Abstract
Countries around the world have committed to achieving universal health coverage as part of the Sustainable Development Goals agreed on by all United Nations members, intended to be achieved by 2030. But important population groups such as older adults are rarely examined as part of Sustainable Development Goals’ monitoring and evaluation efforts. This study uses recent (2014/16) high-quality, individual-level data from several aging cohorts representing more than 100,000 adults ages fifty and older in twenty-three high- and middle-income countries. After controlling for individual characteristics and health needs, national rates varied up to tenfold for poor access (no doctor visit) and threefold for potential overuse (fifteen or more doctor visits and multiple hospitalizations) in the past year. Catastrophic expenditures (25 percent or more of household income spent on health care) averaged 9 percent, with the highest rates observed in middle-income countries and among sicker populations in some high-income countries. Strengthening universal health coverage for older adults will require greater tailoring and targeting of benefits to meet this population’s health needs while protecting them from catastrophic health expenditures.
Universal health coverage is an essential component of the health-related Sustainable Development Goals, a set of objectives all United Nations member countries agreed on in 2015 and intended to be achieved by 2030. Although many of the Sustainable Development Goals focus on improving the underlying social determinants of health, meeting the Sustainable Development Goals also requires that a set of preventive and curative measures be delivered through accessible, high-quality health care that is affordable for individuals. Previous studies have examined progress on universal health coverage using aggregate measures across social groups, but older individuals have an increased need for health care services and generally earn lower incomes than the rest of the adult population. To date, there has been less work published on universal health coverage within the context of older adults, especially in middle-income countries.
Previous cross-national documentation of health services use among older adults has come from two main sources. The first wave of the Study on Global Aging and Adult Health (2007–10) has been used to demonstrate that among several large emerging economies (China, Ghana, India, Mexico, Russia, and South Africa), health services use has generally been related to chronic health conditions, with considerable variation across countries as well as within them.1,2 The other main source of data is the Survey of Health, Aging and Retirement in Europe. The survey has pioneered comparisons across health systems to identify a range of important individual- and country-level factors associated with different levels of health care access, use, expenditures, and equity within and among more than a dozen European countries and Israel.3-5
Comparing the experiences of older adults across different health systems and among countries at different levels of socioeconomic development is especially important in terms of benchmarking current and future health care needs and identifying best practices, as well as estimating the extent to which middle-income countries will need to increase health care resources to meet the needs of their rapidly aging populations.
This article uses data from cohorts of older adults representing twenty-three high- and middle-income countries and seeks to assess levels and predictors of a set of health services access, use, and expenditure measures indicative of different aspects of universal health coverage. This article contributes to the literature by incorporating more recent data, comparing countries using a standard set of indicators tailored toward the needs of older adults, and assessing the extent to which health system–level factors facilitate universal health coverage among older adults in very different national contexts.
Study Data And Methods
Data And Participants
The countries included in this study were chosen because they are represented in ongoing studies of aging that share a similar overall framework and protocols based on those of the Health and Retirement Survey and include recent data on health services access, use, and expenditures.6,7 Data were obtained from nationally representative surveys of people ages fifty and older and include the 2015 wave of the Brazilian Longitudinal Study of Aging8; the 2015 wave of the Mexican Health and Aging Study9; the 2016 wave of the Korean Longitudinal Study of Aging10; the 2014/15 wave of the Survey of Health and Aging and Retirement in Europe, which includes Austria, Belgium, Croatia, the Czech Republic, Denmark, Estonia, France, Germany, Greece, Israel, Luxembourg, Italy, Poland, Portugal, Slovenia, Spain, Sweden, and Switzerland11; the 2015 wave of the Chinese Health and Retirement Longitudinal Study12; and the 2016 wave of the U.S. Health and Retirement Study.7
The final pooled sample consists of 110,000 eligible adult respondents.
Measures
We developed four indicators to assess different aspects of universal health coverage.
The first indicator, no doctor visit in the past twelve months, reflects a lack of access to basic health care. Clinical guidelines in most countries recommend an annual doctor visit, especially for older individuals, to assess vital signs, monitor medication use, and ensure individuals are up-to-date with routine preventive care.13,14
Although people with more complex health conditions generally experience greater numbers of health care visits, overuse can reflect poor coordination of care, poor quality, or both.15 The second indicator, fifteen or more doctor visits in the past year, is intended to represent potential overuse, especially when reported by individuals who do not have multiple complex health needs. The threshold of fifteen visits represents the top tenth percentile of the overall distribution of doctor visits in the pooled data set.
The third indicator, two or more hospitalizations in the past year, is intended to reflect tertiary care quality by assessing hospital readmissions.16 Even though some individuals may be hospitalized more than once for completely different health problems, this indicator should capture all hospital readmissions within the recall period.
The final indicator, catastrophic health care expenditures, is a measure of whether household out-of-pocket expenditures on health care reach or exceed a threshold of 25 percent or more of the household’s income, the current definition used in defining catastrophic health care spending for monitoring Sustainable Development Goals.17,18 Lower thresholds (such as 10 percent) sometimes used to define catastrophic health care expenditures may be overly sensitive to the fact that older individuals generally have lower incomes.
