Abstract
Purpose
Hospital policies forbidding or limiting families from visiting relatives on the intensive care unit (ICU) has affected patients, families, healthcare professionals, and patient- and family-centered care (PFCC). We sought to refine evidence-informed consensus statements to guide the creation of ICU visitation policies during the current COVID-19 pandemic and future pandemics and to identify barriers and facilitators to their implementation and sustained uptake in Canadian ICUs.
Methods
We created consensus statements from 36 evidence-informed experiences (i.e., impacts on patients, families, healthcare professionals, and PFCC) and 63 evidence-informed strategies (i.e., ways to improve restricted visitation) identified during a modified Delphi process (described elsewhere). Over two half-day virtual meetings on 7 and 8 April 2021, 45 stakeholders (patients, families, researchers, clinicians, decision-makers) discussed and refined these consensus statements. Through qualitative descriptive content analysis, we evaluated the following points for 99 consensus statements: 1) their importance for improving restricted visitation policies; 2) suggested modifications to make them more applicable; and 3) facilitators and barriers to implementing these statements when creating ICU visitation policies.
Results
Through discussion, participants identified three areas for improvement: 1) clarity, 2) accessibility, and 3) feasibility. Stakeholders identified several implementation facilitators (clear, flexible, succinct, and prioritized statements available in multiple modes), barriers (perceived lack of flexibility, lack of partnership between government and hospital, change fatigue), and ways to measure and monitor their use (e.g., family satisfaction, qualitative interviews).
Conclusions
Existing guidance on policies that disallowed or restricted visitation in intensive care units were confusing, hard to operationalize, and often lacked supporting evidence. Prioritized, succinct, and clear consensus statements allowing for local adaptability are necessary to guide the creation of ICU visitation policies and to optimize PFCC.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12630-022-02235-y.
Keywords: COVID-19, intensive care unit, policy, visiting policies
Résumé
Objectif
Les politiques hospitalières interdisant ou limitant les visites des familles à des proches à l’unité de soins intensifs (USI) ont affecté les patients, les familles, les professionnels de la santé et les soins centrés sur le patient et la famille (SCPF). Nous avons cherché à affiner les déclarations de consensus fondées sur des données probantes afin de guider la création de politiques de visite aux soins intensifs pendant la pandémie actuelle de COVID-19 et les pandémies futures, et dans le but d’identifier les obstacles et les critères facilitants à leur mise en œuvre et à leur adoption répandue dans les unités de soins intensifs canadiennes.
Méthode
Nous avons créé des déclarations de consensus à partir de 36 expériences fondées sur des données probantes (c.-à-d. impacts sur les patients, les familles, les professionnels de la santé et les SCPF) et 63 stratégies fondées sur des données probantes (c.-à-d. moyens d’améliorer les restrictions des visites) identifiées au cours d’un processus Delphi modifié (décrit ailleurs). Au cours de deux réunions virtuelles d’une demi-journée tenues les 7 et 8 avril 2021, 45 intervenants (patients, familles, chercheurs, cliniciens, décideurs) ont discuté et affiné ces déclarations de consensus. Grâce à une analyse descriptive qualitative du contenu, nous avons évalué les points suivants pour 99 déclarations de consensus : 1) leur importance pour l’amélioration des politiques de restriction des visites; 2) les modifications suggérées pour les rendre plus applicables; et 3) les critères facilitants et les obstacles à la mise en œuvre de ces déclarations lors de la création de politiques de visite aux soins intensifs.
Résultats
En discutant, les participants ont identifié trois domaines à améliorer : 1) la clarté, 2) l’accessibilité et 3) la faisabilité. Les intervenants ont identifié plusieurs critères facilitants à la mise en œuvre (énoncés clairs, flexibles, succincts et hiérarchisés disponibles dans plusieurs modes), des obstacles (manque perçu de flexibilité, manque de partenariat entre le gouvernement et l’hôpital, fatigue du changement) et des moyens de mesurer et de surveiller leur utilisation (p. ex., satisfaction des familles, entrevues qualitatives).
Conclusion
Les directives existantes sur les politiques qui interdisaient ou limitaient les visites dans les unités de soins intensifs étaient déroutantes, difficiles à mettre en oeuvre et manquaient souvent de données probantes à l’appui. Des déclarations de consensus hiérarchisées, succinctes et claires permettant une adaptabilité locale sont nécessaires pour guider la création de politiques de visite en soins intensifs et pour optimiser les soins centrés sur le patient et la famille.
