Abstract
Background
Inflammatory bowel disease (IBD) is a chronic and debilitating illness associated with psychosocial comorbidities. Adolescents are vulnerable to the additive stress of managing IBD and navigating developmental milestones. Psychosocial factors, such as catastrophizing, illness stigma, illness uncertainty, and illness-related shame, often contribute to perceived stress in chronic illnesses. However, the combination of these variables on perceived stress in adolescents with IBD has not been examined.
Methods
Participants completed a cross-sectional online self-report survey. Model 4 of PROCESS Macro in SPSS was used to test the parallel mediation model of the relationship between disease severity and perceived stress using catastrophizing, stigma, uncertainty, and shame as mediators using 10,000 bootstrap samples. T-tests were run to assess systematic differences in the dependent variable between subjects.
Results
One hundred and thirty-one adolescents (Mage = 18.95 years; 100 females) completed the survey. Females had higher stress scores than males (P =0.002), and there were no difference in stress between younger and older participants (P = 0.085), location (P = 0.484), or IBD type (P = 0.515). The total effect of disease stress on perceived stress operating through the mediators was significant, b = 0.168, SE = 0.028, 95% CI [0.112, 0.224]. Helplessness catastrophizing, illness uncertainty, and illness-related shame, but not illness stigma, were equally strong, positive mediators.
Conclusions
The present results suggest that helplessness catastrophizing, illness uncertainty, and illness-related shame are central elements to target in stress interventions for adolescents with IBD.
Keywords: Adolescents, Inflammatory Bowel Disease, Mediation, Perceived stress, Psychosocial
Introduction
Inflammatory bowel disease (IBD) is an umbrella term for Crohn’s disease (CD) and ulcerative colitis (UC). IBD is a chronic autoimmune disorder of the digestive tract with symptoms (e.g., diarrhea, rectal bleeding, fatigue) associated with significant perceived stress and uncertainty (1,2). Living with IBD often imposes restrictive lifestyle changes, such as diet constraints and activity limitations, leading to fewer social interactions, increased perceived stress, and illness stigmatization (3–6). Importantly, adolescents with IBD must navigate developmental milestones (e.g., developing mature friendships, exploring sexuality, consolidating self-identity, becoming independent, and moving away for school or work) while managing their disease which is painful, unpredictable, and embarrassing (7–10). This may culminate in feelings of helplessness, stress, negative self-image, social isolation, and school absenteeism (7), prompting calls for integrated biopsychosocial management of adolescent IBD (11,12).
A Common-Sense Model (CSM) of illness representations (13) can be used to conceptualize how psychosocial variables affect adolescent IBD perceived stress. The CSM posits that illness perceptions (e.g., stigma, shame) mediate the relationship between illness stimuli (e.g., disease severity) and illness outcomes (e.g., perceived stress). While depression is considered a primary outcome of IBD disease severity, it is important to note that stress may precede depression and the onset of first depressive episodes (14–17). During adolescence, perceived stress can stem from peer influence, familial conflict, academic workload, and self-esteem struggles (18). Consistent with the CSM, disease severity has a direct influence on IBD illness perceptions; illness perceptions then had a direct influence on stress (19).
To augment the emerging IBD disease related research, four theoretically relevant psychosocial variables (catastrophizing, illness uncertainty, illness stigma, and illness-related shame) were investigated as mediators between disease severity and perceived stress. Catastrophizing is a state of negative cognitive appraisals intensifying adverse experiences, which includes thoughts such as “If I fail this test, I will not graduate, and I will be a total failure” (20). IBD severity is positively associated with higher catastrophizing (21–23), and catastrophizing impairs patients’ quality of life (24). Illness uncertainty contributes to patients’ perceived stress; patients report uncertainty as to how they might manage various lifestyle activities or feelings of threat given the unpredictable nature of IBD symptoms, leading to negative mood states (5,7,25). There is an observed link between adolescent disease severity and depressive symptoms using parent and youth illness uncertainty (26). Next, illness stigma is based on the perception that an individual is apart from functioning in society because of their disease (27). This stigma involves a fear that others hold negative attitudes or beliefs about that individual’s disease, and stigma is associated with disease severity, anxiety, depression, and a lower quality of life in IBD (28,29). Research has also found a positive association between illness stigma and depressive symptoms in youth (30). Illness-related shame is an intense negative emotion caused by perceived failure where patients may internally criticize themselves in relation to their disease (31), and is associated with alienation, a lower quality of life, and feelings of isolation (28). Stigma and shame may be ubiquitous among IBD patients largely due to the embarrassing symptomology (e.g., uncontrollable bowel movements, flatulence, and diarrhea) of IBD (29,30). Although a heightened sense of shame is associated with an IBD diagnosis (6,32), less is known about how disease symptomology influences shame and perceived stress. Recent evidence suggests that shame mediates the relationship between disease severity and depression in adult IBD patients (33,34).
