Abstract
Introduction
Gestational diabetes mellitus (GDM) is a common disorder of pregnancy with health risks for mother and child during pregnancy, delivery and further lifetime, possibly leading to type 2 diabetes mellitus (T2DM). Current treatment is focused on reducing hyperglycaemia, by dietary and lifestyle intervention and, if glycaemic targets are not reached, insulin. Metformin is an oral blood glucose lowering drug and considered safe during pregnancy. It improves insulin sensitivity and has shown advantages, specifically regarding pregnancy-related outcomes and patient satisfaction, compared with insulin therapy. However, the role of metformin in addition to usual care is inconclusive and long-term outcome of metformin exposure in utero are lacking. The primary aim of this study is to investigate the early addition of metformin on pregnancy and long-term outcomes in GDM.
Methods and analysis
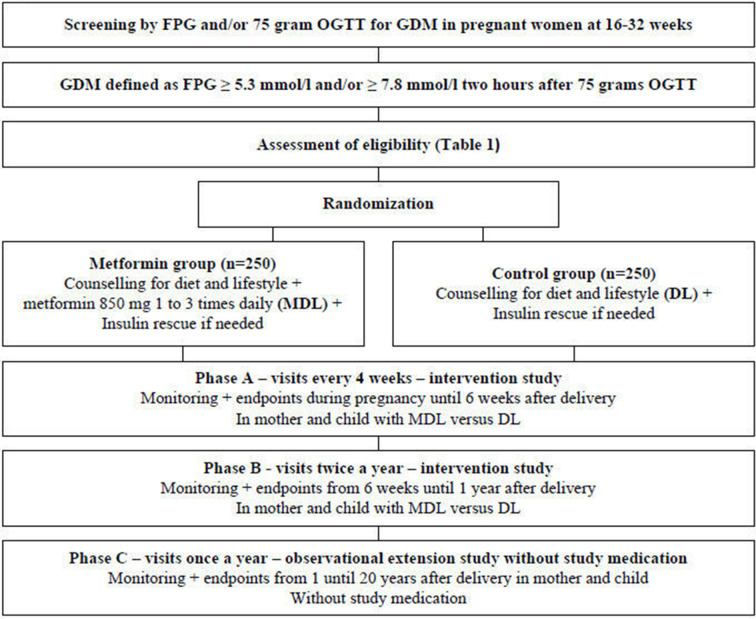
The Pregnancy Outcomes: Effects of Metformin study is a multicentre, open-label, randomised, controlled trial. Participants include women with GDM, between 16 and 32 weeks of gestation, who are randomised to either usual care or metformin added to usual care, with insulin rescue in both groups. Metformin is given up to 1 year after delivery. The study consists of three phases (A–C): A—until 6 weeks after delivery; B—until 1 year after delivery; C—observational study until 20 years after delivery. During phase A, the primary outcome is a composite score consisting of: (1) pregnancy-related hypertension, (2) large for gestational age neonate, (3) preterm delivery, (4) instrumental delivery, (5) caesarean delivery, (6) birth trauma, (7) neonatal hypoglycaemia, (8) neonatal intensive care admission. During phase B and C the primary outcome is the incidence of T2DM and (weight) development in mother and child.
Ethics and dissemination
The study was approved by the Central Committee on Research Involving Human Subjects in the Netherlands. Results will be submitted for publication in peer-reviewed journals.
Trial registration number
Keywords: diabetes in pregnancy, obstetrics, paediatrics
Strengths and limitations of this study.
This is the first randomised controlled trial (RCT) to investigate immediate initiation of metformin at the start of gestational diabetes mellitus (GDM) diagnosis added to dietary and lifestyle intervention versus dietary and lifestyle intervention alone.
It is the first RCT to study the effects of metformin in GDM on mother and child during pregnancy, at delivery and for 20 years thereafter.
The Pregnancy Outcomes: Effects of Metformin (POEM) study is the first RCT that studies the effects of continuing metformin exposure in the direct postpartum period (during lactation).
Although the POEM study is a randomised multicentre RCT, the design is incorporated into usual practice. Confounding could be introduced due to variation in usual care.
Introduction
Gestational diabetes mellitus (GDM) is one of the most common disorders of pregnancy with a prevalence estimated up to 17% worldwide. There is a wide variation between countries, due to different populations, screening approaches and diagnostic criteria.1–5
GDM is an expression of chronic insulin resistance, worsened by the hormonal and metabolic physiology of pregnancy and inadequate pancreatic β-cell adaptation.6–9 Women are often asymptomatic and therefore testing occurs in women with risk factors for GDM with a fasting plasma glucose (FPG) and an oral glucose tolerance test (OGTT). GDM is associated with suboptimal maternal and neonatal outcomes such as offspring large for gestational age (LGA), macrosomia, shoulder dystocia, pregnancy-related hypertension, caesarean section, neonatal hyperinsulinaemia and hyperbilirubinaemia.10–13 After delivery both mother and child show an increased risk of cardiometabolic disease, specifically obesity and progression to type 2 diabetes mellitus (T2DM) in mothers, and early childhood obesity and development of (pre)diabetes in adolescence.14–18
Prior research has shown strong associations between maternal blood glucose levels—even in the near-normal range—and pregnancy-related outcomes as well as childhood adiposity and insulin resistance.15 18 19 Therefore, current treatment primarily strives to normalise glycaemic levels and consists of dietary and lifestyle interventions (DLs) with regular self-monitoring of blood glucose levels.20 If blood glucose levels exceed the target ranges, antihyperglycaemic medication is recommended. Most treatment guidelines recommend insulin therapy as the first choice.20 However, insulin has several disadvantages as it is associated with increased maternal weight gain, maternal and neonatal hypoglycaemia and patients are burdened with storage, intensified self-monitoring and frequent subcutaneous injections.21 In addition, insulin therapy is costly and burdens the healthcare system by medical education and frequent contacts. Finally, although insulin administration could compensate for the β-cell dysfunction, insulin sustains the hyperinsulinaemia and does not treat the underlying insulin resistance. Perhaps this explains why women with GDM and with optimal glycaemic control still show unsatisfactory (pregnancy) outcomes.13 22 23
Mechanisms related to insulin resistance rather than low-grade glucotoxicity may contribute to the pathophysiology of the complications in GDM. This makes metformin a logical option for women with GDM. Metformin (dimethylbiguanide) is an oral blood glucose lowering drug (OBGLD) and has numerous mechanisms of action. It primarily inhibits the gluconeogenesis in the liver and acts as a insulin sensitizer—especially in the liver, and to a lesser extent in muscle and adipose tissue.24 25 Additionally, it improves glucose sensing in the intestine and mechanisms through the incretin system are also involved.25–27 Since insulin secretion is unaltered, the risk of hypoglycaemia is negligible.28 Metformin is widely used in T2DM and to a lesser extent in GDM. In GDM, metformin compared with insulin and other OBGLD, reduces maternal and neonatal weight gain, the risk of pregnancy-related hypertension, neonatal intensive care admission and hypoglycaemia.24 29–32 Additionally, metformin shows anti-inflammatory and antithrombogenic effects33–37 and higher patient satisfaction compared with insulin.21 Several international treatment guidelines already recommend metformin treatment above insulin therapy if DLs fail to adequately treat hyperglycaemia.38–40 No studies on the use of metformin prior to considering insulin therapy exist.
