ABSTRACT
The global adoption of predominantly plant-based, sustainable, healthy diets will help reduce the risk of obesity- and malnutrition-related noncommunicable diseases while protecting the future health of our planet. This review examines the benefits and limitations of different types of plant-based diets in terms of health and nutrition, affordability and accessibility, cultural (ethical and religious) acceptability, and the environment (i.e., the 4 pillars underlying sustainable healthy diets). Results suggest that, without professional supervision, traditional plant-based diets (vegan, vegetarian, and pescatarian diets) can increase the risk of nutritional deficiencies among infants, children/adolescents, women, pregnant/lactating women, and the elderly. In contrast, flexitarian diets and territorial diversified diets (TDDs; e.g., Mediterranean and New Nordic diets) that include large quantities of plant-sourced foods, low amounts of red meat, and moderate amounts of poultry, fish, eggs, and dairy can meet the energy and nutrition needs of different populations without the need for dietary education or supplementation. Compared with vegan, vegetarian, and pescatarian diets, more diverse flexitarian diets and TDDs are associated with reduced volumes of food waste and may be more acceptable and easier to maintain for people who previously followed Western diets. Although flexitarian diets and TDDs have a greater impact on the environment than vegan, vegetarian, and pescatarian diets, the negative effects are considerably reduced compared with Western diets, especially if diets include locally sourced seasonal foods. Further studies are required to define more precisely optimal sustainable healthy diets for different populations and to ensure that diets are affordable and accessible to people in all countries.
Keywords: sustainable healthy diets, flexitarian, territorial diversified diet, plant-based diets, vegan, vegetarian, environment
Statement of Significance: In reviewing the criteria for sustainable healthy diets, we show that flexitarian and territorial diversified diets (TDDs) may offer the optimal balance between human and planetary health without the need for support from health care professionals. This is particularly pertinent to those populations at risk of nutritional deficiency from traditional plant-sourced diets such as veganism or vegetarianism. A global switch to flexitarian/TDDs may be a practical and affordable contributor to controlling climate change.
Introduction
What we eat has a major impact on our health and the health of our planet. “Western-style” omnivorous diets in high-income countries (HICs) typically comprise large amounts of animal-sourced foods and higher than recommended intakes of energy, SFAs, salt, sugar, and refined grains (Table 1), all of which can increase the risk of obesity and other noncommunicable diseases (NCDs) (1–3). In contrast, experience in low-to-middle-income countries (LMICs) suggests that, without access to certain foods, supplements, and nutrition education, predominantly plant-based diets can lead to insufficient energy intake and nutrient deficiencies leading, in turn, to conditions such as stunted growth, delayed development, blindness, and reduced functioning (1, 4, 5). According to the United Nations, unbalanced diets account for approximately 2 billion cases of nutritional deficiencies, 800 million cases of hunger, and 2 billion cases of overweight and obesity worldwide (1). This situation is likely to worsen as the global population grows and as urbanization enables greater, and/or preferential, access to high-energy, low-nutrient foods (6). Moreover, global food production accounts for up to 30% of the world's greenhouse gas emissions (GHGEs), 60% of biodiversity loss, and 70% of freshwater use and has a significant impact on soil quality, deforestation, eutrophication (the leaching of nutrients from land into water leading to increased plant and algae growth in estuaries and coastal waters), and climate change (7). The negative impact of food production on our planet is likely to increase as the population grows (2, 6, 8) and as demand for animal-sourced foods increases in LMICs (1, 9).
TABLE 1.
Definitions, benefits, and limitations of different diet scenarios1
| Diet | Definition | Benefits | Limitations | Suitable for? |
|---|---|---|---|---|
| Western-style diet | Omnivorous diet2 that typically includes high intakes of animal-sourced foods, highly processed foods and lower-than-recommended intakes of plant-sourced foods (2) |
|
|
|
| Flexitarian diet | Omnivorous diet2 that includes high amounts of plant-sourced foods (e.g., fruits, vegetables, unrefined grain, legumes, nuts and seeds), moderate amounts of poultry, dairy and fish, and low amounts (1 serving/wk) of red meat, highly processed foods, and added sugar (2, 14, 15) |
|
|
|
| Territorial diversified diet (TDD) | Flexitarian-style diet that includes high intakes of seasonal, locally produced foods (e.g., Mediterranean diet, New Nordic diet) (16) |
|
• As for flexitarian diets | • As for flexitarian diets |
| Vegetarian diet | Excludes meat, fish/shellfish, insects, and gelatin but includes plant-sourced foods and (usually) dairy and eggs3 (23) |
|
|
|
| Pescatarian diet | Vegetarian diet that includes fish/shellfish |
|
|
|
| Vegan diet | Excludes all animal products including meat, fish/shellfish, insects, gelatin, eggs, dairy, and honey (23) |
|
|
• As for vegetarian diets |
HIC, high-income country; LMIC, low-to-middle-income country; NCD, noncommunicable disease; RNI, recommended nutrient intake.
Diverse diet that includes all types of meat, fish/shellfish, dairy, eggs, honey, insects, and plant-sourced foods (e.g., fruits, vegetables, grains, pulses, legumes, nuts, seeds, tubers, fungi, algae) in any ratio.
Lacto-ovo-vegetarian diets include dairy and eggs; lacto-vegetarian diets include dairy, but not eggs; ovo-vegetarian diets include eggs but not dairy.
The 2015 Paris Agreement on climate change responded to these challenges by highlighting the need for sustainable diets that help ensure the health of the world population and our planet (10). The 4 pillars underlying sustainable diets are “nutrition and health,” “affordability and accessibility,” “cultural acceptability” and “environmental impact” (1). Modeling studies centered on finding food systems that achieve the best balance between these pillars highlight the need to shift toward diverse, predominantly plant-based diets while concomitantly reducing food losses/waste and improving food production practices (2, 5, 6). Various organizations including EAT Lancet, the WHO, World Wide Fund for Nature (formerly World Wildlife Fund), and World Resources Institute (WRI) suggest that these diets should be based on flexitarian or territorial diversified diets (TDDs; e.g., Mediterranean and New Nordic diets) with the option to exclude animal-sourced foods (e.g., vegetarian, pescatarian, or vegan diets) (2, 5, 6, 11–13). While the different types of diets have not been universally defined, the term “flexitarian” is increasingly used to describe omnivorous diets that incorporate high amounts of plant-sourced foods; moderate amounts of poultry, dairy and fish; and low amounts of red meat, highly processed foods, and added sugar (2, 14, 15). Vegetarian diets typically include plant-sourced foods, dairy, and eggs but exclude meat and fish; pescatarian diets are vegetarian diets that include fish; and vegan diets exclude all animal-sourced foods including fish, dairy, eggs, and honey (Table 1). Based on these definitions, TDDs are region-specific diets that have characteristics similar to flexitarian diets but primarily include seasonal, locally sourced foods (16). For some populations (e.g., people consuming Western diets in HICs), the transition to flexitarian diets/TDDs requires considerably greater intakes of plant-sourced foods and large reductions in animal-sourced foods (especially red meat), whereas the opposite may be true for people in LMICs.
Recommended food intakes for sustainable healthy diets are typically based on energy and nutrient requirements for an “average” adult (2, 6, 11–13). However, requirements vary depending on age, sex, pregnancy, and level of activity. Although most organizations recognize this limitation, few provide advice on how to modify the reference diet to suit different populations or how to balance the diet should a population need (or choose) to reduce or exclude 1 or more food groups due to cultural or religious beliefs, ethical reasons (animal welfare or environmental concerns), food allergies/intolerances, or limited access to certain foods (17). The aim of this review is to examine the benefits and limitations of the different types of sustainable healthy diets (vegan, vegetarian, pescatarian, flexitarian/TDDs) for different populations in terms of health and nutrition, environmental impact, affordability, accessibility, and cultural acceptability, and to suggest ways in which these diets might be adapted to suit the needs of specific populations.
What Are the Benefits and Limitations of Different Types of Sustainable Diets in Terms of Health and Nutrition?
Benefits of plant-based diets
The effects of sustainable diets on NCD mortality are unclear, with some studies reporting reductions ranging from 19% with calorie-controlled flexitarian diets to 22% with vegan diets (15, 18) and others reporting no benefits beyond those achieved through calorie control (19, 20). However, diets that exclude or reduce animal-sourced foods are typically associated with a reduced risk of premature mortality (21) and NCDs (1–3, 22–24), primarily due to improvements in cardiometabolic risk factors [insulin resistance/type 2 diabetes (25–27), metabolic syndrome (28), inflammatory markers (29), hypertension (30–32), and dyslipidemia (33–35)], and a reduced risk of certain cancers [e.g., breast (36), prostate (37), and colorectal (38)]. In general, the risk of NCDs is lowest for vegans, followed by vegetarians, flexitarians, and finally, Western diets (14).
Another benefit for plant-based diets is that they reduce the risk of obesity (25, 39–44). The Adventist Health Study-2 (n = 96,000) showed a significant association between meat consumption and BMI among adults in the United States and Canada, with the highest BMI among nonvegetarians (in kg/m2; mean: 28.7), followed by flexitarians (27.3), pescatarians (26.3), and vegetarians (25.7) (25). Vegans were the only group to achieve a mean BMI in the healthy range (<25). Similar results were obtained from the European Prospective Investigation into Cancer and Nutrition (EPIC) study in Oxford (n = 57,498) (43). Although reductions in BMI were primarily related to lower intakes of energy-dense SFAs and higher intakes of satiety-promoting fiber, up to 5% of the difference in BMI was attributed to the relation between plant-based diets and weight-loss–promoting lifestyle choices, such as increased exercise (45) and reduced alcohol consumption (43, 46).
Overall, results suggest that vegan diets might reduce the risk of premature mortality, NCDs, and excessive weight gain. However, the health benefits of any diet partly depend on the variety of foods consumed and the way in which food is stored, processed, and prepared (47). Variety is important because the chemical and physical properties of individual food components interact to alter our ability to digest, absorb, and release nutrients from foods. For example, vitamin C in fruits and vegetables enhances the absorption of nonheme iron from plant-sourced foods (48), whereas lactose and vitamin D increase the absorption of calcium, vitamin B-2, vitamin B-12, folate, magnesium, and zinc (49). Where possible, fried and/or ultra-processed high-energy, low-nutrient foods (e.g., animal- and plant-based burgers, cakes, and pizzas) should be consumed in moderation (47). However, some foods (e.g., some processed tomatoes and fermented foods, such as kefir, tempeh, sprouted seeds, kimchi, and sauerkraut) are processed in ways that increase their health benefits (50, 51). In some cases (e.g., beans), the digestibility and bioavailability of essential minerals can potentially be improved by soaking and/or cooking under pressure to reduce levels of anti-nutrients (phytates, polyphenols, and tannins) (52), and by ensuring appropriate postharvest storage and cooking times (53). Given the benefits and complexities of healthy eating, careful diet planning should be encouraged by promoting lifelong healthy eating strategies in schools, educating families and communities about the benefits and practicalities of meal planning and food preparation, ensuring appropriate health-based dietary guidelines are available in all countries, increasing nutrition training among health care professionals (HCPs), and by increasing public access to registered dietitians/nutritionists.
Limitations of plant-based diets
Human health depends on the consumption of a wide range of macronutrients and micronutrients, some of which may be difficult to obtain in sufficient quantities from plant sources alone (54, 55). Compared with omnivorous diets, vegan/vegetarian diets typically contain lower amounts of long-chain omega-3 (n–3) fatty acids and high-quality proteins [proteins that provide bioavailable essential and branched-chain amino acids when digested (56)], and suboptimal intakes of certain micronutrients, including calcium, vitamin A, riboflavin, niacin, vitamin B-12, iodine, selenium, and zinc (15, 23, 54, 57–62). Although low serum vitamin D concentrations are common irrespective of diet type, risk is higher among people who consume vegan diets or do not consume milk or dairy (63). While some studies report higher intakes of dietary iron among people who consume vegan and vegetarian diets, plasma ferritin and hemoglobin concentrations often remain low, leading to an increased risk of iron deficiency anemia (62, 64, 65). This is partly because plant sources predominantly contain nonheme iron, which has a lower bioavailability than animal-sourced heme iron (62), but also because plants contain iron-absorption inhibitors, such as phenolic compounds, oxalates, and phytates (66). Iron absorption from omnivorous diets is 14–18% compared with 5–12% from vegetarian/vegan diets; thus, the recommended daily iron intake for vegetarians and vegans is 1.8-times higher than for omnivores (67). In addition to iron deficiency anemia, vegan/vegetarian diets have been associated with an increased risk of low birth weight (68–71) and impaired neurocognitive health among infants (72–74), increased risk of stroke among adults (75), impaired vision (74), higher rates of depression (76, 77) and (for vegans) reduced bone mineral density (BMD) (78) and higher rates of bone fracture (79, 80).
Nutritional benefits of flexitarian diets/TDDs compared with vegan and vegetarian diets
A modeling study designed to assess the nutritional benefits of switching from unregulated diets (i.e., diets that are not carefully planned or recommended by health care providers) to well-designed plant-based (vegan, vegetarian, pescatarian, or flexitarian) diets found that most of the nutrients that were low during the baseline diets (vitamin A, iron, potassium, and fiber) increased to above the WHO-recommended reference nutrient intakes (RNIs) with all 4 diets (Table 2) (15). However, vegan diets did not meet RNIs for calcium, and neither vegan nor vegetarian diets met RNIs for vitamin B-12. Similarly, a modeling study designed to generate sustainable healthy diets for adults in the Netherlands found that, whereas flexitarian diets met nutrient needs, vegetarian and vegan diets did not provide sufficient n–3 fatty acids, and the vegan diet only met requirements for vitamin B-12 and calcium through high intakes of fortified soy drinks (e.g., 2 portions/d) (81). This suggests that, although people who consume vegan/vegetarian diets can achieve their RNIs through careful dietary planning and the use of supplements/fortified plant-based products, RNIs are more easily achieved through flexitarian diets/TDDs. Flexitarian diets may be particularly beneficial for populations who require high intakes of certain nutrients (e.g., children/adolescents and women) and for vulnerable populations (e.g., infants, pregnant women, and the elderly), for whom nutritional deficiencies are more likely to lead to adverse health issues.
