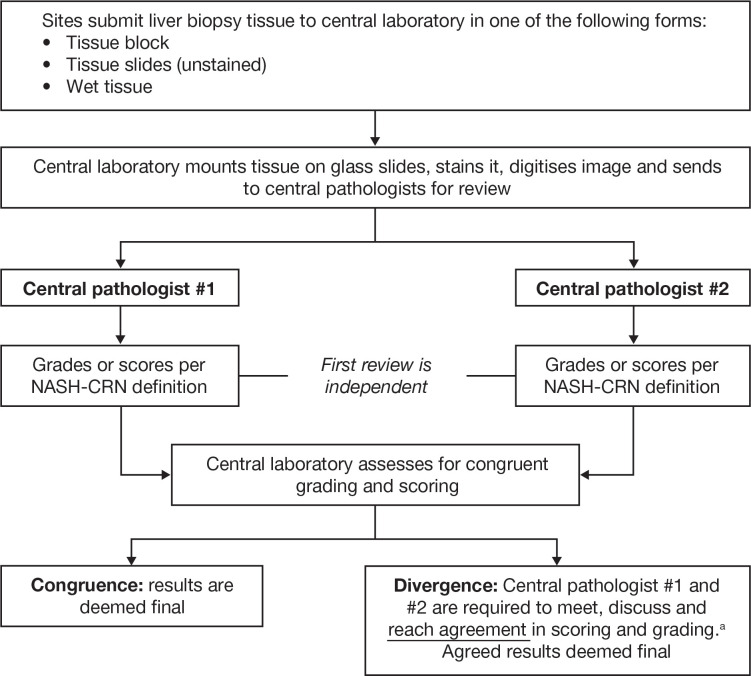
Participants who qualify based on the non-invasive assessments at the pre-qualification and first screening visits undergo a standardised, ultrasound-guided biopsy of the right lobe of the liver using either a 16-guage or 18-gauge suction or cutting needle, to acquire tissue ≥1.5 cm in length to determine eligibility based on liver histology. Biopsies are graded and scored, using the NASH-CRN definition,28 32 by central, NASH-CRN pathologists (figure 3). The eligible population is defined as participants with a NAS ≥4 and either F2 or F3 fibrosis. All eligibility criteria are listed in online supplemental table 2.
Figure 3.
Prospective, centralised grading and scoring of liver biopsies at screening for eligibility using the NASH-CRN definition. aConsensus review to reach agreement is not required if both pathologists agree that either the NAFLD Activity Score or fibrosis grade renders the participant ineligible. NAFLD, non-alcoholic fatty liver disease; NASH-CRN, Non-Alcoholic Steatohepatitis Clinical Research Network.
To optimise the evaluable data and limit sampling variability that can confound biopsy results,33 MIRNA employs careful standardisation of biopsy collection including ultrasound guidance, use of specific biopsy needle size and assessment limited to the right lobe only. MIRNA also utilises prospective, central biopsy reading by two blinded pathologists for eligibility (and evaluating endpoints), using digitised images to shorten the time needed to judge eligibility. Each pathologist qualitatively assesses each domain of NAS and fibrosis.
For assessment of biopsy-related endpoints at week 48 or discontinuation, review by central pathologists initially independently—and when needed, consensus review to reach agreement—will be performed via paired, blinded assessment of digitised images. In this process, each pathologist assesses the eligibility/screening (baseline biopsy) alongside the week 48/discontinuation biopsy, for a given participant. The pathologists are blinded to the nominal timepoints and treatment arm, minimising bias when assessing drug(s) effects. Divergence in grading or staging between pathologists is handled in the same way as outlined in figure 3 except that for endpoint assessment, agreement between the two pathologists is required for all four domains (steatosis, inflammation, ballooning and fibrosis), thus adding rigour to the determination of histological-based endpoints.
Participants are stabilised during run-in and baseline periods
After the liver biopsy is performed (ie, screen 2), participants start a 6-week run-in period prior to randomisation to generate an in-study, stable state for all participants in terms of medical history and medication use (including compliance). In consideration of potential drug–drug interactions, participants taking gemfibrozil are switched to another permitted agent for lipid control, and those taking metformin >1 g/day have their dose adjusted down by one-third to one-half to 1 g/day, starting at the run-in visit (online supplemental table 3). Standardisation of lifestyle guidelines across all sites and countries is advocated;34 35 in MIRNA, accounting for operational considerations and local practices, lifestyle guidelines advocating healthy choices that do not result in overt weight loss during the course of the study are implemented to minimise placebo response. The Alcohol Use Disorders Identification Test questionnaire is used before randomisation and at the end of study dosing to confirm that alcohol intake is in moderation during the study (online supplemental table 1). Single-blind placebo is administered over a 2-week period before randomisation to confirm that participants can comply with dosing instructions for the study drug (ie, three tablets/dose, two times per day with meals). Participants are provided with electronic devices auto-programmed with periodic reminders to enhance compliance (from baseline to end-of-dosing period). These steps are intended to account for the ‘Hawthorne effect’, wherein changes in participant behaviour occur because of increased knowledge or interest or due to the perception of being observed. They help limit placebo response, thus permitting ascertainment of drug effect.