Although hyperglycaemia usually resolves between 48 hours post partum, most GDM patients have a degree of chronic insulin resistance,41 which persists after delivery and is not treated adequately with current therapy. It is hypothesised that the addition of metformin to GDM care reduces the risk of developing T2DM.16 42 43 In mice, metformin exposure in utero and during lactation has been shown to improve glucose tolerance and insulin secretion in the adult male offspring.44 45 Additionally, metformin reduces the incidence of T2DM in pre-diabetic adults with and without a history of GDM.42 43 Despite these findings, no studies investigated the effects of continued administration of metformin in the direct postpartum period.
Despite the confirmed and theoretical advantages of metformin, its role in treatment guidelines is still inconclusive. This multicentre randomised open-label controlled trial addresses this unmet need and will contribute to the primary treatment of GDM by providing insight into (1) immediate metformin treatment on top of DL versus DL, (2) continued metformin exposure in the direct postpartum period and (3) the long-term effects of metformin for both mother and child. As such, results of this study will provide a broad understanding of metformin in GDM and the pregnancy-related outcomes as well as provide data on the long-term outcomes concerning safety and efficacy in mother and child.
Methods and analysis
Design and setting
The Pregnancy Outcomes: Effects of Metformin (POEM study is a long-term, multicentre, randomised controlled, open-label, trial comparing usual care to metformin added to usual care. The trial consists of three distinct phases (A, B and C), and has a 20-year follow-up period after delivery. The first patient was included in December 2019 and the planned end date including phase C is in 2043.
Phase A (from inclusion until 6 weeks after delivery) and phase B (from 6 weeks until 1 year after delivery) are the interventional phases, while phase C (from 1 until 20 years after delivery) is the long-term observational phase.
The study will be conducted in the Netherlands and embedded in regular care with multidisciplinary GDM treatment teams usually consisting of a gynaecologist, internist, diabetes specialist nurse, midwife and dietician.
Ethical compliance
The methods employed in this trial were judged and approved by the Central Committee on Research Involving Human Subjects (Centrale Commissie Mensgebonden Onderzoek, CCMO, the National Medical Ethical Committee in the Netherlands). EudraCT number is 2015-002148-15.
Public involvement
The Dutch Diabetes Association was involved in the preparation of this trial and approved the protocol.
Study population
GDM is diagnosed using a 75 g OGTT according to the national Dutch guidelines.20 Currently, screening for GDM in the Netherlands occurs based on predisposing risk factors, to be known; BMI>30 kg/m², a history of a neonate with a birth weight >p95 or >4500 g, a first degree family member with diabetes mellitus, ethnic groups with a higher risk of diabetes mellitus (women of South-Asian descent, Afro-Caribbean, Middle-East, Morocco or Egypt), a medical history of unexplained foetal death and women with polycystic ovary syndrome. Women with these risk factors are tested between 24 and 28 weeks of gestation. Women with a medical history of GDM are tested at 16 weeks of gestation.20 The OGTT is also performed in case of clinical features of GDM such as suspected macrosomia or polyhydramnios.
Women are eligible for inclusion in this study if they have an FPG≥5.3 mmol/L and/or a 2-hour post-load glucose (PG) ≥7.8 mmol/L after a 75 g OGTT. This inclusion strategy is based on national guidelines and the WHO criteria of 1999 and 2013, also including mild cases of GDM given this population also exhibits some degree of chronic insulin resistance and consequently suboptimal outcome.15 46
The inclusion and exclusion criteria are listed in box 1. The upper gestational age limit for inclusion is set at 32 weeks, to allow at least 6 weeks of metformin exposure during pregnancy. With the current screening policy, we expect that most participants will be treated ≥12 weeks during phase A.
Box 1. Inclusion and exclusion criteria.
Inclusion criteria
Pregnant women with GDM defined as a FPG≥5.3 mmol/L and/or an OGTT with a PG≥7.8 mmol/L, 2 hours after the oral intake of 75 g glucose.
Age 18–45 years.
Written informed consent.
Singleton pregnancy.
Gestational age at inclusion 16–32 weeks.
HbA1c at inclusion ≤48 mmol/mol.
Exclusion criteria
Diabetes mellitus before pregnancy, except GDM.
Proteinuria (UACR>35 mmol/mol) at screening.
Chronic liver disease and/or ASAT/ALAT>3×ULN.
