Abstract
Background:
Studies demonstrated associations between maternal exposure to household air pollution from cooking and increased risk of adverse birth outcomes in offspring; however, the modifying effect of socioeconomic status (SES) on this association has not been explored.
Objectives:
In a cohort of pregnant women with 800 single live births between 2016–2017 in rural and semi urban areas of Bangladesh, we tested the hypotheses that kitchen location and cooking fuel type affect birth outcomes (birth weight, low birth weight [LBW] and small for gestational age [SGA) and these associations vary by SES.
Methods:
Demographic characteristics including SES, kitchen location and fuel type were assessed in prenatal visits. Neonatal anthropometric measurements were recorded within 72 hours of births. We performed multivariable linear and logistic regressions adjusting for potential confounders to test the study hypotheses.
Results:
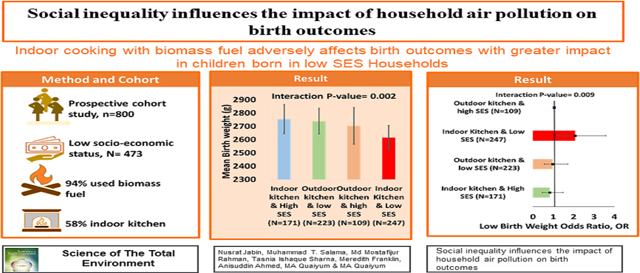
For newborns from households with indoor kitchens, adjusted mean birth weight was 65.13g (95% confidence interval [CI]: −118.37, −11.90) lower and the odds of LBW and SGA were 58% (odds ratio [OR]:1.58, 95% CI: 1.12, 2.24) and 41% (OR: 1.41, 95% CI: 1.05, 1.92) higher compared to those born in households with outdoor kitchens. We found SES significantly modified the associations between kitchen location and birth outcomes in households using biomass fuels. Newborns from low SES households with indoor kitchens had 89g lower birth weight and a higher odds of being born with LBW (OR: 2.08, 95% CI 1.23, 3.58), and SGA (OR: 1.70, 95% CI 1.06, 2.76) than those born in high SES households using outdoor kitchens.
Conclusions:
In areas with poor access or affordability to clean fuel such as in our study population, cooking in an outdoor kitchen can reduce the burden of LBW and SGA, particularly for low SES households. Promoting outdoor kitchens is a possible intervention strategy to mitigate adverse birth outcomes.
Keywords: Kitchen location, Fuel type, Socioeconomic status, Birth weight, Low birth weight, Small for gestational age
Graphical Abstract
1. Introduction
Household air pollution (HAP) from cooking fuel is a significant source of both indoor and outdoor air pollution across the globe with 2.8 billion people relying on biomass fuel.1 A large body of evidence has documented adverse health impacts of HAP on birth outcomes (low birth weight [LBW], preterm birth [PB], small for gestational age [SGA], stillbirth, neonatal mortality).2–7
While promoting clean cooking fuel and technology has been a global priority, inadequate infrastructure to supply electricity and liquid petroleum gas (LPG) has limited universal acceptance of such initiatives. There are 2.6 billion people without access to clean fuel worldwide in 2019, and it is projected that 28% world population will not have such access by 2030.8 While previous studies identified cooking fuel type as main determinant of HAP9, studies have also reported that kitchen location affects HAP levels and higher pollutant concentrations have been observed for indoor cooking regardless of the fuel type used compared to outdoor cooking.10 Thus, investigation of the joint effects of cooking fuel and kitchen location on health outcomes will facilitate a better understanding of these exposure-outcome relationships.
In the context of low to middle income countries (LMIC), the distributions of cooking fuel types and kitchen location vary by socioeconomic status (SES), as people from low SES background are less likely to afford electricity and LPG as cooking fuel and more likely to cook outdoors compared to those with high SES.8 Epidemiologic studies have considered SES in multivariate analyses as a confounding variable since it is linked with the three major determinants to health, namely environmental exposures, healthcare and health behavior.11 Furthermore, SES often accounts as a surrogate for social disparity or inequality as it is correlated with factors such as housing and neighborhood quality, ambient noise, residential crowding,12–15 psychological stress, and health behavior.11,16
Younger et al17 recently published a systematic review where the associations between HAP from unclean cooking fuels and birth outcomes were investigated. The authors conducted literature search of papers published from May 1, 2013 to June 12, 2021 where these associations were investigated in pregnant women who were living in LMIC. Of the 20 papers examining the relationship between HAP exposure and birth weight, LBW and/or SGA as the outcomes, only 4 were from cohort studies.2,18–20 Different SES indicators were used in these cohort studies -Modified Kuppuswamy socioeconomic scale18, maternal education2,20, SES by asset index quintiles obtained from principal component analysis based on asset ownership and various household characteristics20 and asset index which was based on total number household ownership out of ten items.19 While the final models adjusted for these indicators of SES, the effect estimates of SES indicators on birth outcomes from multivariate analysis were not presented and the interactive effects of SES and HAP exposures on birth outcomes were also not reported in these papers. Because many health and social determinants vary by SES, it is important to examine whether the associations between HAP exposures and birth outcomes vary by SES – an investigation that has not been routinely reported in literature.
Based on these contexts from existing literature and knowledge gaps, we aimed to test two hypotheses: (1) Cooking fuel type and kitchen location have independent and joint effects on birth outcomes such as birth weight, LBW and SGA, and (2) these associations vary by SES. We tested these hypotheses in a prospective pregnancy cohort study conducted in Bangladesh.
