Abstract
Background and aims
The World Health Organization included gaming disorder (GD) in the eleventh revision of International Classification of Diseases in 2019. Due to the lack of diagnostic tools for GD, a definition has not been adequately applied. Therefore, this study aimed to apply an operationalized definition of GD to treatment-seekers. The relationship between the diagnoses of GD and Internet gaming disorder (IGD) in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders was also examined.
Methods
Study participants comprised 241 treatment-seekers who had engaged in excessive gaming and experienced related problems. Psychiatrists applied the GD diagnostic criteria to the participants using a diagnostic form developed for this study. Information on gaming behavior and functional impairment was obtained through face-to-face interviews conducted by clinical psychologists.
Results
In total, 78.4 and 83.0% of the participants fulfilled the GD and IGD diagnostic criteria, respectively. The sensitivity and specificity of GD diagnosis were both high when the IGD diagnosis was used as the gold standard. Participants with GD preferred online PC and console games, spent significantly more time gaming, and showed a higher level of functional impairment compared to those who did not fulfill the GD diagnostic criteria.
Discussion and Conclusion
The definition of GD can be successfully applied to treatment-seekers with excessive gaming and related problems. A high concordance of GD and IGD diagnoses was found in those participants with relatively severe symptoms. The development and validation of a diagnostic tool for GD should be explored in future studies.
Keywords: applicability, functional impairment, gaming disorder, Internet gaming disorder, treatment-seeker
Introduction
The World Health Organization (WHO) officially included gaming disorder (GD) as a disorder due to addictive behavior in the eleventh revision of the International Classification of Diseases (ICD-11) in May 2019 (WHO, 2019). The decision for inclusion was based on accumulated evidence and intensive discussion among experts from all over the world (Saunders et al., 2017; WHO, 2016b). According to the definition of GD in ICD-11, three clinical manifestation criteria and one functional impairment criterion need to be met in order to make a diagnosis of GD (WHO, 2019). The first three criteria are: (1) impaired control over gaming, (2) increasing prioritization of gaming in life, and (3) continuation of gaming despite negative consequences. Functional impairment needs to be sufficiently severe in personal, familial, social, educational, occupational, or other important areas of functioning. In addition, these behavior patterns and impairments have to persist for at least 12 months, except in the case of severe symptoms. Prior to inclusion in the ICD-11, diagnostic criteria for Internet gaming disorder (IGD) were published by the American Psychiatric Association in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013 (American Psychiatric Association, 2013). These consisted of nine criteria, at least five of which need to be met to make a diagnosis of IGD. However, these criteria were regarded as preliminary and placed in Section III (“Conditions for further study”).
The ICD is the foundation of the identification of health trends and statistics globally, and the international standard for reporting diseases and health conditions (WHO, 2019). Since the disclosure of diagnostic criteria in 2013, research evidence on IGD has been accumulated in epidemiology (Fam, 2018; Mihara & Higuchi, 2017), neurobiology (Fauth-Bühler & Mann, 2017; Kuss, Pontes, & Griffiths, 2018), clinical assessment (King et al., 2020), treatment (King et al., 2017; Zajac, Ginley, & Chang, 2020), and policy and prevention (Király et al., 2018). However, research on GD has just started, and studies specifically focused on GD, especially clinical studies, are scarce. Against this background, it remains a topic for debate whether sufficient scientific evidence has been presented to justify the inclusion of GD in the ICD-11 (Aarseth et al., 2017; van Rooij et al., 2018). Studies published after the inclusion of GD in the ICD-11 often regard GD and IGD as the same clinical entity. However, the diagnostic criteria of GD and IGD differ, and further study of the relationship between the two is required, including the use of clinical sample groups.
Two studies have sought to apply the definition of GD to clinical samples by examining the relationship between GD and IGD diagnoses. Ko, Lin, Lin, and Yen (2019) recruited participants with IGD, regular gamers, and controls through campus advertisements at a university in Taiwan. Diagnostic evaluations of IGD and GD were carried out based on direct interviews. They reported the diagnostic validity of each criterion for IGD and evaluated functional impairment and unhealthy behaviors among participants with IGD and GD. Another study was conducted in Korea as part of a clinical cohort study (Jo et al., 2019). The individuals who participated in the cohort were divided into three groups—normal, IGD only, and IGD+GD—and then were compared in terms of Internet use patterns, addiction characteristics, and comorbidities.
Those studies focused on the fulfillment of each IGD criterion for the participants and examined their diagnostic status, addictive behaviors, and related problems. To evaluate the diagnostic validity of IGD, the former study developed a semi-structured interview schedule (Ko et al., 2019), while the latter used the Diagnostic Interview for Internet Addiction (Ryu et al., 2019). However, neither study used the exact same criteria for GD or showed how each GD criterion was met. In addition, the participants in these studies were not seeking treatment for GD. As mentioned, the ICD is in use worldwide and serves as the diagnostic classification standard for clinical and research purposes (WHO, 2019). Therefore, it is essential to evaluate the applicability of the GD definition to treatment-seekers because appropriate treatment is predicated on an accurate diagnosis.
In this context, the purpose of this study was twofold. The primary aim was to examine the applicability of the GD definition to treatment-seekers. First, we developed a short-form interview to examine the criteria described in the definition of GD, based on a meeting report of WHO (WHO, 2016b). The relationship between GD and IGD diagnoses was also examined. Second, we investigated online applications and devices used, time spent on gaming, and functional impairment due to gaming in treatment-seekers with GD. These results were compared with those for treatment-seekers who had excessive gaming but who failed to meet the diagnostic threshold for GD.