Chronic renal failure with GFR<45 mL/min/1.73 m2.
Malignancy during the last 5 years, except non-melanoma skin cancer.
Psychiatric and/or mood disorders potentially affecting compliance of treatment.
Chronic pulmonary failure with hypoxia
Significantly uncontrolled hypertension (SBP>160 mm Hg despite medical treatment).
Chronic treatment with corticosteroids.
Intolerance for metformin and/or earlier use of metformin in this pregnancy.
Involvement in the POEM study.
Severe fetal anomaly at inclusion.
Ruptured of membranes (ROM).
Inability to understand or read Dutch language.
Bariatric surgery in medical history.
Hyperemesis gravidarum.
Inclusion and randomisation
Eligible women will be informed about the study by either a research nurse, investigator or a healthcare provider (internist, diabetes specialist nurse, midwife or gynaecologist). Prior to participation full written informed consent is obtained for phase A and B (online supplemental appendices 1 and 2). At the end of phase B, informed consent will be obtained for phase C. Participants are randomised, stratified for age and duration of pregnancy and allocated 1:1 to either metformin and DL or to DL alone. Randomisation with stratification (for age and pregnancy duration) will be performed in the electronic case report form (eCRF) using Castor EDC.
bmjopen-2021-056282supp001.pdf (141.5KB, pdf)
bmjopen-2021-056282supp002.pdf (94.3KB, pdf)
The flowchart for eligibility, randomisation, intervention and control group and visit frequencies in the three phases of this study is presented in figure 1.
Figure 1.
Flow chart. DL, diet and lifestyle intervention; FPG, fasting plasma glucose; GDM, gestational diabetes mellitus; MDL, metformin and diet and lifestyle intervention; OGTT, oral glucose tolerance test.
Intervention: metformin
The intervention group will receive metformin tablets of 850 mg (TEVA), titrated within approximately 15 days up to three times per day, if tolerated. The maximally tolerated dose will be continued until 1 year after delivery. Metformin will be stopped according to clinical judgement during, for example, severe diarrhoea with dehydration, severe illness with fever and/or sepsis. Additionally, metformin will be stopped - if indicated - in case of fetal growth restriction, as was also done in previous studies.47 Fetal growth restriction will be defined according to the criteria proposed by Delphi consensus.48
Obstetric care
Obstetric care will be performed according to usual practice of the participating centre. Regular ultrasonography with fetal biometry (abdominal circumference, femur length, head circumference, estimated fetal weight and amniotic fluid volume) is performed approximately every 4 weeks. Timing of delivery will be performed according to usual practice of GDM with DL without insulin, which is often an expectant approach. If insulin rescue is needed, or in case of expected LGA, it is generally recommended to consider induction of labour around 38–39 weeks.20
Diabetes care
All participants will be referred to a diabetes specialist nurse, dietician and internist according to routine GDM care. In both groups, glucose monitoring and DL will be performed according to usual care with guidance by a diabetic nurse and a dietician. The diabetes specialist or research nurse instructs the participants about measuring procedures according to national guidelines.49 CareSens glucose meters will be used as the standard system for blood glucose measurements in all participants. DLs are embedded in regular care, and are performed according to the Dutch and WHO guidelines (physical activity and a well-balanced diet with carbohydrate redistribution and (mild) carbohydrate restriction).50
The participants will be asked to collect two 7-point blood glucose profiles in the week prior to the research visits. For the other weeks participants will collect 4-point blood glucose profiles according to usual care. The blood glucose levels will be reviewed by a diabetes nurse specialist or medical doctor at least every 1–2 weeks. At inclusion, laboratory safety tests will be performed to exclude, for example, renal or liver diseases. Glycated haemoglobin (HbA1c), renal and liver function will be checked every 8 weeks in phase A.
In both groups, insulin rescue will be started at the discretion of the internist if the allocated treatment is not sufficient to achieve the target values of glycaemic control at least more than two times (FPG<5.3 mmol/L and PG<7.8 mmol/L). According to normal standard of care, the internist may choose to commence insulin rescue only temporarily if there is a reversible factor for dysregulation (medication/food/stress/fever).
If target values are not met more than two times in phase B or C (FPG<7.0 mmol/L or PG<11.1 mmol/L), antihyperglycaemic treatment will be started (or extended) according to national guidelines for the treatment of T2DM.51
Neonatal care
Neonatal care will be performed according to usual care. Most sites will perform glucose monitoring if the neonate has a birth weight >p90 and/or if mother receives insulin therapy.
Follow-up and data collection
The follow-up and data collection per visit are presented in table 1. All data will be recorded in the eCRF per site. In phase A, participants will have visits every 4 weeks until delivery, and 6 weeks after delivery. In phase B, participants will have visits two times a year, at 6 and 12 months after delivery. In phase C, participants will have visits once a year for a duration of 20 years after delivery. Additional blood samples from the mother (research panel) and urine samples from the child will be collected and stored at −80°C for later analyses and to study the effects of metformin regarding metabolic, development and safety outcomes.
Table 1.