When the World Health Organization declared COVID-19 a global pandemic, many hospitals implemented visitation restrictions to mitigate viral transmission,1 conserve personal protective equipment (PPE), and protect hospital staff from increased exposure risk. Families of critically ill patients were often not allowed to visit, though some hospitals made exceptions (e.g., at end of life).2 The lack of family presence disrupted the delivery of patient- and family-centered care (PFCC), which is integral in the intensive care unit (ICU).3 Families were not present to provide in-person emotional support for critically ill patients,4 attend ICU rounds,5 or share individual patient preferences, needs, and values with members of the healthcare team. The absence of family at the bedside made it more challenging for the healthcare team to keep families informed about patient progress, thereby rendering families less prepared to participate in shared decision-making, especially when changes in patient condition necessitated the re-evaluation of the patient’s goals of care.6–10 Restrictive visitation policies have been associated with mental health consequences for families (e.g., symptoms of acute stress disorder),11,12 delayed goals of care conversations,13 negative consequences for healthcare professionals (e.g., moral distress, compassion fatigue, and burnout with staff leaving leave their jobs),14–16 and other adverse outcomes (e.g., increased sepsis rates, decreased patient ratings of medical staff responsiveness, mistrust in healthcare team).17,18
Given the global pandemic continues with many unknown factors (e.g., variants of concern, and availability and effectiveness of vaccines and treatments), future outbreaks are expected, therefore evidence-informed guidance is needed for the development of hospital visitation policies. We embarked on a multiphase research program examining the impact of restricted visitation policies during COVID-19, starting during the first wave of the pandemic (May 2020), which included the following incremental phases:
environmental scan of Canadian hospital/ICU visitation policies to describe the extent of restricted visitation policies across Canada,2
scoping review of the literature and interviews with patients, families, and healthcare professionals to describe the impacts of restricted visitation policies and strategies to mitigate these impacts,19
modified Delphi consensus process to rate and rank key experiences and strategies (derived from phases 1 and 2 and leading to the formation of 36 evidence-informed experiences and 63 evidence-informed strategies) and to organize these experiences and strategies into consensus statements,20 and
national stakeholder meeting to refine (subject of this report) and subsequently re-rank identified consensus statements during the stakeholder meeting (modified Delphi consensus process round 3) and discuss implementation considerations (subject of this report).
To accelerate the adoption of evidence-informed consensus statements at the level of health systems, it is essential to understand the barriers to their implementation and the facilitators of their sustained uptake. The objective of this study was to engage stakeholders to 1) refine the presentation/wording/communication of consensus statements from our previous work2,19,20 to be more applicable and meaningful to the current issues experienced by ICU patients, families, and healthcare professionals; and 2) identify facilitators and barriers associated with the uptake of these consensus statements. The findings of this meeting will inform the refinement and implementation of these consensus statements to guide the creation of ICU visitation policies during the current and future pandemics.
Methods
Study design
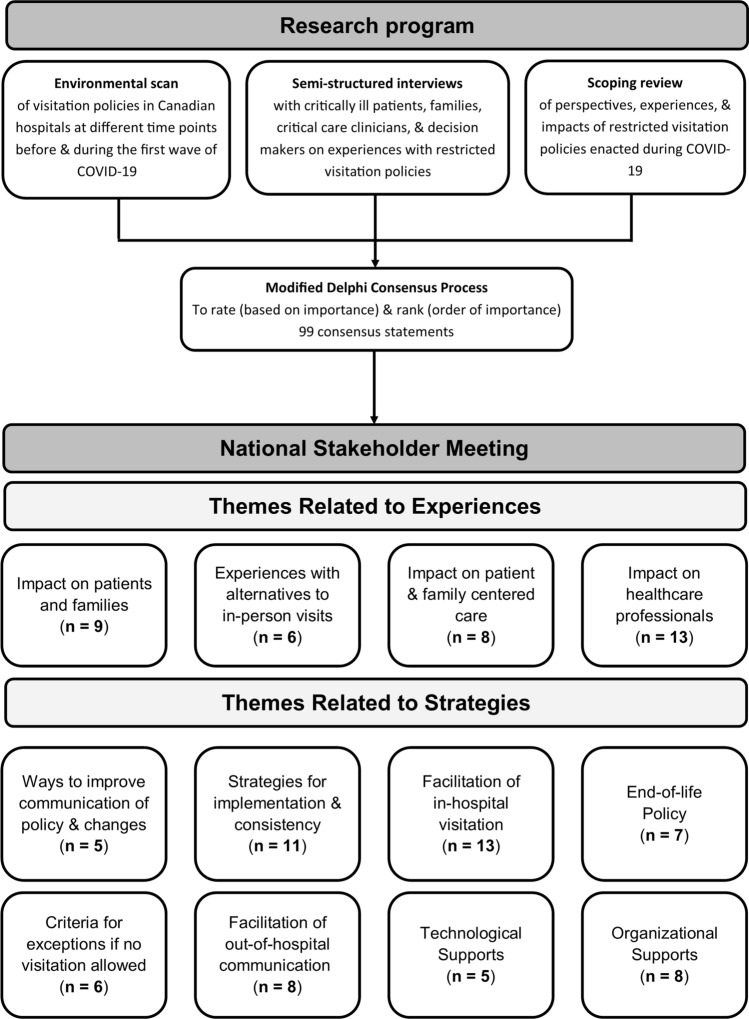
We created consensus statements from 36 evidence-informed experiences (i.e., impacts on patients, families, healthcare professionals, and PFCC) and 63 evidence-informed strategies (i.e., ways to improve restricted visitation) identified during a modified Delphi process20 in the restricted visitation multiphase research program, and thematically analyzed these statements into 12 themes (Fig. 1). We emailed a meeting agenda with consensus statements to participants one week prior to the two half-day virtual meeting (held via Zoom videoconferencing [Zoom Video Communications, Inc., San Jose, CA, USA]).
Fig. 1.