Little is known about how these psychosocial mediators combine to affect perceived stress in adolescents with IBD. The aim of the current study was to investigate the relationship between disease severity and perceived stress using catastrophizing, illness stigma, illness uncertainty, and illness-related shame as psychosocial mediators. It was predicted that all variables would significantly mediate the relationship between disease severity and perceived stress.
METHODS
Participants
This cross-sectional study was approved by the Queen’s University Health Sciences Research Board. Participants were recruited through online patient support groups (Crohn’s and Colitis Canada) and various social media platforms (Instagram, Twitter, Facebook, Reddit) and through snowball sampling. Participants were between the ages of 16 to 21 years, fluent in English, and self-identified as having been diagnosed with IBD. Adolescents reporting a major psychiatric disorder (i.e., psychosis, bipolar disorder) or a major medical condition (i.e., severe cardiac, pulmonary, renal, or hepatic disease) that might interfere with study participation were not eligible to participate.
Measures
Demographic and patient history questions were collected, including age, gender identity, ethnicity, country of residence, highest level of education attained, romantic partner status, IBD diagnosis and intervention information, and past and current access to mental health services.
Disease severity was assessed using the Inflammatory Bowel Disease Symptom Inventory Short Form (IBDSI-SF), a 26-item inventory assessing a broad range of patient-reported IBD symptoms, such as bowel symptoms, abdominal discomfort, bodily discomfort, and fatigue, developed by (35), total scores range from 0 to 95. This measure was reliable; Chronbach’s alpha (α = 0.95).
Catastrophizing was assessed by a modified version of the 13-item Pain Catastrophizing Scale (PCS; 36), referred to as the Generalized Catastrophizing Scale (GCS; 37). Items on the PCS were modified by changing the word ‘pain’ to ‘stress’, but the description of the questionnaire was not altered. The GCS (α = 0.95) is significantly correlated but not redundant with the PCS (33), indicating convergent validity with similar constructs. GCS has three subscales: rumination (α = 0.85), magnification (α = 0.83), and helplessness (α = 0.92). Total scores range from 0 to 52.
The Mishel Uncertainty in Illness Scale- Community (MUIS-C; α = 0.84, 38) is a 22-item self-report survey, asking participants to rate statements such as “I don’t know what is wrong with me,” from 0 (strongly disagree) to 4 (strongly agree); total scores range from 0 to 88.
Illness stigma was assessed using the 8-item Stigma Scale – Child (SS-C; α = 0.88; 39) questionnaire. Respondents selected from 1 (never) to 5 (very often) to questions such as, “How often do you feel people may not want to be friends with you if they know you have IBD”; scores range from 8 to 40.
The Chronic Illness-related Shame Scale (CISS; α = 0.93; 40) assessed the level of shame related with a chronic disease. Participants indicated the degree to which they relate to seven statements such as “I feel inadequate because of my illness and symptoms” with ratings from 0 (never true) to 4 (always true). Scores ranged from 0 to 28.
The Perceived Stress Scale (PSS; α = 0.87; 41) is a 10-item measure where participants responded to items such as “How often had you felt that you were unable to control the important things in your life” on a scale ranging from 0 (never) to 4 (very often); scores range from 0 to 40. Higher scores in all measures indicated higher levels of the constructs measured (disease severity, catastrophizing, uncertainty, stigma, shame, and stress).