We collected country-level data on several components of health systems: whether levels of nurse and doctor staffing were within recommended levels (World Health Organization, Organization for Economic Cooperation and Development); hospital beds per capita, providing a measure of tertiary care availability; per capita health expenditures (expressed in purchasing power parity–adjusted US dollars), which reflects the overall amount of resources devoted toward health; and a measure of health system performance, the Institute for Health Metrics and Evaluation Healthcare Access and Quality Index, which is calculated using data on mortality from conditions that should be amenable to health care.19
Individual control variables include demographics (age, sex, marital status), socioeconomic status (harmonized educational level, household income quintile, private health insurance, rural residence), risk factors (current or ever smoker), and health status (limitations in basic activities of daily living, number of chronic conditions, self-rated health, and obesity based on a measured body mass index of ≥30 kg/m2). Because health status variables were highly correlated, we created a health problem severity scale from principal component analysis, which was then divided into tertiles representing individuals with no/few health problems (tertile 1), some health problems (tertile 2), and many health problems (tertile 3). See the online appendix for details.20
Data were analyzed using survey-weighted robust Poisson regression with standard errors adjusted for country-level clustering. Multilevel models were not used, given the small number of countries included and the complexity of the survey weighting.21,22 To visualize differences among countries, we calculated and plotted predicted probabilities of each outcome after a survey-weighted robust Poisson regression with country fixed effects. All models incorporate each survey’s weights.
Limitations
Whereas the use of high-quality standardized cohort surveys was a major strength of this study, missing data resulted in about 18 percent of the 133,000 potential respondents being dropped from the analysis. There was no single country or category accounting for the majority of missing data, but incomplete data for household income and some health status indicators were the most common. We, therefore, cannot rule out the possibility that those who did not respond may have been sicker or poorer, and thus our results may be underestimated.
Most of the study data (except for some health status indicators such as body mass index) are based on self-report, so we cannot rule out recall bias. A strength of using the Health and Retirement Survey family of studies is that, in addition to imputing some missing data, all countries (except for Brazil) have several previous waves of data collection available, so researchers are able to examine and verify responses that diverge from previous years or that another household member may dispute.
The studies included here share many similarities, but a few important variables differed in terms of recall period or response categories. The appendix provides a detailed explanation of major differences and the strategies undertaken to harmonize indicators across studies.20
Finally, we assess only one wave of each study, so in this cross-sectional analysis, any observed associations cannot be considered causal. This is particularly relevant to health system variables, which should be interpreted with caution.
Study Results
Exhibit 1 shows unadjusted outcomes by country. Overall, about 11 percent of respondents reported having no doctor visit in the previous year. But this figure varied considerably, with two countries (Luxembourg and the Czech Republic) reporting rates of less than 5 percent and two countries (Mexico and Greece) reporting approximately 23 percent of adults without a doctor visit in the past year. About 8.6 percent of the entire sample reported fifteen or more doctor visits in the past year, ranging from a low of less than 5 percent in Mexico and Brazil to a high of nearly 16 percent in Italy. Although China appears to be an outlier for both these indicators, the recall period for Chinese participants was only the past thirty days. Regarding hospitalizations, about 6 percent of the sample reported two or more hospitalizations in the previous year. The lowest rate (less than 2 percent) was observed in South Korea, whereas the highest rate (more than 9 percent) was observed in Mexico and the US. About 9 percent of respondents reported spending 25 percent or more of their household income on health care—the definition of having a catastrophic health care expenditure. This measure varied from less than 1 percent in France, Denmark, Germany, and Sweden to more than 10 percent of the population in Brazil, South Korea, China, and Mexico. The appendix exhibits present additional background information on each country and its health system, as well as weighted means and proportions for individual-level characteristics.20
Exhibit 1:
Health care use and expenditure indicators (unadjusted), adults ages fifty and older, by country
| Country | N | No doctor visit (%) |
