Abstract
Purpose. Preventive measures to curtail the spread of the Coronavirus Disease 2019 (COVID-19)—such as home quarantine, closure of schools/programs—are necessary, yet the impact of these restrictions on children’s weight status is unknown. The purpose of this case report was to investigate changes in children’s body mass index (BMI) and zBMI during COVID-19 quarantine. Methods. Children had their heights and weights recorded early March 2020 (pre-COVID-19) and 5 months later (early August 2020). Paired sample t tests examined changes in BMI and zBMI from baseline to follow-up. Results. Twenty-nine children (62% female; mean age 9.3 years; 27.5% with overweight or obesity) provided height and weight data at both time points. There was a significant difference in pre-COVID-19 BMI (mean [M] = 20.1, standard deviation [SD] = 6.0) and follow-up BMI (M = 20.7, SD = 6.4); t (57) = −3.8, P < .001, and pre-COVID-19 zBMI (M = 0.8, SD = 0.9) and follow-up zBMI (M = 0.9, SD = 0.9); t (57) = -3.1, P = .003. Five of the 29 children moved from normal weight to overweight (n = 4) or obese (n = 1) during 5 months of quarantine. Conclusions. Preliminary evidence shows most children increased their BMI and zBMI values from pre-COVID-19 assessment to the follow-up assessment, 5 months later. These initial findings identify potential incidental negative health consequences of children as a result of COVID-19 preventative measures such as home quarantine.
Keywords: children, COVID-19, obesity, quarantine, public health
Initial evidence reporting weight-related behaviors during COVID-19 has reported decreased physical activity levels, increased sedentary time, and disrupted sleep schedules in children and adolescents.
The coronavirus disease 2019 (COVID-19) has posed a significant threat to public health and the livelihoods of children and families all over the world. Since its arrival, societal restrictions to prevent the spread of COVID-19—such as mandatory home quarantines and the closure of schools, programs, and childcare centers—have been implemented to protect the health and well-being of the population. Although such preventive measures are necessary, the impact of these restrictions on children’s physical and mental health are not well understood, yet are of paramount importance.1-3 In the United States, childhood obesity continues to be a major public health concern, 4 and evidence suggests that during summer months children exhibit accelerated weight gain in comparison to school months.5-7 One possible explanation for this may be due to the reduced exposure to the consistent, structured, school-like settings available to children over this 3-month summer period—referred to as the “Structured Days Hypothesis.” 8 The hypothesis suggests that “structure”—defined as the rules, consistent routines, and compulsory adult-supervised components that can shape a typical “structured day,” such as when children attend school, are less present during the summer, and thus allows for the occurrence of negative weight-related behaviors (eg, less physical activity, increased sedentary/screen time, less-healthful diets, inconsistent and disrupted bed/wake time), and consequentially accelerated weight gain. This same mechanism may be operating as a result of the COVID-19 pandemic, whereby children are limited or prohibited access to schools and school-like programs (eg, daycare, camps, community-operated programs) for a long uninterrupted period of time. Initial evidence reporting weight-related behaviors during COVID-19 has reported decreased physical activity levels, increased sedentary time, and disrupted sleep schedules in children and adolescents. 9 However, the consequences of COVID-19 on children’s weight outcomes remains to be seen. Thus, the purpose of this study is to investigate changes in children’s body mass index (BMI) and zBMI during COVID-19. The authors hypothesize that children will display increases in BMI and zBMI from pre-COVID-19 to 5-month follow-up.
Methods
Study Design and Sample
The present study represented an extension of an existing repeated-measures observational within-subjects pilot study. Children attending an afterschool program located within the southeast region of the United States were invited to be part of the initial study via information fliers sent home with approximately 65 children (first through sixth grade). Study information/consent forms were distributed to children during regular program hours. The afterschool program operated in a small rural town (population <900 residents) that predominately serves non-Hispanic White families. All initial study procedures were approved by the authors’ institutional review board, and parents/guardians provided written informed consent for the child. The initial study was interrupted due to COVID-19 after baseline anthropometric and demographic assessments were collected (March) on 60 children/parents who provided informed consent. The investigators received additional institutional review board approval to invite children/parents for a follow-up anthropometric assessment. The afterschool program site leader facilitated with redistributing informed consent to the parents. Consenting participants (n = 30) were contacted to inform them of the follow-up anthropometric assessment month/date (August). Each parent-child dyad received $20 for participating in both pre- and postmeasurement protocols ($40 total).
