Abstract
Introduction:
Heavy alcohol use negatively impacts health outcomes among people with HIV and is especially prevalent among men who have sex with men (MSM). Alcohol problems among MSM with HIV may occur, in part, due to increased stress caused by experiences of identity-based discrimination, such as heterosexism, HIV stigma, and racism. The current study examined (a) whether MSM with HIV who experience greater identity-based discrimination reported higher levels of alcohol problems over time in the absence of alcohol intervention, and (b) whether motivational interviewing (MI) to reduce alcohol use would attenuate the effects of discrimination on alcohol problems.
Methods:
Data came from a clinical trial in which MSM with HIV were randomized into brief MI for alcohol harm reduction [n = 89] or an HIV treatment as usual assessment only control [TAU; n = 91]. Alcohol use and problems were assessed at baseline, 3, 6, and 12 months.
Results:
Generalized Estimating Equations found a significant interaction between MI and baseline identity-based discrimination, such that in those not receiving MI, discrimination prospectively predicted alcohol problems over time (B = .065, SE = .018, p < .001, 95% Wald CI [.030 - .100]). In those receiving MI, discrimination did not have an effect (B = −.002, SE = .131, p = .987, 95% Wald CI [−.258 - .254]).
Conclusions:
Even without explicitly targeting experiences of identity-based discrimination, a person-centered intervention, like MI, appears to mitigate the negative impact of identity-based discrimination on alcohol-related problems.
Keywords: Men who have sex with Men, HIV, Motivational Interviewing, Alcohol Use
1. Introduction
Heavy alcohol use is an important, modifiable risk factor for poor health among people with HIV (PWH; Edelman et al., 2018; Kelso-Chichetto et al., 2018). Recent reviews document the negative effects of alcohol use among PWH, such as increased mortality (Justice et al., 2016) and disease severity (e.g., lower CD4 cell count, higher viral load, organ system injury; Edelman et al., 2018; Marshall et al., 2017). These associations may reflect the effects of unhealthy alcohol use on treatment outcomes (Williams et al., 2016), such as worse retention in HIV care (Monroe et al., 2016) and suboptimal antiretroviral therapy (ART) adherence (Kahler et al., 2017; Kelso-Chichetto et al., 2018), as well as direct physiological injury from alcohol among PWH (Justice et al., 2016; Kahler et al., 2017).
Heavy drinking and alcohol-related problems are also of particular public health concern in men who have sex with men (MSM). Gay, bisexual, and other men who report male-to-male sexual contact are the community most affected by HIV in the United States (US; Centers for Disease Control and Prevention [CDC], 2020), and alcohol use has been associated with HIV transmission risk behaviors among MSM and PWH (Williams et al., 2016). Nationally representative sample data from 2013 suggest MSM had higher odds of heavy drinking compared with heterosexual men (Gonzales et al., 2016). This pattern was also seen in MSM living with HIV (Crane et al., 2017). These findings are noteworthy given that PWH experience greater harms to their health related to alcohol use than their HIV-negative counterparts (Justice et al., 2016; Marshall et al., 2017). Research is needed to better understand the factors that contribute to heavy drinking and alcohol-related problems among MSM living with HIV.
Experiences of identity-based discrimination (i.e., the unjust or prejudicial treatment of individuals based on one or more identities such as race, sexual orientation, and HIV status; Earnshaw et al., 2013) are one potential driver of alcohol problems in MSM with HIV. Several reviews highlight that experiencing identity-based discrimination is adversely related to health, such as mental health problems, including depression and anxiety (Pachankis et al., 2020), as well as indicators of physical health, including preclinical indicators of disease, health behaviors, utilization of care, and adherence to medical regimens (Ben et al., 2017; Cobbinah and Lewis, 2018; Stockton et al., 2018; Williams et al., 2019). Several studies indicate that identity-based discrimination is also associated with higher levels of alcohol use and alcohol-related problems. For example, experiencing racial discrimination is associated with higher levels of alcohol use and problems among racial/ethnic minority individuals (Boynton et al., 2014; Cheng and Mallinckrodt, 2015; Haeny et al., 2019; López et al., 2020; Su et al., 2020). Similar patterns appear when examining discrimination based on sexual orientation among sexual and gender minority individuals (SGM; Evans-Polce et al., 2020b, 2020a; Fish and Exten, 2020; Lee et al., 2016; McCabe et al., 2019; Rodriguez-Seijas et al., 2019; Rogers et al., 2018; Slater et al., 2017; Vu et al., 2019). MSM who are living with HIV can experience another intersecting layer of discrimination based on their HIV status (Tieu et al., 2020), and among Black MSM living with HIV, racial discrimination is an additional source of oppression that can affect HIV treatment (Tieu et al., 2020). In two studies by Bogart and colleagues, greater overall racial, sexual orientation, and HIV-status based discrimination was associated with lower adherence to medication regimens, lower CD4 count, and higher viral load (Bogart et al., 2013, 2010). In a sample of young MSM and transgender women living with HIV, SGM-identity related discrimination was related to concurrent alcohol problems, but was not prospectively associated with higher rates of alcohol problems six months later (Dyar et al., 2019). Additional research is needed examining longitudinal effects on alcohol outcomes of multiple sources of discrimination based on race, sexual orientation, and HIV status, among MSM with HIV.
Given the public health significance of alcohol use in PWH, multiple intervention modalities to reduce drinking among PWH have been tested, many of which draw on the principles of Motivational Interviewing (MI; Dillard et al., 2017; Madhombiro et al., 2019; Scott-Sheldon et al., 2017). In MI, therapists seek to facilitate behavioral change through working closely with clients to resolve ambivalence about health-related behaviors and to strategize overcoming obstacles to behavior change (Miller and Rollnick, 2012). MI uses an empathic approach to counseling, consistent with self-determination theory (Markland et al., 2005), in which individuals’ basic psychological needs, especially the need for autonomy, are prioritized. Such an approach aligns well with efforts to enhance patient welfare and promote social justice (Patrick and Williams, 2012). By creating an empathic space in which individuals experiencing identity-based discrimination can openly discuss their motives for drinking, life contexts and experiences, as well as potential negative consequences of drinking, a collaborative relationship can be built in which the therapist and client can discuss alternative ways of meeting those contexts and how the client might avoid negative consequences. Thus, MI may provide a conducive environment in which individuals experiencing identity-based discrimination can consider behavior change. However, to our knowledge, the effect of MI on reducing alcohol use and problems specifically with individuals experiencing identity-based discrimination have not yet been examined empirically.
In the present study, we conducted a longitudinal secondary data analysis of a randomized controlled trial testing an MI intervention to reduce heavy alcohol use in MSM with HIV (Kahler et al., 2018). A baseline cross-sectional examination of participants in this study (Wray et al., 2016b) found that greater HIV and sexual orientation-based discrimination was associated with greater coping motives for drinking, which was, in turn, directly associated with alcohol problems. Coping motives were not, however, associated with alcohol use. Extending Wray et al.’s (2016b) cross-sectional analysis, we examined if identity-based discrimination (sexual orientation, racial/ethnic, and HIV status combined) was prospectively associated with alcohol outcomes. We did not expect baseline identity-based discrimination to be prospectively associated with alcohol use based on Wray et al.’s (2016b) cross-sectional examination. Our primary hypothesis is that: (a) In the absence of alcohol intervention, participants reporting more identity-based discrimination at baseline would report greater alcohol problems over 12 months of follow-up, even when accounting for levels of alcohol use; (b) participation in MI, compared to treatment as usual, would significantly attenuate the effect of baseline identity-based discrimination on alcohol problems over follow up.
