As of March, 2022, just over 1 year has passed since the authorisation of first-generation vaccines against COVID-19. Since then, almost 10 billion doses of COVID-19 vaccines have been administered globally.1 Although the delivery of this number of vaccines is a remarkable achievement, there is still a disparity in vaccine equity, access, and affordability between high-income and low-income countries. According to the Global Dashboard for Vaccine Equity (established by the UN Development Programme, WHO, and the University of Oxford), as of Jan 18, 2022, approximately 67·6% of people in high-income countries have had at least one dose, compared with only approximately 11·36% of people in low-income countries.2 This inequity has major negative implications for global pandemic control; thus, there is an imperative to develop more affordable, scalable, and easily distributable vaccines.
In the current landscape of mRNA, viral vector, and inactivated COVID-19 vaccines, one modality that has been largely under-represented is DNA vaccines. In The Lancet, Akash Khobragade and colleagues3 report an interim analysis of a phase 3, randomised, double-blind, placebo-controlled study of a DNA vaccine, ZyCoV-D, against COVID-19. The vaccine contains a 2 mg dose of a DNA plasmid (pVAX-1) expressing the Wuhan Hu-1 spike antigen of SARS-CoV-2 and an IgE signal peptide, which is delivered intradermally using a needle-free injection system. Participants received three doses of vaccine or placebo at 28-day intervals. The primary outcome of this study was the number of participants with first occurrence of symptomatic COVID-19, as determined by a symptomatic RT-PCR test 28 days after the third dose, until the targeted number of 158 cases was achieved. Between Jan 16 and June 23, 2021, 27 703 participants (aged >12 years) were randomly assigned (1:1) to receive ZyCoV-D (n=13 851) or placebo (n=13 852), and 81 cases were eligible for the interim primary efficacy endpoint as per protocol, which yielded a vaccine efficacy of 66·6% (20 cases in the ZyCoV-D group and 61 in the placebo group). There was full protection against more severe disease and death. It is important to keep in mind that this study was done during a surge of the B.1.617.2 (delta) variant in India, and the study population was predominantly male (18 592 [67·11%] male and 9111 [32·89%] female), with no ethnicity data reported. Furthermore, the efficacy analysis was not stratified for age. Age is a known determinant of both COVID-19 outcomes and vaccine effectiveness. Finally, the efficacy analysis was only performed after the third dose, limiting insight into the effect of the first and second doses—this is useful information where incomplete vaccination could occur.
The vaccine was found to be safe, with approximately equivalent prevalence of solicited adverse events between the ZyCoV-D (n=623) and placebo (n=620) groups. The authors state that the safety profile of ZyCoV-D is comparable to another DNA-based vaccine in development.4 Notably, ZyCoV-D was found to be stable at room temperature (25°C) for 2 months in initial studies, although it was stored at 2–8°C for this study. Based on the safety, immunogenicity, and efficacy findings from the phase 3 trial, ZyCoV-D has been granted Emergency Use Authorisation in India: a landmark milestone for DNA vaccines with potential to further contribute to the COVID-19 vaccine diversity and worldwide supply.
Despite decades of research and development of DNA vaccines, including at least eight candidates currently in clinical trials for COVID-19,5 they have had limited success. One of the main challenges for DNA vaccines is the delivery: mRNA vaccines need to cross only one membrane to reach their site of action (cytoplasm), whereas DNA vaccines need to cross the cytoplasm and the nuclear membrane. Because of this difference, the lipid nanoparticles that effectively deliver mRNA do not work as well for DNA. Historically, DNA vaccines have required a physical method of delivery such as electroporation, or the needle-free injection system used in this study.6, 7, 8 Although these physical devices appear to be effective—as shown in this study—they pose a potential challenge for widespread use and scale-up. The device used in Khobragade and colleagues’ study3 is small and portable (<50 g) and consists of an injector, syringe, and filling adapter. However, widespread administration of ZyCoV-D will be limited not only by production and availability of the DNA, but also the injection device, which is vulnerable to global manufacturing disruptions. If these delivery system challenges can be overcome then the amenable storage conditions, efficacy against COVID-19 (including the delta strain), and low cost (<US$10) have poised ZyCoV-D to be another global solution in our fight against SARS-CoV-2, and might act as a catalyst for DNA-based vaccines against other diseases, such as tuberculosis and HIV-1, especially in areas that have restricted access and affordability.
