Abstract
Background and aims
Patients with schizophrenia are known to use potentially addictive psychoactive substances as self-medication and to ease psychological distress. Other potentially addictive behaviors such as online gaming are also used to self-medicate and ease psychological distress. However, the role of online gaming and problematic gaming (in the form of internet gaming disorder [IGD]) has not previously been investigated for patients with schizophrenia facing distress.
Methods
One hundred and four participants diagnosed with schizophrenia were recruited and completed a number of psychometric scales including the Personal and Social Performance Scale (PSPS), Internet Gaming Disorder Scale-Short Form (IGDS-SF9), Self-Stigma Scale-Short (SSS-S), and Depression, Anxiety, Stress Scale (DASS-21).
Results
The results showed significant negative associations between PSPS, IGDS-SF9, and DASS-21, and significant positive correlations between the IGDS-SF-9, SSS-S and DASS-21. Moreover, IGD did not mediate the association between self-stigma and depression. However, IGD significantly mediated the association between self-stigma and anxiety, and the association between self-stigma and stress. In addition, (i) age and self-stigma were significant predictors for IGD; (ii) social function and self-stigma were significant predictors for depression; (iii) social function, self-stigma, and IGD were significant predictors for anxiety; and (iv) self-stigma and IGD were significant predictors for stress.
Conclusion
The findings suggest that online gaming may be a coping strategy for individuals with schizophrenia with psychological stress and self-stigma and that for some of these individuals, their gaming may be problematic.
Keywords: Internet gaming disorder, psychological distress, schizophrenia, self-stigma, social function
Introduction
Individuals who suffer from schizophrenia, a severe and chronic mental disorder, are often devalued and face discrimination from others because they have misunderstandings about the disorder (Dickerson, Sommerville, Origoni, Ringel, & Parente, 2002). Additionally, individuals with severe mental disorders may develop self-stigma (aka internalized stigma) because of the social context (Link & Phelan, 2001). Self-stigma among those with a mental health diagnosis refers to when such individuals become aware of the public stereotypes concerning stigma, and internalizes the stereotypes applying them to the self (Yanos, Roe, Markus, & Lysaker, 2008), and has become a commonly discussed topic in the literature (Chang, Wu, Chen, & Lin, 2016; Chang, Wu, Chen, Wang, & Lin, 2014; Huang, Chen, Pakpour, & Lin, 2018; Lin, Chang, Wu, & Wang, 2016). Self-stigma can become a type of distress which leads to further psychological stress, such as depression and anxiety, impacting quality of life negatively (Park, Bennett, Couture, & Blanchard, 2013). Patients with schizophrenia have been reported to have low self-esteem due to self-stigma (Werner, Aviv, & Barak, 2008). In addition, studies have demonstrated that elevated self-stigma is associated with poor social relationships (Yanos, Roe, & Lysaker, 2010) and low adherence to treatment (Fung, Tsang, & Corrigan, 2008) among help-seeking patients with schizophrenia (Vogel, Wade, & Hackler, 2007).
Previous research has shown associations between self-stigma, coping avoidance, social withdrawal, and depressive symptoms. For example, self-stigma has been reported as having an important role in negative prognosis affected by reduced hope and self-esteem (Yanos et al., 2008). Additionally, studies have shown that patients with schizophrenia have lower self-efficacy and lower self-esteem, and are vulnerable to having high levels of stigma-related stress because of the uncertainty surrounding their social identity (Major & O'Brien, 2005). It has also been found that patients with schizophrenia often use the internet (e.g., online gaming, social media use) as a method to cope with their self-stigma and related psychological problematic issues (Lee et al., 2018). However, one study reported that although using internet may have positive effect for individuals with shyness, such an activity may have risk of developing problematic internet use (Qing, Zongkui, Hua, Yuan, & Fanchang, 2013). In brief, patients with schizophrenia who have high levels of self-stigma and low self-esteem may use the internet as a way of keeping themselves at a distance from the outside world. However, this behavior may increase their possibility of being addicted to activities on the internet (e.g., online gaming).
Because individuals with major mental disorders (like schizophrenia) have been reported to have high comorbid prevalence with addiction to psychoactive substances (Dixon, 1999; Regier et al., 1990), they may be more likely to have comorbid behavioral addictions (e.g., online gaming addiction). Previous studies have reported that cigarette smoking can provide mood-modifying pleasure as well as reducing depression and stress (Addington & Duchak, 1997; Chambers, Krystal, & Self, 2001). Other studies have also indicated that cigarette smoking is used as a self-medicating activity for schizophrenics to help reduce psychological distress (Dickerson et al., 2013; Kumari & Postma, 2005). It has also been reported that patients with schizophrenia use psychoactive substances (nicotine being the most common) as self-medication to allay their clinical symptoms and side effects of their schizophrenia medication treatment (Manzella, Maloney, & Taylor, 2015). Indeed, the prevalence of cigarette smoking among schizophrenic patients is much higher than that among the general population (Dickerson et al., 2013).
Given the increased global availability of the internet via smartphones, tablets, laptops, and computers (O'Dea, 2020), individuals with schizophrenia may use activities on the internet (such as online gaming) to cope with their symptoms and side effects because such activities share similar features to substance use (e.g., mood-modifying properties that increase pleasure and reduce stress and anxiety) (Aliyari et al., 2018; von der Heiden, Braun, Müller, & Egloff, 2019). As technology has developed, the internet has become an integral and important part of modern life. Online gaming provides opportunities to connect people worldwide without self-disclosure (Laconi, Pirès, & Chabrol, 2017). Therefore, patients with schizophrenia are able to enhance their self-esteem and reduce their self-stigma when they engage in online gaming. However, literature has shown that online gaming among a small minority of individuals may lead to internet gaming disorder (IGD). This can result in educational and/or occupational impairment, relationship problems, daily dysfunction, and psychological distress (Alimoradi et al., 2019; Chen, Huang, Wu, Kuo, & Lin, 2019; Hawi, Samaha, & Griffiths, 2018; Leung et al., 2020; Strong, Lee, Chao, Lin, & Tsai, 2018). The latest (fifth) edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) listed IGD as a tentative disorder and a type behavioral addiction like gambling disorder (American Psychiatric Association, 2013). Additionally, the World Health Organization also included gaming disorder (online and/or offline) in the eleventh revision of the International Classification of Diseases (ICD-11) (Higuchi, 2019; World Health Organization, 2018).