2. Material and methods
2.1. Participants
Data were drawn from participants in a randomized controlled trial testing the efficacy of an MI intervention to reduce alcohol use among heavy drinking MSM with HIV in a Boston community health center that has long specialized in HIV and sexual and gender minority primary care (ClinicalTrials.gov Identifier: NCT01328743). One hundred eighty MSM with HIV, recruited regardless of interest in changing drinking, were randomly assigned to MI or an assessment-only HIV treatment as usual control (TAU; Kahler et al., 2018). Participants were eligible if they were: (a) ≥18 years of age; (b) drank >14 drinks per week or ≥5 drinks on a single occasion at least once in a typical month; (c) diagnosed with HIV; and (d) self-identified as gay/bisexual or reported oral or anal sex with another man in the past year. Participants were excluded if they were currently receiving treatment for an alcohol or substance use problem. Sample size was calculated based on the original clinical trial’s primary hypotheses and outcomes. The recruited sample size of 180 provided power of .80 to detect an effect size d of 0.38 (Kahler et al., 2018). See Kahler and colleagues (2018) for additional details on study procedures. The study was approved by the Institutional Review Boards at Fenway Health and Brown University.
Details of the recruitment flow based on the Consolidated Standards of Reporting Trials (CONSORT) guidelines are published elsewhere (Kahler et al., 2018). All participants randomized to MI received the initial session (n = 89). Of these, 66 (74.2%) participants received a 2-week follow-up call, and 34 (38.2%) received an optional 8-week phone call. Seventy-six participants (85.4%) received both in-person booster sessions at 3 and 6 months, four (4.5%) received one of the two in-person booster sessions, and nine (10.1%) received no in-person booster sessions (Kahler et al., 2018).
2.2. Procedures
Participants then completed the baseline interview. Participants were randomized using a computerized urn randomization program to ensure balance across key study variables: HIV viral load, engagement in condomless sex with a seronegative or unknown HIV status partner in the past three months, currently taking ART, and the number of alcoholic drinks consumed per week.
Participants assigned to the MI condition received the intervention immediately, at the end of the baseline visit. Those assigned to TAU (n = 91) met briefly with a counselor who explained that their participation for the day was complete. TAU participants completed assessments only and continued with their HIV care as usual. Participants were compensated $100 for the baseline assessment (Kahler et al., 2018). All participants were asked to complete follow-up assessments at 3, 6, and 12 months post-baseline, and were compensated $40, $50, and $60 for each follow-up assessment, respectively. For participants in the MI condition, two weeks following the baseline visit, counselors provided brief (5-min) check-in phone calls to discuss reactions to the session, follow up on goal setting, and review behavior change progress. An additional optional phone call was offered to participants in the MI condition at eight weeks post-baseline. At 3 and 6 months post baseline, in-person booster sessions were offered to participants in the MI condition. The goal of the booster sessions was to reinforce changes in drinking since last assessment or, for those who had not changed their drinking, to encourage consideration of further potential benefits of change (Kahler et al., 2018).
2.3. Measures
2.3.1. Identity-based discrimination
Discrimination experiences based on race/ethnicity, sexual orientation, and HIV status were measured using the Multiple Discrimination Scale (MDS; Bogart et al., 2011, 2013). The MDS asks participants to report experiences with 10 different discrimination events in the past year, with response options yes (score of 1) and no (score of 0). Items assess verbal or physical violence, being ridiculed or made fun of, and being excluded or avoided, among other experiences. An example item states, “Were you denied a job or did you lose a job because someone thought that you were gay?” The same 10 items are used for each type of discrimination (race/ethnicity, sexual orientation, HIV status) with stems replaced for each identity (i.e., “of your race/ethnicity” “someone thought that you were gay” “you are HIV-positive‖) for a total of 30 items. Questions around discrimination related to race/ethnicity were asked of all participants regardless of self-reported racial or ethnic identity. Past research supports the construct validity of the MDS (Bogart et al., 2013, 2011, 2010), and internal consistency in this sample was within acceptable ranges (race/ethnicity α = .72; sexual orientation α = .73; HIV α = .73). Items were summed to create a total score; higher scores represent more discrimination events in the past year.
2.3.2. Alcohol Use
Alcohol use was measured using the Timeline Followback (TLFB) interview, a structured interview using a calendar to cue participant’s memory and enhance accuracy when recalling behaviors. TLFB has demonstrated test-retest reliability with outpatients over a 6-week period (r = .94, p < .001; (Maisto et al., 1979) and validity (Sobell et al., 1980). Data collected through the interview provided the average number of drinks consumed per week in the past 30 days (Kahler et al., 2018).
2.3.3. Alcohol-related problems
Alcohol-related problems were measured with the Short Inventory of Problems (SIP; Miller, 1995). Items assess various negative consequences associated with drinking over the past month. Response options include a count-type scale, although not strictly additive (never, once or a few times, once or twice a week, and daily or almost daily), coded in the current study as 0, 1, 2, 3, respectively. The SIP is a clinically face valid and psychometrically sound measure when the purpose is to assess overall levels of alcohol-related problems (Forcehimes et al., 2007). Internal consistency for the current study was excellent (baseline α = .95; 3-month α = .93; 6-month α = .95; 12-month α = .95).
2.4. Data analytic plan
Means with standard deviations and proportions for baseline characteristics are reported overall and by study condition. Differences in baseline alcohol use, problems, and discrimination by treatment condition were examined using independent samples t-tests. Available case information was used so no data were imputed. Out of 180 participants, 9 were excluded due to missing follow-up data. Out of 513 observations (N = 171 participants, three time points) 21 observations were missing. Generalized estimating equations (GEE; Liang and Zeger, 1986) in IBM SPSS 26 were used to test study hypotheses. GEE analyses using an unstructured correlation matrix to model the correlations between follow-ups included intervention condition dummy-coded with TAU as the reference group, baseline discrimination, and baseline alcohol outcomes as time-invariant predictors. Follow-up month (3, 6, or 12) was included as a centered linear predictor, and alcohol outcomes at each follow-up was included as time-varying predictors. We specified a Gaussian distribution for drinks per week. To account for the count-type distribution of SIP total scores that showed high overdispersion (i.e., positive skewness), we specified a negative binomial distribution for all models and used maximum likelihood estimation.
To test the first hypothesis that greater discrimination at baseline would predict greater alcohol problems over follow-up (3, 6, and 12 months), in the absence of alcohol intervention, an interaction term of discrimination × intervention condition was added to the main effects model. With the interaction term in the model and treatment condition dummy coded, the main effect of discrimination on alcohol problems over follow-up represents the effect in participants receiving TAU. The interaction term tests the hypothesis MI moderates the effect of discrimination on alcohol problems. Given a significant interaction, we tested the magnitude and significance of the effect of discrimination on alcohol problems in those receiving MI. In post hoc analyses, we estimated the effect of the interaction between intervention and discrimination on mean alcohol problems over follow-up, separated by discrimination type (sexual orientation, HIV, racial). In these post-hoc analyses, we maintained all control variables from the main effects model.
