ABSTRACT
The purpose of this study is to examine trends in spine surgeries at ten facilities over 15 years, and to analyze relationships with the number of spine surgeons at these facilities. The subjects were patients who underwent spine surgery at the ten facilities from 2003 to 2017. Data were collected every year via a questionnaire designed to obtain clinicopathological and surgical information. There were 37,601 spine surgeries (60.2% male) recorded in the registry at 9 facilities in the Nagoya Spine Group (NSG) between 2003 and 2017, with an increase in the annual number of surgeries by 2.4 times over 15 years. On the other hand, the number of spine surgeons has increased by just under 1.5 times. Instrumentation surgeries increased from 959 in 2003 to 2,276 in 2017 (2.3 times). There was a particularly marked increase in surgeries for spinal degenerative disease from 1,075 in 2003 to 2,821 in 2017 (2.6 times). The number of surgeries performed per surgeon increased from 61.4 in 2003 to 102.8 in 2017, while the average number of spine surgeons per hospital increased from 2.6 in 2003 to 3.7 in 2017. In conclusion, with heavier burden on spine surgeons and the major changes in the spine surgery environment, training and increasing surgeons with advanced expertise and skills will become increasingly important.
Key Words: spine surgery, epidemiology, elderly, specialist, Japanese Spine Surgery and Related Research (JSSR)
INTRODUCTION
Japan is the most advanced aging society worldwide, and in line with aging, the population structure has greatly changed. The number of total households with at least one-person aged ≥65 years has markedly increased from 6.3% in 1986 to 24.2% in 2014.1 A society with over 20% of residents aged 65 or older is defined as a super-aging society.2 Japan became the first super-aging society in 2006 and its aging rate is unparalleled worldwide3 and unprecedented in absolute terms.
One characteristic of an aging society is the increased occurrence of spinal disorders. Such conditions are painful, and may result in deformity or paralysis of the trunk or extremities, with a resulting negative effect on physical activity. These changes have increased the need for spinal surgery in elderly patients to improve quality of life, and this has been facilitated by improved surgical techniques and better anesthesia.4-6 Minimally invasive surgery (MIS), use of percutaneous pedicle screws (PPS), imaging and intraoperative navigation methods have become more common. Sagittal alignment has become a focus of surgical approaches,7 and introduction of lateral lumbar interbody fusion (LLIF) to Japan in 2012 changed the approach to spinal surgery. In general, these changes have broadened the indications for surgery and widened the goals of treatment.
The NSG comprises the orthopedic departments at the Nagoya University School of Medicine and its affiliated hospitals. We established the NSG Registry to document all spine surgeries in our hospitals, and data from this system have been used as the basis for a series of epidemiological studies.8-16 To our knowledge, there have been few reports focused on spine surgeons in the context of the increasing number of spine surgeries in Japan.17,18 Therefore, the aims of this study are to review spine surgeries in the NSG over 15 years in longitudinal study to clarify the characteristics and recent trends, and to analyze the relationships between details of spine surgery and the number of spine surgeons in our facilities. An understanding of changes in spine surgery in the context of aging trends might allow for improved planning of future directions of spine surgery.
MATERIALS AND METHODS
The subjects were patients who underwent spine surgery at ten facilities in the NSG over 15 years from 1st January 2003 to 31st December 2017. A retrospective analysis was performed using data from the NSG Registry, which is a prospectively maintained database. All institutions were educational hospitals certified by the Japanese Spine Surgery and Related Research (JSSR). The details of surgery were determined by spine surgeons at each facility who were certified by the JSSR. In this study, a specialist is defined as a JSSR-board certified spine surgeon instructor, and a non-specialist as a spine surgeon who could perform the operation under a specialist.
The number of hospital beds available to the orthopedic departments remained unchanged over the study period. Every year, a questionnaire was used to capture clinicopathological and surgical information. This and a recordable optical disc for data storage were sent to the ten facilities of the NSG, and annual data were returned by the end of March of the following year. The study protocol was approved by the Committee on Ethics in Human Research at our hospital. We examined changes in the number of operations over 15 years, and in the number of surgeons and specialists. Statistical analysis was performed to evaluate changes in the characteristics of spinal surgery over the study period.
