Abstract
Rationale & Objective
Having a usual source of care increases use of preventive services and is associated with improved survival in the general population. We evaluated this association in adults with chronic kidney disease (CKD).
Study Design
Prospective, observational cohort study.
Setting & Participants
Adults with CKD enrolled in the Chronic Renal Insufficiency Cohort (CRIC) Study.
Predictor
Usual source of care was self-reported as: 1) clinic, 2) emergency department (ED)/urgent care, 3) other.
Outcomes
Primary outcomes included incident end-stage kidney disease (ESKD), atherosclerotic events (myocardial infarction, stroke, or peripheral artery disease), incident heart failure, hospitalization events, and all-cause death.
Analytical Approach
Multivariable regression analyses to evaluate the association between usual source of care (ED/urgent care vs clinic) and primary outcomes.
Results
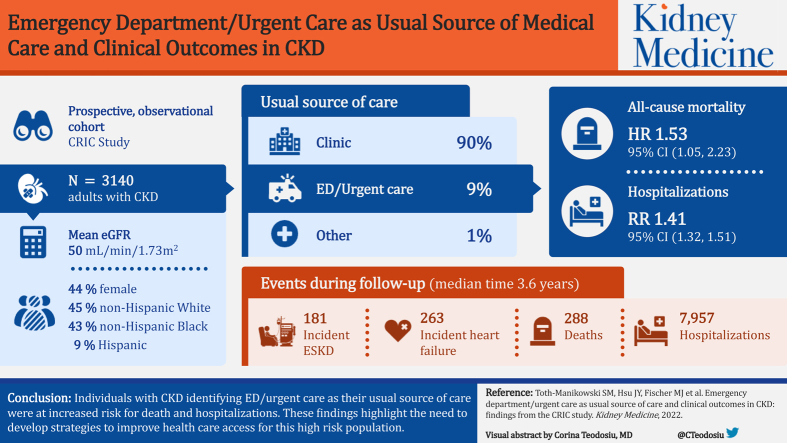
Among 3,140 participants, mean age was 65 years, 44% female, 45% non-Hispanic White, 43% non-Hispanic Black, and 9% Hispanic, mean estimated glomerular filtration rate 50 mL/min/1.73 m2. Approximately 90% identified clinic as usual source of care, 9% ED/urgent care, and 1% other. ED/urgent care reflected a more vulnerable population given lower baseline socioeconomic status, higher comorbid condition burden, and poorer blood pressure and glycemic control. Over a median follow-up time of 3.6 years, there were 181 incident end-stage kidney disease events, 264 atherosclerotic events, 263 incident heart failure events, 288 deaths, and 7,957 hospitalizations. Compared to clinic as usual source of care, ED/urgent care was associated with higher risk for all-cause death (HR, 1.53; 95% CI, 1.05-2.23) and hospitalizations (RR, 1.41; 95% CI, 1.32-1.51).
Limitations
Cannot be generalized to all patients with CKD. Causal relationships cannot be established.
Conclusions
In this large, diverse cohort of adults with moderate-to-severe CKD, those identifying ED/urgent care as usual source of care were at increased risk for death and hospitalizations. These findings highlight the need to develop strategies to improve health care access for this high-risk population.
Index Words: Access to health care, chronic kidney disease, emergency department, health care access, usual source of care
Graphical abstract
Plain-Language Summary.
Patients with chronic kidney disease (CKD) are medically complex and may benefit from having coordinated care, most easily provided in a clinic setting. We sought to evaluate how certain outcomes differed among patients with CKD based on where they usually seek medical care. We used data from the Chronic Renal Insufficiency Cohort Study and found that individuals who usually went to an emergency department or urgent care were more likely to be hospitalized or die compared to those who primarily received care in a clinic. Our work identifies patients with CKD who use the emergency department or urgent care as high risk, and highlights the importance of understanding barriers to accessing clinic-based care in order to improve health care in this group.
Editorial, p ●
Having a usual source of care implies having an ongoing relationship with a primary care provider or facility that enables patient-centered care in a coordinated and accessible manner.1,2 It is an important marker of health care access and has been associated with increased use of preventive services and decreased use of emergency department (ED) services, hospitalizations, and mortality.3, 4, 5, 6, 7, 8, 9, 10, 11 In the general US population, approximately 15% of adults do not have a usual source of care; however, this estimate is not known in populations with chronic kidney disease (CKD).12
Effective management of patients with CKD is vital to reducing the risk of adverse consequences of kidney disease progression and associated morbidity from cardiovascular disease. For this reason, having a usual source of care is important in this high-risk population. This is supported by data published in other chronic conditions including diabetes, chronic obstructive pulmonary disease, and cancer, which have demonstrated a positive association between continuity of care and improved outcomes, decreased cost, and fewer ED visits and hospitalizations.13, 14, 15, 16, 17 In a study of Korean patients with diabetic nephropathy, superior quality continuity of care was associated with a decreased likelihood of progressing to end-stage kidney disease (ESKD) when compared to poorer quality continuity of care.18 However, we are unaware of other studies that have evaluated the impact of usual source of care on adverse outcomes in a US CKD cohort. The objective of this study was to examine this association in US adults with mild-to-moderate CKD. We hypothesized that individuals using an ED or urgent care center would be at higher risk for adverse outcomes over the study period as compared to those using a clinic for care.
