Abstract
Background:
Suicide is a major threat to public health worldwide. Evidence suggests alcohol use disorders (AUD) are associated with suicide ideation. There is a paucity of studies in India regarding suicidal ideation among individuals receiving in-patient treatment for alcohol dependence.
Aim:
To assess the suicidal ideation and its severity among persons with alcohol use disorder.
Methods:
Cross-sectional research design was used. Totally 47 persons with alcohol use disorder receiving in-patient treatment were screened for suicidal ideation using a consecutive sampling technique based on inclusion and exclusion criteria at centre for addiction medicine, tertiary care teaching hospital at Bangalore. An interview schedule was used to collect the data. Tools: Mini+ suicidality was used for screening suicidal ideation and Columbia suicide severity rating scale was used to assess the frequency and severity of the suicidal ideation. Descriptive statistics such as frequency, percentage, mean were used for data analysis.
Results & Discussion:
Out of 47 patients, 29 reported having suicidal ideations (62%). AUD suicidal ideation was more among persons belong to below poverty line, lower education level, unemployed, married, living with family of origin, nuclear family, urban, using tobacco. Their mean age was 35 years (±6.6). Majority (62%) of them had suicidal ideation in the past one month, 43% reported having thought to kill themselves over the past one month. One-third (35%) able to control suicidal thought with lot of difficulty, 83% reported that deterrents stopped them attempting suicide, 82%wanted to end their life to end or stop the pain that they are enduring.
Conclusion:
The prevalence of suicidal ideations is high among persons with alcohol use disorder. Socio-demographic factors likely to have an influence on suicidal ideation among persons with alcohol use disorder.
Keywords: Deliberate Self-Harm, Death Wishes, Social Work, Substance Use Disorder
Introduction
Suicide is a major threat to public health. Worldwide, one million people die by committing suicide every year. Suicide is the second leading cause of death among people between the age group 15–29 years. Globally about 79% of suicide occurred in lower and middle-income countries in 2016 (WHO, 2018). Substance use is one of the primary causes of suicide in India (Kamalja, 2017). Suicide rate in the India was 11.3% showing increase trend. Substance abuse was third leading cause, accounted for 6% of suicides in India, [NCRB, 2020]
Alcohol use and suicide ideation
Suicidal ideation refers to the contemplation of ending one's own life (Pederson 2018). Suicidal ideation is a broad term used to describe a range of contemplations, wishes, and preoccupations with death and thoughts or ideas about suicide (Harmer, 2021). Many countries have reported an association between alcohol consumption and suicide rate (Lester, 2000). Suicide rates are associated with heavy drinking. Studies show that suicide ideation in alcohol use disorder indicate multiple socio-cultural and environmental factors influencing suicide rates (Nemtsov 2003; Pirkola 2004). Alcohol use disorder is associated with an elevated risk of suicide, as shown by meta-analyses of follow-up studies (Harris 1997; Inskip 1998; Wilcox 2004). The risk for suicide is associated with alcohol dependence and it is directly proportional to their age (Connor 2003). Persons with depression and a history of alcohol dependence syndrome have higher suicide ideation (Sher, 2005).
Persons having substance use disorder and suicidal ideations are prone to have several emotional and behavioural problems(Wojnar 2009). Alcohol dependence, comorbid psychopathology and adverse life events act as risk factors for suicide. Alcohol intoxication act as a important risk factor for suicidal behaviour among alcohol users. Factors responsible for alcohol induced suicidal behaviour include increased psychological distress, increased aggressiveness, propelled suicidal ideation into action through suicide-specific alcohol expectancies, and limited cognition which impairs the alternative coping strategies (Hufford 2001).
Most patients with suicidal risk presented a severity in their substance use. Patients with suicidal ideation and suicide attempts showed a more severe addiction profile and maladjustment to everyday life. About 40% of the persons with substance use disorder had attempted suicide. Psychiatric conditions, previous hospitalization for psychological problems, and history of delirium were associated suicide attempts (Lopez 2019).
About 44% of the patients had lifetime suicidal ideation (8.7% in the last month), and 17.7% had suicide attempts (1.5% in the last month). Persons with suicidal ideation showed more psychopathological symptoms. Moreover, the rate of suicidal ideation was significantly higher in inpatients than in outpatients (Lopez 2018).