3. Results
The majority of participants identified as White (74%), and non-Hispanic/Latinx (83%), and most identified as gay (93%). Just under half of the sample were post-high school educated or college graduate (49.2%), employed full time (43.3%) and made less than $30,000 per year (36.8%). Sample demographics, means and standard deviations of key study variables at baseline by treatment condition are provided in Table 1. Groups did not differ at baseline on most characteristics. However, the MI group had significantly higher scores on perceived sexual orientation discrimination than TAU. Reported experiences of discrimination were relatively low in this sample overall, with average subscale scores close to one out of a possible ten, indicating that respondents experienced on average at least one type of discriminatory experience based on the identity of interest (i.e., race/ethnicity, sexual orientation, HIV status) in the past year. The most commonly endorsed items were 1) being ignored, excluded, or avoided; 2) being insulted; and 3) being treated with hostility by strangers across race/ethnicity, sexual orientation, and HIV status. Of note, the most frequently endorsed item overall (just under half of the sample) was ‘being rejected by a sexual or romantic partner because of being HIV positive’ in the past year (n = 71 endorsed yes, 41.5%).
Table 1.
Baseline sample characteristics, means and standard deviations of key study variables
| Variable | Total (n = 171) | TAU (n = 90) | MI (n = 81) |
|---|---|---|---|
| Age (M, SD) | 42.1, 10.4 | 43.22, 10.59 | 41.27, 10.13 |
| Race (n, %)a | |||
| American Indian/Alaskan Native | 7, 4.1 | 3, 3.3 | 4, 4.9 |
| Asian | 2, 1.2 | 1, 1.1 | 1, 1.2 |
| Black/African American | 40, 23.4 | 23, 25.6 | 17, 21.0 |
| White | 126, 73.7 | 64, 71.1 | 62, 76.5 |
| Ethnicity (n, %) | |||
| Hispanic or Latino | 29, 17.0 | 15, 16.7 | 14, 17.3 |
| Not Hispanic or Latino | 142, 83.0 | 75, 83.3 | 67, 82.7 |
| Education (n, %) | |||
| ≤ High school graduate/GED | 27, 15.8 | 13, 14.4 | 14, 17.3 |
| Some post-high school education | 65, 38.0 | 35, 38.9 | 30, 37.0 |
| College graduate | 79, 46.2 | 42, 46.7 | 37, 45.7 |
| Income (n, %) | |||
| $0–29,999 | 63, 36.8 | 32, 35.6 | 41, 50.6 |
| $30,000–99,999 | 66, 38.6 | 41, 45.6 | 25, 30.9 |
| $100,000 or more | 32, 18.7 | 17, 18.9 | 15, 18.5 |
| Employment (n, %) | |||
| Unemployed | 57, 33.3 | 25, 27.8 | 32, 39.5 |
| Employed part time | 25, 14.6 | 14, 15.6 | 11, 13.6 |
| Employed full time | 74, 43.3 | 43, 47.8 | 31, 38.3 |
| Full time student | 6, 3.5 | 3, 3.3 | 3, 3.7 |
| Part time student | 2, 1.2 | 1, 1.1 | 1, 1.2 |
| Retired | 7, 4.1 | 4, 4.4 | 3, 3.7 |
| Sexual identity (n, %) | |||
| Gay | 159, 93 | 85, 94.4 | 74, 91.4 |
| Bisexual | 9, 5.3 | 4, 4.4 | 5, 6.2 |
| Other | 3, 1.8 | 1, 1.1 | 2, 2.5 |
| Other substance use ≥ once in past 3 months (n, %) | |||
| Cannabis | 86, 50.3 | 42, 46.7 | 44, 54.3 |
| Weekly or more | 48, 28.1 | 24, 26.7 | 24, 29.6 |
| Cocaine/crack | 41, 24 | 18, 20 | 23, 28.4 |
| Methamphetamines | 18, 10.5 | 11, 12.2 | 7, 8.6 |
| Inhalants | 65, 38 | 35, 38.9 | 30, 37 |
| Psychedelics | 12, 7 | 9, 10 | 3, 3.7 |
| Opiates | 14, 8.2 | 5, 5.6 | 9, 11.1 |
| Discrimination (M, SD) | 3.15, 4.18 | 2.42, 3.10 | 4.09, 5.12* |
| Racial | .79, 1.85 | .57, 1.20 | 1.11, 2.40 |
| Sexual orientation | 1.25, 1.85 | .92, 1.49 | 1.63, 2.16* |
| HIV status | 1.11, 1.54 | .93, 1.38 | 1.35, 1.73 |
| Alcohol use | 20.79, 16.96 | 19.84, 13.48 | 21.52, 19.87 |
| Alcohol problems | 9.28, 8.51 | 9.36, 9.04 | 9.33, 8.14 |
Note.
indicates a significant difference between TAU and MI at p < .05 using independent samples t-tests.
Participants can select more than one race so the total across the categories is greater than the sample size.
Results of the GEE analysis showed consistent with expectations, baseline discrimination did not prospectively predict alcohol use in those assigned to TAU (B = −.217, SE = .605, p = .719, 95% Wald CI [−1.40 - .968]), nor was there a significant interaction with MI (B = .835, SE = .723, p = .248, 95% Wald CI [−.581 – 2.25]). As hypothesized, in those assigned to TAU, baseline discrimination predicted greater alcohol problems during follow up, over and above the effect of concurrent drinking level (B = .063, SE = .021, p = .002, 95% Wald CI [.022 - .103]). Baseline level of alcohol problems (B = .080, SE = .006, p < .001, 95% Wald CI [.067 - .092]) and time varying drinks per week (B = .011, SE = .004, p = .001, 95% Wald CI [.004 - .018]) were positively associated with alcohol problems, when controlling for the discrimination by treatment interaction.
As shown in Table 2, treatment condition significantly moderated the effect of discrimination on alcohol problems during follow up (B = −.063, SE = .029, p = .029, 95% Wald CI [−.119 - −.007]). In those receiving MI, discrimination was not significantly associated with greater alcohol problems at follow-up (B = .072, SE = .171, p = .675, 95% Wald CI [−.264 - .408]). Conversely, the significant interaction indicated MI was more effective at reducing alcohol problems at higher levels of baseline discrimination. At higher levels of discrimination (i.e., 1 SD above the mean), MI resulted in over a 35% reduction in the count of alcohol problems compared to TAU (IRR = .633, p < .001, 95% CI [.492 - .813]). In those not reporting any discrimination experiences (i.e., MDS total score = 0, just less than 1 SD below the mean), MI had a minimal effect on reducing alcohol problems compared to TAU (IRR = .960, p = .723, 95% CI [.972 – 1.206]).
Table 2.
GEE modeling alcohol problems at follow-up (3, 6, 12 month) predicted by baseline discrimination, controlling for treatment condition, time-varying alcohol use, baseline alcohol problems, and the discrimination by treatment condition interaction.
| Variable | B | SE | p | 95% Wald CI | |
|---|---|---|---|---|---|
| Within participant | |||||
| Time | −.069 | .048 | .145 | −.162 | .024 |
| Time-varying alcohol use | .011 | .004 | .001 | .004 | .018 |
| Between participants | |||||
| MI (vs. TAU) | .072 | .171 | .675 | −.264 | .408 |
| Baseline discriminationa | .063 | .021 | .002 | .022 | .103 |
| Baseline alcohol problems | .080 | .006 | .000 | .067 | .092 |
| Baseline drinks per week | −.004 | .005 | .480 | −.014 | .007 |
| Interaction | |||||
| Discrimination by MI | −.063 | .029 | .029 | −.119 | −.007 |
Note. MI = motivational interviewing treatment. TAU = HIV treatment as usual assessment only control condition. Discrimination by MI reference group for MI = TAU.
