Abstract
Background
The coronavirus disease-2019 (COVID-19) pandemic has profoundly impacted aspects of human life globally. Playing videogames has been encouraged by several organizations to help individuals cope with the COVID-19 pandemic and associated restrictive measures. This longitudinal study was the first to examine gaming in the context of the pandemic and its association with depressive and anxiety symptoms.
Methods
The sample comprised 1,778 children and adolescents (50.7% male) who were part of the Project of School Mental Health in Southwest China. Data were collected at two-time intervals: before the COVID-19 pandemic (October to November 2019 – [T1]) and during the COVID-19 pandemic (April to May 2020 – [T2]). Data were collected on perceived COVID-19 impacts, videogame use, Internet Gaming Disorder (IGD), and depressive and anxiety symptoms. Cross-lagged panel models were computed to examine longitudinal relationships.
Results
The results indicated that both videogame use and IGD increased significantly for adolescents at T2. The cross-lagged panel model results suggested that depressive and anxiety symptoms at T1 positively predicted IGD and videogame use at T2 (especially for boys), but not inversely. Perceived COVID-19 impacts mediated the relationship between depressive and anxiety symptoms at T1 and IGD at T2.
Conclusion
Children and adolescents both increased videogame use at T2, but only adolescents significantly increased IGD severity at T2. The findings supported the compensatory hypothesis, and are consistent with the Interaction of Person-Affect-Cognition-Execution model as individual responses to COVID-19 may function as a mediator between personal predisposing variables and IGD.
Keywords: perceived COVID-19 impacts, videogame use, Internet gaming disorder, depressive symptoms, anxiety symptoms
Introduction
The coronavirus disease-2019 (COVID-19) pandemic has profoundly impacted aspects of human life globally. Recently, the World Health Organization (WHO) has recommended playing videogames as part of the #HealthyAtHome campaign to help mitigate the impacts of the COVID-19 pandemic on individuals' mental health (WHO, 2020). However, the long-term potential impacts of such recommendation on children and adolescents' well-being, particularly among excessive gamers, remains unknown. This is particularly problematic given that play may be on the rise due to the COVID-19 pandemic as the industry reported a surge in sales during the pandemic (BBC, 2020).
Furthermore, the experience of chronic stress during the COVID-19 pandemic may also lead to negative emotional distress, especially in terms of depression and anxiety (e.g., Pfefferbaum, & North, 2020; Qiu et al., 2020). Consequently, although, playing videogames may help individuals to cope with these aversive feelings (King, Delfabbro, Billieux, & Potenza, 2020; Ko & Yen, 2020), increased engagement may render individuals more prone to experiencing internet gaming disorder (IGD) as IGD may be a stress response (Snodgrass et al., 2014). Thus, this longitudinal study examined the potential associations between IGD, depressive and anxiety symptoms, and the role of perceived COVID-19 impacts on children and adolescent gamers.
Depressive symptoms, anxiety symptoms, and IGD
Depressive and anxiety symptoms have been among the most common mental health problems experienced by children and adolescents during the COVID-19 pandemic (e.g., Duan et al., 2020; Wang, Zhang, Zhao, Zhang, & Jiang, 2020). Investigating mental health problems (e.g., depression and anxiety disorders) has been suggested as one of the key COVID-19 research priorities (Holmes et al., 2020). However, most previous studies have been cross-sectional in nature, and there is a need for longitudinal and prospective studies to examine how the experience of depressive and anxiety symptoms may change during the pandemic (Shanahan et al., 2020).
IGD has been proposed as a tentative disorder in the fifth Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (American Psychiatric Association [APA], 2013) and recently recognized as an official mental health disorder by the WHO (Pontes & Griffiths, 2019). When considering the potential associations between depressive, anxiety symptoms, and IGD, three potential explanations can be considered. Firstly, the interpersonal impairment hypothesis views IGD as a maladaptive response to interpersonal stress rather than a pathology per se (Cheng, Cheung, & Wang, 2018). This hypothesis is aligned with the definition of IGD in the DSM-5 wherein IGD is viewed as a mental health disorder associated with impaired psychosocial well-being (Brunborg, Mentzoni, & Frøyland, 2014; Gentile et al., 2011; Teng et al., 2020). Secondly, the compensatory/gratification hypothesis (e.g., Kardefelt-Winther, 2014) views IGD as a consequence of psychological distress and decreased well-being in daily life. Consequently, individuals with impaired psychological health and well-being would be likely to engage in excessive gaming, further increasing IGD vulnerability while attempting to escape from adverse mental health experiences and negative feelings (e.g., Li et al., 2011). Thirdly, the common causes/comorbidity hypothesis suggests a dynamic and bi-directional relationship between IGD and psychological health (e.g., González-Bueso et al., 2018; Wichstrøm, Stenseng, Belsky, von Soest, & Hygen, 2019). This hypothesis was supported by previous cross-sectional (e.g., Burleigh, Stavropoulos, Liew, Adams, & Griffiths, 2018; King & Delfabbro, 2016) and longitudinal studies (e.g., Jeong et al., 2019; Krossbakken et al., 2018; Liu et al., 2018).
Although the aforementioned views help explain the nature of IGD and its potential etiological course, these views have been proposed within a typical developmental context and, to the best of our knowledge, no current evidence exists testing such explanations longitudinally during an atypical developmental context (i.e., before and during the COVID-19 pandemic).
Perceived COVID-19 impacts
Research has not only investigated how the COVID-19 pandemic has affected individuals' mental health, but also examined individuals' perceptions and responses to the COVID-19 pandemic and its association with mental health. For instance, the subjective fear of COVID-19 is closely associated with depression and anxiety symptoms (Fitzpatrick, Harris, & Drawve, 2020). Moreover, adults perceiving greater impacts due to the COVID-19 pandemic have reported higher levels of anxiety (Tull et al., 2020), which is unsurprising because perceived impacts of the COVID-19 pandemic have been shown to affect overall mental health (Kang et al., 2020). Based on this, it may be the case that if individuals perceive COVID-19 to be impacting on different life domains and activities (e.g., working, studying, sleeping, and socializing), they then may be more prone to engage in videogame playing to help them cope with their perceived negative experiences, further increasing their risk for developing IGD.
Theoretically, the Interaction of Person-Affect-Cognition-Execution (I-PACE) model (Brand et al., 2019) helps explain the processes implicated in the development of problematic internet behavior, including IGD. According to the I-PACE model, personal predisposing variables (that are thought to influence the development of IGD) include genetic and biological factors, personality factors, cognitive factors, motivation factors, and psychopathology variables. Within this theoretical framework, depressive and anxiety symptoms can be conceptualized as predisposing variables affecting gaming severity. Moreover, the I-PACE model also conceptualizes perceptions of affective and cognitive responses (e.g., attention bias, coping, and response to stress) as the consequences of predisposing variables that further influence the development of IGD. According to the I-PACE model, it is likely that individuals' responses to COVID-19 in terms of perceived COVID-19 impacts experienced may relate to the affective and cognitive processes that are regarded as underlying mechanisms between predisposing factors and IGD. This contention is also supported by recent research using the I-PACE model suggesting that COVID-19 anxiety symptoms mediate the relationship between generalized anxiety symptoms and problematic smartphone use (Elhai, Yang, McKay, & Asmundson, 2020).