Methods
Study Population
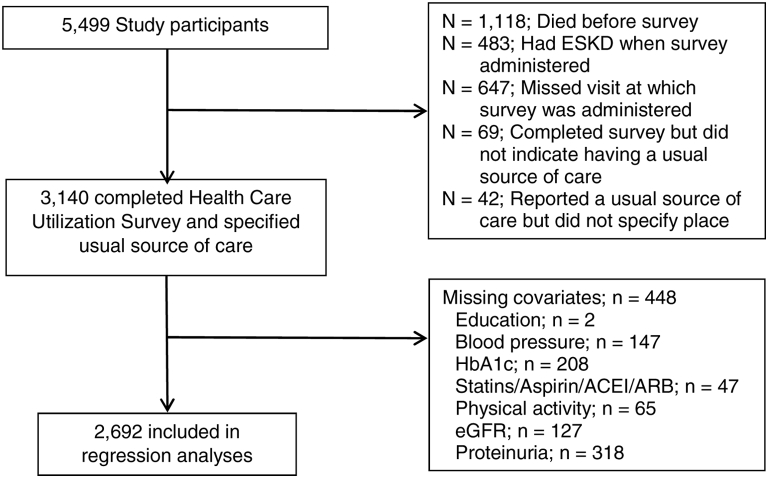
The Chronic Renal Insufficiency Cohort (CRIC) Study is an ongoing multicenter, observational study of diverse adults with CKD. The rationale, design, methodology, and baseline characteristics of study participants have been previously described.19, 20, 21 Recruitment of 3,939 adults with CKD occurred between 2003-2008 at 7 US clinical centers in Chicago, Illinois; Ann Arbor, Michigan; Philadelphia, Pennsylvania; Baltimore, Maryland; New Orleans, Louisiana; Cleveland, Ohio; and Oakland, California. Inclusion criteria were age (21-74 years) and estimated glomerular filtration rate ([eGFR] 20-70 mL/min/1.73 m2) at enrollment. Between 2013-2015, the study recruited an additional 1,560 adults; participants were slightly older (45-79 years) and had milder CKD (eGFR 45-70 mL/min/1.73 m2 and proteinuria).22 Detailed exclusion criteria have been previously described.19 For the current study, 3,140 participants met inclusion criteria (Fig 1). The study protocol was approved by the Institutional Review Board of all participating centers and is in accordance with the Declaration of Helsinki. All participants provided informed consent.
Figure 1.
Analytic cohort flow chart. Abbreviations: ACEi/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; eGFR, estimated glomerular filtration rate; ESKD, end-stage kidney disease; HbA1c, hemoglobin A1c.
Measurements and Variable Definition
Sociodemographic, lifestyle, and medical history information was obtained at baseline using self-reported questionnaires (eg, sex, age, race/ethnicity [non-Hispanic White, non-Hispanic Black, Hispanic, or other], education, marital status, health insurance, receipt of nephrology care, physical activity, smoking). Usual source of care was derived from the Health Care Utilization questionnaire which was adapted from the 2012 National Health Interview Survey Adult Access to Health Care and Utilization, and administered between 2013-2015.23 Participants were asked, “Is there a place that you usually go to when you are sick or need advice about your health?” Responses included: “1) Yes, there is one place; 2) Yes, there is more than one place; 3) No, there is no place; 4) Don’t know.” Participants were subsequently asked: “What kind of place is it—a clinic, doctor’s office, emergency department, or some other place?” Participants who responded “more than one place” were asked to indicate which place they frequented most often. Responses included: “1) Clinic or health center; 2) Doctor’s office or health maintenance organization (HMO); 3) Hospital emergency department or urgent care center; 4) Some other place; 5) Don’t go to one place most often; 6) Don’t know.” Participants choosing “clinic or health center” or “doctor’s office or HMO” were categorized as receiving their usual source of care in a clinic. Participants choosing “Hospital ED or urgent care center” were categorized as receiving their usual source of care in an ED/urgent care. Few participants responded with options other than clinic or ED/urgent care (options 4-6, n = 42; 1.3%) and therefore were excluded from the analysis.
Participants underwent annual study visits during which they were asked about medication use and underwent standardized anthropometric and blood pressure measurements.24 Fasting blood samples were collected to measure serum creatinine, electrolytes, lipids, and plasma glucose. Serum creatinine, cystatin C, urinary total protein, and creatinine were measured using standard assays.25, 26, 27 Glomerular filtration rate (GFR) was estimated using an equation developed in a subgroup of CRIC participants with measured iothalamate GFR, which has been demonstrated to have superior accuracy in this cohort compared to other eGFR equations.27 Diabetes mellitus was defined by a fasting glucose ≥126 mg/dL or use of insulin or oral hypoglycemic medications. Hypertension was defined by a systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of antihypertensive medications.
Outcomes
Outcomes included incident ESKD (defined as receipt of maintenance dialysis therapy or kidney transplant), atherosclerotic events (myocardial infarction, stroke, or peripheral artery disease), incident heart failure, hospitalization events, and all-cause death. Outcomes were acquired by study personnel who reviewed hospital billing codes and queried participants every 6 months by telephone or during annual visits about recent hospitalizations, outpatient tests, or interventions. Two independent reviewers adjudicated these events using standardized criteria when reviewing hospital records.19 Criteria for heart failure events were adapted from the Framingham Heart Study and included a combination of clinical symptoms, radiographic evidence of pulmonary congestion, physical examination of the heart and lungs, and when available, central venous hemodynamic monitoring data and echocardiographic imaging.28,29 Hospitalizations events were recorded as counts using the Agency for Healthcare Research and Quality Clinical Classifications Software categorization scheme as per the International Classification of Diseases, Ninth Revision code.30 Any hospitalizations falling within a “disease of the circulatory system” category were designated as cardiovascular; all others were deemed noncardiovascular.31 Ascertainment of ESKD was supplemented by cross-linkage with the US Renal Data System. Deaths were ascertained from reports by next of kin, death certificates, hospital records, and linkage with the Social Security Death Master File. Participants were followed until the occurrence of death, withdrawal from the study, or January 2018, when the database was locked for analysis.
