Abstract
Background
Study results vary on whether depressive symptoms are associated with worse prognosis for low back pain (LBP). We assessed the association between depressive symptoms or depression and health outcomes in persons with LBP.
Methods
We searched MEDLINE, Embase, CINAHL, and PsycINFO from inception to June 2020. Eligible studies were cohort and case-control studies assessing the association between depressive symptoms (questionnaires) or depression (diagnoses) and health outcomes in persons aged ≥16 years with LBP in the absence of major pathology. Reviewers independently screened articles, extracted data, and assessed risk of bias using the Quality in Prognosis Studies tool. We classified exploratory versus confirmatory studies based on phases of prognostic factor investigation. We conducted random-effects meta-analyses and descriptive synthesis where appropriate.
Results
Of 13,221 citations screened, we included 62 studies (63,326 participants; 61 exploratory studies, 1 confirmatory study). For acute LBP, depressive symptoms were associated with self-reported disability (descriptive synthesis: 6 studies), worse recovery (descriptive synthesis: 5 studies), and slower traffic injury–related claim closure (1 study), but not pain or work-related outcomes. Depressive symptoms were associated with greater primary healthcare utilization for acute LBP (1 confirmatory study). For chronic LBP, depressive symptoms were associated with higher pain intensity (descriptive synthesis: 9 studies; meta-analysis: 3 studies, 2902 participants, β=0.11, 95% confidence interval (CI) 0.05–0.17), disability (descriptive synthesis: 6 studies; meta-analysis: 5 studies, 3549 participants, β=0.16, 95% CI 0.04–0.29), and worse recovery (descriptive synthesis: 2 studies; meta-analysis: 2 studies, 13,263 participants, relative risk (RR)=0.91, 95% CI 0.88–0.95), but not incident chronic widespread pain (1 study).
Discussion
Depressive symptoms may be associated with self-reported disability and worse recovery in persons with acute and chronic LBP, and greater primary healthcare utilization for acute LBP. Our review provides high-quality prognostic factor information for LBP. Healthcare delivery that addresses depressive symptoms may improve disability and recovery in persons with LBP. Confirmatory studies are needed to assess the association between depressive symptoms and health outcomes in persons with LBP.
Protocol Registration
PROSPERO database (CRD42019130047)
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-07079-8.
KEY WORDS: low back pain, depressive symptoms, prognosis, systematic review, meta-analysis
BACKGROUND
Low back pain (LBP) is the leading cause of disability globally, with years lived with disability related to LBP increasing 54% from 1990 to 20151–3. The prevalence of LBP was 7.8% worldwide in 20174, and although most LBP episodes resolve, recurrences are common5. LBP is also a driver of high healthcare utilization and costs6–9.
As leading causes of disability, depressive symptoms are common comorbidities among individuals with LBP and may negatively impact outcomes10–15. Prior systematic reviews examining depressive symptoms as prognostic factors for LBP have yielded inconsistent results16–21. The estimated magnitude of associations between depressive symptoms (or depression) and outcomes varied greatly across reviews17,18,20,21, with some reviews reporting weak or no association with work-related outcomes16,19. Inconsistent results may be due to differences in methodological quality, as some reviews were limited by using scoring with cutoffs to determine study quality17,21, excluding potentially relevant studies based on study design (e.g., secondary analyses of randomized trials)18, or synthesizing results across different study designs20. Importantly, these systematic reviews require updating16–22; reviews with most recent literature searches were conducted by Alhowimel et al. (up to 2016)20 and Pinheiro et al. (up to 2014)18. Alhowimel et al. restricted to adults with chronic LBP receiving physiotherapy and excluded spinal stenosis20, whereas Pinheiro et al. focused on adults with acute/subacute LBP, excluding sciatica and spinal stenosis18. Relevant studies have been published since 201623–32, particularly on disability and healthcare utilization. To our knowledge, existing reviews have not assessed the impact of depressive symptoms on healthcare utilization for LBP.
It is critically important to identify prognostic factors for LBP to guide management, facilitate recovery, and inform future research. Prognostic research is particularly informative, as individual-based treatments for LBP tend to provide small or short-term benefits33,34. In healthcare, high-quality evidence on prognostic factors can guide healthcare providers and patients with education and patient-centered care35. At the health system level, identifying factors associated with healthcare utilization for LBP can inform healthcare planning and resource allocation tailored to priority groups.
Our objective was to conduct a systematic review to assess the association between depressive symptoms or depression and health outcomes (i.e., pain, disability, overall health status, satisfaction with care, healthcare utilization) in persons with LBP.
METHODS
Our protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO CRD42019130047)36 and was previously published37. Guidance from the Cochrane Prognosis Methods Group informed our conduct of the review35,38. Our review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and Meta-analyses Of Observational Studies in Epidemiology Checklist39,40(Appendix I).
Eligibility Criteria
Population
We included inception cohorts of individuals aged ≥16 years with LBP with or without radiculopathy (Appendix IIIa). LBP is defined as pain localized between the costal margin and inferior gluteal folds with or without leg pain in the absence of major pathology41. Radiculopathy is defined as inflammation, injury an inflammation, injury, or compression of spinal nerve roots with pain, weakness, or numbness in a myotomal or dermatomal distribution, and may be attributed to spinal stenosis or lumbar disc herniation42,43. We focused on non-specific LBP, which is LBP not attributed to recognizable and specific major pathology such as fractures, infections, ankylosing spondylitis, inflammatory process, and tumours41. Therefore, we excluded LBP due to major pathology (e.g., fractures, spinal cord injury, inflammatory arthritis, tumors, malignancies) and surgical populations.
Exposure
Depressive symptoms are self-reported characteristic attitudes and symptoms of depression, such as little interest or pleasure in doing things or feeling down, depressed, or hopeless. We included depressive symptoms measured on standardized questionnaires (e.g., Center for Epidemiologic Studies Depression Scale). We included diagnosed depression, including diagnoses using standardized codes in administrative data and self-report of diagnosed depression on standardized questionnaires, such as major depressive disorder/episode and dysthymia44. Higher severity of depressive symptoms compared to lower severity were also examined based on scoring of standardized questionnaires (e.g., severe versus mild depressive symptoms using standardized thresholds on the Beck Depression Index).
Outcomes
We targeted the following outcomes: (1) pain (e.g., pain intensity); (2) disability (e.g., activity limitations, participation restriction); (3) overall health status (e.g., health-related quality of life); (4) satisfaction with care; and (5) healthcare utilization (e.g., physician visits). These were informed by outcomes considered important for LBP research among international expert panels45–47. Based on previous literature in LBP populations, we included time-to-claim closure for traffic injury and workers’ compensation claims as common proxies for recovery48–52. Only standardized outcome measures (e.g., standardized questionnaires or administrative data) were included. We evaluated the validity and reliability of standardized questionnaires during the risk of bias assessment.
In addition to the above criteria, eligible studies were published in English to increase feasibility, and cohort studies, case-control studies, or secondary analyses of randomized trials. We excluded guidelines, letters, editorials, commentaries, books, conference proceedings, abstracts, consensus statements, case reports, case series, cross-sectional studies, qualitative studies, reviews, laboratory studies, studies not reporting methodology, and cadaveric and animal studies.
Information Sources
We searched MEDLINE, Embase, CINAHL, and PsycINFO from inception to June 25, 2020. The search strategy was developed in consultation with an experienced librarian (Appendix II) and peer-reviewed by a second librarian using the Peer Review of Electronic Search Strategies Checklist13,53. Search terms included subject headings and free-text words for the concepts of LBP, psychological factors, and depressive symptoms/depression. We used EndNote to de-duplicate references electronically. Supplemental searches were conducted using reference lists of included studies and related systematic reviews16–22.
Study Selection
We used a two-level screening process (titles/abstracts, full-text screening) to select eligible studies. We conducted training with screening a random sample of citations (50 titles/abstracts, 25 full-texts) to achieve agreement ≥80% between reviewers before starting screening. Pairs of reviewers independently screened citations to determine eligibility of studies (JJW, CYL, JAL). Reviewers met to discuss disagreements and reach consensus, and a third reviewer was involved if consensus could not be reached.
Data Collection
The data extraction form was pilot-tested on a random sample of five citations. Two reviewers independently extracted study results (effect estimates, 95% confidence interval (CI)) from included studies and discussed to reconcile differences. For all other data items, the lead author extracted data from studies. A second reviewer verified all other data extraction items by checking extracted data to minimize error. From each study, we extracted data on author, year, study design, setting and participant characteristics, duration of follow-up, definition of exposure and outcomes, and effect estimates.
Methodological Quality Appraisal
Paired reviewers independently appraised a random set of five studies as training using the Quality in Prognosis Studies (QUIPS) tool54 (Appendix XIIa). We originally indicated the Risk of Bias in Non-randomized Studies of Exposures tool in our protocol37. We decided to use the QUIPS tool as it is recommended by the Cochrane Prognosis Methods Group, is designed for prognostic factor review questions, and has adequate inter-rater reliability38,54. Trained reviewers assessed study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting (Appendix XIIb). Reviewers summarized judgments to assess overall risk of bias as low, moderate, or high for all studies. Any discrepancies between reviewers were resolved through discussion or by involving a third reviewer.