The present study
During the COVID-19 pandemic, it is likely that children and adolescents may have increased their engagement with videogames in terms of time spent with the activity (King et al., 2020; Király et al., 2020; Ko & Yen, 2020) to help them meet basic psychosocial needs during the “stay-at-home” period brought about by the pandemic. However, since the COVID-19 pandemic is a prominent life stressor, children and adolescents may choose to play videogames as a coping strategy to help reduce stress, and some may also play videogames problematically, further increasing their potential risk for IGD. Therefore, it is critical to distinguish these two kinds of gaming behaviors and investigate their unique association with depressive and anxiety symptoms during the pandemic. Because the long-term “stay-at-home” order may lead to depressive symptoms and acute stress elicited by the COVID-19 pandemic may lead to anxiety symptoms for children and adolescents, the present study focused on investigating these two mental health problems (i.e., depression and anxiety symptoms). Based on the assumptions of the I-PACE model (Brand et al., 2019), the present longitudinal study examines the role of two key predisposing variables (e.g., depression and anxiety symptoms), and perceptions of affective and cognitive triggers (e.g., perceived COVID-19 impacts) on IGD among Chinese children and adolescents before and during the COVID-19 pandemic. Moreover, the model may have developmental (children and adolescents) and gender (boys and girls) differences, therefore, multi-group analyses will be carried out in the present study. Overall, the following key research questions (RQs) and hypotheses (Hs) will be investigated:
RQ1
Were videogame use and IGD severity exacerbated during the COVID-19 pandemic? It is hypothesized that both videogame use and IGD severity increased during the COVID-19 pandemic in comparison to the period before the COVID-19 outbreak (Hypothesis 1 [H1]).
RQ2
Are depressive and anxiety symptoms meaningful predictors of IGD symptoms during the COVID-19 pandemic or vice versa? It is hypothesized that both Time 1 depressive and anxiety symptoms will positively predict IGD at Time 2 after controlling for baseline IGD (Hypothesis 2 [H2]).
RQ3
Do perceived COVID-19 impacts mediate the relationship between early depressive, anxiety symptoms, and subsequent IGD severity? It is hypothesized that perceived COVID-19 impacts will mediate the relationship between depressive and anxiety symptoms at Time 1 and IGD at Time 2 (Hypothesis 3 [H3]).
Method
Participants and procedure
The sample comprised 1,778 children and adolescents (50.7% male) who were part of the Project of School Mental Health in Southwest China, a large longitudinal investigating the contextual factors (e.g., school, family, internet use) influencing the development of mental health of primary and secondary school students. All participants were sampled using cluster sampling from eight Chinese schools (four primary and four middle schools) at Chongqing, Sichuan, and Yunnan province in Southwest China during the 2018–2019 academic year. The present study used the data from Wave 3 (October to November 2019, before COVID-19 outbreak, Time 1 [T1]) and Wave 4 (April to May 2020, during the COVID-19 pandemic, Time 2 [T2]).
All schools provided authorization for data collection. Students from the 4th and 7th grades were required to additionally provide parental informed consent, and students' consent rates averaged 98% while parental consent rates averaged 94%. Only students who provided both personal and parental informed consent participated in the study (n = 2,111). At T1, participants completed the study survey in the classroom setting while at T2 students completed an online survey from home (https://www.wjx.cn/app/survey.aspx) due to the COVID-19 restrictions. All participants received a ballpoint pen for taking part in the study.
The inclusion criteria approach included three steps. First, participants with missing data at T2 (n = 94, 21 children and 73 adolescents) were excluded because they did not have data related to COVID-19. Second, participants who indicated their responses were “entirely false” or “false” were excluded (n = 99, 54 children and 45 adolescents) using the question “How truthful were your survey responses? (Entirely false, false, true, entirely true)”. Third, participants who did not play any videogames at both T1 and T2 were excluded (n = 140, 57 children and 83 adolescents). Therefore, the final sample comprised 1,778 participants (875 children and 903 adolescents).
Monte Carlo power analysis for indirect effects (Schoemann, Boulton, & Short, 2017) was conducted. Previous meta-analytic research suggested effect sizes for the association between IGD and poor psychological well-being to be small (r = 0.07–0.15, Cheng et al., 2018). Therefore, a small effect size was set for a (r = 0.10) and b (r = 0.10) paths. Consequently, recruiting a total of 1,000 participants would lead to power between 77% and 79% for the indirect effects (i.e., a × b) at the p < 0.05 level with 20,000 Monte Carlo replications. Thus, the sample recruited for the present study (n = 1,778) was more than sufficient to provide adequate statistical power (>80%) to detect small indirect effects.
Measures
Demographic information included age, gender, family monthly income, parental education level, infection of COVID-19 related information, time spent at home during the pandemic period. This information is presented in Table 1.
Table 1.
Key demographic information of the samples
| Children | Adolescents | |||
| Sample characteristics | n | % | n | % |
| Full sample | 875 | 49.2 | 903 | 50.8 |
| Gender | ||||
| Male | 456 | 52.1 | 445 | 50.7 |
| Female | 419 | 47.9 | 458 | 49.3 |
| Family monthly income | ||||
| <3,000 ¥ | 214 | 24.5 | 202 | 22.4 |
| 3,001–10,000 ¥ | 445 | 50.9 | 501 | 55.5 |
| >10,000 ¥ | 216 | 24.7 | 200 | 22.1 |
| Infection of COVID-19 related information | ||||
| Infection COVID-19 within community | 36 | 4.1 | 23 | 2.6 |
| Infection COVID-19 with family members | 11 | 1.3 | 6 | 0.7 |
| Infection COVID-19 with teachers/classmates | 10 | 1.1 | 7 | 0.8 |
| Time spent at home | ||||
| <1 week | 66 | 7.5 | 69 | 7.6 |
| 1 week to 1 month | 291 | 33.3 | 273 | 30.3 |
| >1 month | 518 | 59.2 | 561 | 62.1 |
Videogame use was assessed using a previously reported method (e.g., Teng et al., 2019). Participants were required to list the names of their three favorite videogames, indicating how frequently they played each game (e.g., 1 = once each month, 2 = once to twice each week, 3 = three to six times each week, 4 = once each day, 5 = many times each day) and the amount of time spent playing during each gaming session (e.g., 1 = 1–5 mins, 2 = 6–15 mins, 3 = 16–30 mins, 4 = 31–60 mins, 5 = more than 1 h). Participants could also report whether they had not played videogames by indicating “not applicable” for videogame names and for frequency/amount of time spent gaming. A videogame use index was then computed by multiplying the frequency of gaming ratings and time spent on each session, with the average scores of the three games computed as an overall measure of videogame use. For the score of the three videogames, the internal consistency coefficients were high across both waves (T1, McDonald's ω = 0.843; T2, McDonald' ω = 0.843).