Procedure
Questions were administered through a de-identified online survey using Qualtrics. Eligible participants checked off a box confirming their consent to participate. Completion of the survey took approximately 25 minutes. Participants could decline any questions they did not feel comfortable answering and were provided with a debriefing form outlining resources for dealing with feelings of distress.
Data Analyses
Total scores for each variable were calculated if at least 80% of the items within the relevant questionnaire were completed according to their standard scoring procedure; missing data for participants with at least 80% of the items complete were imputed using the mean of all other items completed in the questionnaire (42). T-tests assessed differences in perceived stress between age groups 16 to 18 and 19 to 21 years, gender identity, whether the participant had previously used mental health services, and whether the participant currently accessed mental health services. A one-way ANOVA assessed the differences in location and IBD disease type. Model 4 of PROCESS macro (43) for SPSS Statistics Version 25 (IBM Corp.) was used to test the parallel mediation model. If mediations of any variables with subscales were significant, the subscale mediation effects were tested.
RESULTS
One hundred and thirty-one adolescents (Mage = 18.95 years) completed the survey. As shown in Table 1, slightly older participants completed the survey and most were Caucasian females from the UK and North America, in the high school and early university years. Most participants found the study through social media platforms, had CD, and were not receiving mental health services. Based off 172 participants attempting at least one item on any of the survey questions, 23.8% of the study participants did not complete the study. Younger participants (16 to 18 years) reported similar stress (M = 22.26, SD = 6.83) to older participants (M = 24.22, SD = 6.03); t(129) = 1.73, P = 0.085. Participants had similar stress scores across locations [Canada (M = 21.58, SD = 6.59), United States (M = 23.92, SD = 6.12, United Kingdom (M = 23.97, SD = 7.15, and Other (M = 23.3, SD = 5.42); F (1,3) =.822, P = 0.484]. Females had higher stress (M = 24.39, SD = 6.20) compared to males (M = 20.15, SD = 6.33); t(125) = 3.14, P = 0.002. Participants receiving mental health services in the past had higher stress (M = 24.88, SD = 6.47) compared to participants who did not (M = 21.91, SD = 6.04); t(129) = 2.72, P = 0.007. Stress scores of participants who were accessing mental health services at survey completion (M = 24.15, SD = 6.18) did not differ scores of those not accessing services (M = 23.23, SD = 6.49); t(129) = 0.68, P = 0.501. There were no differences in stress between different IBD subtypes [CD (M = 24.06, SD = 6.17), UC (M = 22.67, SD = 5.65), and unknown IBD type (M = 23.14, SD = 6.42); F (1,2) = 0.667, P = 0.515].
Table 1.
Patient history information of participants
| n (%) | |
|---|---|
| Age | |
| 16–18 years old | 53 (40.5) |
| 19–21 years old | 78 (59.5) |
| Gender Identity | |
| Man | 27 (20.6) |
| Woman | 100 (76.3) |
| Non-binary | 3 (2.3) |
| Another gender not listed | 1 (.8) |
| Ethnicity | |
| Caucasian | 117 (89.3) |
| Hispanic/Latino | 5 (3.8) |
| Asian | 2 (1.5) |
| Black/African Canadian | 1 (.8) |
| Other/Missing | 6 (4.6) |
| Place of Residence | |
| Canada | 23 (17.6) |
| United States | 49 (37.4) |
| United Kingdom | 39 (29.8) |
| Australia | 3 (2.3) |
| New Zealand | 3 (2.3) |
| Other | 14 (10.8) |
| Education | |
| Less than high school | 7 (5.3) |
| High school/GED | 41 (31.3) |
| Some college/university | 75 (57.3) |
| College/university graduate | 6 (4.6) |
| Some graduate or professional school after college/university | 2 (1.5) |
| Disease Type | |
| Crohn’s Disease | 66 (50.4) |
| Ulcerative Colitis | 49 (37.4) |
| IBD Type Unknown | 16 (12.2) |
| Currently Receiving Mental Health Services | |
| Yes | 28 (21.4) |
| No | 103 (78.6) |
| How they Found the Study | |
| Social Media (Facebook, Instagram, Reddit, Twitter) | 115 (87.8) |
| IBD Specialist/Nurse at Hospital | 2 (1.5) |
| Hospital Support Group | 1 (.8) |
| Other | 13 (9.9) |
GED, General educational development.
