Abstract
The highly contagious novel Coronavirus Disease 2019 (COVID-19) broke out at the end of 2019 and has lasted for nearly one year, and the pandemic is still rampant around the world. The diagnosis of COVID-19 is on the basis of the combination of epidemiological history, clinical symptoms, and laboratory and imaging examinations. Among them, imaging examination is of importance in the diagnosis of patients with suspected clinical cases, the investigation of asymptomatic infections and family clustering, the judgment of patient recovery, rediagnosis after disease recurrence, and prognosis prediction. This article reviews the research progress of CT imaging examination in the COVID-19 pandemic.
Keywords: Novel coronavirus, pneumonia, computed tomography, diagnosis, chest radiograph, COVID-19
1. INTRODUCTION
Since December 2019, unknown cases of pneumonia were reported in Wuhan City, Hubei Province [1]. Subsequently, this pneumonia outbreak was transmitted rapidly to many countries and subsequently to regions all over the world, including South Korea [2], Japan, France, Italy, and the United States [3, 4]. By the second week of October 2020, the disease had infected more than 37.4 million people worldwide, killing 1.07 million [5]. This horrible, frightening pneumonia that has swept the globe was subsequently confirmed to be an infection by a novel coronavirus through gene sequencing [6].
Although the original source of the virus is still unknown, current existing studies shown that it shares more than 95% homology with a bat virus [7], and it was speculated that the natural host of the virus was probably bats. After evolution and variation, bat intermediated host human transmission completed. Through the interaction between S protein and human angiotensin converting enzyme 2, the virus finally infected human lung epithelial cells [8]. Eventually, this virus has a strong human-to-human infection ability.
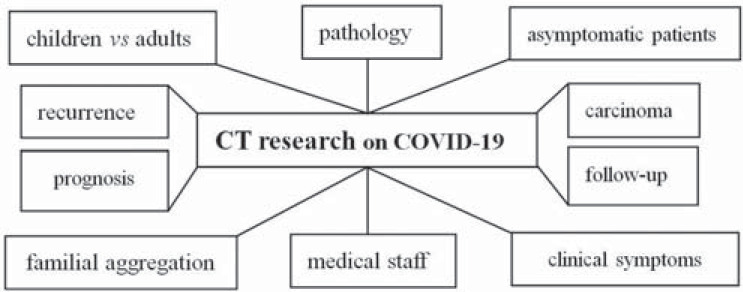
The International Committee on Taxonomy of Viruses officially named the virus severe acute respiratory syndrome (SARS) coronavirus [9], and the WHO named the disease coronavirus disease 2019 (COVID-19) [10]. The clinical diagnosis of COVID-19 is based on a comprehensive assessment, including epidemiological history, clinical manifestation, laboratory test, and imaging examination [11]. The diagnostic gold standard is reverse transcription quantitative polymerase chain reaction nucleic acid detection [11]. However, the number of nucleic acid detection tests is limited, the detection time is long, the overall positive rate of detection is not high at only 30%-50% [12], and some cases have even reported typical computed tomography (CT) manifestations associated with multiple negative nucleic acid detections [13]. The positive detection rate of COVID-19 through CT is approximately 89% [14], and its sensitivity is higher than that of nucleic acid detection. Therefore, imaging is valuable in the diagnosis of COVID-19. This article reviews the chest imaging of COVID-19 (Fig. 1).
Fig. (1).
Research contents of pulmonary CT imaging on COVID- 19 patients.
1.1. Imaging Findings of COVID-19 Pneumonia
Professor Guan Hanxiong of Wuhan Tongji Hospital first reported the CT manifestations of COVID -19 disease on February 3, 2020 [15]. In the early stage of the disease, localized inflammatory infiltration in one or both lungs was found, and Ground-Glass Opacity (GGO) was seen under the pleura. GGO is characterized by reduced local transparency of lung tissue, a very light shadow, and uneven density. During this period, lung texture structure can be seen, which is generally only displayed on the lung window and not on the mediastinal window. COVID-19 can also present with consolidation. The density of consolidation was higher than that of GGO, the distribution was even, and there was no lung texture present. In the progressive stage, CT showed more focus in larger range, gradually involving multiple lung lobes. GGO coexisted with consolidation shadow, accompanied by thickening of the interlobular septum, presenting a “paving stone” sign or combined with a fibrosis focus. The “paving stone sign” showed that the interlobular septal thickening was similar to a fine mesh under the background of diffuse or scattered ground glass. Severe cases showed diffuse lesions in both lungs, presenting as “white lung” [15]. “White lung” was a large, patchy shadow in two lungs. The disease developed rapidly in a short term, involving multiple lobes or segments. In the remission stage, the lesions gradually absorbed, then fibrous bands formed.
After these observations, Professor Shi Heshui et al. studied the manifestations of chest film and CT of COVID-19 on February 6, 2020 [16]. At the early stage of the lesion, the chest radiograph showed no abnormality or bronchitis and bronchiolitis. When the lesions were obvious, there were multiple patchy or patchy consolidation shadows in both lungs. When the lesions were serious, the two lungs showed diffuse consolidation, even presenting “white lung”. Shi et al. [16] divided COVID into three stages: early stage, advanced stage and severe stage. The results indicated that the main imaging manifestations of COVID-19 comprised single or double lung; multiple, patchy, or segmental GGOs, or a “paving stone” sign in most lesions. Most of the lesions were distributed along the bronchovascular bundle or dorsolateral or subpleural, and a few showed interlobular pleural thickening, while others were shown with a small amount of pleural effusion or pericardial effusion.