Randomised participants are treated for up to 48 weeks and followed for an additional 4 weeks
On day 1, eligible participants are randomised to one of nine arms using a computer-generated randomisation code (random permuted blocks method) and stratified by fibrosis stage (F2 or F3), to ensure a balance of participants across regimens. Participants are randomly allocated to treatment groups by blinded investigators using an interactive response technology system (interactive web response) programmed with instructions for unblinding only in emergency situations for reasons of participant safety, as determined by the investigator. Study drugs are self-administered in a double-blind, double-dummy manner for 48 weeks, in line with regulatory guidance for agents in development for NASH with fibrosis.36 37 A follow-up on-site visit occurs 2 weeks post-last dose with a follow-up phone call approximately 4 weeks after the last dose. Participants and all persons involved in trial conduct, participant interactions and data analysis are blinded to treatment assignment.
Approximately half of the total sample size are participating in an imaging substudy to characterise the effect on liver steatosis and liver volume over time
Approximately 50% of participants are forecast to be enrolled in an imaging substudy to (1) characterise the dose–response for effect on liver steatosis using MRI-PDFF; (2) characterise the drug effect over time and define the time to maximum effect (ie, nadir) and (3) assess the correlation of liver fat and volume assessed by MRI-PDFF (and other associated imaging and laboratory-based endpoints) with histology endpoints.
Concomitant medications are allowed with some adjustments
All concomitant medications taken during the study (online supplemental table 3), including herbal supplements in countries where they are part of standard of care to lower liver function test measurements, are recorded along with indication of use. Additional information including daily dose and duration of administration are captured for medications used for glycaemic control, lipid control and blood pressure control.
Patient and public involvement
Input from patients with biopsy-confirmed diagnoses of NASH was sought while designing MIRNA. Their feedback led to revisions in the protocol (final version 22 January 2020) regarding the manner by which information is provided to prospective participants in the informed consent document. These included explaining why the intervention may work and the associated benefits and risks, information about efforts to minimise biopsy for diagnosis and about tracking drug effects and the rationale for the blood volume collected and the intent to use blood samples to evaluate preidentified and new biomarkers at a later date. Blister packs (rather than bottles) are being utilised to aid compliance and acknowledge pill burden, while balancing the requirements of the double-blind, double-dummy design. Additionally, participant-friendly reminders and milestone communications were incorporated into the study.
Selection of DGAT2i and ACCi doses to maximise liver fat reduction
Dose selection was informed by exposure–response modelling of historical pharmacokinetic and reduction in liver fat data observed following 2 weeks of DGAT2i dosing;18 6 weeks of DGAT2i, ACCi and DGAT2i+ACCi; and 16 weeks of ACCi.23 The half-maximal effective concentration (EC50) for liver fat reduction was estimated as 41 ng/mL for DGAT2i, and represents a dose of approximately 30 mg BID. A 300-mg BID dose was projected to achieve a near maximal effect on liver fat reduction, and it was hypothesised that DGAT2i 300 mg BID coadministered with ACCi would further extend the effect of DGAT2i. Using both exposure–response analysis and quantitative systems pharmacology modelling, DGAT2i doses of 25, 75, 150 and 300 mg BID were chosen. Additionally, DGAT2i doses of 150 mg and 300 mg once a day (QD) were selected to compare QD with BID regimens at the same daily dose (75 and 150 mg BID). This will help determine if similar efficacy is achievable with equivalent QD and BID dosing while testing for potential dissociation between plasma pharmacokinetic profiles and pharmacology.
Two dose levels of DGAT2i+ACCi are being evaluated—DGAT2i 300 mg BID+ACCi 10 mg BID and DGAT2i 150 mg BID+ACCi 5 mg BID — to assess whether ACCi coadministration extends DGAT2i efficacy. ACCi 10 mg BID yields 80% DNL inhibition;22 on a mg-per-mg basis for both doses the ratio is maintained at 30:1 (DGAT2i:ACCi) to enable evaluation of both efficacy and safety of DGAT2i+ACCi relative to DGAT2i alone. Although ACCi has a pharmacokinetic half-life conducive to QD dosing,22 a BID dosing regimen was selected to match the likely frequency of clinical dosing for DGAT2i.
Dose selection and dose range from this and the ongoing phase IIa trial (NCT04399538) investigating a wider dose range for DGAT2i+ACCi in patients with presumed NASH may aid in determining the optimal dose(s) of DGAT2i and DGAT2i+ACCi to evaluate in confirmatory phase III trials.
Objectives, estimands and endpoints
Clinical responders based on histological evidence
The primary endpoint of MIRNA is the proportion of participants achieving resolution of NASH (ie, absence of ballooning with no or minimal inflammation by histology)36 without worsening of fibrosis, or improvement in fibrosis by ≥1 stage without worsening of NASH, or both, at week 48, as assessed by central pathologists. This is based on histological assessment at screening/baseline liver biopsy, and at end of drug administration (ie, week 48 or earlier in cases of premature withdrawal of study drug, provided the study drug was administered up to at least week 24), in all randomised and treated participants with evaluable baseline biopsy data. Using a composite estimand strategy, drug effect is estimated in terms of the proportion of ‘clinical responders’, defined as participants achieving the primary endpoint.38 All cases of withdrawal from study drug(s) due to lack of efficacy or toleration are treated as non-responders. Participants who withdraw from study drug(s) for other reasons but have evaluable biopsy data at withdrawal or week 48 will have their biopsy data assessed to determine whether they are responders or not. Participants with no week 48 biopsy data are considered to be non-responders.