2. Methodology
2.1. Study Population and Design
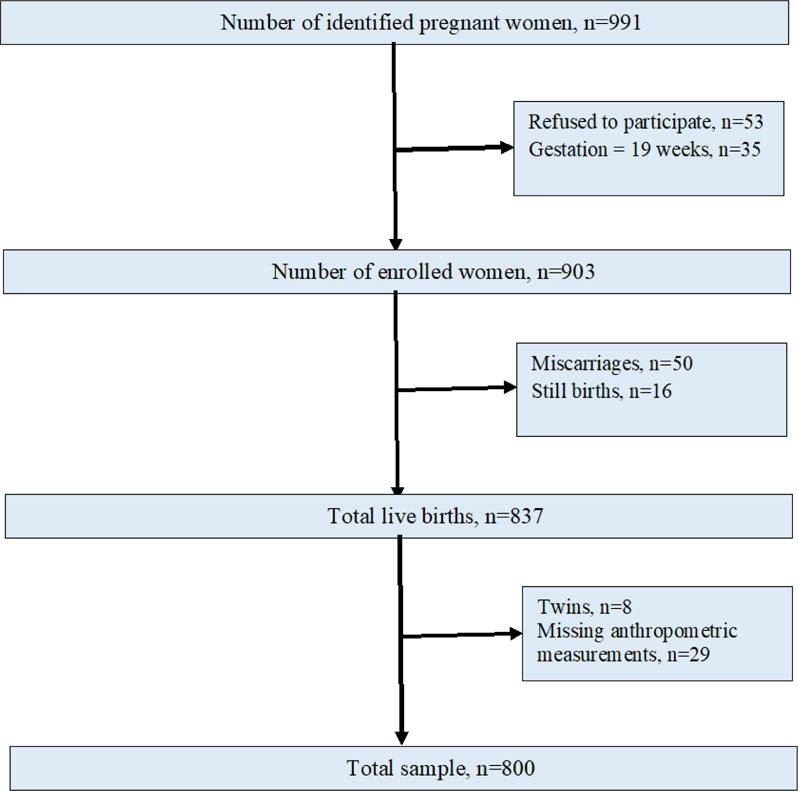
The study was conducted in Chirirbandar and Saidpur upazillas (smallest administrative areas) of Rangpur division (largest administrative units), located in the northwestern part of Bangladesh. Both areas are comprised of a mix of rural and semi-urban populations. Saidpur has a population of 264,461 in 58,137 households within an area of 121.68 km2 (30,067 acres),21 and Chirirbandar (308.68 km2 or 76,276 acres) has a population of 292,500 in 68,415 households.22 As part of the Cook Stove Pregnancy Cohort Study (CSPCS), we recruited women within their first 18 weeks of pregnancy from these two adjacent upazillas through active surveillance between November 1, 2016 and March 31, 2017. During recruitment, each of the study field workers (N=10) worked with 15–20 village health workers who belonged to different governmental and nongovernmental organizations that were involved in child and maternal healthcare at the community level. The village health workers regularly made house visits covering all households within their jurisdiction once a month to identify newly pregnant women based on menstrual history or medical diagnosis. An early detection qualitative urine strip [“Diaspot”® hCG Urine Card, DiaSpot Diagnostics, USA; overall accuracy: >90%, sensitivity: 100%, 95% CI (95%-100%), and specificity: 100%, 95% CI (95%- 100%)] was used to assess pregnancy among women who had missed at least two menstrual periods. The village health workers were provided the incentive to inform the assigned study field workers of any pregnancies within 18 weeks of gestation. The study field workers then visited the identified women and details of the study was communicated. Both verbal and written consents were obtained from the women and their husbands. During the recruitment period, 938 women were requested to come to a health facility to complete a pelvic ultrasound to assess the gestational week of pregnancy, collect blood and urine samples, measure height and weight, and to complete the baseline questionnaire along with a routine antenatal check-up by a physician who screened the mothers for anemia, hypertension, diabetes, and presence of helminths and treated these conditions when indicated. Women with confirmed pregnancies within 18 weeks were invited to participate in the study. We excluded 35 women from the study who were 19 or more weeks of gestation based on ultrasound. Of the 903 women enrolled in this study between 6–18 weeks of pregnancy (mean:14 weeks), there were 837 live births of which 8 were twins who were excluded from the study to minimize outcome misclassification. A total of 93 women moved out of the study area to their parental home prior to delivery. Of those 93 women, 29 were unable to provide their infants’ birth weight over phone as they had home delivery, and no one measured these infants’ birth weight. The other 64 mothers provided the birth weight of the newborn over the phone as the delivery took place at some health facility. Therefore, the final sample size comprised of 800 singleton live birth with birth weight measurements available within 72 hours of birth (Figure 1).
Figure 1:
Flowchart of study population.
2.2. Data Collection
Each study health worker was involved with 80–90 expectant mothers for the duration of the study period. They conducted in-person survey of the mothers once every trimester, starting immediately after confirming pregnancy, within 72-hours of a childbirth, and every 3-months during the first year after birth. All women were provided with mobile phone numbers of the assigned study health worker and study office number to respond to any query and to coordinate care about pregnancy and childbirth. Mobile phone numbers of at least one of the members of the household and one neighbor were also collected. Detailed information of sociodemographic characteristics, household characteristics, kitchen location, types of cooking fuel used, and data on maternal physical health were collected at each survey. For data analysis, information on sociodemographic characteristics, kitchen location, and fuel types were used from the baseline survey as no changes were observed during the pregnancy among this population. Each mother’s weight and height were measured during the baseline survey to obtain body mass index (BMI).