Individuals with schizophrenia sometimes engage in potentially addictive behaviors (e.g., psychoactive substance use, gambling, gaming, etc.) as a method for coping with feelings of anxiety or depression (Potvin, Stip, & Roy, 2003). Given the rapid spread of online gaming internationally, the activity has become relatively easy to access. In short, it has become another way that individuals (including schizophrenic patients) to relieve psychological distress. It is also known that individuals with schizophrenia and co-occurring substance use disorder show high levels of self-stigma and low levels of self-esteem, which reduce treatment compliance, increase relapses, and impede recovery (Rodrigues et al., 2013). Given the similarity between addictions to psychoactive substances use and gaming, it is reasonable to postulate that patients with co-occurring schizophrenia and IGD will experience high levels of self-stigma and psychological distress. The present study investigates a mediation model where internet gaming disorder mediates the association between self-stigma and psychological distress (depression, anxiety, stress).
Methods
Participants and procedure
The present study employed a cross-sectional design in the Jianan Psychiatric Center (JPC). To facilitate protection of privacy for vulnerable population, participants were recruited at the most convenient location (i.e., the JPC). The JPC is the only psychiatric teaching center in the Tainan area, and is also the core hospital of psychiatric treatment network in southern Taiwan which comprises more than three million residents. The JPC provides daycare services for 200 patients with severe mental illness. Also, more than 5,000 patients with severe mental illness seek outpatient treatment there every month. All eligible participants were recruited from the daycare and outpatient units between April and July 2019 at the JPC. The inclusion criteria included: (i) a diagnosis of schizophrenia by at least one psychiatrist using the DSM-IV criteria; (ii) having the ability to use a smartphone and engaging in daily internet use at least for three months; (iii) having admission into the daycare programs or regular follow-up during outpatient treatment, indicating that the patient was in a stable condition (i.e., no or very little active psychotic symptoms); (iv) being more than 20 years old; and (v) having sufficient mental capacity to provide consent and complete the assessments. The exclusion criteria were having: (i) a severe and unstable medical disease or a history of neurological disease; (ii) a history of alcohol or substance dependence, excluding nicotine dependence; and (iii) a history of head injury. Those with a history of alcohol or substance dependence were excluded because of the reported comorbidities between alcohol/substance dependence and online gaming disorder (Burleigh et al., 2020). A total of 104 individuals with schizophrenia (60 females; 57.7%) with a mean age of 41.42 years (SD = 8.98) years participated in the present study.
Measures
Demographic and clinical characteristics information
These data were collected using a background information sheet and medical records. The background information sheet asked for information on age, gender, years of education, marital status, employment status (having a job or not), living status (with others or alone), and physical illness (having any physical illness or not). The medical records comprised the diagnosis and illness duration information of the participants. Therefore, self-reported physical illnesses were confirmed using the medical records.
Social function
This was assessed using the Personal and Social Performance Scale (PSPS), administered by psychiatrists in the JPC during the study period. The PSPS was developed based on the social functioning component of the DSM-IV and the Social Occupational Functioning Assessment Scale (SOFAS). The PSPS comprises four items: socially-useful activities; personal and social relationships; self-care; and disturbing and aggressive behaviors. Each item uses a six-point Likert scale ranging from 1 (Absent) to 6 (Very severe). A single overall score (which reflects global functioning) is derived from the levels of impairment in each of the four domains, ranging from 1 to 100. Higher scores represent better social functioning, with ratings from 91–100 referring to more than adequate functioning (Morosini, Magliano, Brambilla, Ugolini, & Pioli, 2000). The PSPS has been found to have satisfactory psychometric properties with the test–retest reliability coefficient of 0.91 (P < 0.01) and internal consistency (Cronbach's α) coefficient of 0.73 (Wu et al., 2013). Moreover, the PSPS is highly correlated with the Activities of Daily Living Scale (ADLS), the SOFAS, and the Positive and Negative Syndrome Scale (PANSS) (Hsieh et al., 2011; Nasrallah, Morosini, & Gagnon, 2008). The internal consistency of the PSPS in the present study was good (α = 0.76).
Internet gaming disorder
IGD was assessed using the nine-item Internet Gaming Disorder Scale-Short Form (IGDS-SF9) which was developed based on DSM-5 IGD criteria. Each item represents one diagnostic criterion. Participants are asked to report their frequency of each symptom on a five-point Likert scale, ranging from 1 (Never) to 5 (Very often). A higher score indicates higher level of internet gaming addiction. A sample item is “Do you systematically fail when trying to control or cease your gaming activity?” The IGDS-SF9 has been translated into Chinese for the Taiwanese population with satisfactory psychometric properties (α = 0.94) (Leung et al., 2020; Yam et al., 2019). The internal consistency of the IGDS-SF9 in the present study was excellent (α = 0.93).
Self-stigma
This was assessed using the Self-Stigma Scale-Short Form (SSS-S). The SSS-S comprises nine items and was first designed for different minority groups (e.g., mental health consumers, immigrants, and sexual-orientation minorities: lesbians, gay men, and bisexuals). Therefore, the terms describing the minority group can be replaced and this present study the term of schizophrenia was used as the replacement. Participants indicate the agreement on each item using a four-point Likert scale, ranging from 1 (Strongly disagree) to 4 (Strongly agree). A higher score indicates a higher level of self-stigma. A sample item is “My identity as a person with schizophrenia is a burden to me.” The SSS-S has been translated into Chinese for the Taiwanese population with satisfactory psychometric properties (α = 0.95) (Chang, Lin, Gronholm, & Wu, 2018; Wu, Chang, Chen, Wang, & Lin, 2015). The internal consistency of the SSS-S in the present study was excellent (α = 0.93).
Psychological distress
This was assessed using the Depression, Anxiety, and Stress Scale (DASS-21). The DASS-21 comprises 21 items distributed across three types of psychological distress: depression (seven items; sample item “It was hard for me to have the initiative to do things”), anxiety (seven items; sample item “My mouth felt dry”), and stress (seven items; sample item “I found it difficult to calm myself”) (Oei, Sawang, Goh, & Mukhtar, 2013). Participants indicate the agreement on each item using a four-point Likert scale, ranging from 0 (Strongly disagree) to 3 (Strongly agree). A higher score indicates a higher level of psychological distress. The internal consistency of the DASS-21 and its subscales in the present study were very good to excellent (α = 0.88 for depression; 0.85 for anxiety; 0.87 for stress; and 0.95 for entire DASS-21).