Secondary endpoints include the percent change in liver fat (assessed via MRI-PDFF in the substudy population), the proportion of participants achieving improvements in responder definitions (resolution of NASH without fibrosis worsening, ≥1- or ≥2-stage fibrosis improvement without NASH worsening, ≥2-point improvement in total NAS score), assessment of adverse events (AEs) up to week 52 and safety-related clinical laboratory tests (including full blood and platelet counts), vital signs and 12-lead ECGs to at least week 50. The secondary efficacy endpoints employ a composite estimand strategy for the histological assessments, whereby the responder definitions are evaluated based on histological assessment at week 48 relative to baseline.
The tertiary endpoint is the proportion of the population with worsening disease at week 48, defined as progression of fibrosis by ≥1 stage and worsening of ≥2 points in total NAS.
Secondary and tertiary objectives include evaluation of safety/tolerability and clinical response on imaging and blood-based biomarkers
Analysis of all imaging and laboratory parameters is performed by external vendors who are blinded to treatment assignment to ensure the blind is preserved and to minimise any bias in assessment of the study endpoints.
Safety and tolerability
These assessments include 12-lead ECG, blood pressure, pulse rate, body weight measurements, open-ended enquiries of AEs, collection of blood and urine for assessment of haematology, chemistry and urinalysis (online supplemental table 4). Reasons for discontinuation of study drug include sustained fasting serum triglyceride levels ≥800 mg/dL (≥9 mmol/L), platelet count <75 000/mm3 or other AEs based on medical judgement. An independent external data monitoring committee consisting of medical experts and a statistician will be responsible for ongoing review of unblinded data to assess safety. Unblinded data analysis for this explicit purpose is undertaken by a dedicated independent external vendor (Statistical Data Analysis Center, University of Wisconsin, USA). In addition, an independent adjudication committee consisting of external experts will perform blinded review of all potential fatal events, hepatic events (including decompensation, histological progression to cirrhosis, hepatocellular carcinoma or drug-induced liver injury) or cardiovascular events (including major adverse cardiovascular events) to confirm that the data support the endpoint designation. Interim analyses will be performed to assess safety, at a minimum, after approximately 25%, 50% and 75% of planned total sample size have been randomised in the study. Interim analysis results may be used for future study planning, including adapting safety-related endpoints.
Imaging assessments
Considering the primary pharmacology of DGAT2i and ACCi, liver fat and volume (via MRI-PDFF) are assessed as a secondary objective in the imaging substudy. In addition, FibroScan is being used to measure liver fat via the controlled attenuation parameter (CAP), and liver stiffness via vibration-controlled transient elastography (VCTETM), over time. Study-specific manuals emphasise the use of M and XL probes guided by SMART tools on the FibroScan® device, including evaluation of tissue change in TM-mode and ultrasound signal strength and propagation in A-mode.
Both MRI-PDFF and FibroScan assessments are performed following a fast (except water) of ≥4 hours. The MRI-PDFF acquisition protocol is standardised a priori across all sites participating in the substudy, with images centrally analysed using validated, two-dimensional, six-echo, spoiled gradient-recalled-echo, breath-hold pulse sequences.39 MRI-PDFF image analyses are performed by a blinded external vendor; a 2.5 cm diameter region of interest is applied on each of nine anatomical liver segments, except for the caudate where a 1.5 cm diameter region of interest is identified.
Blood-based biomarkers
Any potential pharmacological consequences of DGAT2i and DGAT2i+ACCi are being studied via blood-based biomarkers summarised in table 1.
Table 1.
Blood-based biomarkers assessed in MIRNA
| Parameter | Biomarker |
| Liver function tests |
|
| NASH-related |
|
| Fasting lipid parameters/markers of target engagement |
|
| Glycaemic |
|
Additional samples collected for exploratory biomarker analysis are listed in online supplemental table 4.
HbA1c, glycated haemoglobin; MIRNA, Metabolic Interventions to Resolve NASH with fibrosis; NASH, non-alcoholic steatohepatitis.
Sparse blood sampling for pharmacokinetic analyses over the 48-week dosing period is included to estimate drug exposure and help describe the relationship between dose, concentration and efficacy/safety of DGAT2i and DGAT2i+ACCi via population pharmacokinetics and pharmacokinetic/pharmacodynamic analyses. Additionally, blood samples are collected for exploration of other plasma-biomarkers or serum-biomarkers and single nucleotide polymorphisms linked to NASH.
Statistical considerations
Sample size
Sample size estimation is driven by the characterisation of dose–response and drug effect using a Bayesian maximum effect of drug (Emax) study design and modelling approach, which utilises weakly informative priors for model parameters. This approach increases the precision in drug/dose comparisons (online supplemental table 5) and enables the required sample size to be reduced by almost half compared with conventional pairwise comparisons. Nonetheless, MIRNA is over-enrolling by approximately 20% (450 participants with 50 per arm) to minimise the risk of an underpowered study due to a lack of primary endpoint data. Anticipated reasons for insufficient primary endpoint data include non-evaluable biopsies, participant withdrawal and inconsistencies in scoring/grading digitised slides when determining eligibility and pairwise (second screening and end-of-dosing period visits) blinded review.40 The decision to over-enrol in MIRNA was informed by learnings from a previous trial, which reported statistically significant improvements in some secondary endpoints (glucose, HbA1c, fasting plasma insulin, liver enzymes and NAS), but not primary and secondary histological endpoints after treatment with an insulin sensitiser for NASH, due to issues with interpretation of liver biopsies.41
Priors for Emax model parameters were evaluated and for DGAT2i, ED50 was estimated to be approximately 30 mg BID (based on the projected EC50) and the placebo responder rate (E0) was estimated to be 16%. Based on the above assumptions, at the theoretical Emax of 0.6 (ie, a 60% responder rate) and an estimated sample size of 450 participants, there is enough precision to show a >24% difference in the primary endpoint responder rate between placebo and the second-highest DGAT2i dose, 150 mg BID, with a probability of ≥89%. In addition, a sample size of 450 participants provides 75% power to demonstrate a 24% difference in the primary endpoint responder rates between QD doses and placebo, and adequate precision to assess whether DGAT2i+ACCi provides a higher responder rate than DGAT2i with a probability of 82% if the true effect size is at least 6%.