TABLE 2.
Nutrient supply per day by dietary scenario for the “average” person across 150 countries, worldwide, in 20101
| Diet scenario | |||||
|---|---|---|---|---|---|
| Nutrient | Recommendation2 | Flexitarian | Pescatarian | Vegetarian | Vegan |
| Calories, kcal | 2084 | 2084 | 2084 | 2084 | 2084 |
| Protein, g | >52 | 70.6 | 72.5 | 65.0 | 64.7 |
| Carbohydrates, g | <391 | 274 | 278 | 289 | 304 |
| Fat, g | — | 81.8 | 78.1 | 77.3 | 71.3 |
| SFAs, g | <23 | 19.7 | 17.5 | 17.2 | 13.4 |
| MUFAs, g | — | 31.4 | 28.1 | 27.7 | 26.1 |
| PUFAs, g | >14 | 27.7 | 27.2 | 27.4 | 27.6 |
| Vitamin C, mg | >4 2 | 148 | 163 | 171 | 196 |
| Vitamin A, μg | >544 | 627 | 679 | 694 | 703 |
| Folate, μg | >364 | 553 | 577 | 644 | 733 |
| Calcium, mg | >520 | 621 | 660 | 630 | 489 |
| Iron, mg | >17 | 18.8 | 19.3 | 19.5 | 21.1 |
| Zinc, mg | >6.1 | 10.4 | 10.4 | 10.2 | 10.3 |
| Potassium, mg | >3247 | 3383 | 3555 | 3634 | 3952 |
| Fiber, g | >29 | 35.5 | 36.6 | 39.9 | 44.6 |
| Copper, mg | >0.8 | 2.3 | 2.3 | 2.5 | 2.7 |
| Phosphorus, mg | >757 | 1379 | 1429 | 1366 | 1337 |
| Thiamin, mg | >1.1 | 1.5 | 1.5 | 1. 5 | 1.6 |
| Riboflavin, mg | >1.1 | 0.9 | 1.0 | 0.9 | 0.9 |
| Niacin, mg | >14 | 17.5 | 17.4 | 16.0 | 16.8 |
| Vitamin B-6, mg | >1.2 | 6.1 | 6.2 | 6.1 | 2.3 |
| Magnesium, mg | >205 | 527 | 543 | 561 | 596 |
| Pantothenate, mg | >4.7 | 5.4 | 5.4 | 5.3 | 4. 9 |
| Vitamin B-12, μg | >2.2 | 2.4 | 3.7 | 0.8 | 0.0 |
Adapted from reference 15 with permission under the terms of the Creative Commons CC-BY license.
Recommended nutrient intakes are based on WHO guidelines (204) for all nutrients other than phosphorus and copper, which are based on recommendations from the US Institute of Medicine (205). Because the recommended nutrient intakes differ by age and sex, population-level average values were calculated using the age and sex structure based on data from the Global Burden of Disease project and forward projections by the UN Population Division. Estimates of recommended energy intake account for the age- and sex-specific energy needs for a moderately active population with US height as an upper bound and include the energy costs of pregnancy and lactation.
Infants
The WHO advises that infants should be breastfed exclusively for the first 6 mo of life and alongside complementary food ideally until 2 y of age (82). The duration of breastfeeding varies considerably between countries and regions, with some infants not being breastfed at all and others being breastfed longer than 2 y of age. There is some evidence that the duration of breastfeeding is longer for infants whose mothers follow vegan/vegetarian diets than for other infants, possibly because vegan/vegetarian mothers consider breast milk to be safer and more natural than other options (83). Although the energy and nutrient content of breast milk is largely similar irrespective of the maternal diet (84), breast milk produced by women consuming vegan/vegetarian diets may contain low concentrations of B vitamins, which may detrimentally impact infant development and neurological function, growth, and/or anemia (84–89). Consequently, lactating women following plant-based diets should not only follow local guidelines on vitamin and mineral supplementation during lactation but may also need to increase their vitamin B-12 intake through supplementation and higher intakes of fortified foods and (for vegetarians/pescatarians) dairy, eggs, and/or fish (Table 3) (83, 85, 87, 88, 90, 91). For women without religious, cultural, or ethical restrictions, flexitarian diets/TDDs (particularly Mediterranean diets) that provide high intakes of B vitamins, magnesium, iron, zinc, and vitamins A, E, and C may reduce the risk of nutritional deficiencies, both for the infant and the mother (92–95). If breastfeeding is not possible/acceptable, sufficient volumes of infant formulas based on cow/goat milk or soy can provide the recommended intakes of energy, protein, vitamins, and minerals for infants during the first year of life (96).
TABLE 3.
Energy/nutrient inadequacies and dietary advice for different populations following vegan, vegetarian, pescatarian, or flexitarian diets/TDDs1
| Nutrient | Function | Food sources | Advice |
|---|---|---|---|
| Good-quality proteins | Involved in a wide range of metabolic interactions; essential for growth and repair; help maintain healthy skin, bones, muscles, and organs (206, 207) | Eggs; milk and dairy products; soy products; meat substitutes; legumes; lentils; nuts; seeds; selected whole grains (207) | People following vegan/vegetarian/flexitarian/TDD diets should aim to replace meat protein sources with high-quality protein alternatives; to ensure nutritional adequacy, HCP advice may particularly be required for young children and pregnant women |
| Calcium | Helps develop and maintain healthy teeth and bones; vital roles in intracellular signaling for metabolic regulation, information transmission via the nervous system, muscle contraction, and blood clotting (206, 208) | Milk and dairy products; low-oxalate green-leafy vegetables with high calcium bioavailability, such as kale (106, 107); calcium-enriched plant-based milks and products (e.g., soya milk, yogurt, oat milk and yogurt, coconut milk and yoghurt, and tofu); calcium-enriched juices; fortified cereals; sesame paste (tahini); almonds; seaweed and figs (206) | If insufficient calcium-enriched plant-based alternatives are consumed, HCP advice needs to be sought to advise a suitable calcium supplement |
| n–3 Fatty acids | Essential fatty acid that must be supplied by diet; important components of cell membranes; substrates for signaling molecules that control cellular functions; important for heart health (206, 209) | Oily fish; n–3 enriched eggs; canola/rapeseed oil; walnuts; ground flaxseed; hemp seed; chia seed; fortified products (206) | If no fish is consumed (i.e., vegan, vegetarian diet) HCP advice may be required to advise on vegetarian sources of DHA and EPA and suitable supplementation may be needed |
| Iron | Component of hemoglobin in RBCs, allowing oxygen transportation; important roles in the immune system; required for energy and drug metabolism (206, 208) | Heme sources: beef, liver; nonheme sources: dried beans and peas; lentils; enriched cereals; nuts and seeds, selected whole-grain products; dark leafy green vegetables but bioavailability can be low due to phytate and tannin content; dried fruit; eating foods rich in vitamin C helps absorb nonheme iron (206) | In high-risk population (i.e., young children and during pregnancy), an iron supplement may be needed if intake of nonheme/heme alternatives do not meet iron requirements |
| Zinc | Co-factor for many enzymes involved in digestion, carbohydrate and bone metabolism, oxygen transport, immune response, stabilizing the structure of DNA, RNA, and ribosomes (210) | Beef; crab and shellfish; lamb; leafy or root vegetables; whole grains; pork; poultry; milk and dairy products; eggs; nuts; offal (210); foods high in phytates (e.g., whole grains) reduce the bioavailability of zinc | In high-risk populations (i.e., young children) and, in particular, if growth is affected, a zinc supplement may be required |
| Iodine | Maintenance of metabolic rate controlling energy production and oxygen consumption; growth and cognitive development; protein metabolism in fetuses/neonates (210) | Milk and dairy products; sea fish; seaweed; iodized salt, local iodine fortified foods (210) | In particular, young vegan children may need an iodine supplement, as salt intake should be limited in the young |
| Selenium | Protects against oxidative damage; antioxidant and transport functions (210) | Offal; fish; Brazil nuts; eggs; poultry; meat products (210) | HCP advice may be required to assess need for selenium supplementation, in particular in individuals who are vegetarian/vegan |
| Vitamin A (retinol, beta-carotene) | Involved in adaptation of vision in the dark, growth, cell differentiation, embryogenesis, immune response (210) | Retinol: liver products, kidney, offal, oily fish and fish liver oils, eggs; beta-carotene: carrots, red peppers, spinach, broccoli, tomatoes (210) | There are many sources of plant-based alternatives for vitamin A; however, availability of these alternatives needs to be considered in conjunction with local prevalence of vitamin A deficiency; HCP advice may be useful on whether supplementation is required |
| Riboflavin (vitamin B-2) | Oxidation-reduction reactions in metabolic pathways; promotion of normal growth; assists synthesis of steroids, RBCs, and glycogen; maintenance of mucous membrane, skin, eyes and nervous system; aids iron absorption (210) | Eggs; milk and dairy products; liver; kidney; yeast extract; fortified breakfast cereal (210) | Ensure that nutritional alternatives are consumed, in particular in individuals who follow vegan diets |
| Niacin (vitamin B-3) | Glycolysis; fatty acid metabolism; detoxification | Beef; pork; chicken; wheat flour; maize flour; eggs; milk and dairy products (210) | Ensure that nutritional alternatives are consumed, in particular in individuals who follow vegan diets |
| Vitamin B-12 (cobalamin) | Recycles folate coenzymes; normal myelination of nerves; synthesis of methionine from homocysteine (210) | Meat products; eggs; milk and dairy products; fish products; yeast products; fortified vegetable extracts; fortified breakfast cereal (210) | HCP advice may be required, in particular if a vegan diet is followed; a vitamin B-12 supplement may be required |
| Vitamin D (calciferols) | Calcium absorption and excretion; involved in bone mineralization; may inhibit cell proliferation in some forms of cancer (210) | Cod liver oil; oily fish; fortified milk and dairy products; fortified margarine; fortified breakfast cereals; eggs (in particular, egg yolk); liver | The WHO supports routine supplementation for a wide range of populations (204); local advice for vitamin D supplementation should be followed and the increased risk of vitamin D deficiency with a plant-based diet should be considered |
HCP, health care professional; TDD, territorial diversified diet.
The proportion of infants in HICs who are fed vegan/vegetarian diets during complementary feeding has increased over recent years, with some countries reporting rates of approximately 10% (83). Vegan/vegetarian complementary feeding has little effect on height among infants aged 1–3 y, while these infants are less likely to be overweight than their omnivorous counterparts (97, 98). However, unsupervised vegan/vegetarian weaning (i.e., weaning without the support of educated HCPs) may increase the risk of nutritional deficiencies in infants and children, including deficiencies in n–3 fatty acids, calcium, iron, zinc, vitamins B-12, and in vegans, vitamin D (Table 3) (83, 99, 100). Cases of vitamin D deficiency–related bone fracture (100), hypocalcemia leading to seizures, severe anemia, respiratory distress with metabolic alkalosis, growth retardation, and even death have been reported among infants following restrictive diets due to food allergies (99) and inadequate vegan diets without fortified plant-based alternatives (101). Consequently, professional organizations suggest that parents who wish to wean their infants to vegan/vegetarian diets due to medical (e.g., cow-milk allergy), ethical, or religious reasons should follow WHO guidance for vitamin D supplementation (102) and should seek additional guidance from adequately qualified HCPs (e.g., pediatricians and pediatric dietitians) (83, 96, 99, 103–105). In particular, meat should be replaced with greater intakes of iron- and protein-rich plant-based alternatives, such as pulses, legumes, tofu, and nut butters, and fortified flours and cereals should be used in preference (Table 3). Cow milk and its derivatives should be replaced with fortified plant-based (soy, oat, nut, coconut, rice, pea, hemp) drinks (suitable only from 1 y of age) and/or yogurts and calcium levels could be augmented by increasing the consumption of low-oxalate green-leafy vegetables with high calcium bioavailability, such as kale (106, 107). While nonorganic fortified plant-based alternatives are similar in calcium content to cow-milk products, these products vary in other micronutrient additions and they are generally lower in energy and significantly lower in protein, except for soy-based alternatives. Ideally, a suitable alternative should be recommended by a registered dietitian/nutritionist. Parents should be strongly dissuaded from making their own plant-based drinks, which are nutritionally inferior to those that are fortified.
A survey conducted in Italy found that almost one-quarter (22.6%) of all families weaning their infant to vegetarian diets did not consult their pediatrician for nutritional advice and support (83). This may be related to the fact that 77% of pediatricians were resistant to alternative complementary feeding styles and 45.2% of families considered their pediatrician was unable to provide sufficient information to support a vegetarian diet for their child. Consistent with these observations, a survey of HCPs found that 79.9% had not attended a nutrition course in the previous 5 y, 34.1% were unable to define correctly vegetarian/vegan diets, and nutrient knowledge was generally poor (108). These results highlight the need for greater nutritional education among pediatricians and the need to develop resources that can adequately support families choosing (for religious, cultural, or ethical reasons) or needing to wean their infants to vegan/vegetarian diets. Where possible, families should be referred to a registered dietitian nutritionist.
Children and adolescents
Infants, children, and especially adolescents (who experience rapid growth at puberty) require more energy and nutrients per kilogram of body weight than adults to ensure normal growth rate and development of neural, endocrine, and immunological systems (109, 110). However, the energy density and (for some nutrients) nutrient density of vegan/vegetarian diets are lower than for omnivorous diets. Consequently, children/adolescents require relatively high intakes of food to meet their recommended energy/nutrient intakes. This might prove challenging for smaller children with limited stomach capacity and for adolescents with very high nutritional demands. Although it is possible for children/adolescents to meet their RNIs through well-planned vegan/vegetarian diets that are often acceptable to this age group, advice on the suitability of vegan and vegetarian diets for different age groups varies between guidelines, with some suggesting that well-planned plant-based diets are safe throughout childhood and adolescence (90, 111, 112) and others suggesting they should be avoided (99, 103, 113). If vegan/vegetarian diets are followed for religious or ethical reasons, appropriate HCP-directed family education and follow-up over time are required to ensure the nutritional needs of the child/adolescent are met.