Fifteen or more doctor visits (%) |
Two or more hospital visits (%) |
Catastrophic health care expenditures (%)a |
|---|---|---|---|---|---|
| Austria | 3,358 | 10.18 | 12.68 | 7.67 | 1.84 |
| Belgium | 5,700 | 5.97 | 13.32 | 5.92 | 1.63 |
| Brazil | 9,412 | 16.79 | 2.55 | 3.28 | 10.02 |
| China | 16,583 | 80.94 | 0.13 | 5.78 | 15.84 |
| Croatia | 2,444 | 17.37 | 12.38 | 4.96 | 2.44 |
| Czech Rep. | 4,793 | 4.98 | 11.68 | 5.60 | 1.79 |
| Denmark | 3,661 | 13.02 | 6.85 | 4.25 | 0.87 |
| Estonia | 5,557 | 14.3 | 7.52 | 5.42 | 4.18 |
| France | 3,870 | 6.91 | 5.31 | 5.46 | 0.44 |
| Germany | 4,347 | 6.2 | 13.31 | 6.52 | 0.91 |
| Greece | 4,816 | 23.99 | 5.67 | 3.92 | 4.9 |
| Israel | 2,013 | 9.02 | 7.6 | 5.87 | 2.7 |
| Italy | 5,214 | 12.94 | 15.77 | 4.13 | 4.66 |
| Luxembourg | 1,543 | 4.48 | 13.68 | 6.48 | 1.27 |
| Mexico | 14,203 | 22.39 | 4.66 | 9.22 | 22.1 |
| Poland | 1,802 | 14.73 | 10.41 | 6.58 | 4.61 |
| Portugal | 1,662 | 6.04 | 6.1 | 4.23 | 7.93 |
| Slovenia | 4,186 | 14.25 | 6.97 | 5.97 | 1.35 |
| South Korea | 7,490 | 15.34 | 13.78 | 1.78 | 13.23 |
| Spain | 5,560 | 10.29 | 7.42 | 3.91 | 2.08 |
| Sweden | 3,881 | 16.54 | 6.26 | 4.68 | 0.94 |
| Switzerland | 2,772 | 13.44 | 6.65 | 5.23 | 1.71 |
| United States | 18,363 | 8.46 | 5.3 | 9.34 | 3.21 |
| Meanb | 10.73c | 8.58c | 6.13 | 9.32 |
SOURCE Authors’ analysis. NOTES Recall period is the past 12 months for all countries except for the United States and South Korea (recall period is 2 years or last interview, so numbers have been divided by two) and China (recall period is thirty days).
Defined as out-of-pocket expenditures on health services that were more than 25 percent of the total household income.
Weighted average.
China was not included in the mean calculation because of its different recall period.
Exhibit 2 presents regression results on each outcome. Factors associated with a higher chance of reporting no doctor visit in the previous twelve months include male sex, being in the lowest income quintile, and being a current or former smoker. Older age, a greater number of health problems, private health insurance, and an adequate supply of physicians working in the country were all negatively associated with having no doctor visits. The second indicator, fifteen or more doctor visits in the past year, was more frequently reported among those with a greater number of health problems, current and former smokers, and those living in countries with an adequate supply of physicians and a greater number of hospital beds. Being male, living in a country with an adequate supply of nurses, and overall health expenditures per capita were negatively associated with fifteen or more doctor visits. Reporting two or more hospitalizations in the past twelve months was positively associated with older age, being in the lowest income quintile, having a greater number of health problems, and being a current or former smoker, as well as greater health expenditures per capita. Catastrophic health expenditures were more prevalent among rural inhabitants, those in the lowest income quintile, people with a greater number of health problems, and current/former smokers. Protective factors include being male, having an adequate supply of nurses and physicians in one’s country, and a higher Healthcare Access and Quality Index. The appendix presents additional details including 95% confidence intervals.20
Exhibit 2:
Individual- and country-level predictors of health services use and expenditures among older adults
| No doctor visita |
Fifteen or more doctor visitsa |
Two or more hospital visits |
Catastrophic health care expendituresb |
|
|---|---|---|---|---|
| Individual level | ||||
| Age (years) | ||||
| 60–69 (versus 50–59) | 0.8*** | 0.91 | 1.14 | 1.16 |
| 70–79 | 0.66**** | 0.96 | 1.2**** | 1.11 |
| 80+ | 0.64**** | 1.01 | 1.46**** | 1.07 |
| Male | 1.56**** | 0.84**** | 1.11 | 0.86**** |
| Married or partnered | 0.86**** | 0.99 | 0.94 | 0.92 |
| Lowest education | 1.32 | 0.99 | 0.89** | 1.05 |
| Rural (versus urban) | 1.05 | 0.95 | 0.99 | 1.35*** |
| Lowest income quintile | 1.53**** | 0.89 | 1.12** | 2.44**** |
| Some health problems (versus none/few)c | 0.45**** | 3.44**** | 3.61**** | 1.67**** |
| Many health problems | 0.26**** | 8.77**** | 10.42**** | 2.84**** |
| Private health insurance | 0.66**** | 0.96 | 0.95 | 0.93 |
| Current/former smoker | 1.08** | 1.12*** | 1.18** | 1.1**** |
| Country level | ||||
| Adequate (>3.2) physicians/1,000 | 0.53**** | 1.42** | 0.54 | 0.29**** |
| Adequate (>9.1) nurses/1,000 | 0.91 | 0.7** | 1.37 | 0.37*** |
| Healthcare Access and Quality Index | 1.00 | 1.07**** | 0.99 | 0.95*** |
| Health expenditures per capita ($1,000s) | 0.98 | 0.93**** | 1.1*** | 0.95 |
| Hospital beds per 1,000 population | 0.97 | 1.09*** | 0.94 | 0.96 |
SOURCE Authors’ analysis. NOTES Results are prevalence ratios from survey-weighted Poisson regression with country cluster robust standard errors. Low education is less than secondary education, low income is the lowest income quintile (by country), ever smoke is current or ever smoking, rural is rural residence, and private insurance is any private (supplemental) health insurance.