Overview of research program and themes discussed during the national stakeholder meeting. Numbers (n) refer to the number of related items in each theme.
Participants
Attendees included 45 individual stakeholders (patients, families, researchers, front-line critical care clinicians, decision-makers) who self-identified as being directly impacted by COVID-19 restricted visitation policies (Table 1). We purposively recruited participants from prior stages of the research program. This meeting received ethical approval from the University of Calgary’s Conjoint Health Research Ethics Board (REB20-0944). Participants provided informed consent prior to participating in the meeting. We reported this study in accordance with the Consolidated Criteria for Reporting Qualitative Research checklist (Electronic Supplementary Material [ESM] eTable 1).21
Table 1.
Participant characteristics of National Stakeholder Meeting
| Characteristic | n/total N (%) |
|---|---|
| Age category, yr | |
| 20–29 | 4/45 (9%) |
| 30–39 | 12/45 (27%) |
| 40–49 | 15/45 (33%) |
| 50–59 | 10/45 (22%) |
| 60–69 | 4/45 (9%) |
| Sex | |
| Female | 25/45 (56%) |
| Ethnic origin* | |
| North American | 26/45 (58%) |
| British Isles | 12/45 (27%) |
| Western European | 9/45 (20%) |
| East and Southeast Asian | 4/45 (9%) |
| South Asian | 4/45 (9%) |
| Eastern European | 2/45 (4%) |
| Northern European | 1/45 (2%) |
| Indigenous | 1/45 (2%) |
| Prefer not to answer | 0/45 (0%) |
| Southern European | 0/45 (0%) |
| Latin, Central, and South American | 0/45 (0%) |
| Ocean and Pacific Islands | 1/45 (2%) |
| Province | |
| British Columbia | 1/45 (2%) |
| Alberta | 20/45 (44%) |
| Saskatchewan | 3/45 (7%) |
| Manitoba | 2/45 (4%) |
| Ontario | 12/45 (27%) |
| Quebec | 3/45 (7%) |
| Nova Scotia | 2/45 (4%) |
| New Brunswick | 0/45 (0%) |
| Newfoundland & Labrador | 0/45 (0%) |
| Prince Edward Island | 1/45 (2%) |
| Territories (Northwest Territories, Nunavut, and Yukon) | 1/45 (2%) |
| Stakeholder group* | |
| Patient1 | 3/45 (7%) |
| Family members2 | 2/45 (4%) |
| Nurse | 9/45 (20%) |
| Physician | 20/45 (47%) |
| Researcher | 8/45 (18%) |
| Respiratory therapist | 5/45 (11%) |
| Social worker | 1/45 (2%) |
| Physiotherapist | 3/45 (7%) |
| Decision-maker3 | 8/45 (18%) |
*Participants self-selected their stakeholder group. As such, responses are not mutually exclusive and add up to more than 100%.
1None were hospitalized for COVID-19
2None were family members of patients hospitalized for COVID-19
3Decision-makers included a program director, a provincial clinical services lead, a health zone manager, an administrator of a network of teaching hospitals, a unit manager, a medical director, a research manager, a research chair in pandemic preparedness, and a health authority provincial medical director of pandemic critical care
Meeting activities
The two half-day meetings included the final two rounds of the Delphi consensus process, which are presented elsewhere20 and two breakout sessions (described in ESM eAppendix 1). Participants were divided into six groups for day 1 and six different groups for day 2 (5 ± 1 participant per group). Where possible, groups included representatives from each key stakeholder group. Each group was assigned one research assistant trained in qualitative methods to facilitate the discussion and one notetaker to record observations. The aims of the meeting were for stakeholders to: 1) discuss and refine consensus statements created from the Delphi consensus process20 (ESM eAppendix 2) (day 1) and 2) discuss implementation of the consensus statements that included evidence-informed strategies to improve restricted visitation (i.e., themes 5–12, Fig. 1). Although stakeholder experiences (i.e., themes 1–4, Fig. 1) are relevant to the context of visitation policies, they are unlikely to inform policies and thus were not included (ESM eAppendix 3).
Data analysis
Each breakout session was audio-recorded, transcribed verbatim, reviewed for accuracy of transcription, deidentified, and imported into NVivo-12 (QSR International, Melbourne, Australia) for data organization and analysis. Data analysis incorporated both deductive (i.e., guided by predetermined objectives to understand implementation of the consensus statements) and data-driven inductive approach to coding. Five researchers (K. K., N. J., L. H., K. M., E. S.) conducted qualitative, thematic content analysis on the transcribed recordings, independently and in duplicate.22 The same researchers met regularly to discuss emerging themes, resolve discrepancies, and develop a list of codes. Coding discrepancies were resolved through discussion and, if necessary, reviewed by a third researcher (K. F.). The researchers kept an audit trail to track the evolving analysis and used a reflexive journal to enhance the study’s methodological rigor. Four of the five researchers then systematically applied the final list of codes to all transcripts.
Results
Considerations for refining and compiling consensus statements
Analysis from the day 1 discussions identified that consensus statements could be improved in three areas: 1) clarity, 2) accessibility, and 3) feasibility. Electronic Supplementary Material eTable 2 includes the original (from the modified Delphi process) and refined (from the stakeholder meeting) consensus statements. Final prioritized and refined recommendation consensus statements (from the stakeholder meeting) are included in Table 2.