Interpathologist and intrapathologist variability
Variability is assessed quarterly on a randomly selected sample comprising 10% of screening biopsies and week 48/discontinuation biopsies from randomised participants. Pathologists review the same biopsy images ≥3 months apart, to ascertain if the same levels of calibre are maintained over time (intrapathologist variability). Reviews by the pathologists are compared with NASH-CRN peers using weighted kappa statistics (interpathologist variability).
Statistical models
In assessing the primary objective, a Bayesian dose–response model will characterise the dose–response across all DGAT2i BID arms, to estimate the proportion of responders (and 95% CI) for each dose, and to estimate the placebo-adjusted proportion of responders for each dose (with 95% CI). The Bayesian estimation of the Emax dose–response model uses prior distributions on the placebo response (E0), as well as the ED50 (30 mg BID) and Emax parameters. A normal prior distribution for the logit of the placebo response centred at logit (0.16) with a prior SD of 2.0 (logistic scale) is planned to be used, and similarly, the prior for the Emax parameter will be centred at logit (0.6) with a prior SD of 2.0. These are diffuse parameters on the logistic scale, which will ensure that the data collected in this study are not overly influenced by these prior distributions, while ensuring convergence of the Bayesian dose–response model. If an Emax dose–response model cannot be fitted to the data, other models that allow dose–response to be estimated will be fitted (ie, linear, log-linear, or exponential).
Similar Bayesian dose–response models will be utilised for the secondary objectives of achievement of different responder definitions based on histological outcomes. Other comparisons (DGAT2i QD doses vs placebo, and DGAT2i+ACCi BID doses vs placebo and vs corresponding DGAT2i BID doses) will be analysed using logistic regression models to estimate the proportion of responders in each arm and OR (95% CI) for each comparison.
For the secondary objective of percent change from baseline in liver fat, all drug effect contrasts will be based on a hypothetical estimand strategy, which assumes that all participants remained in the trial for 48 weeks and received study drug(s) as planned without withdrawal. Any available MRI data for all participants is included, including those who withdrew from study drug(s) due to lack of efficacy or toleration. If the week 48 response is missing, this is imputed using a model-based analysis based on the treatment arm assigned at randomisation. This will follow the average treatment effect as observed in the same assigned treatment arm. A Bayesian Emax dose–response model for the DGAT2i BID doses will also be utilised. Other dose group comparisons will use an analysis of covariance performed on log-transformed relative change from baseline, with dose group and baseline fibrosis stage (F2 or F3) as factors and log-transformed baseline liver fat value as a covariate. Estimates of the mean relative changes for each dose comparison and 95% CI will be obtained from the model and will be exponentiated to provide estimates of the percent change. For comparisons of DGAT2i+ACCi BID doses vs corresponding DGAT2i BID doses, 50% CI will also be calculated. No adjustment for multiple comparisons will be made. Safety analyses will be summarised descriptively.
Ethics and dissemination
MIRNA is conducted in accordance with ethical principles derived from the Declaration of Helsinki and CIOMS International Ethical Guidelines, applicable International Council for Harmonisation Good Clinical Practice guidelines, and applicable laws and regulations, including privacy laws. Before the study is initiated, the protocol, protocol amendments (if any), informed consent and other forms are reviewed and approved by local independent review board/ethics committees (IRB/ECs): central IRB, WCB IRB tracking number 20200277, for sites initiated in the USA. Local approvals are ongoing, and a full list of IRB/ECs will be disclosed with the study results on completion. Study participants provide written informed consent to investigators at pre-qualification and separately when entering the main study at the first screening visit, with additional consent required for the imaging substudy. Participants may withdraw from the study at any time. Given a screening population without biopsy-confirmed NASH, the triage approach necessitates screening many prospective participants. Only those participants with biopsy-confirmed NASH and fibrosis receive study-specific information to minimise anxiety in those who do not have NASH with fibrosis. Information provided at pre-qualification incorporates education about NAFLD and NASH, including risk factors. All parties are required to comply with all applicable laws, including laws regarding the implementation of organisational and technical measures to ensure protection of participant data. All participant data relating to the study will be recorded on printed or electronic case report forms (CRFs) unless transmitted to the sponsor or designee electronically (eg, laboratory data). The investigator is responsible for verifying that data entries are accurate, maintaining accurate documentation (source data) that supports information entered into the CRFs and ensuring that the CRFs are securely stored at the study site in encrypted electronic form, password protected to prevent access by unauthorised third parties. The investigator must permit study-related monitoring, audits, IRB/EC review and regulatory agency inspections and provide direct access to source data documents. The sponsor or designee is responsible for the data management of this study, including quality checking of the data.