Methods
Participants
The study participants were 269 consecutive new patients who visited the specialist clinic for Internet addiction at our center for treatment between November 2016 and August 2018. Those whose primary issue was excessive online and/or offline gaming were included in the study (N = 241; 89.6% of the original sample), whereas the remaining 28, whose main issues were related to applications other than gaming, were excluded.
Instruments for making diagnoses
To make a diagnosis of GD based on the ICD-11, we used the ICD-11 beta draft released in October 2016 (WHO, 2016a). The content of the definition in the beta version essentially mirrors that of the final version (WHO, 2016a, 2019). As no published instrument for making a diagnosis of GD based on the ICD-11 was available when we began the data collection, we developed a new instrument specifically for this study. To evaluate how well a participant met the clinical manifestation criteria, we used the three criteria that had been proposed by WHO and were subsequently published in a meeting report (WHO, 2016b). We used one criterion to evaluate the first clinical manifestation – impaired control over gaming. To evaluate the remaining two clinical manifestations accurately, we divided each criterion proposed by the WHO into two sub-criteria. Each criterion was considered to be met when at least one sub-criterion of the respective criterion was met. To evaluate the functional impairment criterion, we used the identical criterion described in the 2016 beta draft version of the ICD-11 (WHO, 2016a).
A previous study suggested that the cutoff level for GD was overly stringent and may be, at least partially responsible for a low concordance between GD and IGD in samples (Jo et al., 2019). If this is true, it may result in an underdiagnosis of individuals with problems caused by excessive gaming. In consideration of this notion, this study offered a provisional definition of GD with a less stringent cutoff, which is referred to as “gaming disorder-revised (GDR)”, and applied this to the participants. For the GDR, at least two criteria from the three clinical manifestation criteria need to be met. The functional impairment criterion remained essential because this is regarded as a key criterion that prevents overpathologizing gaming behavior (Billieux et al., 2017; Billieux, Schimmenti, Khazaal, Maurage, & Heeren, 2015).
For each criterion and sub-criterion met, the duration was also evaluated. We used the Japanese version of this instrument (the English version is provided in APPENDIX). For the purposes of this study, we used the Japanese version of the DSM-5 criteria for IGD (American Psychiatric Association, 2013).
Procedures
Upon their first visit to our center, trained clinical psychologists conducted interviews with treatment-seekers and their families to obtain background information and medical histories. This information included demographic characteristics, internet usage and gaming habits, and problems associated with excessive internet usage and gaming habits. For this purpose, we developed a formatted instrument. Next, psychiatrists, who were experts in GD, conducted interviews with treatment-seekers and their families and made diagnoses of ICD-11 GD and DSM-5 IGD using the aforementioned instruments.
Statistical analysis
The data obtained were uploaded and analyzed. Categorical and continuous data were compared using the chi-squared test and t-test, respectively. Cronbach's alpha was used to evaluate the internal consistency of the ICD-11 GD definition and DSM-5 IGD criteria. The level of statistical significance was set at 0.05. All analyses were conducted using the Statistical Analysis System, Version 9.4 (SAS Institute Inc., 2016).
Ethics
This study was approved by the Ethics Committee of the Kurihama Medical and Addiction Center (Approval No. 362). Data analyzed in this study was obtained as part of the basic information gathered in the course of individuals' medical treatment and therefore, informed consent was not obtained at the time the information was collected. The use of these data for research purposes has been communicated via the center's website. Those who declined to participate in the study were excluded from this study.
Results
Background characteristics of the participants
Table 1 shows the participants' background characteristics by ICD-11 GD status (the results regarding GD status are described in the next section). Treatment-seekers who were diagnosed as having ICD-11 GD were classified as the GD group, while those whose main issue was excessive gaming, but who did not meet the GD definition, were classified as the non-GD group. Although there were substantial overlaps, the 28 participants whose main issues were related to non-gaming applications instead made excessive use of information searches (64%), social networking sites (SNS) (39%), and video viewing (61%). As shown in the table, no difference was found with regard to age, gender ratio, distribution of marital status and occupation, onset age of internet use, or offline or online gaming, between the GD and non-GD groups. However, age and the onset age of internet use were older in the “Other than gaming group” compared to the GD and non-GD groups.
Table 1.
Characteristics of treatment-seekers
| Characteristics | Main applications involving addiction or excessive use | ||
| Gaming (N = 241) | Other than gaming (N = 28) | ||
| GD (N = 189)a | Non-GD (N = 52)b | ||
| Gender | |||
| Male | 171 (90.5%) | 44 (84.6%) | 24 (85.7%) |
| Age (years) | |||
| Mean (SD) | 18.2 (7.4) | 19.3 (7.6) | 22.6 (14.1)c |
| Range | 9–66 | 8–41 | 11–77 |
| Marital status | |||
| Married | 5 (2.7%) | 2 (3.9%) | 3 (10.7%) |
| Widowed | 0 (0.0%) | 1 (1.9%) | 0 (0.0%) |
| Divorced | 1 (0.5%) | 0 (0.0%) | 1 (3.6%) |
| Unmarried | 183 (96.8%) | 49 (94.2%) | 24 (85.7%) |
| Occupation (%) | |||
| Full-time worker | 5 (2.7%) | 2 (3.9%) | 3 (10.7%) |
| Part-time worker | 7 (3.7%) | 9 (17.3%) | 1 (3.6%) |
| Student | 144 (76.2%) | 34 (65.4%) | 18 (64.3%) |
| Unemployed | 31 (16.4%) | 6 (11.5%) | 5 (17.9%) |
| Other | 2 (1.1%) | 1 (1.9%) | 1 (3.6%) |
| Onset age of internet use (years) | |||
| Mean (SD) | 10.9 (4.9) | 11.0 (3.9) | 13.9 (11.8)c |
| Onset age of offline gaming (years) | |||
| Mean (SD) | 7.3 (2.6) | 7.4 (3.3) | 8.4 (3.3) |
| Onset age of online gaming (years) | |||
| Mean (SD) | 13.4 (5.7) | 14.1 (5.6) | 16.3 (8.3) |
Note. GD = gaming disorder; ICD-11 = eleventh revision of the International Classification of Diseases; SD = standard deviation.