Because of its different recall period for doctor visits, China is not included in these analyses.
Defined as out-of-pocket expenditures on health services that were more than 25 percent of total household income.
Health problems are tertiles of the principle component from principal component analysis of poor/very poor self-rated health, any reported chronic condition, any basic activity of daily living limitation, and a measured body mass index of 30 kg/m2 or more.
p < 0.05
p < 0.01
p < 0.001
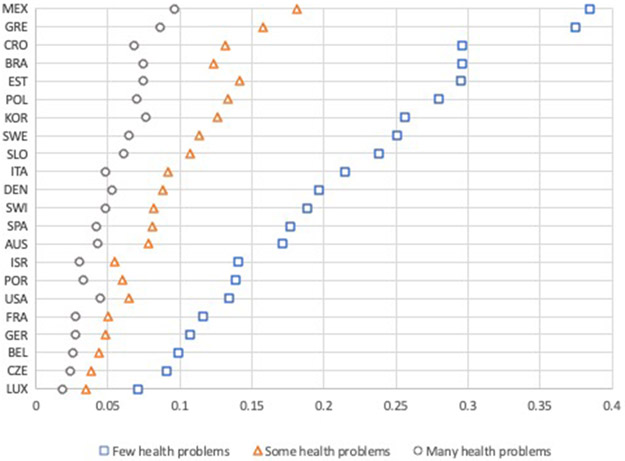
Exhibit 3 displays the predicted probability of having had no doctor visit in the previous twelve months for each country and each category of health problems, controlling for all individual-level factors listed in Exhibit 2. In every country, sicker adults were less likely to have had no doctor visits than those with no or only a few health problems. However, in Mexico and Greece, nearly 10 percent of those with many health problems reported no doctor visits, whereas in Luxembourg, this figure was closer to 2 percent. There is also considerable country-to-country variation among individuals reporting no or only a few health problems. In Luxembourg and the Czech Republic, less than 10 percent of healthier adults reported no doctor visit, whereas in Mexico and Greece, the corresponding figure was approximately 38 percent. Values of predicted probabilities for all outcomes are provided in the appendix.20
Exhibit 3: Predicted probability of no doctor visit, by country and level of health needs.
Source/Note: SOURCE Authors’ analysis. NOTE From robust Poisson regression controlling for covariates in exhibit 2 and country fixed effects. China was not included because it had a different recall period.
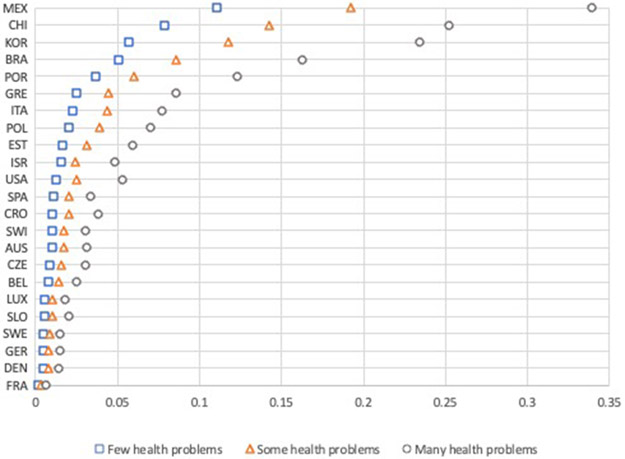
Exhibit 4 shows the predicted probability of having spent 25 percent or more of one’s household income on out-of-pocket medical expenditures, controlling for individual-level sociodemographic factors. In general, sicker adults tended to have a higher probability of such catastrophic expenditures. However, in Germany, Sweden, France, Denmark, and Slovenia, catastrophic expenditures were near zero, with no significant difference between healthy and sicker adults. In contrast, Italy, Greece, Portugal, Brazil, South Korea, Mexico, and China all demonstrate a clear gradient whereby those with greater health problems are more likely to experience potentially catastrophic health expenditures.
Exhibit 4: Predicted probability of catastrophic expenditures (>25 percent of household income on out-of-pocket medical expenses), by country and level of health needs.
Source/Note: SOURCE Authors’ analysis. NOTE From robust Poisson regression controlling for covariates in exhibit 2 and country fixed effects.
Discussion
Using nationally representative surveys containing data on more than 100,000 older adults in twenty-three high- and middle-income countries, we find large variations across countries and social groups on health care access, use, and expenditures. After controlling for individual sociodemographics, income, and a comprehensive measure of health needs, national rates varied up to tenfold for our indicator of access barriers (no doctor visit) and threefold for our indicator of potential health care overuse (fifteen or more doctor visits). Multiple hospitalizations, although having a lower prevalence overall, similarly varied threefold among countries with the highest rates observed in both a rich country (US) and a middle-income country (Mexico). Catastrophic expenditures were surprisingly prevalent, with a 10 percent or greater prevalence rate in the middle-income countries (Brazil, China, Mexico), as well as among sicker populations in some wealthier countries (South Korea, Portugal, Greece).