Primary health concerns for vegan or vegetarian children and adolescents include lower than recommended intakes of vitamin B-12 (required for RBC formation, nerve function), zinc (growth and sexual development), calcium (skeletal growth), iodine (physical and neurological development), and n–3 fatty acids (healthy neurological function and eyesight) (Table 3) (109, 114–119). As for other populations, the incidence of iron deficiency among vegan or vegetarian children and adolescents is high, with the prevalence of low ferritin concentrations ranging from 4.3% to 73% and the prevalence of low hemoglobin concentrations ranging from 0% to 47.5% (64). While vegetarians/pescatarians can increase their intakes of most of these nutrients by increasing their consumption of eggs, dairy, and/or fish (Table 3) (118, 120), some guidelines suggest that vegan children and adolescents should be regularly monitored for iron, n–3 fatty acid, and zinc deficiencies and (as with other pediatric populations) require regular vitamin B-12 and D supplements (96).
Consistent with these reports, a study conducted among Dutch children aged 2–6 y (n = 1279) found that diets in which 100% of dairy and meat was replaced with plant-sourced alternatives were associated with a 26% lower SFA intake and 29% higher fiber intake (121). However, 5–13% reductions in mean intakes of calcium, zinc, and thiamin; a 49% reduction in vitamin B-12; and reduced iron bioavailability were also observed. Overall, thiamin, vitamin B-12, and zinc intakes from the plant-based diets were lower than the national recommended levels for 15%, 10%, and 8% of females aged 4, 5, or 6 y, respectively. In contrast, diets in which 30% of dairy and meat (by gram) was replaced by plant-sourced alternatives potentially improved children's health by lowering SFA intake by 9% and increasing fiber content by 8%, while maintaining similar micronutrient intakes, with the exception of vitamin B-12. This suggests that careful consideration of nutrient intakes is required to ensure that vegan/vegetarian diets meet the needs of growing children and that, for people without religious or cultural restrictions, nutrient adequacy may be easier to achieve with flexitarian diets/TDDs.
Women
A study of 62 women aged 18–67 y (78% aged 18–45 y; i.e., pre-menopause) found that Western and vegetarian diets were associated with significantly greater intakes of SFAs than vegan diets, and that vegan, vegetarian, and Western diets met the UK-recommended RNI for women (122) in terms of vitamins A, B-6, C, and E; thiamin; riboflavin; niacin; folates; and zinc (54). However, the vegan group failed to achieve RNIs for iodine, vitamin B-12, and calcium; both the vegetarian and vegan groups failed to achieve the RNI for selenium; and all 3 groups failed to achieve RNIs for iron. Vitamin B-12, iodine, and calcium levels can be increased among vegan women through supplementation and/or greater intakes of certain plant-sourced foods, including yeast extract, dried fruits/vegetables, and fortified cereals to meet vitamin B-12 needs; seaweed, peanuts, and iodized table salt for iodine; and beans, leafy green vegetables, citrus fruits, nuts and fortified soy drinks, soy alternatives to yogurt, and tofu for calcium (Table 3) (54). However, iodine supplements and iodized salt may not increase iodine concentrations in the blood to adequate concentrations and iodine is not always fortified in nondairy drinks (123, 124). For vegetarian, pescatarian, and flexitarian diets/TDDs, each of these vitamins/minerals is readily obtained from dairy, eggs, fish, and/or meat. Similarly, while selenium intakes for vegans can be increased by increasing the consumption of nuts (especially Brazil nuts), pulses, and grains, higher concentrations of selenium are available in eggs, dairy, fish, and/or meat (Table 3).
Compared with men, women of reproductive age have considerably higher RNIs for iron due to blood losses during menstruation. For vegetarians, lower than recommended levels of ferritin and hemoglobin are observed in up to 79% and 33% of females over the age of 18 y, respectively, compared with 29% and 15% of males (65). A study in Australian women found that the highest rates of iron deficiency or anemia were observed among people consuming vegetarian diets (42.6%), followed by flexitarian (38.6%), and finally Western diets (25.5%), with rates decreasing with increasing intakes of meat (45). Although vegan/vegetarian women can increase their iron intake by consuming large quantities of iron-rich foods (e.g., green-leafy vegetables, dried fruits, beans, nuts, and whole grains; Table 3), targets are more likely achieved through the consumption of heme iron, which is only found in meat (62).
Pregnancy
Compared with Western diets, plant-based diets in HICs are associated with a reduced risk of excess maternal weight gain during pregnancy and lower rates of pre-eclampsia (125–127) and gestational diabetes (92–94, 128). In contrast, vegan diets in HICs have been linked to small-for-gestational-age (SGA) newborns and lower birth weights (68–71), whereas plant-based diets in LMICs have led to low birth weights, fetal neurological disabilities, and malformations (129). Meta-analysis of data from 111,184 pregnant women found that birth weight and/or length can be significantly increased by increasing the consumption of dairy and that the risks of SGA and low birth weight are inversely correlated with dairy intakes (130). Further studies are required to determine whether plant-sourced dairy alternatives have similar benefits for vegans.
Nutritional guidelines recommend that all women should receive iron supplements (to avoid anemia) and folic acid supplements (to avoid neural tube defects) before, during, and after pregnancy and that increased energy intakes are required from the second trimester (91, 131). In addition, vegan/vegetarian women are advised to increase their protein intake by approximately 20% to achieve a total intake of 1.1 g/kg body weight per day (132), and to increase their intakes of foods rich in iron, iodine, vitamin B-12, calcium, and vitamin D, such as dairy/fortified plant-sourced dairy alternatives, green-leafy vegetables, dried fruits, fortified cereals, nuts, seeds, and (for pescatarians) fish (Table 3) (90, 95). Flexitarian diets/TDDs (in particular Mediterranean diets) that provide low intakes of total fats and SFAs and high intakes of fiber, folate, zinc, B vitamins, vitamin A, vitamin E, magnesium, and vitamin C are considered ideal for pregnant women (92–94).
Older adults
Compared with Western diets, plant-based diets have been associated with improved physical fitness and cognition among elderly populations, and increased longevity (133–135). Although vegetarian diets are traditionally thought to reduce the risk of osteoporosis through improvements in acid-base homeostasis (136), recent studies suggest that elderly people following vegetarian/vegan diets for more than 10 y have significantly reduced BMD at the femoral neck and lumbar spine than omnivorous counterparts (79, 137), and that vegans have significantly reduced BMD and higher fracture rates than vegetarians (79). According to public health guidelines, the use of calcium and vitamin D supplements should be considered for people following vegan diets, females >50 y and males >70 y, and for people living in assisted-care homes (138). However, data from more than 51,000 people aged >50 y found little evidence to support a beneficial association between supplements and bone fractures, leading the authors to conclude that a healthy diet and lifestyle (increased exercise and exposure to sunshine) potentially provide greater protection against bone fractures than supplements (139). Moreover, observational studies show that the risk of osteoporosis and/or fractures can be reduced in menopausal women through adequate intakes of dietary calcium, high-quality proteins, vitamin B-12, vitamin D, and retinol (79, 140, 141). This suggests that elderly populations are likely to benefit from increased intakes of dairy, fortified plant-sourced drinks, soy/coconut/pea/almond alternatives to yogurt, tofu, grains, legumes, nuts, seeds, eggs, and moderate intakes of meat (Table 3). The inclusion of small amounts of meat in the diet will also help maintain vitamin B-12 concentrations, which tend to decrease with age (142).
Health benefits of flexitarian diets/TDDs compared with vegan and vegetarian diets
Whereas vegan/vegetarian diets exclude certain food groups, flexitarian diets/TDDs include a diverse range of foods that help to increase the range of microbial species in our intestinal microbiome (143, 144). This is important because a diverse microbiome is essential for our digestive, metabolic, immune, and mental health, and helps modulate the risk of chronic diseases including obesity, type 2 diabetes, cardiovascular disease, some cancers, inflammatory disorders, and autism (145, 146). Plant-based diets foster greater microbial diversity than Western diets due to increased fiber intake (147, 148). However, diversity can be further increased through the consumption of probiotic and fermented foods (e.g., fermented milk, yogurt, kimchi, soy sauce, tempeh, and kefir) and foods rich in n–3 fatty acids, such as fish (143).
Compared with vegan/vegetarian diets, flexitarian diets/TDDs may have a beneficial effect on mental health. Recent studies suggest that people who consume vegan/vegetarian diets have an increased risk of depression, anxiety, and self-harm compared with people who consume meat (76, 77). However, further work is required to establish whether plant-based diets increase the risk of mental health disorders or whether people with mental disorders choose these diets as a form of self-protective behavior (149). In particular, patients with eating disorders may be attracted to restricted vegan/vegetarian diets as a means to lose weight and disguise dietary restriction behaviors (150, 151). This is another reason why appropriate and early dietary monitoring by suitably qualified HCPs is advised for people following vegan/vegetarian diets.
What Impact Do Different Types of Healthy Sustainable Diet Have on GHGEs and the Environment?
The effects of food production on climate change have led to decreased agricultural yields and increased food insecurity in some regions of the world (152). This, together with the burgeoning worldwide population, means that current food systems are unsustainable. According to the WRI, a combination of changes will be required to reduce the impact of our diets on the environment, including a shift in our food choices, changes in food production (sourcing and transformation), and reductions in food losses and waste (153).
Food choices
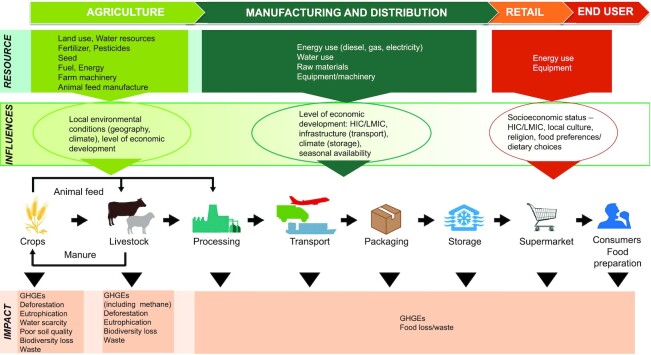
Animal-sourced foods are responsible for more than 60% of food production-related GHGEs worldwide. However, emissions vary within this food group, with meat, fish, and eggs accounting for 2 to 3 times more GHGEs per 2000 kcal of energy than milk and cheese (154) and beef accounting for considerably greater GHGEs per unit of protein or kilogram of edible food than pork, chicken, fish, eggs, and milk (Figure 1) (155, 156). This is largely because ruminants produce methane, but also because beef cattle produce greater volumes of nitrogen and phosphorus (manure) and require up to 28 times more land than all other animals (including dairy cattle) combined (157, 158). This suggests that, while the largest reduction in GHGEs can be achieved by excluding meat from our diets, flexitarian diets/TDDs that significantly reduce the consumption of red meat but include moderate intakes of poultry, dairy, eggs, and fish might also be effective, albeit to a lesser extent.
FIGURE 1.
Greenhouse gas emissions in the production of foods. Values shown in the boxplots are minimum and maximum values, IQRs (rectangle borders), and medians (line inside the rectangle). CO2e, CO2 equivalents; n, number of studies included. Reproduced with permission from reference 156; adapted from reference 155 with permission.
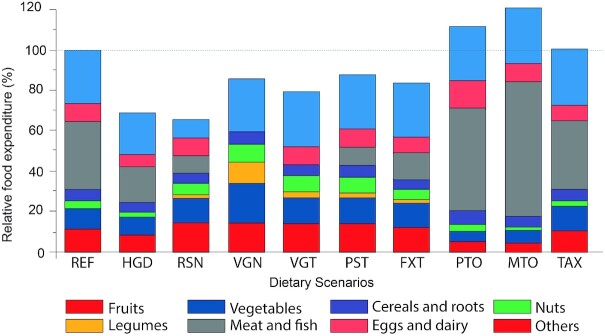
Although the “footprint” method of assessing the impact of food production on a single aspect of the environment (e.g., GHGEs, land or water use) is useful, life cycle assessments that consider the impact of food production, processing, transport, storage, and retail on different aspects of the environment (e.g., climate change, eutrophication, acidification, water scarcity, biodiversity, soil quality, and air pollution) provide a wider picture that should be used to guide our food choices (Figure 2) (153, 159). According to these assessments, the reductions in GHGEs achieved by shifting from animal-sourced foods to plant-sourced alternatives are often offset by the environmental impacts of transporting out-of-season fruits and vegetables across the world, especially when transported by air (160). Similarly, the benefits of reducing GHGEs and land use by replacing animal-sourced foods with isoenergetic volumes of nuts, fruits, and vegetables are reduced for plant-sourced foods that are produced in greenhouses or in climates that require large volumes of freshwater for irrigation (161). This suggests that, while animal-sourced foods (especially red meat) have a more negative impact on the environment than plant-sourced foods in terms of GHGEs, the impact of flexitarian diets that respect regionality and seasonality (i.e., TDDs) may be favorable in terms of energy inputs, pollution, and water use.
FIGURE 2.
The food life cycle and burden on environmental resources. GHGE, greenhouse gas emission; HIC, high-income countries; LMIC, low-/middle-income countries.
Food production
The global consumption of red meat is projected to increase from approximately 190 million metric tons (MMT) in 2018 to more than 376 MMT by 2030 (55). To meet this demand, the expansion of cattle farms has led to large-scale deforestation in some of the most biodiverse regions of the world, with devastating effects on climate change and biodiversity (6, 162). Whereas only 9% of meat is produced using grazing systems, 46% is produced using intensive systems that require large volumes of high-energy, plant-sourced foods, such as soy and alfalfa (163). This is important because the production of animal feeds increases the requirement for land, fertilizer, and water and places cattle in direct competition with humans for nutrition. Converting animal feed to animal-sourced food is also highly inefficient, with as few as 3% of the plant calories in feed converted to calories in beef (164). In addition to land and water use, the expansion of livestock and cattle feed farms has led to eutrophication of freshwater rivers and lakes, and acidification of seawater due to nitrogen and phosphorus leaching from manure and excessive use of fertilizers on animal feed farms (165). Although the environmental impact of animal-sourced foods can be reduced by reducing our consumption of red meat, further benefits can be gained from changes in farming practices, such as recycling manure as fertilizer for crops, converting manure into biogas, and/or feeding cattle on grasslands instead of (or alongside) animal feeds.