Measures
Anthropometric Assessments
For baseline and follow-up assessments, a portable stadiometer (Model S100, Ayrton Corp) and digital scale (Healthometer model 500KL, Health o meter) measured children’s heights (nearest 0.1 cm) and weights (nearest 0.1 kg), without shoes and heavy clothing (eg, removal of jackets, sweatshirts). Measures were administered by the same 2 trained research assistants for both time points. Measures were conducted at the afterschool program in a private area and in the presence of an afterschool program staff member. The follow-up assessment in August was conducted on a “sign-up day” for the afterschool program. Parents/guardians were contacted prior to this day and asked to bring their child for the height and weight measures. Due to the ongoing presence of COVID-19 during follow-up measures, additional safety measures were employed by research staff during height and weight assessments. For example, measures were conducted in an outside but covered area at the afterschool program, and research assistants wore face masks, gloves, and sanitized/disinfected the stadiometer and scale after every individual assessment.
Data Analysis
Children’s height and weight were transformed into BMI values by taking the weight in kilograms and dividing it by the square of height in meters (kg/m2). BMI categories (eg, normal weight, overweight, obese) and zBMI were calculated using age- and sex-specific normative data from the Centers for Disease Control and Prevention 10 using the Stata statistical software zanthro package (v.16.1). Paired samples t tests were used to compare baseline and follow-up changes in anthropometric data (height, weight, BMI, zBMI). Independent samples t test examined differences in baseline BMI percentiles between those children who did not participate in the follow-up anthropometric assessment versus the present study sample. Statistical significance was set at P < .05, and all analyses were performed using Stata.
Results
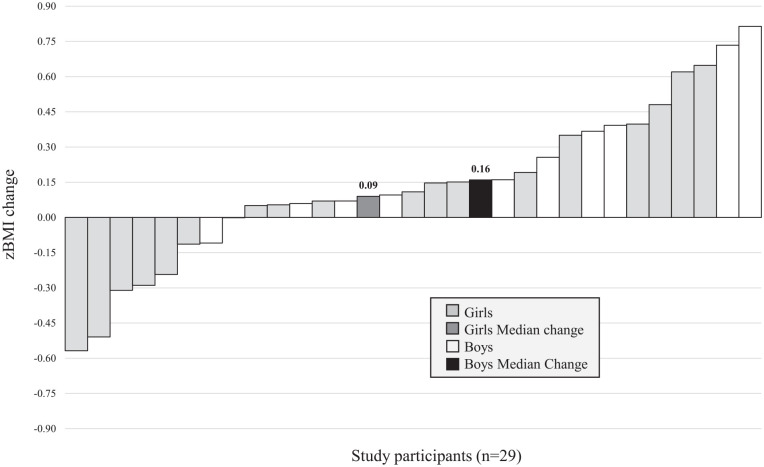
A total of 29 children (mean [M] age 9.3 years; 62% female; 97% non-Hispanic White) provided anthropometric data for both time points. There were no differences in baseline BMI percentiles between children who did (M = 0.70, SD = 0.21) versus did not (M = 0.68, SD = 0.18) participate in the follow-up anthropometric assessment (t[58] = −0.41, P = .687). Children’s anthropometric outcomes at baseline (Pre-COVID-19) and follow-up (During COVID-19), and change values are presented in Table 1. Approximately 150 days elapsed between the baseline (March) and follow-up measures (August). Results from the paired samples t test indicate there was a significant difference in baseline BMI (M = 20.1, SD = 6.0) and follow-up BMI (M = 20.7, SD = 6.4); t(57) = −3.8, P < .001, and baseline zBMI (M = 0.8, SD = 0.9) and follow-up zBMI (M = 0.9, SD = 0.9); t(57) = −3.1, P = .003 (Table 1). The percent of children who were overweight or obese increased from 27.5% to 44.8% from baseline to follow-up, respectively. Figure 1 illustrates boys’ and girls’ individual zBMI changes, and median zBMI change for all boys (n = 11) and all girls (n = 18), over the 5-month period.
Table 1.
Children’s (N = 29) Anthropometric Outcomes Following 5 Months of COVID-19 (Coronavirus Disease 2019) Quarantine.