Data analysis
Apart from the descriptive statistics (where categorical variables were analyzed using frequencies and percentages; continuous variables using means and SDs), Pearson correlations were used to test the associations between the studied variables. Pearson correlations were used because all the studied variables were normally distributed according to acceptable skewness (range between −0.34 and 1.30) and kurtosis (range between −1.24 and 1.30) information.
Mediation models based on ordinary least squares regression method (Alimoradi, Lin, Imani, Griffiths, & Pakpour, 2019; Lin et al., 2019) were constructed to investigate whether IGD was a mediator in the association between self-stigma and psychological distress. More specifically, three mediation models were constructed (the three dependent variables were depression, anxiety, and stress) using the same mediator (IGD), independent variable (self-stigma), and controlling variables (age, gender, social function, presence of physical disease, living status, and employment status). Model 4 in the Process Macro (Hayes, 2013) was used to carry out the mediation models, and 5,000 bootstrap samples were used to examine the mediated effects for each model: if the 95% lower limit confidence interval (LLCI) and upper limit confidence interval (ULCI) cover the value of 0, it indicates no mediated effect; if the LLCI and ULCI do not cover 0, it supports mediated effect (Lin & Tsai, 2016).
Ethics
The research proposal was approved by the Institutional Review Board (IRB) of Jianan Psychiatric Center (JPC), Ministry of Health and Welfare (IRB numbers: 18-039 & 19-034). Before data collection, all ethical considerations including description of the study, privacy and confidentiality of data, anonymity, and freedom of participation (or withdrawal) were fully explained. Additionally, all participants signed written informed consent.
Results
Among the 104 individuals with schizophrenia, just over half of them did not have any part-time or full-time work. The self-reported physical illnesses by participants were identical to official registered information. However, no participants had a formal IGD diagnosis given that such a diagnosis is not common within the Taiwanese medical system. Approximately one-quarter of the participants had comorbid diagnosis of depression (n = 24; 23.1%), and none of the participants had other comorbid psychiatric disorder. Approximately three-quarters of participants were recruited from outpatient units and the remainders were recruited from daycare programs. The participants had received a mean average of 12.46 years of education (SD = 2.46). Most of the participants were single. Their scores in social functioning (assessed using PSPS), internet gaming disorder (using IGDS-SF9), self-stigma (using SSS-S), and psychological distress (using DASS-21) is presented in Table 1.
Table 1.
Participant characteristics (N = 104)
| Variable | Mean (±SD) or n (%) |
|---|---|
| Gender (female) | 60 (57.7) |
| Age (year) | 41.42 (±8.98) |
| Years of education | 12.46 (±2.46) |
| Marital status (single) | 68 (65.4) |
| Employment (no) | 57 (54.8) |
| Registered physical illness (no) | 71 (68.3) |
| Living status (alone) | 10 (9.6) |
| Years since diagnosis | 8.46 (±5.34) |
| Diagnosis (schizoaffective) | 22 (21.4) |
| Diagnosis (depression) | 24 (23.1) |
| Personal and Social Performance Scale score (0–100 scale); n = 87 | 83.79 (±5.66) |
| Internet Gaming Disorder Scale-Short Form score (1–5 scale) | 1.61 (±0.76) |
| Internet Gaming Disorder Scale-Short Form score (9–45 scale)a | 14.52 (±6.85) |
| Self-Stigma Scale-Short score (1–4 scale); n = 103 | 2.30 (±0.72) |
| Depression score (0–3 scale)b | 0.84 (±0.71) |
| Anxiety score (0–3 scale)b | 0.79 (±0.69) |
| Stress score (0–3 scale)b | 0.90 (±0.72) |
| Depression, Anxiety, Stress Scale (DASS-21) total score (0–3 scale) | 0.84 (±0.66) |
| Depression score (0–21 scale)a,b | 5.85 (±4.99) |
| Anxiety score (0–21 scale)a,b | 5.55 (±4.84) |
| Stress score (0–21 scale)a,b | 6.33 (±5.03) |
| DASS-21 total score (0–63 scale)a | 17.72 (±13.91) |
aClinical cutoffs are 5 (mild), 7 (moderate), 11 (severe), and 14 (extremely severe) for depression; 4 (mild), 6 (moderate), 8 (severe), and 10 (extremely severe) for anxiety; 8 (mild), 10 (moderate), 13 (severe), and 17 (extremely severe) for stress; 21 for Internet Gaming Disorder Scale-Short Form score.
bAssessed using Depression, Anxiety, Stress Scale (DASS-21).
The relationships between the studied variables are shown in Table 2, where all the correlation coefficients were significant, except for the correlation between PSPS score and SSS-S score. Furthermore, PSP score was negatively associated with IGDS-SF9 and DASS-21 scores with moderate magnitude; IGDS-SF9, SSS-S, and DASS-21 scores were mutually associated in positive direction with moderate to strong magnitude.
Table 2.
