Abstract
The in vitro activity of ABT-773 was evaluated against Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis isolates. ABT-773 was the most active antimicrobial tested against S. pneumoniae. ABT-773 and azithromycin were equivalent in activity against H. influenzae and M. catarrhalis and more active than either clarithromycin or erythromycin.
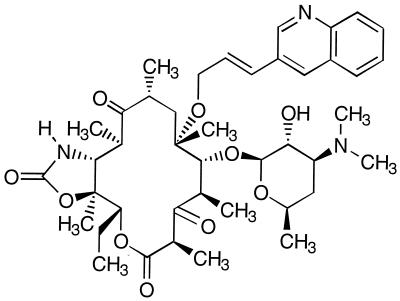
ABT-773 (A-195773) is a new ketolide having a potent antibacterial spectrum including activity against penicillin- and macrolide-resistant gram-positive bacteria. Its chemical name is 11-amino-11-deoxy-3-oxo-5-O-desosaminyl-6-O-[1′-(3′-quinolyl-2′-propenyl)] erythronolide A 11,12-cyclic carbamate (Fig. 1). This investigation assessed the in vitro activity of ABT-773 against three common bacterial respiratory tract pathogens, Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. These three organisms are the most frequent causative agents of acute otitis media, acute maxillary sinusitis, and acute purulent exacerbation of chronic bronchitis. The first two organisms are also major causes of community-acquired pneumonia.
FIG. 1.
Chemical structure of ABT-773 (A-195773).
The organisms examined in this study included isolates of S. pneumoniae (n = 1,601), H. influenzae (n = 1,529), and M. catarrhalis (n = 726) all collected as part of a large, prospective national surveillance study conducted from 1 November 1997 through 30 April 1998. Thirty-four medical centers contributed isolates. Details of this study have been reported previously (1, 5). Prior to testing, organisms having been stored at −70°C using an absorbent bead system (ProLab Diagnostics, Austin, Tex.), were subcultured twice. MICs of ABT-773, erythromycin, azithromycin, and clindamycin were determined by broth microdilution susceptibility testing according to the recommendations of the National Committee for Clinical Laboratory Standards (3, 4). The following media were used: S. pneumoniae, cation-adjusted Mueller-Hinton broth plus 3% lysed horse blood; H. influenzae, haemophilus test medium; and M. catarrhalis, Mueller-Hinton broth. The following control strains were tested on a daily basis: S. pneumoniae ATCC 49619 and H. influenzae ATCC 49247; H. influenzae ATCC 49247, 49766, and 10211; and Escherichia coli ATCC 25922 and Staphylococcus aureus ATCC 29213. Antimicrobials were provided by their respective manufacturers. A final inoculum concentration of ca. 5 × 105 CFU/ml per well was employed; microdilution trays were incubated for 24 h at 35°C in ambient air before MICs were determined visually.
Results of MIC determinations for S. pneumoniae are listed in Table 1. ABT-773 was the most active of the seven antimicrobials tested: 78.9% of S. pneumoniae isolates were inhibited by ABT-773 at a concentration of ≤0.008 μg/ml. The MIC at which 90% of the isolates were inhibited (MIC90) was 0.03 μg/ml. The highest ABT-773 MIC was 0.5 μg/ml (n = 3). When isolates were sorted according to penicillin susceptibility category, the ABT-773 MIC90s were as follows: penicillin susceptible (penicillin MIC, ≤0.06 μg/ml), ≤0.008; penicillin intermediate (penicillin MIC = 0.12 to 1 μg/ml), 0.03; and penicillin resistant (penicillin MIC, ≥2 μg/ml), 0.12 μg/ml. Comparison compounds included the macrolides erythromycin, clarithromycin, and azithromycin and a lincosamide, clindamycin. The MIC50s and MIC90s and ranges of MICs obtained with these agents were 0.06, 8, and ≤0.03 to >64; ≤0.03, 4, and ≤0.03 to >64; 0.12, 16, and ≤0.03 to >64; and 0.06, 0.06, and ≤0.008 to >8 μg/ml, respectively.
TABLE 1.