As per patient feedback that was incorporated into the design of MIRNA, aggregate-level summaries of study results in lay language are to be disseminated to randomised participants; study results will be publicly disclosed 24 months after completion, through posting on www.clinicaltrials.gov, the EudraCT and/or www.pfizer.com and other public registries in accordance with applicable local laws/regulations. Participant-level data will be anonymised in accordance with applicable privacy laws and regulations. The results of MIRNA may be published or presented at scientific meetings by the investigators after disclosure of the overall study results or 1 year after the end of the study (or study termination), whichever comes first.
Discussion
MIRNA represents the first clinical study to assess an oral DGAT2i alone and coadministered with another investigational chemical entity, ACCi, in patients with biopsy-confirmed NASH with F2 or F3.
The rationale for MIRNA is supported by non-clinical and clinical data. Reduced liver steatosis (accompanied by an increase in hepatic free fatty acids and increasing fibrosis) was observed with an antisense oligonucleotide DGAT2 inhibitor in a specific rodent model,42 but this increase in fibrosis has not been replicated with orally administered DGAT2i.17 Furthermore, non-clinical data showed no change in fasting (4 hours) non-esterified fatty acids at day 17 of dosing in Western-diet fed rats with DGAT2i (PF-06865571, ervogastat) alone or in combination with ACCi (unpublished data), which is consistent with previous data showing that DGAT1 rather than DGAT2 is the active DGAT isoform during stimulated lipolysis, promoting fatty acid re-esterification to protect adipocytes from lipid-induced endoplasmic reticulum stress.43 Dose-dependent reductions in liver fat of ≤41% (vs 11% with placebo) and fasting serum triglycerides of ≤24.5 mg/dL (vs 7.0 mg/dL with placebo) were reported following oral administration of the DGAT2i ≤300 mg BID for 14 days in patients with NAFLD.18 Moreover, preliminary data suggest that DGAT2i+ACCi could extend the efficacy of DGAT2i and also mitigate ACCi-induced increases in serum triglycerides.23 Further data from MIRNA will help elucidate the benefit-to-risk profile of these new chemical entities, particularly when considering that hepatic fibrosis (defined by VCTE ≥8.2 kPa) is associated with several cardiometabolic disease risk factors.44
This study has several strengths, including a triage approach with double-confirmation prior to screening/baseline liver biopsy, coupled with central reading of all liver biopsies with consensus required to determine eligibility and assess drug(s) effects, that is designed to improve efficiency in identifying participants likely to meet histological entry criteria and robust confidence in histological findings. Assessing a wide range of DGAT2i doses via QD and BID regimens along with DGAT2i+ACCi allows for a thorough assessment of several objectives, using statistically efficient methodology to identify potentially well tolerated and efficacious dose(s) and dosing regimen(s) for pivotal phase III/IV trials.45 The ongoing phase IIa trial (NCT04399538) will provide additional information on optimal doses of DGAT2i+ACCi. Furthermore, evaluating drug effects on imaging and blood-based biomarkers alongside regulatory-mandated histological endpoints during the dosing period could help identify surrogate endpoints for NASH with F2 or F3 fibrosis.36 46 This is particularly pertinent as European and US guidelines currently recommend striving for validated, non-invasive endpoints for NASH.37 47 MIRNA is designed to satisfy this recommendation with adequate statistical power to assess the primary endpoint. Enrolment above the minimum requirement, double screening by two pathologists, and collection of plasma and serum samples for future non-invasive endpoints further supports the robustness of the study design. The study is limited in that the design relies on assumptions around the translation of effects observed in earlier non-biopsy studies to a histological endpoint; the impact of the drug(s) on clinical outcomes will need confirmation in an adequately sample-sized phase III trial.
MIRNA incorporates learnings from previous trials in patients with NASH and F2 or F3 fibrosis, and other metabolic diseases (eg, type 2 diabetes).48 49 This dose-ranging, dose-finding study in patients with NASH and F2 or F3 fibrosis aims to collect robust data for histological, imaging and blood-based biomarkers to provide confidence in the efficacy of DGAT2i and ACCi, so that the pivotal phase III trials can focus on confirming efficacy and evaluate safety in a much larger sample size.
Supplementary Material
Acknowledgments
The authors would like to thank Adam Ogden (Pfizer Inc) for contributions to the clinical pharmacology aspects of the dose selection for DGAT2i, Theodore Rieger (Pfizer Inc) for contributions to physiology-based quantitative systems modelling and Patanjali Ravva (Pfizer Inc) for contributions to PD-PK modelling and simulation used for selection of DGAT2i and ACCi doses. Medical writing support, under the direction of the authors, was provided by Kate Silverthorne, PhD, on behalf of CMC Connect, McCann Health Medical Communications, with funding from Pfizer Inc, New York, USA, in accordance with Good Publication Practice (GPP3) guidelines.
Footnotes
Contributors: Conception and study design: NBA, AD, DSL, MV, QMA, VW-SW, FT and CY. Oversight and leadership of the study planning and execution: NBA, AD and CY. Study conduct: NBA, AD, QMA, VW-SW, FT, MV, MC, NA, AN and CY. Drafting, revising and final approval of the manuscript: NBA, AD, QMA, VW-SW, FT, MV, DSL, MC, NA, AN and CY.
Funding: This work is supported by Pfizer Inc.
Disclaimer: The study sponsor is involved in the design, analysis, interpretation and reporting of this study.