Synthesis
We assessed inter-rater agreement for screening and risk of bias assessments using percent agreement and kappa coefficients. Clinical, methodological, and statistical heterogeneities among studies were assessed. Clinical heterogeneity may result from differences in populations, exposures, comparators, or outcomes across studies. Results were stratified by LBP type (LBP versus LBP with radiculopathy), duration (acute/subacute: <3 months’ duration versus chronic: ≥3 months’ duration), exposure (depressive symptoms versus depression), and health outcome (Appendix IIIb). We stratified results for LBP without radiculopathy versus LBP with radiculopathy due to differences in the course, prognosis, and management of the conditions34,55,56. Methodological and statistical heterogeneity may result from differences in risk of bias and outcomes across studies beyond what could be expected by chance alone. We assessed methodological heterogeneity across studies as low-to-moderate versus high risk of bias based on overall judgment from the QUIPS tool. We assessed statistical heterogeneity using the I2 statistic, whereby I2>75% was deemed considerable heterogeneity as recommended in the Cochrane Handbook57.
Random-effects meta-analyses were conducted to assess associations between depressive symptoms (or depression) and health outcomes when ≥2 studies reported sufficiently similar data and were clinically homogeneous (Appendix IIIb). Effect measures included odds ratios, risk differences, risk ratios, rate differences, rate ratios, mean differences, and hazard ratios. If not reported, we computed these effect measures when applicable based on available data37. As recommended for prognostic factor systematic reviews, we conducted separate meta-analyses for different effect measures and study designs35. To explore potential impact of methodological quality on results, the following meta-analyses were conducted: (1) including all studies (low, moderate, high risk of bias studies); and (2) excluding high risk of bias studies. Summary statements in evidence syntheses were based on results from low/moderate risk of bias studies. We used random-effects meta-analyses, which assume heterogeneity of treatment effect sizes across the studies. For meta-analyses with considerable statistical heterogeneity, we conducted subgroup analyses to explore sources of heterogeneity. All meta-analyses were conducted in R v3.6.3 using the metafor package58. We descriptively synthesized results of studies that were clinically heterogeneous.
When interpreting results, we classified studies into exploratory (phase I, phase II) and confirmatory studies (phase III) based on levels of evidence for prognostic factor studies59 (Table 1). Finally, for meta-analyses involving ≥10 studies, we visually inspected funnel plots for asymmetry suggestive of publication bias60,61.
Table 1.
Levels of Evidence for Prognostic Factor Studies
| Study Phase | Description |
|---|---|
| Phase I Exploratory | Associations between potential prognostic factors and health outcomes explored in a descriptive way. Only crude (univariable) associations are reported. |
| Phase II Exploratory | Includes use of well-formulated comparison groups, stratified analyses, or multivariable analyses to identify sets of predictors. |
| Phase III Confirmatory | The goal is to test a specific hypothesis to confirm or disconfirm an independent relationship between an identified prognostic factor and a health outcome, while explicitly identifying and controlling for confounding. |
RESULTS
Study Selection
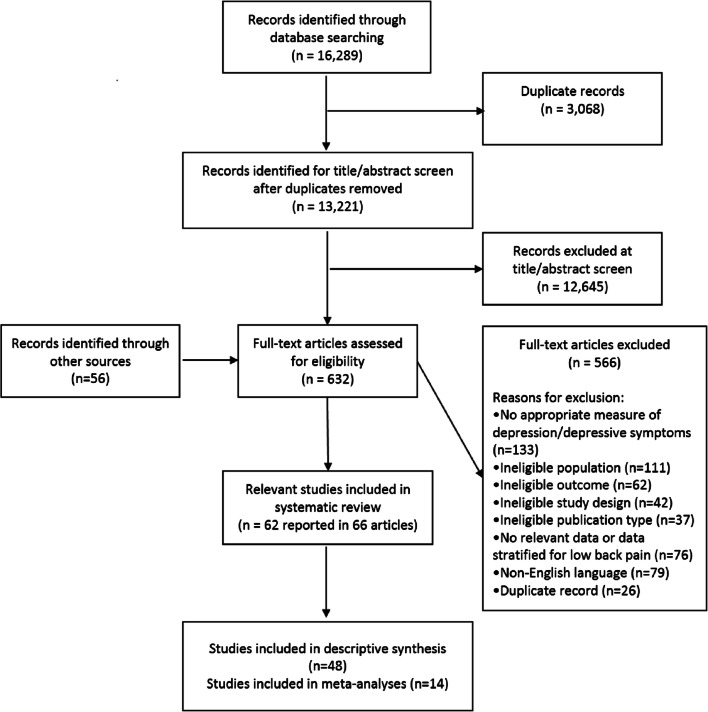
We screened 13,221 citations for inclusion (Fig. 1). We identified 62 studies reported in 66 articles (63,326 participants) as relevant, of which 14 studies (18,843 participants) were included in meta-analyses. We descriptively synthesized results of 48 studies deemed clinically heterogeneous. Inter-rater agreement for screening was kappa=0.79 (95% CI 0.76–0.81). Pilot screening achieved 82% (titles/abstracts) and 80% (full-texts) agreement based on independent results.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram showing identification and selection of included studies.
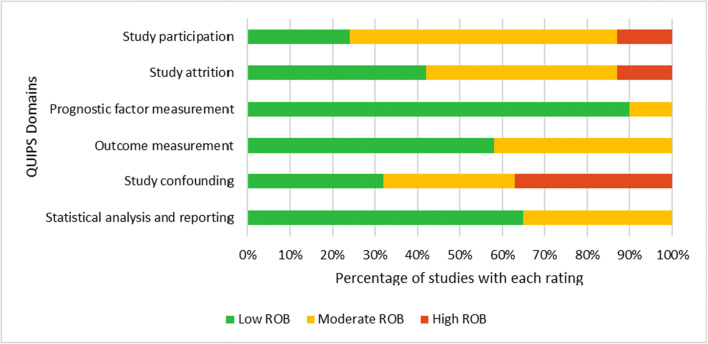
Independent critical appraisal before discussion to reach consensus had 85% agreement (312/366 items across the QUIPS tool) (Fig. 2; Appendix XIIb). After risk of bias assessment, 55 studies had low-to-moderate and 7 studies had high risk of bias. We identified 61 exploratory studies (23 phase I, 38 phase II) and one confirmatory study. We identified <10 studies per outcome in meta-analyses, which precluded us from assessing publication bias.
Fig. 2.
Risk of bias graph showing assessment of each risk of bias (ROB) domain using the Quality in Prognosis Studies (QUIPS) tool presented as percentages across all included studies (n=62).
Study Characteristics
Of the 62 included studies, 89% were cohort studies, 10% were secondary analyses of randomized trials, and one study was a combined cohort study and secondary analysis of a randomized trial (Table 2). Sample size ranged 28 to 16,567 participants with LBP, with a median of 339 (interquartile range (IQR) 161–675). The proportions of women in study populations ranged from 0% to 100% (median 51.5%, IQR 41–58%) and mean age ranged 30 to 67 years. Study populations were 34% acute LBP, 42% chronic LBP, 6% mixed duration, and 18% other (e.g., LBP with an index healthcare visit). Fifty-nine studies targeted depressive symptoms and three targeted diagnosed depression62–64.
Table 2.