Table 2.
Prioritized and refined restricted visitation policy recommendations for implementation
| Domain 2: Recommendations |
|---|
| Theme 5: Ways to improve communication of restricted visitation policy and policy changes |
| Communicate policy changes to hospital staff during regular working hours and at least 24 hr before the change becomes effective or is communicated to the public (i.e., all staff should know the policy change before the media does). |
| Create multiple vehicles of communication of current restricted visitation policies at each institution (e.g., website, electronic messaging subscriptions, portal for families to ask questions or submit appeals to visitor restriction policies). |
| Theme 6: Strategies for restricted visitation policy implementation and consistency |
| Assign designated staff members to address questions regarding visitation and policy changes, address concerns, exceptions, and appeals, and consistently apply the policy (e.g., authoritative decision-makers that do not allow for special circumstances to occur, support from patient relations department, hospital liaison individual or team that families can contact, designated staff members to communicate outcome back to front-line staff). |
| Permit hospitals to adapt provincial policies for their facilities and individual units (e.g., ICUs are permitted to adjust their restricted visitation policies). |
| Include key stakeholders in policy development and adaptation (e.g., patients and families, nurses, physicians, spiritual care providers, allied health professionals, decision-makers, infection prevention and control expert). |
| Implement a clear, straightforward, timely and accessible process to request exceptions and appeals to restricted visitation polices (e.g., end of life, other adults that would benefit from being present). |
| Create proactive and staged implementation of restricted visitation policies that are dependent on community COVID-19 caseload or hospital capacity and patient circumstances (e.g., hospitals with no COVID-19 cases should be able to modify the policy). These policies may differ for essential care providers and visitors. |
| Theme 7: Facilitation of in-hospital visitation for families and visitors |
| Do not exclude children from visitation if they visit with an adult who ensures they comply with public health recommendations (e.g., PPE, hand washing, physical distancing). |
| Implement a straightforward process to appeal the restricted visitation policy. |
| Designate unit-level “visitor advisors” if feasible. The role of these “visitor advisors” may include the following: communicate the policy, demonstrate donning and doffing of PPE, teach proper handwashing, answer questions, inform visitor what to expect on the unit, communicate consequences for noncompliance with hospital PPE policies, etc. |
| Allow one designated visitor per patient at a time but allow the designated visitor to be changed to include multiple visitors throughout the patient's ICU stay. |
| Theme 8: End-of-life policy |
| Visitors are permitted at all times for end of life regardless of patient's COVID-19 status. If a patient is COVID-19 positive, this should be accompanied with a well-defined protocol (e.g., informing families of risk, requiring PPE, self-isolation, hand washing, and COVID-19 testing). |
| Create a clear policy for end of life. This should include clear rules on the number of people who can visit, consider end-of-life process for other cultural backgrounds, and when visitors are COVID-19 positive. This end-of-life policy should include a clear definition of end of life, which allows visitors while patient is lucid and able to interact (i.e., not comatose at end of life). |
| Theme 9: Criteria for visitation exceptions if no visitation is allowed |
| Allow visitation for all critically ill patients regardless of the patient’s COVID-19 status (e.g., implement clinical follow up with the family members who must agree to comply with confinement measures at home and to alert the healthcare team if symptoms appear in the next 14 days). |
| Consider family caregivers as an integral member of the healthcare team, and a distinct entity from visitors (e.g., consider family presence or families to be essential care partners). |
| Theme 10: Facilitation of out of hospital communication with family or visitors |
| Provide videoconferencing options to family members and patients who are separated. |
| An effort should be made to provide frequent (medical) updates (including allied healthcare) to the family and provide opportunities for families to ask questions. |
| Designate one to two identified family spokespersons to be notified in advance of daily virtual rounds, participate in clinical decision-making, and receive and disseminate family updates. |
| Theme 11: Technological supports to facilitate communication during restrictions |
| Increase availability of technological devices to facilitate family involvement in daily rounds, family conferences, virtual visits, and communication of family messages to patient (e.g., iPads, tablets, phones, etc.) including tech support for staff and family. |
| Theme 12: Organizational supports |
| Provide clear and consistent messaging to staff about visitation policy; clearly outline circumstances when policy exceptions can apply or defer designated visitor approvals to senior leadership. |
| Provide mental health supports (e.g., self-care and coping strategies, bereavement, wellness, etc.) for families, patients, and staff, including onsite support options for staff. |
ICU = intensive care unit; PPE = personal protective equipment
Clarity
Participants discussed several issues regarding the clarity of the proposed consensus statements. Exemplar quotations and select statements are included in ESM eTable 3. For example, participants were concerned about the ambiguity of the term “family” used in some of the consensus statements. Several participants suggested that “family” be more explicitly defined because it may affect who is permitted to visit (quotation 1 [Q1]). Moreover, participants felt that “family” should be considered distinct from “visitors” and proposed the use of the phrase “essential care partners” instead (Q2). Others also noted the ambiguity in using the word “children” in the consensus statements. Participants suggested ways to clarify the use of the word “children” in the statements, such as “children who are under the age of 16” (Q3) and making exceptions for specific situations (Q4). Lastly, participants agreed that it is important for a statement that included visitation at the end of life to clearly state “while the patient is lucid and able to interact” (Q5), based on their experiences of family only being able to visit after the patient was intubated or confused and delirious (Q6) and not being able to visit while a patient was lucid and not intubated.