The Internet Gaming Disorder Scale-Short Form (IGDS9-SF) (Pontes & Griffiths, 2015) was used to assess the severity of IGD symptoms. This scale was developed based on the DSM-5 criteria for IGD. A 5-point Likert scale (1 = never to 5 = very often) was used to rate all nine items during the past year (e.g., “Do you systematically fail when trying to control or cease your gaming activity?”). These nine items were averaged to create an IGD composite score, with higher scores suggesting greater IGD severity. The Chinese version of IGDS9-SF has shown adequate psychometric properties in previous research (e.g., Teng et al., 2020). In the present study, McDonald's ω coefficients for the IGDS9-SF were 0.891 (T1) and 0.916 (T2), further supporting its high levels of reliability.
Perceived COVID-19 impacts were assessed with five self-report questions which examined the degree of perceived impacts caused by the COVID-19 pandemic on different life domains (i.e., study activities, sleep quality, lifestyle habits [e.g., eating habits, physical exercise, and entertainment], social activities, and family relationships) at T2. Participants rated the degree of perceived impact on a 10-point Likert scale (1 = no impact to 10 = extreme impact), with greater scores suggesting greater perceived negative impact associated with COVID-19. This measure exhibited high internal consistency (McDonald's ω = 0.800) and adequate model fit in the confirmatory factor analysis (χ2[5] = 63.79, p < 0.001, CFI = 0.964, TLI = 0.929, RMSEA = 0.078, 90% CI [0.062, 0.096], SRMR = 0.031).
The Chinese version of the Center for Epidemiologic Studies Depression Scale (CES-D; Chen, Yang, & Li, 2009) was used to assess depressive symptoms. The scale comprises 20 items examining the frequency of depressive symptoms rated on a 4-point Likert scale (0 = never to 3 = many times). The scale includes four sub-factors (i.e., depressed affect, positive affect, somatic activity, and interpersonal problems), and the scores range from 0 to 60, with higher scores indicating greater severity of depression. The scale showed high internal consistency coefficient in the present study at both T1 (McDonald's ω = 0.925) and T2 (McDonald's ω = 0.933).
The Chinese version of the State-Trait Anxiety Inventory was used to assess anxiety (STAI; Shek, 1993). Because state anxiety is more transient in nature, this study only included the trait anxiety subscale which comprises 20 items assessing the frequency of anxiety symptoms (1 = almost to 4 = almost always). However, one item was excluded (“I wish I could be as happy as others seem to be”) due to cultural reasons (Chen et al., 2013). The scale includes two factors (i.e., anxiety absence and anxiety presence), and the scores range from 19 to 76. Higher scores indicate a greater severity of anxiety symptoms. This scale showed high-reliability coefficients in the present study at both T1 (McDonald's ω = 0.927) and T2 (McDonald's ω = 0.926).
Analytical procedure
To address RQ1, paired sample t-test analysis was conducted to compare mean differences at T1 and T2 between the main study variables. Following this, descriptive and correlational analyses were conducted relating to the main study variables. To address RQ2, two cross-lagged panel models were estimated utilizing Mplus 8.4 (Muthén & Muthén, 1998–2017). The first model focused on depressive symptoms, IGD, and videogame use (see Fig. 1) and the second model focused on anxiety symptoms, IGD, and videogame use (see Fig. 3). Because previous research (e.g., Burleigh et al., 2018; Cheng et al., 2018; Liu et al., 2018) suggested positively close relationships between the study variables, both cross-sectional correlations were calculated at T1 and T2. Moreover, the potential effects of gender, parental highest education levels, family monthly income, and time spent at home were controlled by entering these variables as covariates. To address RQ3, perceived COVID-19 as mediator was added to the cross-lagged panel models (see Figs 2 and 4). To decrease estimation bias and obtain robust results, both models were estimated using robust maximum likelihood estimation (MLR) and used a full information maximum likelihood estimation method to deal with missing data (Enders, 2010). Moreover, to account for the nesting effects of students within school classrooms, the standard errors were corrected with the “type=complex” command (McNeish, Stapleton, & Silverman, 2017) in Mplus 8.4. Moreover, 95% confidence intervals (CIs) were computed for standardized path coefficients and indirect effect (β). Both the measurement model fits are shown in Table S1.
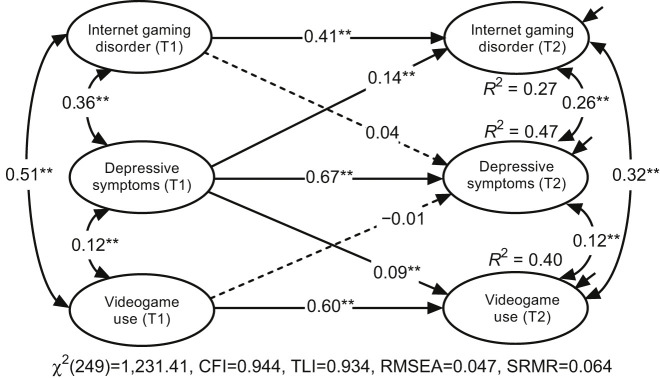
Fig. 1.
Cross-lagged panel model between Internet gaming disorder, videogame use and depressive symptoms before and during COVID-19 pandemic. Note. T1 = before COVID-19 pandemic, T2 = during COVID-19 pandemic. The model included covariate (age, sex, family monthly income, parental education level, time spent at home). * p < 0.05, ** p < 0.01
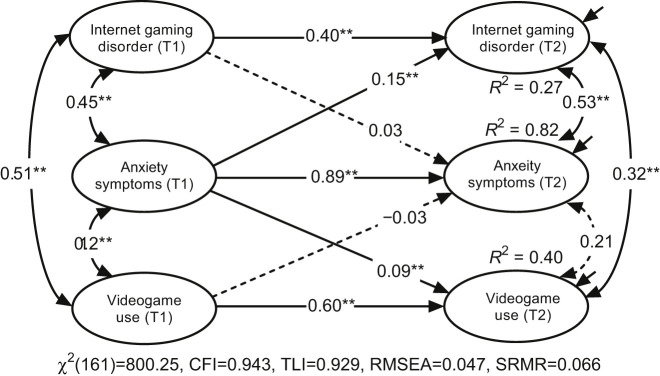
Fig. 3.
Cross-lagged panel model between Internet gaming disorder, videogame use and anxiety symptoms before and during COVID-19 pandemic. Note. T1 = before COVID-19 pandemic, T2 = during COVID-19 pandemic. The model included covariate (age, sex, family monthly income, parental education level, time spent at home). * p < 0.05, ** p < 0.01
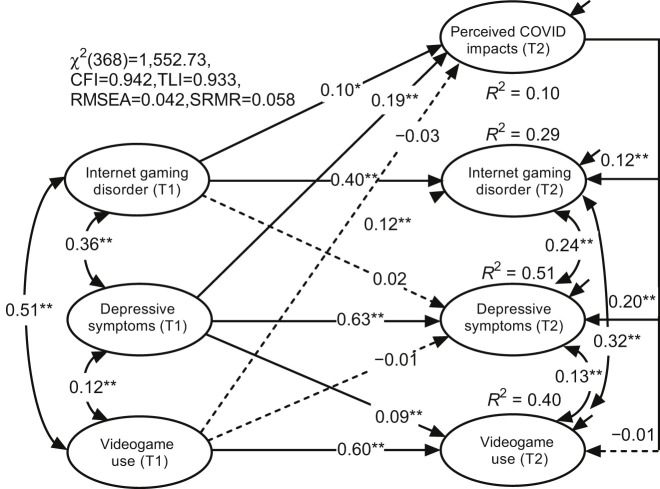
Fig. 2.