Characteristics of Included Studies on the Association Between Depressive Symptoms or Depression and Health Outcomes in Individuals with Low Back Pain, Organized by Type of Low Back Pain
| Study | Study design | Region | Study period | Setting | Sample size | Type of LBP* | Mean age (years)† | Sex (% female) | Length of follow-up |
|---|---|---|---|---|---|---|---|---|---|
| Acute LBP* | |||||||||
| Lehmann, 199387 | Cohort study | USA | Not reported | Occupational | 70 | Acute | 37.2 | 33 | 6 months |
| Gatchel, 199586 | Cohort study | USA | Not reported | Health care | 421 | Acute | 35 | 38 | 12 months |
| Epping-Jordan, 199865 | Cohort study | USA | Not reported | Health care | 78 | Acute | 31.9 | 0 | 12 months |
| Fritz, 200185 | Cohort study | USA | Not reported | Occupational | 78 | Acute | 37.4 | 38 | 1 month |
| Cassidy, 200390 | Cohort study | Canada | 1994–1995 | MVC claims | 3232 | Acute | Subgroups: ranged 33.9 to 35.8 | Subgroups: ranged 57 to 65 | Up to claim closure |
| Sieben, 200581 | Cohort study | The Netherlands | 2001–2003 | Health care | 222 | Acute | ≥18 | 44 | 12 months |
| Truchon, 200584 | Cohort study | Canada | Not reported | Occupational | 321 | Acute | 39 | 44 | 6 months |
| Ritzwoller, 200664 | Cohort study | USA | 1997–1998 | Health care | 16,567 | Acute | 51.1 | 54 | 24 months |
| Patel, 200669 | Cohort study | USA | 1991–1996 | Occupational | 107 | Acute | 29.8 | 0 | 6 months |
| Henschke, 200879 | Cohort study | Australia | 2003–2005 | Health care | 973 | Acute | 43.3 | 45 | 12 months |
| Gurcay, 200978 | Cohort study | Turkey | 2007 | Health care | 91 | Acute | 37.9 | 36 | 3 months |
| Reme, 200983 | Cohort study | USA | 2000–2004 | Occupational | 496 | Acute | 37 | 42 | 3 months |
| Smeets, 200970 | Secondary analysis of RCT | Australia, New Zealand | 2001–2003 | Health care | 259 | Acute | 18–80 | Subgroups: ranged 44 to 54 | 12 months |
| Shaw, 201063 | Cohort study | USA | 1992–1994 | Health care | 140 | Acute | 30 | 0 | 6 months |
| Hiebert, 201282 | Cohort study | USA | 2009 | Occupational | 253 | Acute | 32.3 | 26 | 3 months |
| Melloh, 201368, 73–76 | Cohort study | New Zealand | 2008–2010 | Health care | 286 | Acute | Subgroups: ranged 33.5 to 36.1 | Subgroups: ranged 60 to 71 | 6 months |
| Enthoven, 201671 | Cohort study | The Netherlands | Not reported | Health care | 675 | Acute | 66.4 | 59 | 3 years |
| Steenstra, 201689 | Cohort study | Canada | 2005 | Occupational | 113 | Acute | 44 | 53 | 12 months |
| Traeger, 201691 | Cohort study | Australia | 2003–2005, 2009–2013 | Health care | 2891 | Acute | Subgroups: ranged 43.9 to 44.8 | 47 | Study 1: 3 months; Study 2: 12 months |
| Friedman, 201772 | Secondary analysis of RCT | USA | 2012–2014 | Health care | 323 | Acute | 39 | 51 | 3 months |
| Klyne, 202067 | Cohort study | Australia | Not reported | Health care | 28 | Acute | 29.5 | 46 | 6 months |
| Chronic LBP* | |||||||||
| Rainville, 1993104 | Cohort study | USA | 1991 | Health care | 72 | Chronic | 37 | 16 | Post-treatment |
| Harkapaa, 1996107 | Cohort study | Finland | Not reported | Health care | 175 | Chronic | 42.1 | 48 | 12 months |
| Dionne, 1997102 | Cohort study | USA | 1989–1990 | Health care | 1213 | Chronic | 46.7 | 52 | 24 months |
| Vendrig, 1999108 | Cohort study | The Netherlands | Not reported | Health care | 143 | Chronic | Subgroups: ranged 41.2 to 42.1 | Subgroups: ranged 29 to 41 | 6 months |
| Michaelson, 200493 | Cohort study | Sweden | 1997–1999 | Health care | 167 | Chronic | 43 | 62 | 12 months |
| Weidenhammer, 200794 | Cohort study | Switzerland | Not reported | Health care | 4032 | Chronic | 57.7 | 79 | 6 months |
| Van Der Hulst, 2008100 | Secondary analysis of RCT | The Netherlands | 1998–2000 | Health care | 163 | Chronic | Subgroups: ranged 38 to 40 | Subgroups: ranged 38 to 40 | 6 months |
| Streitberger, 201197 | Cohort study | Switzerland | 2006–2008 | Health care | 41 | Chronic | 59 | 41 | 12 months |
| Hicks, 201295 | Cohort study | Italy | 2007–2008 | Health care | 392 | Chronic | 66.8 | 84 | 12 months |
| van Hooff, 2014101 | Cohort study | The Netherlands | Not reported | Health care | 524 | Chronic | 45.4 | 58 | 12 months |
| Cougot, 2015106 | Cohort study | France | 2009 | Occupational | 217 | Chronic | 41.3 | 55 | 24 months |
| Scherrer, 2015109 | Cohort study | USA | 2008–2009 | Health care | 355 | Chronic | ≥18 | 72 | 24 months |
| Viniol, 201599 | Cohort study | Germany | Not reported | Health care | 484 | Chronic | 56.6 | 58 | 12 months |
| Yarlas, 201698 | Secondary analysis of RCT | USA | Not reported | Health care | 541 | Chronic | Subgroups: ranged 49.0 to 49.6 | Subgroups: ranged 52 to 64 | 3 months |
| Jegan, 201727 | Cohort study | Germany | Not reported | Health care | 484 | Chronic | 56.6 | 58 | 12 months |
| Nordeman, 201726 | Cohort study | Sweden | 2004–2005 | Health care | 130 | Chronic | 45 | 100 | 24 months |
| Nordstoga, 2017105 | Cohort study | Norway | 1995–1997, 2006–2008 | General population | 7523 | Chronic | Subgroups: ranged 47.9 to 51.8 | 60 | 11 years |
| Dengler, 201823 | Secondary analysis of RCT | Europe | 2013–2015 | Health care | 101 | Chronic | Subgroups: ranged 47.8 to 48.2 | Subgroups: ranged 73 to 74 | 6 months |
| Glattacker, 201828 | Cohort study | Germany | 2012–2013 | Health care | 214 | Chronic | 50.7 | 53 | 6 months |
| Demarchi, 201992 | Cohort study | Brazil | 2015–2017 | Health care | 92 | Chronic | 40.4 | 64 | 6 months |
| Halonen, 201929 | Cohort study | Sweden | 2010–2016 | Occupational | 5740 | Chronic | 54.1 | 61 | 6 years |
| Oliveira, 201930 | Cohort study | Portugal | Not reported | Health care | 284 | Chronic | 60.4 | 75 | 24 months |
| Page, 201996 | Cohort study | Canada | 2008–2011 | Health care | 686 | Chronic | 56.5 | 56 | 12 months |
| Imagama, 2020103 | Cohort study | Japan | 2014–2016 | Health care | 474 | Chronic | 73 (median) | 58 | 6 months |
| Ranger, 202031 | Cohort study | Denmark | 2013–2014 | Health care | 633 | Chronic | 44.5 | 54 | 12 months |
| Zackova, 202032 | Cohort study | Italy | 2017–2018 | Health care | 413 | Chronic | Subgroups: ranged 62.7 to 65.5 | Subgroups: ranged 54 to 59 | 6 months |
| Mixed duration* | |||||||||
| Grotle, 200666 | Cohort study | Norway | Not reported | Health care | 173 | Mixed duration | Subgroups: ranged 38.0 to 40.4 | Subgroups: ranged 54 to 62 | 12 months |
| Newell, 200780 | Cohort study | UK | 2006 | Health care | 788 | Mixed duration | Not reported | 52 | 3 months |
| Grotle, 201077 | Cohort study | UK | 2001–2002, 2004–2006 | Health care | 926 | Mixed duration | 46 | Subgroups: ranged 58 to 59 | 12 months |
| Adnan, 201725 | Cohort study | Belgium | 2007-2010 | Health care | 565 | Mixed duration | 41.5 | 58 | Post-treatment |
| Other | |||||||||
| Cherkin, 1996114 | Secondary analysis of RCT | USA | 1992–1993 | Health care | 219 | Other (index healthcare visit for LBP) | 43.1 | 47 | 12 months |
| Fransen, 200288 | Cohort study | New Zealand | 1994–1995 | Occupational | 854 | Other (new claimants) | ≥15 | 26 | 3 months |
| Tubach, 2004113 | Cohort study | France | 1991–1992 | Occupational | 622 | Other (LBP with radiculopathy ≥1 day in past year) | ≥35 | 16 | 24 months |
| Campello, 2006117 | Cohort study | USA | 1996–2000 | Occupational | 67 | Other (off/restricted duty >8 weeks) | 40 | 27 | 24 months |
| Scheele, 2013116 | Cohort study | The Netherlands | Not reported | Health care | 675 | Other (new healthcare visit for LBP) | 66.4 | 59 | 3 months |
| Fischer, 2014118 | Cohort study | Germany | Not reported | Health care | 395 | Other (work absenteeism) | 44.3 | 57 | 6 months |
| Kerr, 201562 | Secondary analysis of RCT, cohort study | USA | 2000–2004 | Health care | 392 | Other (LBP with radiculopathy of ≥6 weeks’ duration) | 43.8 | 41 | 8 years |
| Kim, 2017111 | Cohort study | USA | 2012–2014 | Health care | 161 | Other (LBP with radiculopathy with non-response to care) | 61.3 | 50 | 12 months |
| Lubelski, 2015112 | Cohort study | USA | 2010–2013 | Health care | 1346 | Chronic with radiculopathy | 66.3 | 49 | 12 months |
| Hartvigsen, 2018115 | Cohort study | Denmark | 2010–2012 | Health care | 928 | Other (index healthcare visit for LBP) | 44 | 47 | 12 months |
| Bahar-Ozmedir, 2020110 | Cohort study | Turkey | 2013–2015 | Health care | 161 | Acute with radiculopathy | 48.9 | 53 | 3 months |
LBP, low back pain; MVC, motor vehicle collision; RCT, randomized clinical trial
*Acute refers to <3 months’ duration; chronic refers to ≥3 months’ duration; studies with mixed duration report results stratified by duration
†Mean age of study sample unless otherwise specified
ACUTE LBP
Pain
Eight studies (2069 participants; 3 phase I, 5 phase II) assessed pain outcomes63,65–76; three provided similar data for meta-analysis66–68 (Table 3; Appendices V and VI). Unadjusted results suggest that depressive symptoms were associated with pain intensity68–70, but not pain trajectory (i.e., trajectory of back pain severity at different time points identified using latent class growth analysis)71. Pooled results from three phase II studies found depressive symptoms to be associated with slightly higher odds of pain (3 studies, 487 participants, odds ratio (OR)=1.15, 95% CI 0.97–1.36, I2=78.67%)66–68. When excluding one high risk of bias phase II study from the meta-analysis, we observed no association between depressive symptoms and pain67,68 (2 studies, 314 participants, OR=1.05, 95% CI 0.97–1.15, I2=35.09%). Two phase II studies found no association between depressive symptoms and pain intensity65,72. Overall, exploratory evidence suggests that depressive symptoms are not associated with pain intensity in persons with acute LBP.
Table 3.
