1. Introduction
Until today, COVID-19 has had a high impact on the population worldwide. The first cases of the virus were reported in 2019 and on the 11th of March 2020, the World Health Organisation (WHO) officially declared the rapid spread of the virus as a global pandemic (WHO, 2020a; Zhu et al., 2020). To prevent the rapid spread of the virus, enhanced hygienic rules and social restrictions have been introduced among other pandemic measures in Germany. After one and a half years later, in 2021, the global pandemic and the accompanying measures still play a major role in people's life. As prevalences, incidences, and mortality rates are still high in Germany, the pandemic retains its high societal toll (Bendau et al., 2020; Robert Koch Institut, 2021b; Scholz et al., 2021). Even though specific vaccinations have been made available to the public, vaccination skepticism is present and leaves approximately 15 million people in Germany unvaccinated (Ashton, 2021; Bendau et al., 2021; Umakanthan and Lawrence, 2022; Robert Koch Institut, 2021a). Additionally, novel virus mutations like the omicron variant emerged (Burki, 2022). As a result, restrictions and governmental measures to prevent the spread of the virus are still part of everyday life. Those rules and measures negatively influence the population's level of satisfaction which is further highlighted by sinking trust in the government related to the handling of the pandemic (Skoda et al., 2021). All over the world, a decrease in well-being has been reported as well (Vindegaard and Benros, 2020).
Not only does the COVID-19 pandemic influence well-being, but it also has a negative impact on mental health globally (Bäuerle et al., 2020; Brodeur et al., 2021; Castelli et al., 2020; Gray et al., 2020; Liu et al., 2021; Serafini et al., 2020; Vindegaard and Benros, 2020). Compared to prevalences before the onset of the pandemic, higher levels of anxiety symptoms, depressive symptoms, sleeping problems, stress, and psychological distress have been reported during the initial phase of the pandemic (Bäuerle et al., 2020; Hetkamp et al., 2020; Vindegaard and Benros, 2020). The psychological distress seems to increase throughout the pandemic, as higher levels of depressive symptoms have been reported during the second lockdown phase than during the first lockdown phase in Germany (Bendau et al., 2020; Moradian et al., 2021). Another factor, the so-called “pandemic fatigue” has now emerged during the ongoing pandemic and causes distress globally (WHO, 2020b). According to the WHO (2020a), pandemic fatigue is a reaction to the ongoing and long-lasting COVID-19 pandemic. Pandemic fatigue is a state of exhaustion and it leads to distress, negatively affects emotions, cognitions, and behavior (WHO, 2020b). Moreover, it is associated with sleep problems, fear, sadness, and worrying (Labrague and Ballad, 2021). Also, pandemic fatigue can decrease the motivation to tackle the COVID-19 pandemic and to adhere to the restrictions (WHO, 2020b). Even though it is assumed that pandemic fatigue is a factor that negatively influences well-being (WHO, 2020b), specific research investigating its associated factors is rare.
The impact of the COVID-19 pandemic on mental health during its initial phase has been displayed in a great part of the recent literature (Bäuerle et al., 2020; Brodeur et al., 2021; Castelli et al., 2020; Gray et al., 2020; Serafini et al., 2020; Vindegaard and Benros, 2020). However, most of the research was merely conducted in 2020 during earlier phases of the pandemic and only few research examining the mental health situation during the COVID-19 pandemic in 2021 exists (Creswell et al., 2021; Vahratian et al., 2021). In addition to that, past research mostly investigated how distinct and often smaller sets of variables are related to each other, using a top-down hypothesis testing approach (Taylor, 2020). This top-down approach can detect relationships between variables by analyzing variables in an isolated manner, however, inconspicuous but significant relationships when examining variables altogether might not get detected. When investigating the COVID-19 pandemic and its associated factors, the top-down approach alone might be deficient as a complex interconnectedness between several variables is assumed (Di Blasi, 2021; Taylor, 2019; Taylor et al., 2020).
Network analysis offers a bottom-up approach to analyze multivariate data by investigating complex relationships between different sets of variables (Borsboom et al., 2021). Specifically, network analysis investigates the organization and interconnectedness between variables represented in a network based on the assumption that distinct components within a system interact with each other (Borsboom and Cramer, 2013; Borsboom et al., 2021). Within this approach, the variables in a network are referred to as “nodes”, whereas the connections among nodes are called “edges” (Borsboom and Cramer, 2013; Borsboom et al., 2021). The strength of the association between nodes is called “edge weight” which is represented by a statistical parameter, most commonly by partial correlations (Borsboom and Cramer, 2013; Borsboom et al., 2021). Network analysis is a useful tool in psychology research, as most theories, such as the biopsychosocial model and cognitive-behavioral models, are based on diverse variables and the complex interactions between them (Hevey, 2018; Taylor, 2020). Therefore, the network approach is a promising method to reveal interconnections within a multivariate set of relevant determinants like psychological and behavioral factors during the COVID-19 pandemic.
Although recent studies examined the relation of different psychological and behavioral variables in the face of the COVID-19 pandemic (Bäuerle et al., 2020; Morgul et al., 2020; Skoda et al., 2021; Weismüller et al., 2021; Wismans et al., 2021), there is lack of research on how they are related to each other in an interplay of a set of multiple variables, particularly during the pandemic situation in 2021. Moreover, the role that pandemic fatigue might have in relation to mental health concerns is not fully understood. Therefore, the current study investigated how pandemic fatigue, COVID-19 related fear, depressive symptoms, generalized anxiety symptoms, sleep problems, COVID-19 related cognitions and behavior, and vaccination attitudes were related to each other using the network analysis approach. Already existing psychometric network analyses analyzed different sets of variables during earlier phases of the pandemic in 2020 (Di Blasi et al., 2021; Liu et al., 2021; Taylor et al., 2020; Zavlis et al., 2021). However, pandemics are dynamic, and their impact differs between specific phases (Taylor, 2017). As a result, the goal of the current study was to obtain a coherent picture of the COVID-19 pandemic in 2021, to explore the role of pandemic fatigue, and to pinpoint possible risk factors that affect mental health.