Mediation model of Perceived COVID-19 impacts between depressive symptoms and Internet gaming disorder. Note. T1 = before COVID-19 pandemic, T2 = during COVID-19 pandemic. The model included covariate (age, sex, family monthly income, parental education level, time spent at home). * p < 0.05, ** p < 0.01
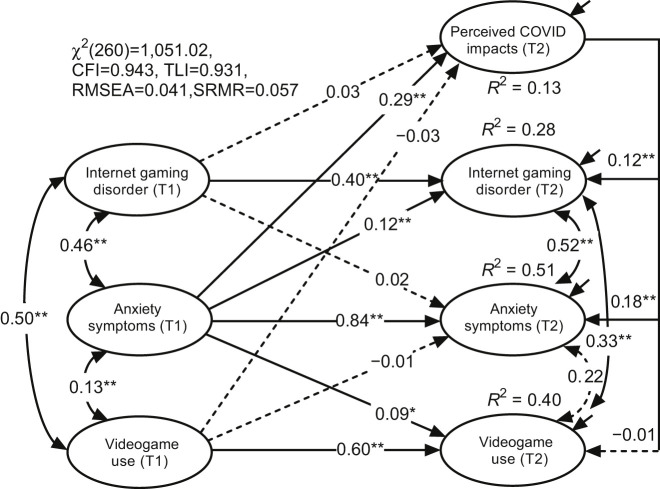
Fig. 4.
Mediation model of Perceived COVID-19 impacts between anxiety symptoms and Internet gaming disorder. Note. T1 = before COVID-19 pandemic, T2 = during COVID-19 pandemic. The model included covariate (age, sex, family monthly income, parental education level, time spent at home). * p < 0.05, ** p < 0.01
Ethics
The study procedures were carried out following the Declaration of Helsinki. The Institutional Review Board of the Faculty of Psychology, Southwest University approved the study.
Results
Descriptive and correlational findings
Using the cutoff ≥ 20 for CES-D (Chen et al., 2009), 33.6% of participants at T1 (267 boys and 336 girls) and 33.8% at T2 (267 boys and 334 girls) had depressive symptoms. Using the cutoff ≥ 44 for STAI, 36.2% of participants at T1 (289 boys and 355 girls) and 40.2% of participants at T2 (330 boys and 385 girls) had anxiety symptoms. Additionally, according to the DSM-5 (APA, 2013), 3.6% of participants at T1 (55 boys and 9 girls) and 5.0% at T2 (72 boys and 17 girls) endorsed at least five IGD items “often, or very often”.
As shown in Table 2, both samples had higher levels of videogame use at T2 compared to T1 (children, d = −0.20, and adolescents, d = −0.15). Furthermore, adolescents exhibited a higher severity of IGD at T2 (p = 0.035, d = −0.07) compared to T1, but not found among children (p = 0.287, d = −0.04). For anxiety symptoms, the results showed significantly higher scores at T2 in comparison to T1 in the total sample (p = 0.004, d = −0.07) and adolescent sample (p = 0.008, d = −0.09) but not in the children sample (p = 0.117, d = −0.05). With regards to depressive symptoms, no significant differences emerged across the total sample (p = 0.090), children sample (p = 0.546), and adolescent sample (p = 0.066) at T1 and T2. As shown in Table 3, positive correlations among the main study variables were found at both T1 and T2 (r = 0.07–0.81, all p-values < 0.01).
Table 2.
Mean differences between among the main study variables before the COVID-19 pandemic (T1) and during the COVID-19 pandemic (T2)
| T1 | T2 | |||||||
| Indicators | M | SD | M | SD | Correlations | t (df) | p | Cohen's d |
| Overall sample (n = 1,778) | ||||||||
| Videogame use | 6.86 | 4.67 | 7.55 | 4.96 | 0.55** | −6.96 (1,522) | <0.001 | −0.18 |
| Internet gaming disorder | 1.73 | 0.76 | 1.77 | 0.80 | 0.48** | −2.25 (1,777) | 0.025 | −0.05 |
| Depressive symptoms | 0.81 | 0.59 | 0.83 | 0.60 | 0.68** | −1.69 (1,756) | 0.090 | −0.04 |
| Anxiety symptoms | 1.95 | 0.65 | 1.98 | 0.66 | 0.71** | −2.88 (1,741) | 0.004 | −0.07 |
| Children sample (n = 875) | ||||||||
| Videogame use | 6.86 | 4.75 | 7.70 | 4.90 | 0.49** | −5.57 (754) | <0.001 | −0.20 |
| Internet gaming disorder | 1.67 | 0.75 | 1.70 | 0.78 | 0.45** | −1.06 (874) | 0.287 | −0.04 |
| Depressive symptoms | 0.70 | 0.58 | 0.71 | 0.59 | 0.64** | −0.61 (870) | 0.546 | −0.02 |
| Anxiety symptoms | 1.77 | 0.65 | 1.81 | 0.66 | 0.64** | −1.57 (853) | 0.117 | −0.05 |
| Adolescent sample (n = 903) | ||||||||
| Videogame use | 6.85 | 4.60 | 7.41 | 5.02 | 0.61** | −4.22 (767) | <0.001 | −0.15 |
| Internet gaming disorder | 1.79 | 0.77 | 1.84 | 0.81 | 0.50** | −2.11 (902) | 0.035 | −0.07 |
| Depressive symptoms | 0.91 | 0.59 | 0.94 | 0.58 | 0.69** | −1.84 (885) | 0.066 | −0.06 |
| Anxiety symptoms | 2.11 | 0.60 | 2.15 | 0.61 | 0.75** | −2.66 (887) | 0.008 | −0.09 |
Note: ** p < 0.01. T1 = before COVID-19 pandemic, T2 = during COVID-19 pandemic.
Table 3.
Correlation matrix between the main variables of the study
| Indicators | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
| 1. Videogame use [T1] | − | ||||||||
| 2. Videogame use [T2] | 0.56 | − | |||||||
| 3. Internet gaming disorder [T1] | 0.44 | 0.36 | − | ||||||
| 4. Internet gaming disorder [T2] | 0.30 | 0.42 | 0.48 | − | |||||
| 5. Depressive symptoms [T1] | 0.13 | 0.15 | 0.36 | 0.27 | − | ||||
| 6. Depressive symptoms [T2] | 0.10 | 0.16 | 0.28 | 0.35 | 0.68 | − | |||
| 7. Anxiety symptoms [T1] | 0.09 | 0.12 | 0.36 | 0.26 | 0.81 | 0.63 | − | ||
| 8. Anxiety symptoms [T2] | 0.08 | 0.14 | 0.31 | 0.35 | 0.65 | 0.81 | 0.71 | − | |
| 9. Perceived COVID-19 impacts [T2] | 0.08 | 0.07 | 0.17 | 0.22 | 0.24 | 0.35 | 0.26 | 0.34 | − |
| Range | 1–25 | 1–25 | 1–5 | 1–5 | 0–3 | 0–3 | 1–4 | 1–4 | 1–10 |
| Mean | 6.86 | 7.55 | 1.73 | 1.77 | 0.81 | 0.83 | 1.95 | 1.98 | 3.32 |
| Standard Deviation | 4.67 | 4.96 | 0.76 | 0.80 | 0.59 | 0.60 | 0.65 | 0.66 | 1.94 |
| Skewness | 1.65 | 1.33 | 1.35 | 1.21 | 0.99 | 1.03 | 0.46 | 0.29 | 1.00 |
| Kurtosis | 3.25 | 1.81 | 2.08 | 1.34 | 0.65 | 0.90 | −0.40 | −0.63 | 0.85 |
Note: All correlations were significant at the p < 0.01 level. T1 = before COVID-19 pandemic, T2 = during COVID-19 pandemic.