RESULTS
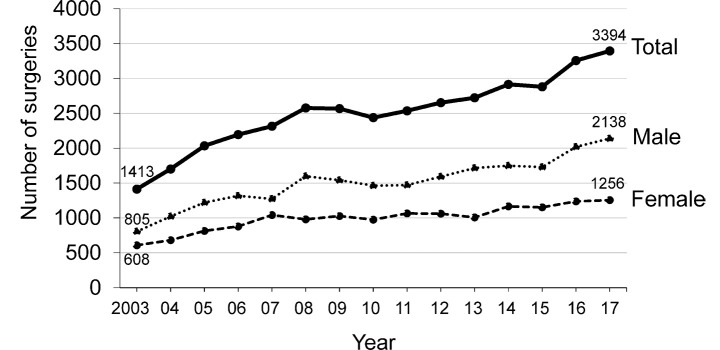
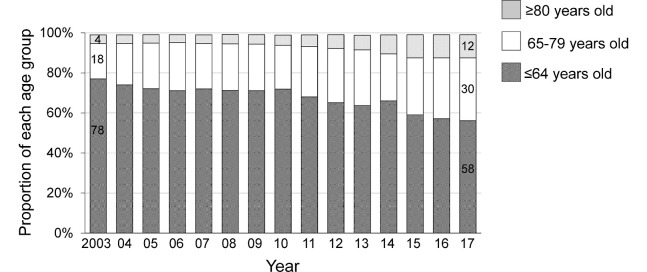
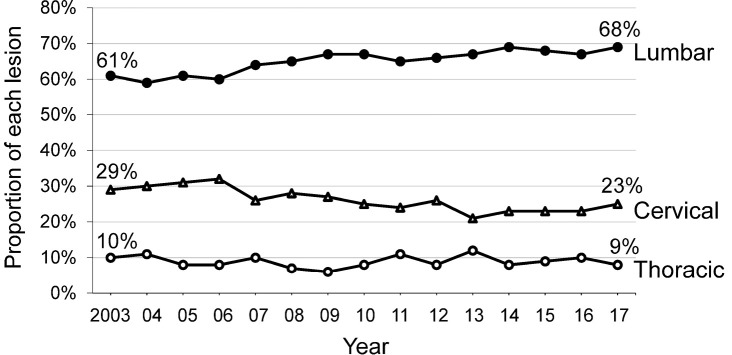
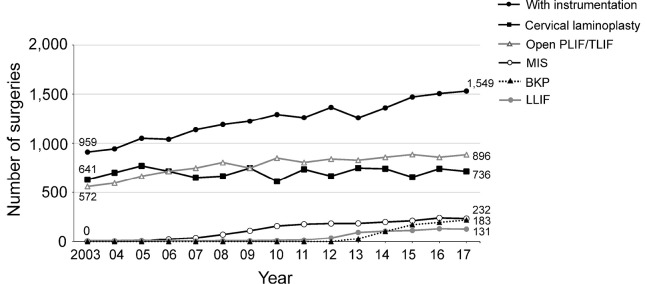
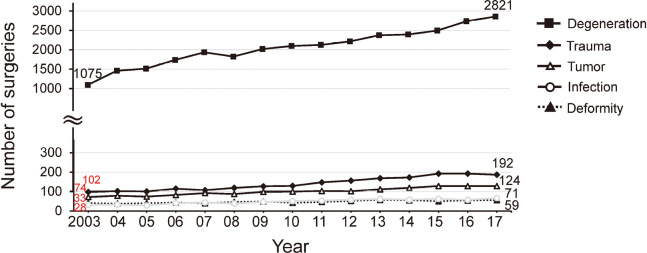
This analysis included a total of 37,601 spinal surgeries at ten facilities recorded in the NSG Registry between 2003 and 2017 (Figure 1). The patients were 39.8% female and 60.2% male. There was an increase in the annual number of spinal surgeries by 2.4 times over 15 years, and the percentage of elderly people has increased year by year (Figure 2). The proportions of surgically treated lesions did not change significantly over the study period, but lumbar surgeries gradually increased and cervical surgeries gradually decreased over time (Figure 3). Instrumentation surgeries increased from 959 in 2003 to 2,276 in 2017 (2.3 times), and the new procedures of MIS, balloon kyphoplasty (BKP), and LLIF also increased in recent years (Figure 4). Evaluation of the etiology of the treated pathology showed a particularly marked increase in surgeries for spinal degenerative disease from 1,075 in 2003 to 2,821 in 2017 (2.6 times) (Figure 5).
Fig. 1.
Annual numbers of spine surgeries
Fig. 2.