2. Methods
2.1. Study design, participants, and procedure
The study consisted of a cross-sectional study design. The ethics committee of the Medical Faculty of the University of Duisburg-Essen approved the setup of the study (20-9307-BO). From the 18th of January 2021 until the 16th of September 2021, the online survey was spread via several media platforms, such as social media, online newspapers, and print media. Participation was voluntary and without reimbursement. After obtaining electronic informed consent, the participants filled out the questionnaire, which took approximately 14 min. The questionnaire was administered in German. Withdrawal from the study was possible at any time. The data were processed anonymously. In total, 5138 participants filled in the survey, of which 4462 completed it. As only participants who completed the survey were included, the final sample consisted of 4462 participants. Of them, 39,6% identified as male (n = 1766), whereas 60,4% identified as female (n = 2969). All participants were between 18 and 85 years old. The inclusion criteria for participating were (1) age above 18, and (2) sufficient knowledge of the German language. See Table 1 for demographic characteristics.
Table 1.
Demographic characteristics of the final Sample (N = 4462).
| N | % | ||
|---|---|---|---|
| Gender | |||
| Female | 2969 | 60.4 | |
| Male | 1766 | 39.6 | |
| Age | |||
| 18-24 | 786 | 17.6 | |
| 25-34 | 1047 | 23.5 | |
| 35-44 | 975 | 21.9 | |
| 45-54 | 899 | 20.1 | |
| 55-64 | 576 | 12.9 | |
| 65 or older | 179 | 4.0 | |
| Level of Education | |||
| University Degree | 1630 | 36.5 | |
| High School Degree | 1423 | 31.9 | |
| Higher Middle School Degree | 1089 | 24.4 | |
| Lower Middle School Degree | 236 | 5.3 | |
| Without School Degree | 24 | .5 | |
| Other Form of Schooling | 60 | 1.3 | |
| Residence area | |||
| Urban area (population size > 20000) | 2726 | 61.1 | |
| Rural area (population size < 20000) | 1736 | 38.9 | |
| Marital Status | |||
| Single | 1349 | 30.2 | |
| Married | 1772 | 39.7 | |
| In a relationship | 991 | 22.2 | |
| Separated/Divorced | 270 | 6.1 | |
| Widowed | 40 | .9 | |
| Other | 40 | .9 | |
| Work area | |||
| Not employed | 965 | 21.6 | |
| Health Care System | 503 | 11.3 | |
| Economy Sector | 1004 | 22.5 | |
| Industry | 414 | 9.3 | |
| Academic Research | 54 | 1.2 | |
| Civil Service | 218 | 4.9 | |
| IT | 199 | 4.5 | |
| Gastronomy | 66 | 1.5 | |
| Architecture & Construction | 168 | 3.8 | |
| Art & Culture | 63 | 1.4 | |
| Media | 55 | 1.2 | |
| Social Sector | 401 | 9.0 | |
| Other | 352 | 7.8 | |
| Health Status | |||
| Physical Illness | 1003 | 22.5 | |
| Mental Illness | 460 | 10.3 |
2.2. Measures
Generalized anxiety symptoms were assessed with the German version of the Generalized Anxiety Disorder 7-item Scale (GAD-7; Williams, 2014). The GAD 7 is a questionnaire, which assesses different anxiety symptoms during the past two weeks. The items were based on a four-point Likert scale (0 = never; 3 = almost every day). The internal consistency was high (α = .91).
Depressive symptoms were assessed based on the German version of the Patient Health Questionnaire-2 (PHQ-2; Löwe et al., 2005): The German version of the PHQ-2 consists of two items measuring depressive symptoms during the past two weeks. The items were based on a four-point Likert scale (0 = never; 3 = almost every day). The internal consistency was high (α = .84).
Sleep problems were assessed based on the following item: “In the past two weeks, did you have problems falling asleep and staying asleep?”. The item was scored on a four-point Likert scale (0 = never; 3 = almost every day). The item is part of the Patient-Health-Questionnaire-9 (PHQ-9; Kroenke and Spitzer, 2002).
Pandemic fatigue was assessed with four items which measured levels of restlessness, shiftlessness, exhaustion, and fatigue on a 7-point-Likert scale (1 = disagree at all; 7 = totally agree). The questions were part of the German version of the SF-36-Health Survey (SF-36; Bullinger, 2000) and they were adapted to the current COVID-19 pandemic. A total score was calculated and a high score indicated a high level of pandemic fatigue, whereas a low score indicated a low level of pandemic fatigue. The internal consistency was high to excellent (α = .88).
COVID-19 related fear was assessed with the COVID-19 Anxiety Questionnaire (C-19-A; Petzold et al., 2020). The C-19-A is a validated questionnaire, and an item example includes “In the past seven days, I felt restless and anxious while thinking about the COVID-19 pandemic”. The items are scored on a five-point-Likert scale (1 = never; 7 = always). A total score was calculated, and a high score indicated a high level of COVID-19 related fear, whereas a low score indicated a low level of COVID-19 related fear. The internal consistency was high (α = .85).
Attitudes towards vaccinations during the COVID-19 pandemic were assessed with the German version of the 5C scale (G5C; Betsch et al., 2018). The G5C scale is a validated questionnaire that assesses psychological antecedents of vaccinations. The following psychological antecedents were measured: trust in the security of vaccinations, complacency, constraints of getting vaccinated, calculated reservation, and belief in collective responsibility (Betsch et al., 2018). The items were scored on a 7-point Likert scale (1 = disagree at all; 7 = totally agree). When interpreting the G5C scale, each item was analyzed separately. The G5C shows high concurrent and construct validity (Betsch et al., 2018).