In terms of plant-sourced foods, agricultural practices increasingly rely on the use of chemical fertilizers to restore nutrients to the soil, thereby enabling farmers to plant just 1 crop, without the need for rotational cropping (i.e., monocropping) (166). Although monocropping can result in higher food yields and lower prices in the short term, it is also associated with deforestation, poor soil quality, and reduced biodiversity and food security in the long term (167). Organic farming (which uses ecologically based pest control and fertilizers derived from animal/plant waste and nitrogen-fixing crops) can help improve soil quality, prevent soil erosion, and reduce the risk of eutrophication and water contamination due to nitrate, phosphate, and chemical leaching from the soil while recycling plant and animal waste (168). However, the benefits of organic farming are typically offset by the need for more land due to lower yields. Mixed-farming strategies that combine animal farms with crop agriculture can improve our land use while enabling farmers to recycle plant and animal waste into natural fertilizers for crops, thereby reducing the need for chemical fertilizers and reducing eutrophication. Overall, data suggest that the environmental impact of foods varies depending on the way in which they are produced and that the impact of both animal-sourced foods and plant-sourced foods can be reduced by changing the way in which food is produced.
Food losses and waste
Food losses (food lost during production) and food waste (food produced but not used) have a major impact on the environment (169, 170). Food losses are more common in LMICs than in HICs due to increased rates of animal mortality, crop failure, and inadequate farm storage facilities (170). In contrast, food waste is 5- to 10-fold greater per person in HICs than in LMICs, with Europe and North America wasting 18–30 kg of meat per person per year in 2013 compared with 2–5 kg in sub-Saharan Africa and South/Southeast Asia (171). In the United States, consumers waste an average of 422 g of food per person per day, which amounts to 25% of daily food production by weight, 30% of available calories, 4.2 trillion gallons of wasted irrigation water, 3.3 billion pounds of wasted nitrogen/phosphorus fertilizer, and 30 million acres (>120,000 km2; 7%) of wasted cropland per year (169). Globally, the amount of food wasted each year is sufficient to feed nearly 2 billion people a 2100-kcal/d diet (172).
Compared with animal-sourced foods, plant-sourced foods (especially fruits and vegetables) are associated with greater food waste, but less land waste (169, 173, 174). Consistent with this observation, a study conducted among Canadian families found that daily per capita fruit and vegetable waste increased as the quality of the parental diet improved (174). This highlights a need to educate people (particularly those in HICs and/or those people who eat a healthy plant-based diet) about the impact of waste on the environment, the need to balance food purchases with needs, and how to prepare and store (e.g., freeze) perishable foods (175).
Environmental impact of diet type
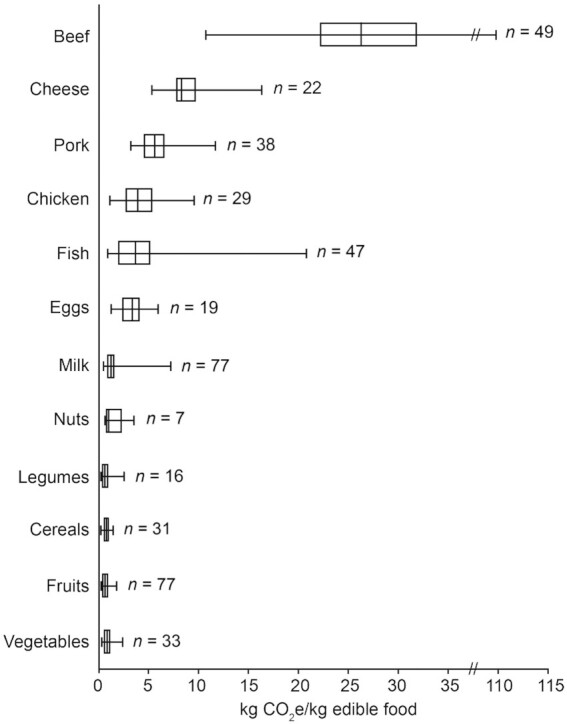
Studies suggest that the environmental impact of food production is higher for omnivorous diets and lower for vegetarian/vegan diets. For example, a meta-analysis of data from 25 studies focusing on the effects of food production on GHGEs found that, compared with omnivorous diets, vegetarian and vegan diets reduced median GHGEs by 35% (range: 13% to 85%) and 49% (23% to 89%), respectively, while reducing land use by 42% (27% to 74%) and 49.5% (29% to 80%) (156). Although vegetarian diets were associated with reduced water use (median: 28%; range: 7% to 52%), the effects of vegan diets varied, with 1 study showing a reduction of 22% and others showing increases ranging from 1% to 107%. Consistent with these data, a modeling study examining the environmental impacts of different dietary scenarios across 150 countries found that transitioning to sustainable healthy diets reduced GHGEs by 54% (flexitarian diets) to 87% (vegan diets), with moderate to small reductions in nitrogen application (23–25%), phosphorus application (18–21%), land use (8–11%), and freshwater use (2–11%) (Figure 3) (15). However, whereas GHGEs and nitrogen application were reduced in all countries, land use, freshwater use, and phosphorus applications were reduced in high- to middle-income countries but increased in low-income countries (LICs) due to differences in crop yields and agricultural inputs (fertilizers, pesticides, and irrigation).
FIGURE 3.
Percentage change in environmental impacts for different diet scenarios worldwide in 2030. Environmental impacts were estimated using a model that combines regional food consumption, production and country-specific environmental footprints for greenhouse gas emissions, cropland use, freshwater use, and nitrogen and phosphorus application, taking into account trade, feed, and processing of primary commodities. The model was calibrated using data from the IMPACT agriculture–economic model. Adapted from reference 15 with permission under the terms of the Creative Commons CC-BY license.
Overall, data suggest that vegan/vegetarian diets are likely to have less impact on the environment than flexitarian diets/TDDs. However, flexitarian diets/TDDs that include very low intakes of red meat; moderate intakes of poultry, eggs, and dairy; and a wide range of seasonal, locally produced plant-sourced foods grown using mixed-farming techniques will have a lower impact on the environment than Western diets.
What Are the Benefits and Limitations of Different Sustainable Healthy Diets in Terms of Affordability, Accessibility, and Cultural Acceptability?
Affordability and accessibility
Accessibility and affordability of nutritious diets vary between countries. According to the United Nations, approximately 26% of the world population does not have regular access to nutritious foods and currently experiences food insecurity, whereas wealthier populations have access to excessive amounts of food, leading to high rates of obesity and large volumes of waste (176). For example, vegetables, fruits, and certain nuts (excluding peanuts) that are high in essential nutrients are often less affordable in LMICs than in HICs. Moreover, more than 40% of all red meat produced globally in 2018 was consumed in HICs by less than 25% of the world's population (171). Greater efforts are required to ensure that affordable and nutritious foods are evenly distributed across the world.
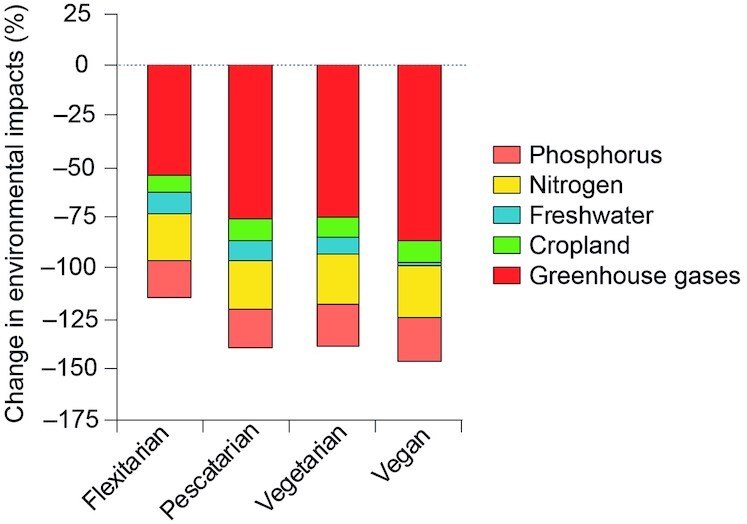
According to food prices for 159 countries, the minimum daily cost in US$ of EAT Lancet diets in 2011 ranged from $2.42 per person in LICs to $2.66 in HICs, with the greatest costs attributed to fruits and vegetables (31.2%); legumes and nuts (18.7%); meat, eggs, and fish (15.2%); and dairy (13.2%) (177). This suggests that sustainable healthy diets account for a small proportion of average income in HICs and are generally similar or less expensive than national diets (13, 178, 179). In contrast, EAT Lancet diets can be 1.5 times more expensive than the cheapest nutritional diet in LICs (180), with costs exceeding income for approximately 1.6 billion people in the developing world. A study assessing food prices in Switzerland in 2011 found that vegetarian and flexitarian diets were slightly cheaper than vegan and pescatarian diets (Figure 4) (179). However, further studies are required to determine whether this relationship applies to other countries.
FIGURE 4.
Cost of 9 diet scenarios relative to the current diet (REF = 100%). FXT, flexitarian; HGD, healthy global diet; MTO, meat oriented; PST, pescatarian; PTO, protein oriented; REF, reference diet; RSN, recommendation of Swiss Society in Nutrition; TAX, food greenhouse gas tax diet; VGN, vegan; VGT, vegetarian. Adapted from reference 179 with permission under the terms of the Creative Commons CC-BY license.
Acceptability
The acceptability of different foods depends on nutritional and environmental factors as well as functionality (convenience, availability, packaging, durability), socialization (family, friends, habits), sensory attributes (taste and texture), culture (traditions, religions), and context (place, time, and company) (55). However, people's notions of acceptability vary between countries and cultures. Whereas plant-based diets and dairy are generally acceptable in LMICs, meat is often excluded from the diet due to cultural, financial, ethical, and/or religious reasons (4). In contrast, people in HICs often consider meat to be an important part of a meal and believe vegetarian/vegan diets to be inconvenient, difficult to prepare, and less enjoyable than omnivorous diets (181, 182). Whereas consumers in Europe are moderately open to substituting meat with dairy, fish, and eggs, they are less keen to replace meat with plant-sourced alternatives and even more unwilling to try novel foods, such as insects or synthetic meat (183, 184). In the United States, up to 84% of people transitioning from Western diets to vegan/vegetarian diets eventually revert back to their original diet, with 53% giving up after 1 y (185). For these people, flexitarian diets/TDDs that include a wider range of foods than vegan/vegetarian diets can provide an easier transition to sustainable healthy diets, due to increased availability and convenience in HICs and because there is no need to exclude certain foods, making it easier to share and enjoy mealtimes with people who eat omnivorous as well as plant-based diets (32, 186). Moreover, flexitarian diets/TDDs enable the use of animal sources as a minor part of a meal or as seasoning in order to provide the tastes that humans seek (umami, salt, fat) but cannot easily obtain from “neutral” tasting plant-sourced foods (187, 188). Overall, evidence suggests that flexitarian diets/TDDs are more acceptable and easier to sustain in HICs than vegetarian/vegan diets, whereas the opposite might be true for some LMICs. However, trends are changing in both regions (9, 189).
Sustainable Healthy Diets Should Be Optimized for Different Populations
Diet-modeling studies show that the number and types of food items that need to be changed to achieve sustainable healthy diets vary between countries depending on baseline diets, food availability/preferences, local culture and traditions, and national targets (4, 54, 190, 191). To minimize the number of food changes (thereby maximizing acceptability and the likelihood of long-term compliance with recommended dietary changes), sustainable healthy diets are often optimized for different countries (12, 13, 33, 81, 179, 192–200). Most sustainable healthy diets are based on energy/nutrient requirements for the “average” adult/adult male (2). However, energy and nutrient requirements vary between populations and, without careful adjustment, recommended diets might not be suitable for populations with different energy or nutrient needs. Consequently, modeling studies are beginning to emerge that optimize country-specific sustainable healthy diets for different populations. Population-specific recommendations are available for children over 9 y of age, adolescents, women, the elderly, and vegans (12, 54, 201–203). Further studies are required to optimize sustainable healthy diets for other populations, including infants, young children, pregnant and/or lactating women, vegetarians, pescatarians, flexitarians, and people following TDDs.
Conclusions
Traditional plant-based diets (vegan/vegetarian/pescatarian diets) are consumed by large numbers of people who wish to reduce their intake of animal-sourced foods due to religious, cultural, health, or ethical (i.e., animal welfare and/or environmental) reasons. Compared with Western diets, plant-based diets can reduce the risk of obesity, NCDs, and premature mortality while reducing the impact of food production on the environment (Table 1). However, without professional supervision, traditional plant-based diets (i.e., vegan/vegetarian/pescatarian diets) can also increase the risk of nutritional deficiencies, mainly among infants, children/adolescents, women, pregnant and/or lactating women, and the elderly. Greater efforts are required to ensure that HCPs receive adequate nutritional training and that nutritional support is available for people following these diets across the world.
Unlike vegan/vegetarian/pescatarian diets, predominantly plant-based flexitarian diets/TDDs can meet the energy and nutrition needs of different populations without the need for dietary education or supplementation (Table 1). Moreover, studies suggest they have a more sustainable impact on the environment than Western diets (especially if diets include locally sourced seasonal foods), and may be more acceptable and easier to maintain than less diverse vegan/vegetarian/pescatarian diets for people transitioning from Western diets to sustainable healthy alternatives. Further studies are required to define more precisely optimal sustainable healthy diets (taking into account the 4 pillars underlying these diets) for different populations and to ensure that diets are accessible to people in LMICs as well as in HICs. Ensuring the adoption and maintenance of healthy sustainable diets will require educating all stakeholders (including families, HCPs, governments, food industries, and marketing companies) about the need for sustainable healthy diets, providing guidance to tailor sustainable healthy diets according to the energy/nutritional requirements of specific populations, while reducing food waste and ensuring the food system can provide different types of affordable, nutritious foods across all regions of the world.