Mediation Models
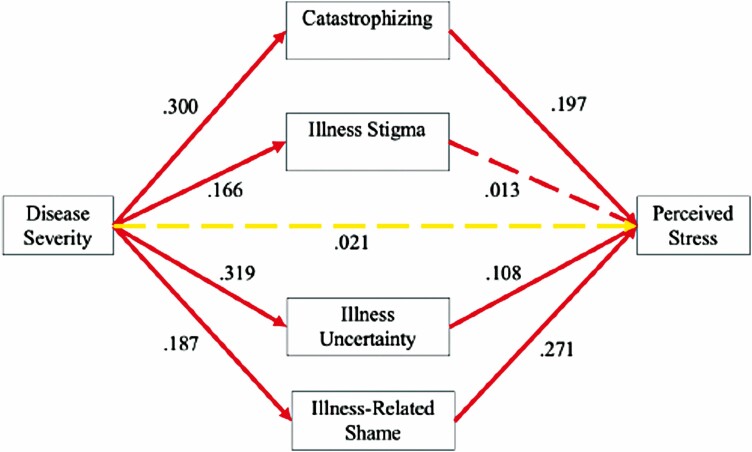
Model 4 (43) was run using 95% confidence intervals (CIs) with 10,000 bootstrap samples using unstandardized regression coefficients. The sum of the indirect and direct effects, or the total effect of disease severity on perceived stress operating through all four mediators was significant, b = 0.168, SE = 0.028, 95% CI [0.112, 0.224]. As shown in Figure 1, the direct effect of disease severity on perceived stress independent of the effects of any of the mediators was smaller and not significant; b = 0.021, SE = 0.023, 95% CI [−0.024, 0.067].
Figure 1.
The completed mediation model. Note. Solid lines represent significant effects, dotted lines represent nonsignificant effects; red represents indirect effects, and yellow represents direct effects.
The indirect effect of catastrophizing (the mediation effect of catastrophizing controlling for illness stigma, illness uncertainty, and illness-related shame) was significant; b = 0.059, SE = 0.016, 95% CI [0.032, 0.094]. Higher levels of disease severity were related to higher levels of catastrophizing, b = 0.300, SE = 0.057, 95% CI [0.187, 0.413], and controlling for disease severity, greater catastrophizing was related to higher levels of perceived stress; b = 0.197, SE = 0.035, 95% CI [0.127, 0.267]. The indirect effect of illness uncertainty was significant; b = 0.035, SE = 0.013, 95% CI [0.011, 0.063]. Higher levels of disease severity were related to higher levels of illness uncertainty, b = 0.319, SE = 0.053, 95% CI [0.216, 0.423], and controlling for disease severity, greater illness uncertainty was related to greater perceived stress; b = 0.108, SE = 0.036, 95% CI [0.037, 0.180]. The indirect effect of illness-related shame was significant; b = 0.051, SE = 0.019, 95% CI [0.019, 0.095]. Higher levels of disease severity were related to higher levels of illness-related shame, b = 0.187, SE = 0.035, 95% CI [0.119, 0.256], and controlling for disease severity, greater illness-related shame was related to higher levels of perceived stress; b = 0.271, SE = 0.075, 95% CI [0.122, 0.420]. The indirect effect of illness stigma was not significant; b = 0.002, SE = 0.012, 95% CI [−0.022, 0.025]. Higher levels of disease severity were related to higher levels of illness stigma; b = 0.166, SE = 0.034, 95% CI [0.099, 0.233]. Controlling for disease severity, illness stigma was not significantly related to perceived stress; b = 0.013, SE = 0.064, 95% CI [−0.114, 0.141].
The magnitude of the indirect effects of catastrophizing and illness uncertainty did not differ; b = 0.025, SE = 0.019, 95% CI [−0.010, 0.064]. The magnitude of the indirect effects of catastrophizing and illness-related shame did not differ; b = 0.008, SE = 0.023, 95% CI [−0.039, 0.052]. The magnitude of the indirect effects of illness uncertainty and illness-related shame did not differ; b = −0.016, SE = 0.024, 95% CI [−0.067, 0.027]. However, the magnitude did differ between catastrophizing and illness stigma, b = 0.057, SE = 0.021, 95% CI [0.020, 0.101], illness uncertainty and illness stigma, b = 0.032, SE = 0.017, 95% CI [0.001, 0.070], and illness-related shame and illness stigma, b = 0.049, SE = 0.028, 95% CI [−0.110, −0.003]. Catastrophizing, illness uncertainty, and illness-related shame were equally strong mediators.