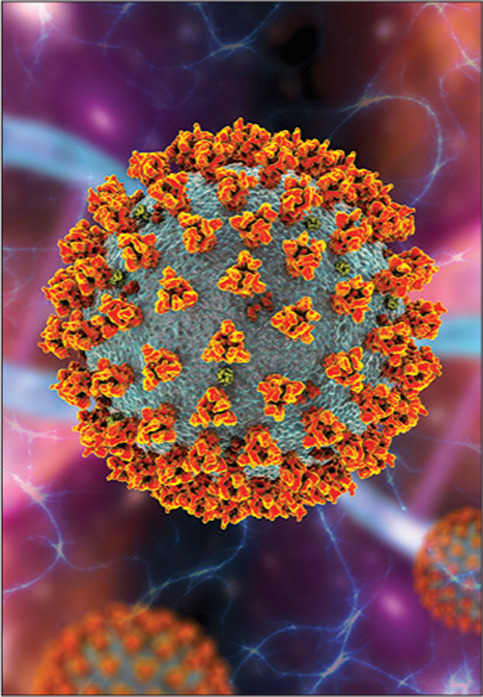
© 2022 Kateryna Kon\Science Photo Library
AKB is a co-founder and reports holding shares in VaxEquity, a for-profit company that aims to develop self-amplifying RNA vaccines for infectious diseases, but is not currently actively involved in the company. VaxEquity does not produce DNA vaccines. L-GB has received honoraria from Gilead Sciences and Merck for advisory work in HIV prevention.
References
- 1.Our World in Data Coronavirus (COVID-19) vaccinations. 2022. https://ourworldindata.org/covid-vaccinations?country=OWID_WRL
- 2.UN Development Programme Vaccine access. https://data.undp.org/vaccine-equity/accessibility/
- 3.Khobragade A, Bhate S, Ramaiah V, et al. Efficacy, safety, and immunogenicity of the DNA SARS-CoV-2 vaccine (ZyCoV-D): the interim efficacy results of a phase 3, randomised, double-blind, placebo-controlled study in India. Lancet. 2022;399:1313–1321. doi: 10.1016/S0140-6736(22)00151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tebas P, Yang S, Boyer JD, et al. Safety and immunogenicity of INO-4800 DNA vaccine against SARS-CoV-2: a preliminary report of an open-label, phase 1 clinical trial. EClinicalMedicine. 2021;31 doi: 10.1016/j.eclinm.2020.100689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheridan C. First COVID-19 DNA vaccine approved, others in hot pursuit. Nat Biotechnol. 2021;39:1479–1482. doi: 10.1038/d41587-021-00023-5. [DOI] [PubMed] [Google Scholar]
- 6.Lee J, Arun Kumar S, Jhan YY, Bishop CJ. Engineering DNA vaccines against infectious diseases. Acta Biomaterialia. 2018;80:31–47. doi: 10.1016/j.actbio.2018.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Modjarrad K, Roberts CC, Mills KT, et al. Safety and immunogenicity of an anti-Middle East respiratory syndrome coronavirus DNA vaccine: a phase 1, open-label, single-arm, dose-escalation trial. Lancet Infect Dis. 2019;19:1013–1022. doi: 10.1016/S1473-3099(19)30266-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gaudinski MR, Houser KV, Morabito KM, et al. Safety, tolerability, and immunogenicity of two Zika virus DNA vaccine candidates in healthy adults: randomised, open-label, phase 1 clinical trials. Lancet. 2018;391:552–562. doi: 10.1016/S0140-6736(17)33105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