About 40% of persons treated for substance dependence report a history of suicide attempt(s). Suicidal risk is a significant problem for persons with SUD seeking treatment. Several predisposing and precipitating risk factors such as marital and interpersonal relationship problems, occupational and financial stressors, recent heavy substance use and intoxication, and previous suicide attempts and sexual abuse, personality traits, and mental illnesses intensify suicide risk in SUD. Depression, bipolar disorder, borderline personality disorder and post-traumatic stress disorder are associated with suicidal risk in people with addictive disorders (Yuodelis, 2015). Lifetime suicidal ideation in alcohol dependents is associated with borderline personality disorder, sexual abuse, polydrug abuse, attention-deficit hyperactivity disorder, and impulsivity, lifetime abuse, co-morbid psychiatric disorders such as anxiety disorders and depressive disorders (Rodriguez, 2018).
Alcohol dependence and post-traumatic stress disorder are both associated with increased suicidality. Most persons with alcohol use disorder (AUD) experienced suicidal ideation at some point in their lives. Covert hostility, PTSD symptoms severity, depressive symptoms was found to be associated with the presence of lifetime suicidal ideation (Kachadourian, 2018)
The association between suicide and mental illnesses such as depression and alcohol disorders is well established in high-income countries. Most suicides happen impulsively when there is a crisis which interrupts the potential to deal with pressure one experience in their life, such as economic issues, interpersonal issues or long-lasting pain and illnesses. Meta-analysis of mortality studies revealed that persons with substance use disorder are at a high risk of suicide, about 8% more in their lifetime. Compared to other psychiatric disorders, suicide risk among alcohol dependents remained persistently high (Inskip 1998). Psychiatric disorders such as psychosis, mood disorders and anxiety disorders, vulnerability to stress, increase the risk of suicidal behavior. These also have reciprocal influences with alcohol drinking patterns (Pompili 2010).
Suicidal ideation among persons with AUD differs in terms of employment, economic state, family history, hospitalization, the number of suicide attempts, and the degree of hopelessness (Woo 2019). Younger age, female sex, and current depression are risk factors for severe suicidality in SUD patients (Matsumoto 2012).
Acute alcohol use is associated with suicide. Suicide completers have high blood alcohol content. Intoxicated persons are more likely to attempt suicide using more lethal methods (Sher 2006). Three-fourth of alcohol dependents belonged to the high-risk group of suicidal ideation. Suicidal ideation was associated with alexithymia among alcohol dependents characterized by the inability to communicate feelings (Sakuraba 2005).
A meta-analysis reported that suicide risk among persons with substance use disorders (SUD) is almost six times higher. Persons with alcohol dependence are likely to commit suicide five times more than social drinkers (Harris, 1997)Prevalence of suicidal ideations among persons with AUD is 21% and attempted suicide is 12.4%(Abdalla et al., 2019). Men with comorbid depression and alcohol use have the highest suicide risk (Holmstrand, 2015). The prevalence of lifetime suicide attempts among persons with AUD is 21%.(Oquendo, 2010) Alcohol misuse is prone to suicidal behaviour through its depressogenic effects and adverse life events. Acute alcohol use can lead to suicidal behaviours through induction of negative impact and impairment of problem-solving skills, as well as exasperation of impulsive personality traits, possibly through effects on serotonergic neurotransmission (Brady, 2006).
Alcohol dependence is associated with depression and suicidal ideation (Lee 2021). Nearly half (43%) of suicide attempters had consumed alcohol at the time of attempt. One-third of persons who attempted suicide had alcohol dependence. There is a positive correlation between suicidal intent, lethality, stressors and psychiatric co-morbidity among persons with AUD (Sreelatha, 2019).
Persons with alcohol dependence syndrome had high suicidal ideation (22%) when compared to normal. Suicidal ideation was associated with severity of alcohol dependence. Persons with AUD had significantly higher scores on suicidal ideation, depression, state and trait anxiety scores (Kumar et al 2016)
However, there is a paucity of studies from India on the suicidal ideations among persons with alcohol use disorder (AUD). Therefore, the study examines suicidal ideation among persons treated for with alcohol use disorder.
Objective:
To assess suicidal ideation among persons with alcohol use disorder.
Hypothesis:
Suicidal ideation would be more among persons treated for alcohol use disorder.