These findings suggest that general catastrophizing, illness uncertainty, and illness-related shame, but not illness stigma, mediate the relationship between disease severity and perceived stress. Given that the mediation effect through generalized catastrophizing was significant, a parallel mediation model was run with the subscales.
The sum total effect of disease severity on perceived stress operating through rumination, magnification, and helplessness was significant, b = 0.165, SE = 0.029, 95% CI [0.108, 0.222], as was the direct effect of disease severity on perceived stress independent of the effects of any of the mediators; b = 0.068, SE = 0.025, 95% CI [0.019, 0.117]. The indirect effects of rumination and magnification were not significant; respectively, b = 0.002, SE = 0.019, 95% CI [−0.029, 0.045]and b = 0.019, SE = 0.015, 95% CI [−0.007, 0.053]. Whereas higher levels of disease severity were related to higher levels of rumination, b = 0.086, SE = 0.019, 95% CI [0.049, 0.123], higher levels of rumination were not related to higher perceived stress; b = 0.019, SE = 0.201, 95% CI [−0.379, 0.417]. Similarly, although higher levels of disease severity were significantly related to higher levels of magnification, b = 0.057, SE = 0.015, 95% CI [0.028, 0.087], higher scores of magnification were not related to higher scores of perceived stress; b = 0.329, SE = 0.206, 95% CI [−0.078, 0.737]. The indirect effect of helplessness was significant; b = 0.077, SE = 0.024, 95% CI [0.033, 0.128]. Higher levels of disease severity were related to higher helplessness, b = 0.156, SE = 0.029, 95% CI [0.098, 0.213], and higher helplessness was related to higher levels of perceived stress; b = 0.494, SE = 0.124, 95% CI [0.249, 0.739]. These findings suggest that helplessness is salient with higher levels of IBD disease severity being associated with greater perceived stress through helplessness.
Discussion
This study aimed to discover the pertinent psychosocial mediators between disease severity and perceived stress using the CSM as a theoretical framework. It adds to an understanding of adolescent IBD by showing that the variables of helplessness, illness uncertainty, and illness shame mediated the relationship between disease severity and perceived stress. Broadly, the present results support the CSM and underscore the importance of psychosocial variables in affecting perceived stress in adolescent IBD populations. As there is significant stress involved with having IBD during a sensitive developmental period, our results emphasize the importance of targeting these factors for interventions.
As in previous research (44), catastrophizing was a mediator and strongly correlated with stress. Helplessness was the mediator between disease severity and stress. Helplessness is considered a secondary stress appraisal where an individual feels overwhelmed by circumstances in attempting to address their stress (45). In this current study, when adolescents with IBD reported helplessness in managing their symptoms it is associated with greater stress. Such thought patterns include worrying whether their stress will end, feeling like they cannot endure their position any longer, and feeling helpless to stop their stress (36). Given that catastrophizing and coping mechanisms can be altered through cognitive-behavioural exposure such as de-catastrophizing therapy that examines and challenges thinking patterns that inflame strong negative emotional responses (46). The present results support an increased focus on modalities to mitigate catastrophizing.
As in other research in non-IBD conditions, illness uncertainty was also associated with increased stress. Uncertainty about symptoms, treatments, and outcomes was a predictor of stress in hospitalized patients (47), and both disease activity and illness uncertainty predicted anxiety and depression in patients with ankylosing spondylitis (48). Addressing illness uncertainty is important; illness uncertainty was shown to be reduced following cognitive behavioural therapy in patients with functional somatic syndrome (49).