Shi et al. [16] first presented the application of Artificial Intelligence (AI) in the diagnosis of COVID-19 pneumonia. The technology can automatically, quickly and accurately provide doctors with diagnosis and treatment advice, greatly reduce the medical burden, alleviate the difficult situation of isolation, prevention, and control, and help address the medical staff shortage. Later, other researchers also found that AI can accurately evaluate pneumonia on CT imaging in COVID-19 patients [17]. It can also reliably diagnose chest X-ray radiographs of COVID-19 disease [18].
X-ray helps to monitor the rapid progression of lung abnormalities in COVID-19, particularly in critical patients admitted to Intensive Care Units (ICU). It grades severity based on three patterns: 1, interstitial infiltrates; 2, interstitial and alveolar infiltrates (interstitial predominance); and 3, interstitial and alveolar infiltrates (alveolar predominance) [19]. Other scholars believe that CT is recommended as the first choice [20].
Imaging was researched in a total of 130 patients with COVID-19 from several hospitals [21]. The most common CT sign is GGO (70 cases), followed with GGO+consolidation. The most common accompanying signs were vascular thickening (100 cases), followed by pleural parallel sign, intralobular septal thickening, halo sign, reversed-halo sign, and pleural effusion. The rarest sign is pneumatocele (2 cases). No cases exhibited pulmonary cavity [21].
These CT features were confirmed by subsequent studies [22-25]. The initial CT features included bilateral multifocal GGO peripheral or posterior distributed, mainly in the lower lobe. With the development of the disease, follow-up CT showed that the number and size of GGOs increased, and GGOs gradually changed into multifocal consolidation, septal thickening, and crazy paving mode. These CT manifestations were the most common signs within approximately 10 days after the symptoms appeared. Acute Respiratory Distress Syndrome (ARDS) is the most common symptom for the transfer of COVID-19 to the ICU, and it is also the main cause of death of the patients [26]. Compared with non- COVID-19, COVID-19 had more peripheral distribution, GGO, fine reticular opacity, and vascular thickening, but less central and peripheral distribution, pleural effusion, or lymphadenopathy [27].
1.2. Imaging Findings of COVID-19 in Different Ages
The CT manifestations of 36 elderly patients (61-82 years) [28] with COVID-19 were analyzed, and it was found that elderly patients with COVID-19 had more basic diseases. CT characteristics included diversity and multifocality mainly showing the coexistence of GGO and consolidation in the lung (72.2%), most of which were located in the outer lung field of bilateral lung (69.4%); air bronchogram was found in the focus (58.3%); and the progress of the disease was relatively fast. Most of the patients with severe pneumonia were male patients. Older patients with COVID-19 had a more serious condition after infection due to the decrease in immunity. Disease progression was faster than that of young people, development into severe or critical stages was more common, and the mortality rate increased [28].
Pediatric COVID-19 patients have certain differences compared with adult patients. A total of 9 pediatric patients (3 months to 12 years old) with COVID-19 were included in a study [29]. The initial CT scans of 5 patients were positive with GGO or spotty mixed consolidation. Three patients underwent CT examination, but false negative results were found. One child had negative CT findings at the first examination, and the lesion appeared at the follow-up. After therapy, the lesions with positive findings on initial CT had different degrees of absorption. Children with COVID-19 seem to have a milder CT findings and a better prognosis than the adults [29]. Pediatric patients with COVID-19 have relatively mild signs and symptoms, and CT images indicate that children with COVID-19 have more subtle and focal lesions than adult patients. CT images during follow-up showed that lesions diminished shortly after the treatment, indicating that pediatric patients may have a better outcome.
The chest CT findings of 9 infants (0-3 years old) diagnosed with COVID-19 by nucleic acid testing were studied [30]. The focus shape was nodular in 6 cases, with the largest focus cross-sectional area of approximately 16 mm × 12 mm. The focus density was ground-glass shadow in 7 cases, of which 3 cases exhibited the “halo sign” ; no “anti-halo sign” and no “paving stone sign”; air bronchogram in 1 case [30]. The pulmonary inflammatory response of children with COVID-19 is not as strong as that of adults. The range of focus in children is usually small, which makes it difficult to distinguish from other child pneumonia images. The diagnosis needs to be combined with the epidemiological history of the children.
Overall, compared with adults, child with COVID-19 were featured with lower incidence, fewer severe clinical symptoms, more mild cases, faster absorption and shorter course of disease [31]. The CT characteristics of COVID-19 in children were atypical, more localized, and lower GGO attenuation (Table 1) [31].