Competing interests: NBA, AD, DSL, MV and CY are employees of, and hold stock or stock options with, Pfizer Inc. QMA has received fees for consultancy on behalf of Newcastle University, grant funding via the EU IMI2 scheme and speaker fees from Pfizer Inc in relation to the submitted work. QMA has received grant funding from AbbVie, Allergan/Tobira, AstraZeneca, Genfit SA, GlaxoSmithKline, Glympse Bio, Intercept Pharma Europe Ltd (via the EU IMI2 scheme), Novartis Pharma AG, Pfizer Inc (via the EU IMI2 scheme); speaker fees from Bristol Myers Squibb, Gilead, Kenes, Novo Nordisk, Pfizer Inc; consultancy fees on behalf of Newcastle University from 89Bio, Allergan/Tobira, Altimmune, AstraZeneca, Axcella, BGMBio, Blade, BNN Cardio, Bristol Myers Squibb, Celgene, Cirius, CymaBay, E3Bio, EcoR1, Eli Lilly & Co, Galmed, Genentech, Genfit SA, Gilead, Grunthal, HistoIndex, Imperial Innovations, Indalo, Intercept Pharma Europe Ltd., Inventiva, IQVIA, Janssen, Madrigal, MedImmune, Metacrine, NewGene, NGMBio, North Sea Therapeutics, Novartis Pharma AG, Novo Nordisk, PathAI, Pfizer Inc, Poxel, Raptor Pharma, Servier, Terns, Viking Therapeutics, outside the submitted work. VW-SW has received medical writing and article processing charges support from Pfizer Inc for the submitted work. VW-SW’s institution has received grant funding from Gilead and support for meetings attendance from AbbVie and Gilead; VW-SW has received consulting fees and payments for participation on a Data Safety Monitoring Board or Advisory Board from 3V-Bio, AbbVie, Allergan, Boehringer Ingelheim, Centre for Outcomes Research in Liver Diseases, Echosens, Gilead, Hanmi Pharmaceutical, Intercept, Inventiva, Merck, Novartis, Novo Nordisk, Perspectum Diagnostics, Pfizer Inc, ProSciento, Sagimet Biosciences, TARGET PharmaSolutions, Terns; VW-SW has received payment or honoraria for lectures, presentations, speakers bureaux, manuscript writing or educational events from Abbott, AbbVie, Bristol Myers Squibb, Echosens, Gilead; VW-SV has stock or stock options in Illuminatio Medical Technology Ltd. FT’s institution has received grants or contracts from Allergan, Bristol Myers Squibb, Galapagos, Gilead and Inventiva; FT has received consulting fees from AbbVie, Allergan, Boehringer Ingelheim, Bristol Myers Squibb, Galapagos, Gilead, Ionis, Ipsen, Inventiva, Novartis, Pfizer Inc and Roche; FT has received payment or honoraria for lectures, presentations, speakers bureaux, manuscript writing or educational events from Falk, Intercept and Gilead; he has received payment for expert testimony from Alnylam. NA has received grants or contracts from Akero, Allergan, Bristol Myers Squibb, DSM, Genentech, Genfit, Gilead, Intercept, Inventiva, Madrigal, NGMBio, North Sea Therapeutics, Novo Nordisk, Pfizer Inc, Poxel and Zydus; NA has received payment or honoraria for lectures, presentations, speakers bureaux, manuscript writing or educational events from Gilead and Intercept.
MC and AN declare no competing interests. A patent rationalising the invention of administering DGAT2i+ACCi to mitigate effects of ACCi alone has been submitted.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease – meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73–84. 10.1002/hep.28431 [DOI] [PubMed] [Google Scholar]
- 2.LaBrecque DR, Abbas Z, Anania F. World gastroenterology organisation global guidelines: nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. J Clin Gastroenterol 2014;48:467–73. 10.1097/MCG.0000000000000116 [DOI] [PubMed] [Google Scholar]
- 3.Diehl AM, Day C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis. N Engl J Med 2017;377:2063–72. 10.1056/NEJMra1503519 [DOI] [PubMed] [Google Scholar]
- 4.Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 2018;15:11–20. 10.1038/nrgastro.2017.109 [DOI] [PubMed] [Google Scholar]
- 5.Friedman SL, Neuschwander-Tetri BA, Rinella M, et al. Mechanisms of NAFLD development and therapeutic strategies. Nat Med 2018;24:908–22. 10.1038/s41591-018-0104-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015;149:389–97.e10. 10.1053/j.gastro.2015.04.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hagström H, Nasr P, Ekstedt M, et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol 2017;67:1265–73. 10.1016/j.jhep.2017.07.027 [DOI] [PubMed] [Google Scholar]
- 8.Taylor RS, Taylor RJ, Bayliss S, et al. Association between fibrosis stage and outcomes of patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Gastroenterology 2020;158:1611–25.e12. 10.1053/j.gastro.2020.01.043 [DOI] [PubMed] [Google Scholar]
- 9.Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology 2017;65:1557–65. 10.1002/hep.29085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lambert JE, Ramos-Roman MA, Browning JD, et al. Increased de novo lipogenesis is a distinct characteristic of individuals with nonalcoholic fatty liver disease. Gastroenterology 2014;146:726–35. 10.1053/j.gastro.2013.11.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim C-W, Addy C, Kusunoki J, et al. Acetyl CoA carboxylase inhibition reduces hepatic steatosis but elevates plasma triglycerides in mice and humans: a bedside to bench investigation. Cell Metab 2017;26:394–406. 10.1016/j.cmet.2017.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zammit VA. Hepatic triacylglycerol synthesis and secretion: DGAT2 as the link between glycaemia and triglyceridaemia. Biochem J 2013;451:1–12. 10.1042/BJ20121689 [DOI] [PubMed] [Google Scholar]