Given the interaction of discrimination and MI, this equals the effect of discrimination in participants receiving TAU.
3.1. Post hoc analyses
To examine the separate effects of discrimination type (sexual orientation, HIV status, race/ethnicity) by treatment condition on alcohol problems over follow up, we tested the same model displayed in Table 2 with the three discrimination subscales entered as separate predictors along with three corresponding interaction terms. Sexual orientation discrimination was reported most frequently in the sample, and racial/ethnic discrimination was reported least frequently in this predominantly White sample. Among participants who reported being non-Hispanic White, the racial/ethnic discrimination score was very low at 0.42 (SD = 1.49), with 97 of 113 (85.8%) reporting no race/ethnicity related discrimination experiences. By contrast, in those who identified as Hispanic/Latino or as a racial group other than White, the racial/ethnic discrimination score was 0.96 (SD = .85), with only 35 of 67 (52.2%) reporting no race/ethnicity related discrimination experiences. In the TAU condition, sexual orientation discrimination was a significant positive predictor of alcohol problems over the 3-, 6-, and 12-month follow ups (B = .130, SE = .048, p = .007, 95% Wald CI [.04 - .22]). Treatment condition significantly moderated the effect of sexual orientation discrimination (B = −.180, SE = .072, p = .012, 95% Wald CI [−.321 - −.039]), such that receiving MI buffered the effect of sexual orientation discrimination on alcohol problems during follow-up (Figure 1). Racial/ethnic discrimination (B = .071, SE = .055, p = .194, 95% Wald CI [−.036 - .179]) and HIV discrimination (B = −.026, SE = .060, p = .671, 95% Wald CI [−.144 - .092]) were nonsignificant. The interaction terms for treatment condition and racial/ethnic discrimination (B = −.015, SE = .070, p = .834, 95% Wald CI [−.151 - .122]) and HIV discrimination (B = .012, SE = .088, p = .888, 95% Wald CI [−.160 −.185]) were nonsignificant.
Figure 1.
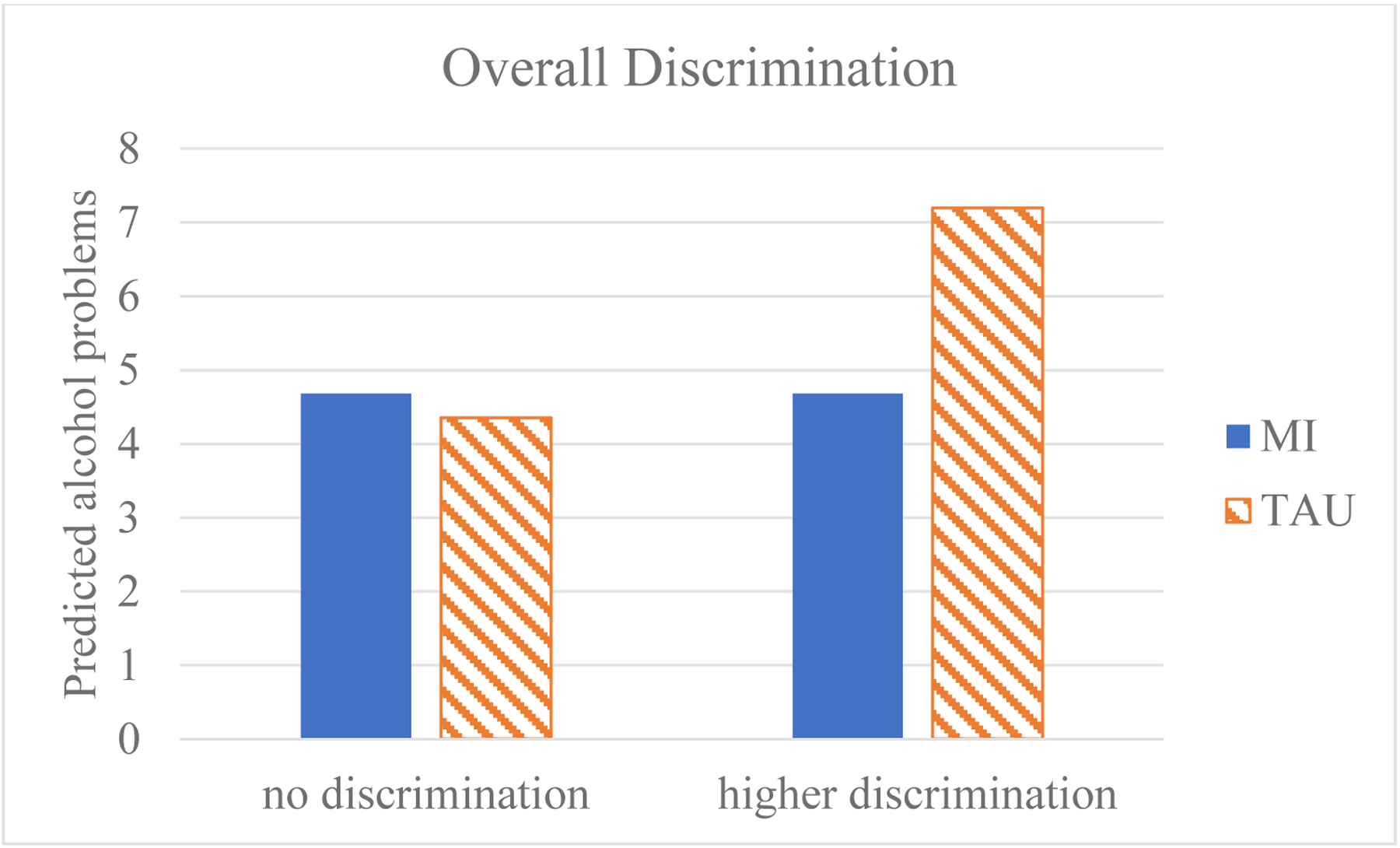
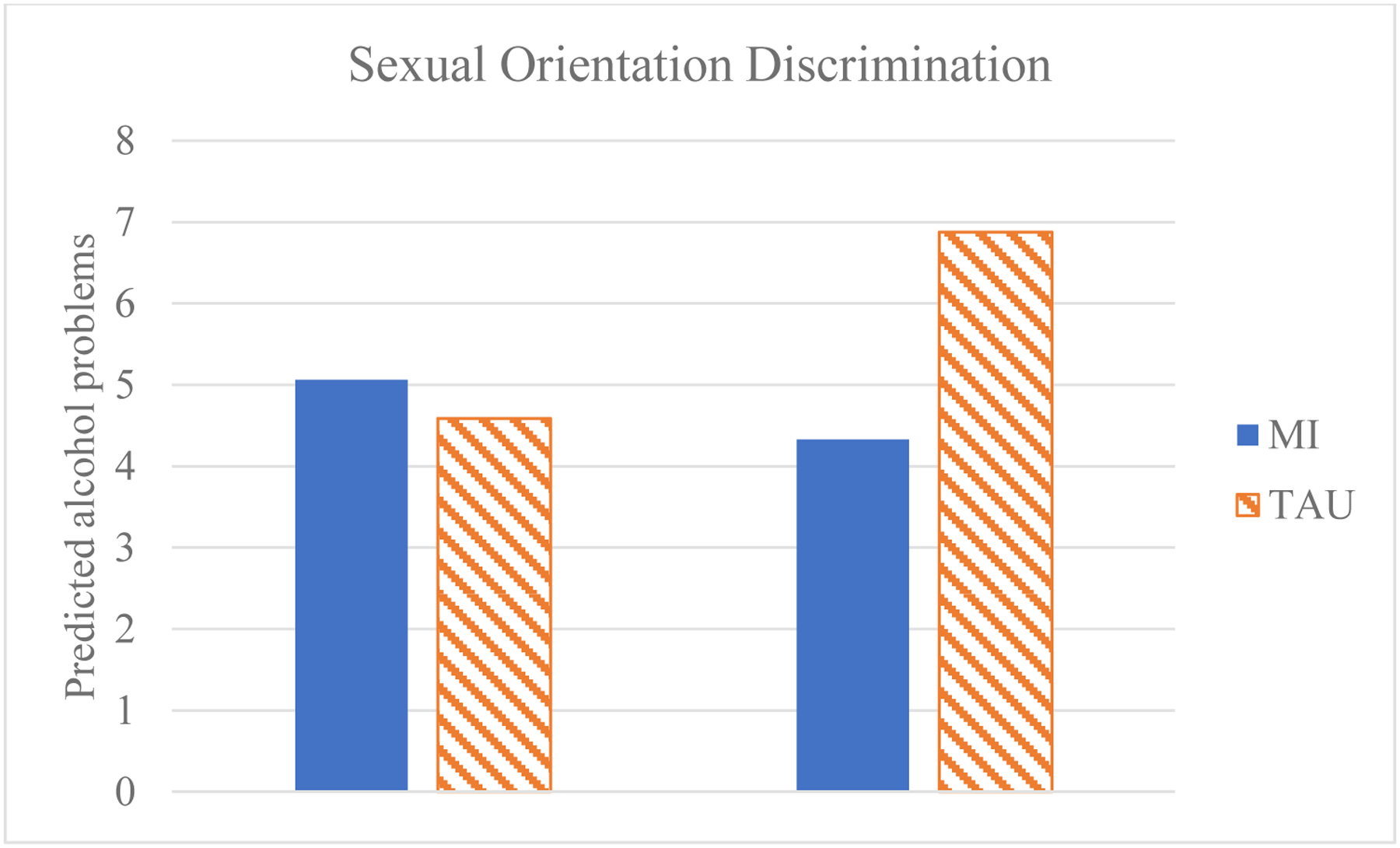
Moderation effect of treatment condition and baseline discrimination on alcohol problems during follow up.
Note. MI = motivational interviewing treatment, TAU = HIV treatment as usual, SO = sexual orientation, * = p < .05, ns = p > .05. Figures present the predicted Short Inventory of Problems (SIP) total score averaged across time points (3, 6, and 12 months) by baseline discrimination and treatment group, holding all covariates at the sample average (i.e., time-varying alcohol use, baseline alcohol use, baseline alcohol problems). Higher discrimination represents one SD above the mean (overall discrimination M, SD = 3.22, 4.26; SO discrimination M, SD = 1.25,1.86). One SD below the mean was zero. SO discrimination included the sample average for baseline racial discrimination, baseline HIV discrimination, and interaction terms baseline racial discrimination × MI, baseline HIV discrimination × MI, in the model.
4. Discussion
The present study used a longitudinal design to examine how experiences of identity-based discrimination predicted alcohol problems over time in heavy drinking MSM with HIV. As hypothesized, identity-based discrimination predicted more alcohol-related problems over follow-up, over and above the effect of concurrent levels of alcohol use, in men receiving HIV care as usual. By contrast, in participants receiving MI, the association between identity-based discrimination and greater alcohol problems was near zero. Conversely, this moderation effect reflected that MI was particularly effective in reducing alcohol problems at higher levels of experienced discrimination. For example, at higher levels of identity-based discrimination, MI compared to treatment as usual resulted in a 35% reduction in the number of alcohol problems reported. Post hoc analyses indicated that, in this sample, sexual orientation discrimination primarily drove the observed interaction effect rather than HIV or race/ethnicity-related discrimination.