Table 1.
| - | Children | Adults |
|---|---|---|
| History of epidemiology | Familial clustering history | History of living in epidemic area/ community communication |
| Chronic basic disease | No | 25% |
| Dyspnea | No | 31% |
| Develop into severe pneumonia | No | Easily |
| Clinical types | Mild, common | Mild, common, severe, fatal |
| rRT-PCR | Positive | Positive |
| Imaging features | A typical, mild, subtle, focal | Typical, various, multifocal, diffuse |
| Pulmonary nodules distribution | Limited | Widely |
| Initial CT findings | Negative/GGO/ minor GGO /spot-like mixed consolidation | GGO/GGO accompanied with air bronchogram sign or thickened vascular shadow/consolidation/fibrous streak shadow |
| "Paving stone sign" | No | Yes |
| "Anti halo sign" | No | Yes |
| "White lung" | No | Yes |
| Follow-up CT after therapy or treatment | Mixed spot-like patchy GGO/ slightly absorbed/absorbed | Absorbed /fibrous streak/ turning into "paving stone" sign even "white lung" |
| Severe pneumonia, even death | No | A few |
| Prognosis | Good | Good/bad/worse/death |
rRT-PCR: Real-time Reverse Transcription Polymerase Chain Reaction for SARS-CoV-2.
Since children have incomplete immune system development, the immune response during infection is relatively low compared with adults. This might help to explain why children tend to have minor clinical symptoms and subtle imaging features.
1.3. CT Findings of COVID-19 with Familial Aggregation
Scholars studied the clinical and CT manifestations of three family groups of patients with COVID-19 pneumonia, comprising a total of 7 cases, 4 males and 3 females [32]. Family members may not have the disease at the same time. There are temporal differences in clinical symptoms, nucleic acid detection and CT manifestations. Nucleic acid was positive and CT was negative at first in some cases [32]. It is possible that the virus is mainly located in the upper respiratory tract and does not cause infiltrative and exudative lesions in the lung. Therefore, CT screening alone may result in a missed diagnosis. In some cases, the CT was positive while the nucleic acid test was negative. The reason for this may be that the ability of respiratory tract detoxification in such patients was very high, and nucleic acid test couldn’t detect the virus. It is therefore suggested that if one person in a family has a confirmed infection, other close contact members, even if there are no obvious symptoms, should receive CT screening for the purpose of early detection, early isolation, and early treatment. Other studies also show that while clinical symptoms are not obvious [33], foci may have already appeared in the lung. This indicates that the imaging manifestations of COVID-19 may not completely match the clinical manifestations, suggesting that patients with family onset tendencies need to be screened simultaneously [33].
1.4. Comparison of Imaging Features Between COVID-19 and Lung Carcinoma
It is worth noting that lung imaging GGO can also be a sign of benign lesions, such as focal interstitial fibrosis, inflammation, infection or bleeding; alternatively, they can be lung cancer or precancerous lesions. The imaging characteristics of 71 patients with COVID-19 were studied and compared with 80 patients with early lung tumors in the same period [34]. The COVID-19-related GGO pneumonia group had specific clinical symptoms and epidemic history. To distinguish COVID-19-related GGO pneumonia from early tumors, in addition to the CT manifestations mentioned above, it is necessary to perform a comprehensive analysis based on the patients' symptoms, epidemic history, blood test, and nucleic acid test results. Patients with COVID-19 pneumonia often have fever, cough, fatigue, myalgia, dyspnea, or other clinical symptoms. COVID-19 patients with GGO changes are mostly in the early stage, but they can rapidly progress to severe dyspnea or even ARDS. On the contrary, early lung tumor patients with GGOs mostly lack these symptoms.
CT shows more than two GGO lesions, mainly distributed in the peripheral 1/2 band of both lungs, with most of the lesion diameter > 1 cm in COVID-19 cases. In the early stage of the pandemic, the morphology of COVID-19 was similar to that of the early stage of lung tumor. With the disease progression, fusion and consolidation appeared. COVID-19 cases show indications such as “paving stone sign” or “bronchial inflation sign”. On the other hand, if the lesion shows a solid component or if the edge shape of the lesion exhibits indications such as the “lobed sign”, “traction sign”, “pleural depression sign”, “bronchial truncation sign”, or “vascular bundle sign”, this usually indicates the possibility of an early lung tumor (Table 2) [34].
Table 2.
Clinical and imaging comparison between COVID-19 and early lung tumor [34].
| - | - | COVID-19 | Early Lung Tumor |
|---|---|---|---|
| Epidemic history | - | Yes | No |
| Symptoms (fever, dyspnea) | - | Yes | No |
| Virus nucleic acid test | - | Positive | Negative |
| Lesions location | Peripheral 1/2 band | 97% | 62% |
| - | Inner 1/2 band | 3% | 38% |
| Number of lesions | - | Multiple | Single |
| Lesions diameter | > 1 cm | 92% | 64% |
| - | ≤1 cm | 8% | 36% |
| In 5-7ds, GGO turns into | “Paving stone sign” | Some | No |
| - | Consolidation | Some | No |
| - | “White lung” | A few | No |
| Image features change | - | Fast | Slow |
| Lobed sign | - | No | Yes |
| Traction sign | - | No | Yes |
| Pleural depression sign | - | No | Yes |
| Bronchial truncation sign | - | No | Yes |
| Vascular bundle sign | - | No | Yes |
| Rapid deterioration into | Severe dyspnea | A few | No |
| - | ARDS | A few | No |
| Pathology | - | Inflammatory reaction: Hyaline membrane, neutrophil infiltration | Adenocarcinoma in situ or minimally invasive adenocarcinoma |
ARDS: Acute Respiratory Distress Syndrome.