Statistical Analysis
Descriptive statistics for demographic and clinical characteristics were summarized as means (standard deviations) or medians (interquartile ranges) for continuous variables and as frequencies (proportions) for categorical variables. T tests or Wilcoxon rank sum tests were used to compare continuous variables, and χ2 tests were used to compare categorical variables. Event rates for time-to-event outcomes were calculated as the ratio of the number of participants with the event divided by the total person-years of follow-up. Cox proportional hazards modeling was used to evaluate the association between usual source of care and incident ESKD, atherosclerotic events, incident heart failure, and all-cause death, and cardiovascular death. Model assumptions were checked, including the proportionality assumption of Cox models. Poisson regression was used to evaluate the association between usual source of care and the total number of hospitalization events over the follow-up period. We assessed for overdispersion and calculated negative binomial regression models as a sensitivity analysis.
Models were stratified by clinical center and adjusted as follows: Model 1: unadjusted; Model 2: clinical center, enrollment phase, age, sex, race/ethnicity, education, income; Model 3: 2+ hemoglobin A1c, statin, aspirin, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker use, smoking status, physical activity, blood pressure <140/90 mm Hg, eGFR, and log urine protein-creatinine ratio. These covariates, which were ascertained at the time of the baseline visit, were chosen using the Andersen-Aday conceptual framework, as well as evidence from published literature.32, 33, 34 We examined eGFR as a potential effect modifier for each outcome. All regression models used a complete data analysis approach. The number of missing variables is shown in Table S1. All hypothesis tests were 2-sided with a type 1 error rate of 5%. All analyses were performed using SAS 9.3 (SAS Institute).
Results
Baseline Characteristics
Of the 3,140 eligible participants, 2,862 (91%) identified a clinic as usual source of care and 278 (9%) identified an ED/urgent care as usual source of care (Table 1). At study entry, mean age was 65 years, 44% were female, 45% were non-Hispanic White, 43% were non-Hispanic Black, and 9% were Hispanic. Baseline mean eGFR was 50 mL/min/1.73 m2 and median urinary protein excretion was 0.2 g/24 hours. Compared to those identifying a clinic as usual source of care, participants identifying ED/urgent care as usual source of care were more likely to be a racial/ethnic minority, have less than a high school education, earn less than $20,000 annually, be permanently disabled, and have a higher baseline urine protein. These individuals were also less likely to be full-time employed and currently married. Although a large proportion of the cohort had health insurance (97%), those identifying an ED/urgent care as usual source of care were less likely to have private/commercial health insurance and to have seen a nephrologist in the past. Compared to those identifying a clinic as usual source of care, those identifying ED/urgent care as usual source of care were more likely to be active smokers and less likely to have blood pressure <140/90 mm Hg, hemoglobin A1c <7%, and to be taking an angiotensin-converting enzyme inhibitor/angiotensin receptor blocker. Of the 3,140 participants, 286 were excluded from the regression analyses due to missing data (see Fig 1, Table S1). Compared to participants excluded from the regression analyses, those included in the regression analyses (n = 2,854) were similar in terms of age, sex, and other demographic and clinical characteristics (Table S2).
Table 1.
Baseline Characteristics by Usual Source of Care
| Characteristic | Overall (N = 3,140) | Clinic (n = 2,862) | Emergency Department/Urgent Care (n =278) |
|---|---|---|---|
| Age, y, mean (SD) | 65 (9) | 65 (9) | 65 (9) |
| Female sex | 1,380 (44%) | 1,270 (44%) | 110 (40%) |
| Race/ethnicity | — | — | — |
| Non-Hispanic White | 1,421 (45%) | 1,365 (48%) | 56 (20%)a |
| Non-Hispanic Black | 1,344 (43%) | 1,145 (40%) | 199 (72%) |
| Hispanic | 273 (9%) | 261 (9%) | 12 (4%) |
| Other | 102 (3%) | 91 (3%) | 11 (4%) |
| Less than high school education | 457 (15%) | 394 (14%) | 63 (23%)a |
| Annual income <$20,000 | 784 (25%) | 672 (24%) | 112 (41%)a |
| Health insurance | 2,953 (97%) | 2,696 (97%) | 257 (97%) |
| Health insurance type | — | — | — |
| Private/commercial | 616 (20%) | 595 (21%) | 21 (8%)a |
| Any Medicare | 1,269 (42%) | 1,163 (42%) | 106 (40%) |