- 13.Yen C-LE, Stone SJ, Koliwad S, et al. Thematic review series: glycerolipids. DGAT enzymes and triacylglycerol biosynthesis. J Lipid Res 2008;49:2283–301. 10.1194/jlr.R800018-JLR200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kammoun HL, Chabanon H, Hainault I, et al. GRP78 expression inhibits insulin and ER stress-induced SREBP-1c activation and reduces hepatic steatosis in mice. J Clin Invest 2009;119:1201–15. 10.1172/JCI37007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest 2002;109:1125–31. 10.1172/JCI15593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi CS, Savage DB, Kulkarni A, et al. Suppression of diacylglycerol acyltransferase-2 (DGAT2), but not DGAT1, with antisense oligonucleotides reverses diet-induced hepatic steatosis and insulin resistance. J Biol Chem 2007;282:22678–88. 10.1074/jbc.M704213200 [DOI] [PubMed] [Google Scholar]
- 17.Amin NB, Carvajal-Gonzalez S, Purkal J, et al. Targeting diacylglycerol acyltransferase 2 for the treatment of nonalcoholic steatohepatitis. Sci Transl Med 2019;11:eaav9701. 10.1126/scitranslmed.aav9701 [DOI] [PubMed] [Google Scholar]
- 18.Saxena AR, Chidsey K, Somayaji V, et al . Diacylglycerol acyltransferase 2 (DGAT2) inhibitor PF-06865571 reduces liver fat by MRI-PDFF after 2 weeks in adults with NAFLD [abstract]. Hepatology 2019;70(Suppl 1):1260A. [Google Scholar]
- 19.Bates J, Vijayakumar A, Ghoshal S, et al. Acetyl-CoA carboxylase inhibition disrupts metabolic reprogramming during hepatic stellate cell activation. J Hepatol 2020;73:896–905. 10.1016/j.jhep.2020.04.037 [DOI] [PubMed] [Google Scholar]
- 20.Loomba R, Kayali Z, Noureddin M, et al. GS-0976 reduces hepatic steatosis and fibrosis markers in patients with nonalcoholic fatty liver disease. Gastroenterology 2018;155:1463–73.e6. 10.1053/j.gastro.2018.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lawitz EJ, Coste A, Poordad F, et al. Acetyl-CoA carboxylase inhibitor GS-0976 for 12 weeks reduces hepatic de novo lipogenesis and steatosis in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol 2018;16:1983–91.e3. 10.1016/j.cgh.2018.04.042 [DOI] [PubMed] [Google Scholar]
- 22.Bergman A, Carvajal-Gonzalez S, Tarabar S, et al. Safety, tolerability, pharmacokinetics and pharmacodynamics of a liver-targeting ACC inhibitor (PF-05221304): a three-part randomized phase 1 study. Clin Pharmacol Drug Dev 2020;9:514–26. 10.1002/cpdd.782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Calle RA, Amin NB, Carvajal-Gonzalez S, et al. ACC inhibitor alone or co-administered with a DGAT2 inhibitor in patients with non-alcoholic fatty liver disease: two parallel, placebo-controlled, randomized phase 2a trials. Nat Med 2021;27:1836–48. 10.1038/s41591-021-01489-1 [DOI] [PubMed] [Google Scholar]
- 24.Alkhouri N, Lawitz E, Noureddin M, et al. GS-0976 (Firsocostat): an investigational liver-directed acetyl-CoA carboxylase (ACC) inhibitor for the treatment of non-alcoholic steatohepatitis (NASH). Expert Opin Investig Drugs 2020;29:135–41. 10.1080/13543784.2020.1668374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moon YA. The SCAP/SREBP pathway: a mediator of hepatic steatosis. Endocrinol Metab 2017;32:6–10. 10.3803/EnM.2017.32.1.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goedeke L, Bates J, Vatner DF, et al. Acetyl-CoA carboxylase inhibition reverses NAFLD and hepatic insulin resistance but promotes hypertriglyceridemia in rodents. Hepatology 2018;68:2197–211. 10.1002/hep.30097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ross TT, Crowley C, Rinaldi A, et al . Co-administration of the ACC inhibitor PF-05221304 and the DGAT2 inhibitor PF-06865571 produces greater efficacy and mitigates ACC inhibitor-mediated increases in circulating triglyceride NAFLD/NASH models [abstract]. Hepatology 2019;70(Suppl 1:1258A. [Google Scholar]
- 28.Kleiner DE, Brunt EM, Wilson LA, et al. Association of histologic disease activity with progression of nonalcoholic fatty liver disease. JAMA Netw Open 2019;2:e1912565. 10.1001/jamanetworkopen.2019.12565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018;67:328–57. 10.1002/hep.29367 [DOI] [PubMed] [Google Scholar]
- 30.European Association for the Study of the Liver . EASL Clinical Practice Guidelines on non-invasive tests for evaluation of liver disease severity and prognosis - 2021 update. J Hepatol 2021;75:659–89. 10.1016/j.jhep.2021.05.025 [DOI] [PubMed] [Google Scholar]
- 31.Newsome PN, Sasso M, Deeks JJ, et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study. Lancet Gastroenterol Hepatol 2020;5:362–73. 10.1016/S2468-1253(19)30383-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005;41:1313–21. 10.1002/hep.20701 [DOI] [PubMed] [Google Scholar]
- 33.Castera L, Friedrich-Rust M, Loomba R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology 2019;156:1264–81.e4. 10.1053/j.gastro.2018.12.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noureddin N, Han MAT, Alkhouri N, et al. Accounting for the placebo effect and optimizing outcomes in clinical trials of nonalcoholic steatohepatitis (NASH). Curr Hepatol Rep 2020;19:63–9. 10.1007/s11901-020-00505-1 [DOI] [Google Scholar]
- 35.Glass O, Filozof C, Noureddin M, et al. Standardisation of diet and exercise in clinical trials of NAFLD-NASH: Recommendations from the Liver Forum. J Hepatol 2020;73:680–93. 10.1016/j.jhep.2020.04.030 [DOI] [PubMed] [Google Scholar]
- 36.Filozof C, Chow S-C, Dimick-Santos L, et al. Clinical endpoints and adaptive clinical trials in precirrhotic nonalcoholic steatohepatitis: facilitating development approaches for an emerging epidemic. Hepatol Commun 2017;1:577–85. 10.1002/hep4.1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) . Noncirrhotic nonalcoholic steatohepatitis with liver fibrosis: developing drugs for treatment – guidance for industry, 2018. Available: https://www.fda.gov/media/119044/download [Accessed 6 Apr 2021].