Perceived COVID-19 impacts, depressive symptoms, and IGD
After controlling for the covariates (e.g., age, gender, parental educational level, family monthly income, and time spent at home), the cross-lagged panel model analyses yielded adequate fits. As shown in Fig. 1, autoregression path coefficients were significant in depressive symptoms, IGD, and videogame use from T1 to T2. Cross-sectional correlation coefficients were also significant both in T1 and T2 (all p-values<0.01). The paths further suggested that depressive symptoms were a significant predictor of videogame use (β = 0.09, 95% CI[0.04, 0.14]) and IGD (β = 0.14, 95% CI[0.10, 0.19]) from T1 to T2. However, videogame use (β = −0.01, 95% CI[−0.07, 0.05]) and IGD (β = 0.04, 95% CI[−0.02, 0.10]) were not predictors of depressive symptoms from T1 to T2.
Furthermore, when perceived COVID-19 impacts were included as a mediator in the model, the results also suggested adequate fits. The path coefficients further indicated that depressive symptoms at T1 predicted perceived COVID-19 impacts at T2 (β = 0.19, 95% CI[0.13, 0.25]) and that perceived COVID-19 impacts also predicted IGD at T2 (β = 0.12, 95% CI[0.08, 0.17]). Furthermore, the specific indirect effect of depressive symptoms at T1 on IGD at T2, via perceived COVID-19 impacts was statistically significant (effect: a × b = 0.023, 95% CI[0.010, 0.036]). Moreover, all three variables showed significant autoregression path coefficients and cross-sectional correlation coefficients (see Fig. 3). The covariates and other path coefficients can be found in Table S2.
Perceived COVID-19 impacts, anxiety symptoms, and IGD
After controlling the covariates, the model also yielded adequate fit. As shown in Fig. 3, autoregression path coefficients were significant for anxiety symptoms, IGD, and videogame use from T1 to T2. Cross-sectional correlation coefficients were also significant both at T1 and T2 (in addition to T2 videogame use and T2 anxiety symptoms). Anxiety symptoms at T1 predicted IGD at T2 (β = 0.15, 95% CI[0.09, 0.21]) and videogame use at T2 (β = 0.09, 95% CI[0.04, 0.14]). However, videogame use (β = −0.03, 95% CI[−0.12, 0.07]) and IGD (β = 0.03, 95% CI[−0.04, 0.09]) were not predictors of anxiety symptoms from T1 to T2.
Moreover, when perceived COVID-19 impacts were included as a mediator in the model (Fig. 4), the results also suggested adequate fits. The path coefficients further indicated that anxiety symptoms at T1 were the predictors of perceived COVID-19 impacts (β = 0.29, 95% CI[0.23, 0.36]) and that perceived COVID-19 impacts were also the predictors of IGD at T2 (β = 0.12, 95% CI[0.07, 0.17]). Furthermore, the specific indirect effect of anxiety symptoms at T1→Perceived COVID impacts→IGD at T2 (a × b = 0.034, 95% CI[0.017, 0.051]), was statistically significant. Moreover, all three variables showed significant autoregression path coefficients and cross-sectional correlation coefficients (in addition to T2 videogame use and T2 anxiety symptoms). More details about covariates and other path coefficients are shown in Table S3. Depression and anxiety symptoms factors were also combined as a common latent variable to run the cross-lagged panel model. The results remained the same as the aforementioned separated models (see Figs S1 and S2).
Additional analyses
To compare model differences between children and adolescents, multiple-group analyses were conducted (restricted and unrestricted models fit comparison are shown in Table S4). For the depressive symptoms model, no effect was found for the developmental difference between the children and adolescent samples (Δχ2[13] = 7.03, p = 0.901). However, for the anxiety symptoms model, multiple-group analyses indicated a significant developmental difference (Δχ2[13] = 30.51, p = 0.004). More specifically, three paths were significantly different: (i) T1 anxiety symptoms→T2 anxiety symptoms (Wald χ2 = 4.59, p = 0.032, βchildren = 0.76 vs. βadolescents = 0.90); (ii) T1 videogame use→T2 videogame use (Wald χ2 =5.04, p = 0.025, βchildren = 0.54 vs. βadolescents = 0.65); and (iii) T2 COVID-19 impacts→T2 anxiety symptoms (Wald χ2 = 12.07, p = 0.001, βchildren = 0.30 vs. βadolescents = 0.09). Further details concerning the multiple-group path coefficients are shown in Table S5.
To compare gender differences between boys and girls, multiple-group analyses were also conducted. For the depressive symptoms model, a significant gender difference was found (Δχ2[13] = 30.59, p = 0.004). More specifically, three paths were significantly different: (i) T1 IGD→T2 IGD (Wald χ2 = 5.31, p = 0.021, βboys = 0.34 vs. βgirls = 0.47); (ii) T1 videogame use→T2 videogame use (Wald χ2 = 4.89, p = 0.027, βboys = 0.64 vs. βgirls = 0.49); and (iii) T1 depressive symptoms→T2 IGD (Wald χ2 = 7.90, p = 0.005, βboys = 0.17 vs. βgirls = 0.06). Further details concerning the multiple-group path coefficients are shown in Table S6. For the anxiety symptoms model, multiple-group analyses indicated a significant gender difference (Δχ2[13] = 27.09, p = 0.012). More specifically, three paths were significantly different: (i) T1 videogame use→T2 videogame use (Wald χ2 = 4.73, p = 0.030, βboys = 0.63 vs. βgirls = 0.48); (ii) T1 IGD→T2 IGD (Wald χ2 = 5.99, p = 0.014, βboys = 0.32 vs. βgirls = 0.47); and (iii) T1 anxiety symptoms→T2 IGD (Wald χ2 = 5.16, p = 0.023, βboys = 0.18 vs. βgirls = 0.04). Further details concerning the multiple-group path coefficients are shown in Table S7.
Discussion
The present study used a longitudinal design to investigate whether changes in videogame use and IGD severity occurred in the context of the COVID-19 pandemic. The results indicated that the amount of videogame use and IGD severity increased significantly among adolescents during the COVID-19 pandemic. Furthermore, the findings suggested that depressive and anxiety symptoms before the COVID-19 pandemic positively predicted IGD severity and videogame use during the COVID-19 pandemic, but not inversely, further supporting the compensatory hypothesis (e.g., Kardefelt-Winther, 2014). The findings were also consistent with the I-PACE model (Brand et al., 2019) and indicated that perceived COVID-19 impacts was a significant mediator in the relationship between depressive symptoms and anxiety symptoms before the COVID-19 pandemic and IGD severity during the COVID-19 pandemic.