A few individual-level factors (age, relationship status, education, and low income) help explain why some individuals may experience the outcomes assessed here, with the magnitude and severity of an individual’s health problems associated with all outcomes. Some gender differences also existed, where men were more likely to have no doctor visit and were significantly less likely to visit more than fifteen doctors or to have catastrophic health expenditures. Interestingly, having private health insurance was only associated with the measure of access barriers (no doctor visit).
Once individual-level factors are controlled for, differences in health systems, whether they result from better healthcare access and quality or the supply of health professionals, have an important impact on health care use and expenditures for older adults in the twenty-three countries studied here.23,24 All else being equal, a higher Healthcare Access and Quality Index was associated with the increased use of doctors and lower catastrophic expenditures. National health care expenditures were negatively associated with the potential overuse of doctors but reflected greater use of hospitals. This relationship is likely a result of the higher costs of inpatient, relative to outpatient, care in most countries. Having adequate numbers of health professionals was generally protective for general access to doctors, as well as catastrophic expenditures. In other words, having an adequate supply of doctors increased patient access to them and likely reduced the need to seek services in urgent care or hospital emergency departments, both of which are likely to result in larger out-of-pocket expenditures, compared with expenditures related to doctor office visits.
To our knowledge, this is the largest study investigating cross-national differences in health care access, use, and related health expenditures among older adults, and one of only a handful that investigated health system factors. Previous studies have used the Survey of Health, Aging and Retirement in Europe cohort to explore differences in health care use and out-of-pocket expenditures,25,26 but we expand on these studies by incorporating additional high-income countries such as the US and South Korea, as well as upper middle-income countries such as Brazil, China, and Mexico.
Some of our findings are similar to those of previous studies. For instance, we show that additional health problems, such as morbidity and disability, are associated with higher rates of health care use and higher costs.27-30 Similar to a previous study using the Survey of Health, Aging and Retirement in Europe, we found that low education level is associated with fewer doctor visits, but no association is found with multiple hospitalizations.4 The study also confirms that older adults in the US who are sicker tend to be hospitalized more often than adults in other high-income countries.31 But we also found that even though medical costs in the US are high, catastrophic expenses were relatively low, perhaps as a result of higher average income levels and the fact that in the US, individuals ages sixty-five and older have access to a national health insurance program (Medicare) and additional coverage options are available to help defray costs through Medigap, employer-sponsored insurance, or Medicaid.
For the middle-income countries in our sample, the literature has focused primarily on assessing the impact of expansions on health insurance or government-financed health services on access and use for the general population, as well as older adults with chronic conditions. Studies using Chinese Health and Retirement Longitudinal Study pilot data have found increased access to and use of health services in China as a result of that country’s 2009 health reforms.32 A 2013 study using the second wave of the Chinese Health and Retirement Longitudinal Study found rates of doctor visits (21.4 percent) and hospitalizations (12.1 percent) that were largely in line with those we identified here using data from the 2015 wave.33 Health services–related studies using the Mexican Health and Aging Study have focused on the impact of Mexico’s different health insurance programs, finding that their expansion over time successfully increased access to preventive services34 and the diagnosis and treatment of common chronic conditions.35 Studies using the Brazilian Longitudinal Study of Aging have focused on barriers and facilitators to access and use of primary care36 and hospitalizations37 and demonstrated the important roles of chronic conditions, geographic variation, and different forms of health care coverage.
Policy Implications
Access Problems Persist For Many Older Adults
In the highest-performing health systems such as those of the richer countries of Western Europe, older individuals almost all consulted a doctor in the past year, use of hospitals depended primarily on the health needs of the individual (not socioeconomic factors), and regardless of the level of health problems, patients were unlikely to have catastrophic out-of-pocket health expenditures. However, access to care remains a problem for 11 percent of all adults examined here, and in six countries, this figure reached or exceeded 15 percent. There are numerous ways to enhance access, including telemedicine for remote consultation and triage,38 community health workers for home care and control of some chronic disease risks,39 and innovative ways to reorganize care to guarantee access after hours and on weekends without relying on urgent care or hospital emergency departments.40 All these approaches may also strengthen the primary care basis of health systems, which should further enhance access, improve care coordination and integration for chronic conditions, and contain health care expenditure growth.41,42
High Out-Of-Pocket Health Care Expenditures Remain A Major Problem For Many Older Adults
Although ensuring access to care is essential, exposing older, sicker adults to high out-of-pocket health care costs can be inefficient and inequitable. This suggests a need to identify better ways to target social protections. In middle-income countries such as Mexico and China, new insurance schemes have facilitated access to needed health care, but have so far been less effective in protecting sicker older adults from high health care costs.43,44 Other approaches, such as maintaining access during financial crises by shifting some costs to consumers (as has been done in Italy, Greece, and Portugal) appear to have resulted in a higher-than-expected incidence of catastrophic expenditures for older, primarily sicker adults.25 There is a need to improve many health systems’ ability to identify those most in need and to better target social protections to them.45
Many Countries Will Likely Need To Spend More On Health Care
Some countries (such as Spain), although experiencing increased rates of multimorbidity among older adults, still managed to achieve relatively high levels of access and low levels of out-of-pocket spending with fairly low overall health budgets.26 Although health care spending is not the best indicator of overall health system performance, just to meet the moderate expenditure levels observed in Spain, Brazil and Mexico would need to more than double and China would need to more than triple their current levels of health care spending. Given current aging trends in these middle-income countries, there will be considerable need for greater investments in health and social care.46 Even among richer countries with universal health coverage, health-related problems result in considerable out-of-pocket expenditures for older citizens, particularly those with multiple health problems, suggesting the need to enhance financial protections afforded to these vulnerable populations.