There are a number of reasons why MI may have attenuated the effect of sexual orientation discrimination on alcohol problems across follow up, over and above its effects on alcohol use. The MI protocol in the current trial focused primarily on motivations for drinking, personalized feedback on alcohol and health, and change planning around alcohol use. It did not contain content specifically focused on issues of identity-based discrimination. However, the MI protocol, counselor training, and counselor supervision in this trial strongly emphasized the relational components of MI, specifically an empathic, client-centered, collaborative approach that emphasized client autonomy. Repeated sessions of MI with an empathic counselor who worked to create an environment that supports an individual’s autonomy, health, and well-being, may have provided in-session social support that, in and of itself, had a salubrious effect on alcohol problems for individuals experiencing identity-based discrimination, regardless of whether discrimination was discussed in sessions. Indeed, a broad body of research shows that supportive relationships can buffer the effects of many types of negative stressors on the development of psychological disorders (Bankoff et al., 2013; Moak and Agrawal, 2010), as well as that many therapies are effective for reducing symptoms of psychological disorders through common factors (e.g., therapeutic alliance, confiding healing setting; Mulder et al., 2017). The buffering effect of MI on alcohol problems may have been particularly clear for sexual orientation discrimination in the current study because participants were MSM who received the intervention in an SGM-focused health center from sexual minority men and women whose careers were committed to improving SGM health. Thus, the study setting may have facilitated the creation of connections between participants and counselors in a relatively brief counseling relationship. In terms of other counselor and participant concordant identities, such as HIV status and race/ethnicity, the implications for the current study are less clear. The HIV statuses of counselors in the current study were not apparent or discussed, and all counselors were non-Hispanic/Latinx White. Any potential impact of concordance and discordance along race/ethnicity therefore cannot be assessed.
The buffering effect of MI on alcohol problems over and above its effects on alcohol use has potential implications for clinical training. Individual-level interventions do not solve problems of racism, heterosexism, or HIV stigma at the structural, institutional, or community levels that serve as social determinants of health (Earnshaw et al., 2013). Discrimination is a fundamental cause of health disparities (Hatzenbuehler et al., 2013; Hatzenbuehler and Pachankis, 2016), and structural interventions are sorely needed that address these social conditions. Nonetheless, it is encouraging that MI, a brief, person-centered intervention, can have a beneficial effect in supporting marginalized groups like MSM and preventing some harms that may result from experiences of identity-based discrimination. Further research is needed to examine the essential components of person-centered interventions that cause this buffering effect, such as patient-provider rapport or specific content discussed in counseling sessions, with particular attention paid to discussions of discrimination experiences that may arise spontaneously. Results suggest that, at a minimum, training in core relational components of MI may be valuable for healthcare professionals as a means of fostering supportive relationships with marginalized clients.