Accessibility
Several participants identified that some consensus statements referred to information/personnel/devices that were not accessible to all stakeholders or ICUs (e.g., technology, Wi-Fi, personnel such as an ICU liaison or accessible infection and prevention control expert) (Q7, Q8). Participants recommended addressing these accessibility gaps by amending statements to be more inclusive. For example, one statement referred to using a website to communicate policies. Participants suggested that this statement should include multiple modes of information (e.g., website, pamphlet, notes, in-person) to improve accessibility to the most up-to-date hospital visitation policies (Q9). Moreover, participants suggested amending recommendations to include the word “accessible” such as accessible education information on “infection prevention and control standards” (Q10), accessible supports to debrief among healthcare professionals, and accessible technology literacy support for families and healthcare professionals (Q11).
Participants reworded consensus statements to accurately reflect inequitable access experiences and to use more inclusive language (Q12). Communication barriers between healthcare workers and patients/families or between patients and families (i.e., language, cognitive difficulties, delirium, hearing impairment, translation issues) were added to existing statements regarding the impact of PFCC during restricted visitation (Q13). Geographic considerations (i.e., quarantine for visitors), socioeconomic considerations (i.e., lack of portable devices, Wi-Fi, technical literacy), and cultural and spiritual considerations (i.e., end-of-life practices, ceremonies, familial relationships, last rites) were incorporated as inclusive considerations to consensus statements (Q14).
Feasibility
Time, physical space, coordination efforts, jurisdictional differences, and budgetary considerations were added to make statements more universally feasible since “depending on which hospital you’re at, the policies were different” (Q15). For example, participants agreed with one statement that policy changes should be communicated during regular working hours but added extra context that all staff should be informed about the change before the media (Q16). Participants also agreed that a designated “greeter” would be helpful, though not all agreed it would be feasible (Q17). One statement included designated outdoor spaces for physician-family interaction, which was not deemed feasible in the winter months or with increased healthcare professional workload (Q18). Some participants suggested wording to reflect variable COVID-19 experiences, patient volume in different geographical places, and evolving changes (Q19, Q20) to make statements more generalizable.
Facilitators and barriers
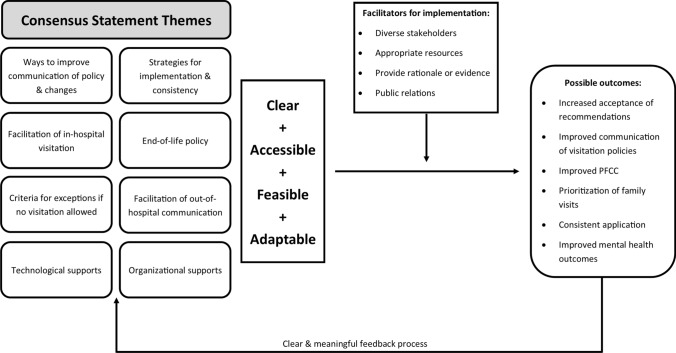
Participant discussions of implementation centered on the facilitators and barriers of consensus statements and how the consensus statements should be measured and monitored (Fig. 2).
Fig. 2.
Conceptual pathway of factors required for the implementation of consensus statements, which could improve communication, consistent application of visitation policies, and patient-and family-centered care (PFCC).
Participants discussed several barriers to the implementation of consensus statements, many of which related to the dynamic pandemic circumstances. Exemplar quotations are listed in ESM eTable 4. These included consensus statement-related factors such as the number of (and length of) consensus statements (i.e., difficult to implement or communicate) (Q21) or their perceived lack of flexibility that would prevent them from being adapted to local contexts (Q22). Consensus statement-related factors also included external barriers such as changes to public health orders that affect the hospital visitation policy (Q23, Q24) and perceived lack of partnership between the government and hospital staff (Q25). Participants discussed several barriers at the individual level, which included individual values (i.e., healthcare professionals that do not follow the process), capacity (i.e., available time to check changes/e-mail), and emotions (e.g., fear, exhaustion). Participants shared their experience with “change fatigue”, which may affect the implementation of consensus statements (Q26). Participants also expressed that “The staff [are] tired, the administrators are tired because they have a hard time to find staff to take care of patients. So to ask them to implement something very complex, would probably just not work at this point” (Q27). One participant reflected that, at the beginning of the pandemic, fear for safety (i.e., of visitors, staff, and community) “was the motivating factor behind us putting really strict family visitation in” (Q28). Though, with the vast majority of the staff being vaccinated (i.e., facilitator), this fear has dissipated to some degree compared with at the beginning of the pandemic (Q29).
Participants discussed the factors that should be prioritized during strategy implementation. These were: 1) structure of the consensus statements (e.g., content, format), 2) process of implementing the consensus statements, and 3) who to engage in implementation. Participants reiterated that the consensus statements should be structured as “guiding principles rather than strict rules” (Q30). They should be clear, direct, and concise (Q31) and should be adaptable to the local context (Q32) or based on the COVID-19 burden in the region (Q33). Participants liked the idea of these consensus statements being available in different formats, but cautioned that all formats should be version-controlled with the same effective dates to ensure consistency of messaging. Participants agreed that providing rationale for why these consensus statements are being implemented is important for stakeholder buy-in (Q34).