Data Systems Need Further Strengthening
The results suggest there is considerable potential for aging cohorts to be used in identifying health care problems affecting older adults and in assessing the impact of health system reforms. None of the indicators used here can be constructed using aggregate data alone. Some studies (such as the Health and Retirement Survey) have linked survey data to medical claims, enhancing their ability to capture the type and timing of health services use. However, aside from the Survey of Health, Aging and Retirement in Europe and the Brazilian Longitudinal Study of Aging, most cohort studies of aging include only a few health services variables, and they vary in how essential measures (such as what counts as a hospitalization), recall periods, and expenditure categories are defined. In addition, some indicators could be improved to better inform health system assessments. Among the studies included here, only the Survey of Health, Aging and Retirement in Europe and the Brazilian Longitudinal Study of Aging differentiate between primary care and specialist doctor visits. This absence limits the ability of these studies to inform strategies to ensure primary care is adequately serving older adults or to aid in future human resources planning. Few studies (except the Mexican Health and Aging Study) include subjective measures of financial and organizational barriers to accessing health care, which means that patient experiences of financial distress may be overlooked. Finally, surveys could provide greater detail on the reasons for high-cost events such as hospital admissions and readmission to assess whether such events were the result of conditions that could have been managed at the primary care level or the result of poor hospital follow-up care.47
Conclusion
There is a need for better evidence on the gaps that must be overcome as countries move toward establishing health care financing and provide strategies that guarantee universal health coverage for their populations. Older populations in many countries have been largely absent from discussions on universal health coverage strategies. However, they represent an important and vulnerable segment of the population, whose exclusion from assessments of universal health coverage attainment will likely have significant health and equity implications.
Supplementary Material
Acknowledgment
The National Institute on Aging at the National Institutes of Health (R01 AG030153, RC2 AG036619, R03 AG043052) funded the Harmonized versions of the Survey of Health Aging and Retirement in Europe (SHARE), the Korean Longitudinal Study of Aging (KLoSA), the Health and Retirement Survey (HRS), and Chinese Health and Retirement Longitudinal Study (CHARLS) data used in this analysis. The Mexican Health and Aging Study (MHAS) receives support from the National Institute on Aging (R01 AG018016). The Brazilian Longitudinal Study of Aging (ELSI) was funded by the Brazilian Ministry of Health (grants 20836, 22566, 23700, and 404965/2012-1). This analysis uses data or information from the Harmonized SHARE data set and codebook (version D.5 as of April 2019), the Harmonized CHARLS data set and codebook (version C as of April 2018) and the Harmonized KLoSA and codebook (version C as of June 2019) developed by the Gateway to Global Aging data. HRS data come from the RAND Center for the Study of Aging, who—with funding and support from the National Institute on Aging and the Social Security Administration—created the RAND HRS data products. This analysis also uses Stata code from the Harmonized HRS data set and codebook, version A, as of February 2018, and the Harmonized MHAS programming codes and codebook, version A. All were developed by the Gateway to Global Aging Data. For more information, please refer to https://g2aging.org/. ELSI information and programming codes were developed by the ELSI research team. The data set and documentation are public use and available at http://elsi.cpqrr.fiocruz.br/. Maria Fernanda Lima-Costa is a fellow of the Brazilian National Research Council (Conselho National de Pesquisa- CNPq).
BIOS for 2019-01570_Macinko:
Bio1: James Macinko (jmacinko@ucla.edu) is a professor in the Fielding School of Public Health at the University of California, Los Angeles.
Bio2: Flavia Cristina Drumond Andrade is an associate professor in the School of Social Work at the University of Illinois at Urbana-Champaign.
Bio3: Fabiola Bof de Andrade is an assistant professor in the Rene Rachou Research Institute at the Fundação Oswaldo Cruz, in Belo Horizonte, Minas Gerais, Brazil.
Bio4: Maria Fernanda Lima-Costa is a professor in the Rene Rachou Research Institute and the Public Health Postgraduate Program at the Federal University of Minas Gerais, in Belo Horizonte, Brazil.
Contributor Information
James Macinko, Fielding School of Public Health at the University of California, Los Angeles..
Flavia Cristina Drumond Andrade, School of Social Work at the University of Illinois at Urbana-Champaign..