| Medicaid/public aid | 407 (13%) | 337 (12%) | 70 (26%) |
| Veterans Affairs/Military/CHAMPUS | 188 (6%) | 155 (6%) | 33 (12%) |
| None | 104 (3%) | 95 (3%) | 9 (3%) |
| Unknown | 473 (16%) | 446 (16%) | 27 (10%) |
| Unable to fill a prescription due to cost | 561 (18%) | 501 (18%) | 60 (22%) |
| Unable to see a doctor due to cost | 266 (9%) | 236 (8%) | 30 (12%) |
| Ever seen a nephrologist (yes) | 2,204 (70%) | 2,030 (71%) | 174 (63%)a |
| Marital status | — | — | — |
| Currently married | 1,705 (54%) | 1,590 (56%) | 115 (41%)a |
| Never married | 425 (14%) | 378 (13%) | 47 (17%) |
| Formerly married | 1,010 (32%) | 894 (31%) | 116 (42%) |
| Employment status | — | — | — |
| Full-time employed | 851 (27%) | 818 (29%) | 33 (12%)a |
| Part-time employed | 321 (10%) | 297 (10%) | 24 (9%) |
| Permanently disabled | 515 (16%) | 416 (15%) | 99 (36%) |
| Retired | 1,155 (37%) | 1,068 (37%) | 87 (31%) |
| Unemployed | 166 (5%) | 144 (5%) | 22 (8%) |
| Hypertension | 2,838 (91%) | 2,572 (90%) | 266 (96%)a |
| Diabetes | 1,671 (53%) | 1,512 (53%) | 159 (57%) |
| Cardiovascular disease | 1,167 (37%) | 1,030 (36%) | 137 (49%)a |
| Current smoker | 284 (9%) | 236 (8%) | 48 (17%)a |
| ACEi/ARB | 2,026 (66%) | 1,860 (66%) | 166 (61%) |
| Ideal physical activityb | 1,552 (51%) | 1,434 (51%) | 118 (43%)a |
| Blood pressure <140/90, mm Hg | 2,287 (76%) | 2,103 (77%) | 184 (70.5%)a |
| BMI, kg/m2, mean (SD) | 32.29 (7.4) | 32 (7) | 32 (8) |
| Hemoglobin A1c <7% | 2,114 (72%) | 1,952 (73%) | 162 (63%)a |
| eGFR, mL/min per 1.73 m2, mean (SD) | 49.87 (17) | 50 (17) | 48 (17) |
| CKD Stage (per mL/min/1.73 m2) | — | — | — |
| Stage 2 (eGFR ≥60) | 833 (28%) | 766 (28%) | 67 (26%)a |
| Stage 3a (eGFR 45-59) | 1,003 (33%) | 925 (34%) | 78 (30%) |
| Stage 3b (eGFR 30-44) | 781 (26%) | 700 (25%) | 81 (31%) |
| Stage 4 (eGFR <30) | 396 (13%) | 361 (13%) | 35 (13%) |
| Urine protein, g/24 h, median (IQR) | 0.2 (0.08-0.70) | 0.1 (0.1-0.4) | 0.2 (0.1-0.8)a |
Note: Data presented as n (%) unless otherwise noted.
Abbreviations: ACEi/ARB, Angiotensin-converting enzyme inhibitor/angiotensin II receptor blocker; CHAMPUS, Civilian Health and Medical Program of the Uniformed Services; eGFR, estimated glomerular filtration rate; IQR, interquartile range; SD, standard deviation.
P < 0.05
≥150 minutes/week vigorous activity ≥75 minutes/week, or moderate plus vigorous activity ≥150 minutes/week.45
Incident ESKD
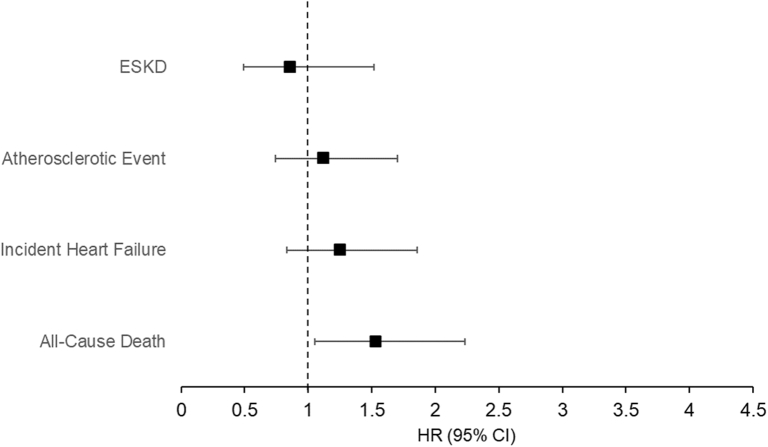
During a median follow-up of 3.6 years, there were 181 incident ESKD events. Unadjusted event rates were significantly higher in those with ED/urgent care as usual source of care compared to those with clinic (27.3 vs 16.2 per 1,000 person-years; Table 2, Fig 2). Participants identifying ED/urgent care as usual source of care were at higher risk to develop ESKD (hazard ratio [HR], 1.68; 95% confidence interval [CI], 1.09-2.58) (Table 2). However, this association became nonsignificant after adjustment for clinical center, enrollment phase, age, sex, race/ethnicity, education, and income (Table 2). All model assumptions were met.
Table 2.
Association Between Usual Source of Care and Outcomes
| Outcome | No. of Events | Unadjusted Event Rate Per 1,000 Person-Year (95% CI) | Hazard Ratio (95% CI) |
||
|---|---|---|---|---|---|
| Model 1 (n = 3,140) | Model 2 (n = 3,138) | Model 3 (n = 2,692) | |||
| Incident ESKD | |||||
| Clinic | 157 | 16.2 (13.9-19.0) | Referent | Referent | Referent |
| ED/urgent care | 24 | 27.3 (18.3-40.8) | 1.68 (1.09-2.58) | 1.49 (0.95-2.33) | 0.86 (0.49-1.52) |
| Atherosclerotic event | |||||
| Clinic | 230 | 24.6 (21.6-28.0) | Referent | Referent | Referent |
| ED/urgent care | 34 | 41.5 (29.6-58.0) | 1.67 (1.16-2.39) | 1.26 (0.86-1.83) | 1.12 (0.74-1.70) |
| Incident heart failure | |||||
| Clinic | 224 | 24.0 (21.0-27.4) | Referent | Referent | Referent |
| ED/urgent care | 39 | 47.9 (35.0-65.6) | 1.95 (1.39-2.75) | 1.43 (1.00-2.05) | 1.25 (0.83-1.86) |
| All-cause death | |||||
| Clinic | 247 | 24.8 (21.9-28.1) | Referent | Referent | Referent |
| ED/urgent care | 41 | 45.3 (33.4-61.6) | 1.86 (1.33-2.58) | 1.52 (1.07-2.15) | 1.53 (1.05-2.23) |
Notes: Model 1: Unadjusted
Model 2: Clinical center, enrollment phase; age, sex, race, ethnicity education, income,
Model 3: 2 + hemoglobin A1c, statin, aspirin, ACEi/ARB, smoking status, physical activity, blood pressure <140/90 mm Hg, eGFR, log urine protein (Model 3 is shown in Fig 2)
Abbreviations: ACEi/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; ED, Emergency department; ESKD, end-stage kidney disease.