Overall, the findings of this study were consistent with previous scholarly contentions suggesting that the COVID-19 pandemic would potentially lead to children and adolescents being more engaged with playing videogames (King et al., 2020; Király et al., 2020; Ko & Yen, 2020). The predicted increase in videogame engagement may be conceptualized as a coping mechanism that helped children and adolescents cope with the mental health burden associated with the COVID-19 pandemic because recent research examining the effects of the COVID-19 pandemic on youth mental health found that children and adolescents are prone to experiencing psychiatric disorders (Liang et al., 2020). Although it is reasonable to expect that children and adolescents may engage in increased video gaming activities to cope with pandemic-related stress, potentially rendering them more vulnerable to IGD due to greater exposure, in the present study only adolescents (and not children) increased their IGD severity during the COVID-19 pandemic. There may be a few potential developmental and parental-related factors underpinning this finding.
In terms of potential developmental factors, it is worth noting that adolescence represents a period of transition from childhood to adulthood that starts with the onset of puberty and finishes with successful parental independence (Casey & Caudle, 2013). It is well-known that adolescence is associated with increased risk for the onset of various emotional and behavioral problems, making it a critical period of vulnerability for addictive disorders (Crews, He, & Hodge, 2007; Steinberg, 2005), including IGD (Gentile et al., 2011; Peeters, Koning, & van den Eijnden, 2018). Therefore, when faced with COVID-19 pandemic-related stress, compared to children, adolescents may select negative coping strategies leading to the development of IGD via excessive and dysregulated gaming. In terms of parental-related factors, it could be that children benefitted more from the closer parental supervision received during the lockdown stage of the pandemic as they are generally more likely to obey their parents than adolescents (Lwin, Stanaland, & Miyazaki, 2008). Consequently, children may have presented with a lower risk of experiencing higher IGD severity than adolescents due to parental mediation, monitoring, and supervision.
The present study also found that pre-pandemic depressive and anxiety symptoms predicted videogame use and IGD severity during the COVID-19 pandemic. This finding provides further support to the compensatory hypothesis (Kardefelt-Winther, 2014), which proposes that IGD may develop as a dysfunctional compensation mechanism, and resulting from poorer psychological health during the pandemic period. This result was also consistent with previous meta-analytic studies (Richard, Fletcher, Boutin, Derevensky, & Temcheff, 2020) and empirical research showing that decreased psychosocial health can lead to IGD (Maroney, Williams, Thomas, Skues, & Moulding, 2019; Wartberg, Kriston, Zieglmeier, Lincoln, & Kammerl, 2019). It may be the case that the adolescents recruited presented with high levels of baseline depressive symptoms, which may have facilitated excessive gaming behaviors because longitudinal research suggests that depression and anxiety are a risk factor for IGD (Burleigh et al., 2018), which may be of particular importance during the COVID-19 pandemic period.
The present study also found that perceived COVID-19 impacts played a key mediating role in the longitudinal relationship between depressive and anxiety symptoms before the COVID-19 pandemic and IGD severity during the COVID-19 pandemic. This finding aligns with previous cross-sectional research (Duan et al., 2020; Huang & Zhao, 2020; Wang et al., 2020) suggesting that increased perceived COVID-19 impacts may elicit psychiatric disorders (Tull et al., 2020), possibly related to addictive disorders (Marsden et al., 2020) alongside depressive and anxiety disorders (Huang & Zhao, 2020). As mentioned, this finding can also be understood within the I-PACE model (Brand et al., 2019) because COVID-19 pandemic-related stress may be conceptualized as a trigger related to cognition and affect that may be affected by predisposing variables (e.g., depression and anxiety symptoms), with greater perceived COVID-19 impacts potentially leading to greater IGD severity. As supported by many previous studies on addiction (Elhai et al., 2020), the I-PACE is a robust model explaining the development of behavioral addictions, such as IGD, smartphone addiction, internet addiction, and alcohol-related addictions (Brand et al., 2019).
The present study did not find any developmental (children and adolescents) or gender (boys and girls) differences in the relationships between depressive symptoms, anxiety symptoms, and IGD. In addition to the autoregression path of videogame use and IGD from T1 to T2, there was only one significant gender difference (i.e., both depressive and anxiety symptoms at T1 suggested strong prediction to IGD at T2). More specifically, boys were more likely to be playing videogames and experiencing IGD. Here, gaming may have been utilized as a way to cope with negative affect (e.g., Blasi et al., 2019; Shi, Renwick, Turner, & Kirsh, 2019). However, other mixed findings concerning developmental and gender differences warrant further research.
The present study has several strengths. Firstly, it is the first longitudinal study, to the best of our knowledge, to examine how the COVID-19 pandemic may influence the development of IGD, depressive symptoms, and anxiety symptoms. Secondly, instead of recruiting an adult or a community-based sample, we recruited a sample of children and adolescents, providing a developmental perspective about the relationship between the mental health effects of the COVID-19 pandemic and IGD. Thirdly, we tested the mediating effect of perceived COVID-19 impacts on the link between depressive symptoms, anxiety symptoms, and subsequent IGD during the pandemic.
Notwithstanding these potential strengths, several potential limitations should be noted. Although this study was guided by the I-PACE model, only a few factors were examined. A wider range of factors should be examined within the I-PACE model, such as personality, cognitive, and motivational factors (Brand et al., 2019). Another potential limitation is that this study did not examine within-person effects (Hamaker, Kuiper, & Grasman, 2015) because we only included two waves of data to test two cross-lagged panel models. Finally, the study relied on self-report data which is subject to well-known methodological biases.
Conclusions and implications
This study adopted a longitudinal research design (albeit relatively short-term) and is the first empirical study to examine the potential effects of the COVID-19 pandemic on videogame use and IGD severity. Overall, the findings demonstrated that both videogame use and IGD severity increased significantly during the COVID-19 pandemic, especially for young adolescents. More specifically, pre-pandemic depressive and anxiety symptoms predicted greater videogame use and IGD severity during the pandemic period. These findings supported the compensatory hypothesis in the context of the pandemic. Furthermore, the results obtained provided further support for the I-PACE model (Brand et al., 2019), in which perceived COVID-19 impacts were a mediator between depression symptoms, anxiety symptoms, and IGD. In conclusion, while videogame use during the COVID-19 increased significantly for both children and adolescents, IGD may not be entirely and directly associated with the COVID-19 pandemic because only adolescents exhibited greater IGD severity during the COVID-19 pandemic in comparison to the pre-pandemic period.
Finally, the findings obtained present important clinical and preventative implications. As the COVID-19 pandemic has influenced various aspects of daily life and fueled greater mental health challenges due to the increased prevalence of psychiatric disorders (e.g., IGD, anxiety, and depression), the importance of early treatment approaches and the role of mental health services should be emphasized, particularly during a pandemic. Although playing videogames can be an effective way to cope with the mental health challenges brought about by the COVID-19 pandemic (Viana & de Lira, 2020), balancing the time spent gaming to cope with the COVID-19 is paramount (Király et al., 2020). More importantly, specific vulnerable populations such as adolescents should be focused on targeted preventative initiatives to curb addictive disorders related to technology use during a pandemic because they appear to present with greater vulnerability in comparison to children.