Fabiola Bof de Andrade, Rene Rachou Research Institute at the Fundação Oswaldo Cruz, in Belo Horizonte, Minas Gerais, Brazil..
Maria Fernanda Lima-Costa, Public Health Postgraduate Program at the Federal University of Minas Gerais, in Belo Horizonte, Brazil..
Notes
- 1.Lee JT, Hamid F, Pati S, Atun R, Millett C. Impact of noncommunicable disease multimorbidity on healthcare utilisation and out-of-pocket expenditures in middle-income countries: cross sectional analysis. PLoS One. 2015;10(7):e0127199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peltzer K, Williams JS, Kowal P, Negin J, Snodgrass JJ, Yawson A, et al. , SAGE Collaboration. Universal health coverage in emerging economies: findings on health care utilization by older adults in China, Ghana, India, Mexico, the Russian Federation, and South Africa. Glob Health Action. 2014;7:25314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ilinca S, Calciolari S. The patterns of health care utilization by elderly Europeans: frailty and its implications for health systems. Health Serv Res. 2015;50(1):305–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terraneo M Inequities in health care utilization by people aged 50+: evidence from 12 European countries. Soc Sci Med. 2015;126:154–63 [DOI] [PubMed] [Google Scholar]
- 5.Orlovic M, Marti J, Mossialos E. Analysis of end-of-life care, out-of-pocket spending, and place of death in 16 European countries And Israel. Health Aff (Millwood). 2017;36(7):1201–10 [DOI] [PubMed] [Google Scholar]
- 6.Juster FT, Suzman R. An overview of the Health and Retirement Study. J Hum Resour. 1995;30(Suppl):S7–56. [Google Scholar]
- 7.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014;43(2):576–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lima-Costa MF, de Andrade FB, de Souza PRB Jr, Neri AL, Duarte YAO, Castro-Costa E, et al. The Brazilian Longitudinal Study of Aging (ELSI-Brazil): objectives and design. Am J Epidemiol. 2018;187(7):1345–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong R, Michaels-Obregon A, Palloni A. Cohort profile: the Mexican Health and Aging Study (MHAS). Int J Epidemiol. 2017;46(2):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jang SN. Korean Longitudinal Study of Ageing (KLoSA): overview of research design and contents. In: Pachana N, editor. Encyclopedia of geropsychology. Singapore: Springer; 2016. p. 1–9. [Google Scholar]
- 11.Börsch-Supan A, Brandt M, Hunkler C, Kneip T, Korbmacher J, Malter F, et al. , SHARE Central Coordination Team. Data resource profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol. 2013;42(4):992–1001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gorbenko K, Metcalf SA, Mazumdar M, Crump C. Annual physical examinations and wellness visits: translating guidelines into practice. Am J Prev Med. 2017;52(6):813–6 [DOI] [PubMed] [Google Scholar]
- 14.Misra A, Lloyd JT. Hospital utilization and expenditures among a nationally representative sample of Medicare fee-for-service beneficiaries 2 years after receipt of an Annual Wellness Visit. Prev Med. 2019;129:105850. [DOI] [PubMed] [Google Scholar]
- 15.Coon ER, Quinonez RA, Morgan DJ, Dhruva SS, Ho T, Money N, et al. 2018 update on pediatric medical overuse: a review. JAMA Pediatr. 2019;173(4):379–84 [DOI] [PubMed] [Google Scholar]
- 16.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365(24):2287–95 [DOI] [PubMed] [Google Scholar]
- 17.Wagstaff A, Flores G, Hsu J, Smitz MF, Chepynoga K, Buisman LR, et al. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Glob Health. 2018;6(2):e169–79 [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization, World Bank. Global monitoring report on financial protection in health 2019 [Internet]. Geneva: WHO; 2019. [cited 2020 Sep 4]. Available from: https://www.who.int/healthinfo/universal_health_coverage/report/fp_gmr_2019.pdf?ua=1 [Google Scholar]
- 19.GBD 2015 Healthcare Access and Quality Collaborators. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet. 2017;390(10091):231–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.To access the appendix, click on the Details tab of the article online.