Correlation matrix among studied variables (N = 104)
| r (P) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
| 1. Gender (Ref: female) | – | |||||||||
| 2. PSPS | −0.27∗ (0.01) | – | ||||||||
| 3. IGDS-SF9 | 0.26∗∗ (0.007) | −0.22∗ (0.04) | – | |||||||
| 4. SSS-S | 0.09 (0.35) | −0.11 (0.31) | 0.31∗∗ (0.001) | – | ||||||
| 5. Depression | −0.06 (0.55) | −0.32∗∗ (0.003) | 0.28∗∗ (0.004) | 0.43∗∗∗ (<0.001) | – | |||||
| 6. Anxiety | −0.05 (0.59) | −0.28∗∗ (0.008) | 0.33∗∗ (0.001) | 0.43∗∗∗ (<0.001) | 0.77∗∗∗ (<0.001) | – | ||||
| 7. Stress | 0.01 (0.89) | −0.28∗∗ (0.009) | 0.38∗∗∗ (<0.001) | 0.49∗∗∗ (<0.001) | 0.82∗∗∗ (<0.001) | 0.85∗∗∗ (<0.001) | – | |||
| 8. Physical illness (Ref: No) | 0.09 (0.39) | −0.14 (0.20) | 0.07 (0.50) | 0.04 (0.67) | −0.02 (0.84) | 0.05 (0.61) | −0.02 (0.81) | – | ||
| 9. Years since diagnosis | −0.02 (0.83) | −0.003 (0.98) | 0.08 (0.44) | −0.07 (0.46) | −0.01 (0.93) | −0.03 (0.74) | −0.09 (0.39) | 0.16 (0.10) | – | |
| 10. Diagnosis (Ref: schizophrenia) | −0.02 (0.85) | −0.05 (0.63) | 0.03 (0.79) | −0.10 (0.33) | 0.12 (0.25) | 0.21 (0.03) | 0.17 (0.08) | −0.05 (0.59) | 0.07 (0.48) | – |
PSPS = Personal and Social Performance Scale; IGDS-SF9 = Internet Gaming Disorder Scale-Short Form; SSS-S = Self-Stigma Scale-Short; Depression, Anxiety, and Stress were assessed using the Depression, Anxiety, Stress Scale (DASS-21).
∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001
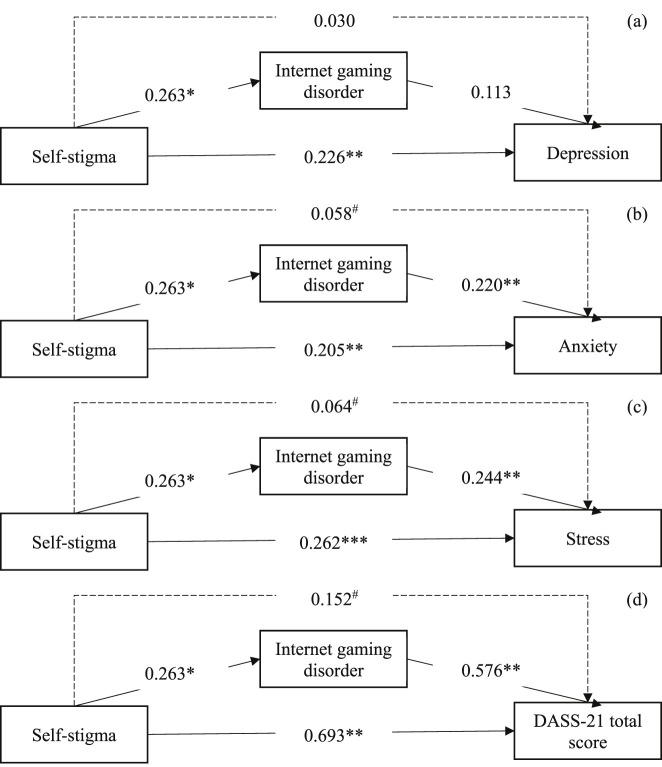
Table 3 demonstrates the mediated effects of IGD in the associations between self-stigma and psychological distress. More specifically, IGD mediated the association between self-stigma and depression by a marginally significant effect, while IGD significantly mediated the association between self-stigma and anxiety and the association between self-stigma and stress. In addition, age and self-stigma were significant predictors for IGD; social function and self-stigma were significant predictors for depression; social function, self-stigma, and IGD were significant predictors for anxiety; self-stigma and IGD were significant predictors for stress (Fig. 1).
Table 3.
Mediated effects of internet gaming disorder in the association between self-stigma and psychological distress among people with schizophrenia (N = 104)
| Coefficient (SE)/P-value | |||||
|---|---|---|---|---|---|
| Mediator | Dependent variable | ||||
| Internet gaming disorder | Depression | Anxiety | Stress | DASS-21 total score | |
| Age | −0.242 (0.082)/0.004 | 0.021 (0.060)/0.731 | 0.057 (0.057)/0.327 | 0.031 (0.055)/0.579 | 0.108 (0.157)/0.495 |
| Gender (Ref: female) | 1.041 (1.481)/0.484 | −1.093 (1.032)/0.293 | −1.237 (0.987)/0.214 | −0.101 (0.944)/0.915 | −2.432 (2.705)/0.372 |
| Social function | −0.198 (0.129)/0.130 | −0.215 (0.091)/0.021 | −0.174 (0.087)/0.049 | −0.132 (0.084)/0.119 | −0.521 (0.239)/0.033 |
| Physical disease (Ref: no) | 1.766 (1.542)/0.255 | −0.556 (1.080)/0.608 | −0.745 (1.033)/0.473 | −1.232 (0.988)/0.216 | −2.533 (2.830)/0.374 |
| Living status (Ref: alone) | 2.677 (2.462)/0.280 | −1.356 (1.722)/0.434 | −0.186 (1.648)/0.911 | −1.630 (1.576)/0.304 | −3.172 (4.515)/0.484 |
| Employment (Ref: no) | −0.824 (1.394)/0.556 | −0.925 (0.970)/0.344 | −0.627 (0.928)/0.502 | −0.523 (0.888)/0.557 | −2.075 (2.544)/0.417 |
| Self-stigma | 0.263 (0.108)/0.017 | 0.226 (0.078)/0.005 | 0.205 (0.075)/0.008 | 0.262 (0.071)/<0.001 | 0.693 (0.204)/0.001 |
| Internet gaming disorder | – | 0.113 (0.079)/0.156 | 0.220 (0.075)/0.005 | 0.244 (0.072)/0.001 | 0.576 (0.206)/0.007 |
| Mediated effectsa | – | 0.030 (0.029)/−0.005, 0.111 | 0.058 (0.037)/0.006, 0.156 | 0.064 (0.038)/0.002, 0.150 | 0.152 (0.098)/0.006, 0.383 |
| Model fit | |||||
| R 2 | 0.262 | 0.247 | 0.293 | 0.367 | 0.265 |
| F (P-value) | 3.959 (0.001) | 3.153 (0.004) | 3.995 (0.001) | 5.588 (<0.001) | 4.011 (0.001) |
DASS-21 = Depression, Anxiety, Stress Scale.
Mediated effects were tested using bootstrapping methods (5,000 random bootstrap samples) with the presentation as coefficient (SE)/lower limit confidence interval, upper limit confidence interval.
Fig. 1.