Proportions of elderly people in total spinal surgery cases
Fig. 3.
Trends in surgically treated lesions
Fig. 4.
Trends in main surgical procedures
These data include duplicates.
Fig. 5.
Trends in main etiologies
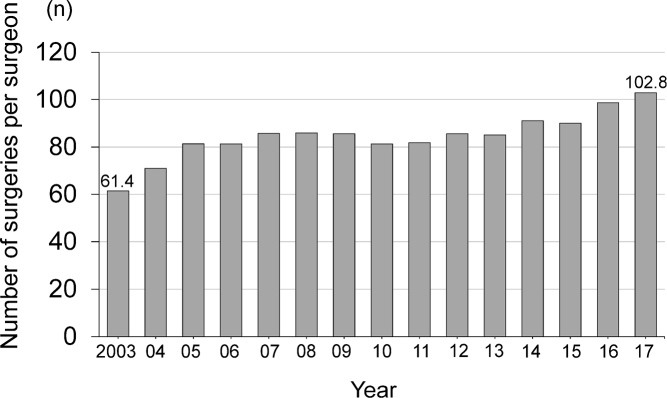
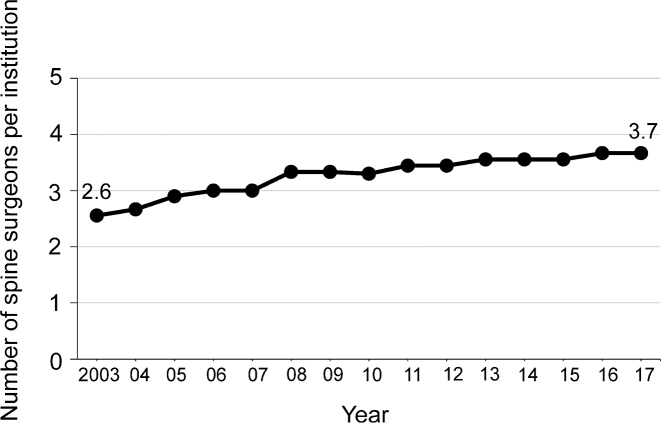
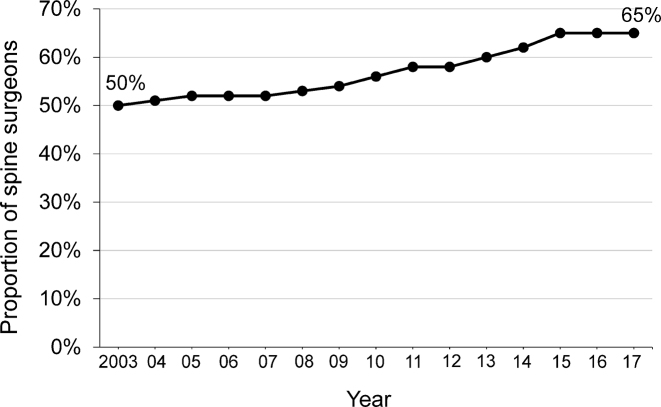
At the ten facilities in this study, the number of spine surgeries performed per surgeon increased from 61.4 in 2003 to 102.8 in 2017 (Figure 6), while the average number of spine surgeons per hospital increased from 2.6 in 2003 to 3.7 in 2017 (Figure 7). The percentage of specialists among all spine surgeons increased from 50% in 2003 to 65% in 2017 (Figure 8).
Fig. 6.
Trend in number of spine surgeries performed per surgeon
Fig. 7.
Trend in number of spine surgeons per institution
Fig. 8.
Trend of proportion of JSSR-board certified spine surgeon instructors (specialists) in ten facilities
DISCUSSION
An increase in healthy life expectancy is important in a super-aging society, and surgeries for spinal diseases can play a major role in achieving this goal. In this study, we found particular increases in instrumented cases and degenerative spinal surgery. Spinal degeneration, and lumbar degenerative disease in particular, is common in musculoskeletal disease and requires treatment with spinal column alignment.7,19 Corrective surgery using instrumentation for whole spinal alignment can now be performed in elderly patients due to improved surgical techniques and technology.
In surgery for elderly patients with comorbidities such as malnutrition and diabetes, there is a high risk of postoperative complications, and these and aging-related perioperative concerns often lengthen the hospital stay.8 Therefore, careful preoperative planning that includes evaluation of comorbidities and assessment of surgical risk, in combination with good perioperative care, are essential for good treatment prognoses. These requirements have increased burdens on spine surgeons at a time when our data show an increasing case-to-surgeon ratio. This is the first report of this trend based on spinal surgeries over a 15-year period, and the information provided is important for understanding the burden on spinal surgeons in a super-aging society.