Treatment-seekers who were diagnosed with ICD-11 gaming disorder.
Treatment-seekers with excessive gaming who did not meet the ICD-11 criteria for gaming disorder.
Mean age and the onset age of internet use of this group were significantly older than those in the other two groups (P = 0.0341 and P = 0.0365, respectively).
Application of the GD definition and IGD criteria
The results of applying the ICD-11 GD definition and the DSM-5 IGD criteria to treatment-seekers whose main issue was excessive gaming are summarized in Table 2. Cronbach's alphas for GD and IGD were 0.886 and 0.873, respectively. The first and third ICD-11 GD criteria were met by 93.0% of the participants, whereas the rate of participants who met the second criterion was somewhat lower (81.3%). The functional impairment criterion was met by 86.3% of the participants. As a result, 78.4% of the participants met all four criteria, meaning that they were diagnosed as having ICD-11 GD. If the GDR criteria were applied, 84.2% of the participants fulfilled the diagnostic criteria. Although the data are not shown, the duration of GD before the first visit to our center was also examined. The duration was defined as the length of time for which all four criteria were met. The majority of treatment-seekers with GD (82.5%) had a duration of 12 months or longer, while 4.2% had less than 6 months and 13.2% between 6 and 11 months.
Table 2.
The rate of treatment-seekers engaging in excessive gaming who met each diagnostic criterion of ICD-11 GD definition and DSM-5 IGDa
| N = 241% | |||
| ICD-11 GD definition | % | ||
| 1 | Impaired control over gaming | 93.0% | |
| 2 | Increasing prioritization of gaming in life | 81.3% | |
| 3 | Continuation of gaming despite negative consequences | 93.0% | |
| 4 | Functional impairment due to gaming | 86.3% | |
| GD diagnosis (all four criteria met) | 78.4% | ||
| GD diagnosis (at least two of the first three criteria and criterion 4 met) | 84.2% | ||
| DSM-5 IGD criteria | % | ||
| 1 | Preoccupation | 78.8% | |
| 2 | Withdrawal symptoms | 60.6% | |
| 3 | Tolerance | 68.9% | |
| 4 | Unsuccessful control of participation in Internet gaming | 91.7% | |
| 5 | Loss of interest in other activities | 85.4% | |
| 6 | Excessive use despite knowledge of psychosocial problems | 87.6% | |
| 7 | Deception | 68.5% | |
| 8 | Escaping or relieving a negative mood | 48.6% | |
| 9 | Jeopardizing or loss of opportunities | 84.2% | |
| IGD diagnosis | 83.0% | ||
Note. GD = gaming disorder; ICD-11 = eleventh revision of the International Classification of Diseases; IGD=Internet gaming disorder; DSM-5= Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Each item of ICD-11 GD and DSM-5 IGD is abbreviated.
With regard to the DSM-5 IGD criteria, four criteria—“unsuccessful control”, “loss of interest in other activities”, “excessive use despite knowledge of problems”, and “loss of opportunities”—were met by higher percentages of participants, ranging between 84% and 92%. However, criteria such as “mood modification”, “withdrawal symptoms”, “tolerance”, and “deception” were met by lower percentages of participants. Notably, the percentage for “mood modification” was less than 50%. As a result, 83.0% of the participants were diagnosed as having DSM-5 IGD, which was slightly higher than the rate for ICD-11 GD.
The concordance between the diagnoses of ICD-11 GD and DSM-5 was fairly high (Table 3A and 3B). If the IGD criteria was used as the gold standard, the sensitivity and specificity of the GD criteria were 0.940 and 0.976, respectively. In the case of the less stringent cutoff (GDR), the sensitivity was comparable with that of GD, but the specificity decreased to 0.805.
Table 3A.
Concordance of the diagnoses of ICD-11 GD and DSM-5 IGD for treatment-seekers engaged in excessive gaming
| DSM-5 IGDc | ||||
| IGD | Non-IGD | Total | ||
| ICD-11 GDa | GD | 188 | 1 | 189 |
| Non-GD | 12 | 40 | 52 | |
| ICD-11 GDRb | GDR | 195 | 8 | 203 |
| Non-GDR | 5 | 33 | 38 | |
| Total | 200 | 41 | 241 | |
GD are treatment-seekers who met the four ICD-11 GD criteria and non-GD are those who did not.
GDR are treatment-seekers who met at least two of the three clinical manifestation criteria and functional impairment criterion, and non-GDR are those who did not.
IGD are those who met the diagnostic criteria for DSM-5 IGD and non-IGD are those who did not.
Table 3B.