Summary Table of Associations Between Depressive Symptoms or Depression and Health Outcomes in Persons with Low Back Pain Based on Levels of Evidence in Prognostic Factor Studies
| Population | Prognostic factor | Outcome | Association | Level of evidence |
|---|---|---|---|---|
| Acute low back pain (<3 months’ duration) | Depressive symptoms | Pain intensity | No | Exploratory (phases I and II)63,65–76 |
| Depression | Pain intensity | Yes (Phase I) | Exploratory (phase I)63 | |
| Depressive symptoms | Self-reported disability | Yes | Exploratory (phases I and II)65,66,68–70,72–77 | |
| Depressive symptoms | Worse recovery | Yes | Exploratory (phases I and II)25,78–81 | |
| Depressive symptoms | Work-related outcome | No | Exploratory (phases I and II)68,73–76,82–84 | |
| Depressive symptoms | Slower traffic injury claim closure | Yes | Exploratory (phase II)90 | |
| Depressive symptoms | Healthcare utilization (primary care visits) | Yes | Confirmatory (phase III)91 | |
| Depression | Healthcare utilization (inpatient admissions) | Inconclusive | Exploratory (phase II)64 | |
| Chronic low back pain (≥3 months’ duration) | Depressive symptoms | Pain intensity | Yes | Exploratory (phases I and II)30,77,92 |
| Depressive symptoms | Chronic widespread pain | No | Exploratory (phase II)99 | |
| Depressive symptoms | Self-reported disability | Yes | Exploratory (phases I and II)27,30,77,92,100 | |
| Depressive symptoms | Worse health-related quality of life | Inconclusive | Exploratory (phases I and II)32,94,98,100,103 | |
| Depressive symptoms | Worse recovery | Yes | Exploratory (phases I and II)25,29,104,105 | |
| Depressive symptoms | Work-related outcome | Inconclusive | Exploratory (phase I)106–108 | |
| Depressive symptoms | Healthcare utilization (opioid use) | Inconclusive | Exploratory (phase II)23,109 | |
| Low back pain with an index healthcare visit | Depressive symptoms | Pain intensity | Yes (Phase I) | Exploratory (phase I)115 |
| Depressive symptoms | Self-reported disability | Yes (Phase I) | Exploratory (phase I)115 | |
| Depressive symptoms | Worse recovery | Yes (Phase I) | Exploratory (phase I)116 | |
| Depressive symptoms | Poor tolerability of symptom severity | Yes | Exploratory (phase II)114 | |
| Lumbar radiculopathy ≥6 weeks' duration | Depression | Self-reported disability | Yes (Phase I) | Exploratory (phase I)62 |
One phase I study reported that diagnosed major depression was associated with higher pain intensity63 (OR ranged 2.42–12.71). Overall, exploratory evidence suggests that major depression is associated with higher pain intensity in persons with acute LBP, but further investigation is needed.
Self-reported Disability
Seven studies (1484 participants; 2 phase I, 5 phase II) assessed self-reported disability65,66,68–70,72–77 (Table 3; Appendix V). Five studies reported a positive association between depressive symptoms and self-reported disability based on one phase I and four phase II studies65,66,68–70,77, with β=0.20, 95% CI 0.04–0.3677. Overall, exploratory evidence suggests that depressive symptoms are associated with self-reported disability in persons with acute LBP.
Recovery
Five studies (2227 participants; 4 phase I, 1 phase II) assessed LBP recovery, which included composite measures of pain and disability25,78–81 (Table 3; Appendix V). Results from four phase I studies varied on whether depressive symptoms were associated with worse recovery25,78,80,81. Based on one phase II study, depressive symptoms were associated with slower time to recovery79 (hazard ratio (HR)=0.94, 95% CI 0.91–0.97). Overall, exploratory evidence suggests that depressive symptoms are associated with worse recovery in persons with acute LBP.
Work-related Outcomes
Nine studies (2892 participants; 7 phase I, 2 phase II) assessed work-related outcomes; four provided similar data for meta-analysis68,73–76,82–84 (Table 3; Appendices V and VII). Pooled results from four phase I studies found no association between depressive symptoms and work non-participation (4 studies, 1356 participants, OR=0.92, 95% CI 0.84–1.01, I2=93.46%)68,82–84. When excluding one high risk of bias study from the meta-analysis, pooled results remained as no association (3 studies, 1035 participants, OR=0.96, 95% CI 0.92–1.00, I2=75.70%)68,82,83. Five phase I studies reported varied results, of which two reported that depressive symptoms were associated with work status83,85, while three reported no association82,86,87. One phase II study found depressive symptoms to be associated with compensation payments based on age/sex-adjusted results88. One phase II study reported depressive symptoms as not associated with time-on-benefits during workers’ compensation claim89. The body of exploratory evidence suggests that depressive symptoms are not associated with work-related outcomes in persons with acute LBP.
Traffic Injury–related Outcomes
Exploratory evidence from one phase II study suggests that depressive symptoms are associated with slower time-to-claim closure from traffic injuries in persons with acute LBP (3232 participants; HR ranged 0.62–0.70)90 (Table 3; Appendix V).
Healthcare Utilization
Two studies (19,458 participants; 1 phase II, 1 phase III) assessed healthcare utilization64,91. One phase III study found depressive symptoms to be associated with rate of LBP-specific primary care visits over 1 year (rate ratio=1.04, 95% CI 1.02–1.07)91(Table 3; Appendix V). Overall, confirmatory evidence suggests that depressive symptoms are associated with greater LBP-specific primary care utilization in persons with acute LBP.
Diagnosis of depression was associated with all-cause inpatient admissions (OR=1.27, 95% CI 1.13–1.46), but not musculoskeletal-related inpatient admissions based on one phase II study64. Overall, exploratory evidence suggests that depression is associated with all-cause, but not musculoskeletal-related inpatient admissions in persons with acute LBP.
CHRONIC LBP
Pain
Twelve studies (8433 participants; 2 phase I, 10 phase II) assessed pain outcomes; three had similar data for meta-analysis30,77,92 (Table 3; Appendices V and VIII). Three studies reported no association between depressive symptoms and pain intensity based on unadjusted results32,93,94. Pooled results from three phase II studies found depressive symptoms to be associated with higher pain intensity (3 studies, 2902 participants, β=0.11, 95% CI 0.05–0.17, I2=1.04%)30,77,92. Of five phase II studies31,95–98, three studies found depressive symptoms to be associated with higher pain intensity31 (relative risk (RR)=1.47, 95% CI 1.13–1.94), lower odds of pain reduction95 (OR=0.47, 95% CI 0.25–0.89), and shorter duration of pain reduction97 (HR=2.97, 95% CI 1.32–6.65). Overall, exploratory evidence suggests that depressive symptoms are associated with higher pain intensity in persons with chronic LBP.
One phase II study found no association between depressive symptoms and the incidence of chronic widespread pain99 (OR=1.01, 95% CI not reported, p>0.05). Overall, exploratory evidence suggests that depressive symptoms are not associated with incident chronic widespread pain in persons with chronic LBP.
Self-reported Disability
Ten studies (4732 participants; 2 phase I, 8 phase II) assessed self-reported disability; five had similar data for meta-analysis27,30,77,92,100 (Table 3; Appendices V and IX). Three studies reported unadjusted results26,98,101, of which two found depressive symptoms to be associated with self-reported disability26,101. Pooled results from five phase II studies found depressive symptoms to be associated with self-reported disability (5 studies, 3549 participants, β=0.16, 95% CI 0.04–0.29, I2=74.69%)27,30,77,92,100. We observed similar results when excluding one phase II study with high risk of bias (4 studies, 3065 participants, β=0.15, 95% CI 0.02–0.27, I2=78.70%)30,77,92,100. Three phase II studies found depressive symptoms to be associated with self-reported disability (RR=1.34, 95% CI 1.04–1.72) and family/social disability (β=1.94, 95% CI 1.27–2.60)30,31,102. Overall, exploratory evidence suggests that depressive symptoms are associated with self-reported disability in persons with chronic LBP.
Health-related Quality of Life (HRQOL)
Six studies (5837 participants; 1 phase I, 5 phase II) assessed HRQOL32,94,98,100,103; two provided similar data for meta-analysis100,103 (Table 3; Appendices V and X). Pooled results from two phase II studies found no association between depressive symptoms and mental HRQOL (2 studies, 637 participants, β=1.09, 95% CI −1.83 to 4.02, I2=96.22%). One phase II study found no association between depressive symptoms and mental HRQOL94. In contrast, one phase II study found depressive symptoms to be associated with lower odds of improvement in mental HRQOL32. Results varied for overall or physical HRQOL based on one phase I (reported no association)28 and four phase II studies (three studies reported an association32,98,100, one study reported no association94). Overall, the evidence is inconclusive on the association between depressive symptoms and HRQOL in persons with chronic LBP due to inconsistent results across studies.
Recovery
Four studies (13,747 participants; 1 phase I, 3 phase II) assessed LBP recovery, including combined measures of pain and disability25,29,104,105; two provided similar data for meta-analysis29,105 (Table 3; Appendices V and XI). Pooled results from two phase II studies found depressive symptoms to be associated with worse recovery29,105 (2 studies, 13,263 participants, RR=0.91, 95% CI 0.88–0.95, I2=0%). Similarly, depressive symptoms were associated with worse recovery based on results from one phase I and one phase II study25,104. Overall, exploratory evidence suggests that depressive symptoms are associated with worse recovery in persons with chronic LBP.
Work-related Outcomes
Three phase I studies (535 participants) assessed work-related outcomes106–108 (Table 3; Appendix V). Depressive symptoms were not associated with work status based on three phase I studies106–108. Overall, exploratory evidence suggests that depressive symptoms are not associated with work status in persons with chronic LBP, but further investigation is needed.