Acknowledgments
Editorial assistance for the preparation of this article was provided by Jackie Read, PhD, from Chill Pill Media Ltd., funded by Danone Institute International (a nonprofit organization). This article was based on discussions held during a workshop dedicated to healthy and sustainable diets, during which PVV, OG, JH, and SD presented background information and all authors discussed key concepts and identified the need to compare the different types of plant-based diets in terms of health and nutrition, affordability and accessibility, cultural acceptability, and the environment. Tables were provided by RM and SD. All authors contributed to the writing of the manuscript, and read and approved the final manuscript.
Notes
Author disclosures: OG is a member of the board of Danone Institute International, a nonprofit organization. OG, SMD, and FJK are members of the Scientific Advisory Board of the Yogurt In Nutrition Initiative for Sustainable and Balanced Diets (YINI), which is funded by the Danone Institute International. LAM is a past member of the Scientific Advisory Board of the YINI. SMD has received support for attending meetings and/or travel from Danone Institute International; consulting fees from Danone Institute International in her role as a YINI Board member, The Dannon Company, ByHeart, Alcimed, and Austnutria; and payment or honoraria for lectures, presentations, speakers’ bureaus, manuscript writing, or educational events from The Beef Council, Austnutria, Danone Institute International, and PRIME education. Grants have been paid to SMD's institution by the NIH, USDA, National Dairy Council, Nestle Nutrition, Mead Johnson Nutrition, the Dannon Company, The Gerber Foundation, International Flavors & Fragrances Inc., Kyowa Hakka Bio, and Triton Algae Innovations. JH reports grants or contracts paid to her institution by the Canadian Institutes for Health Research, Danone Institute North America, Health Canada, and the NIH. JH has been awarded the 2021 Danone International Prize for Alimentation. She has also received an honorarium from Danone Institute International for presenting at an international meeting and support for attending meetings from Health Canada, Danone Institute International, and the Canadian Nutrition Society. PvV has received research grants for a Top Institute Food and Nutrition (TiFN)-coordinated Public Private Partnership (2015–2020), and a grant from the Dutch Dairy Association (2020–2021). He also reports payments or small honoraria for public presentations, manuscript writing, or educational events from Danone Institute International. RM reports consulting fees and payment or honoraria for lectures, presentations, speakers’ bureaus, manuscript writing, or educational events from Abbott Laboratories, Nutricia/Danone, Nestle, and Mead Johnson.
Perspective articles allow authors to take a position on a topic of current major importance or controversy in the field of nutrition. As such, these articles could include statements based on author opinions or point of view. Opinions expressed in Perspective articles are those of the author and are not attributable to the funder(s) or the sponsor(s) or the publisher, Editor, or Editorial Board of Advances in Nutrition. Individuals with different positions on the topic of a Perspective are invited to submit their comments in the form of a Perspectives article or in a Letter to the Editor.
Abbreviations used: BMD, bone mineral density; GHGE, greenhouse gas emission; HCP, health care professional; HIC, high-income country; LIC, low-income country; LMIC, low-to-middle-income country; MMT, million metric tons; NCD, noncommunicable disease; RNI, reference nutrient intake; SGA, small-for-gestational age; TDD, territorial diversified diet; WRI, World Resources Institute.
Contributor Information
Luis A Moreno, GENUD (Growth, Exercise, Nutrition and Development) Research Group, Universidad de Zaragoza, Instituto Agroalimentario de Aragón (IA2), Instituto de Investigación Sanitaria de Aragón (IIS Aragón), Zaragoza, Spain; Centro de Investigación Biomédica en Red de Fisiopatología de la Obesidad y Nutrición (CIBEROBN), Instituto de Salud Carlos III, Madrid, Spain.
Rosan Meyer, Department of Pediatrics, Imperial College London, London, United Kingdom.
Sharon M Donovan, Department of Food Science and Human Nutrition, University of Illinois, Urbana, IL, USA.
Olivier Goulet, Department of Pediatric Gastroenterology-Hepatology-Nutrition, University Hospital Necker-Enfants Malades, University Paris-Centre, Paris, France.
Jess Haines, Department of Family Relations and Applied Nutrition, University of Guelph, Guelph, Ontario, Canada.
Frans J Kok, Division of Human Nutrition and Health, Wageningen University, Wageningen University, Wageningen, The Netherlands.
Pieter van't Veer, Division of Human Nutrition and Health, Wageningen University, Wageningen University, Wageningen, The Netherlands.
References
- 1. Food and Agriculture Organization of the United Nations . The future of food and agriculture—alternative pathways to 2050 [Internet]. Rome (Italy): FAO; 2018. Available from: https:ca1553en.pdf (accessed May 2021). [Google Scholar]
- 2. Willett W, Rockstrom J, Loken B, Springmann M, Lang T, Vermeulen S, Garnett T, Tilman D, DeClerck F, Wood Aet al. Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet North Am Ed. 2019;393(10170):447–92. [DOI] [PubMed] [Google Scholar]
- 3. WHO . A Comprehensive Global Monitoring Framework, including indicators, and a set of voluntary global targets for the prevention and control of noncommunicable diseases, 2012 [Internet]. Available from: https://www.who.int/nmh/events/2012/discussion_paper2_20120322.pdf (accessed May 2021). [Google Scholar]
- 4. Sharma M, Kishore A, Roy D, Joshi K. A comparison of the Indian diet with the EAT-Lancet reference diet. BMC Public Health. 2020;20(1):812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Food and Agriculture Organization of the United Nations/WHO . Sustainable healthy diets: guiding principles, 2019 [Internet]. Available from: www.who.int/publications/i/item/9789241516648 (accessed May 2021). [Google Scholar]
- 6. Ranganathan JVD, Waite R, Dumas P, Lipinski P, Searchinger T; GlobAgri-WRR Model Authors . Shifting diets for a sustainable food future [Internet]. Washington (DC): World Resources Institute; 2016. Available from: www.wri.org/research/shifting-diets-sustainable-food-future (accessed May 2021). [Google Scholar]
- 7. United Nations System Standing Committee on Nutrition. Sustainable diets for healthy people and a healthy planet 2017 [Internet]. Available from: www.unscn.org/uploads/web/news/document/Climate-Nutrition-Paper-EN-WEB.pdf (accessed May 2021). [Google Scholar]
- 8. Food and Agriculture Organization of the United Nations . Plates, Pyramid, planet [Internet]. 2016. Available from: www.i5640e.pdf (accessed May 2021). [Google Scholar]
- 9. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. United Nations . Report of the Conference of the Parties on its twenty-first session, held in Paris from 30 November to 13 December 2015. Addendum. Part two: Action taken by the Conference of the Parties at its twenty-first session 2016 [Internet]. Available from: www.unfccc.int/resource/docs/2015/cop21/eng/10a01.pdf (accessed May 2021). [Google Scholar]
- 11. Ranganathan J, Waite R. Sustainable diets: what you need to know in 12 charts [Internet]. Available from: www.wri.org/insights/sustainable-diets-what-you-need-know-12-charts (accessed May 2021). [Google Scholar]
- 12. World Wide Fund for Nature (WWF) EATWELL. Contributors: G Kramer, B Durlinger, L Kuling, W-J van Zeist, H Blonk, R Broekema, S Ha . Eating for 2 degrees. New and updated LIVEWELL plates [Internet]. 2017. Available from: www.wwf.org.uk/sites/default/files/2017-09/WWF_Livewell_Plates_Full_Report_Sept2017_Web.pdf (accessed May 2021). [Google Scholar]
- 13. World Wide Fund for Nature (WWF) . Towards a low carbon, healthy and affordable diet [Internet]. 2017. Available from: www.wwf.fr/sites/default/files/doc-2020-11/%5BEN%5D_UPD201905_Rapport_Towards-a-low-carbon-diet_WWF.pdf (accessed May 2021). [Google Scholar]
- 14. Derbyshire EJ. Flexitarian diets and health: a review of the evidence-based literature. Front Nutr. 2016;3:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Springmann M, Wiebe K, Mason-D'Croz D, Sulser TB, Rayner M, Scarborough P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: a global modelling analysis with country-level detail. Lancet Planet Health. 2018;2(10):e451–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hachem F, Vanham D, Moreno LA. Territorial and sustainable healthy diets. Food Nutr Bull. 2020;41(2_suppl):87S–103S. [DOI] [PubMed] [Google Scholar]
- 17. Lawrence MA, Baker PI, Pulker CE, Pollard CM. Sustainable, resilient food systems for healthy diets: the transformation agenda. Public Health Nutr. 2019;22(16):2916–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Springmann M, Afshin A, Rivera JA, Wang DD, Willett W. The benefits of the EAT-Lancet Commission's dietary recommendations are significant and robust. J Nutr. 2020;150(10):2837–8. [DOI] [PubMed] [Google Scholar]
- 19. Zagmutt FJ, Pouzou JG, Costard S. The EAT-Lancet Commission: a flawed approach?. Lancet North Am Ed. 2019;394(10204):1140–1. [DOI] [PubMed] [Google Scholar]
- 20. Knuppel A, Papier K, Key TJ, Travis RC. EAT-Lancet score and major health outcomes: the EPIC-Oxford study. Lancet North Am Ed. 2019;394(10194):213–14. [DOI] [PubMed] [Google Scholar]
- 21. Orlich MJ, Singh PN, Sabate J, Jaceldo-Siegl K, Fan J, Knutsen S, Beeson WL, Fraser GE. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med. 2013;173(13):1230–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dinu M, Abbate R, Gensini GF, Casini A, Sofi F. Vegetarian, vegan diets and multiple health outcomes: a systematic review with meta-analysis of observational studies. Crit Rev Food Sci Nutr. 2017;57(17):3640–9. [DOI] [PubMed] [Google Scholar]
- 23. Rocha JP, Laster J, Parag B, Shah NU. Multiple health benefits and minimal risks associated with vegetarian diets. Curr Nutr Rep. 2019;8(4):374–81. [DOI] [PubMed] [Google Scholar]
- 24. Appleby PN, Key TJ. The long-term health of vegetarians and vegans. Proc Nutr Soc. 2016;75(3):287–93. [DOI] [PubMed] [Google Scholar]
- 25. Tonstad S, Butler T, Yan R, Fraser GE. Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diabetes Care. 2009;32(5):791–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tonstad S, Stewart K, Oda K, Batech M, Herring RP, Fraser GE. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2. Nutr Metab Cardiovasc Dis. 2013;23(4):292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Agrawal S, Millett CJ, Dhillon PK, Subramanian SV, Ebrahim S. Type of vegetarian diet, obesity and diabetes in adult Indian population. Nutr J. 2014;13(1):89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rizzo NS, Sabate J, Jaceldo-Siegl K, Fraser GE. Vegetarian dietary patterns are associated with a lower risk of metabolic syndrome: the adventist health study 2. Diabetes Care. 2011;34(5):1225–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mayr HL, Tierney AC, Thomas CJ, Ruiz-Canela M, Radcliffe J, Itsiopoulos C. Mediterranean-type diets and inflammatory markers in patients with coronary heart disease: a systematic review and meta-analysis. Nutr Res. 2018;50:10–24. [DOI] [PubMed] [Google Scholar]
- 30. Rodenas S, Sanchez-Muniz FJ, Bastida S, Sevillano MI, Larrea Marin T, Gonzalez-Munoz MJ. Blood pressure of omnivorous and semi-vegetarian postmenopausal women and their relationship with dietary and hair concentrations of essential and toxic metals. Nutr Hosp. 2011;26(4):874–83. [DOI] [PubMed] [Google Scholar]
- 31. Pettersen BJ, Anousheh R, Fan J, Jaceldo-Siegl K, Fraser GE. Vegetarian diets and blood pressure among white subjects: results from the Adventist Health Study-2 (AHS-2). Public Health Nutr. 2012;15(10):1909–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mantzioris E, Villani A. Translation of a Mediterranean-style diet into the Australian Dietary Guidelines: a nutritional, ecological and environmental perspective. Nutrients. 2019;11(10):2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Paivarinta E, Itkonen ST, Pellinen T, Lehtovirta M, Erkkola M, Pajari AM. Replacing animal-based proteins with plant-based proteins changes the composition of a whole Nordic diet—a randomised clinical trial in healthy Finnish adults. Nutrients. 2020;12(4):943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Li SS, Blanco Mejia S, Lytvyn L, Stewart SE, Viguiliouk E, Ha V, de Souza RJ, Leiter LA, Kendall CWC, Jenkins DJAet al. Effect of plant protein on blood lipids: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2017;6(12):e006659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Viguiliouk E, Kendall CW, Kahleova H, Rahelic D, Salas-Salvado J, Choo VL, Mejia SB, Stewart SE, Leiter LA, Jenkins DJet al. Effect of vegetarian dietary patterns on cardiometabolic risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trials. Clin Nutr. 2019;38(3):1133–45. [DOI] [PubMed] [Google Scholar]
- 36. Penniecook-Sawyers JA, Jaceldo-Siegl K, Fan J, Beeson L, Knutsen S, Herring P, Fraser GE. Vegetarian dietary patterns and the risk of breast cancer in a low-risk population. Br J Nutr. 2016;115(10):1790–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tantamango-Bartley Y, Knutsen SF, Knutsen R, Jacobsen BK, Fan J, Beeson WL, Sabate J, Hadley D, Jaceldo-Siegl K, Penniecook Jet al. Are strict vegetarians protected against prostate cancer?. Am J Clin Nutr. 2016;103(1):153–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Orlich MJ, Fraser GE. Diet and colorectal cancer incidence—reply. JAMA Intern Med. 2015;175(10):1727. [DOI] [PubMed] [Google Scholar]