Current spine surgery is usually performed in regional centers because of the high risk and the requirement of cooperation of other specialist physicians. Orthopedic training for a supervising doctor (specialist) requires several years of academic study. However, a specialist report must be submitted for each surgery in accordance with training guidelines, and this has increased the demand on surgeons for provision of medical care. Our data show that the number of spine surgeons has increased by 1.5 times over 15 years, and in 2017, 65% of all spine surgeons were specialists. However, the number of spine surgeries over the past 15 years had increased by more than 2.4 times.
These data indicate a discrepancy between the increase of surgeons and surgeries. Furthermore, it is almost certain that degenerative diseases will become more common and the number of required spine surgeries will increase with the current aging of the population. However, it will be difficult to handle this increased requirement for surgeries without an increase in the number of surgeons, and this situation will place a heavier burden on spine surgeons. With the growing need for medical safety in recent years, the role of training more surgeons with a high level of expertise and skills will become increasingly important. Coordination with nurses and administrators, and with postoperative rehabilitation facilities will also be required to cope with the increase in surgery. The environment surrounding spine surgery has changed markedly, including new surgical instruments and use of BKP and LLIF, as well as new surgical approaches and reduction of surgical invasion. In particular, major changes have included MIS becoming more common and the expanding indications of spine surgery. Therefore, it is increasingly important to develop specialists with these skills and advanced knowledge. Spine surgeons must strive to improve their skills in pursuit of quality medical care.
There were several limitations in this study. First, only 9 facilities are included, and the characteristics and differences between facilities were not considered. Second, although JSSR board-certified surgeons had important roles in surgeries, only the number of specialists was not a significant factor for improving the outcome of surgeries. However, the data in our registry did allow longitudinal study of spine surgeons and the trends of characteristics and changes in the number of surgeries. To meet the high demand for spine surgery, surgeons will need to perform more surgeries. This will require maintaining or increasing the number of specialists, the efficiency of surgery, and collaboration with other healthcare professionals to enhance the efficacy of spinal surgery.
In conclusion, we reviewed spine surgeries and surgeons over 15 years in longitudinal study. There were marked trends of aging of patients and an increase in the number of surgeries, especially those for degenerative diseases. It is likely that instrumentation use will continue to increase, and that new surgical procedures and approaches will emerge. This heavier burden on spine surgeons and the changing environment around spine surgery will make the role of training more surgeons with advanced expertise and skills increasingly important.
DISCLOSURE STATEMENT
Financial support was from institutional sources only. None of the authors have a conflict of interest to declare.
REFERENCES
- 1.Aizawa T, Kokubun S, Ozawa H, et al. Increasing incidence of degenerative spinal diseases in Japan during 25 years: the registration system of spinal surgery in Tohoku University Spine Society. Tohoku J Exp Med. 2016;238(2):153–163. doi: 10.1620/tjem.238.153. [DOI] [PubMed]
- 2.Statement of the United Nations 2016. https://www.un.emb-japan.go.jp/jp/statements/okamura071316.html. Accessed January 20, 2021.
- 3.Statistics Bureau, Ministry of Internal Affairs and Communications. 2–7 Population by age (1920–2013) [in Japanese]. In: Japan Statistical Yearbook. 64th ed. Tokyo, Statistics Bureau, Ministry of Internal Affairs and Communications; 2014. https://www.stat.go.jp/data/nenkan/back64/zenbun/jp64/top.html. Accessed January 20, 2021.