Mediated effects of internet gaming disorder in the association between self-stigma and psychological distress; (a) depression, (b) anxiety, (c) stress, and (d) Depression, Anxiety, Stress Scale (DASS-21) total score. Age, gender, social function, physical disease, living status, and employment were controlled in the mediation models. #Indicates significant indirect effects using bootstrapping method (i.e., confidence interval of 5000 bootstrap samples does not cover the value of 0. ∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001
Discussion
Approximately 65% of individuals with schizophrenia recruited in the present study had single status, and on average had low educational level. The demographic information is consistent with previous reports among individuals with schizophrenia because their schizophrenic symptoms may prevent them from receiving formal education and attaining intimate relationships (Deshmukh, Bhagat, Shah, Sonavane, & Desousa, 2016). Such demographic features (i.e., single and low educational level) would likely impact on their social functioning with poor self-care and occupation (Li et al., 2015).
The positive correlation between self-stigma (assessed using the SSS-S) and psychological distress (assessed using the DASS-21), suggested that patients with schizophrenia might have their psychological distress (i.e., depression, anxiety, and stress) initiated by their self-stigma (although the cross-sectional nature of the study means that such a hypothesis is speculative). Low levels of stress can sometimes be good because it helps individuals achieve things in their day-to-day lives. However, higher levels of stress increase anxiety and may make individuals with mental health issues worse, although stress in itself is not a clinical diagnosis. Psychological stress has been long considered to have an important role in the expression of symptoms in schizophrenic patients (Corcoran, Mujica-Parodi, Yale, Leitman, & Malaspina, 2002). Previous research has shown that the more emotional stress and distress that schizophrenic patients perceive they have, the more severe symptoms they tend to have (Horan & Blanchard, 2003). More specifically, compared to healthy controls, patients with schizophrenia have been found to have significantly higher stress levels, and which is correlated with their negative symptoms (Betensky et al., 2008). Although research into anxiety disorder and anxiety syndrome among schizophrenic patients is scant (Braga, Petrides, & Figueira, 2004; Dernovsek & Sprah, 2009; Temmingh & Stein, 2015), psychological stress among individuals with schizophrenia should be taken into account in clinic care. Therefore, the association between self-stigma and psychological distress found in the present study may associate with a third variable (e.g., social functioning or the severity of symptoms of schizophrenia).
The association between self-stigma and IGD in the present study may be explained by the coping strategy of online gaming. Online gaming or online use more generally can help schizophrenic patients to connect with others without any self-disclosure via the internet because of the perceived anonymity that the online medium provides. Consequently, individuals with schizophrenia may use the online medium to escape from social stigma in the outside world (Athanasopoulou et al., 2017; Lee et al., 2018). However, online gaming could bring pleasure and positive outcomes for schizophrenic patients, but for a minority, the negative impact of developing IGD may increase individuals' stress due to low success in the virtual world (King & Delfabbro, 2018) and poor sleep quality (Mannikko, Billieux, & Kaariainen, 2015). For those who have comorbid IGD and schizophrenia, the higher the likelihood of psychological distress.
The present study found that IGD was associated with anxiety, stress and depression. However, IGD was found to mediate only self-stigma and stress and anxiety, and not depression. The results suggested that IGD may not trigger all types of psychological distress. Thus, future studies are needed to more deeply investigate in this topic. To the best of the present authors' knowledge, this is the first study to examine the mediation effects of IGD in the association between self-stigma and different types of psychological distress among individuals with schizophrenia. Although the present findings cannot be directly compared to other studies' findings given the lack of such evidence in literature, research on psychoactive substance misuse of individuals with schizophrenia is comparable to the present study's findings. More specifically, Rodrigues et al. (2013) reported that individuals with schizophrenia and co-occurring substance use disorder showed high levels of self-stigma. This partially mirrors the association found between self-stigma and IGD in the present study.
The finding that IGD was associated with self-stigma and psychological distress suggests several implications. First, healthcare providers should teach individuals with schizophrenia appropriate and reasonable coping strategies to tackle their self-stigma problems. For example, several self-stigma reduction programs have been found to be effective (Yanos, Lucksted, Drapalski, & Roe, 2015) and patients with schizophrenia are encouraged to participate in these programs. Second, the use of online gaming to cope with self-stigma should perhaps be discouraged for the patients with schizophrenia or at least limited so that they are not engaged in excessive gaming. Patients with schizophrenia can of course engage in their leisure time. However, they should be instructed that such gaming activities are not good for their psychological health if they over-engage.
There are some limitations in the present study. First, the measures on self-stigma and psychological distress were assessed using self-reports. Therefore, common biases due to self-reporting such as recall bias and social desirability may influence the results of present study. Moreover, common variance bias may have resulted from the same method being used for assessments and may contribute to an overestimation in the associations found in the present study. Future studies should therefore use mixed-methods to assess self-stigma and psychological distress. For example, using self-reports to assess self-stigma and using observations to assess psychological distress. Second, given that all the participants were recruited from a single psychiatric center, the generalizability of the present sample is restricted. Moreover, all the participants were in a stable condition at the time of data collection. Consequently, the present study's findings are hard to generate to acute patients with schizophrenia. Future studies recruiting individuals with schizophrenia at different stages and from different areas are warranted to corroborate the present study's findings. Recruiting participants with schizophrenia from different stages and areas may also resolve the limitation of the relatively small sample size in the present study. Finally and importantly, the present study utilized a cross-sectional design and therefore cannot provide strong evidence concerning the causality between the studied variables. Therefore, a longitudinal study assessing the relationships between self-stigma, IGD, and psychological distress is needed to further examine any potential causal relationship.
Conclusions
The age of individuals and the level of self-stigma were predictors of IGD among patients with schizophrenia in the present study. Online gaming appears to be another way for patients to reduce psychological distress and to help them escape from their reality into a virtual world free of alienation and stigma. Although playing online games may have some positive benefits by helping patients with schizophrenia cope with their psychological distress or help them to connect with others, an unintended consequence might occur as suggested by the present study's findings (i.e., a ‘vicious cycle’ in which gaming is engaged in to relieve psychological distress). More specifically, the excessive gaming itself might become a stressor due to the impacts on other areas of their life, exacerbating the overall level of psychological distress arising from comorbid schizophrenia and IGD.