1.5. Imaging Findings of COVID-19 Infection in Medical Staff
Due to the close contact between medical staff and patients with COVID-19, there is a great risk of cross infection from patients to medical staff. High-intensity virus exposure is an important factor leading to infection. COVID-19 pneumonia was also studied in medical personnel (22 doctors and 8 nurses) [35]. All 30 patients underwent chest CT examination on admission. All patients had lung imaging abnormalities at the initial stage of onset, mainly manifested as multiple small patchy shadows and interstitial changes. In a short period of time, the lesions increased rapidly and progressed to multiple ground-glass shadows and infiltrating shadows in both lungs. Consolidation and fiber strip shadows could appear in some patients during the recovery period. Eleven cases (36.67%) involved one side, and 19 cases (63.33%) involved both lungs. Nineteen cases had complete absorption, 9 cases had partial absorption, and 2 cases had no absorption. With the development of the disease, CT imaging showed a dynamic evolution process in the initial, progressive and recovery stages. The average time from onset to progression was 7 ± 2 days and that from progression to recovery was 16 ± 7 days [35].
The imaging findings of medical staff after infection were the same as those of ordinary patients. Novel coronavirus pneumonia is highly infectious, and medical staff infection risk is great [36]. Medical personnel should strictly follow the classified protective measures in cases of inevitable need to contact novel coronavirus pneumonia patients. The risk of infection can be prevented and reduced by wearing isolation clothes, shoe covers, working caps, medical protective masks and gloves and by strict implementation of basic protective measures such as hand hygiene. Patients and their family members should wear masks when visiting and hospitalizing. In short, good protection is an important measure to prevent infection to medical staff.
There were 95 patients in one study, all of whom were hospital staff, including 44 nurses [37]. The average age of all patients was 37 years (21-63 years). The average time from symptom onset to the first chest CT manifestation was 4 days, the time to the most serious condition was 8 days, and the time to the absorption was 15 days [37]. In the early stage of disease (0-4 d), a single ground-glass shadow can be seen in patients, but with disease progression, most patients show new lesions. A consolidation shadow most often appears in the progressive stage (8 d). There was a trend of gradual absorption (15 d) and over the dissipated course of the disease, fiber strip shadow is more common than grid shadow [37].
1.6. Imaging Findings of Asymptomatic COVID-19 Patients
It is worth noting that some patients may be asymptomatic while the lung undergoes inflammatory changes. Therefore, we should pay attention to the identification of these atypical patients because these patients may be the source of community communication. Novel coronavirus pneumonia patients with clinically asymptomatic infection in Wuhan Central Hospital were retrospectively analyzed [38]. The CT images showed that the lesions of new coronavirus pneumonia were mostly distributed in the periphery of the lung (89.3%), the distribution between the two lungs was common (57.2%), and most of the imaging was mainly distributed in GGO (95%). In the short-term reexamination, the prognosis of most patients was good (73.7%) [38].
Different GGO manifestations occur in asymptomatic cases with COVID-19 patients [39]. A study of 58 asymptomatic cases reported that while the number of cases showing pure GGO was 30 (51.7%), GGO was accompanied by other signs as follows: fine reticulation, subpleural curviliner line, halo sign, air bronchogram, vascular enlargement, and consolidation [39].
CT images of asymptomatic infection have certain imaging characteristics. Chest CT screening is particularly important for the asymptomatic patients who have close contact with the infected population, as it is conducive to early diagnosis, early isolation, and early therapy.
1.7. Imaging Findings of Patients with COVID-19 Recurrence
The positive retest patients who were readmitted to the hospital were treated as confirmed cases. Five cases of COVID-19 were reported to be admitted again after being cured [40]. Among the 5 patients who were readmitted with COVID-19, the oldest was 60 years old, and the youngest was 19 years old; four patients had the basic disease; 5 cases had an epidemiological history, with their first symptoms being fever and diarrhea; 4 cases were of the common type of COVID-19, and 1 case was the severe type; 4 cases were confirmed by nucleic acid test, and 1 case was diagnosed by clinical diagnosis. All of them showed GGO on CT imaging examination, which improved after being given antiviral drugs and treatment according to the symptoms, such as anti-infection, anti-virus, or Chinese herbal medicine therapy. It seems that there is no worsening of CT imaging in patients who are readmitted after recovery.
1.8. Correlation between the CT Dynamic Changes and Clinical Manifestations
Correlation between the dynamic imaging in CT and the age of patients. In 38 patients, CT reexamination was performed [38]. It was found that the lesions were basically absorbed in 6 patients; the median age of these patients was 29 years old, and the average reexamination interval was 11.3 days [38]. The basic absorption of lesions may be related to patients’ own immunity and early and timely isolation treatment. On the other hand, seven patients had poor progress on chest CT reexamination. The average age of the patients was 46 years old, and the average reexamination interval was 11.6 days [38]. The median age of patients in the different groups is reflected in different CT imaging [38].