Healthcare Utilization
Two phase II studies (456 participants) assessed opioid use23,109 (Table 3; Appendix V). One phase II study found no association between depressive symptoms and continued opioid use23, while one phase II study reported higher odds of having high-dose (>50 mg/day) opioid use109 (OR=1.65, 95% CI 0.97–2.81). Overall, the evidence is inconclusive on the association between depressive symptoms and opioid use in persons with chronic LBP due to inconsistent results across studies when comparing continued versus high-dose opioid use.
Lumbar Radiculopathy
Five studies (2682 participants; 2 phase I, 3 phase II) targeted individuals with lumbar radiculopathy62,110–113 (Table 3; Appendix V). One phase I study found that diagnosed depression was associated with disability for lumbar radiculopathy ≥6 weeks’ duration62. One phase I and three phase II studies targeted various durations of lumbar radiculopathy but were moderate-to-high risk of bias110–113.
LBP with Index Healthcare Visit
Three studies (1822 participants; 2 phase I, 1 phase II) assessed outcomes in persons with an index healthcare visit for LBP114–116 (Table 3; Appendix V). Depressive symptoms were associated with poor tolerability of symptom severity reported by the patient based on one phase II study114 (OR=2.3, 95% CI 1.4–3.6), and higher pain intensity, disability, and worse recovery based on two phase I studies115,116 (OR ranged 1.1–2.3). Overall, exploratory evidence suggests that depressive symptoms are associated with self-reported poor tolerability of symptom severity in individuals with an index healthcare visit for LBP. Other outcomes of pain, disability, and recovery need further investigation.
Other LBP Populations
Two studies (462 participants; 1 phase I, 1 phase II) reported on different populations with LBP in occupational settings117,118 (Table 3; Appendix V). One phase I study reported no association between depressive symptoms and work retention in individuals with off/restricted duty >8 weeks117. In individuals on sick leave for LBP, depressive symptoms were associated with reduced HRQOL, but not return-to-work or pain based on one phase II study118. Overall, evidence is limited on the association between depressive symptoms and work-related outcomes in these LBP populations.
DISCUSSION
Exploratory evidence suggests that depressive symptoms are associated with self-reported disability, worse recovery, and slower traffic injury–related claim closure, but not pain or work-related outcomes in persons with acute LBP. Depressive symptoms are associated with greater healthcare utilization in persons with acute LBP based on one confirmatory study. In persons with chronic LBP, exploratory evidence suggests that depressive symptoms are associated with higher pain intensity, disability, and worse recovery, but not incident chronic widespread pain.
Our systematic review provides more comprehensive prognostic factor evidence for depressive symptoms than previous reviews16–21. Alhowimel et al. reported an association between depression and disability, and that depression was predictive of poor quality of life and failure to return to work for chronic LBP based on two studies20. This review was limited by synthesizing results from one cross-sectional and one cohort study, and a narrow scope that restricted to patients with chronic LBP treated by physiotherapists20. In contrast, our systematic review found that depressive symptoms were associated with self-reported disability but not work-related outcomes, and inconclusive evidence for HRQOL due to inconsistent results across studies. Pinheiro et al. reported that depressive symptoms were associated with worse outcomes for acute LBP, including disability and non-recovery18. Pinheiro et al. may have missed studies by excluding secondary analyses of randomized trials18. We identified seven studies as secondary analyses of randomized trials, of which five were phase II targeting pain, disability, recovery, HRQOL, symptom tolerability, and healthcare utilization. Similar to the findings of Pinheiro et al.18, we found that depressive symptoms were associated with disability and worse recovery for acute LBP. Our review extends these findings by synthesizing new information on healthcare utilization for acute LBP and prognosis for chronic LBP.
Our findings have implications for clinical management, healthcare delivery, and research for LBP. Understanding the potential impact of depressive symptoms on disability and recovery can guide expectations and management of LBP among patients and healthcare providers. Healthcare providers may assess for depressive symptoms early to identify patients potentially at risk of disability and worse recovery and guide patient-centered care. From a health system perspective, health programs considering depressive symptoms may improve outcomes for LBP. Further investigation of new interventions may be warranted to help manage comorbid depressive symptoms in patients with LBP. Confirmatory studies are needed to assess the association between depressive symptoms and health outcomes with adequate control for confounding. In addition, studies are needed to assess the role of diagnosed depression as a prognostic factor for LBP, as we identified only three studies. For acute LBP, we found that depressive symptoms were not associated with pain intensity based on phase I and II studies. In contrast, diagnosed depression may be associated with higher pain intensity based on one phase I study. It is unclear whether findings differ due to differences in the exposure (e.g., diagnosed depression may present with greater severity compared to self-reported depressive symptoms) or the need for phase II and III studies to account for important covariates in the analysis.
Strengths and Limitations
Our systematic review provides comprehensive prognostic evidence for depressive symptoms and, to our knowledge, is the first to assess outcomes of healthcare utilization for LBP. Our review was planned a priori with a published protocol37 based on guidance of the Cochrane Prognosis Methods Group35,38. We followed guidelines on the conduct and reporting of prognostic factor systematic reviews, including the PRISMA statement, QUIPS tool, and phases of prognostic factor investigation38,39,59. Finally, we used meta-analyses and descriptive syntheses to synthesize evidence using carefully outlined criteria to assess for heterogeneity.
Our review has limitations. First, only English studies were included to increase feasibility. However, a previous study found no evidence of systematic bias when using language restrictions in systematic reviews with meta-analyses in conventional medicine119. We identified only six possibly relevant non-English articles (1256 participants; Appendix XIII). Second, studies for one outcome (HRQOL for chronic LBP) had considerable heterogeneity, which we could not adequately explore due to a limited number of studies. However, we used descriptive syntheses and meta-analyses to synthesize evidence when appropriate. Third, we could not conduct planned analyses to assess publication bias due to insufficient data. Research is needed to investigate potential publication bias and explore approaches such as protocol registration and reporting checklists for prognostic factor studies120.
CONCLUSION
Depressive symptoms serve as prognostic factors for consideration in healthcare delivery and resource planning that may improve disability and recovery in persons with LBP. Our systematic review provides high-quality prognostic factor information to guide management among patients and healthcare providers for LBP. Confirmatory studies are needed to assess the association between depressive symptoms and health outcomes in persons with LBP.
Supplementary Information
(PDF 1330 kb)
Acknowledgements
We would like to thank Beata Pach, BA, MA, MISt (Information Specialist) for developing the literature search strategy and Jane Beehler, MLIS (Librarian) for peer-reviewing the search strategy.
Author Contribution
Conceptualization: Jessica J. Wong, Laura C. Rosella, Andrea C. Tricco, Pierre Côté
Methodology: Jessica J. Wong, Laura C. Rosella, Andrea C. Tricco, Pierre Côté
Data collection: Jessica J. Wong, Catherine Y. Liang, Jeremy A. Lewis, Zachary Bouck
Statistical analysis: Jessica J. Wong
Supervision: Laura C. Rosella, Andrea C. Tricco, Pierre Côté
Writing – original draft: Jessica J. Wong
Writing – review and editing: Laura C. Rosella, Andrea C. Tricco, Pierre Côté, Catherine Y. Liang, Jeremy A. Lewis, Zachary Bouck, Jessica J. Wong
Funding
Funding for this project was supported by the Canada Research Chair held by Dr. Laura Rosella. Dr. Jessica Wong is funded by a Canadian Institutes of Health Research (CIHR) Frederick Banting and Charles Best Canada Graduate Scholarships Doctoral Award and the tuition assistance program at the Canadian Memorial Chiropractic College. Dr. Laura Rosella is funded by a Tier 2 Canada Research Chair in Population Health Analytics. Dr. Pierre Côté is funded by a Tier 2 Canada Research Chair in Disability Prevention and Rehabilitation. Dr. Andrea Tricco is funded by a Tier 2 Canada Research Chair in Knowledge Synthesis. Zachary Bouck is supported by a CIHR Frederick Banting and Charles Best Canada Graduate Scholarships Doctoral Award.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of Interest
Dr. Tricco reports grants from Tier 2 Canada Research Chair in Knowledge Synthesis, outside the submitted work. Dr. Côté reports research grants from the Canadian Chiropractic Research Foundation and the College of Chiropractors of British Columbia to Ontario Tech University, outside the submitted work. For the remaining authors, no conflicts of interest were declared.