- 39. Turner-McGrievy G, Mandes T, Crimarco A. A plant-based diet for overweight and obesity prevention and treatment. J Geriatr Cardiol. 2017;14(5):369–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Turner-McGrievy GM, Davidson CR, Wingard EE, Wilcox S, Frongillo EA. Comparative effectiveness of plant-based diets for weight loss: a randomized controlled trial of five different diets. Nutrition. 2015;31(2):350–8. [DOI] [PubMed] [Google Scholar]
- 41. Huang RY, Huang CC, Hu FB, Chavarro JE. Vegetarian diets and weight reduction: a meta-analysis of randomized controlled trials. J Gen Intern Med. 2016;31(1):109–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rosell M, Appleby P, Spencer E, Key T. Weight gain over 5 years in 21,966 meat-eating, fish-eating, vegetarian, and vegan men and women in EPIC-Oxford. Int J Obes. 2006;30(9):1389–96. [DOI] [PubMed] [Google Scholar]
- 43. Spencer EA, Appleby PN, Davey GK, Key TJ. Diet and body mass index in 38000 EPIC-Oxford meat-eaters, fish-eaters, vegetarians and vegans. Int J Obes. 2003;27(6):728–34. [DOI] [PubMed] [Google Scholar]
- 44. Newby PK, Tucker KL, Wolk A. Risk of overweight and obesity among semivegetarian, lactovegetarian, and vegan women. Am J Clin Nutr. 2005;81(6):1267–74. [DOI] [PubMed] [Google Scholar]
- 45. Baines S, Powers J, Brown WJ. How does the health and well-being of young Australian vegetarian and semi-vegetarian women compare with non-vegetarians?. Public Health Nutr. 2007;10(5):436–42. [DOI] [PubMed] [Google Scholar]
- 46. Rizzo NS, Jaceldo-Siegl K, Sabate J, Fraser GE. Nutrient profiles of vegetarian and nonvegetarian dietary patterns. J Acad Nutr Diet. 2013;113(12):1610–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Comerford KB, Miller GD, Reinhardt Kapsak W, Brown KR. The complementary roles for plant-source and animal-source foods in sustainable healthy diets. Nutrients. 2021;13(10):3469–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Teucher B, Olivares M, Cori H. Enhancers of iron absorption: ascorbic acid and other organic acids. Int J Vitam Nutr Res. 2004;74(6):403–19. [DOI] [PubMed] [Google Scholar]
- 49. Melse-Boonstra A. Bioavailability of micronutrients from nutrient-dense whole foods: zooming in on dairy, vegetables, and fruits. Front Nutr. 2020;7:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Tan S, Ke Z, Chai D, Miao Y, Luo K, Li W. Lycopene, polyphenols and antioxidant activities of three characteristic tomato cultivars subjected to two drying methods. Food Chem. 2021;338:128062. [DOI] [PubMed] [Google Scholar]
- 51. Fardet A. Characterization of the degree of food processing in relation with its health potential and effects. Adv Food Nutr Res. 2018;85:79–129. [DOI] [PubMed] [Google Scholar]
- 52. Feitosa S, Greiner R, Meinhardt AK, Muller A, Almeida DT, Posten C. Effect of traditional household processes on iron, zinc and copper bioaccessibility in black bean (Phaseolus vulgaris L.). Foods. 2018;7(8):123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rousseau S, Kyomugasho C, Celus M, Hendrickx MEG, Grauwet T. Barriers impairing mineral bioaccessibility and bioavailability in plant-based foods and the perspectives for food processing. Crit Rev Food Sci Nutr. 2020;60(5):826–43. [DOI] [PubMed] [Google Scholar]
- 54. Fallon N, Dillon SA. Low intakes of iodine and selenium amongst vegan and vegetarian women highlight a potential nutritional vulnerability. Front Nutr. 2020;7:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hicks TM, Knowles SO, Farouk MM. Global provisioning of red meat for flexitarian diets. Front Nutr. 2018;5:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Leser S. The 2013 FAO report on dietary protein quality evaluation in human nutrition: recommendations and implications. Nutr Bull. 2013;38(4):421–8. [Google Scholar]
- 57. Petti A, Palmieri B, Vadalà M, Laurino C. Vegetarianism and veganism: not only benefits but also gaps. Prog Nutr. 2017;19:229–42. [Google Scholar]
- 58. Marinangeli CPF, House JD. Potential impact of the digestible indispensable amino acid score as a measure of protein quality on dietary regulations and health. Nutr Rev. 2017;75(8):658–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kahleova H, Hlozkova A, Fleeman R, Fletcher K, Holubkov R, Barnard ND. Fat quantity and quality, as part of a low-fat, vegan diet, are associated with changes in body composition, insulin resistance, and insulin secretion: a 16-week randomized controlled trial. Nutrients. 2019;11(3):615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kornsteiner M, Singer I, Elmadfa I. Very low n-3 long-chain polyunsaturated fatty acid status in Austrian vegetarians and vegans. Ann Nutr Metab. 2008;52(1):37–47. [DOI] [PubMed] [Google Scholar]
- 61. Davey GK, Spencer EA, Appleby PN, Allen NE, Knox KH, Key TJ. EPIC-Oxford: lifestyle characteristics and nutrient intakes in a cohort of 33 883 meat-eaters and 31 546 non meat-eaters in the UK. Public Health Nutr. 2003;6(3):259–68. [DOI] [PubMed] [Google Scholar]
- 62. Schupbach R, Wegmuller R, Berguerand C, Bui M, Herter-Aeberli I. Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland. Eur J Nutr. 2017;56(1):283–93. [DOI] [PubMed] [Google Scholar]
- 63. National Institutes of Health . Vitamin D factsheet for health professionals [Internet]. 2020. Available from: https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#en1 (accessed May 2021). [Google Scholar]
- 64. Pawlak R, Bell K. Iron status of vegetarian children: a review of literature. Ann Nutr Metab. 2017;70(2):88–99. [DOI] [PubMed] [Google Scholar]
- 65. Pawlak R, Berger J, Hines I. Iron status of vegetarian adults: a review of literature. Am J Lifestyle Med. 2018;12(6):486–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Zijp IM, Korver O, Tijburg LB. Effect of tea and other dietary factors on iron absorption. Crit Rev Food Sci Nutr. 2000;40(5):371–98. [DOI] [PubMed] [Google Scholar]
- 67. Institute of Medicine (US) Panel on Micronutrients . Dietary Reference Intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington (DC): The National Academies Press; 2001. [PubMed] [Google Scholar]
- 68. Avnon T, Paz Dubinsky E, Lavie I, Ben-Mayor Bashi T, Anbar R, Yogev Y. The impact of a vegan diet on pregnancy outcomes. J Perinatol. 2021;41(5):1129–33. [DOI] [PubMed] [Google Scholar]
- 69. Piccoli GB, Clari R, Vigotti FN, Leone F, Attini R, Cabiddu G, Mauro G, Castelluccia N, Colombi N, Capizzi Iet al. Vegan-vegetarian diets in pregnancy: danger or panacea? A systematic narrative review. BJOG Int J Obstet Gynaecol. 2015;122(5):623–33. [DOI] [PubMed] [Google Scholar]
- 70. Ferrara P, Sandullo F, Di Ruscio F, Franceschini G, Peronti B, Blasi V, Bietolini S, Ruggiero A. The impact of lacto-ovo-/lacto-vegetarian and vegan diets during pregnancy on the birth anthropometric parameters of the newborn. J Matern Fetal Neonatal Med. 2019;25:1–7., doi: 10.1080/14767058.2019.1590330. [DOI] [PubMed] [Google Scholar]
- 71. Kesary Y, Avital K, Hiersch L. Maternal plant-based diet during gestation and pregnancy outcomes. Arch Gynecol Obstet. 2020;302(4):887–98. [DOI] [PubMed] [Google Scholar]
- 72. Maruvada P, Stover PJ, Mason JB, Bailey RL, Davis CD, Field MS, Finnell RH, Garza C, Green R, Gueant JLet al. Knowledge gaps in understanding the metabolic and clinical effects of excess folates/folic acid: a summary, and perspectives, from an NIH workshop. Am J Clin Nutr. 2020;112(5):1390–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Honzik T, Adamovicova M, Smolka V, Magner M, Hruba E, Zeman J. Clinical presentation and metabolic consequences in 40 breastfed infants with nutritional vitamin B12 deficiency—what have we learned?. Eur J Paediatr Neurol. 2010;14(6):488–95. [DOI] [PubMed] [Google Scholar]
- 74. Roda M, di Geronimo N, Pellegrini M, Schiavi C. Nutritional optic neuropathies: state of the art and emerging evidences. Nutrients. 2020;12(9):2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Tong TYN, Appleby PN, Bradbury KE, Perez-Cornago A, Travis RC, Clarke R, Key TJ. Risks of ischaemic heart disease and stroke in meat eaters, fish eaters, and vegetarians over 18 years of follow-up: results from the prospective EPIC-Oxford study. BMJ. 2019;366:l4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Iguacel I, Huybrechts I, Moreno LA, Michels N. Vegetarianism and veganism compared with mental health and cognitive outcomes: a systematic review and meta-analysis. Nutr Rev. 2021;79(4):361–81. [DOI] [PubMed] [Google Scholar]
- 77. Dobersek U, Wy G, Adkins J, Altmeyer S, Krout K, Lavie CJ, Archer E. Meat and mental health: a systematic review of meat abstention and depression, anxiety, and related phenomena. Crit Rev Food Sci Nutr. 2021;61(4):622–35. [DOI] [PubMed] [Google Scholar]
- 78. Menzel J, Abraham K, Stangl GI, Ueland PM, Obeid R, Schulze MB, Herter-Aeberli I, Schwerdtle T, Weikert C. Vegan diet and bone health-results from the cross-sectional RBVD study. Nutrients. 2021;13(2):685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Iguacel I, Miguel-Berges ML, Gomez-Bruton A, Moreno LA, Julian C. Veganism, vegetarianism, bone mineral density, and fracture risk: a systematic review and meta-analysis. Nutr Rev. 2019;77(1):1–18. [DOI] [PubMed] [Google Scholar]
- 80. Tong TYN, Appleby PN, Armstrong MEG, Fensom GK, Knuppel A, Papier K, Perez-Cornago A, Travis RC, Key TJ. Vegetarian and vegan diets and risks of total and site-specific fractures: results from the prospective EPIC-Oxford study. BMC Med. 2020;18(1):353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Broekema R, Tyszler M, van ’t Veer P, Kok FJ, Martin A, Lluch A, Blonk HTJ. Future-proof and sustainable healthy diets based on current eating patterns in the Netherlands. Am J Clin Nutr. 2020;112(5):1338–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. WHO . Breastfeeding [Internet]. 2018. Available from: https:///www.who.int/news-room/facts-in-pictures/detail/breastfeeding (accessed May 2021). [Google Scholar]
- 83. Baldassarre ME, Panza R, Farella I, Posa D, Capozza M, Mauro AD, Laforgia N. Vegetarian and vegan weaning of the infant: how common and how evidence-based? A population-based survey and narrative review. Int J Environ Res Public Health. 2020;17(13):4835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Karcz K, Krolak-Olejnik B. Vegan or vegetarian diet and breast milk composition—a systematic review. Crit Rev Food Sci Nutr. 2021;61(7):1081–98. [DOI] [PubMed] [Google Scholar]
- 85. Donohue JA, Solomons NW, Hampel D, Shahab-Ferdows S, Orozco MN, Allen LH. Micronutrient supplementation of lactating Guatemalan women acutely increases infants' intake of riboflavin, thiamin, pyridoxal, and cobalamin, but not niacin, in a randomized crossover trial. Am J Clin Nutr. 2020;112(3):669–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Perrin MT, Pawlak R, Dean LL, Christis A, Friend L. A cross-sectional study of fatty acids and brain-derived neurotrophic factor (BDNF) in human milk from lactating women following vegan, vegetarian, and omnivore diets. Eur J Nutr. 2019;58(6):2401–10. [DOI] [PubMed] [Google Scholar]
- 87. Pawlak R, Vos P, Shahab-Ferdows S, Hampel D, Allen LH, Perrin MT. Vitamin B-12 content in breast milk of vegan, vegetarian, and nonvegetarian lactating women in the United States. Am J Clin Nutr. 2018;108(3):525–31. [DOI] [PubMed] [Google Scholar]
- 88. Roed C, Skovby F, Lund AM. [Severe vitamin B12 deficiency in infants breastfed by vegans]. Ugeskr Laeger. 2009;171(43):3099–101. [PubMed] [Google Scholar]
- 89. Kuhne T, Bubl R, Baumgartner R. Maternal vegan diet causing a serious infantile neurological disorder due to vitamin B12 deficiency. Eur J Pediatr. 1991;150(3):205–8. [DOI] [PubMed] [Google Scholar]
- 90. Committee for Dietary Guidelines for Americans . Scientific report of the 2020 Dietary Guidelines Advisory Committee: advisory report to the Secretary of Agriculture and the Secretary of Health and Human Services [Internet]. 2020. Available from: www.dietaryguidelines.gov/sites/default/files/2020-07/ScientificReport_of_the_2020DietaryGuidelinesAdvisoryCommittee_first-print.pdf (accessed May 2021). [Google Scholar]
- 91. Committee for Dietary Guidelines for Americans . Dietary Guidelines for Americans, 2020-2025 [Internet]. Available from: www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_Guidelines_for_Americans-2020-2025.pdf (accessed May 2021). [Google Scholar]
- 92. Assaf-Balut C, Garcia de la Torre N, Duran A, Fuentes M, Bordiu E, Del Valle L, Familiar C, Valerio J, Jimenez I, Herraiz MAet al. A Mediterranean diet with an enhanced consumption of extra virgin olive oil and pistachios improves pregnancy outcomes in women without gestational diabetes mellitus: a sub-analysis of the St. Carlos Gestational Diabetes Mellitus Prevention Study. Ann Nutr Metab. 2019;74(1):69–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. de la Torre NG, Assaf-Balut C, Jimenez Varas I, Del Valle L, Duran A, Fuentes M, Del Prado N, Bordiu E, Valerio JJ, Herraiz MAet al. Effectiveness of following Mediterranean diet recommendations in the real world in the incidence of gestational diabetes mellitus (GDM) and adverse maternal-foetal outcomes: a prospective, universal, interventional study with a single group. The St Carlos Study. Nutrients. 2019;11(6):1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Sebastiani G, Herranz Barbero A, Borras-Novell C, Alsina Casanova M, Aldecoa-Bilbao V, Andreu-Fernandez V, Pascual Tutusaus M, Ferrero Martinez S, Gomez Roig MD, Garcia-Algar O. The effects of vegetarian and vegan diet during pregnancy on the health of mothers and offspring. Nutrients. 2019;11(3):557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Hanson MA, Bardsley A, De-Regil LM, Moore SE, Oken E, Poston L, Ma RC, McAuliffe FM, Maleta K, Purandare CNet al. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition: “Think nutrition first.” Int J Gynecol Obstet. 2015;131:S213–53. [DOI] [PubMed] [Google Scholar]