Given the number of consensus statements, participants felt the process for implementing these statements should either involve prioritization of strategies (i.e., those with significant impact up front) or a tiered approach (i.e., a group of statements targeting different stakeholders) (Q35). Several participants liked the option for stakeholders to provide feedback on the consensus statements, with clear (i.e., who the feedback is going to) and meaningful (i.e., how their feedback is used) feedback avenues (Q36). Some participants suggested dissemination may include informing decision-makers, ICU unit managers, and critical care societies about the consensus statements or publishing consensus statements in traditional peer-reviewed publications (Q37). Participants agreed that public awareness of the consensus statement is important but felt that, like most successful campaigns, they should engage an expert in public relations. All participants agreed that multiple stakeholders should be engaged, including patients, families, local patient or family advisory councils, government, healthcare professionals, and critical care societies.
Participants suggested several ways to measure the effect of the implementation of these consensus statements. This should include both quantitative measures (e.g., family satisfaction, surveys but not virtual/in-person visits) and qualitative measures (e.g., asking different stakeholders about their awareness and perceived impact of the consensus statements) (Q38). Participants agreed that evaluation will reveal “which parts of these policies and the way they are implemented are most meaningful and important to keep moving forward, and which might actually not be a good use of resources” (Q39).
Discussion
We brought together nationally representative Canadian stakeholders affected by restricted visitation during the COVID-19 pandemic to refine and discuss evidence-informed consensus statements on restricted visitation policies. Stakeholders suggested improving clarity, accessibility, and equity of the statements and allowing consensus statements to be adapted to local context to improve cross-national uptake. Patients, families, and healthcare professionals recommended that effective implementation of consensus statements would require prioritization of strategies and broad dissemination to increase awareness, and that monitoring the impact and awareness of these strategies would act as means of further refinement.
With the onset of the COVID-19 pandemic, there were uncertainties surrounding the severity of COVID-19 and its transmission. Hospital visitation policy decisions were made with limited data, frequently changed in response to variation in the supply of PPE and as data emerged about COVID-19 infection rates and modes of transmission.23,24 Healthcare professionals or decision-makers reported experiencing “change fatigue” due to the reported frequent changes to COVID-19-related policies and procedures25,26 and distress when a patient’s family could not be present at the bedside at the end of life.27–29 Aligned with research showing that the COVID-19 pandemic affected the mental health of the general public and front-line healthcare professionals,30–36 we found that participants shared similar experiences including change fatigue and psychological and emotional distress. As such, final consensus statements should be succinct and engage multidisciplinary stakeholders, and their implementation should be minimally burdensome. The consensus statements should be flexible to the local context such as the design and staffing of each ICU (which may differ between hospitals)37 and the local burden of COVID-19.
The findings from this research program align with the “Policy Guidance for the Reintegration of Caregivers as Essential Care Partners” created by Healthcare Excellence Canada38 for healthcare institutions. The refined consensus statements in the current study share the same foundational principles, which include that caregivers are distinct from general visitors (stringently limited in visitation time) and should be considered “essential care partners” and that patients, families, and caregivers should have a voice in the adaptation of visitation policies. The current study includes additional strategies to improve communication of policy and policy changes to patients, families, and healthcare professionals; strategies for policy implementation and consistency; facilitation of in-person/virtual visitation; and criteria to consider if visitation restrictions are necessary. Results of the research program can provide a foundation to further guide restricted visitation policies for critically ill adult populations during future waves of COVID-19 or other infectious disease outbreaks. In addition to essential care partners being important for safety and patient outcomes, family presence at the bedside is important for the family to process the critical condition of their loved one before engaging in goals of care discussions.39 We will facilitate collaborative working groups with diverse nationwide representation of stakeholders to further refine and package these consensus statements into feasible and actionable evidence-informed recommendations with planned implementation of active dissemination strategies to local decision-makers and health ministers across Canada.
This study has several strengths. First, all steps of the research program engaged a diverse group of stakeholders from Canadian regions that experienced varying burdens of COVID-19 (i.e., from few cases [e.g., Northwest Territories] to the high incidence of COVID-19 and significant burden to ICU capacity [e.g., Alberta, Ontario]). The collective studies within the research program used multiple methodologies, which informed the statements evaluated by stakeholders. Our study also has limitations. First, this meeting united stakeholders from across Canada and the findings may not be generalizable to other contexts (i.e., care settings outside the ICU and outside Canada). Second, although all target stakeholder groups were represented, there were few patients and family members. Though a variety of decision-makers were invited to participate, only in-hospital leadership and not ministry/local public health officers attended the stakeholder meeting. Third, consensus statements were synthesized prior to vaccinations and only briefly discussed within the context of upcoming vaccination. Statements will need to be revised in the setting of the vaccination campaign as visitation policies may vary by vaccination status. Future work to refine the consensus statements should aim to include more patients, families, and health workers managing visitor presence (i.e., healthcare aides, spiritual care providers, unit clerks, social workers).