Measurements per visit
| Phase A | Phase B | Phase C | |||||||||||
| R | D | ||||||||||||
| Visit number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10* | 11 | 12 | 13–31 |
| Weeks | −1 | 0 | 8 | 12 | 16 | 20 | 24 | +6 | |||||
| Time (months) after delivery | 1.5 | 6 | 12 | 2–20 years | |||||||||
| Visit window (±days) | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 14 | 14 | 14 |
| General | |||||||||||||
| Baseline characteristics | X | ||||||||||||
| Medical/obstetric history | X | ||||||||||||
| Concomitant medication | X | X | X | X | X | X | X | X | X | X | X | X | Every visit |
| Physical examination | X | X | X | Every four visits | |||||||||
| Vital signs, body weight | X | X | X | X | X | X | X | X | X | X | X | X | Every visit |
| 7 points BGM review | X | X | X | X | X | X | X | X | X | X | |||
| AE/SAE/endpoint report | X | X | X | X | X | X | X | X | X | X | X | Every visit | |
| Check compliance | X | X | X | X | X | X | X | X | X | ||||
| Check GOS | X | X | |||||||||||
| Check fetal sonography | X | X | X | X | X | X | X | ||||||
| EQ-5D-5L and WHO-5 | X | X | X | X | X | Every other visit | |||||||
| Lactation evaluation | X | X | X | ||||||||||
| Development child | X | X | X | Every visit | |||||||||
| Samples | |||||||||||||
| Safety panel mother† | X | X | X | ||||||||||
| Regular panel mother‡ | X | X | X | X | X | X | X | Every visit | |||||
| Research panel mother | X | X | X | X | X | X | X | Every visit | |||||
| OGTT mother§ | X | X | Every other visit | ||||||||||
| Morning urine mother | X | X | X | X | X | X | Every four visits | ||||||
| Urinalysis | X | X | X | X | |||||||||
| Morning urine child | X | X | Every four visits | ||||||||||
| Delivery | |||||||||||||
| Umbilical cord sampling | X | ||||||||||||
| Placenta examination | X | ||||||||||||
| Neonatal glucose¶ | X | ||||||||||||
| First urine child | X | ||||||||||||
*Visit 10 is completing phase A and starting phase B.
†Safety panel (fasting): urine albumin creatinine ratio, blood cell count, haemoglobin, creatinin, urea, sodium, potassium, γGT, AF, ASAT, ALAT, LDH, CRP, TSH, FT4 (if TSH is abnormal).
‡Regular panel (fasting): HbA1c, haemoglobin, FPG, creatinin, ASAT, ALAT, B12, MMA (if B12<220 mmol/L).
§When the OGTT is performed prior to visit 1, this data will be used.
¶According to the standard of care a neonatal plasma glucose can be measured post partum.
AE, adverse event; BGM, blood glucose monitoring; D, delivery; GDM, gestational diabetes mellitus; GOS, GDM Outcome Score; OGTT, oral glucose tolerance test; R, randomisation; SAE, serious adverse event.
Additional pregnancies
If a new pregnancy occurs during phase B, this pregnancy will be entirely exposed to the allocated treatment strategy. There is no evidence for safety issues concerning metformin exposure in the first trimester.47 52–56 If a pregnancy occurs during phase C this pregnancy will be treated according to regular clinical practice.
Primary outcome measures
The primary outcome measure during phase A consists of a composite endpoint at delivery and is termed the GDM Outcome Score (GOS). The GOS is an ordinal variable ranging from 0 to 8 and consists of eight components which are shown in table 2. Additionally, the dichotomous endpoint GOS positive (1–8) versus GOS negative (0) will be evaluated as a variant of the primary outcome. The incidence of T2DM and weight development in mother and child are the coprimary outcome measures in phase B and C.
Table 2.
Primary outcome measures
| Phase A | Phase B and C |
GDM Outcome Score (GOS) score (range 0–8)
|
Incidence of maternal T2DM Weight and BMI (category) development mother Weight and BMI (percentile) development child |
BMI, body mass index; T2DM, type 2 diabetes mellitus.
Secondary outcome measures
The secondary outcome measure during phase A consists of two composite endpoints at delivery and is termed the Maternal Outcome Score (MOS) and Neonatal Outcome Score (NOS). Both are ordinal variables consisting of the components shown in table 3. Moreover, each separate component of the eight components of GOS is a secondary endpoint in phase A.
Table 3.
Secondary outcome measures
| Phase A | |
| Mother | Child |
|
Maternal Outcome Score (MOS) Caesarean delivery Pre-eclampsia, eclampsia, HELPP and PIH Maternal mortality Postpartum haemorrhage Thrombosis Each separate maternal component of GOS |
Neonatal Outcome Score (NOS) IRDS requiring oxygen therapy Stillbirth and neonatal death Preterm birth Shoulder dystocia Instrumental delivery Caesarean delivery Neonatal hypoglycaemia <2.6 mmoL/L Neonatal jaundice needing phototherapy NICU admission Apgar score as a variable Apgar score <7 at 5 min Congenital anomaly Each separate neonatal component of GOS |
| Phase B and C | |
| Mother | Child |
| Hypertension development Thrombotic and CVD events Development of chronic disease |
Gonadal and gender development Puberty and maturation Educational and intellectual development Development of chronic disease |
CVD, Cardiovascular disease; GDM, gestational diabetes mellitus; GOS, GDM Outcome Score; HELLP, Hemolysis Elevated Liver enzymes and Low Platelets; IRDS, Infant Respiratory Distress Syndrome; NICU, neonatal intensive care unit; PIH, Pregnancy induced hypertension.
The Dutch version of the EuroQol-5D-5L (EQ-5D-5L) and The World Health Organisation- Five Well-Being Index (WHO-5) will be administered to evaluate health-related quality of life. The EQ-5D-5L is a commonly used questionnaire to measure health-related quality of life.57 This questionnaire can be used to obtain quality-adjusted life years. Using the Dutch algorithm,58 a utility score can be produced ranging from 0 to 1, with 0 indicating the worst imaginable health and 1 indicating the best imaginable health state.58 The WHO-5 is a 5-item short and non-invasive generic rating scale measuring subjective psychological well-being.59 The questionnaire consists of five items and the participant is asked to rate how well each of the five statements applies to her when considering the last 14 days. It has been used as a screening tool for depression but is also widely used as outcome measure in clinical trials to capture (improvement in) well-being caused by various pharmacological interventions.59 60
Finally, biometric, metabolic and hormonal variables collected during the study will be evaluated as a variant to the secondary outcome during phase A and B. During phase C, the secondary outcome concerns the developmental milestones of the child, anthropometric measurements and development of chronic disease for mother and child. A complete overview of secondary outcome measures is presented in online supplemental appendix 3.