2.3. Ethical approval
Ethical approval for the study protocol, consent forms (verbal and written), and data collection forms were obtained from the Institutional Review Board of the University of Southern California and the ethical review committee of the International Centre for Diarrhoeal Disease Research, Bangladesh.
2.4. Exposure variables
Detailed information on cooking stove type, cooking fuel type, and kitchen location were collected from the mothers. Cooking fuel types were categorized into two categories: clean fuel vs. biomass fuel. Gas or/and electricity were considered as clean fuel and cow dung, wood, leaves, straw, and other crop residues were considered as biomass fuel. The clean fuel users used either electric or gas stoves while 96% of the biomass fuel users used traditional stoves and 4% used improved stoves. Kitchen location was defined as a binary variable: indoor vs outdoor. Kitchen ‘indoor’ included kitchens both inside the bedroom or as a separate kitchen adjacent to the living quarters within the house, whereas ‘outdoor’ kitchens were separated by open spaces from the living quarters. We also created a composite variable from fuel type and kitchen location to capture HAP exposure of the mother. Mothers using clean fuel in outdoor kitchen were considered to have lowest HAP exposures while those using biomass fuel in indoor kitchen were considered to have highest HAP exposures.
2.5. Outcome variables
We included a range of birth outcome variables in this study: birth weight, low birth weight (LBW) and small for gestational age (SGA). Birth weight was measured within 72 hours (on average 24 hrs) of birth by field team personnel. The field team measured birth weights for 736 infants of this study population by themselves and for the remaining 64 infants, birth weights were reported by their mothers. The measurements were done with the infant clad only in thin clothing without any shoes or caps. The cradle was attached to an electronic digital weighing scale (WeiHeng WH-A25 Rechargeable Portable Electronic Scale, double accuracy 5 gm for 0–10 kg range) and calibrated using a 2kg weight before measuring the weight of the infant. LBW was defined as birth weight <2500g and SGA as birth weight less than 10th percentile of specific sex and gestational age as per the INTERGROWTH-21st new-born size standards.23
2.6. Covariates
Gestational age at delivery was estimated based on ultrasonography confirmed gestational age at the time of recruitment. Maternal age (as continuous), parity, and health conditions (maternal body mass index, any diagnosis of diabetes, hypertension, or other chronic diseases) were self-reported.
We created Wealth Index by applying principal component analysis to 43 variables including productive assets (land ownership, livestock, poultry, etc.), non-productive assets (own home, refrigerator, TV, bicycle, motorbike, etc.), household utilities (water source and toilet type), household characteristics, type of family (nuclear or extended) and number of family members, educational level and occupations of the mother and father, and parental religion and ethnicity (language used at home).24 The first principal component, which explained 13.65% of the total variance, served as the Wealth Index and was split into quintiles where the lowest three quintiles represented low socioeconomic status (SES). Further details regarding construction of the Wealth Index are available in the supplement “Construction of Wealth Index”.
2.7. Statistical analysis
Summary statistics included means and standard deviations to describe continuous variables and frequencies and percentages for categorical variables. We investigated the associations of type of cooking fuel and kitchen location on birth outcomes, adjusted for potential confounders using multivariable regression. For birth weight, adjusted effect estimates and their 95% confidence intervals (95% CI) were reported form multiple linear regressions; for LBW and SGA, odds ratios (ORs) and their 95% CI were reported from multivariable logistic regressions. All models were adjusted for maternal age, maternal BMI, parity, gestational age, infant sex, and SES. Logistic regression analysis of SGA was not adjusted for infant sex or gestational age as SGA was determined based on gestational age and infant sex-specific cut-offs. We tested effect modification by SES for the associations between kitchen location and birth outcomes using likelihood ratio tests, comparing the goodness of fit of models with and without the interaction term. Stata version 15 was used to prepare the dataset and R 4.0.3 (R studio 1.3.1093) was used to perform all statistical analyses.
3. Results:
3.1. Study Population
More than half of the pregnant women (60%) were from Chirirbandar and had low socioeconomic background (Table 1). About 40% of the mothers were nulliparous with mean maternal age of 22.2 years and mean BMI of 21.9 kg/m2 in the first trimester. Nearly 75% of the mothers completed at least elementary school (5th grade). In our cohort, 52.4% newborns were male, about 11% were preterm, and the mean birth weight was 2700g (±377g). About 39% of the infants were SGA and 29% were LBW. About 58% of the kitchens were located indoors and biomass fuels were used for cooking in about 94% households. Of the 50 household that used clean fuel, 33 of them used gas and 17 used electricity as their cooking fuel. None of the mothers in this study were active smokers, but about 40% mothers reported presence of a smoker in the household.
Table 1:
Basic information of study population (N=800): Demographics, exposure, and outcomes.