Sensitivity, specificity, and positive and negative predictive values of GD and GDR when IGD diagnosis was used as the gold standarda
| GDb | GDRc | |
| Sensitivity | 0.940 (0.898–0.969) | 0.975 (0.943–0.992) |
| Specificity | 0.976 (0.871–0.999) | 0.805 (0.651–0.911) |
| Positive predictive value | 0.995 (0.971–0.999) | 0.961 (0.924–0.983) |
| Negative predictive value | 0.769 (0.632–0.847) | 0.868 (0.719–0.956) |
Values in parentheses are 95% confidence intervals.
GD are treatment-seekers who met the four ICD-11 GD criteria.
GDR are treatment-seekers who met at least two of the three clinical manifestation criteria and the functional impairment criterion.
Types of applications and electronic devices
As shown in Table 4, responses to the multiple-choice questions regarding the types of applications and electronic devices used were in the form of percentages. Therefore, the percentage for each response item totaled less than 100% for each question. The percentage of participants in the GD group who played online games using devices other than a smartphone was significantly higher than the percentage of those in the non-GD group who played online games using the same device (65.5% vs 40.4%, P = 0.0010). Conversely, the rate of participants in the non-GD group who played online games using a smartphone tended to be higher than that in the GD group (64.6% vs 78.9%, P = 0.0923). Offline games were played by only about one-third of the participants in both groups. Although the main problem for the GD and non-GD groups was excessive gaming, they both frequently used other online applications. The highest percentage observed in both groups was for video viewing. In addition, the percentages of those demonstrating excessive use of information searches and SNS were relatively high in both groups.
Table 4.
Types of applications and electronic devices used by GD status
| GD status | P-valued | ||
| GDa (N = 189) | Non-GDb (N = 52) | ||
| Types of applicationsc | |||
| Information search and electronic bulletin boards | 76.2% | 75.0% | NS |
| E-mail, chat, Skype, and Messenger | 43.4% | 48.1% | NS |
| SNS | 78.3% | 67.3% | NS |
| Online games (other than a smartphone, including PCs and game machines) | 65.6% | 40.4% | 0.0010 |
| Online games (smartphone) | 64.6% | 78.9% | 0.0923 |
| Offline games | 33.3% | 34.6% | NS |
| Video viewing | 90.5% | 94.2% | NS |
| Types of electronic devicesc | |||
| PC | 52.9% | 57.7% | NS |
| Tablet PC | 26.5% | 26.9% | NS |
| Game console | 45.0% | 46.2% | NS |
| Smartphone | 76.7% | 82.7% | NS |
| Feature phone | 10.1% | 5.8% | NS |
| Music player | 9.5% | 9.6% | NS |
Note. NS = Not statistically significant.
GD: Treatment-seekers who were diagnosed with ICD-11 gaming disorder.
Non-GD: Treatment-seekers with excessive gaming who did not meet the ICD-11 criteria for gaming disorder.
Multiple choice questions and percentages do not total 100%.
Results of the 2 × 2 chi-squared tests.
The distribution of each type of electronic device was similar between the two groups. Smartphones were used most frequently in both groups, followed by PCs and game consoles.
Time spent on gaming
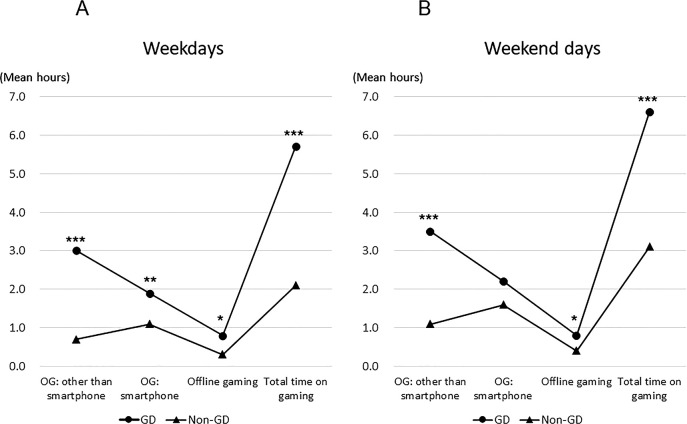
Figure 1 shows the mean hours spent on different types of gaming by ICD-11 GD status. On weekdays, the GD group spent significantly more time on different types of gaming and gaming overall than did the non-GD group (Fig. 1A). For example, the GD group spent 3.0 hours on online gaming using devices other than a smartphone compared with 0.7 hours for the non-GD group. The total time spent on gaming was 5.7 and 2.0 hours for the GD and non-GD groups, respectively. The mean time spent on gaming tended to be longer on weekend days than on weekdays (Fig. 1B). The mean total time spent on gaming on a weekend day was as high as 6.6 hours for the GD group and 3.1 hours for the non-GD group.
Fig. 1.
Average daily hours spent on each type of gaming on a weekday (A) and weekend day (B) by gaming disorder (GD) status. OG = online gaming. *P < 0.05, **P < 0.01, ***P < 0.001
Functional impairment
Table 5 shows the results of a comparison in occurrence rates of a set of problems associated with excessive gaming 6 months prior to the first visit between the GD and non-GD groups. As shown in the table, “50% or more in 6 months” implies that a problem persisted for a total of 3 months or more in the previous 6 months. The occurrence rate for each problem tended to be higher in the GD than in the non-GD group, and in the former this was surprisingly high. For, example, more than 80% reported being unable to wake up in the morning for a period of 3 months or more in the previous 6 months. This was followed by “Day–night reversal” (62%), “Poor school grades or work performance” (57%), “Hitting and/or breaking things” (55%), and “Absence from school or work” (51%). “Hitting and/or breaking things” and “Physical violence” usually occurred when the participants were instructed to stop or reduce their gaming activities, when gaming devices were removed, or when their online connection was turned off. All participants in the GD group and all but 4 participants in the non-GD group experienced at least one problem listed in Table 5. Moreover, these 4 participants in the non-GD group showed at least loss of control over gaming among the four diagnostic criteria of GD.