Funding sources
This study was supported by the Fundamental Research Funds for the Central Universities (grant numbers, SWU1909106), the China Postdoctoral Science Foundation (grant numbers, 2018M640892), and the Chongqing Special Postdoctoral Science Foundation (grant numbers, XmT2018010).
Authors' contribution
ZT and CG contributed to conception and design of the study. ZT and QN contributed to data collection and statistical analysis. HMP and QN contributed to the literature review. ZT, HMP and MDG contributed to writing of the manuscript. ZT, HMP and MDG contributed to revising the manuscript. ZT and CG provided funds to conduct the study. All authors have approved the final version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Supplementary Material
Appendix A. Supplementary material
The online version of this article offers supplementary material https://doi.org/10.1556/2006.2021.00016.
Contributor Information
Zhaojun Teng, Email: tzj450@email.swu.edu.cn.
Halley M. Pontes, Email: contactme@halleypontes.com.
Qian Nie, Email: 499787409@qq.com.
Mark D. Griffiths, Email: mark.griffiths@ntu.ac.uk.
Cheng Guo, Email: guochen@swu.edu.cn.
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- BBC . (2020). Lockdown and loaded: Coronavirus triggers video game boost . Retrieved September 3, 2020, from https://www.bbc.com/news/business-52555277.
- Blasi, M. D., Giardina, A., Giordano, C., Coco, G. L., Tosto, C., Billieux, J., et al. (2019). Problematic video game use as an emotional coping strategy: Evidence from a sample of MMORPG gamers. Journal of Behavioral Addictions, 8(1), 25–34. 10.1556/2006.8.2019.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand, M., Wegmann, E., Stark, R., Müller, A., Wölfling, K., Robbins, T. W., et al. (2019). The Interaction of Person-Affect-Cognition-Execution (I-PACE) model for addictive behaviors: Update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neuroscience & Biobehavioral Reviews, 104, 1–10. 10.1016/j.neubiorev.2019.06.032. [DOI] [PubMed] [Google Scholar]
- Brunborg, G. S., Mentzoni, R. A., & Frøyland, L. R. (2014). Is video gaming, or video game addiction, associated with depression, academic achievement, heavy episodic drinking, or conduct problems? Journal of Behavioral Addictions, 3(1), 27–32. 10.1556/jba.3.2014.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burleigh, T. L., Stavropoulos, V., Liew, L. W., Adams, B. L., & Griffiths, M. D. (2018). Depression, internet gaming disorder, and the moderating effect of the gamer-avatar relationship: An exploratory longitudinal study. International Journal of Mental Health and Addiction, 16(1), 102–124. 10.1007/s11469-017-9806-3. [DOI] [Google Scholar]
- Casey, B. J., & Caudle, K. (2013). The teenage brain: Self-control. Current Directions in Psychological Science, 22(2), 82–87. 10.1177/0963721413480170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y., Cao, Y., & Liu, Z. (2013). The application of a revised Chinese version of the State-Trait Anxiety Inventory in migrant children. Chinese Journal of Behavioral Medicine and Brain Science, 22(8), 755–757. 10.3760/cma.j.issn.1674-6554.2013.08.025. [DOI] [Google Scholar]
- Cheng, C., Cheung, M. W. L., & Wang, H. Y. (2018). Multinational comparison of internet gaming disorder and psychosocial problems versus well-being: Meta-analysis of 20 countries. Computers in Human Behavior, 88, 153–167. 10.1016/j.chb.2018.06.033. [DOI] [Google Scholar]
- Chen, Z. Y., Yang, X. D., & Li, X. Y. (2009). Psychometric features of CES-D in Chinese adolescents. Chinese Journal of Clinical Psychology, 17(4), 443–445. [Google Scholar]
- Crews, F., He, J., & Hodge, C. (2007). Adolescent cortical development: A critical period of vulnerability for addiction. Pharmacology Biochemistry and Behavior, 86(2), 189–199. 10.1016/j.pbb.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan, L., Shao, X., Wang, Y., Huang, Y., Miao, J., Yang, X., et al. (2020). An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. Journal of Affective Disorders. 275, 112–118. 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai, J. D., Yang, H., McKay, D., & Asmundson, G. J. (2020). COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. Journal of Affective Disorders. 274, 576–582. 10.1016/j.jad.2020.05.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders, C. K. (2010). Applied missing data analysis . New York: Guilford Press. [Google Scholar]
- Fitzpatrick, K. M., Harris, C., & Drawve, G. (2020). Living in the midst of fear: Depressive symptomatology among US adults during the COVID‐19 pandemic. Depression and Anxiety, 37(10), 957–964. 10.1002/da.23080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentile, D. A., Choo, H., Liau, A., Sim, T., Li, D., Fung, D., et al. (2011). Pathological video game use among youths: A two-year longitudinal study. Pediatrics, 127(2), e319–e329. 10.1542/peds.2010-1353. [DOI] [PubMed] [Google Scholar]
- González-Bueso, V., Santamaría, J. J., Fernández, D., Merino, L., Montero, E., & Ribas, J. (2018). Association between internet gaming disorder or pathological video-game use and comorbid psychopathology: A comprehensive review. International Journal of Environmental Research and Public Health, 15(4), 668. 10.3390/ijerph15040668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker, E. L., Kuiper, R. M., & Grasman, R. P. P. P. (2015). A critique of the cross-lagged panel model. Psychological Methods, 20(1), 102–116. 10.1037/a0038889. [DOI] [PubMed] [Google Scholar]
- Holmes, E. A., O'Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., et al. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y., & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research, 288, 112954. 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong, H., Yim, H. W., Lee, S. Y., Lee, H. K., Potenza, M. N., Jo, S. J., et al. (2019). Reciprocal relationship between depression and internet gaming disorder in children: A 12-month follow-up of the iCURE study using cross-lagged path analysis. Journal of Behavioral Addictions, 8(4), 725–732. 10.1556/2006.8.2019.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, L., Ma, S., Chen, M., Yang, J., Wang, Y., Li, R., et al. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain, Behavior, and Immunity, 87, 11–17. 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kardefelt-Winther, D. (2014). A conceptual and methodological critique of internet addiction research: Towards a model of compensatory internet use. Computers in Human Behavior, 31, 351–354. 10.1016/j.chb.2013.10.059. [DOI] [Google Scholar]
- King, D. L., & Delfabbro, P. H. (2016). The cognitive psychopathology of Internet gaming disorder in adolescence. Journal of Abnormal Child Psychology, 44(8), 1635–1645. 10.1007/s10802-016-0135-y. [DOI] [PubMed] [Google Scholar]