Trust in government related to the COVID-19 pandemic measures was assessed, based on Bäuerle et al. (2020), with four self-generated items based on a seven-point Likert scale (1 = disagree at all; 7 = totally agree). The following items were used: “I feel like Germany is well prepared regarding the COVID-19 pandemic.”, “I think that all relevant measures are taken to tackle the COVID-19 virus.”, “I have trust in the governmental system in Germany”, “I think the selected measures to tackle the COVID-19 crisis are appropriate.”. A total score was calculated and a high score indicated a high level of trust, whereas a low score indicated a low level of trust. The internal consistency was acceptable to high (α = .76).
The perceived limitation through the pandemic measures was assessed with the following item: “How much do you and your family feel restricted regarding the pandemic measures?”. This item was based on a five-point Likert scale (1 = not at all; 5 = a lot).
Safety behavior was assessed with eight items and, based on Weismüller et al. (2021), divided into adherent and dysfunctional safety behavior. Adherent safety behavior (ASB; Weismüller et al., 2021) was assessed with four items based on a 7-point Likert scale (1 = disagree at all; 7= totally agree). Item examples include: “In the past two weeks, I used to wash and disinfect my hands more often.”, and “In the past two weeks, I avoided public and crowded places.”. The internal consistency was high to excellent (α = .87). Dysfunctional safety behavior (DSB; Weismüller et al., 2021) was assessed with four items based on a 7-point Likert scale (1 = disagree at all; 7= totally agree) as well. The internal consistency for DSB was high (α = .8). For both ASB and DSB, a total score was calculated and a high score indicated a high level of safety behavior, whereas a low score indicated a low level of safety behavior.
How much time individuals spend in individual research was assessed by the following item: “How much time, on average, do you use every day to inform yourself about COVID-19?”. Participants could choose between zero to ten minutes, ten to 30 min, 30 to 60 min, one to two hours, more than two hours, or more than 5 h.
Subjective level of information related to COVID-19 was assessed, based on Bäuerle et al. (2020), with three self-generated items based on a 7-point Likert scale (1 = disagree at all; 7 = totally agree). The following items were used: “I feel well informed about the COVID-19 virus.”, “I feel well informed about the restrictions that are being used to prevent the spread of the virus.”, and “I understand the advice from the health authorities related to the COVID-19 virus”. A total score was calculated, and a high score indicated a high level of personal education, whereas a low score indicated a low level of personal education. The internal consistency was high (α = .79).
2.3. Data analysis
To achieve sufficient power, a minimum sample size from 250 to 350 is required, if the network consists of 20 nodes or less (Constantin et al., 2021).
The data were analyzed using the statistical software R, version 4.1.1 (R Core Team, 2021). Missing data was handled using listwise deletion. The following packages were used: qgraph, igraph, bootnet, and EGAnet (Csardi and Nepusz, 2006; Epskamp et al., 2012, 2018; Golino and Epskamp, 2017). First, the network was estimated and visualized. Next, centrality indices were computed. Then, an exploratory graph analysis (EGA; Golino and Epskamp, 2017) was conducted. Last, the network's stability and accuracy were assessed via bootnet.
The following measures were selected as nodes: trust in government related to COVID-19 pandemic, perceived limitations through pandemic measures, pandemic fatigue, COVID-19 related fear, adherent safety behavior, dysfunctional safety behavior, subjective level of information related to COVID-19, time invested in personal research, mistrust in the security of vaccinations, complacency, constraints of getting vaccinated, calculated reservation, belief in collective responsibility, generalized anxiety symptoms, depressive symptoms, and sleep problems. This resulted in a partial correlation network of 16 nodes. Within a partial correlation network, partial correlations display the relationship between two nodes, while controlling for all other nodes in the network. A graphical Least Absolute Shrinkage and Selection Operator (glasso; Friedman et al., 2008) was used for edge estimation. The Extended Bayesian Information Criterion (EBIC; Chen and Chen, 2008) was applied with a tuning parameter of .5.
Degree centrality and three centrality indices namely strength, closeness, and betweenness were estimated. Degree centrality adds up the number of edges that the node has. The strength index expresses the sum of the edge weights of all edges that a corresponding node has with other nodes in the network. Node strength is the most important centrality index (Hevey, 2018). A high strength index reflects the high importance of that particular node in the network. The closeness index identifies the average distance of a node to all other nodes by taking into account the indirect connections that node has to other nodes (Hevey, 2018). Closeness gives insight into how nodes affect changes in the network and vice versa (Hevey, 2018; Borgatti, 2005). A high closeness index indicates that a node which considerably affects changes in the network but which is also highly affected by changes within the network (Borgatti, 2005). The betweenness index quantifies how often a node is placed on the shortest path between two other nodes (Opsahl et al., 2010). A high betweenness index indicates that the node plays an important role in connecting other nodes (Saramäki et al., 2007).
When analyzing network topology, it is recommended to not identify clusters of communities by visual inspection, but to conduct a corresponding statistical analysis (Fried, 2016). Therefore, an exploratory graph analysis (EGA) using the EGAnet package was conducted (Golino and Epskamp, 2017). EGA detects and graphically displays communities in the network using the walktrap algorithm (Golino and Epskamp, 2017).
Bootstrap procedures were conducted for edge weight variation, significance of edge weight and node strength differences, and correlation stability of the centrality indices.