Illness-related shame was another important mediator in our study. In related research, shame was associated with feelings of stress, avoidance of social situations, and decreased intimacy and quality of relationships (32). Shame was also associated with suicidality in body dysmorphic and obsessive-compulsive disorder (50) and with depressive symptoms in IBD patients (32,40). Shame is distinct because it involves not only how one is perceived as different by others, but also how one internally devaluates and criticizes themselves (51,52). Perhaps internal devaluation and criticism that is specific to shame may drive the increase in perceived stress seen here. Indeed, adolescents with chronic health conditions view their disease as extensions of their identity and devaluation by their illness ultimately increases shame and perceived stress (9,53). Compassion-based interventions may be used to reduce illness shame (40).
Although there was an association between disease severity and stigma, illness-related stigma was not a mediator. Other research studying illness stigma points to high variability, where some individuals are largely unaffected by stigma, while others perceive stigma as stressful (54,55). In this study, shame may be a construct incorporating stigma; shame accounts for greater variance in perceived stress in adolescents compared to stigma.
Given that the analyses were cross-sectional, causal conclusions are prohibited. Longitudinal designs will be required for a stronger explanation of how perceived stress is predicted by disease severity and psychosocial mediators. Additionally, there were systematic differences in perceived stress scores across demographic variables. Investigating the systematic differences in perceived stress in the current sample was not feasible due to sample size discrepancy between males and females. While our sample of IBD patients was not medically diagnosed, our sampling strategy provided greater access to as many patients as possible; we did not want to restrict ourselves to clinic patients. In so doing, the generalizability of the results provides greater generalizability to the IBD population. The GCS is also not widely adopted, despite being significantly correlated with the PCS (37), further work on the psychometric properties and validation of this scale is warranted. Finally, given most of the participants were Caucasian, the current study lacks representation of minority populations; future research should emphasize equitable recruitment practises to obtain a diverse sample.
Contributor Information
Adam Sunavsky, Department of Psychology, Queen’s University, Kingston, Ontario, Canada.
Julia Moreau, Department of Psychology, Queen’s University, Kingston, Ontario, Canada.
Dean A Tripp, Departments of Psychology, Anesthesiology and Urology, Queen’s University, Kingston, Ontario, Canada.
Funding
No funding sources.
AUTHOR CONTRIBUTIONS
A.S. authored the manuscript, ran data analyses and data collection. J.M. collected data and provided editing on the manuscript. D.T. supervised and edited the manuscript at all stages.
CONFLICT OF INTEREST
The authors have no conflicts of interest.
References
- 1. Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med 2009;361(21):2066–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Casati J, Toner BB, de Rooy EC, et al. Concerns of patients with inflammatory bowel disease: a review of emerging themes. Dig Dis Sci 2000;45(1):26–31. [DOI] [PubMed] [Google Scholar]
- 3. Cervesi C, Battistutta S, Martelossi S, et al. Health priorities in adolescents with inflammatory bowel disease: physicians’ versus patients’ perspectives. J Pediatr Gastroenterol Nutr 2013;57(1):39–42. [DOI] [PubMed] [Google Scholar]
- 4. Keeton RL, Mikocka-Walus A, Andrews JM. Concerns and worries in people living with inflammatory bowel disease (IBD): A mixed methods study. J Psychosom Res 2015;78(6):573–8. [DOI] [PubMed] [Google Scholar]
- 5. Fourie S, Jackson D, Aveyard H. Living with inflammatory bowel disease: a review of qualitative research studies. Int J Nurs Stud 2018;87:149–56. [DOI] [PubMed] [Google Scholar]
- 6. Casati J, Toner BB. Psychosocial aspects of inflammatory bowel disease. Biomed Pharmacother 2000;54(7):388–93. [DOI] [PubMed] [Google Scholar]