- King, D. L., Delfabbro, P. H., Billieux, J., & Potenza, M. N. (2020). Problematic online gaming and the COVID-19 pandemic. Journal of Behavioral Addictions. 9(2), 184–186. 10.1556/2006.2020.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Király, O., Potenza, M. N., Stein, D. J., King, D. L., Hodgins, D. C., Saunders, J. B., et al. (2020). Preventing problematic internet use during the COVID-19 pandemic: Consensus guidance. Comprehensive Psychiatry, 100, 152180. 10.1016/j.comppsych.2020.152180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko, C. H., & Yen, J. Y. (2020). Impact of COVID-19 on gaming disorder: Monitoring and prevention. Journal of Behavioral Addictions, 9(2), 187–189. 10.1556/2006.2020.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krossbakken, E., Pallesen, S., Mentzoni, R. A., King, D. L., Molde, H., Finserås, T. R., et al. (2018). A cross-lagged study of developmental trajectories of video game engagement, addiction, and mental health. Frontiers in Psychology, 9, 2239. 10.3389/fpsyg.2018.02239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, L., Ren, H., Cao, R., Hu, Y., Qin, Z., Li, C., et al. (2020). The effect of COVID-19 on youth mental health. Psychiatric Quarterly, 91(3), 841–852. 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, D., Liau, A., & Khoo, A. (2011). Examining the influence of actual-ideal self discrepancies, depression, and escapism, on pathological gaming among massively multiplayer online adolescent gamers. Cyberpsychology, Behavior, and Social Networking, 14(9), 535–539. 10.1089/cyber.2010.0463. [DOI] [PubMed] [Google Scholar]
- Liu, L., Yao, Y. W., Li, C. S. R., Zhang, J. T., Xia, C. C., Lan, J., et al. (2018). The comorbidity between internet gaming disorder and depression: Interrelationship and neural mechanisms. Frontiers in Psychiatry, 9, 154. 10.3389/fpsyt.2018.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lwin, M. O., Stanaland, A. J., & Miyazaki, A. D. (2008). Protecting children's privacy online: How parental mediation strategies affect website safeguard effectiveness. Journal of Retailing, 84(2), 205−217. 10.1016/j.jretai.2008.04.004. [DOI] [Google Scholar]
- Maroney, N., Williams, B. J., Thomas, A., Skues, J., & Moulding, R. (2019). A stress-coping model of problem online video game use. International Journal of Mental Health and Addiction, 17(4), 845−858. 10.1007/s11469-018-9887-7. [DOI] [Google Scholar]
- Marsden, J., Darke, S., Hall, W., Hickman, M., Holmes, J., Humphreys, K., et al. (2020). Mitigating and learning from the impact of COVID-19 infection on addictive disorders. Addiction, 115(6), 1007−1010. 10.1111/add.15080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeish, D., Stapleton, L. M., & Silverman, R. D. (2017). On the unnecessary ubiquity of hierarchical linear modeling. Psychological Methods, 22(1), 114−140. 10.1037/met0000078. [DOI] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (1998-2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Peeters, M., Koning, I., & van den Eijnden, R. (2018). Predicting internet gaming disorder symptoms in young adolescents: A one-year follow-up study. Computers in Human Behavior, 80, 255−261. 10.1016/j.chb.2017.11.008. [DOI] [Google Scholar]
- Pfefferbaum, B., & North, C. S. (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383, 510−512. 10.1056/nejmp2008017. [DOI] [PubMed] [Google Scholar]
- Pontes, H. M., & Griffiths, M. D. (2015). Measuring DSM-5 Internet gaming disorder: Development and validation of a short psychometric scale. Computers in Human Behavior, 45, 137−143. 10.1016/j.chb.2014.12.006. [DOI] [Google Scholar]
- Pontes, H. M., & Griffiths, M. D. (2019). A new era for gaming disorder research: Time to shift from consensus to consistency. Addictive Behaviors, 103, 106059. 10.1016/j.addbeh.2019.106059. [DOI] [PubMed] [Google Scholar]
- Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), e100213. 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard, J., Fletcher, É., Boutin, S., Derevensky, J., & Temcheff, C. (2020). Conduct problems and depressive symptoms in association with problem gambling and gaming: A systematic review. Journal of Behavioral Addictions. 9(3), 497–533 10.1556/2006.2020.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoemann, A. M., Boulton, A. J., & Short, S. D. (2017). Determining power and sample size for simple and complex mediation models. Social Psychological and Personality Science, 8(4), 379–386. 10.1177/1948550617715068. [DOI] [Google Scholar]
- Shanahan, L., Steinhoff, A., Bechtiger, L., Murray, A., Nivette, A., Hepp, U., et al. (2020). Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine. Advance online publication. 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shek, D. T. (1993). The Chinese version of the State‐Trait Anxiety Inventory: Its relationship to different measures of psychological well-being. Journal of Clinical Psychology, 49(3), 349–358. [DOI] [PubMed] [Google Scholar]
- Shi, J., Renwick, R., Turner, N. E., & Kirsh, B. (2019). Understanding the lives of problem gamers: The meaning, purpose, and influences of video gaming. Computers in Human Behavior, 97, 291−303. 10.1016/j.chb.2019.03.023. [DOI] [Google Scholar]
- Snodgrass, J. G., Lacy, M. G., Dengah, H. F., Eisenhauer, S., Batchelder, G., & Cookson, R. J. (2014). A vacation from your mind: Problematic online gaming is a stress response. Computers in Human Behavior, 38, 248−260. 10.1016/j.chb.2014.06.004. [DOI] [Google Scholar]
- Steinberg, L. (2005). Cognitive and affective development in adolescence. Trends in Cognitive Sciences, 9(2), 69−74. 10.1016/j.tics.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Teng, Z., Nie, Q., Guo, C., Zhang, Q., Liu, Y., & Bushman, B. J. (2019). A longitudinal study of link between exposure to violent video games and aggression in Chinese adolescents: The mediating role of moral disengagement. Developmental Psychology, 55(1), 184–195. 10.1037/dev0000624. [DOI] [PubMed] [Google Scholar]
- Teng, Z., Pontes, H. M., Nie, Q., Xiang, G., Griffiths, M. D., & Guo, C. (2020). Internet gaming disorder and psychological well-being: A longitudinal study of older-aged adolescents and emerging adults. Addictive Behaviors, 110, 106530. 10.1016/j.addbeh.2020.106530. [DOI] [PubMed] [Google Scholar]
- Tull, M. T., Edmonds, K. A., Scamaldo, K., Richmond, J. R., Rose, J. P., & Gratz, K. L. (2020). Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Research, 289, 113098. 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viana, R. B., & de Lira, C. A. B. (2020). Exergames as coping strategies for anxiety disorders during the COVID-19 quarantine period. Games for Health Journal, 9(3), 147–149. 10.1089/g4h.2020.0060. [DOI] [PubMed] [Google Scholar]
- Wang, G., Zhang, Y., Zhao, J., Zhang, J., & Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet, 395(10228), 945–947. 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wartberg, L., Kriston, L., Zieglmeier, M., Lincoln, T., & Kammerl, R. (2019). A longitudinal study on psychosocial causes and consequences of Internet gaming disorder in adolescence. Psychological Medicine, 49(2), 287–294. 10.1017/S003329171800082X. [DOI] [PubMed] [Google Scholar]
- Wichstrøm, L., Stenseng, F., Belsky, J., von Soest, T., & Hygen, B. W. (2019). Symptoms of internet gaming disorder in youth: Predictors and comorbidity. Journal of Abnormal Child Psychology, 47(1), 71–83. 10.1007/s10802-018-0422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). #HealthyAtHome – mental health. Retrieved September 3, 2020, from: https://www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health.