Table 5.
Prevalence of problems associated with excessive gaming in the previous 6 months by ICD-11 GD status
| List of problems | GD status | P-valuec | ||
| GDa (N = 189) | Non-GDb (N = 52) | |||
| 1 | Unable to wake up in the morning (50% or more in 6 months) | 80.4% | 58.8% | 0.0014 |
| 2 | Day–night reversal (50% or more in 6 months) | 62.4% | 37.3% | 0.0013 |
| 3 | Poor school grades or work performance | 56.6% | 37.3% | 0.0140 |
| 4 | Hitting and/or breaking things or verbal abuse of a family member | 54.5% | 60.8% | NS |
| 5 | Absent from school or work (50% or more in 6 months) | 50.8% | 27.5% | 0.0030 |
| 6 | Not consuming meals regularly | 49.7% | 31.4% | 0.0195 |
| 7 | Poor relationships with friends | 31.8% | 19.6% | NS |
| 8 | Socially withdrawing (50% or more in 6 months) | 30.9% | 21.6% | NS |
| 9 | Physical abuse of a family member | 29.7% | 19.6% | NS |
| 10 | Late for school or work (50% or more in 6 months) | 18.6% | 11.8% | NS |
| 11 | Spending too much money on items | 13.2% | 21.6% | NS |
Note. NS=Not statistically significant.
GD: Treatment-seekers who were diagnosed with ICD-11 gaming disorder.
Non-GD: Treatment-seekers with excessive gaming who did not meet the ICD-11 criteria for gaming disorder.
Results of the 2 × 2 chi-squared tests.
Discussion
Application of GD and IGD criteria to treatment-seekers
A fairly high rate of treatment-seekers whose primary issue was excessive gaming met the criteria for impaired control over gaming, continuation of gaming despite negative consequences, and functional impairment due to gaming. The criterion for increasing priority given to gaming was met by the lowest rate of treatment-seekers, which increased the diagnostic threshold of the GD criteria. However, all four criteria were met at relatively high rates and did not significantly differ. Colder Carras et al. (2018) recruited two focus groups of gamers and let them discuss and rank the criteria in order of conceptual importance. The strongest concurrence found with regard to the participants' rankings of four criteria for DSM-5 IGD was comparable to that for GD. These findings, combined with our data, support the diagnostic validity of the GD criteria.
Next, we applied the less stringent cutoff, GDR, to the participants. A modest increase in the prevalence of GD, from 78.4 to 84.2%, was observed. One of the reasons for this was the relatively severe symptoms of the treatment-seekers, and the fact that each clinical manifestation criterion was met by more than 80% of the participants. If the revised criteria were used for less severely affected groups of gamers, the differences between the prevalence of GD and GDR may be much larger; a subject for exploration in future studies.
With regard to meeting the diagnostic criteria for DSM-5 IGD, relatively high rates (higher than 80%) were observed for unsuccessful control, loss of interest, excessive use despite problems, and jeopardizing or loss of opportunities. These criteria were comparable to the four GD criteria and those ranked highly by gamers for conceptual importance (Colder Carras et al., 2018).
Withdrawal and tolerance are basic physiological responses that occur during the process of neuroadaptation when an addictive substance acts on the brain. These were included as DSM-5 IGD criteria which proved controversial among experts in addiction (Griffiths et al., 2016). Unlike previous studies involving clinical samples, the rates for meeting the criteria for withdrawal and tolerance in this study were relatively low (Jo et al., 2019; Ko et al., 2019; Müller, Beutel, Dreier, & Wölfling, 2019). Withdrawal symptoms are sometimes confused with the negative emotions arising from gaming being suddenly stopped by external forces, and can therefore be difficult to detect. Regarding tolerance, the time spent on gaming often fluctuates among individuals with GD, and the timing and duration are sometimes regulated not by an urge to play, but rather, by the availability of their online gaming friends. To evaluate withdrawal and tolerance accurately, individuals' symptoms should be more clearly defined, and more sophisticated instruments developed to identify them.
A definition of “hazardous gaming” is included in ICD-11 (WHO, 2019). It refers to a pattern of gaming that appreciably increases the risk of harmful physical or mental health consequences and the increased risk from frequency of gaming, amount of time spent on these activities, the adverse consequences of gaming, or from others (WHO, 2019). Although not clearly stated in ICD-11, GD and hazardous gaming are mutually exclusive diagnostic entities. If these conditions are applied to the study participants, those belonging to the non-GD group seem to fulfill the definition of hazardous gaming, because they are not diagnosed with GD but at least showed either adverse consequences of gaming or loss of control over gaming. However, this group is close to the GD group in the representation of symptoms related to excessive gaming, and therefore, may constitute a severe manifestation of hazardous gaming. Needless to say, future studies are warranted to more fully elucidate this diagnostic entity.
Relationship between GD and IGD diagnoses
Although the content of the criteria and scoring methods differed, the concordance between GD and IGD diagnoses was fairly high. High concordance was found not only for the GD, but also the GDR criteria, although the former tended to be superior when sensitivity and specificity were taken into account. However, this high concordance has not been found in previous studies. For example, Ko et al. (2019) reported that the percentage of participants with IGD who were also diagnosed as having GD was 63.8%, and Jo et al. (2019) reported a much lower rate (16.4%). The corresponding figure for having GD in our study was 94.0%.