Inclusion Criteria:
Persons who have primary diagnosis of Alcohol dependence as per DSM V criteria, patients who are aged between 18–45 years.
Exclusion Criteria:
Persons those who receive outpatient treatment, who have severe withdrawal symptoms and delirium tremens at the time of data collection, those who refuse consent to participate were excluded from the study.
Methods
Sample:
A Cross-sectional research design was used. Persons receiving in-patient treatment at centre for addiction medicine, tertiary care teaching hospital, Bangalore, formed the universe of the study. Total 47 subjects receiving treatment as inpatients at centre for addiction medicine were selected for the study using a consecutive sampling technique. Data was collected during Jan - March 2020. Persons having primary diagnosis of alcohol dependence syndrome as per DSM-V criteria, those who are treated as inpatients, those who are aged between 18–45 years, those who have given consent to participate were included and those who had delirium at the time of collecting data were excluded from the study. An interview schedule was used to collect the data.
Tools used:
Mini+ Suicidality was used to screen suicidal ideation among persons treated for alcohol use disorder. Columbia suicide severity rating scale (Posner et al 2011) was used to assess the severity of suicidal ideation among persons treated for alcohol use disorder. Suicide ideation subscale has a Guttmann split-half reliability of 0.91 and a Cronbach's alpha of 0.87, 0.89 and 0.93 for the sample, the suicide-risk and control groups respectively, with good internal consistency. Suicide intensity, severity and behavior subscales had Cronbach's alpha of 0.73 Written Informed consent was obtained from participants before data collection. Ethical clearance was obtained from Institute Ethics Committee.
Procedure
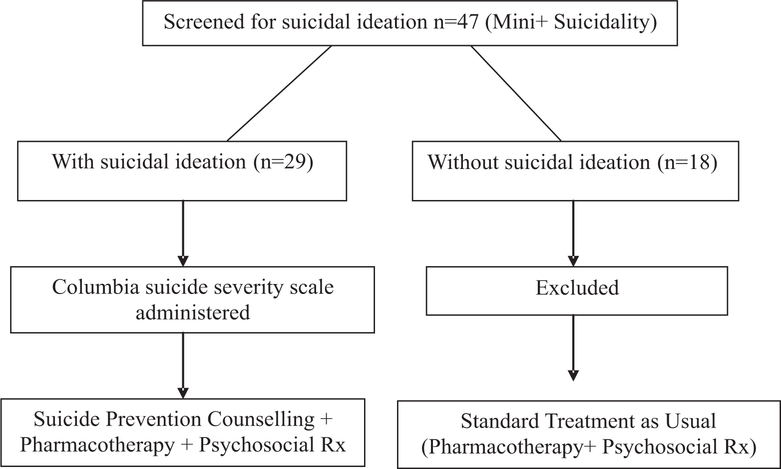
Persons who are admitted in the male ward with primary diagnosis of alcohol dependence syndrome was screened for suicidal ideation, using MINI+ suicidal ideation screening. The selection of the patients was based on the admission list i.e., all the even number patients were recruited after taking permission from the officer in charge of the centre. When even number patient was not having alcohol dependence syndrome as the primary diagnosis or the patient was not willing to participate then the next patient was recruited for the study. The data collection was done in two sessions; in the first session rapport was established and the socio demographic details and clinical information about the substance use were collected. In the second session patients were screened for suicidal ideations. All the respondents were given a brief supportive counseling, facilitated ventilation as the questionnaire focused more on psychosocial factors. Totally 47 persons availing in-patient care at centre for addiction medicine was screened for suicidal ideation using MINI+ suicidality. Out of 47 individuals, 29 were reported suicidal ideation. There are totally 60 beds available at the centre. Data was collected over a period of one month during Feb 2020. Severity of suicidal ideation was assessed for the 29 individuals who reported suicidal ideation using Columbia suicide severity scale. All the 29 data were included for analysis.
Statistical Analysis:
Quantitative data was analyzed using percentage, frequency and mean to describe the demographic variables and suicidal ideation among persons seeking in-patient treatment for alcohol use disorder.