Figure 2.
Forest plot of the fully-adjusted hazard ratios for the association between usual source of care and outcomes. Abbreviations: CI, Confidence interval, HR, hazard ratio; ESKD, end-stage kidney disease.
Atherosclerotic Events
There were 264 atherosclerotic events. Atherosclerotic event rates were higher among those identifying an ED/urgent care as usual source of care (Table 2). On multivariable analyses, there was no significant association between usual source of care and atherosclerotic events (Table 2). There was a potential violation of the proportional hazards assumption for this outcome (Fig S1).
Incident Heart Failure
During follow-up, there were 263 incident heart failure events. Heart failure events were almost 2-fold higher among those identifying ED/urgent care as usual source of care (Table 2). In our unadjusted model, those identifying ED/urgent care as usual source of care were more likely to develop heart failure compared to those identifying a clinic (HR, 1.95; 95% CI, 1.39-2.75). This association was no longer significant after adjustment for clinical center, enrollment phase, age, sex, race, ethnicity, education, and income (Table 2). All model assumptions were met.
Death
There were 288 deaths during follow-up. Compared to clinic as usual source of care, ED/urgent care was associated with higher risk for death after adjustment for sociodemographic and clinical variables (HR, 1.53; 95% CI, 1.05-2.23) (Table 2). All model assumptions were met.
There was no evidence of effect modification by eGFR for the outcomes of incident ESKD, cardiovascular events, or death.
Hospitalizations
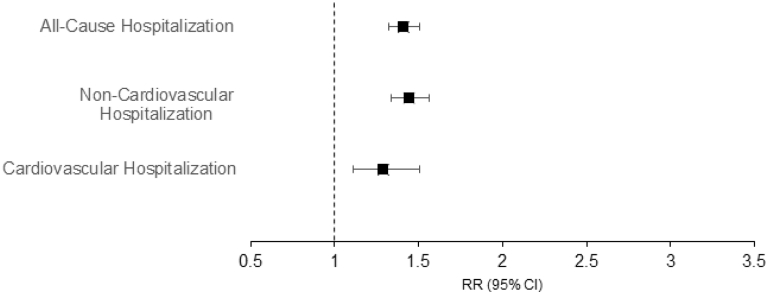
There were a total 7,957 hospitalization events, of which 6,301 (79%) were noncardiovascular and 1,656 (21%) cardiovascular. Unadjusted hospitalization rates were markedly higher among those identifying ED/urgent care as usual source of care (1,341 per 1,000 person-years) as compared to clinic (680 per 1,000 person-years). In the fully-adjusted model, ED/urgent care was associated with higher risk for hospitalizations as compared to clinic (rate ratio [RR], 1.41; 95% CI, 1.32-1.51) (Table 3, Fig 3). This association was significant for both noncardiovascular and cardiovascular hospitalizations (RR, 1.44; 95% CI, 1.34-1.56 and RR, 1.29; 95% CI, 1.11-1.51, respectively). We found a statistically significant interaction for eGFR. Therefore, hospitalization RRs are presented by eGFR categories (Table S3). Negative binomial regression results were similar to the main analysis (Table S4).
Table 3.
Association Between Usual Source of Care and Hospitalizations
| Hospitalizations | No. of Events | Unadjusted Event Rate per 1,000 Person-Year (95% CI) | Rate Ratio (95% CI) |
||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||
| All-cause | |||||
| Clinic | 6,751 | 680 (664-696) | Referent | Referent | Referent |
| ED/urgent care | 1,206 | 1,341 (1,268-1,419) | 1.97 (1.86-2.10) | 1.43 (1.35-1.53) | 1.41 (1.32-1.51) |
| Noncardiovascular | |||||
| Clinic | 5,365 | 540 (526-555) | Referent | Referent | Referent |
| ED/urgent care | 936 | 1,040 (976-1,110) | 1.93 (1.80-2.07) | 1.43 (1.33-1.53) | 1.44 (1.34-1.56) |
| Cardiovascular | |||||
| Clinic | 1,386 | 140 (132-147) | Referent | Referent | Referent |
| ED/urgent care | 270 | 300 (267-338) | 2.15 (1.89-2.45) | 1.47 (1.28-1.68) | 1.29 (1.11-1.51) |
Model 1: Unadjusted
Model 2: clinical center, enrollment phase; age, sex, race, ethnicity education, income,
Model 3: 2 + hemoglobin A1c, statin, aspirin, ACEi/ARB, smoking status, physical activity, blood pressure <140/90 mm Hg, eGFR, log urine protein (Model 3 is shown in Fig 3)
Abbreviations: ACEi/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; CI, confidence interval; ED, emergency department.
Figure 3.
Forest plot of the fully-adjusted hazard ratios for the association between usual source of care and hospitalizations. Abbreviations: CI, Confidence interval; RR, rate ratio.
Discussion
In this large prospective CKD cohort, use of ED/urgent care as usual source of care was associated with higher risk for hospitalizations and death as compared to using a clinic. We found that individuals who relied on ED/urgent care as usual source of care were a vulnerable population in terms of lower socioeconomic status, higher comorbid condition burden, and poorer blood pressure and glycemic control. Future efforts are needed to better understand barriers to care and facilitate access to care for this group.