One obvious reason for the discrepancy between our findings and those of previous studies is the difference in evaluating the diagnosis of ICD-11 GD. Two previous studies used four IGD criteria (the fourth, fifth, sixth, and ninth criteria), in which all four had to be met to make a diagnosis of GD (Jo et al., 2019; Ko et al., (2019)). However, these criteria are not identical to the four GD criteria, especially the fifth and sixth IGD criteria. Another possible reason may be related to the characteristics of the study participants. The participants in this study were treatment-seekers with excessive gaming and related problems who visited a specialist clinic for internet addiction and had severe symptoms. The ninth IGD criterion which evaluated the presence of functional impairments was met by 84% of the participants, and this finding was reflected by the relatively high prevalence of both GD and IGD among the study participants. Jo et al. (2019) reported that the rate of meeting the ninth IGD criterion was quite low - 23% of participants with IGD or both IGD and GD. This explains the low concordance between GD and IGD in their sample. It may also suggest a potential pitfall of overdiagnosis common to polythetic approaches such as the DSM-5 IGD diagnostic criteria (Billieux et al., 2017).
Comparison of gaming behavior and related problems between GD and non-GD
An interesting finding regarding Internet applications was that significantly more participants in the GD group played online games using a PC or game console compared with those in the non-GD group. These electronic devices may be preferred by individuals who are addicted to gaming because of the devices' high functional specifications. In addition, the game genres usually played on these devices may play a role. Eichenbaum, Kattner, Bradford, Gentile, and Green (2015) surveyed university students and found that compared with action-style and smartphone games, real-time strategy and role-playing games, which are usually played on PCs and game consoles, were more strongly associated with IGD symptoms. This finding indicates that in addition to game genres, the choice of gaming devices is associated with risks for GD and IGD (Eichenbaum et al., 2015; Na et al., 2017).
The primary way in which individuals with GD are negatively affected by their gaming activities relates to the extreme investment of time in gaming (Baggio et al., 2016). Time spent on gaming results in the displacement of and interference with normal routines and functioning, and leads to missed opportunities (King & Delfabbro, 2018). In this study, participants with GD spent significant amounts of time on gaming, with means of 5.7 hours on weekdays and 6.6 hours on weekend days. These figures are comparable to the average of 47.5 hours a week among adolescents with IGD in Spain who sought treatment voluntarily (Torres-Rodriguez, Griffiths, Carbonell, & Oberst, 2018). A similar average time (375 minutes per day) was reported in adolescents identified as having IGD in a state-wide survey in Germany (Rehbein, Kliem, Baier, Mößle, & Petry, 2015). Although time spent on gaming does not serve as a proxy for problematic gaming, playing games for long periods of time has been reported to be associated with higher risks of developing GD (Stavropoulos et al., 2018). Our results clearly showed that participants in the GD group spent a significantly longer time playing each type of game and in total compared with those in the non-GD group.
Functional impairment is considered to be an essential element in preventing the overdiagnosis of GD (Billieux et al., 2017). The definition of GD clearly states that significant impairments should be found in personal, familial, social, educational, occupational, or other important areas of functioning (WHO, 2019). In accordance with this criterion, the participants with GD in this study showed high rates of impairment in different areas of functioning. High rates were found of impaired daily life cycles and impaired academic and job performance. Often, these are the main reasons for affected individuals to seek treatment. However, these problems may simply represent those issues commonly observed among students and young people, as the majority of the study participants were of this cohort. Consequently, the distribution pattern of these issues may change if study subjects are adult-dominant individuals with GD.
One problem which may be worth discussing is “Spending too much money on items”. The rate positive for this problem tended to be higher in the non-GD group than the GD group. This problem sometimes also occurs outside the context of GD and can constitute an independent problem related to gaming (King, Russel, Delfabbro, & Polisena, 2020). In fact the main reason for the hospital visit in some of the non-GD participants was exactly this problem rather than GD.
Limitations
This study did have some methodological limitations. First, we developed and used a short-form interview to evaluate the four GD diagnostic criteria. However, this instrument has not been validated. When we began this study, only the beta draft of the ICD-11 was available, containing a draft version of the GD definition (WHO, 2016a), though the content was essentially the same as the final version (WHO, 2019). As a result, no screening or assessment tools for GD existed, so our sole option was to develop a new instrument. Fortunately, a longer version of the three clinical manifestation criteria was available (WHO, 2016b), which we were able to use as the basis for developing our instrument. A validated screening tool for GD has actually become available quite recently (Paschke, Austermann, & Thomasius, 2020).
The second limitation concerns the lack of a control group. Due to the absence of a control group, we were unable to evaluate the diagnostic accuracy of the GD criteria. In addition, the characteristics of the participants in the GD and non-GD groups, including “Time spent on gaming” and “Severity of functional impairment”, could not be compared with those of healthy gamers or non-gamers. However, this was not a key aim of the study. However, future clinical studies on GD, incorporating comorbidity and effective treatment data are warranted.
Conclusions
In this study, we applied the definition of GD to treatment-seekers for internet addiction and developed a diagnostic tool to examine the relationship between the diagnoses of GD and IGD. Compared with participants in the non-GD group, those in the GD group preferred online games played with a PC and console, spent a significantly longer time on gaming, and showed a higher tendency to exhibit functional impairment. These findings suggest that diagnostic and screening tools for GD should be developed and validated in future studies.
Funding sources
No financial support was received for this study.