3. Results
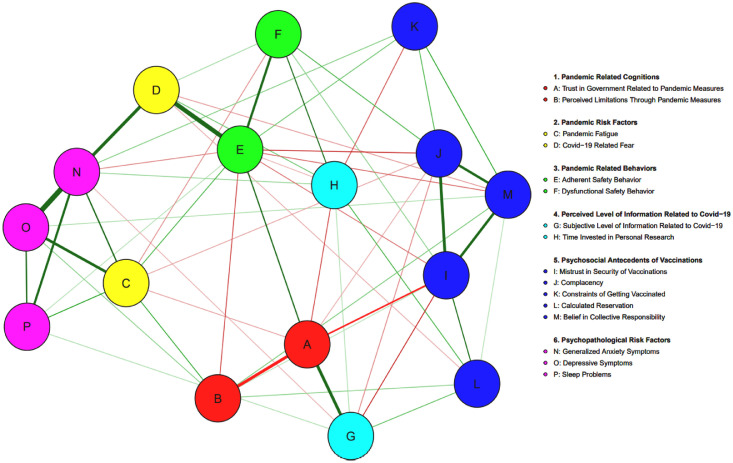
Fig. 1. shows the visualized partial correlation network. In total, 64 out of 120 edges have emerged, which indicates a dense network structure. In total, 44 edges were positive (69%) and 20 (31%) were negative. See Appendix A of the supplementary material for a graphical representation of the network with displayed edge weights. The following strongest positive edges have been identified: depressive symptoms (O) and generalized anxiety symptoms (N) (r = .49), adherent safety behavior (E) and COVID-19 related fear (D) (r = .43), generalized anxiety symptoms (N) and COVID-19 related fear (D) (r = .33), trust in government related to pandemic measures (A) and subjective level of information related to COVID-19 (G) (r = .31), mistrust in security of vaccinations and complacency (r = .30), pandemic fatigue (C) and depressive symptoms (O) (r = .29), mistrust in security of vaccinations and belief in collective responsibility (r = .28), complacency and belief in collective responsibility (r = .27), and generalized anxiety symptoms (N) and sleep problems (P) (r = .26). The strongest negative edge weights were between trust in government related to pandemic measures (A) and perceived limitations through pandemic measures (B) (r = -.31), and trust in government related to pandemic measures (A) and mistrust in the security of vaccinations (I) (r = -.20).
Fig. 1.
Visualized Partial Correlation Network. Letters A to P represent the selected nodes and the lines between those nodes represent edges. Colors of the nodes represent the theoretical topics the nodes have been divided into. Green edges display positive partial correlations, whereas red edges display negative partial correlations. The thickness of the edges represents the indication of the strength of the edge. The thicker the edge, the higher the edge weight.
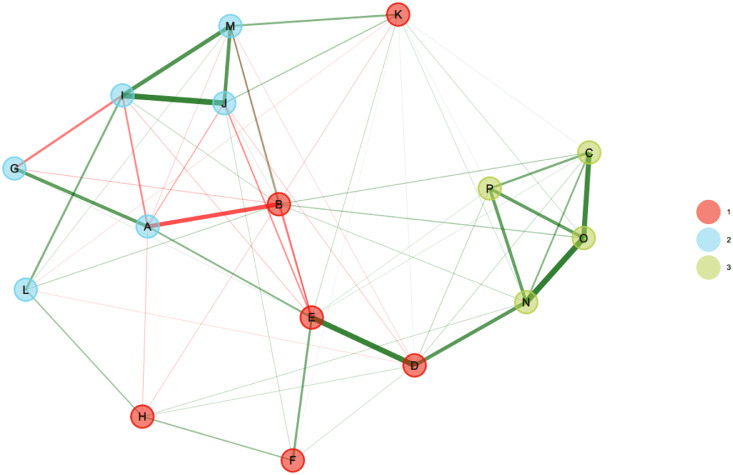
An EGA, which can be seen in Fig. 2 ., was conducted to detect node communities in the network. In total, three communities have been identified. The first community consisted of nix nodes, namely perceived limitations through pandemic measures (B), constraints of getting vaccinated (K), time invested in personal research (H), COVID-19 related fear (D), adherent safety behavior (D), and dysfunctional safety behavior (F). Within this community, edge weights were both positive and negative. The other six nodes, namely trust in government related to pandemic measures (A), subjective level of information related to COVID-19 (G), and the vaccination attitudes mistrust in the safety of vaccinations (I), complacency (J), belief in collective responsibility (M), and calculated reservation (L) built up the second community. This community displayed both positive and negative edges as well. The third community consisted of the four nodes pandemic fatigue (C), depressive symptoms (O), generalized anxiety symptoms (N), and sleep problems (P). This cluster showed only strong positive edges indicating a dense interconnectedness of these variables. Overall, the network topology revealed that the second and the third community were not directly connected, as they did not share significant edges. In contrast, the first community was densely connected with both other communities through significant edges.
Fig. 2.
Visualized Exploratory Graph Analysis. For node legend, see Fig. 1. The colors of the node represent the community the respective node belongs to. In total, three communities have been identified. Green lines between the nodes represent positive edges, whereas red lines between the nodes stand for negative edges. The thickness of the edge represents the strength of the edge weights.
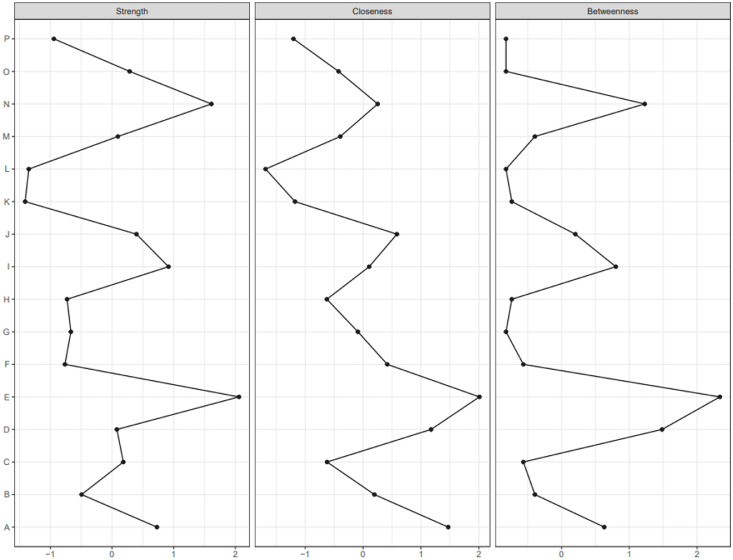
The centrality indices can be seen in Fig. 3 . The nodes with the highest degree centrality were adherent safety behavior (E), generalized anxiety symptoms (N), trust in government related to pandemic measures (A), pandemic fatigue (C), and complacency (M). The nodes adherent safety behavior (E), generalized anxiety symptoms (N), mistrust in the security of vaccinations (I), and trust in government related to pandemic measures (A) have been found to have the highest strength index. The nodes adherent safety behavior (E), trust in government related to pandemic measures (A), and COVID-19 related fear (D) showed the highest closeness index. The highest betweenness index was displayed by adherent safety behavior (E), COVID-19 related fear (D), and generalized anxiety symptoms (N). Based on the centrality indices, adherent safety behavior (E), generalized anxiety symptoms (N), COVID-19 related fear (D), and trust in the government related to pandemic measures (A) were identified as the most influential nodes.