It is well established that patients with CKD experience higher rates of hospitalizations than those without CKD.35,36 Among patients with CKD, we found that those who identified ED/urgent care as usual source of care were at a particularly high risk for hospitalizations, experiencing rates 2-fold higher than those with a clinic as usual source of care. These findings have important implications in view of the physical and mental toll of hospitalizations on patients, as well as the high costs associated with hospitalizations. Furthermore, patients with CKD are particularly vulnerable to experiencing hospital-acquired complications. In a Canadian population study, patients with CKD had 20% higher odds for developing hospital-acquired complications than those without CKD.37
Providing care for patients with CKD requires managing multiple comorbid conditions and often necessitates multispecialty care.38 EDs and urgent care centers are not designed to deliver care for chronic conditions. In our cohort, the lack of coordinated care for those relying on ED/urgent care likely contributed to the lower achievement of guideline recommended goals (ie, blood pressure, Hemoglobin A1c, and use of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker) and the higher rates of adverse clinical events and hospitalizations.
It is very likely that individuals in our cohort who used ED/urgent care as usual source of care faced significant barriers to accessing primary care. Two studies using data from the Medical Expenditure Panel Survey reported that individuals who were dissatisfied with their usual source of care or perceived access barriers to primary care were more likely to have nonurgent ED visits.39,40 Furthermore, it is well established that populations with lower socioeconomic status face greater barriers to primary care (eg, transportation issues, difficulty making limited office hours, affordability, etc).41 An important finding in our cohort was that those reporting ED/urgent care as usual source of care were disproportionately people of color and had significantly lower educational attainment and annual income. Similarly, a recent report examining ED use in the state of New Jersey reported that individuals from poorer communities were more likely to seek care in the ED for management of chronic conditions.42 In our cohort, although over 90% of individuals relying on ED/urgent care as usual source of care had medical insurance, the majority had public insurance, which may have led to greater difficulty accessing primary care services. This suggests efforts to expand health coverage (eg, the Affordable Care Act) must also address barriers to establishing and maintaining access to primary care.
Our findings suggest that there is a critical need for interventions to facilitate access to primary care for individuals with CKD who rely on ED/urgent care as usual source of care. For example, case management at the time of the ED encounter could be used to evaluate potential barriers to regular care and facilitate follow-up. Of note, a recent systematic review reported that interventions targeting frequent ED users were successful in decreasing ED visits and costs.43 Furthermore, lessons may be learned from system-based coordination of care for other health conditions. For example, in heart failure patients, transitional care interventions have been found to lower hospitalization rates and improve quality of life.44 Finally, our finding that baseline differences in education and income explained the higher risk for incident ESKD and heart failure among those relying on ED/urgent care reinforces the importance of taking into account social determinants of health and addressing broader systemic issues facing the US health care system.42
Strengths of this study include the large, diverse, and well-characterized cohort. In addition, the study captured comprehensive information on access to health care, as well as extensive clinical and laboratory measures. One important limitation of our study is that location of care is used as a proxy for measuring health care continuity, coordination, and quality. Unfortunately, these factors are difficult to capture with any single measure. In addition, the National Health Interview Survey does not capture information regarding type of provider delivering care in the clinic setting or the frequency of clinic visits. Another factor that limits generalizability of our findings is that study participants were recruited from academic centers. It is possible that study participants may be more actively engaged in their care than patients with CKD in the general population. Finally, in view of the observational study design, causal relationships cannot be established.
In summary, we found that ED/urgent care as usual source of care was associated with a higher risk for hospitalizations and death in patients with CKD. Future interventions are needed to facilitate access to care for this high-risk group with the goal of improving health outcomes and reducing costs.
Article Information
CRIC Study Investigators
Lawrence J. Appel, MD, MPH, Harold I. Feldman, MD, MSCE, Alan S. Go, MD, Robert G. Nelson, MD, PhD, MS, Mahboob Rahman, MD, Panduranga S. Rao, MD, Vallabh O Shah, PhD, MS, Raymond R. Townsend, MD, and Mark L. Unruh, MD, MS
Authors’ Full Names and Academic Degrees
Stephanie M. Toth-Manikowski, MD, MHS, Jesse Y. Hsu, PhD, Michael J. Fischer, MD, MSPH, Jordana B. Cohen, MD, MSCE, Claudia M. Lora, MD, Thida C. Tan, MPH, Jiang He, MD, PhD, Raquel C. Greer, MD, MHS, Matthew R. Weir, MD, Xiaoming Zhang, MS, PhD, Sarah J. Schrauben, MD, MSCE, Milda R. Saunders, MD, MPH, Ana C. Ricardo, MD, MPH, and James P. Lash, MD on behalf of the Chronic Renal Insufficiency Cohort (CRIC) Study Investigators
Authors’ Contributions
Research idea and study design: STM, JPL, ACR; data acquisition: JPL, MRW, TCT, XZ; data analysis/interpretation: STM, JYH, XZ, MJF, JBC, CML, TCT, JH, RCG, SJS, MRS, ACR, JPL; statistical analysis: JYH, XZ; supervision and mentorship: JPL. Each author contributed important intellectual content during manuscript drafting and revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
Funding for the CRIC Study was obtained under a cooperative agreement from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK U01DK060990, U01DK060984, U01DK061022, U01DK061021, U01DK061028, U01DK060980, U01DK060963, and U01DK060902). In addition, this work was supported in part by: the Perelman School of Medicine at the University of Pennsylvania Clinical and Translational Science Award NIH/National Center for Advancing Translational Sciences (NCATS) UL1TR000003, Johns Hopkins University UL1TR000424, University of Maryland GCRC M01RR16500, Clinical and Translational Science Collaborative of Cleveland, NIH/NCATS UL1TR000439 and NIH Roadmap for Medical Research, Michigan Institute for Clinical and Health Research (MICHR) UL1TR000433, University of Illinois at Chicago CTSA UL1RR029879, Tulane COBRE for Clinical and Translational Research in Cardiometabolic Diseases P20GM109036, Kaiser Permanente NIH/NCRR UCSF-CTSI UL1RR024131. Dr. Toth-Manikowski is funded by the NIDDK 3R01DK072231-13S1. Dr. Ricardo is funded by the NIDDK R01DK118736 Award. Dr. Lash is funded by the NIDDK K24DK092290 and R01DK072231-91 Awards.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received July 21, 2021 as a submission to the expedited consideration track with 3 external peer reviews. Direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form December 5, 2021.