Consistent with prior research, we found that experiences of identity-based discrimination, and more specifically sexual orientation discrimination, were associated with alcohol problems over time, over and above alcohol use, in the absence of alcohol intervention. Identity-based discrimination may be related to alcohol problems through a multi-step mediational pathway, such that discrimination leads to motives to drink in order to cope with stressors (Bresin and Mekawi, 2021; Kahler et al., 2015), leading to increased rates of heavy drinking (Elliott et al., 2016), and subsequent alcohol problems (Wray et al., 2016b). Cross-sectional studies show that drinking to cope statistically mediates the association between discrimination (based on gender, race/ethnicity, sexual orientation, and HIV status) and alcohol problems (Feinstein and Newcomb, 2016; Hatzenbuehler et al., 2011; Wray et al., 2016b), over and above alcohol use (Hatzenbuehler et al., 2011; Wray et al., 2016b). Results of longitudinal research conducted with Asian American college students found a temporal association between racial discrimination, coping motives, and alcohol problems, such that racial discrimination at baseline was associated with drinking to cope six months later, which was related to alcohol problems one year later—controlling for time-varying alcohol use and baseline alcohol problems (Le and Iwamoto, 2019). Coping motives were measured only at baseline in the current study, which limited our ability to test longitudinal associations among discrimination, coping motives, alcohol use and problems. Future analyses should consider how drinking motives change over time and how that change may be related longitudinally to changes in alcohol outcomes.
4.1. Strengths & Limitations
This study has several strengths, most notably the large sample size and randomized controlled trial design. Additionally, given the sample shared being gay, bisexual or MSM and cisgender, we can be more confident that our findings are representative of the population of MSM with HIV in this geographic region. However, this study had a few key limitations. First, the sample lacked racial diversity which likely contributed to the low racial discrimination scores in this sample. Moreover, participants recruited from Boston, MA may experience relatively less sexual orientation-based discrimination when compared to states with fewer LGBTQ-equality laws and policies (Movement Advancement Project, 2020). This limits the generalizability of these findings for groups disproportionately impacted by HIV not well represented within this sample, namely predominately Black or Latinx adults with HIV and individuals living in less LGBTQ-protective geographic regions experiencing greater discrimination. Future studies should recruit more representative samples, especially given the disproportionately high rates of HIV among Black MSM (CDC, 2020). Additionally, all participants were asked discrimination questions about their race/ethnicity, and there were some, albeit few, who endorsed racial/ethnic discrimination experiences and also identified as non-Hispanic White. Our current measures did not ask participants about other oppressed ethnic identities that could also identify as White race, such as Middle Eastern/North African or Jewish ancestry or birth, for example. Thus, it is difficult to determine what identity these participants were thinking about when responding to the assessment. Rather than discounting participants’ lived experiences and responses to what are considered valid or invalid experiences of discrimination based on race or ethnicity, we included these data in the current analysis, recognizing that future research should include more comprehensive measures of race or ethnicity. Finally, because the MI intervention was compared to HIV care as usual, we cannot say that MI specifically drove the effects found. Relatedly, the current study did not examine the content of MI sessions specifically. It would be useful to understand what content arose in sessions and the context of the counseling sessions that may facilitate an empathic, supportive conversation and relationship likely to provide a buffering effect on alcohol problems.
4.2. Conclusions
In the present study, we found that an MI intervention reduced the impact of identity-based discrimination on alcohol-related problems among a sample of MSM living with HIV. Put another way, MI, compared to HIV care as usual was especially effective in reducing alcohol problems in those with higher levels of experienced discrimination, and in fact, had minimal impact on alcohol problems in those reporting no past year discrimination experiences. This suggests that in context of resource constraints, individuals experiencing more recent incidents of identity-based discrimination should be prioritized for person-centered, empathic interventions like MI, to reduce potentially increasing alcohol problems over time. These results are notable given that MI sessions were not designed to incorporate discussions of identity-based discrimination and its relation to drinking behavior and consequences. We posit that the nature of MI and its emphasis on creating an empathetic environment in which clients are encouraged to explore individually relevant factors related to their health behaviors facilitated participants’ ability to reduce or avoid negative consequences of their drinking. Therefore, this research further supports the efficacy of MI as a behavioral modification tool with marginalized groups. MI has been shown to be efficacious with MSM (Kahler et al., 2018; Wray et al., 2016a), but there are other marginalized populations who show health disparities as a result of identity-based discrimination. For example, transgender and non-binary samples have been shown to have substantial alcohol-related health disparities (James et al., 2016; Reisner et al., 2016). Future research should examine how MI-based interventions can be leveraged to address these disparities and attenuate the impact of identity-based discrimination on these groups.
Highlights.
Experiences of Identity-based discrimination are common among MSM with HIV
Such discrimination is related to alcohol problems over time among MSM with HIV
Brief MI for alcohol use substantially reduced this negative impact
This empathic counseling may facilitate avoiding negative consequences of drinking
Author Disclosures
This work was supported by the NIAAA Alcohol Research Center on HIV at Brown University (ARCH; P01 AA019072, PI: C.W. Kahler), the Providence/Boston Center for AIDS Research (P30AI042853), and the Center for Addiction and Disease Risk Exacerbation (CADRE; P20GM130414, PI: P.M. Monti); AG was supported by the NIMH Adolescent/Young Adult Biobehavioral HIV Research Training Grant at Rhode Island Hospital (T32 MH 07878, PI: L.K. Brown) while developing this manuscript.
Conflict of Interest
KM has received unrestricted research grants to study antiretrovirals for prevention from Gilead Science, Merck, and ViiV Healthcare, and HIV vaccines with Janssen, outside the submitted work. The authors have no other conflicts of interest to declare.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bankoff SM, McCullough MB, Pantalone DW, 2013. Patient-provider relationship predicts mental and physical health indicators for HIV-positive men who have sex with men. J. Health Psychol 18, 762–772. 10.1177/1359105313475896 [DOI] [PubMed] [Google Scholar]