Authors' contributions
SH and HN developed the conception and design of the study. All authors contributed to the collection, analysis, and interpretation of data. SH drafted the article. All authors contributed to the revision and approved the final version of the article. All authors had full access to the data in this study, and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
All authors report no financial conflict or other relationship relevant to the subject of this article.
Acknowledgments
The authors wish to thank the members of the Treatment of Internet Addiction and Research Section of Kurihama Medical Addiction Center for contributing to the data collection for this study.
APPENDIX: The short-form interview used to evaluate the definition of ICD-11 gaming disorder for treatment-seekers
| Items | Duration (months) | ||
| Clinical manifestation | |||
| 1 | Impaired control over gaming in terms of onset, level, circumstances, or termination of gaming, often accompanied by urges or cravings and/or a subjective desire to stop or reduce gaming | (m) | |
| 2 | 2a | Gaming takes precedence over other interests and areas of enjoyment, daily activities, responsibilities, health, or personal care | (m) |
| 2b | Gaming plays an increasingly central role in the person's life and relegates other areas to the periphery | (m) | |
| 3 | 3a | Gaming often continues despite the occurrence of resulting problems | (m) |
| 3b | Gaming often continues despite the jeopardizing of school, work, or relationship opportunities | (m) | |
| Functional impairment due to gaming | |||
| 4 | The behavioral pattern is of sufficient severity to result in significant impairment in personal, familial, social, educational, occupational, or other important areas of functioning | (m) | |
Contributor Information
Susumu Higuchi, Email: h-susumu@db3.so-net.ne.jp.
Hideki Nakayama, Email: matimi19750519@hotmail.com.
Takanobu Matsuzaki, Email: takanobum@gmail.com.
Satoko Mihara, Email: mihara.satoko.pd@mail.hosp.go.jp.
Takashi Kitayuguchi, Email: kitayuguchi.takashi.vc@mail.hosp.go.jp.
References
- Aarseth, E., Bean, A. M., Boonen, H., Colder Carras, M., Coulson, M., Das, D., et al. (2017). Scholars’ open debate paper on the World Health Organization ICD-11 gaming disorder proposal. Journal of Behavioral Addictions, 6, 267–270. 10.1556/2006.5.2016.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders, 5th ed. (DSM-5). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Baggio, S., Dupuis, M., Studer, J., Spilka, S., Daeppen, J. B., Simon, O., et al. (2016). Reframing video gaming and Internet use addiction: Empirical cross-national comparison of heavy use over time and addiction scales among young users. Addiction, 111, 513–522. 10.1111/add.13192. [DOI] [PubMed] [Google Scholar]
- Billieux, J., King, D., Higuchi, S., Achab, S., Bowden-Jones, H., Hao, W., et al. (2017). Functional impairment matters in the screening and diagnosis of gaming disorder. Journal of Behavioral Addictions, 6, 285–289. 10.1556/2006.6.2017.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billieux, J., Schimmenti, A., Khazaal, Y., Maurage, P., & Heeren, A. (2015). Are we overpathologizing everyday life? A tenable blueprint for behavioral addiction research. Journal of Behavioral Addictions, 4, 119–123. 10.1556/2006.4.2015.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder Carras, M., Porter, A. M., van Rooij, A. J., King, D., Lange, A., Carras, M., et al. (2018). Gamers’ insights into phenomenology of normal gaming and game “addiction”. A mixed methods study. Computers in Human Behavior, 79, 238–246. 10.1016/j.chb.2017.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichenbaum, A., Kattner, F., Bradford, D., Gentile D. A., & Green, C. S. (2015). Role-playing and real-time strategy games associated with greater probability of Internet gaming disorder. Cyberpsychology, Behavior, and Social Networking, 18, 480–485. 10.1089/cyber.2015.0092. [DOI] [PubMed] [Google Scholar]
- Fam, J. Y. (2018). Prevalence of internet gaming disorder in adolescents: A meta-analysis across three decades. Scandinavian Journal of Psychology, 59, 524–531. 10.1111/sjop.12459. [DOI] [PubMed] [Google Scholar]
- Fauth-Bühler, M., & Mann, K. (2017). Neurobiological correlates of Internet gaming disorder: Similarities to pathological gambling. Addictive Behaviors, 64, 349–356. 10.1016/j.addbeh.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Griffiths, M., van Rooij, A. J., Kardefelt-Winther, D., Starcevic V., Király, O., Pallesen S., et al. (2016). Working towards an international consensus on criteria for assessing internet gaming disorder: A critical commentary on Petry et al. (2014). Addiction, 111, 167–175. 10.1111/add.13057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo, Y. S., Bhang, S. Y., Choi, J. S., Lee, H. K., Lee, S. Y., Kweon, Y. S., et al. (2019). Clinical characteristics of diagnosis of internet gaming disorder: Comparison of DSM-5 IGD and ICD-11 GD diagnosis. Journal of Clinical Medicine, 8, 945. 10.3390/jcm8070945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, D. L., Chamberlain, S. R., Carragher, N., Billieux, J., Stein, D., Mueller, K., et al. (2020). Screening and assessment tools for gaming disorder: A comprehensive systematic review. Clinical Psychology Review, 77, 101831. 10.1016/j.cpr.2020.101831. [DOI] [PubMed] [Google Scholar]