Results
Table 1:
Socio-demographic profile
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
|
| |||
| Socio-economic status | Below Poverty Line | 24 | 82 |
| Above Poverty Line | 05 | 18 | |
| Marital Status | Single | 06 | 21 |
| Married | 17 | 57 | |
| Separated | 04 | 14 | |
| Divorced | 01 | 04 | |
| Widower | 01 | 04 | |
| Living arrangement | Alone | 02 | 07 |
| Family of Origin | 18 | 62 | |
| Family of Procreation | 09 | 31 | |
| Domicile | Rural | 06 | 21 |
| Semi-urban | 02 | 07 | |
| Urban | 21 | 72 | |
| Family type | Nuclear | 20 | 69 |
| Joint family | 04 | 14 | |
| Extended family | 05 | 17 | |
| Other substances used | Tobacco | 21 | 72 |
| Cannabis | 05 | 17 | |
Table 1 shows that the mean age of the persons who had suicidal ideation was 35.5 years (SD±6.6), and the mean years of education was nine(SD±4.4). More than half (57%) the respondents who had suicidal ideations were married, living with their family of origin (62%), 82% belonged to below poverty line,72% belonged to urban domicile, 69% of them were from nuclear families. Nearly half of them (41%) were unemployed. The mean age at initiation of alcohol use was 19 years. Most of them (59%) had past history of abstinent with the help of medication. The reason for relapse was interpersonal issues with family and financial problems (28%), followed by peer pressure and craving (17%). Most respondents (59%) were able to maintain abstinence for more than three months. Majority were using tobacco (72%) and reported suicidal ideation (62%).
Table 2.
Suicidal ideation profile among persons with Alcohol Use Disorder
| Sr. No | Variable | Category | Frequency (n=29) | Percentage |
|---|---|---|---|---|
|
| ||||
| 1 | Wish to be dead | Lifetime | 29 | 100 |
| Past 1 month | 29 | 100 | ||
| 2 | Non- Specific Active Suicidal Thoughts | Lifetime | 29 | 100 |
| Past 1 month | 29 | 100 | ||
| 3 | Active Suicidal Ideation with Any Methods (Not Plan) without Intent to Act | Lifetime (Yes) | 26 | 90 |
| Lifetime (No) | 03 | 10 | ||
| Past 1 month (Yes) | 17 | 59 | ||
| Past 1 month (No) | 12 | 41 | ||
| 4 | Active Suicidal Ideation with some Intent to Act, without Specific Plan | Lifetime (Yes) | 20 | 69 |
| Lifetime (No) | 09 | 31 | ||
| Past 1 month (Yes) | 12 | 41 | ||
| Past 1 month (No) | 17 | 59 | ||
| 5 | Active Suicidal Ideation with Specific Plan and Intent | Lifetime (Yes) | 19 | 65 |
| Lifetime (No) | 10 | 34 | ||
| Past 1 month (Yes) | 03 | 10 | ||
| Past 1 month (No) | 26 | 90 | ||
Table 2 revealed that almost all (100%) of them reported experiencing a wish to die and non-specific active suicidal ideation in their lifetime and in the last month. A majority (90%) of the participants had active suicidal ideation without intent to act was reported in their lifetime and 59% in the last month.. Majority (69%) reported active suicidal ideations with some intention to act in their lifetime and 41% in the previous month. About 65% of the respondents had active suicidal ideations with specific plans and intent in their lifetime, and 10% during the last month.
Table 3.
Severity of suicidal ideation among persons with AUD in the last month (N=29)
| Sr.No | Variable | Category | Frequency | Percentage |
|---|---|---|---|---|
|
| ||||
| 1 | Frequency | Less than once a week | 10 | 34 |
| Once a week | 07 | 24 | ||
| 2–5 times in week | 09 | 31 | ||
| Daily or almost daily | 03 | 10 | ||
| 2 | Duration | Fleeting– few seconds or minutes | 09 | 30 |
| Less than 1 hour/some of the time | 13 | 45 | ||
| 1–8 hours/a lot of time | 06 | 20 | ||
| More than 8 hours/persistent | 01 | 03 | ||
| 3 | Controllability | Can control thoughts with little difficulty | 08 | 27 |
| Can control with some difficulty | 08 | 28 | ||
| Can control thoughts with lot of difficulty | 10 | 35 | ||
| Unable to control thoughts | 02 | 07 | ||
| Does not attempt to control thoughts | 01 | 3 | ||
| 4 | Deterrents | Definitely stopped me attempting suicide | 11 | 38 |
| Deterrents probably stopped me attempting | 13 | 45 | ||
| Uncertain that deterrents stopped me | 01 | 03 | ||
| Deterrents most likely did not stop me | 03 | 10 | ||
| Does not apply | 01 | 03 | ||
| 5 | Reasons for Ideation | To get attention | 03 | 10 |
| Mostly to end or stop the pain | 24 | 82 | ||
| Completely to end or stop the pain | 02 | 07 | ||
| Does not apply | 01 | 03 | ||
Table 3 shows the severity of suicidal ideation in the past one month. More than one-third (34%) of them experienced suicidal ideation less than once in a week, 31% of them experienced it 2-5 times in a week. Nearly half (45%) of the respondents reported that the duration of suicidal ideations was less than 1 houror sometimes in the last month. More than one-third (35%) were able to control the suicidal thoughts with lot of difficultyand 28% of them were able to control the suicidal thoughts with some difficulty.Nearly half (45%) of the respondents reported that the deterrents probably stopped them attempting suicide and 38% reported that the deterrents definitely stopped them attempting suicide. Majority (83%) of the respondents reported that the reason for wanting to die or killing themselves was to mostly to end or stop pain which they were undergoing.