- 7. Nicholas DB, Otley A, Smith C, et al. Challenges and strategies of children and adolescents with inflammatory bowel disease: a qualitative examination. Health Qual Life Outcomes 2007;5:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reed-Knight B, Mackner LM, Crandall WV. Psychological aspects of inflammatory bowel disease in children and adolescents. In: Mamula P, Grossman A, Baldassano R, Kelsen J, Markowitz J, eds. Pediatric Inflammatory Bowel Disease. Springer, Cham: Springer International Publishing AG; 2017:615–23. [Google Scholar]
- 9. Stapersma L, van den Brink G, van der Ende J, et al. Illness perceptions and depression are associated with health-related quality of life in youth with inflammatory bowel disease. Int J Behav Med 2019;26(4):415–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cunningham C, Drotar D, Palermo TMet al. Health-related quality of life in children and adolescents with inflammatory bowel disease. Children’s Healthcare 2007;36:29–43. [Google Scholar]
- 11. Faust AH, Halpern LF, Danoff-Burg S, et al. Psychosocial factors contributing to inflammatory bowel disease activity and health-related quality of life. Gastroenterol Hepatol (N Y) 2012;8(3):173–81. [PMC free article] [PubMed] [Google Scholar]
- 12. Szigethy EM, Allen JI, Reiss M, et al. White paper AGA: the impact of mental and psychosocial factors on the care of patients with inflammatory bowel disease. Clinical Gastroenterology and Hepatology 2017;15:986–97. [DOI] [PubMed] [Google Scholar]
- 13. Leventhal H, Benyamini Y, Brownlee S, et al. Perceptions of health and illness: current research and applications. Illness representations: theoretical foundations. London: Harwood Publishers Ltd, 1997:19–45. [Google Scholar]
- 14. Cohen S. Contrasting the hassles scale and the perceived stress scale: who’s really measuring appraised stress? American Psychologist 1986;41:716–18. [Google Scholar]
- 15. Naicker K, Galambos NL, Zeng Y, et al. Social, demographic, and health outcomes in the 10 years following adolescent depression. J Adolesc Health 2013;52(5):533–8. [DOI] [PubMed] [Google Scholar]
- 16. Zhang B, Yan X, Zhao F, et al. The relationship between perceived stress and adolescent depression: The roles of social support and gender. Social Indicators Research 2015;123:501–18. [Google Scholar]
- 17. Stroud CB, Davila J, Moyer A. The relationship between stress and depression in first onsets versus recurrences: a meta-analytic review. J Abnorm Psychol 2008;117(1):206–13. [DOI] [PubMed] [Google Scholar]
- 18. Moksnes UK, Bradley Eilertsen ME, et al. The association between stress, self‐esteem and depressive symptoms in adolescents. Scand J Psychol 2016;57(1):22–9. [Google Scholar]
- 19. Zhang M, Hong L, Zhang T, et al. Illness perceptions and stress: mediators between disease severity and psychological well-being and quality of life among patients with Crohn’s disease. Patient Prefer Adherence 2016;10:2387–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sullivan MJ. The communal coping model of pain catastrophising: Clinical and research implications. Canadian Psychology 2012;53:32. [Google Scholar]
- 21. Chaves JF, Brown JM. Spontaneous cognitive strategies for the control of clinical pain and stress. J Behav Med 1987;10(3):263–76. [DOI] [PubMed] [Google Scholar]
- 22. Hirsh AT, George SZ, Riley JL 3rd, et al. An evaluation of the measurement of pain catastrophizing by the coping strategies questionnaire. Eur J Pain 2007;11(1):75–81. [DOI] [PubMed] [Google Scholar]
- 23. Edman JS, Greeson JM, Roberts RS, et al. Perceived stress in patients with common gastrointestinal disorders: associations with quality of life, symptoms and disease management. Explore (NY) 2017;13(2):124–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Katz L, Tripp DA, Ropeleski M, et al. Mechanisms of quality of life and social support in inflammatory bowel disease. J Clin Psychol Med Settings 2016;23(1):88–98. [DOI] [PubMed] [Google Scholar]
- 25. Wolfe BJ, Sirois FM. Beyond standard quality of life measures: the subjective experiences of living with inflammatory bowel disease. Qual Life Res 2008;17(6):877–86. [DOI] [PubMed] [Google Scholar]