Comparison of the in vitro activities of five antimicrobial agents against 1,601 isolates of S. pneumoniae by penicillin categorya
| Antimicrobial | Penicillin-susceptible strains (n = 1,127)
|
Penicillin-intermediate strains (n = 278)
|
Penicillin-resistant strains (n = 196)
|
All strains (n = 1,601)
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC50 | MIC90 | MIC range | % I | % R | MIC50 | MIC90 | MIC range | % I | % R | MIC50 | MIC90 | MIC range | % I | % R | MIC50 | MIC90 | MIC range | % I | % R | |
| ABT-773 | ≤0.008 | ≤0.008 | ≤0.008–0.5 | ≤0.008 | 0.03 | ≤0.008–0.5 | 0.015 | 0.12 | ≤0.008–0.25 | ≤0.008 | 0.03 | ≤0.008–0.5 | ||||||||
| Clarithromycin | ≤0.03 | ≤0.03 | ≤0.03–>64 | 0.5 | 5.2 | ≤0.03 | >64 | ≤0.03–>64 | 2.2 | 35.3 | 2 | >64 | ≤0.03–>64 | 3.6 | 64.8 | ≤0.03 | 4 | ≤0.03–>64 | 1.2 | 17.7 |
| Erythromycin | 0.06 | 0.06 | ≤0.03–>64 | 0.3 | 5.7 | 0.06 | >64 | ≤0.03–>64 | 0.7 | 37.4 | 4 | >64 | ≤0.03–>64 | 0.5 | 68.4 | 0.06 | 8 | ≤0.03–>64 | 0.4 | 18.9 |
| Azithromycin | 0.06 | 0.12 | ≤0.03–>64 | 0.2 | 5.6 | 0.12 | >64 | ≤0.03–>64 | 0.7 | 37.8 | 8 | >64 | ≤0.03–>64 | 1.5 | 67.3 | 0.12 | 16 | ≤0.03–>64 | 0.4 | 18.7 |
| Clindamycin | 0.06 | 0.06 | ≤0.008–>8 | 0.1 | 1.1 | 0.06 | >8 | ≤0.008–8 | 0.0 | 12.9 | 0.06 | >8 | ≤0.008–>8 | 0.5 | 21.4 | 0.06 | 0.06 | ≤0.008–>8 | 0.1 | 5.6 |
Penicillin susceptible, MIC ≤ 0.06 μg/ml; penicillin intermediate, MIC of 0.12 to 1 μg/ml; penicillin resistant, MIC ≥ 2 μg/ml. % I, percent intermediate; % R, percent resistant. MICs are expressed as micrograms per milliliter.
Table 2 depicts the relationship between ketolide and erythromycin MICs. S. pneumoniae has two principal mechanisms of macrolide resistance, efflux and constitutively expressed macrolide-lincosamide-streptogramin B resistance as a result of ribosomal alterations (2, 6). Efflux, the result of expression of the mefE gene, usually results in erythromycin MICs of 1 to 32 μg/ml and clindamycin MICs of ≤0.25 μg/ml (1). Altered ribosomal targets as a consequence of ermAM gene-mediated methylation typically result in erythromycin MICs of ≥64 μg/ml and clindamycin MICs of ≥8 μg/ml. In the current study, 222 of 302 (73.5%) macrolide-resistant S. pneumoniae strains displayed the efflux phenotype and 80 of 302 (26.5%) macrolide-resistant S. pneumoniae strains were characterized by the ermAM phenotype. Among the macrolide-resistant S. pneumoniae strains with the efflux phenotype, for 82.0% (n = 182) the ABT-773 MICs were ≥0.015 μg/ml. Similarly, among the S. pneumoniae strains with the ermAM phenotype, for 81.3% (n = 65) the ABT-773 MIC was ≥0.015 μg/ml. In other words, higher ketolide MICs were noted with S. pneumoniae isolates harboring either efflux or ermAM-mediated resistance determinants. Studies aimed at further evaluating this relationship are in progress.
TABLE 2.
Comparison of ABT-773 MICs for isolates of S. pneumoniae by erythromycin categoriesa
| MIC (μg/ml) | No. of strains | No. of strains (%) for which erythromycin MIC (μg/ml) is:
|
||
|---|---|---|---|---|
| ≤0.5 | 1–32 | ≥64 | ||
| ≤0.008 | 1,318 | 1,263 (95.8) | 40 (3.0) | 15 (1.1) |
| 0.015 | 99 | 29 (29.3) | 44 (44.4) | 26 (26.3) |
| 0.03 | 79 | 2 (2.5) | 62 (78.5) | 15 (19.0) |
| 0.06 | 48 | 4 (8.3) | 34 (70.8) | 10 (20.8) |
| 0.12 | 41 | 1 (2.4) | 33 (80.5) | 7 (17.1) |
| 0.25 | 13 | 8 (61.5) | 5 (38.5) | |
| 0.5 | 3 | 1 (33.3) | 2 (66.7) | |
Strains for which erythromycin MIC is ≤0.5 μg/ml are erythromycin susceptible or intermediate; strains for which erythromycin MIC is 1 to 32 μg/ml and clindamycin MIC is ≤0.25 have the efflux phenotype; strains for which erythromycin MIC is ≥64 μg/ml and clindamycin MIC is ≥8 μg/ml have the ermAM genotype.
The activity of ABT-773 against H. influenzae and M. catarrhalis was also evaluated and compared to that of the macrolides (Table 3). ABT-773 and azithromycin had identical activity against H. influenzae, with MIC50s and MIC90s of 2 and 4 μg/ml, respectively. ABT-773 and azithromycin were fourfold more active against H. influenzae than were erythromycin and clarithromycin, whose MIC50s and MIC90s were also identical at 8 and 16 μg/ml, respectively. The rate of beta-lactamase production was 31.1% among these isolates of H. influenzae. No differences in susceptibility were seen between beta-lactamase-positive and beta-lactamase-negative strains.