Table 4.
Severity of suicidal ideation in participants’ lifetime
| Sr.No | Variable | Category | Frequency | Percentage |
|---|---|---|---|---|
|
| ||||
| 1 | Frequency | Less than once a week | 08 | 28 |
| Once a week | 04 | 14 | ||
| 2–5 times in week | 04 | 14 | ||
| Daily or almost daily | 08 | 28 | ||
| Many times each day | 05 | 17 | ||
| 2 | Duration | Fleeting – few seconds or minutes | 07 | 24 |
| Less than 1 hour/some of the time | 04 | 14 | ||
| 1–4 hours/a lot of time | 04 | 14 | ||
| 4–8 hours/most of day | 10 | 34 | ||
| More than 8 hours/persistent | 05 | 14 | ||
| 3 | Controllability | Easily able to control thoughts | 06 | 21 |
| Can control thoughts with little difficulty | 04 | 14 | ||
| Can control with some difficulty | 08 | 28 | ||
| Can control thoughts with lot of difficulty | 07 | 24 | ||
| Unable to control thoughts | 04 | 14 | ||
| 4 | Deterrents | Definitely stopped me attempting suicide | 07 | 24 |
| Deterrents probably stopped you | 08 | 28 | ||
| Uncertain that deterrents stopped you | 02 | 07 | ||
| Deterrents most likely did not stop you | 03 | 10 | ||
| Deterrents definitely did not stop you | 09 | 31 | ||
| 5 | Reasons for Ideation | Completely to get attention | 01 | 03 |
| Mostly to end or stop the pain | 19 | 65 | ||
| Completely to end or stop the pain | 09 | 31 | ||
| Does not apply | 01 | 03 | ||
Table 4 reveals the severity of suicidal ideation in their life time. About 28% of the respondents reported of experiencing suicidal ideation in less than once a week and daily or almost daily each and another 28% less than once a week. More than one-third reported duration of suicidal ideation was ranging from four to eight hours most of the day. Nearly one-fourth of them (24%) reported that they can control the suicidal thoughts with lot of difficulty. One-third reported that deterrents definitely did not stop them from attempting suicide, another 52% of them reported deterrents stopped them attempting suicide. A majority of them (65%) reported that in their lifetime they thought ending their life mostly due to end or stop the pain.
Discussion
Persons with substance use disorders are at greater risk for suicide than any other psychiatric disorder. The current study focused on the suicidal ideation among persons treated for alcohol dependence syndrome. The study was carried out using a quantitative method.