- 96. Lemale J, Mas E, Jung C, Bellaiche M, Tounian P, French-speaking Pediatric Hepatology, Gastroenterology and Nutrition Group . Vegan diet in children and adolescents. Recommendations from the French-speaking Pediatric Hepatology, Gastroenterology and Nutrition Group (GFHGNP). Arch Pediatr. 2019;26(7):442–50. [DOI] [PubMed] [Google Scholar]
- 97. Weder S, Hoffmann M, Becker K, Alexy U, Keller M. Energy, macronutrient intake, and anthropometrics of vegetarian, vegan, and omnivorous children (1-3 years) in Germany (VeChi Diet Study). Nutrients. 2019;11(4):832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, Pfaffle R, Kiess W, Korner A. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. 2018;379(14):1303–12. [DOI] [PubMed] [Google Scholar]
- 99. Fewtrell M, Bronsky J, Campoy C, Domellof M, Embleton N, Fidler Mis N, Hojsak I, Hulst JM, Indrio F, Lapillonne Aet al. Complementary feeding: a position paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2017;64(1):119–32. [DOI] [PubMed] [Google Scholar]
- 100. Lemoine A, Giabicani E, Lockhart V, Grimprel E, Tounian P. Case report of nutritional rickets in an infant following a vegan diet. Arch Pediatr. 2020;27(4):219–22. [DOI] [PubMed] [Google Scholar]
- 101. Lemale J, Salaun JF, Assathiany R, Garcette K, Peretti N, Tounian P. Replacing breastmilk or infant formula with a nondairy drink in infants exposes them to severe nutritional complications. Acta Paediatr. 2018;107(10):1828–9. [DOI] [PubMed] [Google Scholar]
- 102. WHO . Vitamin D supplementation for infants [Internet]. Available from: www.who.int/elena/titles/bbc/vitamind_infants/en/ (accessed May 2021). [Google Scholar]
- 103. Agnoli C, Baroni L, Bertini I, Ciappellano S, Fabbri A, Papa M, Pellegrini N, Sbarbati R, Scarino ML, Siani Vet al. Position paper on vegetarian diets from the working group of the Italian Society of Human Nutrition. Nutr Metab Cardiovasc Dis. 2017;27(12):1037–52. [DOI] [PubMed] [Google Scholar]
- 104. Baroni L, Goggi S, Battino M. Planning well-balanced vegetarian diets in infants, children, and adolescents: the Vegplate Junior. J Acad Nutr Diet. 2019;119(7):1067–74. [DOI] [PubMed] [Google Scholar]
- 105. Mangels RD, Driggers J. The youngest vegetarians: vegetarian infants and toddlers. ICAN Infant Child Adolesc Nutr. 2012;4(1):8–20. [Google Scholar]
- 106. Amalraj A, Pius A. Bioavailability of calcium and its absorption inhibitors in raw and cooked green leafy vegetables commonly consumed in India—an in vitro study. Food Chem. 2015;170:430–6. [DOI] [PubMed] [Google Scholar]
- 107. Charoenkiatkul S, Kriengsinyos W, Tuntipopipat S, Suthutvoravut U, Weaver CM. Calcium absorption from commonly consumed vegetables in healthy Thai women. J Food Sci. 2008;73(9):H218–21. [DOI] [PubMed] [Google Scholar]
- 108. Bettinelli ME, Bezze E, Morasca L, Plevani L, Sorrentino G, Morniroli D, Gianni ML, Mosca F. Knowledge of health professionals regarding vegetarian diets from pregnancy to adolescence: an observational study. Nutrients. 2019;11(5):1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Rudloff S, Buhrer C, Jochum F, Kauth T, Kersting M, Korner A, Koletzko B, Mihatsch W, Prell C, Reinehr Tet al. Vegetarian diets in childhood and adolescence: position paper of the Nutrition Committee, German Society for Paediatric and Adolescent Medicine (DGKJ). Mol Cell Pediatr. 2019;6(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Leroy F, Cofnas N. Should dietary guidelines recommend low red meat intake?. Crit Rev Food Sci Nutr. 2020;60(16):2763–72. [DOI] [PubMed] [Google Scholar]
- 111. Craig WJ, Mangels AR; American Dietetic Association . Position of the American Dietetic Association: vegetarian diets. J Am Diet Assoc. 2009;109(7):1266–82. [DOI] [PubMed] [Google Scholar]
- 112. Amit M. Vegetarian diets in children and adolescents. Paediatr Child Health. 2010;15(5):303–14. [PMC free article] [PubMed] [Google Scholar]
- 113. Richter MB, Grünewald-Funk D, Heseker H, Kroke A, Leschik-Bonnet E, Oberritter H, Strohm D, Watzl B. Vegan diet position of the German Nutrition Society (DGE). Ernaehrungs Umschau Int. 2016;4:92–102. [Google Scholar]
- 114. Muller P. Vegan diet in young children. Nestle Nutr Inst Workshop Ser. 2020;93:103–10. [DOI] [PubMed] [Google Scholar]
- 115. Leroy F, Barnard ND. Children and adults should avoid consuming animal products to reduce risk for chronic disease. Am J Clin Nutr. 2020;112(4):931–6. [DOI] [PubMed] [Google Scholar]
- 116. Hovinen T, Korkalo L, Freese R, Skaffari E, Isohanni P, Niemi M, Nevalainen J, Gylling H, Zamboni N, Erkkola Met al. Vegan diet in young children remodels metabolism and challenges the statuses of essential nutrients. EMBO Mol Med. 2021;13(2):e13492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Willett WC, Ludwig DS. Milk and health. N Engl J Med. 2020;382(7):644–54. [DOI] [PubMed] [Google Scholar]
- 118. Oyen J, Kvestad I, Midtbo LK, Graff IE, Hysing M, Stormark KM, Markhus MW, Baste V, Froyland L, Koletzko Bet al. Fatty fish intake and cognitive function: FINS-KIDS, a randomized controlled trial in preschool children. BMC Med. 2018;16(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Chamorro R, Gonzalez MF, Aliaga R, Gengler V, Balladares C, Barrera C, Bascunan KA, Bazinet RP, Valenzuela R. Diet, plasma, erythrocytes, and spermatozoa fatty acid composition changes in young vegan men. Lipids. 2020;55(6):639–48. [DOI] [PubMed] [Google Scholar]
- 120. Montenegro-Bethancourt G, Johner SA, Stehle P, Remer T. Dietary ratio of animal:plant protein is associated with 24-h urinary iodine excretion in healthy school children. Br J Nutr. 2015;114(1):24–33. [DOI] [PubMed] [Google Scholar]
- 121. Temme EH, Bakker HM, Seves SM, Verkaik-Kloosterman J, Dekkers AL, van Raaij JM, Ocke MC. How may a shift towards a more sustainable food consumption pattern affect nutrient intakes of Dutch children?. Public Health Nutr. 2015;18(13):2468–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Public Health England . Government dietary recommendations [Internet]. 2016. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/618167/government_dietary_recommendations.pdf (accessed May 2021). [Google Scholar]
- 123. Bath SC, Hill S, Infante HG, Elghul S, Nezianya CJ, Rayman MP. Iodine concentration of milk-alternative drinks available in the UK in comparison with cows' milk. Br J Nutr. 2017;118(7):525–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Lindorfer H, Krebs M, Kautzky-Willer A, Bancher-Todesca D, Sager M, Gessl A. Iodine deficiency in pregnant women in Austria. Eur J Clin Nutr. 2015;69(3):349–54. [DOI] [PubMed] [Google Scholar]
- 125. Carter JP, Furman T, Hutcheson HR. Preeclampsia and reproductive performance in a community of vegans. South Med J. 1987;80(6):692–7. [DOI] [PubMed] [Google Scholar]
- 126. Qiu C, Coughlin KB, Frederick IO, Sorensen TK, Williams MA. Dietary fiber intake in early pregnancy and risk of subsequent preeclampsia. Am J Hypertens. 2008;21(8):903–9. [DOI] [PubMed] [Google Scholar]
- 127. Longo-Mbenza B, Tshimanga KB, Buassa-bu-Tsumbu B, Kabangu MJ. Diets rich in vegetables and physical activity are associated with a decreased risk of pregnancy induced hypertension among rural women from Kimpese, DR Congo. Niger J Med. 2008;17(3):265–9. [PubMed] [Google Scholar]
- 128. Asemi Z, Samimi M, Tabassi Z, Esmaillzadeh A. The effect of DASH diet on pregnancy outcomes in gestational diabetes: a randomized controlled clinical trial. Eur J Clin Nutr. 2014;68(4):490–5. [DOI] [PubMed] [Google Scholar]
- 129. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell Ret al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet North Am Ed. 2013;382(9890):427–51. [DOI] [PubMed] [Google Scholar]
- 130. Perez-Roncero GR, Lopez-Baena MT, Chedraui P, Perez-Lopez FR. The effect of consuming milk and related products during human pregnancy over birth weight and perinatal outcomes: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020;251:235–45. [DOI] [PubMed] [Google Scholar]
- 131. European Food Safety Authority (EFSA) . Dietary Reference Values for nutrients: summary report. Parma (Italy): European Food Safety Authority; 2017. Available from: 10.2903/sp.efsa.2017.e15121(accessed May 2021). [DOI] [Google Scholar]
- 132. Physicians Committee for Responsible Medicine . Vegetarian diets for pregnancy [Internet]. Available from: www.pcrm.org/health/veginfo/pregnancy.html (accessed May 2021). [Google Scholar]
- 133. Lyu Y, Yu X, Yuan H, Yi X, Dong X, Ding M, Lin X, Wang B. Associations between dietary patterns and physical fitness among Chinese elderly. Public Health Nutr. 2021;24(14): 4466–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Ramey MM, Shields GS, Yonelinas AP. Markers of a plant-based diet relate to memory and executive function in older adults. Nutr Neurosci. 2020:1–10.. doi: 10.1080/1028415X.2020.1751506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Norman K, Klaus S. Veganism, aging and longevity: new insight into old concepts. Curr Opin Clin Nutr Metab Care. 2020;23(2):145–50. [DOI] [PubMed] [Google Scholar]
- 136. Lanham-New SA. Is “vegetarianism” a serious risk factor for osteoporotic fracture?. Am J Clin Nutr. 2009;90(4):910–11. [DOI] [PubMed] [Google Scholar]
- 137. Ho-Pham LT, Nguyen ND, Nguyen TV. Effect of vegetarian diets on bone mineral density: a Bayesian meta-analysis. Am J Clin Nutr. 2009;90(4):943–50. [DOI] [PubMed] [Google Scholar]
- 138. Force U, Grossman DC, Curry SJ, Owens DK, Barry MJ, Caughey AB, Davidson KW, Doubeni CA, Epling JW Jr, Kemper ARet al. Vitamin D, calcium, or combined supplementation for the primary prevention of fractures in community-dwelling adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(15):1592–99. [DOI] [PubMed] [Google Scholar]
- 139. Zhao JG, Zeng XT, Wang J, Liu L. Association between calcium or vitamin D supplementation and fracture incidence in community-dwelling older adults: a systematic review and meta-analysis. JAMA. 2017;318(24):2466–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Rizzoli R. Dairy products, yogurts, and bone health. Am J Clin Nutr. 2014;99(5):1256S–62S. [DOI] [PubMed] [Google Scholar]
- 141. Rizzoli R, Bischoff-Ferrari H, Dawson-Hughes B, Weaver C. Nutrition and bone health in women after the menopause. Women Health. 2014;10(6):599–608. [DOI] [PubMed] [Google Scholar]
- 142. Marchi G, Busti F, Zidanes AL, Vianello A, Girelli D. Cobalamin deficiency in the elderly. Med J Hematol Infectious Dis. 2020;12(1):e2020043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. European Society for Gastroenterology and Motility . Gut microbiota for health [Internet]. Available from: www.gutmicrobiotaforhealth.com (accessed May 2021). [Google Scholar]
- 144. Ghosh TS, Rampelli S, Jeffery IB, Santoro A, Neto M, Capri M, Giampieri E, Jennings A, Candela M, Turroni Set al. Mediterranean diet intervention alters the gut microbiome in older people reducing frailty and improving health status: the NU-AGE 1-year dietary intervention across five European countries. Gut. 2020;69(7):1218–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. BMJ. 2018;361:k2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, Abrouk M, Farahnik B, Nakamura M, Zhu THet al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017;15(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Tomova A, Bukovsky I, Rembert E, Yonas W, Alwarith J, Barnard ND, Kahleova H. The effects of vegetarian and vegan diets on gut microbiota. Front Nutr. 2019;6:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. McDonald D, Hyde E, Debelius JW, Morton JT, Gonzalez A, Ackermann G, Aksenov AA, Behsaz B, Brennan C, Chen Yet al. American gut: an open platform for citizen science microbiome research. mSystems. 2018;3(3). doi: 10.1128/mSystems.00031-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Michalak J, Zhang XC, Jacobi F. Vegetarian diet and mental disorders: results from a representative community survey. Int J Behav Nutr Phys Activity. 2012;9(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Paslakis G, Richardson C, Nohre M, Brahler E, Holzapfel C, Hilbert A, de Zwaan M. Prevalence and psychopathology of vegetarians and vegans—results from a representative survey in Germany. Sci Rep. 2020;10(1):6840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Zickgraf HF, Hazzard VM, O'Connor SM, Simone M, Williams-Kerver GA, Anderson LM, Lipson SK. Examining vegetarianism, weight motivations, and eating disorder psychopathology among college students. Int J Eat Disord. 2020;53(9):1506–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Rockstrom J, Steffen W, Noone K, Persson A, Chapin FS 3rd, Lambin EF, Lenton TM, Scheffer M, Folke C, Schellnhuber HJet al. A safe operating space for humanity. Nature. 2009;461(7263):472–5. [DOI] [PubMed] [Google Scholar]
- 153. World Resources Institute . Creating a sustainable food future. In: A menu of solutions to feed nearly 10 billion people by 2050. Washington (DC): World Resources Institute; 2018 [Internet]. Available from: www.research.wri.org/wrr-food (accessed May 2021). [Google Scholar]
- 154. Mertens EKA, van Zanten HHE, Kaptijn G, Dofkova M, Mistura L, D'Addezio L, Turrini A, Dubuisson C, Havard S, Trollw E, Geleijnse JM, van't Veer P. Dietary choices and environmental impact in four European countries. J Cleaner Prod. 2019;237:117827. [Google Scholar]