| Total (N=800) | High SES (N=327) | Low SES (N=473) | P-value* | |
|---|---|---|---|---|
|
| ||||
| Maternal factors | ||||
| Age (years) | ||||
| Mean ± SD | 22.2 ± 4.3 | 22.7 ±4.43 | 21.9 ±4.10 | 0.007 |
| Education level | ||||
| ≤5th grade | 207 (25.9%) | 48 (14.7%) | 159 (33.6%) | <0.001 |
| Body Mass Index (Kg/m2) | ||||
| Mean ± SD | 21.9 ± 3.9 | 22.8 ±4.34 | 21.3 ±3.36 | <0.001 |
| Parity | ||||
| Nulliparous | 316 (39.5%) | 141 (43.1%) | 175 (37.0%) | 0.095 |
| Delivery types | ||||
| Normal | 343 (42.9%) | 101 (30.9%) | 242 (51.2%) | |
| Episiotomy | 104 (13.0%) | 48 (14.7%) | 56 (11.8%) | <0.001 |
| Cesarean | 353 (44.1%) | 178 (54.4%) | 175 (37.0%) | |
| Infant factors | ||||
| Infant sex | ||||
| Male | 419 (52.4%) | 171 (52.3%) | 248 (52.4%) | 0.99 |
| Gestational age (weeks) | ||||
| Mean ± SD | 38.5 ± 1.9 | 38.4 ±1.95 | 38.6 ±1.81 | 0.207 |
| Birth weight (g) | ||||
| Mean ± SD | 2700 ± 377 | 2740 ±394 | 2670 ±421 | 0.017 |
| Low birth weight | ||||
| Yes | 228 (29.2%) | 83 (25.4%) | 153 (32.3%) | 0.041 |
| Small for Gestational Age (SGA) | ||||
| Yes | 308 (39.4%) | 113 (34.6%) | 203 (42.9%) | 0.021 |
| Preterm Birth | ||||
| Yes | 91 (11.4%) | 39 (11.9%) | 52 (11.0%) | 0.768 |
| Exposures | ||||
| Kitchen location | ||||
| Outdoor | 337 (42.1%) | 114 (34.9%) | 223 (47.1%) | <0.001 |
| Indoor | 463 (57.9%) | 213 (65.1%) | 250 (52.9%) | |
| Cooking fuel type | ||||
| Biomass fuel | 750 (93.8%) | 280 (85.6%) | 470 (99.4%) | <0.001 |
| Clean fuel | 50 (6.2%) | 47 (14.4%) | 3 (0.6%) | |
| Secondhand tobacco smoke exposure | ||||
| Yes | 319 (39.9%) | 108 (33.0%) | 211 (44.6%) | 0.001 |
P-value is based on Chi-square tests for categorical variables and t-tests for continuous variables.
Compared to mothers from low SES households, mothers of high SES were less likely to have 5th grade or lower education (33.6% vs. 14.7%, p-value <0.001), higher BMI (21.3 vs. 22.8 kg/m2, p-value <0.001), and less likely to have normal delivery (51.2% vs. 30.9%, p-value <0.001). Kitchen location and mothers’ choice of cooking fuel were also significantly associated with socioeconomic status (p-value <0.001). Compared to high SES households, households of lower SES were less likely to cook indoor (65.1% vs. 52.9%, p-value <0.001) and use clean fuel (14.4% vs. 0.6%, p-value <0.001). LBW (32.3% vs. 25.4% p-value 0.041) and SGA (42.9% vs. 34.6% p-value 0.021) were more frequent among infants born in the low SES households compared to infants born in high SES households.
3.2. Risk Factors of Birth weight, LBW and SGA
Based on the multivariate regression model, we observed that male sex, assisted birth (via episiotomy or Cesarean section), maternal BMI, and higher gestational age at birth were all statistically significantly associated with higher mean birth weight, whereas nulliparity, low SES, and presence of an indoor kitchen were statistically significantly associated with lower birth weight (Table 2). In households with indoor kitchens, the mean birth weight was about 65.13g (95% CI −118.37g, −11.90g) lower compared to infants born in households with outdoor kitchens. The odds of LBW and SGA were 58% (95% CI 1.12, 2.24) and 41% (95% CI 1.05, 1.92) higher, respectively for infants born to households with indoor kitchens. Although clean fuel use was associated with higher birth weight and lower risk of SGA, the associations were not statistically significant. No association was observed between secondhand smoking and birth outcomes, and it did not confound the associations observed in Table 2 (not shown).
Table 2:
Multivariable regression model for possible risk factors of birth outcomes: birth weight, low birth weight and small for gestational age. *
| Weight (g)† | Low Birth Weight (LBW)‡ | Small for Gestational Age (SGA)† | |
|---|---|---|---|
| Risk factors | Estimates (95% CI) | Odds Ratios (95% CI) | Odds Ratios (95% CI CI) |
|
| |||
| Infant sex: male | 55.97 | 1.07 | --- |
| (4.54, 107.40) | (0.77, 1.49) | ||
| Gestational age | 86.09 | 0.65 | --- |
| (72.25, 99.92) | (0.59, 0.72) | ||
| Maternal age | −5.77 | 1.00 | 1.02 |
| (−14.24, 2.70) | (0.95, 1.06) | (0.97, 1.07) | |
| Maternal BMI | 12.73 | 0.99 | 0.93 |
| (5.21, 20.26) | (0.95, 1.04) | (0.89, 0.98) | |
| Nulliparity | −135.18 | 1.75 | 1.80 |
| (−206.88, −63.47) | (1.10, 2.78) | (1.20, 2.72) | |
| Low SES | −63.98 | 1.60 | 1.31 |
| (−120.20, −7.76) | (1.11, 2.33) | (0.95, 1.80) | |
| Episiotomy delivery | 99.85 | 0.51 | 0.76 |
| (15.37, 184.32) | (0.28, 0.90) | (0.47, 1.21) | |
| Cesarean delivery | 65.13 | 0.71 | 0.76 |
| (7.17, 123.09) | (0.49, 1.03) | (0.55, 1.05) | |
| clean fuel use | 63.10 | 1.03 | 0.71 |
| (−52.04, 178.25) | (0.49, 2.10) | (0.35, 1.40) | |
| Kitchen location: indoor | −65.13 | 1.58 | 1.41 |
| (−118.37, −11.90) | (1.12, 2.24) | (1.05, 1.92) | |
All multivariate regression models were adjusted for infant sex, gestational age, maternal age, maternal BMI, parity, SES, delivery type, fuel type and kitchen location. SGA models were not adjusted for infant sex and gestational age since SGA was generated adjusting for infant sex and gestational age. Mother’s age was centered to mean age of 22.2 years; BMI to mean value of 21.9 kg/m2, and gestational age to mean of 38.5 weeks. Statistically significant effect estimates and odds ratios with respective 95% CIs are presented in bold.