- 4.Kobayashi K, Imagama S, Ando K, et al. Complications associated with spine surgery in patients aged 80 years or older: Japan Association of Spine Surgeons with Ambition (JASA) multicenter study. Global Spine J. 2017;7(7):636–641. doi: 10.1177/2192568217716144. [DOI] [PMC free article] [PubMed]
- 5.Kobayashi K, Imagama S, Ando K, et al. Risk factors for delirium after spine surgery in extremely elderly patients aged 80 years or older and review of the literature: Japan Association of Spine Surgeons with Ambition (JASA) multicenter study. Global Spine J. 2017;7(6):560–566. doi: 10.1177/2192568217700115. [DOI] [PMC free article] [PubMed]
- 6.Kobayashi K, Ando K, Nishida Y, Ishiguro N, Imagama S. Epidemiological trends in spine surgery over 10 years in a multicenter database. Eur Spine J. 2018;27(8):1698–1703. doi: 10.1007/s00586-018-5513-4. [DOI] [PubMed]
- 7.Schwab F, Ungar B, Blondel B, et al. Scoliosis research society-Schwab adult spinal deformity classification. Spine (Phila Pa 1976). 2012;37(12):1077–1082. doi: 10.1097/BRS.0b013e31823e15e2. [DOI] [PubMed]
- 8.Kobayashi K, Ando K, Nakashima H, et al. Prognostic factors in the new Katagiri scoring system after palliative surgery for spinal metastasis. Spine (Phila Pa 1976). 2020;45(13):E813–E819. doi: 10.1097/BRS.0000000000003415. [DOI] [PubMed]
- 9.Kobayashi K, Ando K, Kato F, et al. Predictors of prolonged length of stay after lumbar interbody fusion: a multicenter study. Global Spine J. 2019;9(5):466–472. doi: 10.1177/2192568218800054. [DOI] [PMC free article] [PubMed]
- 10.Kobayashi K, Ando K, Kato F, et al. Trends of postoperative length of stay in spine surgery over 10 years in Japan based on a prospective multicenter database. Clin Neurol Neurosurg. 2019;177:97–100. doi: 10.1016/j.clineuro.2018.12.020. [DOI] [PubMed]
- 11.Kobayashi K, Imagama S, Sato K, et al. Postoperative complications associated with spine surgery in patients older than 90 years: a multicenter retrospective study. Global Spine J. 2018;8(8):887–891. doi: 10.1177/2192568218767430. [DOI] [PMC free article] [PubMed]
- 12.Kobayashi K, Ando K, Kato F, et al. Surgical outcomes of spinal cord and cauda equina ependymoma: Postoperative motor status and recurrence for each WHO grade in a multicenter study. J Orthop Sci. 2018;23(4):614–621. doi: 10.1016/j.jos.2018.03.004. [DOI] [PubMed]
- 13.Kobayashi K, Ando K, Kato F, et al. Reoperation within 2 years after lumbar interbody fusion: a multicenter study. Eur Spine J. 2018;27(8):1972–1980. doi: 10.1007/s00586-018-5508-1. [DOI] [PubMed]
- 14.Kobayashi K, Ando K, Kato F, et al. MRI characteristics of spinal ependymoma in WHO grade II: A review of 59 cases. Spine (Phila Pa 1976). 2018;43(9):E525–E530. doi: 10.1097/BRS.0000000000002496. [DOI] [PubMed]
- 15.Imagama S, Matsuyama Y, Sakai Y, et al. An arterial pulse examination is not sufficient for diagnosis of peripheral arterial disease in lumbar spinal canal stenosis: a prospective multicenter study. Spine (Phila Pa 1976). 2011;36(15):1204–1210. doi: 10.1097/BRS.0b013e3181ebd86f. [DOI] [PubMed]
- 16.Imagama S, Matsuyama Y, Yukawa Y, et al. C5 palsy after cervical laminoplasty: a multicentre study. J Bone Joint Surg Br. 2010;92(3):393–400. doi: 10.1302/0301-620X.92B3.22786. [DOI] [PubMed]
- 17.Takenaka S, Kashii M, Iwasaki M, Makino T, Sakai Y, Kaito T. Risk factor analysis of surgery-related complications in primary cervical spine surgery for degenerative diseases using a surgeon-maintained database. Bone Joint J. 2021;103-B(1):157–163. doi: 10.1302/0301-620X.103B1.BJJ-2020-1226.R1. [DOI] [PubMed]
- 18.Miyahara J, Ohya J, Kawamura N, Ohtomo N, Kunogi J. Adverse effects of surgeon performance after a night shift on the incidence of perioperative complications in elective thoracolumbar spine surgery. J Orthop Sci. 2021;26(6):948–952. doi: 10.1016/j.jos.2020.09.019. [DOI] [PubMed]
- 19.Liu Y, Liu Z, Zhu F, et al. Validation and reliability analysis of the new SRS-Schwab classification for adult spinal deformity. Spine (Phila Pa 1976). 2013;38(11):902–908. doi: 10.1097/BRS.0b013e318280c478. [DOI] [PubMed]