| Outcome | Baseline (pre-COVID-19) | Follow-up (during COVID-19) | 5-Month outcome change a | P b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | ±SD | Min | Max | Median | ±SD | Min | Max | Change | ±SD | Min | Max | ||
| Height (cm) | 137.1 | 12.6 | 111.6 | 162.6 | 140.0 | 12.4 | 114.4 | 163.2 | 2.6 | 1.1 | 0.5 | 5.2 | <.001 |
| Weight (lbs) | 71.3 | 37.8 | 40.3 | 206.1 | 78.3 | 40.3 | 40.5 | 221.8 | 5.8 | 5.5 | −7.5 | 15.6 | <.001 |
| Body mass index (BMI) | 17.8 | 6.0 | 14.7 | 41.5 | 19.1 | 6.41 | 14.06 | 43.9 | 0.6 | 1.2 | −3.0 | 3.0 | <.001 |
| zBMI | 0.66 | 0.87 | −0.39 | 2.89 | 0.77 | 0.90 | −0.96 | 2.94 | 0.14 | 0.34 | −0.57 | 0.81 | <.003 |
| Percentile | 71.3 | 20.2 | 34.75 | 99.81 | 75.1 | 21.0 | 16.9 | 99.8 | 3.7 | 9.8 | −17.9 | 22.1 | <.005 |
| BMI classification (n, %) | |||||||||||||
| Normal weight | 21 (72.4) | 16 (55.2) | –5 (–17.4) | n/a | |||||||||
| Overweight | 3 (10.3) | 7 (24.1) | +4 (13.8) | n/a | |||||||||
| Obese | 5 (17.2) | 6 (20.7) | +1 (3.5) | n/a | |||||||||
Paired samples t test examining pre-post changes in mean.
Bolded values indicate statistically significant change at P < .05 level.
Figure 1.
Girls’ (n = 18) and boys’ (n = 11) individual zBMI changes after 5 months of home quarantine due to COVID-19.
Discussion
The present study is one of the first to present changes in children’s BMI and zBMI during the COVID-19 pandemic. Preliminary evidence shows that most children increased their BMI and zBMI values from pre-COVID-19 assessment to the follow-up assessment, 5 months later. This finding highlights the indirect impact COVID-19 can have on the weight status of children and raises awareness toward the potential negative consequences of prolonged periods of time quarantined at home where children are removed from their “typical” daily structure and routine.
The potential implications of COVID-19 on children’s physical and mental health have been previously noted.1-3 Yet the data presented herein provides additional evidence of the impact COVID-19 can have on children’s weight outcomes. The compulsory and deliberate actions adopted by families, school districts, and local/state authorities to curtail the spread of COVID-19 have not come without consequence. Confirming the authors’ hypothesis, the current sample of children in this study showed significant gains in BMI and zBMI over the 5-month period where they were removed from their “typical” day-to-day lives. This finding aligns with the “Structured Days Hypothesis” 8 in the sense that children were fundamentally removed from all aspects of daily “structure” typically present in their lives: in the form of the school, camps, and/or extracurricular programs. The magnitude of the increases in BMI and zBMI are similar to, if not greater than, other studies that have examined changes in children’s weight outcomes over long, uninterrupted periods of less-structured time, such as summer.5,6,11-13 For example, children’s monthly BMI change in this study was approximately 0.12 kg/m2 per month (0.60 kg/m2 ÷ 5 months), which is at the high end of a range estimates (0.04-0.15 kg/m2 per month) provided by studies assessing BMI changes during 3 months of summer break from school in samples of ethnically diverse children.5,11,13 Furthermore, the monthly changes in zBMI during COVID-19 (0.02 to 0.03) were similar in magnitude to zBMI changes observed in a large longitudinal study of ethnically diverse elementary school-aged children (0.01 to 0.03) reporting zBMI changes during summer. 12 Previous studies have reported larger BMI and zBMI gains during summer in children from racial or ethnic minority groups in comparison to children who are non-Hispanic White.5,7,12 This is of concern as the present study sample data (mostly) represent children who are non-Hispanic White; thus, it is conceivable that the impact of home quarantine because of COVID-19 could be even greater on children from racial or ethnic minority groups. In the present study, notable shifts in BMI classifications were observed. Six of the 29 children (~21%) classified as “normal weight” Pre-COVID-19 moved into the “overweight” or “obese” category 5 months later. It is also worth noting that 6 (33%) of the 18 girls in this study lost weight during this 5-month period (Figure 1), and collectively, median weight gain (zBMI) was lower in girls than boys. Although this study lacks the contextual and observational data to investigate potential reasons for this, it is plausible that girls were engaging in more favorable weight-related behaviors such as increased physical activity in and around the home, and reduced sedentary/screen time activities. Evidence shows boys are typically more active than girls, 14 and spend more time engaged in sedentary pursuits such as screen time activities. 15 Perhaps the removal of “external” opportunities to be active (eg, school programs, organized sports, etc) has affected boys to a greater extent than girls, and consequentially, boys are choosing to replace this time engaged in more sedentary pursuits at home. Collectively, these data provide initial evidence showing that the majority of children experience accelerated weight gain above and beyond what is observed during a typical 3-month summer—an existing period of time identified as “critical” for childhood obesity 16 —suggesting an “added effect” as a result of COVID-19 quarantine and community-wide lockdown restrictions.