- Ben J, Cormack D, Harris R, Paradies Y, 2017. Racism and health service utilisation: A systematic review and meta-analysis. PLoS ONE 12, 1–22. 10.1371/journal.pone.0189900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Landrine H, Galvan FH, Wagner GJ, Klein DJ, 2013. Perceived Discrimination and Physical Health Among HIV-Positive Black and Latino Men Who Have Sex with Men. AIDS Behav 17, 1431–1441. 10.1007/s10461-012-0397-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Wagner GJ, Galvan FH, Klein DJ, 2010. Longitudinal Relationships Between Antiretroviral Treatment Adherence and Discrimination Due to HIV-Serostatus, Race, and Sexual Orientation Among African–American Men with HIV. Ann. Behav. Med 40, 184–190. 10.1007/s12160-010-9200-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Wagner GJ, Galvan FH, Landrine H, Klein DJ, Sticklor LA, 2011. Perceived Discrimination and Mental Health Symptoms among Black Men with HIV. Cultur. Divers. Ethnic Minor. Psychol 17, 295–302. 10.1037/a0024056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boynton MH, O’Hara RE, Covault J, Scott D, Tennen H, 2014. A mediational model of racial discrimination and alcohol-related problems among african american college students. J. Stud. Alcohol Drugs 75, 228–234. 10.15288/jsad.2014.75.228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresin K, Mekawi Y, 2021. The “Why” of Drinking Matters: A Meta-Analysis of the Association Between Drinking Motives and Drinking Outcomes. Alcohol. Clin. Exp. Res 45, 38–50. 10.1111/acer.14518 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2020. HIV Surveillance Report 2018 (updated) (No. 31) Centers for Disease Control. [Google Scholar]
- Cheng H-L, Mallinckrodt B, 2015. Racial/ethnic discrimination, posttraumatic stress symptoms, and alcohol problems in a longitudinal study of Hispanic/Latino college students. J. Couns. Psychol 62, 38–49. 10.1037/cou0000052 [DOI] [PubMed] [Google Scholar]
- Cobbinah SS, Lewis J, 2018. Racism & Health: A public health perspective on racial discrimination. J. Eval. Clin. Pract 24, 995–998. 10.1111/jep.12894 [DOI] [PubMed] [Google Scholar]
- Crane HM, McCaul ME, Chander G, Hutton H, Nance RM, Delaney JAC, Merrill JO, Lau B, Mayer KH, Mugavero MJ, Mimiaga M, Willig JH, Burkholder GA, Drozd DR, Fredericksen RJ, Cropsey K, Moore RD, Simoni JM, Christopher Mathews W, Eron JJ, Napravnik S, Christopoulos K, Geng E, Saag MS, Kitahata MM, 2017. Prevalence and Factors Associated with Hazardous Alcohol Use Among Persons Living with HIV Across the US in the Current Era of Antiretroviral Treatment. AIDS Behav 21, 1914–1925. 10.1007/s10461-017-1740-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillard PK, Zuniga JA, Holstad MM, 2017. An integrative review of the efficacy of motivational interviewing in HIV management. Patient Educ. Couns 100, 636–646. 10.1016/j.pec.2016.10.029 [DOI] [PubMed] [Google Scholar]
- Dyar C, Newcomb ME, Mustanski B, 2019. Longitudinal associations between minority stressors and substance use among sexual and gender minority individuals. Drug Alcohol Depend 201, 205–211. 10.1016/j.drugalcdep.2019.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Bogart LM, Dovidio JF, Williams DR, 2013. Stigma and racial/ethnic HIV disparities: Moving toward resilience. Am. Psychol 68, 225–236. 10.1037/a0032705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EJ, Williams EC, Marshall BDL, 2018. Addressing unhealthy alcohol use among people living with HIV: recent advances and research directions. Curr. Opin. Infect. Dis 31, 1–7. 10.1097/QCO.0000000000000422 [DOI] [PubMed] [Google Scholar]
- Elliott JC, Stohl M, Aharonovich E, O’Leary A, Hasin DS, 2016. Reasons for drinking as predictors of alcohol involvement one year later among HIV-infected individuals with and without hepatitis C. Ann. Med 48, 634–640. 10.1080/07853890.2016.1206668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce RJ, Kcomt L, Veliz PT, Boyd CJ, McCabe SE, 2020a. Alcohol, Tobacco, and Comorbid Psychiatric Disorders and Associations With Sexual Identity and Stress-Related Correlates. Am. J. Psychiatry 177, 1073–1081. 10.1176/appi.ajp.2020.20010005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce RJ, Veliz PT, Boyd CJ, Hughes TL, McCabe SE, 2020b. Associations between sexual orientation discrimination and substance use disorders: differences by age in US adults. Soc. Psychiatry Psychiatr. Epidemiol 55, 101–110. 10.1007/s00127-019-01694-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein BA, Newcomb ME, 2016. The role of substance use motives in the associations between minority stressors and substance use problems among young men who have sex with men. Psychol. Sex. Orientat. Gend. Divers 3, 357–366. 10.1037/sgd0000185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN, Exten C, 2020. Sexual Orientation Differences in Alcohol Use Disorder Across the Adult Life Course. Am. J. Prev. Med 59, 428–436. 10.1016/j.amepre.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forcehimes AA, Tonigan JS, Miller WR, Kenna GA, Baer JS, 2007. Psychometrics of the Drinker Inventory of Consequences (DrInC). Addict. Behav 32, 1699–1704. 10.1016/j.addbeh.2006.11.009 [DOI] [PubMed] [Google Scholar]
- Gonzales G, Przedworski J, Henning-Smith C, 2016. Comparison of Health and Health Risk Factors Between Lesbian, Gay, and Bisexual Adults and Heterosexual Adults in the United States: Results From the National Health Interview Survey. JAMA Intern. Med 176, 1344. 10.1001/jamainternmed.2016.3432 [DOI] [PubMed] [Google Scholar]
- Haeny AM, Sartor CE, Arshanapally S, Ahuja M, Werner KB, Bucholz KK, 2019. The association between racial and socioeconomic discrimination and two stages of alcohol use in blacks. Drug Alcohol Depend 199, 129–135. 10.1016/j.drugalcdep.2019.02.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, Fromme K, 2011. Discrimination and alcohol-related problems among college students: a prospective examination of mediating effects. Drug Alcohol Depend 115, 213–220. 10.1016/j.drugalcdep.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Pachankis JE, 2016. Stigma and Minority Stress as Social Determinants of Health Among Lesbian, Gay, Bisexual, and Transgender Youth. Pediatr. Clin. North Am 63, 985–997. 10.1016/j.pcl.2016.07.003 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG, 2013. Stigma as a Fundamental Cause of Population Health Inequalities. Am. J. Public Health 103, 813–821. 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S, Herman J, Rankin S, Keisling M, Mottet L, Anafi M, 2016. The Report of the 2015 U.S. Transgender Survey
- Justice AC, McGinnis KA, Tate JP, Braithwaite RS, Bryant KJ, Cook RL, Edelman EJ, Fiellin LE, Freiberg MS, Gordon AJ, Kraemer KL, Marshall BDL, Williams EC, Fiellin DA, 2016. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend 161, 95–103. 10.1016/j.drugalcdep.2016.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Liu T, Cioe PA, Bryant V, Pinkston MM, Kojic EM, Onen N, Baker JV, Hammer J, Brooks JT, Patel P, 2017. Direct and Indirect Effects of Heavy Alcohol Use on Clinical Outcomes in a Longitudinal Study of HIV Patients on ART. AIDS Behav 21, 1825–1835. 10.1007/s10461-016-1474-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Pantalone DW, Mastroleo NR, Liu T, Bove G, Ramratnam B, Monti PM, Mayer KH, 2018. Motivational interviewing with personalized feedback to reduce alcohol use in HIV-infected men who have sex with men: A randomized controlled trial. J. Consult. Clin. Psychol 86, 645–656. 10.1037/ccp0000322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Wray T, Pantalone D, Mastroleo N, Kruis R, Mayer KH, Monti PM, 2015. Assessing Sexual Motives for Drinking Alcohol among HIV-Positive Men who have Sex with Men. Psychol. Addict. Behav. J. Soc. Psychol. Addict. Behav 29, 247–253. 10.1037/adb0000006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelso-Chichetto NE, Plankey M, Abraham AG, Ennis N, Chen X, Bolan R, Cook RL, 2018. Association between alcohol consumption trajectories and clinical profiles among women and men living with HIV. Am. J. Drug Alcohol Abuse 44, 85–94. 10.1080/00952990.2017.1335317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le TP, Iwamoto DK, 2019. A longitudinal investigation of racial discrimination, drinking to cope, and alcohol-related problems among underage Asian American college students. Psychol. Addict. Behav. J. Soc. Psychol. Addict. Behav 33, 520–528. 10.1037/adb0000501 [DOI] [PubMed] [Google Scholar]