TABLE 3.
Comparison of the in vitro activities of ABT-773 and the macrolides against 1,529 isolates of H. influenzae and 726 isolates of M. catarrhalisa
| Organism | Antimicrobial agent | Value for strain type:
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta-lactamase positive
|
Beta-lactamase negative
|
||||||||||
| MIC50 | MIC90 | MIC range | % I | % R | MIC50 | MIC90 | MIC range | % I | % R | ||
| H. influenzae | ABT-773 | 2 | 4 | 0.12–>8 | 2 | 4 | 0.06–>8 | ||||
| Azithromycin | 2 | 4 | 0.25–64 | 2 | 4 | ≤0.12–>256 | |||||
| Clarithromycin | 8 | 16 | 0.5–128 | 26.9 | 6.5 | 8 | 16 | ≤0.12–>256 | 29.1 | 3.1 | |
| Erythromycin | 8 | 16 | 0.25–64 | 8 | 16 | ≤0.12–>256 | |||||
| M. catarrhalis | ABT-773 | 0.06 | 0.06 | ≤0.004–0.12 | 0.12 | 0.12 | 0.008–0.12 | ||||
| Azithromycin | 0.06 | 0.12 | 0.03–0.25 | 0.0 | 0.0 | 0.06 | 0.12 | 0.06–0.25 | 0.0 | 0.0 | |
| Clarithromycin | 0.12 | 0.12 | ≤0.015–0.5 | 0.0 | 0.0 | 0.12 | 0.12 | 0.03–0.12 | 0.0 | 0.0 | |
| Erythromycin | 0.25 | 0.25 | 0.06–1 | 0.0 | 0.0 | 0.25 | 0.25 | 0.06–0.25 | 0.0 | 0.0 | |
For beta-lactamase-positive strains, n = 476 for H. influenzae and 687 for M. catarrhalis; for beta-lactamase-negative strains, n = 1,053 for H. influenzae and 39 for M. catarrhalis. MICs are expressed as micrograms per milliliter. % I, percent intermediate; % R, percent resistant.
ABT-773 was considerably more active against M. catarrhalis than against H. influenzae. The MIC50 and MIC90 of ABT-773 for M. catarrhalis were 0.06 μg/ml. This was nearly identical to the activity of azithromycin, twofold more active than clarithromycin, and fourfold more active than erythromycin. The MIC50s and MIC90s of those agents were as follows: 0.06 and 0.12, 0.12 and 0.12, and 0.25 and 0.25 μg/ml, respectively. Nearly all M. catarrhalis strains produced beta-lactamase (94.6%). ABT-773 was consistently twofold less active against beta-lactamase-negative than against beta-lactamase-positive strains. No differences between beta-lactamase-positive and -negative strains were seen with any of the macrolides.
The results of the current study indicate that ABT-773, a new ketolide antimicrobial agent, has potent in vitro activity against recent clinical isolates of S. pneumoniae. Although the drug is less active against H. influenzae and M. catarrhalis, the overall activity of ABT-773 against these three pathogens would be sufficient to warrant performance of clinical trials with patients with respiratory tract infections due to these organisms, assuming acceptable pharmacokinetic and toxicity profiles.
Acknowledgments
This investigation was funded by a grant from Abbott Laboratories.
REFERENCES
- 1.Doern, G. V., A. B. Brueggemann, H. Huynh, E. Wingert, and P. Rhomberg. Antimicrobial resistance with Streptococcus pneumoniae—results of 1997–98 34 center United States surveillance study. Emerg. Infect. Dis., in press. [DOI] [PMC free article] [PubMed]
- 2.Johnston N J, DeAzavedo J C, Kellner J D, Low D E. Prevalence and characterization of the mechanisms of macrolide, lincosamide, and streptogramin resistance in isolates of Streptococcus pneumoniae. Antimicrob Agents Chemother. 1998;42:2425–2426. doi: 10.1128/aac.42.9.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. 4th ed. 1997. Approved standard M7-A4. National Committee for Clinical Laboratory Standards, Wayne, Pa. [Google Scholar]
- 4.National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. Eighth informational supplement, M100-S8. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 5.Richter S S, Brueggemann A B, Huynh H K, Rhomberg P R, Wingert E M, Doern G V. A 1997–1998 national surveillance study: Moraxella catarrhalis and Haemophilus influenzae antimicrobial resistance in 34 U.S. institutions. Int J Antimicrob Agents. 1999;13:99–107. doi: 10.1016/s0924-8579(99)00112-0. [DOI] [PubMed] [Google Scholar]
- 6.Shortridge V D, Flamm R K, Ramer N, Beyer J, Tanaka S K. Novel mechanism of macrolide resistance in Streptococcus pneumoniae. Diagn Microbiol Infect Dis. 1996;26:73–78. doi: 10.1016/s0732-8893(96)00183-6. [DOI] [PubMed] [Google Scholar]