Correlation between clinical symptoms and CT scanning. Dynamic CT pulmonary lesions developed from local to multiple and diffuse lesions, and the involved area was significantly expanded [16]. At this time, the clinical symptoms of the patients were aggravated. In a short period of time, diffuse ground-glass density shadows or consolidation shadows of two lungs developed, presenting as “white lung”. The clinical manifestation was mainly a decrease in oxygen partial pressure, suggesting that early ARDS may be possible. It can be recommended that patients receive high-flow nasal catheter oxygen therapy or noninvasive mechanical ventilation-assisted respiration [41]. On the other hand, when the range of pulmonary lesions decreased, GGO density decreased, and consolidation of the lung turned into a cord fibrosis shadow or was even gradually absorbed [16]. These changes were simultaneously accompanied by improvements in clinical manifestations, including body temperature decrease and reduction of dry cough and dyspnea [41].
In summary, the changes in clinical symptoms were consistent with the dynamic changes in CT of COVID-19. As clinical symptoms worsened, CT also showed aggravation. On the contrary, as clinical symptoms were relieved, CT showed gradual absorption of the lesions.
1.9. Correlation Between Imaging and Pathology
One research team analyzed minimally invasive samples from a 50-year-old man who died of severe COVID-19 [42]. Histopathological samples were obtained from the autopsy. Histologic examination showed bilateral diffuse alveolar injury with fibrous mucoid exudate. In the right lung tissue, there was obvious cell exfoliation and hyaline membrane formation, suggesting ARDS. Left lung tissue also had hyaline membrane formation with pulmonary edema. After treatment, the patient had many X-ray examinations (without CT), which indicated that there were multiple patchy shadows, progressive infiltration, and diffuse reticular shadows in both lungs. Compared with the pathological results, chest X-rays showed “progressive infiltration and diffuse reticular shadow of both lungs”, indicating “diffuse alveolar injury with cellular fibrous mucoid exudate”. The patient's pneumonia progressed rapidly, and the chest radiograph results were consistent with the pathological findings [42].
Subsequently, Professor Liu Liang in the Department of Forensic Medicine, Huazhong University of Science and Technology, conducted the first systematic autopsy of dead bodies of COVID-19 in China starting on February 16, 2020, and general observations of an autopsy were reported [43]. Bilateral lung lobules were filled, dilated and mixed with dark red congestion and bleeding areas, especially in the lung marginal zone. A large amount of gray-white viscous liquid spilled out, and fiber cords were seen after incision. On the 20th day after admission, CT scans showed multiple patchy ground-glass shadows in both lungs, air bronchogram signs, with the left lung being more serious, and fibrous cord shadows in both lower lungs [43]. The results of autopsy examination were consistent with the distribution of imaging changes, and the lesions were further developed. It is suggested that COVID-19 may cause an inflammatory reaction characterized by deep airway and alveolar injury.
Autopsies were performed on ten African American descendants [44]. The pulmonary alveoli of the patients who died of COVID-19 contained a large amount of hyaline membrane, with thrombosis and microangiopathy in their pulmonary vessels [44].
Acute COVID-19 pneumonia is characterized by interstitial pneumonia, diffuse alveolar injury, microvascular fibrin deposition and neutrophil infiltration [45]. Bronchial mucosa edema and alveolar inflammation have been reported [46].
The postmortem core biopsies also revealed diffuse type II pneumocyte hyperplasia, epithelial damage and fibrin exudates [47]. In the early exudative stage, COVID-19 was characterized by GGO on chest X-ray. With the disease progression, consolidation occurred in severe patients due to fibroblasts proliferation, extracellular matrix formation and the interstitial thickening [47].
1.10. CT Follow-up After Discharge
The chest CT follow-up of 68 patients after discharge was analyzed [48]. In group one, 45 cases were of the common type. The first chest CT follow-up after discharge was performed at an average of 17 days. In group two, 23 patients had the severe type, and chest CT was reexamined for the first time at an average of 19 days after discharge. The CT signs of residual lung lesions were compared between the two groups. In both groups, GGO was the most common CT lesion, followed by streak shadow. The proportion of patients without obvious residual lung lesions in group one was higher than that in group two (35% vs. 4%) (P < 0.01), and the proportion of patients with two or more lobes involved in group one was less than that in group two (44% vs. 82%) (P < 0.01) [48]. In common type patients, the absorption of lesions is faster, and the time required for complete absorption of lesions is shorter than that of patients with severe type disease (Table 3).
Table 3.
Comparison of CT follow-up in different types of patients after discharge [48].
| - | Common Type | Severe Type |
|---|---|---|
| No obvious residual lesion | 36% | 4% |
| Lesion ≥ 2 lung lobes involved | 44% | 82% |
| Residual lesions number | Fewer | More |
| CT | GGO/fibrous shadow/Interlobular septal thickening | GGO/ streak shadows/Consolidation |
| Lesions absorption | Faster | Slower |
The lung lesions were absorbed quickly after discharge in the common type; some patients even had complete absorption of lung lesions, with only a few patients exhibiting fibrous lung shadow. The main residual lesions on CT in severe patients were GGO and streak shadows, which need further follow-up. Chest CT is an important method for the follow-up of COVID-19 patients. Patients with more lesions should be followed up to observe their dynamic changes [48].