Disclaimer
The funders had no role in the design and conduct of the research; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Presentations: This research has been presented as a poster presentation at the Canadian Society for Epidemiology and Biostatistics (CSEB) 2021 Conference on June 1–3, 2021.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cassidy JD, Carroll LJ, Côté P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). 1998;23(17);1860-6; discussion 7. [DOI] [PubMed]
- 2.Cassidy JD, Côté P, Carroll LJ, Kristman V. Incidence and course of low back pain episodes in the general population. Spine (Phila Pa 1976). 2005;30(24);2817-23. [DOI] [PubMed]
- 3.Hincapie CA, Cassidy JD, Côté P, Carroll LJ, Guzman J. Whiplash injury is more than neck pain: a population-based study of pain localization after traffic injury. J Occup Environ Med. 2010;52(4);434-40. [DOI] [PubMed]
- 4.Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, Blyth FM, Smith E, Buchbinder R, Hoy D. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8(6);299. [DOI] [PMC free article] [PubMed]
- 5.Hayden JA, Dunn KM, van der Windt DA, Shaw WS. What is the prognosis of back pain? Best Pract Res Clin Rheumatol. 2010;24(2);167-79. [DOI] [PubMed]
- 6.Global Burden of Disease 2015 Disease and Injury Incidence and Prevalence Collaborators, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053);1545-602. [DOI] [PMC free article] [PubMed]
- 7.Global Burden of Disease 2015 Disease and Injury Incidence and Prevalence Collaborators, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995);743-800. [DOI] [PMC free article] [PubMed]
- 8.Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, Murray C, Burstein R, Buchbinder R. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6);968-74. [DOI] [PubMed]
- 9.Wong JJ, Côté P, Tricco AC, Watson T, Rosella LC. The effect of back problems on health care utilization and costs in Ontario, Canada: a population-based matched cohort study. PAIN. 9000;Articles in Press [DOI] [PubMed]
- 10.Green BN, Johnson CD, Haldeman S, Griffith E, Clay MB, Kane EJ, Castellote JM, Rajasekaran S, Smuck M, Hurwitz EL, Randhawa K, Yu H, Nordin M. A scoping review of biopsychosocial risk factors and co-morbidities for common spinal disorders. PLoS One. 2018;13(6);e0197987. [DOI] [PMC free article] [PubMed]
- 11.Patten SB, Williams JV, Wang J. Mental disorders in a population sample with musculoskeletal disorders. BMC Musculoskelet Disord. 2006;737. [DOI] [PMC free article] [PubMed]
- 12.Ha JY, Kim ES, Kim HJ, Park SJ. Factors associated with depressive symptoms in patients with chronic low back pain. Ann Rehabil Med. 2011;35(5);710-8. [DOI] [PMC free article] [PubMed]
- 13.McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;7540-6. [DOI] [PubMed]
- 14.Bener A, Dafeeah EE, Salem MO. Determinants of depression and somatisation symptoms in low back pain patients and its treatment: global burden of diseases. J Pak Med Assoc. 2015;65(5);473-9. [PubMed]
- 15.Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159);1789-858. [DOI] [PMC free article] [PubMed]
- 16.Iles RA, Davidson M, Taylor NF. Psychosocial predictors of failure to return to work in non-chronic non-specific low back pain: a systematic review. Occup Environ Med. 2008;65(8);507-17. [DOI] [PubMed]
- 17.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976). 2002;27(5);E109-20. [DOI] [PubMed]
- 18.Pinheiro MB, Ferreira ML, Refshauge K, Maher CG, Ordonana JR, Andrade TB, Tsathas A, Ferreira PH. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J. 2016;16(1);105-16. [DOI] [PubMed]
- 19.Steenstra IA, Munhall C, Irvin E, Oranye N, Passmore S, Van Eerd D, Mahood Q, Hogg-Johnson S. Systematic review of prognostic factors for return to work in workers with subacute and chronic low back pain. J Occup Rehabil. 2017;27(3);369-81. [DOI] [PMC free article] [PubMed]
- 20.Alhowimel A, AlOtaibi M, Radford K, Coulson N. Psychosocial factors associated with change in pain and disability outcomes in chronic low back pain patients treated by physiotherapist: a systematic review. SAGE Open Med. 2018;62050312118757387. [DOI] [PMC free article] [PubMed]
- 21.Ramond A, Bouton C, Richard I, Roquelaure Y, Baufreton C, Legrand E, Huez JF. Psychosocial risk factors for chronic low back pain in primary care--a systematic review. Fam Pract. 2011;28(1);12-21. [DOI] [PubMed]
- 22.McKillop AB, Carroll LJ, Battie MC. Depression as a prognostic factor of lumbar spinal stenosis: a systematic review. Spine J. 2014;14(5);837-46. [DOI] [PubMed]
- 23.Dengler J, Sturesson B, Kools D, Prestamburgo D, Cher D, van Eeckhoven E, Erk E, Gasbarrini A, Pflugmacher R, Vajkoczy P. Risk factors for continued opioid use in conservative versus surgical management of low back pain originating from the sacroiliac joint. Global Spine J. 2018;8(5);453-9. [DOI] [PMC free article] [PubMed]
- 24.Oliveira DS, Velia Ferreira Mendonca L, Sofia Monteiro Sampaio R, Manuel Pereira Dias de Castro-Lopes J, Ribeiro de Azevedo LF. The impact of anxiety and depression on the outcomes of chronic low back pain multidisciplinary pain management-a multicenter prospective cohort study in pain clinics with one-year follow-up. Pain Med. 2019;20(4);736-46. [DOI] [PubMed]
- 25.Adnan R, Van Oosterwijck J, Cagnie B, Dhondt E, Schouppe S, Van Akeleyen J, Logghe T, Danneels L. Determining predictive outcome factors for a multimodal treatment program in low back pain patients: a retrospective cohort study. J Manipulative Physiol Ther. 2017;40(9);659-67. [DOI] [PubMed]
- 26.Nordeman L, Thorselius L, Gunnarsson R, Mannerkorpi K. Predictors for future activity limitation in women with chronic low back pain consulting primary care: a 2-year prospective longitudinal cohort study. BMJ Open. 2017;7(6);e013974. [DOI] [PMC free article] [PubMed]
- 27.Jegan NR, Brugger M, Viniol A, Strauch K, Barth J, Baum E, Leonhardt C, Becker A. Psychological risk and protective factors for disability in chronic low back pain - a longitudinal analysis in primary care. BMC Musculoskelet Disord. 2017;18(1);114. [DOI] [PMC free article] [PubMed]
- 28.Glattacker M, Heyduck K, Jakob T. Yellow flags as predictors of rehabilitation outcome in chronic low back pain. Rehabil Psychol. 2018;63(3);408-17. [DOI] [PubMed]
- 29.Halonen JI, Shiri R, Magnusson Hanson LL, Lallukka T. Risk and prognostic factors of low back pain: repeated population-based cohort study in Sweden. Spine (Phila Pa 1976). 2019;44(17);1248-55. [DOI] [PubMed]
- 30.Oliveira DS, Vélia Ferreira Mendonça L, Sofia Monteiro Sampaio R, Manuel Pereira Dias de Castro-Lopes J, Ribeiro de Azevedo LF. The impact of anxiety and depression on the outcomes of chronic low back pain multidisciplinary pain management-a multicenter prospective cohort study in pain clinics with one-year follow-up. Pain Med. 2019;20(4);736-46. [DOI] [PubMed]
- 31.Ranger TA, Cicuttini FM, Jensen TS, Manniche C, Heritier S, Urquhart DM. Catastrophization, fear of movement, anxiety, and depression are associated with persistent, severe low back pain and disability. Spine J. 2020;20(6);857-65. [DOI] [PubMed]
- 32.Zackova M, Aspide R, Braghittoni A, Zenesini C, Palandri G. Yellow flag on prognostic factors for non-specific chronic low back pain patients subjected to mini-invasive treatment: a cohort study. Eur Spine J. 2020;29(8);1879-86. [DOI] [PubMed]
- 33.Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J. 2010;10(6);514-29. [DOI] [PubMed]
- 34.Wong JJ, Côté P, Sutton DA, Randhawa K, Yu H, Varatharajan S, Goldgrub R, Nordin M, Gross DP, Shearer HM, Carroll LJ, Stern PJ, Ameis A, Southerst D, Mior S, Stupar M, Varatharajan T, Taylor-Vaisey A. Clinical practice guidelines for the noninvasive management of low back pain: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain. 2017;21(2);201-16. [DOI] [PubMed]
- 35.Riley RD, Moons KGM, Snell KIE, Ensor J, Hooft L, Altman DG, Hayden J, Collins GS, Debray TPA. A guide to systematic review and meta-analysis of prognostic factor studies. Bmj. 2019;364k4597. [DOI] [PubMed]
- 36.PROSPERO International prospective register of systematic reviews. National Institute for Health Research. Available at: https://www.crd.york.ac.uk/prospero/ (Aug 1, 2018).
- 37.Wong JJ, Tricco AC, Côté P, Rosella LC. The association between depressive symptoms or depression and health outcomes in adults with low back pain with or without radiculopathy: protocol of a systematic review. Syst Rev. 2019;8(1);267. [DOI] [PMC free article] [PubMed]
- 38.Cochrane Prognosis Methods Group. Resources: tools. 2021. Available at: https://methods.cochrane.org/prognosis/tools (accessed Mar 1, 2021).
- 39.Page MJ, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, mulrow cindy d, et al. The PRISMA 2020 Statement: an Updated Guideline for Reporting Systematic Reviews 2020. doi:10.31222/osf.io/v7gm2. [DOI] [PMC free article] [PubMed]
- 40.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15);2008-12. [DOI] [PubMed]
- 41.Duthey B. World Health Organization Background Paper 6.24. Low Back Pain, 2013. Available at http://www.who.int/medicines/areas/priority_medicines/BP6_24LBP.pdf (accessed Aug 1, 2018).
- 42.North American Spine Society. NASS Clinical Guidelines: Lumbar Disc Herniation with Radiculopathy. Available at: https://www.spine.org/Documents/ResearchClinicalCare/Guidelines/LumbarDiscHerniation.pdf (accessed Dec 12, 2018).
- 43.American Academy of Orthopaedic Surgeon. OrthoInfo: Lumbar Spinal Stenosis. Available at: https://orthoinfo.aaos.org/en/diseases%2D%2Dconditions/lumbar-spinal-stenosis (accessed Jan 22, 2019).
- 44.World Health Organization. Depression and other common mental health disorders. Available at: http://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf (accessed Oct 1, 2018).