Funding sources
This work was supported partly by grant from Asia University (105-asia-01, 106-asia-15 and 107-asia-06 to Y-HC) and from Ministry of Science Technology (MOST 108-2410-H-468-009 & MOST 109-2628-H-468-001-MY2 to Y-HC; MOST 108-2314-B-695-001 to K-CC).
Authors' contribution
Y-HC, K-CC and C-YL created and organized the study. K-CC collected the data. C-YL analyzed the data; Y-HC, K-CC, and C-YL wrote the first draft, analyzed and interpreted the data. W-LH and C-YL reanalyzed the data in revision status. Y-HC, K-CC, W-LH, C-YL, and MDG critically reviewed the manuscript and provided constructive comments. MDG supervised the entire study and was responsible for all final editing.
Conflict of interest
The authors declare no conflict of interest
Acknowledgments
We sincerely thank for all the participants.
References
- Addington, J., & Duchak, V. (1997). Reasons for substance use in schizophrenia. Acta Psychiatrica Scandinavica, 96(5), 329–333. 10.1111/j.1600-0447.1997.tb09925.x. [DOI] [PubMed] [Google Scholar]
- Alimoradi, Z., Lin, C.-Y., Broström, A., Bülow, P. H., Bajalan, Z., Griffiths, M. D., …, Pakpour, A. H. (2019). Internet addiction and sleep problems: A systematic review and meta-analysis. Sleep Medicine Review, 47, 51–61. 10.1016/j.smrv.2019.06.004. [DOI] [PubMed] [Google Scholar]
- Alimoradi, Z., Lin, C.-Y., Imani, V., Griffiths, M. D., & Pakpour, A. H. (2019). Social media addiction and sexual dysfunction among Iranian women: The mediating role of intimacy and social support. Journal of Behavioral Addictions, 8(2), 318–325. 10.1556/2006.8.2019.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aliyari, H., Sahraei, H., Daliri, M. R., Minaei-Bidgoli, B., Kazemi, M., Agaei, H., …, Dehghanimohammadabadi, Z. (2018). The beneficial or harmful effects of computer game stress on cognitive functions of players. Basic and Clinical Neuroscience, 9(3), 177–186. 10.29252/nirp.bcn.9.3.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Athanasopoulou, C., Valimaki, M., Koutra, K., Lottyniemi, E., Bertsias, A., Basta, M., …, Lionis, C. (2017). Internet use, eHealth literacy and attitudes toward computer/internet among people with schizophrenia spectrum disorders: A cross-sectional study in two distant European regions. BMC Medical Informatics and Decision Making, 17(1), 136. 10.1186/s12911-017-0531-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betensky, J. D., Robinson, D. G., Gunduz-Bruce, H., Sevy, S., Lencz, T., Kane, J. M., … Szeszko, P. R. (2008). Patterns of stress in schizophrenia. Psychiatry Research, 160(1), 38–46. 10.1016/j.psychres.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braga, R. J., Petrides, G., & Figueira, I. (2004). Anxiety disorders in schizophrenia. Comprehensive Psychiatry, 45(6), 460–468. 10.1016/j.comppsych.2004.07.009. [DOI] [PubMed] [Google Scholar]
- Burleigh, T. L., Griffiths, M. D., Sumich, A., & Kuss, D. J. (2020). A systematic review of the co-occurrence of gaming disorder and other potentially addictive behaviors. Current Addiction Reports, 6, 383–401. 10.1007/s40429-019-00279-7. [DOI] [Google Scholar]
- Chambers, R. A., Krystal, J. H., & Self, D. W. (2001). A neurobiological basis for substance abuse comorbidity in schizophrenia. Biological Psychiatry, 50(2), 71–83. 10.1016/s0006-3223(01)01134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang, C.-C., Lin, C.-Y., Gronholm, P. C., & Wu, T.-H. (2018). Cross-validation of two commonly used self-stigma measures, Taiwan versions of the Internalized stigma mental illness scale and self-stigma scale–short, for people with mental illness. Assessment, 25(6), 777–792. 10.1177/1073191116658547. [DOI] [PubMed] [Google Scholar]
- Chang, C.-C., Wu, T.-H., Chen, C.-Y., & Lin, C.-Y. (2016). Comparing internalized stigma between people with different mental disorders in Taiwan. Journal of Nervous & Mental Disease, 204(7), 547–553. 10.1097/NMD.0000000000000537. [DOI] [PubMed] [Google Scholar]
- Chang, C.-C., Wu, T.-H., Chen, C.-Y., Wang, J.-D., & Lin, C.-Y. (2014). Psychometric evaluation of the internalized stigma of mental illness scale for patients with mental illnesses: Measurement invariance across time. PloS One, 9(6), e98767. 10.1371/journal.pone.0098767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y.-P., Huang, Y.-Y., Wu, Y., Kuo, Y.-J., & Lin, C.-Y. (2019). Depression negatively affects patient-reported knee functional outcome after intraarticular hyaluronic acid injection among geriatric patients with knee osteoarthritis. Journal of Orthopaedic Surgery and Research, 14, 387. 10.1186/s13018-019-1419-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran, C., Mujica-Parodi, L., Yale, S., Leitman, D., & Malaspina, D. (2002). Could stress cause psychosis in individuals vulnerable to schizophrenia? CNS Spectrums, 7(1), 33–42. 10.1017/s1092852900022240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dernovsek, M. Z., & Sprah, L. (2009). Comorbid anxiety in patients with psychosis. Psychiatria Danubina, 21(Suppl. 1), 43–50. [PubMed] [Google Scholar]
- Deshmukh, V., Bhagat, A., Shah, N., Sonavane, S., & Desousa, A. (2016). Factors affecting marriage in schizophrenia: A cross-sectional study. Journal of Mental Health and Human Behaviour, 21(2), 122–124. 10.4103/0971-8990.193432. [DOI] [Google Scholar]
- Dickerson, F. B., Sommerville, J., Origoni, A. E., Ringel, N. B., & Parente, F. (2002). Experiences of stigma among outpatients with schizophrenia. Schizophrenia Bulletin, 28(1), 143–155. 10.1093/oxfordjournals.schbul.a006917. [DOI] [PubMed] [Google Scholar]