1.11. CT and Prognosis
CT patterns of COVID-19 can be used to predict the prognosis. Imaging features were divided into 4 patterns [49]. Pattern 4 (diffuse alveolar injury: lesions widely distributed in the whole lung; CT: consolidation and / or air bronchography) showed high risk of ICU admission, mechanical ventilation or death. Pattern 3 (progressive organizing pneumonia: multiple lesions mainly distributed in the middle and lower part of the lung; CT showed consolidation and/ or interlobular septal thickening) is likely to have pulmonary residuals on CT [49]. Pattern 1 (bronchopneumonia: discrete lesions around the bronchus; CT features with GGO or consolidation, or tree-in-bud sign or nodular opacity) and Pattern 2 (organizing pneumonia: multifocal lesions mainly distributed in the middle and lower lung regions; CT features with GGO or consolidation, and/ or interlobular septal thickening) subsequently complete absorption. Researchers suggest that CT patterns 1-2 of COVID-19 can be considered the mild group. These patients could be introduced to community hospital, while patients with patterns 3 or 4 should be recommended to designated hospitals [49]. CT manifestations could be used to predict prognosis, determine the choice of treatment methods and the best utilization of medical resources.
1.12. CT Limitations
CT, the most efficient imaging tool in the diagnosis and follow-up of patients with COVID-19, that its actual diagnostic performance, is needed to be verified using a reference standard [50]. The CT findings of COVID-19 may overlap with the CT imagings of lung diseases caused by other pathogens [51]. That is to say: different pneumonia diseases may have the same CT findings. For example, it is still limited in identifying specific viruses and distinguishing between different viruses. The typical findings of COVID-19, such as GGO or “reversed halo” sign, are not specific to COVID-19 as similar CT results may be found in an influenza epidemic [52].
CONCLUSION
In conclusion, imaging examination is of great value in the COVID-19 diagnosis. CT scan plays an active role in the examination of clinical symptoms, the screening of patients with familial clustering diseases and asymptomatic infections, the reexamination of patients after treatment, and the judgment of prognosis.
ACKNOWLEDGEMENTS
Declared none.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
We are grateful to the projects supported partly by Nantong “226 high level talents training project” fund project (YYRC1710), Nantong Health Commission Research project (Grant No.MB2019018), and Nantong University clinical medicine project (2019LY033).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoon S.H., Lee K.H., Kim J.Y., Lee Y.K., Ko H., Kim K.H., Park C.M., Kim Y.H. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): Analysis of nine patients treated in Korea. Korean J. Radiol. 2020;21(4):494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sigman S.A., Mokmeli S., Monici M., Vetrici M.A.A. A 57-year-old african american man with severe COVID-19 pneumonia who responded to supportive photobiomodulation therapy (PBMT): First use of PBMT in COVID-19. Am. J. Case Rep. 2020;21:e926779. doi: 10.12659/AJCR.926779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H., Spitters C., Ericson K., Wilkerson S., Tural A., Diaz G., Cohn A., Fox L., Patel A., Gerber S.I., Kim L., Tong S., Lu X., Lindstrom S., Pallansch M.A., Weldon W.C., Biggs H.M., Uyeki T.M., Pillai S.K. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Premraj A., Aleyas A.G., Nautiyal B., Rasool T.J. Nucleic acid and immunological diagnostics for SARS-CoV-2: Processes, platforms and pitfalls. Diagnostics (Basel) 2020;10(11):866. doi: 10.3390/diagnostics10110866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N., Bi Y., Ma X., Zhan F., Wang L., Hu T., Zhou H., Hu Z., Zhou W., Zhao L., Chen J., Meng Y., Wang J., Lin Y., Yuan J., Xie Z., Ma J., Liu W.J., Wang D., Xu W., Holmes E.C., Gao G.F., Wu G., Chen W., Shi W., Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., Chen H.D., Chen J., Luo Y., Guo H., Jiang R.D., Liu M.Q., Chen Y., Shen X.R., Wang X., Zheng X.S., Zhao K., Chen Q.J., Deng F., Liu L.L., Yan B., Zhan F.X., Wang Y.Y., Xiao G.F., Shi Z.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yan R., Zhang Y., Li Y., Xia L., Guo Y., Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367(6485):1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bchetnia M., Girard C., Duchaine C., Laprise C. The outbreak of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): A review of the current global status. J. Infect. Public Health. 2020;13(11):1601–1610. doi: 10.1016/j.jiph.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jee Y. WHO international health regulations emergency committee for the covid-19 outbreak. Epidemiol. Health. 2020;42:e2020013. doi: 10.4178/epih.e2020013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu R., Han H., Liu F., Lv Z., Wu K., Liu Y., Feng Y., Zhu C. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to Feb 2020. Clin. Chim. Acta. 2020;505:172–175. doi: 10.1016/j.cca.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang W., Sirajuddin A., Zhang X., Liu G., Teng Z., Zhao S., Lu M. The role of imaging in 2019 novel coronavirus pneumonia (COVID-19). Eur. Radiol. 2020;30(9):4874–4882. doi: 10.1007/s00330-020-06827-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bao C., Liu X., Zhang H., Li Y., Liu J. Coronavirus disease 2019 (COVID-19) CT findings: A systematic review and meta-analysis. J. Am. Coll. Radiol. 2020;17(6):701–709. doi: 10.1016/j.jacr.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan H.X., Xiong Y., Shen N.Q., et al. Clinical and thin-section CT features of patients with 2019 nCoV-pneumonia. Radiol. Prat. 2020;35(2):125–130. [Google Scholar]
- 16.Shi HS, Han XY, Fan YQ, et al. Radiologic features of patients with 2019-nCoV infection. J. Clin. Radiol. 2020;39(1):8–11. [Google Scholar]
- 17.Zhang H.T., Zhang J.S., Zhang H.H., Nan Y.D., Zhao Y., Fu E.Q., Xie Y.H., Liu W., Li W.P., Zhang H.J., Jiang H., Li C.M., Li Y.Y., Ma R.N., Dang S.K., Gao B.B., Zhang X.J., Zhang T. Automated detection and quantification of COVID-19 pneumonia: CT imaging analysis by a deep learning-based software. Eur. J. Nucl. Med. Mol. Imaging. 2020;47(11):2525–2532. doi: 10.1007/s00259-020-04953-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borkowski A.A., Viswanadhan N.A., Thomas L.B., Guzman R.D., Deland L.A., Mastorides S.M. Using artificial intelligence for COVID-19 chest X-ray diagnosis. Fed. Pract. 2020;37(9):398–404. doi: 10.12788/fp.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Albrandt-Salmeron A., Espejo-Fonseca R., Roldan-Valadez E. Correlation between chest X-Ray severity in COVID-19 and age in Mexican-Mestizo patients: An observational cross-sectional study. Bio. Med. Res. Int. 2021;2021:5571144. doi: 10.1155/2021/5571144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zu Z.Y., Jiang M.D., Xu P.P., Chen W., Ni Q.Q., Lu G.M., Zhang L.J. Coronavirus disease 2019 (COVID-19): A perspective from China. Radiology. 2020;296(2):E15–E25. doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu J., Feng L.C., Xian X.Y., Qiang J., Zhang J., Mao Q.X., Kong S.F., Chen Y.C., Pan J.P. Novel coronavirus pneumonia (COVID-19) CT distribution and sign features. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(4):321–326. doi: 10.3760/cma.j.cn112147-20200217-00106. [DOI] [PubMed] [Google Scholar]
- 22.Zheng Q., Lu Y., Lure F., Jaeger S., Lu P. Clinical and radiological features of novel coronavirus pneumonia. J. XRay Sci. Technol. 2020;28(3):391–404. doi: 10.3233/XST-200687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shen C., Yu N., Cai S., Zhou J., Sheng J., Liu K., Zhou H., Guo Y., Niu G. Quantitative computed tomography analysis for stratifying the severity of Coronavirus Disease 2019. J. Pharm. Anal. 2020;10(2):123–129. doi: 10.1016/j.jpha.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu J., Pan J., Teng D., Xu X., Feng J., Chen Y.C. Interpretation of CT signs of 2019 novel coronavirus (COVID-19) pneumonia. Eur. Radiol. 2020;30(10):5455–5462. doi: 10.1007/s00330-020-06915-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen L., Liu H.G., Liu W., Liu J., Liu K., Shang J., Deng Y., Wei S. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(3):203–208. doi: 10.3760/cma.j.issn.1001-0939.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 26.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): A systematic review of imaging findings in 919 patients. AJR Am. J. Roentgenol. 2020;215(1):87–93. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 27.Bai H.X., Hsieh B., Xiong Z., Halsey K., Choi J.W., Tran T.M.L., Pan I., Shi L.B., Wang D.C., Mei J., Jiang X.L., Zeng Q.H., Egglin T.K., Hu P.F., Agarwal S., Xie F.F., Li S., Healey T., Atalay M.K., Liao W.H. Performance of radiologists in differentiating covid-19 from non-covid-19 viral pneumonia at chest CT. Radiology. 2020;296(2):E46–E54. doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cao J., Zhou J., Liao X.N., Ling G.H., Ding X., Long Q.Y. Clinical characteristics and CT signs of coronavirus disease 2019(COVID-19) in the elderly. Wuhan Daxue Xuebao Yixue Ban. 2020;41(4):551–554. [Google Scholar]
- 29.Zhong Z., Xie X., Huang W., Zhao W., Yu Q., Liu J. Chest CT findings and clinical features of coronavirus disease 2019 in children. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2020;45(3):236–242. doi: 10.11817/j.issn.1672-7347.2020.200206. [DOI] [PubMed] [Google Scholar]
- 30.Zhou Y., Yang G.D., Feng K., Huang H., Yun Y.X., Mou X.Y., Wang L.F. Clinical features and chest CT findings of coronavirus disease 2019 in infants and young children. Zhongguo Dang Dai Er Ke Za Zhi. 2020;22(3):215–220. doi: 10.7499/j.issn.1008-8830.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duan Y.N., Zhu Y.Q., Tang L.L., Qin J. CT features of novel coronavirus pneumonia (COVID-19) in children. Eur. Radiol. 2020;30(8):4427–4433. doi: 10.1007/s00330-020-06860-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Du Y.H., Jin C.W., Yang J., et al. Clinical features and CT signs of early family clustering corona virus disease 2019. J. Xi'an Jiaotong Univ. 2020;41(3):435–438. [Google Scholar]