bmjopen-2021-056282supp003.pdf (36.3KB, pdf)
Drug safety
Observational studies and randomised trials did not show a drug safety issue in patients with GDM, polycystic ovarian syndrome, T2DM and obesity.21 47 53 54 56 61 Metformin is considered as a safe and non-teratogenic drug.52 55 56 Limited concentrations of metformin are observed in breast milk (median concentrations ranging between 0.17 and 0.41 mg/L).62–64 The mean relative infant dose ranges between 0.20% and 0.65% of the weight adjusted maternal dose.62–64 Metformin use during lactation did no show adverse effects on the infants blood glucose levels or on growth, motor and social development.62–65
Safety monitoring
According to the risk classification of investigator-initiated research, this study has a small chance to induce minor damage leading to the qualification of a negligible risk study. Nevertheless, we installed a Data and Safety Monitoring Board to secure the safety of the participants. All serious adverse events will be reported. A study monitor will periodically visit all participating centres and ensure the rights and well-being of the participating subjects and to assess the quality of data collection and check if the rights, safety and well-being of the participants are reassured.
Sample size
The eight components of GOS and their estimated prevalence in GDM patients in the Netherlands are: LGA (16.5%–19.9%), preterm delivery (4.4%–6.4%), admission to neonatal intensive care (5%), instrumental delivery (7.5%–8.2%), birth trauma (3.7%), neonatal hypoglycaemia (3.4%–27.1%), caesarean delivery (12.1%–23.8%) and pregnancy-related hypertension (8.8–12.5).10 13 Metformin added to DL has never been compared with DL alone. Several meta-analyses comparing metformin to insulin showed a lower incidence of LGA (pooled risk ratio (RR): 0.80 (0.64–0.99)) and macrosomia (pooled RR: 0.60 (0.45–0.79)), pregnancy induced hypertension (pooled RR: 0.56 (0.37–0.85)), neonatal hypoglycaemia (pooled RR: 0.63 (0.45–0.87)) and neonatal intensive care unit admission (pooled RR: 0.72 (0.59–0.88)).29 30 32 66 Rates of caesarean section (pooled RR: 0.97 (0.80–1.19)), birth trauma (pooled RR: 0.86 (0.45–1.63)), preterm birth (pooled RR: 1.18 (0.67–2.07)) and assisted delivery (pooled RR: 1.34 (0.65–2.75)) did not differ between the groups.29 30 32 66 67 By pooling the known effects of metformin versus insulin, so far, the effect size of metformin on GOS can be estimated as a relative risk reduction of 15%. We anticipated the early addition of metformin to DL results in a relative risk reduction of 25% on the GOS scale compared with the control group.
Based on the Groningen Pregnancy Outcome Database, the distribution of GOS was observed to be distributed according to a Poisson distribution of mean λ (and equal variance) close to 1. Assuming a Poisson parameter of λ=1, a ratio rate of 0.7 and a baseline final correlation in the range 0<R<0.2, we got the following results on several R and λ values in an acceptable pessimistic–optimistic range.
The most likely value without considering the decrease of patients due to correlation corresponds to 221 patients per group (table 4). We expect a drop out in the short-term phase A of less than 10% after inclusion. Nevertheless, we will include an extra number of 29 patients per group, increasing the total sample size up to 500 patients (250 per group).
Table 4.
Sample size calculation
| r=0 | r=0.2 | r=0.4 | r=0.6 | r=0.8 | |
| 0.5 | 442 | 425 | 372 | 283 | 160 |
| 1 | 221 | 213 | 186 | 142 | 80 |
| 1.5 | 148 | 142 | 124 | 95 | 54 |
Rows are values of events. Columns are values of rho (r).
Data handling
All data will be recorded in the eCRF Castor EDC. This record will be filled in by the investigator or research nurses. Data will be handled confidentially and accordingly to the guidelines for privacy protection (AVG). The subjects will be identified only by a subject code in the eCRF and any electronic database. Data will be stored for a minimum of 15 years after study closure.
Data analysis
Data will be presented as means with SD and/or 95% CI or as median with IQR, depending on distribution. Categorical data will be assessed by comparing the event rates in the two groups using a χ2 test. For continuous data, differences between groups will be assessed with the Student’s t-test if the outcome is normally distributed and with the Mann-Whitney U test if not normally distributed.
The primary analysis will be by intention to treat. The effect of metformin on GOS will be studied using linear models. A list of covariates will be prespecified prior to code breaking. During the follow-up before the end of the study, and in any event before the final blinded review, this model will be fitted to the ongoing data by first applying existing predictors, and second adding possible variables, currently not investigated.
The aggregated secondary outcome measures MOS and NOS will be analysed similar to the primary outcome measure. Additionally, we aim to perform a stratified analysis based on known GDM phenotypes: predominantly insulin resistant and predominantly insulin deficient based on OGTT results.68 69 A p value of 0.05 will be considered significant in all analyses.
Ethics and dissemination
The study protocol was approved by the Central Committee on Research Involving Human Subjects in the Netherlands and approval of the institutional review board of each participating centre will be obtained. The content authority of this trial was the Dutch Ministry of Public Health, Well-being and Sports (VWS). Changes in the study protocol will be submitted to the CCMO in amendments for approval.
Interim analyses are planned at the end of phase A, B and C, with their own coprimary endpoints. Results of these interim analyses will be published in peer-reviewed journals. Additional analyses will be reported separately.
Supplementary Material
Footnotes
Contributors: Study design, protocol and acquisition of data: EGMvH, PRvD, JRP, HLL, KH, JJHME, AK. Drafting of initial manuscript: EGMvH. Critical revision of the manuscript for important intellectual content: PRvD, JRP, HLL, KH, JJHME, AK. Final approval of the version submitted: EGMvH, PRvD, JRP, HLL, KH, JJHME, AK.