Fig. 3.
Centrality indices strength (left), closeness (middle), and betweenness (right). Letters on the y-axis represent the allocated nodes. For a node legend, see Fig. 1. Numerical values on the x-axis represent z-values associated with the respective centrality index.
Bootstrap procedures were conducted for edge weight variation, the significance of edge weight and node strength differences, and the correlation stability of the centrality indices. The bootstrapping procedures indicated excellent stability and interpretability of both the network and centrality indices. For visualization and detailed description of the undertaken measures, see appendix B of the supplementary material.
4. Discussion
The current study investigated the interplay between various psychological factors during the COVID-19 pandemic in 2021 using network analysis. Overall, results revealed a dense network with three clusters and many interconnections. Adherent safety behavior, generalized anxiety symptoms, COVID-19 related fear, and trust in government related to pandemic measures have been identified as the most influential nodes during the COVID-19 pandemic.
The strongest connection has been observed between depressive and generalized anxiety symptoms. This shows that depressive and generalized anxiety symptoms are intertwined and are likely co-occur during the COVID-19 pandemic. This is in line with pre-pandemic research as well, in which depression and anxiety show high comorbidity at both disorder and symptom levels (Cramer et al., 2010; Jacobson and Newman, 2017). Moreover, the existence of one symptom serves as a risk factor for the other (Jacobson and Newman, 2017). The second strongest connection has been found between COVID-19 related fear and adherent safety behavior, suggesting that fear and behavior potentially influence each other. This is in line with Weismüller et al. (2021), who identified a link between COVID-19 fear and adherent safety behavior as well. Not only did COVID-19 related fear display a strong connection to adherent safety behavior but it was also related to generalized anxiety symptoms. This suggests that also fear and generalized anxiety are likely to influence each other in the current pandemic situation. Further analyses revealed that generalized anxiety symptoms and COVID-19 related fear were separated into different clusters, suggesting that COVID-19 related fear and generalized anxiety highly correlate but originate from different psychological concepts. This is supported by similar findings in recent literature (Heeren, 2020; Öhman, 2008; Schweda et al., 2021). As a result, it is proposed to address COVID-19 related fear and generalized anxiety differently.
Trust in government has been identified to play a central role during the COVID-19 pandemic, which is in line with past research by Skoda et al. (2021). This factor was most strongly related to the subjective level of information related to COVID-19 and the perceived limitations through the pandemic measures. The positive correlation between trust in government related to pandemic measures and subjective level of information related to COVID-19 indicates that subjective knowledge about COVID-19 can lead to higher trust in the government, possibly because of general knowledge about the virus and the necessary measures to prevent further spread is given. Going along with that, higher trust in the government might decrease the perceived limitations due to the pandemic measures and vice versa. This is in line with Da Silva et al. (2021), who found a positive association between trust in government and the willingness to socially isolate within the COVID-19 pandemic. Overall, these findings highlight the responsibility the government has in fighting the virus. A clear and structured governmental proceeding during the COVID-19 pandemic is important to maintain trust and adherence of the public in important safety measures.
A community of nodes clustering around psychopathology symptoms and pandemic fatigue has been identified. Specifically, the cluster consisted of generalized anxiety symptoms, depressive symptoms, sleep problems, and pandemic fatigue and there was a strong positive correlation between all those variables. The findings are in line with research by Labrague and Ballad (2021), in which pandemic fatigue was associated with similar symptoms such as sleep problems, increased fear, sadness, increased irritability, and worrying among college students. Overall, this cluster shows that psychopathological symptoms and pandemic fatigue are densely interconnected. Thus, it is suggested that these factors can foster each other during the current pandemic. In general, the results of the current study support the assumption of the WHO (2020b) that pandemic fatigue is negatively associated with mental health, as significant connections to psychopathological symptoms have been found.
Another community clustered around vaccination attitudes, trust in government related to pandemic measures, and subjective education related to COVID-19. Especially mistrust in the security of vaccinations was strongly related to trust in government related to pandemic measures and subjective level of information related to COVID-19. This suggests that personal knowledge about COVID-19 is associated with vaccination attitudes, especially trust in the security of vaccinations. The third community consisted of COVID-19 related cognitions like perceived limitations through the pandemic measures and constraints of getting vaccinated, and COVID-19 related behavior including safety behaviors and time invested in personal research about COVID-19. This indicates that COVID-19 related cognitions and behaviors are interrelated, which is in line with Taylor et al. (2020) who suggest that the cognitive-behavioral model can be adapted to the COVID-19 pandemic. This is further supported by the finding that adherent safety behavior was identified as one of the most influential factors, as it displayed many significant connections to COVID-19 related cognitions.