Adjusted effect estimates and 95% confidence interval (CI) are from multivariable linear regression.
Adjusted odds ratio (OR) and 95% confidence interval (CI) are from multivariable logistic regression.
3.3. Joint Effect of Cooking Fuel and Kitchen Location:
A consistent pattern of association was observed when we examined the joint effects of type of cooking fuel and kitchen location through stratified analysis (Table 3). We found that mean birth weight was highest for newborns who were born in households with outdoor kitchens where clean fuel was used, and the lowest in those who were born in households with indoor kitchens and used biomass fuel. The mean difference in birth weight between these two groups was nearly 300g. Similarly, lower ORs were observed for LBW and SGA though the risk estimates did not reach statistical significance for the potentially least exposed group due to low sample size for that group. However, among households using biomass fuels, the ORs for LBW and SGA were significantly lower (0.64 and 0.70, respectively) in newborns who were born in households with outdoor kitchens than those with kitchens indoors.
Table 3:
Joint effects of fuel-type and kitchen location on birth outcomes (N = 800). *
| Factors | Birth Weight (g) | Low Birth Weight (LBW) | Small for Gestational Age (SGA) |
|---|---|---|---|
| Adjusted Estimate (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | |
|
| |||
| Indoor kitchen & biomass fuel used (N=418) | 2671 | Ref | Ref |
| (2635, 2708) | |||
| Indoor kitchen & clean fuel used (N=45) | 2698 | 1.08 | 0.81 |
| (2582, 2812) | (0.50, 2.24) | (0.38, 1.65) | |
| Outdoor kitchen & biomass fuel used (N=332) | 2734 | 0.64 | 0.70 |
| (2695, 2776) | (0.45, 0.90) | (0.51, 0.95) | |
| Outdoor kitchen & clean fuel used (N=5) | 2965 | 0.43 | 0.51 |
| (2630, 3299) | (0.02, 3.39) | (0.02, 4.21) | |
All multivariate regression models were adjusted for infant sex, gestational age, maternal age, maternal BMI, parity, SES, and delivery type. SGA models were not adjusted for infant sex and gestational age since SGA was generated adjusting for infant sex and gestational age. Mother’s age was centered to mean age of 22.2 years; BMI to mean value of 21.9 kg/m2, and gestational age to mean of 38.5 weeks.
Adjusted effect estimates and 95% confidence interval (CI) are from multivariable linear regression.
Adjusted odds ratio (OR) and 95% confidence interval (CI) are from multivariable logistic regression.
3.4. Modifying Effect of Socioeconomic Status
We found that SES significantly modified the associations between kitchen location and mean birth weight (p-value of interaction = 0.002) and LBW (p-value for interaction = 0.009) (Table 4). Because only three households from low SES used clean fuel, we restricted this analysis to households where biomass fuel was used for cooking. Newborns from a low SES household with an indoor kitchen had 89g lower birth weight, had over 2-times higher odds of being born with LBW, and were 1.7 times more likely to have SGA compared to the those born in a high SES household using outdoor kitchen (Table 4). The average birth weight and ORs of having SGA or LBW for infants born in high-SES households with indoor kitchen or low-SES households with outdoor kitchen were not statistically significantly different from infants born in high SES households with outdoor kitchen. Finally, when associations were compared within low SES households using biomass fuel, infants born in households with outdoor kitchens had significantly higher birth weight and significantly lower odds of LBW and SGA compared to infants born in households with indoor kitchens.
Table 4:
Joint effects of SES and kitchen location on birth outcomes among households using biomass fuel (N=750). *
| Birth Weight (g) | Low Birth Weight (LBW) | Small for Gestational Age (SGA) | |
|---|---|---|---|
| Predictors | Mean | Odds Ratios (CI) | Odds Ratios (CI) |
|
| |||
| Outdoor kitchen & high SES (N=109) | 2704 | Ref | Ref |
| (2636, 2774) | |||
| Outdoor kitchen & low SES (N=223) | 2739 | 0.97 | 1.03 |
| (2692, 2788) | (0.56, 1.71) | (0.63, 1.69) | |
| Indoor kitchen & High SES (N=171) | 2754 | 0.82 | 1.06 |
| (2699, 2809) | (0.45, 1.48) | (0.64, 1.77) | |
| Indoor Kitchen & Low SES (N=247) | 2615 | 2.08 | 1.70 |
| (2570, 2661) | (1.23, 3.58) | (1.06, 2.76) | |
| P-value: interaction | 0.002 | 0.009 | 0.151 |
All multivariate regression models were adjusted for infant sex, gestational age, maternal age, maternal BMI, parity, and delivery type. SGA models were not adjusted for infant sex and gestational age since SGA was generated adjusting for infant sex and gestational age. Mother’s age was centered to mean age of 22.2 years; BMI to mean value of 21.9 kg/m2, and gestational age to mean of 38.5 weeks.
Adjusted effect estimates and 95% confidence interval (CI) are from multivariable linear regression.