- King, D., & Delfabbro, P. H. (2018). The concept of “harm” in Internet gaming disorder. Journal of Behavioral Addictions, 7, 562–564. 10.1556/2006.7.2018.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, D. L., Delfabbro, P. H., Wu, A. M. S., Doh, Y. Y., Kuss, D., Pallesen, S., et al. (2017). Treatment of Internet gaming disorder: An international systematic review and CONSORT evaluation. Clinical Psychology Review, 54, 123–133. 10.1016/j.cpr.2017.04.002. [DOI] [PubMed] [Google Scholar]
- King, D.L., Russel, A.M.T., Delfabbro, P.H., Polisena, D. (2020). Fortnite microtransaction spending was associated with peers' purchasing behaviors but not gaming disorder symptoms. Addictive Behaviors, 104, 106311. 10.1016/j.addbeh.2020.106311. [DOI] [PubMed] [Google Scholar]
- Király, O., Griffiths, M. D., King, D. L., Lee, H. K., Lee, S. Y., Bányai, F., et al. (2018). Policy response to problematic video game use: A systematic review of current measures and future possibilities. Journal of Behavioral Addictions, 7, 503–517. 10.1556/2006.6.2017.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko, C. H., Lin, H. C., Lin, P. C., & Yen, J. Y.(2019). Validity, functional impairment and complications related to Internet gaming disorder in the DSM-5 and gaming disorder in the ICD-11. Australian & New Zealand Journal of Psychiatry, 54(7), 707–718. 10.1177/0004867419881499. [DOI] [PubMed] [Google Scholar]
- Kuss, D., Pontes, H. M., & Griffiths, M. D. (2018). Neurobiological correlates in internet gaming disorder: A systematic literature review. Frontiers in Psychiatry , 9, 166. 10.3389/fpsyt.2018.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihara, S., & Higuchi, S. (2017). Cross-sectional and longitudinal epidemiological studies of internet gaming disorder: A systematic review of the literature. Psychiatry and Clinical Neurosciences, 71, 425–444. 10.1111/pcn.12532. [DOI] [PubMed] [Google Scholar]
- Müller, K. W., Beutel, M. E., Dreier, M., & Wölfling, K. (2019). A clinical evaluation of the DSM-5 criteria for Internet gaming disorder and a pilot study on their applicability to further Internet-related disorders. Journal of Behavioral Addictions, 8, 16–24. 10.1556/2006.7.2018.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na, E., Choi, I., Lee, T. H., Lee, H., Rho, M. J., Cho, H., et al. (2017). The influence of game genre on Internet gaming disorder. Journal of Behavioral Addictions, 6, 1–8. 10.1556/2006.6.2017.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paschke, K., Austermann, M. I., & Thomasius, R. (2020). Assessing ICD-11 gaming disorder in adolescent gamers: Development and validation of the gaming disorder scale for adolescents (GADIS-A). Journal of Clinical Medicine, 9, 993. 10.3390/jcm9040993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehbein, F., Kliem, S., Baier, D., Mößle, T., & Petry, N. (2015). Prevalence of Internet gaming disorder in German adolescents: Diagnostic contribution of the nine DSM-5 criteria in a state-wide representative sample. Addiction, 110, 842–851. 10.1111/add.12849. [DOI] [PubMed] [Google Scholar]
- van Rooij, A. J., Ferguson, C. J., Colder Carras, M., Kardefelt-Winther, D., Shi, J., Aarseth, E., et al. (2018). A weak scientific basis for gaming disorder: Let us err on the side of caution. Journal of Behavioral Addictions, 7, 1–9. 10.1556/2006.7.2018.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu, H., Lee, J. Y., Choi, A. R., Chung, S. J., Park, M. K., Bhang, S. Y., et al. (2019). Application of diagnostic interview for Internet addiction (DIA) in clinical practice for Korean adolescents. Journal of Clinical Medicine, 8, 202. 10.3390/jcm8020202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc . (2016). Statistical analysis system for PC, version 9.4. Cary, NC: SAS Institute Inc. [Google Scholar]
- Saunders, J. B., Hao, W., Long, J., King, D. L., Mann, K., Fauth-Büler, M., et al. (2017). Gaming disorder: Its delineation as an important condition for diagnosis, management, and prevention. Journal of Behavioral Addictions, 6, 271–279. 10.1556/2006.6.2017.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stavropoulos, V., Anderson, E. E., Beard, C., Latifi, M. Q., Kuss, D., & Griffiths, M. D. (2018). A preliminary cross-cultural study of Hikikomori and Internet gaming disorder: The modeling effects of game-playing time and living with parents. Addictive Behaviors Reports, 9, 100137. 10.1016/j.abrep.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres-Rodriguez, A., Griffiths M. D., Carbonell, X., & Oberst, U. (2018). Internet gaming disorder in adolescence: Pathological characteristics of a clinical sample. Journal of Behavioral Addictions, 7, 707–718. 10.1556/2006.7.2018.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2016a). ICD-11 update. Health data standards and informatics, June 2016. Retrieved from https://www.who.int/classifications/2016_06_20_ICD11JuneNewsletter.pdf?ua=1.
- World Health Organization (2016b). Behavioural disorders associated with excessive use of the Internet, computers, smartphones and similar electronic devices: Clinical descriptions, diagnostic guidelines and priorities for international research: Meeting report. Geneva, Switzerland: World Health Organization. [Google Scholar]
- World Health Organization (2019). ICD-11 for mortality and morbidity statistics 2019. Retrieved from https://icd.who.int/browse11/l-m/en.
- Zajac, K., Ginley, M. K., & Chang, R. (2020). Treatment of internet gaming disorder: A systematic review of the evidence. Expert Review of Neurotherapeutics, 20, 85–93. 10.1080/14737175.2020.1671824. [DOI] [PMC free article] [PubMed] [Google Scholar]