- 21.Bryan ML, Jenkins SP. Multilevel modelling of country effects: a cautionary tale. Eur Sociol Rev. 2015;32(1):3–22. [Google Scholar]
- 22.Maas CJM, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodology (Gott). 2005;1(3):86–92. [Google Scholar]
- 23.Tchouaket EN, Lamarche PA, Goulet L, Contandriopoulos AP. Health care system performance of 27 OECD countries. Int J Health Plann Manage. 2012;27(2):104–29 [DOI] [PubMed] [Google Scholar]
- 24.Schoen C, Osborn R, Huynh PT, Doty M, Davis K, Zapert K, et al. Primary care and health system performance: adults' experiences in five countries. Health Aff (Millwood). 2004;(Suppl Web Exclusives):W4-487–503 [DOI] [PubMed] [Google Scholar]
- 25.Palladino R, Lee JT, Hone T, Filippidis FT, Millett C. The Great Recession and increased cost sharing in European health systems. Health Aff (Millwood). 2016;35(7):1204–13 [DOI] [PubMed] [Google Scholar]
- 26.Palladino R, Pennino F, Finbarr M, Millett C, Triassi M. Multimorbidity and health outcomes in older adults in ten European health systems, 2006–15. Health Aff (Millwood). 2019;38(4):613–23 [DOI] [PubMed] [Google Scholar]
- 27.Bähler C, Huber CA, Brüngger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015;15:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brinda EM, Kowal P, Attermann J, Enemark U. Health service use, out-of-pocket payments and catastrophic health expenditure among older people in India: the WHO Study on global AGEing and adult health (SAGE). J Epidemiol Community Health. 2015;69(5):489–94. [DOI] [PubMed] [Google Scholar]
- 29.Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, Luppa M, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420 [DOI] [PubMed] [Google Scholar]
- 30.Sambamoorthi U, Tan X, Deb A. Multiple chronic conditions and healthcare costs among adults. Expert Rev Pharmacoecon Outcomes Res. 2015;15(5):823–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Osborn R, Doty MM, Moulds D, Sarnak DO, Shah A. Older Americans were sicker and faced more financial barriers to health care than counterparts in other countries. Health Aff (Millwood). 2017;36(12):2123–32 [DOI] [PubMed] [Google Scholar]
- 32.Li J, Shi L, Liang H, Ma C, Xu L, Qin W. Health care utilization and affordability among older people following China's 2009 health reform—evidence from CHARLS pilot study. Int J Equity Health. 2019;18(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gong CH, Kendig H, He X. Factors predicting health services use among older people in China: an analysis of the China Health and Retirement Longitudinal Study 2013. BMC Health Serv Res. 2016;16:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pagán JA, Puig A, Soldo BJ. Health insurance coverage and the use of preventive services by Mexican adults. Health Econ. 2007;16(12):1359–69. [DOI] [PubMed] [Google Scholar]
- 35.Beltrán-Sánchez H, Drumond-Andrade FC, Riosmena F. Contribution of socioeconomic factors and health care access to the awareness and treatment of diabetes and hypertension among older Mexican adults. Salud Publica Mex. 2015;57(Suppl 1):S6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Macinko J, de Andrade FB, de Souza PRB, Lima-Costa MF. Primary care and healthcare utilization among older Brazilians (ELSI-Brazil). Rev Saude Publica. 2018;52(Suppl 2):6s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Melo-Silva AM, Mambrini JVD, de Souza PRB, de Andrade FB, Lima-Costa MF. Hospitalizations among older adults: results from ELSI-Brazil. Rev Saude Publica. 2018;52(Suppl 2):3s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Batsis JA, DiMilia PR, Seo LM, Fortuna KL, Kennedy MA, Blunt HB, et al. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc. 2019;67(8):1737–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacob V, Chattopadhyay SK, Hopkins DP, Reynolds JA, Xiong KZ, Jones CD, et al. Economics of community health workers for chronic disease: findings from community guide systematic reviews. Am J Prev Med. 2019;56(3):e95–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Weel C, Knottnerus JA, van Schayck OCP. Managing costs and access to healthcare in the Netherlands: impact on primary care. BMJ. 2020;369:m1181. [DOI] [PubMed] [Google Scholar]
- 41.Hansen J, Groenewegen PP, Boerma WG, Kringos DS. Living in a country with a strong primary care system is beneficial to people with chronic conditions. Health Aff (Millwood). 2015;34(9):1531–7. [DOI] [PubMed] [Google Scholar]
- 42.Kringos DS, Boerma W, van der Zee J, Groenewegen P. Europe's strong primary care systems are linked to better population health but also to higher health spending. Health Aff (Millwood). 2013;32(4):686–94. [DOI] [PubMed] [Google Scholar]
- 43.Doubova SV, Pérez-Cuevas R, Canning D, Reich MR. Access to healthcare and financial risk protection for older adults in Mexico: secondary data analysis of a national survey. BMJ Open. 2015;5(7):e007877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhao S-W, Zhang X-Y, Dai W, Ding Y-X, Chen J-Y, Fang P-Q. Effect of the catastrophic medical insurance on household catastrophic health expenditure: evidence from China. Gac Sanit. 2020;34(4):370–6. [DOI] [PubMed] [Google Scholar]
- 45.Kong T, Yang P. Finding the vulnerable among China's elderly: identifying measures for effective policy targeting. J Aging Soc Policy. 2019;31(3):271–90. [DOI] [PubMed] [Google Scholar]
- 46.Glassman A, Zoloa JI. How much will health coverage cost? future health spending scenarios in Brazil, Chile, and Mexico [Internet]. Washington (DC): Center for Global Development; 2014. Oct [cited 2020 Sep 4]. (Working Paper 382). Available from: https://www.cgdev.org/sites/default/files/future-healthcare-costs-brazil-mexico-chile_2.pdf [Google Scholar]
- 47.Goodyear-Smith F, van Weel C. Account for primary health care when indexing access and quality. Lancet. 2017;390(10091):205–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.