Conclusions
Prioritized, succinct, clear, flexible evidence-informed consensus statements are important to guide the creation of ICU visitation policies to maintain PFCC during a pandemic. Evidence-informed consensus statements should be developed by diverse stakeholders and be made available to all persons affected by restricted visitation policies to ensure their uptake during the current and future pandemics.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgments
Author contributions
All authors made substantial contributions to this work. Kirsten M. Fiest, Karla D. Krewulak, Laura C. Hernández, Natalia Jaworska, Kira Makuk, and Emma Schalm worked on the study design, data acquisition, data analysis and interpretation. Kirsten M. Fiest, Karla D. Krewulak, and Laura C. Hernández drafted the manuscript; and all authors critically revised successive versions of the manuscript and approved the final version for submission. Kirsten M. Fiest has full access to all study data and assumes responsibility for the integrity of the data and accuracy of the analysis.
Acknowledgements
The authors would like to thank Rebecca Brundin-Mather, Melanie Columbus, Emily Fitzgerald, Chloe M. de Grood, Regan King, Madison Leia, Sara Mizen, Stephana J. Moss, and Kara Plotnikoff for assisting with breakout sessions. This study was supported by a COVID-19 Rapid Response Funding Grant to Dr. Kirsten M. Fiest from the Canadian Institutes of Health Research. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. This manuscript underwent an internal peer review process with the Canadian Critical Care Trials Group, and we thank the helpful contributions made by Dr. Ian Ball and Dr. Rachel Khadaroo.
Disclosures and source of funding
Dr. Bagshaw is supported by a Canada Research Chair in Critical Care Medicine. Dr. Burns holds a Physician Services Incorporated Mid-Career Research Award. Dr. Fowler is the H. Barrie Fairley Professor of Critical Care Medicine of the University Health Network and the University of Toronto Interdepartmental Division of Critical Care Medicine. All other authors declare no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; and no other relationships or activities that could appear to have influenced the submitted work. Dr. Kirsten Fiest has received a COVID-19 Rapid Response Funding Grant from the Canadian Institutes of Health Research to fund this study. This study is not registered in a public registry of clinical trials.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Banach DB, Bearman GM, Morgan DJ, Munoz-Price LS. Infection control precautions for visitors to healthcare facilities. Expert Rev Anti Infect Ther. 2015;13:1047–1050. doi: 10.1586/14787210.2015.1068119. [DOI] [PubMed] [Google Scholar]
- 2.Fiest KM, Krewulak KD, Hiploylee C, et al. An environmental scan of visitation policies in Canadian intensive care units during the first wave of the COVID-19 pandemic. Can J Anesth. 2021;68:1474–1484. doi: 10.1007/s12630-021-02049-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McAdam JL, Arai S, Puntillo KA. Unrecognized contributions of families in the intensive care unit. Intensive Care Med. 2008;34:1097–1101. doi: 10.1007/s00134-008-1066-z. [DOI] [PubMed] [Google Scholar]
- 4.Rose L, Yu L, Casey J, et al. Communication and virtual visiting for families of patients in intensive care during COVID-19: a UK national survey. Ann Am Thorac Soc. 2021;18:1685–1692. doi: 10.1513/AnnalsATS.202012-1500OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacobowski NL, Girard TD, Mulder JA, Ely EW. Communication in critical care: family rounds in the intensive care unit. Am J Crit Care. 2010;19:421–430. doi: 10.4037/ajcc2010656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feder S, Smith D, Griffin H, et al. "Why Couldn't I Go in To See Him?" Bereaved families' perceptions of end-of-life communication during COVID-19. J Am Geriatr Soc. 2021;69:587–592. doi: 10.1111/jgs.16993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah JR. A comedian watched her mom die from COVID on an iPad. Her live tweets will break you - June 18, 2020. Available from URL: https://www.latimes.com/lifestyle/story/2020-06-18/comedian-laurie-kilmarten-live-tweets-her-mothers-death (accessed February 2022).
- 8.Weiser N. After the Virus Came, 22 Parents Moved Into Their Children’s Hospital. The New York Times; June 10, 2020. Available from URL: https://www.nytimes.com/2020/06/10/nyregion/coronavirus-children-hospital.html (accessed February 2022).