- 33.Gao L., Zhang J.P., Du Y.H., et al. CT features of patients with imported 2019-nCov-pneumonia. J. Xian Jiaotong Univ. 2020;41(3):429–434. [Google Scholar]
- 34.Liu C.Y., Cai Y.X., Hao Z.P., et al. Chest CT comparison of ground glass opacity-like 2019 novel coronavirus pneumonia and early-stage lung carcinoma. Chin. J. Clin. Thorac. Cardiovas. Surg. 2020;27(4):376–380. [Google Scholar]
- 35.Liu M., He P., Liu H.G., Wang X.J., Li F.J., Chen S., Lin J., Chen P., Liu J.H., Li C.H. Clinical characteristics of 30 medical workers infected with new coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(3):209–214. doi: 10.3760/cma.j.issn.1001-0939.2020.03.014. [DOI] [PubMed] [Google Scholar]
- 36.Liu F, Cai ZB, Huang JS, et al. Positive SARS-CoV-2 RNA recurs repeatedly in a case recovered from COVID-19: Dynamic results from 108 days of follow-up. Pathog Dis. 2020;78(4):ftaa031. doi: 10.1093/femspd/ftaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhao K.C., Suo T., Wang Y.N., et al. Application of chest CT scans in the diagnosis and treatment of COVID-19. Medical Journal of Wuhan University. 2020 doi: 10.14188/j.1671-8852.2020.0344. Available from: https://kns.cnki.net/kcms/detail/42.1677.R.20200901.1130.002.html. [DOI] [Google Scholar]
- 38.Wang Y.F., Chen J.P., Wang X. CT image features of asymptomatic patients with novel coronavirus pneumonia. Wuhan Daxue Xuebao Yixue Ban. 2020;41(3):353–356. [Google Scholar]
- 39.Meng H., Xiong R., He R., Lin W., Hao B., Zhang L., Lu Z., Shen X., Fan T., Jiang W., Yang W., Li T., Chen J., Geng Q. CT imaging and clinical course of asymptomatic cases with COVID-19 pneumonia at admission in Wuhan, China. J. Infect. 2020;81(1):e33–e39. doi: 10.1016/j.jinf.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feng X.H., Li Z.H., Ke C.H., et al. Analysis of re-admission of patients with corona virus disease 2019 after treatment. Chin J Nosocomio. 2020;30(11):1630–1636. [Google Scholar]
- 41.Ji G.H., Huang M.H., Zhang Q., et al. CT manifestations and dynamic changes of coronavirus disease 2019. Chin J Med Imaging Technol. 2020;36(2):243–247. [Google Scholar]
- 42.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y., Bai C., Gao T., Song J., Xia P., Dong J., Zhao J., Wang F.S. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu X., Wang R.S., Qu G.Q., et al. General anatomy report of novel coronavirus pneumonia death corpse. J. Forensic Med. 2020;36(1):21–23. [Google Scholar]
- 44.Fox S.E., Akmatbekov A., Harbert J.L., Li G., Quincy Brown J., Vander Heide R.S. Pulmonary and cardiac pathology in African American patients with COVID-19: An autopsy series from New Orleans. Lancet Respir. Med. 2020;8(7):681–686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Buja L.M., Wolf D.A., Zhao B., Akkanti B., McDonald M., Lelenwa L., Reilly N., Ottaviani G., Elghetany M.T., Trujillo D.O., Aisenberg G.M., Madjid M., Kar B. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): Report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc. Pathol. 2020;48:107233. doi: 10.1016/j.carpath.2020.107233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barton L.M., Duval E.J., Stroberg E., Ghosh S., Mukhopadhyay S. COVID-19 Autopsies, Oklahoma, USA. Am. J. Clin. Pathol. 2020;153(6):725–733. doi: 10.1093/ajcp/aqaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tian S., Xiong Y., Liu H., Niu L., Guo J., Liao M., Xiao S.Y. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod. Pathol. 2020;33(6):1007–1014. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhao X.Q., Xing Z.H., Zhang S., et al. The first chest CT imaging follow-up of COVID-19 patients after discharge. Jiangsu Med J. 2020;46(6):553–556. [Google Scholar]
- 49.Jin C., Tian C., Wang Y., Wu C.C., Zhao H., Liang T., Liu Z., Jian Z., Li R., Wang Z., Li F., Zhou J., Cai S., Liu Y., Li H., Li Z., Liang Y., Zhou H., Wang X., Ren Z., Yang J. A pattern categorization of CT findings to predict outcome of COVID-19 pneumonia. Front. Public Health. 2020;8:567672. doi: 10.3389/fpubh.2020.567672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Erturk S.M. CT of coronavirus disease (COVID-19) pneumonia: A reference standard is needed. AJR Am. J. Roentgenol. 2020;215(1):W20. doi: 10.2214/AJR.20.23286. [DOI] [PubMed] [Google Scholar]
- 51.Li Y., Xia L. Coronavirus disease 2019 (COVID-19): Role of chest CT in diagnosis and management. AJR Am. J. Roentgenol. 2020;214(6):1280–1286. doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 52.Hope M.D., Raptis C.A., Shah A., Hammer M.M., Henry T.S. A role for CT in COVID-19? What data really tell us so far. Lancet. 2020;395(10231):1189–1190. doi: 10.1016/S0140-6736(20)30728-5. [DOI] [PMC free article] [PubMed] [Google Scholar]