Most of the (62%)persons treated for alcohol use disorder reported suicidal ideations. This finding was similar to previous studies (Harris, 1997; Inskip, 1998; Wilcox 2004; Connor, 2003; Abdalla et al., 2019; Sreelatha, 2019; Kumar, 2016; Kaur et al 2013; Agrawal et al 2017) Suicidal ideations are very much prevalent among persons with substance use disorder. The persons seeking treatment for alcohol dependence syndrome often reluctant to report suicidal ideations during the treatment process. Treatment-seeking alcohol-dependent individuals often present with multiple risk factors. Early recognition of suicidal behaviour is of paramount importance. Associations between substance use disorder and suicidal behaviors is a complex phenomenon. Several studies have reported strong association between SUD and suicidal ideation (Kumar et al 2016, Sreelatha, 2019)
This study revealed that AUD suicidal ideation was more among persons with lower education level and tobacco users. This finding was in concordance with previous study (Chachamovich, 2012). Suicidal ideation was more among persons belong to below poverty line, unemployed, married, living with family of origin, nuclear family, urban domicile. This finding was in concordance with previous study (Woo, 2019). Present study showed one-third of the samples had suicidal ideation in their life time. This finding was similar to previous study (Oquendo, 2010; Kachadourian, 2018; Rodriguez, 2018).In this study, about 41% of the in-patients had frequent suicidal ideation in the past one month. This findings is concomitant to previous study (Lopez et al 2018).
Increased suicide risk may be precursor of social withdrawal, breakdown of social bonds, and social marginalization, which are common outcomes of untreated alcohol abuse and dependence (Pompili, 2010). Mood disorders, aggression and impulsivity pose additional risk for suicidal behaviour in people with alcohol dependence (Chachamovich, 2012). All individuals with alcohol use disorders should be assessed for mood disorders, aggression, impulsivity, and suicide risk. Frequently, several risk factors act together to increase a person's vulnerability to suicidal behaviour. There are several risk factors related to the health care facilities and the society at a substantial level includes the difficulties in retrieving health care and in undergoing adequate care. The easy accessibility of means of suicide, inappropriate documentation of suicide-related news by the media sensationalizes suicides and increases the risk of copycat suicides and increases stigma for persons who seek help for suicidal ideation or for mental health issues or substance use disorders. Suicide is a continuum that begins with ideation and may continue with planning, attempts and suicide completion. Examining the specific risk factors for suicidal attempts in persons with substance use disorder(SUD) having suicidal ideation is crucial for suicide prevention.
There are several strategies, which reduce the risk factors associated with suicide. The prevention strategies for risk factors are of three kinds. The prevention strategies adapted to reach an entire population are called Universal prevention strategies, which aim to increase access to health care, promote mental health care facilities, promote mental health, reduce harmful alcohol use, and limit access to the means for suicide or promote responsible media reporting. Selective prevention strategies aims to help the high-risk groups who have undergone traumatic events or abuse, those affected by dispute or disaster, refugees and migrants, and bereaved by suicide, by training "gatekeepers" who assist the persons at high risk and by offering services in suicide prevention helpline.
Strategies target specific individuals at high risk with community support, follow-up for those leaving healthcare facilities. Educating and training the health workers to increase the identification and management of mental and substance use disorders. The Prevention strategies can be by enhancing the protective factors such as personal and social support, improving personal belief system good positive coping strategies (WHO, 2014). A systematic screening of suicidal risk in patients seeking treatment for alcohol use is recommended. Addiction treatment centres should develop treatment strategies to prevent persons with SUD from attempting suicide (Lopez 2018). Individuals and family members need to be educated about the risks of suicide and prevention strategies. The precautionary and safety measures of suicide prevention need to be ensured and implemented. There is a paucity of research on psychosocial interventions for co-occurring AUD, suicidal ideation and behavior (Rizk 2021). Hence, future studies can be focused on psychosocial intervention for suicidal ideation in AUD.
Limitation:
Small sample size was one of the major limitation of the study. The study has sampling bias as it included the individuals treated for substance use disorder in a tertiary care government hospital. Hence, the study results cannot be generalized
Conclusion
The prevalence of suicidal ideations is high among persons with alcohol use disorder. As a standard operating procedure, psychosocial intervention must include suicide risk assessment and prevention. Evidence-based and low-cost interventions can prevent suicide. For the effective implementation of such interventions, multidisciplinary strategies are needed.
Flow Chart showing study procedure
Acknowledgement
This work was supported by Indo-US Fogarty Post-Doctoral Fellowship Training in Chronic Non-Communicable Disorders Across Lifespan Grant #1D43TW009120 (Ezhumalai Sinu, Fellow; LB Cottler, PI)
Source of Funding: The study was funded by Ministry of Health & Family Welfare, Govt of India in collaboration with National Institute of Mental Health and Neurosciences under Manpower Development in Mental Health (2018–2020).