- 38.Cheung A, Neuschwander-Tetri BA, Kleiner DE, et al. Defining improvement in nonalcoholic steatohepatitis for treatment trial endpoints: recommendations from the liver forum. Hepatology 2019;70:1841–55. 10.1002/hep.30672 [DOI] [PubMed] [Google Scholar]
- 39.Mashhood A, Railkar R, Yokoo T, et al. Reproducibility of hepatic fat fraction measurement by magnetic resonance imaging. J Magn Reson Imaging 2013;37:1359–70. 10.1002/jmri.23928 [DOI] [PubMed] [Google Scholar]
- 40.Davison BA, Harrison SA, Cotter G, et al. Suboptimal reliability of liver biopsy evaluation has implications for randomized clinical trials. J Hepatol 2020;73:1322–32. 10.1016/j.jhep.2020.06.025 [DOI] [PubMed] [Google Scholar]
- 41.Harrison SA, Alkhouri N, Davison BA, et al. Insulin sensitizer MSDC-0602K in non-alcoholic steatohepatitis: a randomized, double-blind, placebo-controlled phase IIb study. J Hepatol 2020;72:613–26. 10.1016/j.jhep.2019.10.023 [DOI] [PubMed] [Google Scholar]
- 42.Yamaguchi K, Yang L, McCall S, et al. Inhibiting triglyceride synthesis improves hepatic steatosis but exacerbates liver damage and fibrosis in obese mice with nonalcoholic steatohepatitis. Hepatology 2007;45:1366–74. 10.1002/hep.21655 [DOI] [PubMed] [Google Scholar]
- 43.Chitraju C, Mejhert N, Haas JT, et al. Triglyceride Synthesis by DGAT1 Protects Adipocytes from Lipid-Induced ER Stress during Lipolysis. Cell Metab 2017;26:407–18.e3. 10.1016/j.cmet.2017.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Long MT, Zhang X, Xu H, et al. Hepatic fibrosis associates with multiple cardiometabolic disease risk factors: the Framingham heart study. Hepatology 2021;73:548–59. 10.1002/hep.31608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Viele K, Connor JT. Dose-finding trials: optimizing phase 2 data in the drug development process. JAMA 2015;314:2294–5. 10.1001/jama.2015.16702 [DOI] [PubMed] [Google Scholar]
- 46.Rinella ME, Tacke F, Sanyal AJ, et al. Report on the AASLD/EASL joint workshop on clinical trial endpoints in NAFLD. J Hepatol 2019;71:823–33. 10.1016/j.jhep.2019.04.019 [DOI] [PubMed] [Google Scholar]
- 47.Committee for Medicinal Products for Human Use (CHMP) . Reflection paper on regulatory requirements for the development of medicinal products for chronic non-infectious liver diseases (PBC, PSC, NASH): EMA, 2018. Available: https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-regulatory-requirements-development-medicinal-products-chronic-non-infectious-liver_en.pdf [Accessed 6 Apr 2021].
- 48.Amin NB, Wang X, Jain SM, et al. Dose-ranging efficacy and safety study of ertugliflozin, a sodium-glucose co-transporter 2 inhibitor, in patients with type 2 diabetes on a background of metformin. Diabetes Obes Metab 2015;17:591–8. 10.1111/dom.12460 [DOI] [PubMed] [Google Scholar]
- 49.Amin NB, Aggarwal N, Pall D, et al. Two dose-ranging studies with PF-04937319, a systemic partial activator of glucokinase, as add-on therapy to metformin in adults with type 2 diabetes. Diabetes Obes Metab 2015;17:751–9. 10.1111/dom.12474 [DOI] [PubMed] [Google Scholar]
- 50.Yu XX, Murray SF, Pandey SK, et al. Antisense oligonucleotide reduction of DGAT2 expression improves hepatic steatosis and hyperlipidemia in obese mice. Hepatology 2005;42:362–71. 10.1002/hep.20783 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056159supp001.pdf (191.4KB, pdf)