- 45.Chiarotto A, Boers M, Deyo RA, Buchbinder R, Corbin TP, Costa LOP, Foster NE, Grotle M, Koes BW, Kovacs FM, Lin CC, Maher CG, Pearson AM, Peul WC, Schoene ML, Turk DC, van Tulder MW, Terwee CB, Ostelo RW. Core outcome measurement instruments for clinical trials in nonspecific low back pain. Pain. 2018;159(3);481-95. [DOI] [PMC free article] [PubMed]
- 46.Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine (Phila Pa 1976). 2000;25(24);3100-3. [DOI] [PubMed]
- 47.Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976). 1998;23(18);2003-13. [DOI] [PubMed]
- 48.Gross DP, Battié MC. Work-related recovery expectations and the prognosis of chronic low back pain within a workers’ compensation setting. J Occup Environ Med. 2005;47(4);428-33. [DOI] [PubMed]
- 49.Abenhaim L, Suissa S. Importance and economic burden of occupational back pain: a study of 2,500 cases representative of Quebec. J Occup Med. 1987;29(8);670-4. [PubMed]
- 50.Côté P, Hogg-Johnson S, Cassidy JD, Carroll L, Frank JW. The association between neck pain intensity, physical functioning, depressive symptomatology and time-to-claim-closure after whiplash. J Clin Epidemiol. 2001;54(3);275-86. [DOI] [PubMed]
- 51.Sinclair SJ, Hogg-Johnson SH, Mondloch MV, Shields SA. The effectiveness of an early active intervention program for workers with soft-tissue injuries. The Early Claimant Cohort Study. Spine (Phila Pa 1976). 1997;22(24);2919-31. [DOI] [PubMed]
- 52.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine (Phila Pa 1976). 1995;20(8 Suppl);1s-73s. [PubMed]
- 53.Sampson M, McGowan J, Cogo E, Grimshaw J, Moher D, Lefebvre C. An evidence-based practice guideline for the peer review of electronic search strategies. J Clin Epidemiol. 2009;62(9);944-52. [DOI] [PubMed]
- 54.Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4);280-6. [DOI] [PubMed]
- 55.Côté P, Shearer H, Ameis A, Carroll L, Mior S, Nordin M and the OPTIMa Collaboration. Enabling recovery from common traffic injuries: a focus on the injured person. UOIT-CMCC Centre for the Study of Disability Prevention and Rehabilitation. January 31, 2015. Available at: https://www.fsco.gov.on.ca/en/auto/documents/2015-cti.pdf (accessed June 25, 2021).
- 56.Konstantinou K, Hider SL, Jordan JL, Lewis M, Dunn KM, Hay EM. The impact of low back-related leg pain on outcomes as compared with low back pain alone: a systematic review of the literature. Clin J Pain. 2013;29(7);644-54. [DOI] [PubMed]
- 57.Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook (accessed Mar 1, 2021).
- 58.Viechtbauer W. Conducting meta-analyses in R with the metafor package. 2010;36(3):48.
- 59.Côté P, Cassidy JD, Carroll L, Frank JW, Bombardier C. A systematic review of the prognosis of acute whiplash and a new conceptual framework to synthesize the literature. Spine (Phila Pa 1976). 2001;26(19);E445-58. [DOI] [PubMed]
- 60.Higgins J, Green SE. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011. Available from www.handbook.cochrane.org.
- 61.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kerr D, Zhao W, Lurie JD. What are long-term predictors of outcomes for lumbar disc herniation? A randomized and observational study. Clin Orthop Relat Res. 2015;473(6);1920-30. [DOI] [PMC free article] [PubMed]
- 63.Shaw WS, Means-Christensen AJ, Slater MA, Webster JS, Patterson TL, Grant I, Garfin SR, Wahlgren DR, Patel S, Atkinson JH. Psychiatric disorders and risk of transition to chronicity in men with first onset low back pain. Pain Med. 2010;11(9);1391-400. [DOI] [PubMed]
- 64.Ritzwoller DP, Crounse L, Shetterly S, Rublee D. The association of comorbidities, utilization and costs for patients identified with low back pain. BMC Musculoskelet Disord. 2006;772. [DOI] [PMC free article] [PubMed]
- 65.Epping-Jordan JE, Wahlgren DR, Williams RA, Pruitt SD, Slater MA, Patterson TL, Grant I, Webster JS, Atkinson JH. Transition to chronic pain in men with low back pain: predictive relationships among pain intensity, disability, and depressive symptoms. Health Psychol. 1998;17(5);421-7. [DOI] [PubMed]
- 66.Grotle M, Vøllestad NK, Brox JI. Screening for yellow flags in first-time acute low back pain: reliability and validity of a Norwegian version of the Acute Low Back Pain Screening Questionnaire. Clin J Pain. 2006;22(5);458-67. [DOI] [PubMed]
- 67.Klyne DM, Hodges PW. Circulating adipokines in predicting the transition from acute to persistent low back pain. Pain Med. 2020; [DOI] [PubMed]
- 68.Melloh M, Elfering A, Käser A, Salathé CR, Barz T, Aghayev E, Röder C, Theis JC. Depression impacts the course of recovery in patients with acute low-back pain. Behav Med. 2013;39(3);80-9. [DOI] [PubMed]
- 69.Patel SM. Psychosocial predictors of pain chronicity in Navy servicemen: Alliant International University, San Diego; 2006.
- 70.Smeets RJ, Maher CG, Nicholas MK, Refshauge KM, Herbert RD. Do psychological characteristics predict response to exercise and advice for subacute low back pain? Arthritis Rheum. 2009;61(9);1202-9. [DOI] [PubMed]
- 71.Enthoven WT, Koes BW, Bierma-Zeinstra SM, Bueving HJ, Bohnen AM, Peul WC, van Tulder MW, Berger MY, Luijsterburg PA. Defining trajectories in older adults with back pain presenting in general practice. Age Ageing. 2016;45(6);878-83. [DOI] [PubMed]
- 72.Friedman BW, Gensler S, Yoon A, Nerenberg R, Holden L, Bijur PE, Gallagher EJ. Predicting three-month functional outcomes after an ED visit for acute low back pain. Am J Emerg Med. 2017;35(2);299-305. [DOI] [PubMed]
- 73.Elfering A, Käser A, Melloh M. Relationship between depressive symptoms and acute low back pain at first medical consultation, three and six weeks of primary care. Psychol Health Med. 2014;19(2);235-46. [DOI] [PubMed]
- 74.Melloh M, Elfering A, Chapple CM, Käser A, Rolli Salathé C, Barz T, Röder C, Theis JC. Prognostic occupational factors for persistent low back pain in primary care. Int Arch Occup Environ Health. 2013;86(3);261-9. [DOI] [PubMed]
- 75.Melloh M, Elfering A, Salathé CR, Käser A, Barz T, Röder C, Theis JC. Predictors of sickness absence in patients with a new episode of low back pain in primary care. Ind Health. 2012;50(4);288-98. [DOI] [PubMed]
- 76.Melloh M, Elfering A, Stanton TR, Käser A, Salathé CR, Barz T, Röder C, Theis JC. Who is likely to develop persistent low back pain? A longitudinal analysis of prognostic occupational factors. Work. 2013;46(3);297-311. [DOI] [PubMed]
- 77.Grotle M, Foster NE, Dunn KM, Croft P. Are prognostic indicators for poor outcome different for acute and chronic low back pain consulters in primary care? Pain. 2010;151(3);790-7. [DOI] [PMC free article] [PubMed]
- 78.Gurcay E, Bal A, Eksioglu E, Hasturk AE, Gurcay AG, Cakci A. Acute low back pain: clinical course and prognostic factors. Disabil Rehabil. 2009;31(10);840-5. [DOI] [PubMed]
- 79.Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, York J, Das A, McAuley JH. Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. Bmj. 2008;337(7662);a171. [DOI] [PMC free article] [PubMed]
- 80.Newell D, Field J. Who will get better? Predicting clinical outcomes in a chiropractic practice. Clinical Chiropractic. 2007;10(4);179-86.