Footnotes
Complete author and article information provided before references.
Figure S1: Overall and Time-Dependent Hazard Ratios of Atherosclerotic Events for Usual Source of Care
Table S1: Number of Missing Data by Usual Source of Care
Table S2: Baseline Characteristics for Those Included Vs Not Included in Regression Analyses
Table S3: Stratified Association Between Usual Source of Care and Hospitalizations by eGFR Categories
Table S4: Association Between Usual Source of Care and Hospitalizations Using Negative Binomial Regression
Contributor Information
Stephanie M. Toth-Manikowski, Email: stoth3@uic.edu.
Chronic Renal Insufficiency Cohort (CRIC) Study Investigators:
Lawrence J. Appel, Harold I. Feldman, Alan S. Go, Robert G. Nelson, Mahboob Rahman, Panduranga S. Rao, Vallabh O. Shah, Raymond R. Townsend, and Mark L. Unruh
Supplementary Materials
Figure S1; Tables S1-S4.
References
- 1.DeVoe J.E., Petering R., Krois L. A usual source of care: supplement or substitute for health insurance among low-income children? Med Care. 2008;46(10):1041–1048. doi: 10.1097/MLR.0b013e3181866443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jerant A., Fenton J.J., Franks P. Primary care attributes and mortality: a national person-level study. Ann Fam Med. 2012;10(1):34–41. doi: 10.1370/afm.1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ettner S.L. The timing of preventive services for women and children: the effect of having a usual source of care. Am J Public Health. 1996;86(12):1748–1754. doi: 10.2105/ajph.86.12.1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeVoe J.E., Fryer G.E., Phillips R., Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93(5):786–791. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corbie-Smith G., Flagg E.W., Doyle J.P., O’Brien M.A. Influence of usual source of care on differences by race/ethnicity in receipt of preventive services. J Gen Intern Med. 2002;17(6):458–464. doi: 10.1046/j.1525-1497.2002.10733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeVoe J.E., Tillotson C.J., Wallace L.S. Usual source of care as a health insurance substitute for U.S. adults with diabetes? Diabetes Care. 2009;32(6):983–989. doi: 10.2337/dc09-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liaw W., Petterson S., Rabin D.L., Bazemore A. The impact of insurance and a usual source of care on emergency department use in the United States. Int J Fam Med. 2014;2014:842847. doi: 10.1155/2014/842847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janke A.T., Brody A.M., Overbeek D.L., Bedford J.C., Welch R.D., Levy P.D. Access to care issues and the role of EDs in the wake of the Affordable Care Act. Am J Emerg Med. 2015;33(2):181–185. doi: 10.1016/j.ajem.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Liaw W., Jetty A., Petterson S., Bazemore A., Green L. Trends in the types of usual sources of care: a shift from people to places or nothing at all. Health Serv Res. 2018;53(4):2346–2367. doi: 10.1111/1475-6773.12753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Starfield B., Shi L., Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baker D.W., Stevens C.D., Brook R.H. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. JAMA. 1994;271(24):1909–1912. [PubMed] [Google Scholar]
- 12.FastStats Access to Health Care. https://www.cdc.gov/nchs/fastats/access-to-health-care.htm Published October 19, 2020.
- 13.Mainous A.G., 3rd, Koopman R.J., Gill J.M., Baker R., Pearson W.S. Relationship between continuity of care and diabetes control: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2004;94(1):66–70. doi: 10.2105/ajph.94.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kao Y.H., Tseng T.S., Ng Y.Y., Wu S.C. Association between continuity of care and emergency department visits and hospitalization in senior adults with asthma-COPD overlap. Health Policy. 2019;123(2):222–228. doi: 10.1016/j.healthpol.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blozik E., Bähler C., Näpflin M., Scherer M. Continuity of care in Swiss cancer patients using claims data. Patient Prefer Adherence. 2020;14:2253–2262. doi: 10.2147/PPA.S266381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen C.C., Chen S.H. Better continuity of care reduces costs for diabetic patients. Am J Manag Care. 2011;17(6):420–427. [PubMed] [Google Scholar]
- 17.Liu C.W., Einstadter D., Cebul R.D. Care fragmentation and emergency department use among complex patients with diabetes. Am J Manag Care. 2010;16(6):413–420. [PubMed] [Google Scholar]
- 18.Jang Y.J., Choy Y.S., Nam C.M., Moon K.T., Park E.C. The effect of continuity of care on the incidence of end-stage renal disease in patients with newly detected type 2 diabetic nephropathy: a retrospective cohort study. BMC Nephrol. 2018;19(1):127. doi: 10.1186/s12882-018-0932-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feldman H.I., Appel L.J., Chertow G.M., et al. The Chronic Renal Insufficiency Cohort (CRIC) Study: design and methods. J Am Soc Nephrol. 2003;14(7 suppl 2):S148–S153. doi: 10.1097/01.asn.0000070149.78399.ce. [DOI] [PubMed] [Google Scholar]
- 20.Lash J.P., Go A.S., Appel L.J., et al. Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol. 2009;4(8):1302–1311. doi: 10.2215/CJN.00070109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fischer M.J., Go A.S., Lora C.M., et al. CKD in Hispanics: baseline characteristics from the CRIC (Chronic Renal Insufficiency Cohort) and Hispanic-CRIC Studies. Am J Kidney Dis. 2011;58(2):214–227. doi: 10.1053/j.ajkd.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Denker M., Boyle S., Anderson A.H., et al. Chronic Renal Insufficiency Cohort Study (CRIC): overview and summary of selected findings. Clin J Am Soc Nephrol. 2015;10(11):2073–2083. doi: 10.2215/CJN.04260415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NHIS - Data, Questionnaires and Related Documentation. https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm Published June 26, 2018.