- 9.Ness MM, Saylor J, Di Fusco LA, Evans K. Healthcare providers' challenges during the coronavirus disease (COVID-19) pandemic: a qualitative approach. Nurs Health Sci. 2021;23:389–397. doi: 10.1111/nhs.12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tandon S, Medamana J, Roccaforte JD. Searching for humanity in the time of COVID. Intensive Care Med. 2021;47:500–502. doi: 10.1007/s00134-020-06231-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zante B, Erne K, Grossenbacher J, Camenisch SA, Schefold JC, Jeitziner MM. Symptoms of post-traumatic stress disorder (PTSD) in next of kin during suspension of ICU visits during the COVID-19 pandemic: a prospective observational study. BMC Psychiatry. 2021 doi: 10.1186/s12888-021-03468-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hochendoner SJ, Amass TH, Curtis JR, et al. Voices from the pandemic: a qualitative study of family experiences and suggestions regarding the care of critically ill patients. Ann Am Thorac Soc. 2021 doi: 10.1513/AnnalsATS.202105-629OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Azad TD, Al-Kawaz MN, Turnbull AE, Rivera-Lara L. Coronavirus disease 2019 policy restricting family presence may have delayed end-of-life decisions for critically ill patients. Crit Care Med. 2021;49:e1037–e1039. doi: 10.1097/CCM.0000000000005044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bellanti F, Lo Buglio A, Capuano E, et al. Factors related to nurses' burnout during the first wave of coronavirus disease-19 in a university hospital in Italy. Int J Environ Res Public Health. 2021 doi: 10.3390/ijerph18105051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses' burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021;77:3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cook DJ, Takaoka A, Hoad N, et al. Clinician perspectives on caring for dying patients during the pandemic: a mixed-methods study. Ann Intern Med. 2021;174:493–500. doi: 10.7326/M20-6943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Honarmand K, Mehta S. Consequences of visitor restriction policies in the intensive care unit during the COVID-19 pandemic. Can J Anesth. 2021;68:1465–1470. doi: 10.1007/s12630-021-02048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silvera GAWPJSA, Studer Q. The influence of COVID-19 visitation restrictions on patient experience and safety outcomes: a critical role for subjective advocates. Patient Exp J. 2021;8:30–39. doi: 10.35680/2372-0247.1596. [DOI] [Google Scholar]
- 19.Moss SJ, Stelfox HT, Krewulak KD, et al. Impact of restricted visitation policies in hospitals on patients, family members and healthcare providers during the COVID-19 pandemic: a scoping review protocol. BMJ Open. 2021 doi: 10.1136/bmjopen-2020-048227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fiest KM, Krewulak KD, Makuk K, et al. A modified Delphi process to prioritize experiences and guidance related to ICU restricted visitation policies during the coronavirus disease 2019 pandemic. Crit Care Explor 2021; 10.1097/CCE.0000000000000562. [DOI] [PMC free article] [PubMed]
- 21.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 22.Strauss AL. Qualitative analysis for social scientists. NY, USA: Cambridge University Press; 1987. [Google Scholar]
- 23.Ongaro M. Making policy decisions under plural uncertainty: responding to the COVID-19 pandemic. Hist Philos Life Sci. 2021 doi: 10.1007/s40656-021-00411-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Manski CF. Forming COVID-19 policy under uncertainty. J Benefit Cost Anal. 2020;11:341–356. doi: 10.1017/bca.2020.20. [DOI] [Google Scholar]
- 25.Havaei F, Ma A, Staempfli S, MacPhee M. Nurses' workplace conditions impacting their mental health during COVID-19: a cross-sectional survey study. Healthcare (Basel) 2021 doi: 10.3390/healthcare9010084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ead H. Change fatigue in health care professionals–an issue of workload or human factors engineering? J Perianesth Nurs. 2015;30:504–515. doi: 10.1016/j.jopan.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Najeeb U. CMAJ Blogs 2020. Available from URL: http://cmajblogs.com/phone-call/ (accessed February 2022).
- 28.Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental health of staff working in intensive care during Covid-19. Occup Med (Lond) 2021;71:62–67. doi: 10.1093/occmed/kqaa220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hossain F, Clatty A. Self-care strategies in response to nurses' moral injury during COVID-19 pandemic. Nurs Ethics. 2021;28:23–32. doi: 10.1177/0969733020961825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Busch IM, Moretti F, Mazzi M, Wu AW, Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychother Psychosom. 2021;90:178–190. doi: 10.1159/000513733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilbiks JM, Best LA, Law MA, Roach SP. Evaluating the mental health and well-being of Canadian healthcare workers during the COVID-19 outbreak. Healthc Manage Forum. 2021;34:205–210. doi: 10.1177/08404704211021109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waring S, Giles S. Rapid evidence assessment of mental health outcomes of pandemics for health care workers: implications for the Covid-19 pandemic. Front Public Health. 2021 doi: 10.3389/fpubh.2021.629236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bekele F, Hajure M. Magnitude and determinants of the psychological impact of COVID-19 among health care workers: a systematic review. SAGE Open Med. 2021 doi: 10.1177/20503121211012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nochaiwong S, Ruengorn C, Thavorn K, et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep. 2021 doi: 10.1038/s41598-021-89700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fiest KM, Parsons Leigh J, Krewulak KD, et al. Experiences and management of physician psychological symptoms during infectious disease outbreaks: a rapid review. BMC Psychiatry. 2021 doi: 10.1186/s12888-021-03090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rashid M. Two decades (1993–2012) of adult intensive care unit design: a comparative study of the physical design features of the best practice examples. Crit Care Nurs Q. 2014;37:3–32. doi: 10.1097/CNQ.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 38.Healthcare Excellence Canada. Policy Guidance for the Reintegration of Caregivers as Essential Care Partners. Executive Summary and Report November 2020. Available from URL: https://www.cfhi-fcass.ca/docs/default-source/itr/tools-and-resources/policy_guidance_en.pdf?sfvrsn=292a980e_4 (accessed February 2022).
- 39.Curtis JR, Vincent JL. Ethics and end-of-life care for adults in the intensive care unit. Lancet. 2010;376:1347–1353. doi: 10.1016/S0140-6736(10)60143-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.