Adjusted odds ratio (OR) and 95% confidence interval (CI) are from multivariable logistic regression.
3.5. Sensitivity Analyses
To investigate whether maternal report of birth weight influenced the results, we conducted a sensitivity analysis by limiting the analysis to newborns with measured birth weight (n=736). In this restricted sample, the overall association of clean fuel, kitchen location and other risk factors were essentially unchanged from what is presented in Table 2 (See supplementary Table S1). Because fewer households used clean fuel (i.e., 6.2%), we also performed a separate sensitivity analysis investigating whether kitchen location is a risk factor for birth outcomes when restricted to biomass fuel users only. In this sensitivity analysis, we found that having an indoor kitchen was associated with lower birth weight (-61.64g, 95% CI: −114.68, −8.60) and higher odds of LBW (OR:1.58, 95% CI: 1.12, 2.25) and SGA (OR:1.42, 95% CI: 1.05, 1.93) (See Supplementary Table S2).
4. Discussion
The study was unique in its investigation of both independent and joint effects of kitchen location, fuel type, and SES on birth outcomes within a pregnancy cohort in Bangladesh. Our results showed that kitchen location (indoor vs. outdoor) and SES, irrespective of cooking fuel type, were strong determinants of birth outcomes (birth weight, LBW and SGA). Infants born in households with indoor kitchens were more likely to have higher risk of LBW and SGA and lower mean birth weight, while those born to households with lower SES were more likely to have higher risk of LBW and low mean birth weight. Finally, SES significantly modified the relationship between kitchen location and birth outcomes in a way that newborns from low SES background had significant detrimental effects of an indoor kitchen on birth outcomes than any other combination of SES and kitchen location groups.
To date, some studies have documented relationships between the use of biomass fuel and increased risk of LBW and SGA compared to the use of clean fuels (LPG/electricity) across the globe.25,26 Households using biomass fuels have higher levels of household PM2.5 compared to households using clean fuel.9 Intrauterine exposure to PM2.5 can lead to fetal growth retardation through different biological mechanisms involving oxidative stress, DNA methylation, mitochondrial DNA alteration and endocrine disruption.27 Although not statistically significant due to a small proportion of household using clean fuel, we found higher birth weight and lower risk of SGA in newborns born in households that used clean fuel for cooking. A recent pregnancy cohort study in Ghana also observed non-statistically significant positive association between use of biomass fuel and LBW (OR=1.05) or SGA (OR=1.43).2
The detrimental effects of biomass fuel use on birth outcomes were greater in households with indoor kitchens. In Bangladesh, kitchens are often traditionally located outdoors, away from the living quarters, and are often open (having only a roof) or semi-open (have a roof and two to three side walls). Therefore, those kitchens would be better ventilated than indoor kitchens. Currently, following the newer, more urban-like architectural design, kitchens are often located inside households, contiguous to the living quarters, and are closed (roof and four walls). These kitchens often do not have exhaust fans and often are smaller and less ventilated than outdoor kitchens which can lead to higher indoor HAP levels following cooking. Higher pollution levels have been reported in indoor kitchens compared to those outdoors.28 A randomized controlled trial from Rwanda reported that households using improved cookstoves located outside were significantly associated with 73% and 57% reductions in PM2.5 compared to households with indoor cooking using traditional or improved cookstove, respectively.29 A recent study from Sri Lanka found that the risk of LBW among children born to households using biomass fuel in low ventilated kitchens was 4.63 (95% CI: 1.54,13.93) fold higher compared to infants born to households using clean fuel with highly ventilated kitchen.30 We observed that even in households using biomass fuels, the risk of LBW and SGA was significantly lower by 36% and 30% in households with outdoor kitchen compared to indoor kitchen, respectively. A large cross-sectional study (n=22,789) from Bangladesh reported that indoor cooking was significantly associated with higher risk of LBW (OR=1.25) and neonatal mortality (OR=1.25) after controlling for fuel type.5
In the current study, SES and kitchen location had interactive effects on birth outcomes. Lower SES is a known risk factor of lower mean birth weight and increased risk of SGA and LBW.31 While we have also observed similar associations for birth outcomes (Table 2), our results extend previous findings by showing that the adverse effects of HAP are more pronounced in newborns born in low SES households. SES not only represents parental education and/or economic conditions of the household, but also acts as surrogates for environmental exposures, social inequality, healthcare, and health behavior-related factors, that often remains unmeasured in epidemiologic studies. Here we aimed to investigate the effects of SES on birth outcomes beyond the confounding effect of SES. We found that potential risk factors such as maternal age, maternal BMI (surrogate for maternal nutritional status during pregnancy), and access to care (mode of delivery), exposures (secondhand tobacco smoke, biomass fuel use, kitchen location) vary between the high- and low-socioeconomic group (Table 1). It is plausible that low SES in our study acted as surrogates for other unmeasured factors that represent social inequalities, and differences in health-related factors and psychosocial stressors in this group compared to those with high SES in modulating the adverse effects of HAP on birth outcomes.32
The use of biomass fuel for cooking and heating in the LMICs has been identified as a major cause of HAP and global health burden.8 According to the latest Sustainable Development Goal 7 in 2019, 2.6 billion of the world population (66%) had access to clean fuel and technology for cooking, which is only a 9% increase since 2010.8 At this current pace, about 30% of the world population will have no access to clean fuel for cooking by 2030. While all actions should be taken to increase the rate of biomass fuel replacement by cleaner fuel, we also need to acknowledge that many infants will be born during this period with low birth weight, SGA and LBW. Based on the observed effect of indoor kitchen location in the current study we estimated the population attributable risk of indoor kitchen in the general population and the lower socioeconomic status (Supplement Method). Indoor kitchen accounted for 14.4% of LBW and 10.4% of SGA in this population and 2.6% of LBW and 15.6% of SGA among the low SES population, respectively (See Supplementary Table S3). By promoting outdoor kitchens in Bangladesh, a large proportion of LBW can be prevented while steps are taken to move away from biomass fuel in the coming decades.