- 155. Clune S, Crossin E, Verghese K. Systematic review of greenhouse gas emissions for different fresh food categories. J Cleaner Prod. 2017;140:766–83. [Google Scholar]
- 156. Fresan U, Sabate J. Vegetarian diets: planetary health and its alignment with human health. Adv Nutr. 2019;10(Suppl 4):S380–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Eshel G, Shepon A, Makov T, Milo R. Land, irrigation water, greenhouse gas, and reactive nitrogen burdens of meat, eggs, and dairy production in the United States. Proc Natl Acad Sci. 2014;111(33):11996–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Poore JNT. Reducing food's environmental impacts through producers and consumers. Science. 2018;360(6392):987–92. [DOI] [PubMed] [Google Scholar]
- 159. Meyer NL, Reguant-Closa A, Nemecek T. Sustainable diets for athletes. Curr Nutr Rep. 2020;9(3):147–62. [DOI] [PubMed] [Google Scholar]
- 160. Vieux F, Darmon N, Touazi D, Soler LG. Greenhouse gas emissions of self-selected individual diets in France: changing the diet structure or consuming less?. Ecol Econ. 2012;75:91–101. [Google Scholar]
- 161. Tom MS, Fischbeck PS, Hendrickson CT. Energy use, blue water footprint, and greenhouse gas emissions for current food consumption. patterns and dietary recommendations in the US. Environ Syst Decisions. 2016;36(1):92–103. [Google Scholar]
- 162. Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Boykoff M, Byass P, Cai W, Campbell-Lendrum D, Capstick Set al. The 2019 report of the Lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet North Am Ed. 2019;394(10211):1836–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Herrero M, Thornton PK, Notenbaert A, Msangi S, Wood S, Kruska R. Drivers of change in crop–livestock systems and their potential impacts on agro-ecosystems services and human wellbeing to 2030: a study commissioned by the CGIAR Systemwide Livestock Programme. Nairobi: ILRI Project Report; 2012; [Internet]. Available from: https://cgspace.cgiar.org/bitstream/handle/10568/3020/SLP%20drivers%20study%20final%20draft.pdf?sequence=4&isAllowed=y (accessed May 2021). [Google Scholar]
- 164. Shepon A. Energy and protein feed-to-food conversion efficiencies in the US and potential food security gains from dietary changes. Environ Res Lett. 2016;11(10):105002. [Google Scholar]
- 165. Huerta A. Environmental impact of beef production in Mexico through life cycle assessment. Resour Conserv Recycl. 2016;109:44–53. [Google Scholar]
- 166. Lacour C, Seconda L, Alles B, Hercberg S, Langevin B, Pointereau P, Lairon D, Baudry J, Kesse-Guyot E. Environmental impacts of plant-based diets: how does organic food consumption contribute to environmental sustainability?. Front Nutr. 2018;5:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Tauli-Corpuz V, Tamang P. Oil palm and other commercial tree plantations, monocropping: impacts on Indigenous peoples' land tenure and resource management systems and livelihoods. New York; 2007; [Internet]. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwio4-Cbqe71AhVQzRoKHVmIAkEQFnoECAIQAQ&url=https%3A%2F%2Fwww.un.org%2Fesa%2Fsocdev%2Funpfii%2Fdocuments%2F6session_crp6.doc&usg=AOvVaw1MYNNz7jGjks9hkstNpAmL (accessed May 2021). [Google Scholar]
- 168. International Panel of Experts on Sustainable Food Systems . From uniformity to diversity. A paradigm shift from industrial agriculture to diversified agroecological systems [Internet]. 2016. Available from: https:cgspace.cgiar.org/bitstream/handle/10568/75659/UniformityToDiversity_FullReport.pdf?sequence=1&isAllowed=y (accessed May 2021). [Google Scholar]
- 169. Conrad Z, Niles MT, Neher DA, Roy ED, Tichenor NE, Jahns L. Relationship between food waste, diet quality, and environmental sustainability. PLoS One. 2018;13(4):e0195405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Hodges RJ, Buzby JC, Bennett B. Postharvest losses and waste in developed and less developed countries: opportunities to improve resource use. J Agric Sci. 2010;149:37–45. [Google Scholar]
- 171. Food and Agriculture Organization of the United Nations (FAO) . FAOSTAT food balance sheets, April 2015. Rome (Italy): Food and Agriculture Organization of the United Nations (FAO); 2015. [Google Scholar]
- 172. Kummu M, de Moel H, Porkka M, Siebert S, Varis O, Ward PJ. Lost food, wasted resources: global food supply chain losses and their impacts on freshwater, cropland, and fertiliser use. Sci Total Environ. 2012;438:477–89. [DOI] [PubMed] [Google Scholar]
- 173. US Department of Health and Human Services . Manual of laboratory operations, Lipid Research Clinics program, lipid and lipoprotein analysis (revised). Washington (DC): NIH, US Department of Health and Human Services; 1982. [Google Scholar]
- 174. Carroll N, Wallace A, Jewell K, Darlington G, Ma DWL, Duncan AM, Parizeau K, von Massow M, Haines J. Association between diet quality and food waste in Canadian families: a cross-sectional study. Nutr J. 2020;19(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Parfitt J, Barthel M, Macnaughton S. Food waste within food supply chains: quantification and potential for change to 2050. Philos Trans R Soc B Biol Sci. 2010;365(1554):3065–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. FAO; International Fund for Agricultural Development; UNICEF; World Food Program; WHO . The state of food security and nutrition in the world 2019. Safeguarding against economic slowdowns and downturns. Rome (Italy): FAO; 2019. [Google Scholar]
- 177. Hirvonen K, Bai Y, Headey D, Masters WA. Affordability of the EAT-Lancet reference diet: a global analysis. Lancet Global Health. 2020;8(1):e59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Goulding T, Lindberg R, Russell CG. The affordability of a healthy and sustainable diet: an Australian case study. Nutr J. 2020;19(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Chen C, Chaudhary A, Mathys A. Dietary change scenarios and implications for environmental, nutrition, human health and economic dimensions of food sustainability. Nutrients. 2019;11(4):856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. International Institute for Population Sciences (IIPS) and ICF . National Family Health Survey (NFHS-4), 2015-16: India. Mumbai (India): IIPS; 2017. [Google Scholar]
- 181. Bryant C. We can't keep meating like this: attitudes towards vegetarian and vegan diets in the United Kingdom. Sustainability. 2019;11(23):6844. [Google Scholar]
- 182. Alcorta A, Porta A, Tarrega A, Alvarez MD, Vaquero MP. Foods for plant-based diets: challenges and innovations. Foods. 2021;10(2):293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Food System for Health, Environment, Enterprise . Consumers’ knowledge about the determinants for a sustainable diet: SUSFANS, 2016 [Internet]. Available from: https://susfans.eu/system/files/public_files/Publications/Reports/SUSFANS%20D2.1_V1.pdf (accessed May 2021). [Google Scholar]
- 184. Grasso AC, Hung Y, Olthof MR, Verbeke W, Brouwer IA. Older consumers' readiness to accept alternative, more sustainable protein sources in the European Union. Nutrients. 2019;11(8):1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Faunalytics . Just how hard is it to become veg*n?. [Internet]. 2017. Available from: https://faunalytics.org/just-how-hard-is-it-to-become-vegn/(accessed May 2021). [Google Scholar]
- 186. Itsiopoulos C, Kucianski T, Mayr HL, van Gaal WJ, Martinez-Gonzalez MA, Vally H, Kingsley M, Kouris-Blazos A, Radcliffe J, Segal Let al. The AUStralian MEDiterranean Diet Heart Trial (AUSMED Heart Trial): a randomized clinical trial in secondary prevention of coronary heart disease in a multiethnic Australian population: study protocol. Am Heart J. 2018;203:4–11. [DOI] [PubMed] [Google Scholar]
- 187. Schmidt CV, Mouritsen OG. The solution to sustainable eating is not a one-way street. Front Psychol. 2020;11:531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. van Bussel LM, Kuijsten A, Mars M, Feskens EJM, van't Veer P. Taste profiles of diets high and low in environmental sustainability and health. Food Qual Preference. 2019;78:103730. [Google Scholar]
- 189. Le TH, Disegna M, Lloyd T. National food consumption patterns: converging trends and the implications for health. EuroChoices. 2020. doi: 10.1111/1746-692X.12272. [DOI] [Google Scholar]
- 190. Blackstone NT, Conrad Z. Comparing the recommended eating patterns of the EAT-Lancet Commission and Dietary Guidelines for Americans: implications for sustainable nutrition. Curr Dev Nutr. 2020;4(3):nzaa015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Chaudhary A, Krishna V. Country-specific sustainable diets using optimization algorithm. Environ Sci Technol. 2019;53(13):7694–703. [DOI] [PubMed] [Google Scholar]
- 192. Lassen AD, Christensen LM, Trolle E. Development of a Danish adapted healthy plant-based diet based on the EAT-Lancet reference diet. Nutrients. 2020;12(3):738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Perignon M, Masset G, Ferrari G, Barre T, Vieux F, Maillot M, Amiot MJ, Darmon N. How low can dietary greenhouse gas emissions be reduced without impairing nutritional adequacy, affordability and acceptability of the diet? A modelling study to guide sustainable food choices. Public Health Nutr. 2016;19(14):2662–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Song G, Li M, Fullana IPP, Williamson D, Wang Y. Dietary changes to mitigate climate change and benefit public health in China. Sci Total Environ. 2017;577:289–98. [DOI] [PubMed] [Google Scholar]
- 195. Milner J, Joy EJM, Green R, Harris F, Aleksandrowicz L, Agrawal S, Smith P, Haines A, Dangour AD. Projected health effects of realistic dietary changes to address freshwater constraints in India: a modelling study. Lancet Planet Health. 2017;1(1):e26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Eini-Zinab H, Sobhani SR, Rezazadeh A. Designing a healthy, low-cost and environmentally sustainable food basket: an optimisation study. Public Health Nutr. 2021;24(7):1952–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Karlsson JO, Carlsson C, Lindberg M, Sjunnestrand T, Röös E. Designing a future food vision for the Nordics through a participatory modeling approach. Agron Sustainable Dev. 2018;38(6):59. [Google Scholar]
- 198. Milner J, Green R, Dangour AD, Haines A, Chalabi Z, Spadaro J, Markandya A, Wilkinson P. Health effects of adopting low greenhouse gas emission diets in the UK. BMJ Open. 2015;5(4):e007364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Horgan GW, Perrin A, Whybrow S, Macdiarmid JI. Achieving dietary recommendations and reducing greenhouse gas emissions: modelling diets to minimise the change from current intakes. Int J Behav Nutr Phys Activity. 2016;13(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Kramer GF, Tyszler M, Veer PV, Blonk H. Decreasing the overall environmental impact of the Dutch diet: how to find healthy and sustainable diets with limited changes. Public Health Nutr. 2017;20(9):1699–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Brink E, van Rossum C, Postma-Smeets A, Stafleu A, Wolvers D, van Dooren C, Toxopeus I, Buurma-Rethans E, Geurts M, Ocke M. Development of healthy and sustainable food-based dietary guidelines for the Netherlands. Public Health Nutr. 2019;22(13):2419–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Vieux F, Perignon M, Gazan R, Darmon N. Dietary changes needed to improve diet sustainability: are they similar across Europe?. Eur J Clin Nutr. 2018;72(7):951–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Ferrari MB, Rossi L, De Santis A, Sette S, Martone D, Piccinelli R, Le Donne C, Leclercq C, Turrini A. Could dietary goals and climate change mitigation be achieved through optimized diet? The experience of modeling the national food consumption data in Italy. Front Nutr. 2020;7:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. WHO . Human energy requirements: report of a joint FAO/WHO/UNU expert consultation. Secondary human energy requirements: report of a joint FAO/WHO/ UNU expert consultation [Internet]. 2004. Available from: www.who.int/nutrition/publications/micronutrients/9241546123/en/ (accessed October 2021). [Google Scholar]
- 205. Institute of Medicine . Dietary Reference Intakes: the essential guide to nutrient requirements. Washington (DC): The National Academic Press; 2006. doi.org/10.17226/11537. Available from: http://www.nap.edu/catalog/11537.html (accessed October 2021). [Google Scholar]
- 206. Mayo Clinic . Vegetarian diet: how to get the best nutrition. Secondary vegetarian diet: How to get the best nutrition 2020 [Internet]. Available from:www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/vegetarian-diet/art-20046446 (accessed May 2021). [Google Scholar]
- 207. British Nutrition Foundation . Protein [Internet]. 2012. Available from: https://www.nutrition.org.uk/nutritionscience/nutrients-food-and-ingredients/protein.html (accessed May 2021). [Google Scholar]
- 208. British Nutrition Foundation . Minerals and trace elements [Internet]. 2009. Available from: https://www.nutrition.org.uk/nutritionscience/nutrients-food-and-ingredients/minerals-and-trace-elements.html (accessed May 2021). [Google Scholar]
- 209. British Nutrition Foundation . Fat [Internet]. 2012. Available from: https://www.nutrition.org.uk/nutritionscience/nutrients-food-and-ingredients/fat.html (accessed May 2021). [Google Scholar]
- 210. British Dietetic Association . Manual of dietetic practice, sixth edition [Internet]. Chichester (UK): John Wiley & Sons Ltd; 2019. Available from: www.manualofdieteticpractice.com (accessed October 2021). [Google Scholar]