Overall, the results of the current study indicate a dense interconnectedness of various variables during the COVID-19 pandemic in 2021. Especially COVID-19 related fear, generalized anxiety, safety behavior, and trust in the government have been identified as influential factors. This indicates that COVID-19 and its associated anxiety still plays an important role in everyday life, which was also reflected by its many connections to related cognitions and behavior. Interestingly, vaccination attitudes are closely related to subjective knowledge about COVID-19 and trust in the government, but only weakly to COVID-19 related fear. This suggests that COVID-19 related fear does not seem to be a strong motivator for getting vaccinated, which might be also reflected by a relatively low vaccination ratio in Germany.
The current study paves the way to a better understanding of the role of pandemic fatigue and its associated factors during the COVID-19 pandemic. It has been shown that pandemic fatigue, depressive symptoms, generalized anxiety symptoms, and sleep problems were part of an interconnected cluster that possibly foster each other. As pandemic fatigue was strongly connected to psychopathology symptoms, it was identified as a risk factor for mental health during the COVID-19 pandemic as well. The strong interconnection of pandemic fatigue, depressive symptoms, generalized anxiety symptoms, and sleep problems indicates a high psychological burden for the general population during the COVID-19 pandemic. Also, pandemic fatigue showed many significant connections to COVID-19 related behavior and cognitions which supports the assumption of the WHO (2020b) that pandemic fatigue might influence pandemic-related behavior. In addition to that, the high interconnectedness of pandemic fatigue to psychopathology symptoms and COVID-19 related cognitions and behavior supports the adaptation of the cognitive-behavioral model to the COVID-19 pandemic. As a result, pandemic risk factors like pandemic fatigue should be captured and alleviated within the healthcare system, as they can negatively affect the general population in different aspects. Moreover, it highlights the need for interventions supporting mental health especially during later phases of the COVID-19 pandemic. Interventions adapted to the COVID-19 pandemic aim to reduce psychological distress, foster resilience, and improve general well-being (Bäuerle et al., 2021; Labrague, 2021).
This is the first study that investigated COVID-19 related cognitions, COVID-19 related behavior, psychopathology symptoms, pandemic risk factors such as pandemic fatigue and COVID-19 related fear, and vaccination attitudes in a network. The large set of different variables offers an extensive overview of the COVID-19 pandemic in a later phase of the pandemic in Germany with a large and representative sample. However, the study contains some limitations. First, there was gender imbalance in our sample, as the majority of participants that filled in the survey identified as female. Next, the design of the study was cross-sectional and exploratory. Even though network analysis displays significant connections between two nodes while controlling for other nodes in the network, it does not represent causal relationships. Moreover, due to the study design, there is a risk of selection bias. Therefore, further studies are needed to detect causality. Also, the network of the current study represents the pandemic situation in 2021 in Germany. However, the network structure might differ across countries and at different stages of the pandemic (Taylor et al., 2020). Hence, further research replicating the study in different countries and at a later point can give new insights into the network of pandemic variables.
5. Conclusion
Network analysis revealed a dense network with many interconnections between various variables. This highlights a complex interaction of different sets of factors during the COVID-19 pandemic. It has been shown that especially COVID-19 related fear, generalized anxiety, safety behavior, and trust in the government play a central role during the COVID-19 pandemic in 2021. Vaccination attitudes were strongly linked to subjective knowledge concerning COVID-19 and trust in the government but weakly to COVID-19 related fear. Pandemic fatigue was suggested to work as a risk factor for mental health, as it was strongly associated with psychopathology symptoms. The interconnectedness of various COVID-19 related cognitions and behavior support the adaption of the cognitive-behavioral model to the current pandemic.
Supplementary material
The associated supplementary material can be found in the online version.
Funding
None.
CRediT authorship contribution statement
Julia Barbara Krakowczyk: Visualization, Formal analysis, Writing – original draft, Writing – review & editing. Jari Planert: Visualization, Formal analysis, Writing – review & editing. Eva-Maria Skoda: Software, Writing – review & editing. Hannah Dinse: Software, Writing – review & editing. Theodor Kaup: Writing – review & editing. Martin Teufel: Software, Writing – review & editing. Alexander Bäuerle: Visualization, Software, Writing – review & editing.
Declaration of Competing Interest
All Authors declare that they have no competing interests.
Acknowledgements
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jadr.2022.100345.