The present study sample is small; thus, the generalizability of these results is limited. However, a considerable strength of this study was the Pre-COVID-19 measurement time point that occurred approximately 1 week prior to statewide the implementation of statewide restrictions and closures of schools, community programs, and businesses. Previous research prior to COVID-19 has identified summer as a critical window for obesity intervention as children exhibit accelerated weight gain during this long, uninterrupted period of typically less-structured time.16,17 Analogous to summer, this study has provided preliminary evidence of the negative impact COVID-19 can have on children’s BMI and zBMI during 5 months where they have been removed from their “typical” structured environments. Pediatricians, public health practitioners, and health promotion advocates need to be aware of the detrimental impact long periods of less-structured time can have on children’s health as to develop and implement interventions, programs, or initiatives in communities that target children’s weight-related behaviors during COVID-19, such as physical activity, sedentary time, diet, and sleep. 9
Acknowledgments
The authors would like to thank the Center for Behavioral Health and Research Training in the School of Social Work at the University of Central Florida for the opportunity to conduct this research.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: All initial study procedures were approved by the authors’ institutional review board.
Informed Consent: Parents/guardians provided written informed consent for the child.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
ORCID iD: Keith Brazendale  https://orcid.org/0000-0001-9233-1621
https://orcid.org/0000-0001-9233-1621
Contributor Information
Keith Brazendale, Department of Health Sciences, College of Health Professions and Sciences, University of Central Florida, Orlando, Florida.
Jeanette Garcia, Department of Health Sciences, College of Health Professions and Sciences, University of Central Florida, Orlando, Florida.
Ethan T. Hunt, Department of Exercise Science, Arnold School of Public Health, University of South Carolina, Columbia, South Carolina.
Michael Blankenship, Department of Health Sciences, College of Health Professions and Sciences, University of Central Florida, Orlando, Florida.
Daniel Eisenstein, Department of Health Sciences, College of Health Professions and Sciences, University of Central Florida, Orlando, Florida.
Ana Leon, School of Social Work, College of Health Professions and Sciences, University of Central Florida, Orlando, Florida.
References
- 1.Ashikalli L, Carroll W, Johnson C. The indirect impact of COVID-19 on child health. Paediatr Child Health (Oxford). 2020;30:430-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-related school closings and risk of weight gain among children. Obesity (Silver Spring). 2020;28:1008-1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AL van Tilburg M, Edlynn E, Maddaloni M, van Kempen K, Díaz-González de Ferris M, Thomas J. High levels of stress due to the SARS-CoV-2 pandemic among parents of children with and without chronic conditions across the USA. Children (Basel). 2020;7:193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315:2292-2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.von Hippel PT, Workman J. From kindergarten through second grade, US children’s obesity prevalence grows only during summer vacations. Obesity. 2016;24:2296-2300. [DOI] [PubMed] [Google Scholar]
- 6.Moreno JP, Johnston CA, Woehler D. Changes in weight over the school year and summer vacation: results of a 5-year longitudinal study. J Sch Health. 2013;83:473-477. [DOI] [PubMed] [Google Scholar]
- 7.Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014;11:E101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brazendale K, Beets MW, Weaver RG, et al. Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. Int J Behav Nutr Phys Act. 2017;14:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bates LC, Zieff G, Stanford K, et al. COVID-19 impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children. 2020;7:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1-190. [PubMed] [Google Scholar]
- 11.Tanskey LA, Goldberg JP, Chui K, Must A, Sacheck JM. Accelerated summer weight gain in a low-income, ethnically diverse sample of elementary school children in Massachusetts. Child Obes. 2019;15:244-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moreno JP, Johnston CA, Chen TA, et al. Seasonal variability in weight change during elementary school. Obesity (Silver Spring). 2015;23:422-428. [DOI] [PubMed] [Google Scholar]
- 13.Weaver RG, Hunt E, Rafferty A, et al. The potential of a year-round school calendar for maintaining children’s weight status and fitness: preliminary outcomes from a natural experiment. J Sport Health Sci. 2020;9:18-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181-188. [DOI] [PubMed] [Google Scholar]
- 15.LeBlanc AG, Katzmarzyk PT, Barreira TV, et al. Correlates of total sedentary time and screen time in 9-11 year-old children around the world: the international study of childhood obesity, lifestyle and the environment. PLoS One. 2015;10:e0129622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weaver RG, Beets MW, Brazendale K, Brusseau TA. Summer weight gain and fitness loss: causes and potential solutions. Am J Lifestyle Med. 2019;13:116-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tanskey LA, Goldberg J, Chui K, Must A, Sacheck J. The state of the summer: a review of child summer weight gain and efforts to prevent it. Curr Obesity Rep. 2018;7:112-121. [DOI] [PMC free article] [PubMed] [Google Scholar]