- Dickerson, F., Stallings, C. R., Origoni, A. E., Vaughan, C., Khushalani, S., Schroeder, J., et al. (2013). Cigarette smoking among persons with schizophrenia or bipolar disorder in routine clinical settings, 1999–2011. Psychiatric Services, 64(1), 44–50. 10.1176/appi.ps.201200143. [DOI] [PubMed] [Google Scholar]
- Dixon, L. (1999). Dual diagnosis of substance abuse in schizophrenia: Prevalence and impact on outcomes. Schizophrenia Research, 35, S93–S100. 10.1016/s0920-9964(98)00161-3. [DOI] [PubMed] [Google Scholar]
- Fung, K., Tsang, H., & Corrigan, P. W. (2008). Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. Psychiatric Rehabilitation Journal, 32(2), 95–104. 10.2975/32.2.2008.95.104. [DOI] [PubMed] [Google Scholar]
- Hawi, N. S., Samaha, M., & Griffiths, M. D. (2018). Internet gaming disorder in Lebanon: Relationships with age, sleep habits, and academic achievement. Journal of Behavioral Addictions, 7(1):70-78. 10.1556/2006.7.2018.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: The Guilford Press. [Google Scholar]
- von der Heiden, J. M., Braun, B., Müller, K. W., & Egloff, B. (2019). The association between video gaming and psychological functioning. Frontiers in Psychology, 10, 1731. 10.3389/fpsyg.2019.01731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higuchi, S. (2019). Sharpening the focus on gaming disorder. Bulletin of the World Health Organization, 97(6), 382–383. 10.2471/BLT.19.020619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horan, W. P., & Blanchard, J. J. (2003). Emotional responses to psychosocial stress in schizophrenia: The role of individual differences in affective traits and coping. Schizophrenia Research, 60(2–3), 271–283. 10.1016/s0920-9964(02)00227-x. [DOI] [PubMed] [Google Scholar]
- Hsieh, P. C., Huang, H. Y., Wang, H. C., Liu, Y. C., Bai, Y. M., Chen, K. C., et al. (2011). Intercorrelations between the Personal and Social Performance Scale, cognitive function, and activities of daily living. The Journal of Nervous and Mental Disease, 199(7), 513–515. 10.1097/NMD.0b013e318221447e. [DOI] [PubMed] [Google Scholar]
- Huang, W.-Y., Chen, S.-P., Pakpour, A. H., & Lin, C.-Y. (2018). The mediation role of self-esteem for self-stigma on quality of life for people with schizophrenia: A retrospectively longitudinal study. Journal of Pacific Rim Psychology, 12, e10. 10.1017/prp.2017.18. [DOI] [Google Scholar]
- King, D. L., & Delfabbro, P. H. (2018). The concept of “harm” in Internet gaming disorder. Journal of Behavioral Addictions, 7(3), 562–564. 10.1556/2006.7.2018.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari, V., & Postma, P. (2005). Nicotine use in schizophrenia: The self medication hypotheses. Neuroscience & Biobehavioral Reviews, 29(6), 1021–1034. 10.1016/j.neubiorev.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Laconi, S., Pirès, S., & Chabrol, H. (2017). Internet gaming disorder, motives, game genres and psychopathology. Computers in Human Behavior, 75, 652–659. 10.1016/j.chb.2017.06.012. [DOI] [Google Scholar]
- Lee, J. Y., Chung, Y. C., Song, J. H., Lee, Y. H., Kim, J. M., Shin, I. S., …, Kim, S. W. (2018). Contribution of stress and coping strategies to problematic Internet use in patients with schizophrenia spectrum disorders. Comprehensive Psychiatry, 87, 89–94. 10.1016/j.comppsych.2018.09.007. [DOI] [PubMed] [Google Scholar]
- Leung, H., Pakpour, A. H., Strong, C., Lin, Y.-C., Tsai, M.-C., Griffiths, M. D., …, Chen, I.-H. (2020). Measurement invariance across young adults from Hong Kong and Taiwan among three internet-related addiction scales: Bergen social media addiction scale (BSMAS), smartphone application-based addiction scale (SABAS), and Internet gaming disorder scale-short form (IGDS-SF9) (study part A). Addictive Behaviors, 101, 105969. 10.1016/j.addbeh.2019.04.027. [DOI] [PubMed] [Google Scholar]
- Li, X.-J., Wu, J.-H., Liu, J.-B., Li, K.-P., Wang, F., Sun, X.-H., et al. (2015). The influence of marital status on the social dysfunction of schizophrenia patients in community. International Journal of Nursing Science, 2(2), 149–152. 10.1016/j.ijnss.2015.04.015. [DOI] [Google Scholar]
- Lin, C.-Y., Chang, C.-C., Wu, T.-H., & Wang, J.-D. (2016). Dynamic changes of self-stigma, quality of life, somatic complaints, and depression among people with schizophrenia: A pilot study applying kernel smoothers. Stigma and Health, 1(1), 29–43. 10.1037/sah0000014. [DOI] [Google Scholar]
- Lin, C.-Y., Imani, V., Brostrom, A., Huus, K., Bjork, M., Hodges, E. A., et al. (2019). Psychological distress and quality of life in Iranian adolescents with overweight/obesity: Mediating roles of weight bias internalization and insomnia. Eating and Weight Disorders. Advance Online Publication. 10.1007/s40519-019-00795-5. [DOI] [PubMed] [Google Scholar]
- Lin, C.-Y., & Tsai, M.-C. (2016). Effects of family context on adolescents’ psychological problems: Moderated by pubertal timing, and mediated by self-esteem and interpersonal relationships. Applied Research in Quality of Life, 11(3), 907–923. 10.1007/s11482-015-9410-2. [DOI] [Google Scholar]
- Link, B. G., & Phelan, J. C. (2001). Conceptualizing stigma. Annual Review of Sociology, 27(1), 363–385. 10.1146/annurev.soc.27.1.363. [DOI] [Google Scholar]