Footnotes
Conflict of Interest: Nil
References
- Abdalla RR, Miguel AC, Brietzke E, Caetano R, Laranjeira R&Madruga CS (2019). Suicidal behavior among substance users: data from the Second Brazilian National Alcohol and Drug Survey (II BNADS). Revistabrasileira de psiquiatria (Sao Paulo, Brazil: 1999), 41(5), 437–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Tillman R & Grucza RA, et al. (2017). Reciprocal relationships between substance use and disorders and suicidal ideation and suicide attempts in the Collaborative Study of the Genetics of Alcoholism. Journal of Affective Disorders, 213, 96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady J (2006). The association between alcohol misuse and suicidal behaviour. Alcohol and alcoholism (Oxford, Oxford shire), 41(5), 473–478. [DOI] [PubMed] [Google Scholar]
- Chachamovich E, Ding Y&Turecki G (2012). Levels of aggressiveness are higher among alcohol-related suicides: results from a psychological autopsy study. Alcohol 46(6), 529–536. [DOI] [PubMed] [Google Scholar]
- Conner KR, Beautrais AL& Conwell Y (2003). Moderators of the relationship between alcohol dependence and suicide and medically serious suicide attempts: analyses of Canterbury Suicide Project data. Alcoholism, clinical and experimental research, 27(7), 1156–1161. [DOI] [PubMed] [Google Scholar]
- Harmer B, Lee S, Duong T& Saadabadi A (2021). Suicidal Ideation. In Stat Pearls. Stat Pearls Publishing. [PubMed] [Google Scholar]
- Harris EC & Barraclough B (1997). Suicide as an outcome for mental disorders. A meta-analysis. The British Journal of Psychiatry, 170, 205–228. [DOI] [PubMed] [Google Scholar]
- Holmstrand C, Bogren M, Mattisson C&Brådvik L (2015). Long-term suicide risk in no, one or more mental disorders: the Lundby Study 1947–1997. Acta Psychiatrica Scandinavia, 132(6), 459–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hufford MR (2001). Alcohol and suicidal behavior. Clinical Psychology Review, 21(5), 797–811. [DOI] [PubMed] [Google Scholar]
- Inskip HM, Harris EC&Barraclough B (1998). Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. The British Journal of Psychiatry, 172, 35–37. [DOI] [PubMed] [Google Scholar]
- Kachadourian LK, Gandelman E, Ralevski E& Petrakis IL (2018). Suicidal ideation in military veterans with alcohol dependence and PTSD: The role of hostility. The American Journal on Addictions, 27(2), 124–130. [DOI] [PubMed] [Google Scholar]
- Kamalja KK& Khangar NV (2017). A statistical study of suicidal behavior of Indians. Egyptian Journal of Forensic Sciences, 7(1), 1–14.28781894 [Google Scholar]
- Kaur R, Krishna PS, Ravinder E, Sahithi JK & Dattatrey M (2013). Psychiatric disorders in adult males with alcohol dependence—a study in Telangana region of Andhra Pradesh. Int J Res Med, 2(2), 80–86. [Google Scholar]
- Kessler RC, Borges G & Walters EE (1999). Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry, 56(7), 617–626. [DOI] [PubMed] [Google Scholar]
- Lee M, Lee U, Park JH, Shin YC, Sim M, Oh KS & Shin DW, et al. (2021). The Association Between Alcohol Use and Suicidal Ideation Among Employees. Psychiatry investigation, 18(10), 977–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester D (2000). Alcoholism, substance abuse, and suicide. In: Maris RW, Berman AL, Silverman MM. Comprehensive Textbook of Suicidology. New York, The Guilford Press, 357–75. [Google Scholar]
- López-Goñi JJ, Fernández-Montalvo J, Arteaga A&Haro B (2019). Suicidal attempts among patients with substance use disorders who present with suicidal ideation. Addictive Behaviors, 89, 5–9. [DOI] [PubMed] [Google Scholar]
- López-Goñi JJ, Fernández-Montalvo J, Arteaga A&Haro B (2018). Suicidal ideation and attempts in patients who seek treatment for substance use disorder. Psychiatry Research, 269, 542–548. [DOI] [PubMed] [Google Scholar]
- Matsumoto T, Matsushita S, Okudaira K, Naruse N, Cho T, Muto T & Ashizawa T et al. (2012). Sex differences in risk factors for suicidality among Japanese substance use disorder patients: association with age, types of abused substances, and depression. Psychiatry and clinical neurosciences, 66(5), 390–396. [DOI] [PubMed] [Google Scholar]