Funding: The POEM study is supported by grants from ZonMw (Dutch National Ministry of Health, project number 848017010), province of Drenthe (70617), Novo Nordisk BV (reference number 0072016) and Sanofi-Aventis BV (V170120, V160258, V150352). None of the funding partners has or will have any influence on the protocol, performance, data collection, data analysis, interpretation and/or publication of the POEM study.
Competing interests: KH received a lecture fee and travel grant from Novo Nordisk. All other authors declare they have no competing interests related to this study.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Zhu Y, Zhang C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective. Curr Diab Rep 2016;16:e7. 10.1007/s11892-015-0699-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jiwani A, Marseille E, Lohse N, et al. Gestational diabetes mellitus: results from a survey of country prevalence and practices. J Matern Fetal Neonatal Med 2012;25:600–10. 10.3109/14767058.2011.587921 [DOI] [PubMed] [Google Scholar]
- 3.Eades CE, Cameron DM, Evans JMM. Prevalence of gestational diabetes mellitus in Europe: a meta-analysis. Diabetes Res Clin Pract 2017;129:173–81. 10.1016/j.diabres.2017.03.030 [DOI] [PubMed] [Google Scholar]
- 4.Behboudi-Gandevani S, Amiri M, Bidhendi Yarandi R, et al. The impact of diagnostic criteria for gestational diabetes on its prevalence: a systematic review and meta-analysis. Diabetol Metab Syndr 2019;11:11. 10.1186/s13098-019-0406-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guariguata L, Linnenkamp U, Beagley J, et al. Global estimates of the prevalence of hyperglycaemia in pregnancy. Diabetes Res Clin Pract 2014;103:176–85. 10.1016/j.diabres.2013.11.003 [DOI] [PubMed] [Google Scholar]
- 6.Desoye G, Hauguel-de Mouzon S. The human placenta in gestational diabetes mellitus. the insulin and cytokine network. Diabetes Care 2007;30 Suppl 2:S120–6. 10.2337/dc07-s203 [DOI] [PubMed] [Google Scholar]
- 7.Barbour LA, McCurdy CE, Hernandez TL, et al. Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetes. Diabetes Care 2007;30 Suppl 2:S112–9. 10.2337/dc07-s202 [DOI] [PubMed] [Google Scholar]
- 8.Hanley AJ. Each degree of glucose intolerance in pregnancy predicts distinct trajectories of β-cell function, insulin sensitivity, and glycemia in the first 3 years postpartum. Diabetes Care 2014;37. 10.2337/dc14-1529 [DOI] [PubMed] [Google Scholar]
- 9.Retnakaran R, Shah BR. Divergent trajectories of cardiovascular risk factors in the years before pregnancy in women with and without gestational diabetes mellitus: a population-based study. Diabetes Care 2020;43:2500–8. 10.2337/dc20-1037 [DOI] [PubMed] [Google Scholar]
- 10.Kosman MWM, Eskes SA, van Selst J. Perinatal outcomes in gestational diabetes in relation to ethnicity in the Netherlands. Neth J Med 2016;74:22–9. [PubMed] [Google Scholar]
- 11.Goh JEL, Sadler L, Rowan J. Metformin for gestational diabetes in routine clinical practice. Diabet Med 2011;28:1082–7. 10.1111/j.1464-5491.2011.03361.x [DOI] [PubMed] [Google Scholar]
- 12.Balani J, Hyer SL, Rodin DA, et al. Pregnancy outcomes in women with gestational diabetes treated with metformin or insulin: a case-control study. Diabet Med 2009;26:798–802. 10.1111/j.1464-5491.2009.02780.x [DOI] [PubMed] [Google Scholar]
- 13.Koning SH, Hoogenberg K, Scheuneman KA, et al. Neonatal and obstetric outcomes in diet- and insulin-treated women with gestational diabetes mellitus: a retrospective study. BMC Endocr Disord 2016;16:52. 10.1186/s12902-016-0136-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Catalano PM, McIntyre HD, Cruickshank JK, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care 2012;35:780–6. 10.2337/dc11-1790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Metzger BE, Lowe LP, et al. , HAPO Study Cooperative Research Group . Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008;358:1991–2002. 10.1056/NEJMoa0707943 [DOI] [PubMed] [Google Scholar]
- 16.Bellamy L, Casas J-P, Hingorani AD, et al. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 2009;373:1773–9. 10.1016/S0140-6736(09)60731-5 [DOI] [PubMed] [Google Scholar]
- 17.Damm P, Houshmand-Oeregaard A, Kelstrup L, et al. Gestational diabetes mellitus and long-term consequences for mother and offspring: a view from Denmark. Diabetologia 2016;59:1396–9. 10.1007/s00125-016-3985-5 [DOI] [PubMed] [Google Scholar]
- 18.Lowe WL, Lowe LP, Kuang A, et al. Maternal glucose levels during pregnancy and childhood adiposity in the hyperglycemia and adverse pregnancy outcome follow-up study. Diabetologia 2019;62:598–610. 10.1007/s00125-018-4809-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scholtens DM, Kuang A, Lowe LP, et al. Hyperglycemia and adverse pregnancy outcome follow-up study (HAPO FUS): maternal glycemia and childhood glucose metabolism. Diabetes Care 2019;42:381–92. 10.2337/dc18-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.NVOG . Diabetes mellitus en zwangerschap; versie 3.0, 2018. Available: https://www.nvog.nl/wp-content/uploads/2018/10/NVOG-richtlijn-Diabetes-mellitus-en-zwangerschap-v3.0-2018.pdf
- 21.Rowan JA, Hague WM, Gao W, et al. Metformin versus insulin for the treatment of gestational diabetes. N Engl J Med 2008;358:2003–15. 10.1056/NEJMoa0707193 [DOI] [PubMed] [Google Scholar]
- 22.Voormolen DN, de Wit L, van Rijn BB, et al. Neonatal hypoglycemia following diet-controlled and insulin-treated gestational diabetes mellitus. Diabetes Care 2018;41:1385–90. 10.2337/dc18-0048 [DOI] [PubMed] [Google Scholar]