Appendix. Supplementary materials
References
- Ashton J. COVID-19 and the anti-vaxxers. J. R. Soc. Med. 2021;114(1):42–43. doi: 10.1177/0141076820986065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäuerle A., Teufel M., Musche V., Weismüller B., Kohler H., Hetkamp M., Dörrie N., Schweda A., Skoda E. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health. 2020;42(4):672–678. doi: 10.1093/pubmed/fdaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäuerle A., Jahre L., Teufel M., Jansen C., Musche V., Schweda A., Fink M., Dinse H., Weismüller B., Dörrie N., Junne F., Graf J., Skoda E. Evaluation of the E-mental health mindfulness-based and skills-based “Cope it” intervention to reduce psychological distress in times of COVID-19: Results of a Bicentre longitudinal study. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.768132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain Behav. 2020;11(2) doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Petzold M.B., Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021;97 doi: 10.1016/j.intimp.2021.107724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betsch C., Schmid P., Heinemeier D.K., Korn L., Holtmann C., Böhm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13(12) doi: 10.31234/osf.io/ytb7w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgatti S.P. Centrality and network flow. Soc. Netw. 2005;27(1):55–71. doi: 10.1016/j.socnet.2004.11.008. [DOI] [Google Scholar]
- Borsboom D., Cramer A.O. Network analysis: an integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013;9(1):91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Borsboom D., Deserno M.K., Rhemtulla M., Epskamp S., Fried E.I., McNally R.J., Robinaugh D.J., Perugini M., Dalege J., Constantini G., Isvoranu A., Wysocki A.C., Van Borkulo C.D., Van Bork R., Waldorp L.J. Network analysis of multivariate data in psychological science. Nat. Rev. Methods Primers. 2021;1(1) doi: 10.1038/s43586-021-00060-z. [DOI] [Google Scholar]
- Brodeur A., Clark A.E., Fleche S., Powdthavee N. COVID-19, lockdowns and well-being: Evidence from Google trends. J. Public Econ. 2021;193 doi: 10.1016/j.jpubeco.2020.104346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullinger M. Erfassung Der Gesundheitsbezogenen Lebensqualität mit dem SF-36-Health Survey. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2000;43(3):190–197. doi: 10.1007/s001030050034. [DOI] [Google Scholar]
- Burki T.K. Omicron variant and booster COVID-19 vaccines. Lancet Respir. Med. 2022;10(2):e17. doi: 10.1016/s2213-2600(21)00559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castelli L., Di Tella M., Benfante A., Romeo A. The spread of COVID-19 in the Italian population: anxiety, depression, and post-traumatic stress symptoms. Can. J. Psychiatry. 2020;65(10):731–732. doi: 10.1177/0706743720938598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95(3):759–771. doi: 10.1093/biomet/asn034. [DOI] [Google Scholar]
- Constantin, M.A., Schuurman, N.K., Vermunt, J., 2021. “A general Monte Carlo method for sample size analysis in the context of network models.” PsyArXiv. September 24. doi:10.31234/osf.io/j5v7u. [DOI] [PubMed]
- Cramer A.O., Waldorp L.J., Van der Maas H.L., Borsboom D. Comorbidity: a network perspective. Behav. Brain Sci. 2010;33(2-3):137–150. doi: 10.1017/s0140525x09991567. [DOI] [PubMed] [Google Scholar]
- Creswell C., Shum A., Pearcey S., Skripkauskaite S., Patalay P., Waite P. Young people's mental health during the COVID-19 pandemic. Lancet Child Adolesc. Health. 2021;5(8):535–537. doi: 10.1016/s2352-4642(21)00177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csardi G., Nepusz T. The igraph software package for complex network research. Inter J. Complex Syst. 2006;1695 https://igraph.org [Google Scholar]
- Da Silva C.R., Aquino C.V., Oliveira L.V., Beserra E.P., Romero C.B. Trust in government and social isolation during the COVID-19 pandemic: Evidence from Brazil. Int. J. Public Adm. 2021;44(11-12):974–983. doi: 10.1080/01900692.2021.1920611. [DOI] [Google Scholar]
- Di Blasi M., Gullo S., Mancinelli E., Freda M.F., Esposito G., Gelo O.C., Lagetto G., Giordano C., Mazzeschi C., Pazzagli C., Salcuni S., Lo Coco G. Psychological distress associated with the COVID-19 lockdown: a two-wave network analysis. J. Affect. Disord. 2021;284:18–26. doi: 10.1016/j.jad.2021.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Cramer A.O., Waldorp L.J., Schmittmann V.D., Borsboom D. qgraph: network visualizations of relationships in psychometric data. J. Stat. Softw. 2012;48(4):1–18. doi: 10.18637/jss.v048.i04. [DOI] [Google Scholar]
- Fried E. R tutorial: How to identify communities of items in networks. Psych Netw. 2016 https://psych-networks.com/r-tutorial-identify-communities-items-networks/ accessed 2 October 2021. [Google Scholar]
- Friedman J., Hastie T., Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9(3):432–441. doi: 10.1093/biostatistics/kxm045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golino H.F., Epskamp S. Exploratory graph analysis: a new approach for estimating the number of dimensions in psychological research. PLoS One. 2017;12(6) doi: 10.1371/journal.pone.0174035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray N.S., O'Connor C., Knowles J., Pink J., Simkiss N.J., Williams S.D., Snowden R.J. The influence of the COVID-19 pandemic on mental well-being and psychological distress: Impact upon a single country. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.594115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeren A. On the distinction between fear and anxiety in a (post)pandemic world: a commentary on Schimmenti et al. (2020) Clin. Neuropsychiatry. 2020;17(3):189–191. doi: 10.36131/cnfioritieditore20200307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetkamp M., Schweda A., Bäuerle A., Weismüller B., Kohler H., Musche V., Dörrie N., Schöbel C., Teufel M., Skoda EM. Sleep disturbances, fear, and generalized anxiety during the COVID-19 shut down phase in Germany: Relation to infection rates, deaths, and German stock index DAX. Sleep Med. 2020;75:350–353. doi: 10.1016/j.sleep.2020.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hevey D. Network analysis: a brief overview and tutorial. Health Psychol. Behav. Med. 2018;6(1):301–328. doi: 10.1080/21642850.2018.1521283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson N.C., Newman M.G. Anxiety and depression as bidirectional risk factors for one another: a meta-analysis of longitudinal studies. Psychol. Bull. 2017;143(11):1155–1200. doi: 10.1037/bul0000111. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 2002;32(9):509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- Labrague L.J. Pandemic fatigue and clinical nurses’ mental health, sleep quality and job contentment during the covid-19 pandemic: the mediating role of resilience. J. Nurs. Manag. 