- Major, B., & O'Brien, L. T. (2005). The social psychology of stigma. Annual Review of Psychology, 56, 393–421. 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- Mannikko, N., Billieux, J., & Kaariainen, M. (2015). Problematic digital gaming behavior and its relation to the psychological, social and physical health of Finnish adolescents and young adults. Journal of Behavioral Addictions, 4(4), 281–288. 10.1556/2006.4.2015.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manzella, F., Maloney, S. E., & Taylor, G. T. (2015). Smoking in schizophrenic patients: A critique of the self-medication hypothesis. World Journal of Psychiatry, 5(1), 35–46. 10.5498/wjp.v5.i1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morosini, P. L., Magliano, L., Brambilla, L., Ugolini, S., & Pioli, R. (2000). Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatrica Scandinavica, 101(4), 323–329. 10.1034/j.1600-0447.2000.101004323.x. [DOI] [PubMed] [Google Scholar]
- Nasrallah, H., Morosini, P., & Gagnon, D. D. (2008). Reliability, validity and ability to detect change of the Personal and Social Performance scale in patients with stable schizophrenia. Psychiatry Research, 161(2), 213–224. 10.1016/j.psychres.2007.11.012. [DOI] [PubMed] [Google Scholar]
- O’Dea, S. (2020). Number of smartphone users worldwide from 2016 to 2021. Statista, Telecommunications. Retrived from https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/ Accessed at 21 March 2020. [Google Scholar]
- Oei, T. P. S., Sawang, S., Goh, Y. W., & Mukhtar, F. (2013). Using the depression anxiety stress scale 21 (DASS-21) across cultures. International Journal of Psychology, 48(6), 1018–1029. 10.1080/00207594.2012.755535. [DOI] [PubMed] [Google Scholar]
- Park, S. G., Bennett, M. E., Couture, S. M., & Blanchard, J. J. (2013). Internalized stigma in schizophrenia: Relations with dysfunctional attitudes, symptoms, and quality of life. Psychiatry Research, 205(1), 43–47. 10.1016/j.psychres.2012.08.040. [DOI] [PubMed] [Google Scholar]
- Potvin, S., Stip, E., & Roy, J. Y. (2003). Schizophrenia and addiction: An evaluation of the self-medication hypothesis. Encephale, 29(3 Pt. 1), 193–203. doi: ENC-6-2003-29-3-0013-7006-101019-ART1. [PubMed] [Google Scholar]
- Qing, L., Zongkui, Z., Hua, W., Yuan, T., & Fanchang, K. (2013). Shyness and Internet use. Advances in Psychological Science, 21(9), 1651–1659. 10.3724/SP.J.1042.2013.01651. [DOI] [Google Scholar]
- Regier, D. A., Farmer, M. E., Rae, D. S., Locke, B. Z., Keith, S. J., Judd, L. L., et al. (1990). Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. Journal of the American Medical Association, 264(19), 2511–2518. 10.1001/jama.1990.03450190043026. [DOI] [PubMed] [Google Scholar]
- Rodrigues, S., Serper, M., Novak, S., Corrigan, P., Hobart, M., Ziedonis, M., et al. (2013). Self-stigma, self-esteem, and co-occurring disorders. Journal of Dual Diagnosis, 9(2), 129–133. 10.1080/15504263.2013.777988. [DOI] [Google Scholar]
- Strong, C., Lee, C.-T., Chao, L.-H., Lin, C.-Y., Tsai, M.-C. (2018). Adolescent Internet use, social integration, and depressive symptoms: Analysis from a longitudinal cohort survey. Journal of Developmental and Behavioral Pediatrics, 39(4), 318–324. 10.1097/DBP.0000000000000553. [DOI] [PubMed] [Google Scholar]
- Temmingh, H., & Stein, D. J. (2015). Anxiety in patients with schizophrenia: Epidemiology and management. CNS Drugs, 29(10), 819–832. 10.1007/s40263-015-0282-7. [DOI] [PubMed] [Google Scholar]
- Vogel, D. L., Wade, N. G., & Hackler, A. H. (2007). Perceived public stigma and the willingness to seek counseling: The mediating roles of self-stigma and attitudes toward counseling. Journal of Counseling Psychology, 54(1), 40–50. 10.1037/0022-0167.54.1.40. [DOI] [Google Scholar]
- Werner, P., Aviv, A., & Barak, Y. (2008). Self-stigma, self-esteem and age in persons with schizophrenia. International Psychogeriatrics, 20(1), 174–187. 10.1017/S1041610207005340. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2018). Inclusion of “gaming disorder” in ICD-11. Retrieved from https://www.who.int/news-room/detail/16-01-2018-inclusion-of-%E2%80%9Cgaming-disorder%E2%80%9D-in-icd-11 Accessed 21 March 2020. [Google Scholar]
- Wu, T.-H., Chang, C.-C., Chen, C.-Y., Wang, J.-D., & Lin, C.-Y. (2015). Further psychometric evaluation of the self-stigma scale-short: Measurement invariance across mental illness and gender. PLoS One, 10(2), e0117592. doi: 10.1371/journal.pone.0117592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, B. J., Lin, C. H., Tseng, H. F., Liu, W. M., Chen, W. C., Huang, L. S., …, Lee, S. M. (2013). Validation of the Taiwanese Mandarin version of the Personal and Social Performance scale in a sample of 655 stable schizophrenic patients. Schizophrenia Research , 146(1–3), 34–39. 10.1016/j.schres.2013.01.036. [DOI] [PubMed] [Google Scholar]
- Yam, C. W., Pakpour, A. H., Griffiths, M. D., Yau, W. Y., Lo, C. M., Ng, J. M. T., et al. (2019). Psychometric testing of three Chinese online-related addictive behavior instruments among Hong Kong university students. Psychiatric Quarterly, 90(1), 117–128. 10.1007/s11126-018-9610-7. [DOI] [PubMed] [Google Scholar]
- Yanos, P. T., Lucksted, A., Drapalski, A. L., & Roe, D. (2015). Interventions targeting mental health self-stigma: A review and comparison. Psychiatric Rehabilitation Journal; 38(2), 171–178. 10.1037/prj0000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanos, P. T., Roe, D., & Lysaker, P. H. (2010). The impact of illness identity on recovery from severe mental illness. American Journal of Psychiatric Rehabilitation, 13(2), 73–93. 10.1080/15487761003756860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanos, P. T., Roe, D., Markus, K., & Lysaker, P. H. (2008). Pathways between internalized stigma and outcomes related to recovery in schizophrenia spectrum disorders. Psychiatric Services, 59(12), 1437–1442. 10.1176/appi.ps.59.12.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]