- 23.Billionnet C, Mitanchez D, Weill A, et al. Gestational diabetes and adverse perinatal outcomes from 716,152 births in France in 2012. Diabetologia 2017;60:636–44. 10.1007/s00125-017-4206-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farmacotherapeutisch kompas . Metformine (biguaniden). A10BA02. Available: https://www.farmacotherapeutischkompas.nl/bladeren/preparaatteksten/m/metformine
- 25.Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia 2017;60:1577–85. 10.1007/s00125-017-4342-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bauer PV, Duca FA, Waise TMZ, et al. Metformin alters upper small intestinal microbiota that impact a Glucose-SGLT1-Sensing glucoregulatory pathway. Cell Metab 2018;27:101–17. 10.1016/j.cmet.2017.09.019 [DOI] [PubMed] [Google Scholar]
- 27.Kappe C, Patrone C, Holst JJ, et al. Metformin protects against lipoapoptosis and enhances GLP-1 secretion from GLP-1-producing cells. J Gastroenterol 2013;48:322–32. 10.1007/s00535-012-0637-5 [DOI] [PubMed] [Google Scholar]
- 28.Bodmer M, Meier C, Krähenbühl S, et al. Metformin, sulfonylureas, or other antidiabetes drugs and the risk of lactic acidosis or hypoglycemia: a nested case-control analysis. Diabetes Care 2008;31:2086–91. 10.2337/dc08-1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Butalia S, Gutierrez L, Lodha A, et al. Short- and long-term outcomes of metformin compared with insulin alone in pregnancy: a systematic review and meta-analysis. Diabet Med 2017;34:27–36. 10.1111/dme.13150 [DOI] [PubMed] [Google Scholar]
- 30.Gui J, Liu Q, Feng L. Metformin vs insulin in the management of gestational diabetes: a meta-analysis. PLoS One 2013;8:e64585. 10.1371/journal.pone.0064585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feng Y, Yang H. Metformin - a potentially effective drug for gestational diabetes mellitus: a systematic review and meta-analysis. J Matern Fetal Neonatal Med 2017;30:1874–81. 10.1080/14767058.2016.1228061 [DOI] [PubMed] [Google Scholar]
- 32.Tarry-Adkins JL, Aiken CE, Ozanne SE. Comparative impact of pharmacological treatments for gestational diabetes on neonatal anthropometry independent of maternal glycaemic control: A systematic review and meta-analysis. PLoS Med 2020;17:e1003126. 10.1371/journal.pmed.1003126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fidan E, Onder Ersoz H, Yilmaz M, et al. The effects of rosiglitazone and metformin on inflammation and endothelial dysfunction in patients with type 2 diabetes mellitus. Acta Diabetol 2011;48:297–302. 10.1007/s00592-011-0276-y [DOI] [PubMed] [Google Scholar]
- 34.Romero R, Erez O, Hüttemann M, et al. Metformin, the aspirin of the 21st century: its role in gestational diabetes mellitus, prevention of preeclampsia and cancer, and the promotion of longevity. Am J Obstet Gynecol 2017;217:282–302. 10.1016/j.ajog.2017.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xin G, Wei Z, Ji C, et al. Metformin uniquely prevents thrombosis by inhibiting platelet activation and mtDNA release. Sci Rep 2016;6:36222. 10.1038/srep36222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hamidi Shishavan M, Henning RH, van Buiten A, et al. Metformin improves endothelial function and reduces blood pressure in diabetic spontaneously hypertensive rats independent from glycemia control: comparison to vildagliptin. Sci Rep 2017;7:1–12. 10.1038/s41598-017-11430-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kalafat E, Sukur YE, Abdi A, et al. Metformin for prevention of hypertensive disorders of pregnancy in women with gestational diabetes or obesity: systematic review and meta-analysis of randomized trials. Ultrasound Obstet Gynecol 2018;52:706–14. 10.1002/uog.19084 [DOI] [PubMed] [Google Scholar]
- 38.National Institute for Health and Care Excellence . Diabetes in pregnancy: management from preconception to the postnatal period, 2015. Available: https://www.nice.org.uk/guidance/ng3 [PubMed]
- 39.SMFM Statement . SMFM statement: pharmacological treatment of gestational diabetes. Am J Obstet Gynecol 2018;218:B2–4. 10.1016/j.ajog.2018.01.041 [DOI] [PubMed] [Google Scholar]
- 40.Keely E, Berger H, Feig DS, et al. New Diabetes Canada Clinical Practice Guidelines for Diabetes and Pregnancy - What's Changed? J Obstet Gynaecol Can 2018;40:1484–9. 10.1016/j.jogc.2018.06.024 [DOI] [PubMed] [Google Scholar]
- 41.Plows JF, Stanley JL, Baker PN, et al. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci 2018;19:3342. 10.3390/ijms19113342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ratner RE, Christophi CA, Metzger BE, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab 2008;93:4774–9. 10.1210/jc.2008-0772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403. 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gregg BE, Botezatu N, Brill JD, et al. Gestational exposure to metformin programs improved glucose tolerance and insulin secretion in adult male mouse offspring. Sci Rep 2018;8:5745. 10.1038/s41598-018-23965-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carlson Z, Hafner H, Mulcahy M, et al. Lactational metformin exposure programs offspring white adipose tissue glucose homeostasis and resilience to metabolic stress in a sex-dependent manner. Am J Physiol Endocrinol Metab 2020;318:E600–12. 10.1152/ajpendo.00473.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Landon MB, Spong CY, Thom E, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 2009;361:1339–48. 10.1056/NEJMoa0902430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Syngelaki A, Nicolaides KH, Balani J, et al. Metformin versus placebo in obese pregnant women without diabetes mellitus. N Engl J Med 2016;374:434–43. 10.1056/NEJMoa1509819 [DOI] [PubMed] [Google Scholar]