- 24.Pickering T.G., Hall J.E., Appel L.J., et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 25.Joffe M., Hsu C.Y., Feldman H.I., et al. Variability of creatinine measurements in clinical laboratories: results from the CRIC study. Am J Nephrol. 2010;31(5):426–434. doi: 10.1159/000296250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levey A.S., Coresh J., Greene T., et al. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007;53(4):766–772. doi: 10.1373/clinchem.2006.077180. [DOI] [PubMed] [Google Scholar]
- 27.Anderson A.H., Yang W., Hsu C.Y., et al. Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2012;60(2):250–261. doi: 10.1053/j.ajkd.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ho K.K., Anderson K.M., Kannel W.B., Grossman W., Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993;88(1):107–115. doi: 10.1161/01.cir.88.1.107. [DOI] [PubMed] [Google Scholar]
- 29.Lash J.P., Ricardo A.C., Roy J., et al. Race/ethnicity and cardiovascular outcomes in adults with CKD: findings from the CRIC (Chronic Renal Insufficiency Cohort) and Hispanic CRIC Studies. Am J Kidney Dis. 2016;68(4):545–553. doi: 10.1053/j.ajkd.2016.03.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clinical Classifications Software (CCS)-HCUP-AHRQ. www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp
- 31.Cedillo-Couvert E.A., Hsu J.Y., Ricardo A.C., et al. Patient experience with primary care physician and risk for hospitalization in Hispanics with CKD. Clin J Am Soc Nephrol. 2018;13(11):1659–1667. doi: 10.2215/CJN.03170318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kendrick J., Chonchol M. Cardiovascular disease in CKD in 2013: reducing cardiovascular risk--light at the end of the tunnel. Nat Rev Nephrol. 2014;10(2):71–72. doi: 10.1038/nrneph.2013.260. [DOI] [PubMed] [Google Scholar]
- 33.Menon V., Gul A., Sarnak M.J. Cardiovascular risk factors in chronic kidney disease. Kidney Int. 2005;68(4):1413–1418. doi: 10.1111/j.1523-1755.2005.00551.x. [DOI] [PubMed] [Google Scholar]
- 34.Aday L.A., Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- 35.Saran R., Robinson B., Abbott K.C., et al. US Renal Data System 2018 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2019;73(3 suppl 1):A7–A8. doi: 10.1053/j.ajkd.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schrauben S.J., Chen H.Y., Lin E., et al. Hospitalizations among adults with chronic kidney disease in the United States: a cohort study. PLoS Med. 2020;17(12) doi: 10.1371/journal.pmed.1003470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bohlouli B., Tonelli M., Jackson T., Hemmelgam B., Klarenbach S. Risk of hospital-acquired complications in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2016;11(6):956–963. doi: 10.2215/CJN.09450915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tonelli M., Wiebe N., Manns B.J., et al. Comparison of the complexity of patients seen by different medical subspecialists in a universal health care system. JAMA Netw Open. 2018;1(7) doi: 10.1001/jamanetworkopen.2018.4852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sarver J.H., Cydulka R.K., Baker D.W. Usual source of care and nonurgent emergency department use. Acad Emerg Med. 2002;9(9):916–923. doi: 10.1111/j.1553-2712.2002.tb02193.x. [DOI] [PubMed] [Google Scholar]
- 40.Mortensen K. Access to primary and specialty care and emergency department utilization of medicaid enrollees needing specialty care. J Health Care Poor Underserved. 2014;25(2):801–813. doi: 10.1353/hpu.2014.0097. [DOI] [PubMed] [Google Scholar]
- 41.Lewis C., Abrams M.K., Seervai S. Listening to low-income patients: obstacles to the care we need, when we need it. The Commonwealth Fund; 2017. https://www.commonwealthfund.org/blog/2017/listening-low-income-patients-obstacles-care-we-need-when-we-need-it Accessed February 19, 2022.
- 42.Center for Health Analytics Research and Transformation (CHART) at the New Jersey Hospital Association. Chronic Conditions: Eroding the Fabric of a Healthy Society. http://www.njha.com/healthy-communities/understanding-the-healthcare-landscape/chart/2019/january/introduction/ Accessed February 27, 2021.
- 43.Moe J., Kirkland S.W., Rawe E., et al. Effectiveness of interventions to decrease emergency department visits by adult frequent users: a systematic review. Acad Emerg Med. 2017;24(1):40–52. doi: 10.1111/acem.13060. [DOI] [PubMed] [Google Scholar]
- 44.Ba H.M., Son Y.J., Lee K., Kim B.H. Transitional care interventions for patients with heart failure: An integrative review. Int J Environ Res Public Health. 2020;17(8):2925. doi: 10.3390/ijerph17082925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ricardo A.C., Anderson C.A., Yang W., et al. Healthy lifestyle and risk of kidney disease progression, atherosclerotic events, and death in CKD: findings from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2015;65(3):412–424. doi: 10.1053/j.ajkd.2014.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1; Tables S1-S4.