The major strength of the current study is that it is one of the few pregnancy cohort studies from an LMIC (i.e. China20, India,18 Ghana2, and Tanzania19) investigating the associations of intrauterine biomass fuel exposure on birth outcomes.2 The cohort was recruited through active surveillance of pregnancy in the study area, making the study population representative of the source population. Both exposure and outcomes assessments were well characterized in the study with minimum misclassification as maternal exposure was assessed during 2nd and 3rd trimester and anthropometric measurements of the infants were performed by trained field team personnel within 48 hours (24–72 hours) of birth. Due to the availability of detailed information on kitchen and household characteristics and maternal health, we were able to adjust our models for potential confounders and investigate their possible modifying effect.
Despite the strengths of the study, one of the major limitations was that a small number of households used clean fuel for cooking (n=50, 6.2%). Although this prevalence of clean fuel use was representative of the study population, it limited our ability to observe a significant effect of clean fuel on birth outcomes. However, this statistic highlights the fact that large-scale utilization of clean fuel for cooking in rural and semi-urban locales in LMICs remains challenging. Another limitation of the study was that cookstove related pollution exposure was assessed using survey questionnaires. As we used dichotomous variables like fuel type and kitchen location, we could not quantify dose dependent effect of pollution and there could be some level of exposure misclassification. However, this nondifferential misclassification in exposure assessment may have attenuated the observed risk estimates rather than creating spurious associations.
For 64 infants, we were not able to objectively measure their birth weight and relied on maternal reports. The mean of reported birth weight (mean 2890 g, SD=560 g) was higher than the mean of measured birth weight (mean=2680 g, SD=392 g) with lower incidence of LBW and SGA. Newborns whose birth weights were reported rather than measured were more likely to be from high SES households, used clean fuels and had indoor kitchens and were more likely to be preterm, requiring assisted birth (see Table S4). To address this, we conducted sensitivity analysis restricting to newborns with measured birth weight and the results from restricted sample remained unchanged from that found in overall population (See Supplementary Table S1) indicating that maternal report of birth weight did not introduce any bias in our study findings.
4.1. Conclusion
Providing access to clean fuel and newer technology for cooking and heating in LMIC is imperative to reduce the global health burden of biomass fuel use. Until now, the transition from biomass to clean fuel has been slow in these nations.8 While aggressive steps should be undertaken to provide access to clean fuel to as many people as possible, alternative behavioral and environmental approaches should be pursued to minimize the impact of biomass fuel on children’s health before universal utilization of clean fuel can be achieved. Here we provide evidence that promoting outdoor kitchens, away from the living quarters, can help reduce the burden of SGA and LBW in Bangladesh.
Supplementary Material
Highlights.
Indoor cooking increased the odds of low birth weight and small for gestational age
Low Socioeconomic status associated with low birth weight
Socioeconomic status modified the effect of kitchen location on birth outcomes
Footnotes
Credit author statement
Nusrat Jabin: Conceptualization, Data Curation, Formal Analysis, Visualization, Writing – Original Draft Preparation. Muhammad T. Salam: Supervision, Writing – Original Draft Preparation. Mostafijur Rahman:Writing – Analytical support, Review & Editing.Tasnia Ishaque Sharna: Investigation, Data curation, Writing – Review & Editing. Meredith Franklin: Formal Analysis, Writing – Review & Editing. Anisuddin Ahmed: Project administration, Writing – Review & Editing. MA Quaiyum: Project administration, Methodology, Writing – Review & Editing. Talat Islam: Conceptualization, Methodology, Funding Acquisition, Investigation, Supervision, Writing – Original Draft Preparation
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.WHO guidelines for indoor air quality: Household fuel combustion. In: World Health Organization.; 2014. [PubMed] [Google Scholar]
- 2.Weber E, Adu-Bonsaffoh K, Vermeulen R, et al. Household fuel use and adverse pregnancy outcomes in a Ghanaian cohort study. Reprod Health. 2020;17(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roberman J, Emeto TI, Adegboye OA. Adverse Birth Outcomes Due to Exposure to Household Air Pollution from Unclean Cooking Fuel among Women of Reproductive Age in Nigeria. IJERPH. 2021;18(2):634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nisha MK, Alam A, Raynes-Greenow C. Variations in perinatal mortality associated with different polluting fuel types and kitchen location in Bangladesh. International Journal of Occupational and Environmental Health. 2018;24(1–2):47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan MN, CZ B. Nurs, Mofizul Islam M, Islam MR, Rahman MM. Household air pollution from cooking and risk of adverse health and birth outcomes in Bangladesh: a nationwide population-based study. Environ Health. 2017;16(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haider MR, Rahman MM, Islam F, Khan MM. Association of Low Birthweight and Indoor Air Pollution: Biomass Fuel Use in Bangladesh. Journal of Health and Pollution. 2016;6(11):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epstein MB, Bates MN, Arora NK, Balakrishnan K, Jack DW, Smith KR. Household fuels, low birth weight, and neonatal death in India: The separate impacts of biomass, kerosene, and coal. International Journal of Hygiene and Environmental Health. 2013;216(5):523–532. [DOI] [PubMed] [Google Scholar]