2021;29(7):1992–2001. doi: 10.1111/jonm.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague L.J., Ballad C.A. Lockdown fatigue among college students during the COVID-19 pandemic: Predictive role of personal resilience, coping behaviors, and health. Perspect. Psychiatr. Care. 2021;57(4):1905–1912. doi: 10.1111/ppc.12765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Epskamp S., Isvoranu A., Chen C., Liu W., Hong X. Network analysis of physical and psychiatric symptoms of hospital discharged patients infected with COVID-19. J. Affect. Disord. 2021;294:707–713. doi: 10.1016/j.jad.2021.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Kroenke K., Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) J. Psychosom. Res. 2005;58(2):163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Moradian S., Bäuerle A., Schweda A., Musche V., Kohler H., Fink M., Weismüller B., Benecke A., Dörrie N., Skoda E., Teufel M. Differences and similarities between the impact of the first and the second COVID-19-lockdown on mental health and safety behaviour in Germany. J. Public Health. 2021 doi: 10.1093/pubmed/fdab037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgul E., Bener A., Atak M., Akyel S., Aktaş S., Bhugra D., Ventriglio A., Jordan T.R. COVID-19 pandemic and psychological fatigue in Turkey. Int. J. Soc. Psychiatry. 2020;67(2):128–135. doi: 10.1177/0020764020941889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öhman A. In: Handbook of Emotions. Feldmann Barret L., Lewis M., Haviland-Jones J.M., editors. The Guilford Press.; 2008. Fear and anxiety: Overlaps and dissociations; pp. 281–304. [Google Scholar]
- Opsahl T., Agneessens F., Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc. Netw. 2010;32(3):245–251. doi: 10.1016/j.socnet.2010.03.006. [DOI] [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Maricic L.M., Rogoll J., Betzler F., Große J., Ströhle A. Development of the COVID-19-Anxiety questionnaire and first psychometric testing. BJPsych Open. 2020;6(5) doi: 10.1192/bjo.2020.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2021. R: A Language and Environment for Statistical Computing.http://www.R-project.org/ URL. [Google Scholar]
- Robert Koch Institut . Robert Koch Institut; 2021. Digitales Impfquotenmonitoring zur COVID-19-Impfung. Coronavirus SARS-CoV-2.https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Impfquoten-Tab.html accessed 29 November 2021. [Google Scholar]
- RobertKoch Institut . Robert Koch Institut; 2021. Coronavirus SARS-Cov-2: Fallzahlen in Deutschland.https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Fallzahlen.html accessed 15 November 2021. [Google Scholar]
- Saramäki J., Kivelä M., Onnela J., Kaski K., Kertész J. Generalizations of the clustering coefficient to weighted complex networks. Phys. Rev. E. 2007;75(2) doi: 10.1103/physreve.75.027105. [DOI] [PubMed] [Google Scholar]
- Scholz S., Waize M., Treskova-Schwarzbach M., Haas L., Harder T., Karch A., Lange B., Kuhlmann A., Jäger V., Wichmann O. Einfluss von Impfungen und Kontaktreduktionen auf die dritte Welle der SARS-CoV-2-Pandemie und perspektivische Rückkehr zu prä-pandemischem Kontaktverhalten. Epidemiol. Bull. 2021;13:3–22. doi: 10.25646/8256. [DOI] [Google Scholar]
- Schweda A., Weismüller B., Bäuerle A., Dörrie N., Musche V., Fink M., Kohler H., Teufel M., Skoda E. Phenotyping mental health: Age, community size, and depression differently modulate COVID-19-related fear and generalized anxiety. Compr. Psychiatry. 2021;104 doi: 10.1016/j.comppsych.2020.152218. [DOI] [PubMed] [Google Scholar]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM Int. J. Med. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoda E., Spura A., De Bock F., Schweda A., Dörrie N., Fink M., Musche V., Weismüller B., Benecke A., Kohler H., Junne F., Graf J., Bäuerle A., Teufel M. Veränderung der psychischen belastung in der COVID-19-pandemie in deutschland: ängste, individuelles verhalten und die relevanz von information sowie vertrauen in behörden. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2021;64(3):322–333. doi: 10.1007/s00103-021-03278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S. Cambridge Scholars Publishing; 2019. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Rachor G.S., Asmundson G.J. Worry, avoidance, and coping during the COVID-19 pandemic: A comprehensive network analysis. J. Anxiety Disord. 2020;76 doi: 10.1016/j.janxdis.2020.102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umakanthan S., Lawrence S. Predictors of COVID-19 vaccine hesitancy in Germany: a cross-sectional, population-based study. Postgrad. Med. J. 2022 doi: 10.1136/postgradmedj-2021-141365. [DOI] [PubMed] [Google Scholar]
- Vahratian A., Blumberg S.J., Terlizzi E.P., Schiller J.S. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID- 19 pandemic — United States, August 2020–February 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70(13):490–494. doi: 10.15585/mmwr.mm7013e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weismüller B., Schweda A., Dörrie N., Musche V., Fink M., Kohler H., Skoda E., Teufel M., Bäuerle A. Different correlates of COVID-19-Related adherent and dysfunctional safety behavior. Front. Public Health. 2021;8 doi: 10.3389/fpubh.2020.625664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2020. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19-11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-COVID-19—11-march-2020 (accessed 15 October 2021. [Google Scholar]
- World Health Organization . World Health Organization; 2020. Pandemic fatigue: Reinvigorating the public to prevent COVID-19: Policy Considerations for Member States in the Who European Region.https://apps.who.int/iris/handle/10665/335820 accessed 15 October 2021. [Google Scholar]
- Williams N. The GAD-7 questionnaire [review of the test generalized anxiety disorder (gad-7) questionnaire, by R. L. Spitzer] Occup. Med. (Lond) 2014;64(3):224. doi: 10.1093/occmed/kqt161. [DOI] [Google Scholar]
- Wismans A., Thurik R., Baptista R., Dejardin M., Janssen F., Franken I. Correction: psychological characteristics and the mediating role of the 5C model in explaining students’ COVID-19 vaccination intention. PLoS One. 2021;16(11) doi: 10.1371/journal.pone.0259922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zavlis O., Butter S., Bennett K.M., Hartman T.K., Hyland P., Mason L., McBride O., Murphy J., Gibson Miller J., Levita L., Martinez A.P., Shevlin M., Stocks T.V., Vallières F., Bentall R. How does the COVID-19 pandemic impact on population mental health? A network analysis of COVID influences on depression, anxiety and traumatic stress in the UK population. Psychol. Med. 2021:1–9. doi: 10.31234/osf.io/8xtdr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W., China Novel Coronavirus Investigating and Research Team A novel Coronavirus from patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.