- 81.Sieben JM, Vlaeyen JW, Portegijs PJ, Verbunt JA, van Riet-Rutgers S, Kester AD, Von Korff M, Arntz A, Knottnerus JA. A longitudinal study on the predictive validity of the fear-avoidance model in low back pain. Pain. 2005;117(1-2);162-70. [DOI] [PubMed]
- 82.Hiebert R, Campello MA, Weiser S, Ziemke GW, Fox BA, Nordin M. Predictors of short-term work-related disability among active duty US Navy personnel: a cohort study in patients with acute and subacute low back pain. Spine J. 2012;12(9);806-16. [DOI] [PubMed]
- 83.Reme SE, Hagen EM, Eriksen HR. Expectations, perceptions, and physiotherapy predict prolonged sick leave in subacute low back pain. BMC Musculoskelet Disord. 2009;10139. [DOI] [PMC free article] [PubMed]
- 84.Truchon M, Côté D. Predictive validity of the Chronic Pain Coping Inventory in subacute low back pain. Pain. 2005;116(3);205-12. [DOI] [PubMed]
- 85.Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82(10);973-83. [PubMed]
- 86.Gatchel RJ, Polatin PB, Mayer TG. The dominant role of psychosocial risk factors in the development of chronic low back pain disability. Spine (Phila Pa 1976). 1995;20(24);2702-9. [DOI] [PubMed]
- 87.Lehmann TR, Spratt KF, Lehmann KK. Predicting long-term disability in low back injured workers presenting to a spine consultant. Spine (Phila Pa 1976). 1993;18(8);1103-12. [DOI] [PubMed]
- 88.Fransen M, Woodward M, Norton R, Coggan C, Dawe M, Sheridan N. Risk factors associated with the transition from acute to chronic occupational back pain. Spine (Phila Pa 1976). 2002;27(1);92-8. [DOI] [PubMed]
- 89.Steenstra IA, Franche RL, Furlan AD, Amick B, 3rd, Hogg-Johnson S. The added value of collecting information on pain experience when predicting time on benefits for injured workers with back pain. J Occup Rehabil. 2016;26(2);117-24. [DOI] [PubMed]
- 90.Cassidy JD, Carroll L, Côté P, Berglund A, Nygren A. Low back pain after traffic collisions: a population-based cohort study. Spine (Phila Pa 1976). 2003;28(10);1002-9. [DOI] [PubMed]
- 91.Traeger AC, Hübscher M, Henschke N, Williams CM, Maher CG, Moseley GL, Lee H, McAuley JH. Emotional distress drives health services overuse in patients with acute low back pain: a longitudinal observational study. Eur Spine J. 2016;25(9);2767-73. [DOI] [PubMed]
- 92.Demarchi SJ, Oliveira CB, Franco MR, Morelhão PK, Hisamatsu TM, Silva FG, Damato TM, Pinto RZ. Association of perceived physical overload at work with pain and disability in patients with chronic non-specific low back pain: a 6-month longitudinal study. Eur Spine J. 2019;28(7);1586-93. [DOI] [PubMed]
- 93.Michaelson P, Sjölander P, Johansson H. Factors predicting pain reduction in chronic back and neck pain after multimodal treatment. Clin J Pain. 2004;20(6);447-54. [DOI] [PubMed]
- 94.Weidenhammer W, Linde K, Streng A, Hoppe A, Melchart D. Acupuncture for chronic low back pain in routine care: a multicenter observational study. Clin J Pain. 2007;23(2);128-35. [DOI] [PubMed]
- 95.Hicks GE, Benvenuti F, Fiaschi V, Lombardi B, Segenni L, Stuart M, Pretzer-Aboff I, Gianfranco G, Macchi C. Adherence to a community-based exercise program is a strong predictor of improved back pain status in older adults: an observational study. Clin J Pain. 2012;28(3);195-203. [DOI] [PMC free article] [PubMed]
- 96.Pagé MG, Boyd K, Ware MA. Examination of the course of low back pain intensity based on baseline predictors and health care utilization among patients treated in multidisciplinary pain clinics: a Quebec Pain Registry study. Pain Med. 2019;20(3);564-73. [DOI] [PubMed]
- 97.Streitberger K, Müller T, Eichenberger U, Trelle S, Curatolo M. Factors determining the success of radiofrequency denervation in lumbar facet joint pain: a prospective study. Eur Spine J. 2011;20(12);2160-5. [DOI] [PMC free article] [PubMed]
- 98.Yarlas A, Miller K, Wen W, Lynch SY, Munera C, Dain B, Pergolizzi JV, Jr., Raffa R, Ripa SR. A subgroup analysis found no diminished response to buprenorphine transdermal system treatment for chronic low back pain patients classified with depression. Pain Pract. 2016;16(4);473-85. [DOI] [PubMed]
- 99.Viniol A, Jegan N, Brugger M, Leonhardt C, Barth J, Baum E, Becker A, Strauch K. Even worse - risk factors and protective factors for transition from chronic localized low back pain to chronic widespread pain in general practice: a cohort study. Spine (Phila Pa 1976). 2015;40(15);E890-9. [DOI] [PubMed]
- 100.van der Hulst M, Vollenbroek-Hutten MM, Groothuis-Oudshoorn KG, Hermens HJ. Multidisciplinary rehabilitation treatment of patients with chronic low back pain: a prognostic model for its outcome. Clin J Pain. 2008;24(5);421-30. [DOI] [PubMed]
- 101.van Hooff ML, Spruit M, O’Dowd JK, van Lankveld W, Fairbank JC, van Limbeek J. Predictive factors for successful clinical outcome 1 year after an intensive combined physical and psychological programme for chronic low back pain. Eur Spine J. 2014;23(1);102-12. [DOI] [PMC free article] [PubMed]
- 102.Dionne CE, Koepsell TD, Von Korff M, Deyo RA, Barlow WE, Checkoway H. Predicting long-term functional limitations among back pain patients in primary care settings. J Clin Epidemiol. 1997;50(1);31-43. [DOI] [PubMed]
- 103.Imagama S, Murakami H, Kaito T, Matsuyama Y, Yamashita T, Kawakami M, Takahashi K, Yoshida M, Ohtori S, Taguchi T, Haro H, Taneichi H, Yamazaki M, Inoue G, Nishida K, Yamada H, Kabata D, Shintani A, Iwasaki M, Ito M, Miyakoshi N, Yonenobu K, Takura T, Mochida J. Impact of background factors on outcomes of pharmacological therapy for chronic low back pain: a nationwide multicenter prospective study. J Orthop Sci. 2020; [DOI] [PubMed]
- 104.Rainville J, Ahern DK, Phalen L. Altering beliefs about pain and impairment in a functionally oriented treatment program for chronic low back pain. Clin J Pain. 1993;9(3);196-201. [DOI] [PubMed]
- 105.Nordstoga AL, Nilsen TIL, Vasseljen O, Unsgaard-Tøndel M, Mork PJ. The influence of multisite pain and psychological comorbidity on prognosis of chronic low back pain: longitudinal data from the Norwegian HUNT Study. BMJ Open. 2017;7(5);e015312. [DOI] [PMC free article] [PubMed]
- 106.Cougot B, Petit A, Paget C, Roedlich C, Fleury-Bahi G, Fouquet M, Menu P, Dubois C, Geraut C, Roquelaure Y, Tripodi D. Chronic low back pain among French healthcare workers and prognostic factors of return to work (RTW): a non-randomized controlled trial. J Occup Med Toxicol. 2015;1040. [DOI] [PMC free article] [PubMed]
- 107.Harkapaa KJ, A; Estlander, A. Health optimism and control beliefs as predictors for treatment outcome of a multimodal back treatment program. Psychology and Health. 1996;12123-34.
- 108.Vendrig AA. Prognostic factors and treatment-related changes associated with return to work in the multimodal treatment of chronic back pain. J Behav Med. 1999;22(3);217-32. [DOI] [PubMed]
- 109.Scherrer JF, Salas J, Lustman PJ, Burge S, Schneider FD. Change in opioid dose and change in depression in a longitudinal primary care patient cohort. Pain. 2015;156(2);348-55. [DOI] [PMC free article] [PubMed]
- 110.Bahar-Ozdemir Y, Sencan S, Ercalik T, Kokar S, Gunduz OH. The effect of pre-treatment depression, anxiety and somatization levels on transforaminal epidural steroid injection: a prospective observational study. Pain Physician. 2020;23(3);E273-e80. [PubMed]
- 111.Kim EJ, Chotai S, Stonko DP, Wick JB, Schneider BJ, McGirt MJ, Devin CJ. Patient-reported outcomes after lumbar epidural steroid injection for degenerative spine disease in depressed versus non-depressed patients. Spine J. 2017;17(4);511-7. [DOI] [PubMed]
- 112.Lubelski D, Thompson NR, Agrawal B, Abdullah KG, Alvin MD, Khalaf T, Mazanec DJ, Benzel EC, Mroz TE, Krishnaney AA. Prediction of quality of life improvements in patients with lumbar stenosis following use of membrane stabilizing agents. Clin Neurol Neurosurg. 2015;139234-40. [DOI] [PubMed]
- 113.Tubach F, Beauté J, Leclerc A. Natural history and prognostic indicators of sciatica. J Clin Epidemiol. 2004;57(2);174-9. [DOI] [PubMed]
- 114.Cherkin DC, Deyo RA, Street JH, Barlow W. Predicting poor outcomes for back pain seen in primary care using patients’ own criteria. Spine (Phila Pa 1976). 1996;21(24);2900-7. [DOI] [PubMed]
- 115.Hartvigsen L, Kongsted A, Vach W, Salmi LR, Hestbaek L. Baseline characteristics may help indicate the best choice of health care provider for back pain patients in primary care: results from a prospective cohort study. J Manipulative Physiol Ther. 2020;43(1);13-23. [DOI] [PubMed]
- 116.Scheele J, Enthoven WT, Bierma-Zeinstra SM, Peul WC, van Tulder MW, Bohnen AM, Berger MY, Koes BW, Luijsterburg PA. Course and prognosis of older back pain patients in general practice: a prospective cohort study. Pain. 2013;154(6);951-7. [DOI] [PubMed]
- 117.Campello MA, Weiser SR, Nordin M, Hiebert R. Work retention and nonspecific low back pain. Spine (Phila Pa 1976). 2006;31(16);1850-7. [DOI] [PubMed]
- 118.Fischer CA, Neubauer E, Adams HS, Schiltenwolf M, Wang H. Effects of multidisciplinary pain treatment can be predicted without elaborate questionnaires. Int Orthop. 2014;38(3);617-26. [DOI] [PMC free article] [PubMed]
- 119.Morrison A, Polisena J, Husereau D, Moulton K, Clark M, Fiander M, Mierzwinski-Urban M, Clifford T, Hutton B, Rabb D. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care. 2012;28(2);138-44. [DOI] [PubMed]
- 120.Peat G, Riley RD, Croft P, Morley KI, Kyzas PA, Moons KG, Perel P, Steyerberg EW, Schroter S, Altman DG, Hemingway H. Improving the transparency of prognosis research: the role of reporting, data sharing, registration, and protocols. PLoS Med. 2014;11(7);e1001671. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1330 kb)
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.