- 8.Tracking SDG 7: The Energy Progress Report. Washington DC: IEA, IRENA, UNSD, World Bank, WHO.;2021. [Google Scholar]
- 9.Pratiti R. Household air pollution related to biomass cook stove emissions and its interaction with improved cookstoves. AIMS Public Health. 2021;8(2):309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Langbein J. Firewood, smoke and respiratory diseases in developing countrie -The neglected role of outdoor cooking. PLoS One. 2017;12(6):e0178631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adler NE, Newman K. Socioeconomic Disparities In Health: Pathways And Policies. Health Affairs 2002;21(2):60–76. [DOI] [PubMed] [Google Scholar]
- 12.Fiscella K, Williams DR. Health Disparities Based on Socioeconomic Inequities: Implications for Urban Health Care. Academic Medicine. 2004;79(12):1139–1147. [DOI] [PubMed] [Google Scholar]
- 13.Hajat A, Hsia C, O’Neill MS. Socioeconomic Disparities and Air Pollution Exposure: a Global Review. Curr Envir Health Rpt. 2015;2(4):440–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mackenbach JP, Stirbu I, Roskam A-JR, et al. Socioeconomic Inequalities in Health in 22 European Countries. N Engl J Med. 2008;358(23):2468–2481. [DOI] [PubMed] [Google Scholar]
- 15.Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc 2007;99(9):1013–1023. [PMC free article] [PubMed] [Google Scholar]
- 16.Evans GW, Kantrowitz E. Socioeconomic Status and Health: The Potential Role of Environmental Risk Exposure. Annu Rev Public Health. 2002;23(1):303–331. [DOI] [PubMed] [Google Scholar]
- 17.Younger A, Alkon A, Harknett K, Jean Louis R, Thompson LM. Adverse birth outcomes associated with household air pollution from unclean cooking fuels in low- and middle-income countries: A systematic review. Environmental Research. 2021:112274. [DOI] [PubMed] [Google Scholar]
- 18.Balakrishnan K, Ghosh S, Thangavel G, et al. Exposures to fine particulate matter (PM2. 5) and birthweight in a rural-urban, mother-child cohort in Tamil Nadu, India. Environ Res 2018;161:524–531. [DOI] [PubMed] [Google Scholar]
- 19.Wylie BJ, Kishashu Y, Matechi E, et al. Maternal exposure to carbon monoxide and fine particulate matter during pregnancy in an urban Tanzanian cohort. Indoor Air 2017;27(1):136–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jiang M, Qiu J, Zhou M,et al. Exposure to cooking fuels and birth weight in Lanzhou, China: a birth cohort study. BMC Public Health. 2015;15:712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Statsitics BBo. Sistrict Statsitics:-2011 Nilphamari. In: Planning Mo, ed. Bangladesh: Bangaldesh Government; 2013. [Google Scholar]
- 22.Statsitics BBo. District Statistics - 2011 Dinajpur. In: Planning Mo, ed. Bangladesh: Government of Bangladesh; 2013. [Google Scholar]
- 23.Tuzun F, Yucesoy E, Baysal B, Kumral A, Duman N, Ozkan H. Comparison of INTERGROWTH-21 and Fenton growth standards to assess size at birth and extrauterine growth in very preterm infants. J Matern Fetal Neonatal Med 2018;31(17):2252–2257. [DOI] [PubMed] [Google Scholar]
- 24.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy and Planning. 2006;21(6):459–468. [DOI] [PubMed] [Google Scholar]
- 25.Odo DB, Yang IA, Knibbs LD. A Systematic Review and Appraisal of Epidemiological Studies on Household Fuel Use and Its Health Effects Using Demographic and Health Surveys. Int J Environ Res Public Health. 2021;18(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee KK, Bing R, Kiang J, et al. Adverse health effects associated with household air pollution: a systematic review, meta-analysis, and burden estimation study. Lancet Glob Health. 2020;8(11):e1427–e1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Z, Tang Y, Song X, Lazar L, Li Z, Zhao J. Impact of ambient PM(2.5) on adverse birth outcome and potential molecular mechanism. Ecotoxicol Environ Saf. 2019;169:248–254. [DOI] [PubMed] [Google Scholar]
- 28.Nasir ZA, Colbeck I, Ali Z, Ahmad S. Indoor particulate matter in developing countries: a case study in Pakistan and potential intervention strategies. Environ Res Lett. 2013;8(2):024002. [Google Scholar]
- 29.Rosa G, Majorin F, Boisson S, et al. Assessing the Impact of Water Filters and Improved Cook Stoves on Drinking Water Quality and Household Air Pollution: A Randomised Controlled Trial in Rwanda. PLOS ONE. 2014;9(3):e91011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vakalopoulos A, Dharmage SC, Dharmaratne S, et al. Household Air Pollution from Biomass Fuel for Cooking and Adverse Fetal Growth Outcomes in Rural Sri Lanka. Int J Environ Res Public Health. 2021;18(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ngandu CB, Momberg D, Magan A, Norris SA, Said-Mohamed R. Association Between Household and Maternal Socioeconomic Factors with Birth Outcomes in the Democratic Republic of Congo and South Africa: A Comparative Study. Matern Child Health J 2021;25(8):1296–1304. [DOI] [PubMed] [Google Scholar]
- 32.Chen E, Miller GE. Socioeconomic status and health: mediating and moderating factors. Annu Rev Clin Psychol. 2013;9:723–749. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.