- NCRB. Accidental deaths and suicides in India. (2020). Ministry of Home Affairs, The Government of India, New Delhi. [Google Scholar]
- Nemtsov A (2003). Suicides and alcohol consumption in Russia, 1965–1999. Drug and alcohol dependence, 71(2), 161–168. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Currier D, Liu SM, Hasin DS, Grant BF& Blanco C (2010). Increased risk for suicidal behavior in comorbid bipolar disorder and alcohol use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The Journal of Clinical Psychiatry, 71(7), 902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pederson CL (2018). The Importance of Screening for Suicide Risk in Chronic Invisible Illness. J Health Sci Educ, 2(4),141 [Google Scholar]
- Pirkola SP, Suominen K& Isometsä ET (2004). Suicide in alcohol-dependent individuals: epidemiology and management. CNS drugs, 18(7), 423–436. [DOI] [PubMed] [Google Scholar]
- Pompili M, Serafini G, Innamorati M, Dominici G, Ferracuti S, Kotzalidis GD & Serra G, et al. (2010). Suicidal behavior and alcohol abuse. International journal of environmental research and public health, 7(4), 1392–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA &Currier GW, Melvin GA, Greenhill L, Shen S, & Mann JJ (2011). The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. The American journal of psychiatry, 168(12), 1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizk MM, Herzog S, Dugad S, & Stanley B (2021). Suicide Risk and Addiction: The Impact of Alcohol and Opioid Use Disorders. Current addiction reports, 1–14. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Cintas L, Daigre C, Braquehais MD, Palma-Alvarez RF, Grau-López L, Ros-Cucurull E & Rodríguez-Martos L, et al. (2018). Factors associated with lifetime suicidal ideation and suicide attempts in outpatients with substance use disorders. Psychiatry research, 262, 440–445. [DOI] [PubMed] [Google Scholar]
- Sakuraba S, Kubo M, Komoda T& Yamana J (2005). Suicidal ideation and alexithymia in patients with alcoholism: a pilot study. Substance use & misuse, 40(6), 823–830. [DOI] [PubMed] [Google Scholar]
- Kumar S, Kuchhal A, Dixit V & Jaiswal S (2016). Suicidal ideation and its correlates in patients of alcohol dependence syndrome. International Journal of Contemporary Medical Research, 3(5),1392–1397. [Google Scholar]
- Sher L (2006). Alcohol consumption and suicide. QJM: Journal of the Association of Physicians, 99(1), 57–61. [DOI] [PubMed] [Google Scholar]
- Sher L, Oquendo MA, Galfalvy HC, Grunebaum MF, Burke AK, Zalsman G & Mann JJ (2005). The relationship of aggression to suicidal behavior in depressed patients with a history of alcoholism. Addictive behaviors, 30(6), 1144–1153. [DOI] [PubMed] [Google Scholar]
- Sreelatha P, Haritha G, Ryali VS & Janakiraman P (2019). Alcohol dependence syndromein suicide attempters:A cross-sectional study in a rural tertiary hospital. Arch Med Health Sci, 7,195–200. [Google Scholar]
- Wilcox HC, Conner KR& Caine ED (2004). Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug and alcohol dependence, 76 Suppl, S11–S19. [DOI] [PubMed] [Google Scholar]
- Wojnar M, Ilgen MA, Czyz E, Strobbe S, Klimkiewicz A, Jakubczyk A& Glass J, et al. (2009). Impulsive and non-impulsive suicide attempts in patients treated for alcohol dependence. Journal of Affective Disorders, 115 (1–2), 131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo JH, Jang JH & Park JS (2019). The influence factors of suicidal ideation of patients with alcohol dependence. Int J Innovative Technology and Exp Engineering, 8,72–78. [Google Scholar]
- World Health Organisation. (2014). Preventing suicide: A Global imperative. World Health Organisation. [Google Scholar]
- World Health Organization. (2018). National suicide prevention strategies: progress, examples and indicators. World Health Organization. [Google Scholar]
- Yuodelis-Flores C&Ries RK (2015). Addiction and suicide: A review. The American Journal on Addictions, 24(2), 98–104. [DOI] [PubMed] [Google Scholar]