- Lee JH, Gamarel KE, Bryant KJ, Zaller ND, Operario D, 2016. Discrimination, Mental Health, and Substance Use Disorders Among Sexual Minority Populations. LGBT Health 3, 258–265. 10.1089/lgbt.2015.0135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang K-Y, Zeger SL, 1986. Longitudinal Data Analysis Using Generalized Linear Models. Biometrika 73, 13–22. 10.2307/2336267 [DOI] [Google Scholar]
- López CI, Richards DK, Field CA, 2020. Perceived discrimination and alcohol-related problems among Hispanic college students: The protective role of serious harm reduction behaviors. J. Ethn. Subst. Abuse 1–12. 10.1080/15332640.2020.1747040 [DOI] [PubMed] [Google Scholar]
- Madhombiro M, Musekiwa A, January J, Chingono A, Abas M, Seedat S, 2019. Psychological interventions for alcohol use disorders in people living with HIV/AIDS: a systematic review. Syst. Rev 8, 244. 10.1186/s13643-019-1176-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Sobell MB, Cooper AM, Sobell LC, 1979. Test-retest reliability of retrospective self-reports in three populations of alcohol abusers. J. Behav. Assess 1, 315–326. 10.1007/BF01321373 [DOI] [Google Scholar]
- Markland D, Ryan RM, Tobin VJ, Rollnick S, 2005. Motivational Interviewing and Self–Determination Theory. J. Soc. Clin. Psychol 24, 811–831. 10.1521/jscp.2005.24.6.811 [DOI] [Google Scholar]
- Marshall BDL, Tate JP, McGinnis KA, Bryant KJ, Cook RL, Edelman EJ, Gaither JR, Kahler CW, Operario D, Fiellin DA, Justice AC, 2017. Long-term alcohol use patterns and HIV disease severity. AIDS Lond. Engl 31, 1313–1321. 10.1097/QAD.0000000000001473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, West BT, Veliz P, Boyd CJ, 2019. DSM-5 Alcohol Use Disorder Severity as a Function of Sexual Orientation Discrimination: A National Study. Alcohol. Clin. Exp. Res 43, 497–508. 10.1111/acer.13960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, 1995. The Drinker Inventory of Consequences (DrInC): An Instrument for Assessing Adverse Consequences of Alcohol Abuse : Test Manual U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Miller WR, Rollnick S, 2012. Motivational Interviewing: Helping People Change Guilford Press. [Google Scholar]
- Moak ZB, Agrawal A, 2010. The association between perceived interpersonal social support and physical and mental health: results from the national epidemiological survey on alcohol and related conditions. J. Public Health 32, 191–201. 10.1093/pubmed/fdp093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe AK, Lau B, Mugavero MJ, Mathews WC, Mayer KH, Napravnik S, Hutton HE, Kim HS, Jabour S, Moore RD, McCaul ME, Christopoulos KA, Crane HC, Chander G, 2016. Heavy Alcohol Use Is Associated With Worse Retention in HIV Care. J. Acquir. Immune Defic. Syndr 1999 73, 419–425. 10.1097/QAI.0000000000001083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Movement Advancement Project. “Equality Maps: Snapshot: LGBTQ Equality By State” https://www.lgbtmap.org/equality-maps/. Accessed 02/08/2022.
- Mulder R, Murray G, Rucklidge J, 2017. Common versus specific factors in psychotherapy: opening the black box. Lancet Psychiatry 4, 953–962. 10.1016/S2215-0366(17)30100-1 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Mahon CP, Jackson SD, Fetzner BK, Bränström R, 2020. Sexual orientation concealment and mental health: A conceptual and meta-analytic review. Psychol. Bull 146, 831–871. 10.1037/bul0000271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick H, Williams GC, 2012. Self-determination theory: its application to health behavior and complementarity with motivational interviewing. Int. J. Behav. Nutr. Phys. Act 9, 18. 10.1186/1479-5868-9-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, Holland CE, Max R, Baral SD, 2016. Global health burden and needs of transgender populations: a review. The Lancet 388, 412–436. 10.1016/S0140-6736(16)00684-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Eaton NR, Pachankis JE, 2019. Prevalence of psychiatric disorders at the intersection of race and sexual orientation: Results from the National Epidemiologic Survey of Alcohol and Related Conditions-III. J. Consult. Clin. Psychol 87, 321–331. 10.1037/ccp0000377 [DOI] [PubMed] [Google Scholar]
- Rogers AH, Jardin C, Mayorga NA, Bakhshaie J, Leonard A, Lemaire C, Zvolensky MJ, 2018. The relationship of discrimination related to sexual orientation and HIV-relevant risk behaviors among men who have sex with men. Psychiatry Res 267, 102–107. 10.1016/j.psychres.2018.05.081 [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey KB, Johnson BT, Carey MP, The MASH Research Team, 2017. Behavioral Interventions Targeting Alcohol Use Among People Living with HIV/AIDS: A Systematic Review and Meta-Analysis. AIDS Behav 21, 126–143. 10.1007/s10461-017-1886-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater ME, Godette D, Huang B, Ruan WJ, Kerridge BT, 2017. Sexual Orientation-Based Discrimination, Excessive Alcohol Use, and Substance Use Disorders Among Sexual Minority Adults. LGBT Health 4, 337–344. 10.1089/lgbt.2016.0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell MB, Maisto SA, Sobell LC, Cooper AM, Cooper TC, Sanders B, 1980. Developing a prototype for evaluating alcohol treatment effectiveness., in: Evaluating Alcohol and Drug Abuse Treatment Effectiveness: Recent Advances Pergamon Press, New York, NY, pp. 129–150. [Google Scholar]
- Stockton MA, Giger K, Nyblade L, 2018. A scoping review of the role of HIV-related stigma and discrimination in noncommunicable disease care. PloS One 13, e0199602. 10.1371/journal.pone.0199602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su J, Kuo SI-C, Derlan CL, Hagiwara N, Guy MC, Dick DM, 2020. Racial discrimination and alcohol problems among African American young adults: Examining the moderating effects of racial socialization by parents and friends. Cultur. Divers. Ethnic Minor. Psychol 26, 260–270. 10.1037/cdp0000294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tieu H-V, Koblin BA, Latkin C, Curriero FC, Greene ER, Rundle A, Frye V, 2020. Neighborhood and Network Characteristics and the HIV Care Continuum among Gay, Bisexual, and Other Men Who Have Sex with Men. J. Urban Health 97, 592–608. 10.1007/s11524-018-0266-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vu M, Li J, Haardörfer R, Windle M, Berg CJ, 2019. Mental health and substance use among women and men at the intersections of identities and experiences of discrimination: insights from the intersectionality framework. BMC Public Health 19, 108. 10.1186/s12889-019-6430-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Lawrence JA, Davis BA, Vu C, 2019. Understanding how discrimination can affect health. Health Serv. Res 54 Suppl 2, 1374–1388. 10.1111/1475-6773.13222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams EC, Hahn JA, Saitz R, Bryant K, Lira MC, Samet JH, 2016. Alcohol Use and Human Immunodeficiency Virus (HIV) Infection: Current Knowledge, Implications, and Future Directions. Alcohol. Clin. Exp. Res 40, 2056–2072. 10.1111/acer.13204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray TB, Grin B, Dorfman L, Glynn TR, Kahler CW, Marshall BDL, van den Berg JJ, Zaller ND, Bryant KJ, Operario D, 2016a. Systematic review of interventions to reduce problematic alcohol use in men who have sex with men. Drug Alcohol Rev 35, 148–157. 10.1111/dar.12271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray TB, Pantalone DW, Kahler CW, Monti PM, Mayer KH, 2016b. The role of discrimination in alcohol-related problems in samples of heavy drinking HIV-negative and positive men who have sex with men (MSM). Drug Alcohol Depend 166, 226–234. 10.1016/j.drugalcdep.2016.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]