- 48.Gordijn SJ, Beune IM, Thilaganathan B, et al. Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol 2016;48:333–9. 10.1002/uog.15884 [DOI] [PubMed] [Google Scholar]
- 49.EADV (Eerste Associatie van Diabetes Verpleegkundigen) / NDF (Nederlandse Diabetes Federatie) . Een multidisciplinaire richtlijn over zelfcontrole van bloedglucosewaarden door mensen Met diabetes, 2012: 1–54. [Google Scholar]
- 50.van Wijland H. NDF Voedingsrichtlijn diabetes 2015. Tijdschr Prakt Ondersteun 2016;11:17–23. 10.1007/s12503-016-0010-x [DOI] [Google Scholar]
- 51.Barents ESE, Bilo HJG, Bouma M. NHG-Standaard diabetes mellitus type 2, 2018. Available: https://richtlijnen.nhg.org/standaarden/diabetes-mellitus-type-2
- 52.Cassina M, Donà M, Di Gianantonio E, et al. First-Trimester exposure to metformin and risk of birth defects: a systematic review and meta-analysis. Hum Reprod Update 2014;20:656–69. 10.1093/humupd/dmu022 [DOI] [PubMed] [Google Scholar]
- 53.Løvvik TS, Carlsen SM, Salvesen Øyvind, et al. Use of metformin to treat pregnant women with polycystic ovary syndrome (PregMet2): a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 2019;7:256–66. 10.1016/S2213-8587(19)30002-6 [DOI] [PubMed] [Google Scholar]
- 54.Chiswick C, Reynolds RM, Denison F, et al. Effect of metformin on maternal and fetal outcomes in obese pregnant women (EMPOWaR): a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 2015;3:778–86. 10.1016/S2213-8587(15)00219-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Given JE, Loane M, Garne E, et al. Metformin exposure in first trimester of pregnancy and risk of all or specific congenital anomalies: exploratory case-control study. BMJ 2018;361:k2477. 10.1136/bmj.k2477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scherneck S, Schlinke N, Beck E, et al. Pregnancy outcome after first-trimester exposure to metformin: a prospective cohort study. Reprod Toxicol 2018;81:79–83. 10.1016/j.reprotox.2018.07.004 [DOI] [PubMed] [Google Scholar]
- 57.Lamers LM, Stalmeier PFM, McDonnell J. Kwaliteit van leven meten in economische evaluaties: Het Nederlands EQ-5D-tarief. Ned Tijdschr Geneeskd 2005;149:1574–8. [PubMed] [Google Scholar]
- 58.M Versteegh M, M Vermeulen K, M A A Evers S, et al. Dutch tariff for the five-level version of EQ-5D. Value Health 2016;19:343–52. 10.1016/j.jval.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 59.Topp CW, Østergaard SD, Søndergaard S, et al. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom 2015;84:167–76. 10.1159/000376585 [DOI] [PubMed] [Google Scholar]
- 60.Logtenberg SJ, Kleefstra N, Houweling ST, et al. Health-Related quality of life, treatment satisfaction, and costs associated with intraperitoneal versus subcutaneous insulin administration in type 1 diabetes: a randomized controlled trial. Diabetes Care 2010;33:1169–72. 10.2337/dc09-1758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Feig DS, Donovan LE, Zinman B, et al. Metformin in women with type 2 diabetes in pregnancy (MiTy): a multicentre, international, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol 2020;8:834–44. 10.1016/S2213-8587(20)30310-7 [DOI] [PubMed] [Google Scholar]
- 62.Gardiner SJ, Kirkpatrick CMJ, Begg EJ, et al. Transfer of metformin into human milk. Clin Pharmacol Ther 2003;73:71–7. 10.1067/mcp.2003.9 [DOI] [PubMed] [Google Scholar]
- 63.Hale TW, Kristensen JH, Hackett LP, et al. Transfer of metformin into human milk. Diabetologia 2002;45:1509–14. 10.1007/s00125-002-0939-x [DOI] [PubMed] [Google Scholar]
- 64.Briggs GG, Ambrose PJ, Nageotte MP, et al. Excretion of metformin into breast milk and the effect on nursing infants. Obstet Gynecol 2005;105:1437–41. 10.1097/01.AOG.0000163249.65810.5b [DOI] [PubMed] [Google Scholar]
- 65.Glueck CJ, Salehi M, Sieve L, et al. Growth, motor, and social development in breast- and formula-fed infants of metformin-treated women with polycystic ovary syndrome. J Pediatr 2006;148:628–32. 10.1016/j.jpeds.2006.01.011 [DOI] [PubMed] [Google Scholar]
- 66.xin BL, ting SW, xin HY. Metformin versus insulin for gestational diabetes: a systematic review and meta-analysis. J Matern Fetal Neonatal Med 2021;34. 10.1080/14767058.2019.1670804 [DOI] [PubMed] [Google Scholar]
- 67.Balsells M, García-Patterson A, Solà I, et al. Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis. BMJ 2015;350:h102–12. 10.1136/bmj.h102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kotzaeridi G, Blätter J, Eppel D, et al. Characteristics of gestational diabetes subtypes classified by oral glucose tolerance test values. Eur J Clin Invest 2021;51:e13628. 10.1111/eci.13628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ryan EA, Savu A, Yeung RO, et al. Elevated fasting vs post-load glucose levels and pregnancy outcomes in gestational diabetes: a population-based study. Diabet Med 2020;37:114–22. 10.1111/dme.14173 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056282supp001.pdf (141.5KB, pdf)
bmjopen-2021-056282supp002.pdf (94.3KB, pdf)
bmjopen-2021-056282supp003.pdf (36.3KB, pdf)