- 26. Baudino MN, Gamwell KL, Roberts CM, et al. Disease severity and depressive symptoms in adolescents with inflammatory bowel disease: the mediating role of parent and youth illness uncertainty. J Pediatr Psychol 2019;44(4):490–8. [DOI] [PubMed] [Google Scholar]
- 27. Goffman E. Stigma: Notes on the management of spoiled identity. New York: Simon and Schuster, 2009. [Google Scholar]
- 28. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol 2001;27:363–85. [Google Scholar]
- 29. Taft TH, Keefer L, Leonhard C, et al. Impact of perceived stigma on inflammatory bowel disease patient outcomes. Inflamm Bowel Dis 2009;15(8):1224–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gamwell KL, Baudino MN, Bakula DM, et al. Perceived illness stigma, thwarted belongingness, and depressive symptoms in youth with inflammatory bowel disease (IBD). Inflamm Bowel Dis 2018;24(5):960–5. [DOI] [PubMed] [Google Scholar]
- 31. Tangney JP, Miller RS, Flicker L, et al. Are shame, guilt, and embarrassment distinct emotions? J Pers Soc Psychol 1996;70(6):1256–69. [DOI] [PubMed] [Google Scholar]
- 32. Hall NJ, Rubin GP, Dougall A, et al. The fight for ‘health-related normality’: a qualitative study of the experiences of individuals living with established inflammatory bowel disease (ibd). J Health Psychol 2005;10(3):443–55. [DOI] [PubMed] [Google Scholar]
- 33. Farrell D, McCarthy G, Savage E. Self-reported symptom burden in individuals with inflammatory bowel disease. J Crohns Colitis 2016;10(3):315–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Trindade IA, Ferreira C, Pinto-Gouveia J. Shame and emotion regulation in inflammatory bowel disease: Effects on psychosocial functioning. J Health Psychol 2020;25(4):511–21. [DOI] [PubMed] [Google Scholar]
- 35. Sexton KA, Walker JR, Targownik LE, et al. The inflammatory bowel disease symptom inventory: a patient-report scale for research and clinical application. Inflamm Bowel Dis 2019;25(8):1277–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychological Assessment 1995;7:524–532. [Google Scholar]
- 37. Gates J. Development and Feasibility Trial of a Cognitive Behavioural Self-Management Program for Inflammatory Bowel Disease (Doctoral dissertation). Kingston, CA: Queen’s University Library; 2019;1–272. [Google Scholar]
- 38. Mishel MH. Adjusting the fit: development of uncertainty scales for specific clinical populations. West J Nurs Res 1983;5(4):355–70. [DOI] [PubMed] [Google Scholar]
- 39. Austin JK, MacLeod J, Dunn DW, et al. Measuring stigma in children with epilepsy and their parents: instrument development and testing. Epilepsy Behav 2004;5(4):472–82. [DOI] [PubMed] [Google Scholar]
- 40. Trindade IA, Ferreira C, Pinto-Gouveia J. Chronic illness-related shame: development of a new scale and novel approach for IBD patients’ depressive symptomatology. Clin Psychol Psychother 2017;24(1):255–63. [DOI] [PubMed] [Google Scholar]
- 41. Cohen S. Perceived stress in a probability sample of the United States. In S Spacapan, S Oskamp, eds. Thousand Oaks, CA: Sage Publications, Inc, 1988:31–67. [Google Scholar]
- 42. Tabachnick BG, Fidell LS, Ullman JB. Using multivariate statistics. Boston, MA: Pearson, 2007. [Google Scholar]
- 43. Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper], 2012. <https://www.afhayes.com/public/process2012.pdf> [Google Scholar]
- 44. van Tilburg MA, Claar RL, Romano JM, et al. Role of coping with symptoms in depression and disability: comparison between inflammatory bowel disease and abdominal pain. J Pediatr Gastroenterol Nutr 2015;61(4):431–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Folkman S, Lazarus RS. Stress, appraisal, and coping. New York: Springer Publishing Company, 1984. [Google Scholar]
- 46. Vlaeyen JW, De Jong JR, Onghena P, et al. Can pain-related fear be reduced? The application of cognitive-behavioural exposure in vivo. Pain Res Manag 2002;7(3):144–53. [DOI] [PubMed] [Google Scholar]
- 47. Mishel MH. Perceived uncertainty and stress in illness. Res Nurs Health 1984;7(3):163–71. [DOI] [PubMed] [Google Scholar]
- 48. Lim JM, Cho OH. The influence of disease activity and uncertainty on anxiety and depression in patients with ankylosing spondylitis. Journal of Korean Academic Society of Home Health Care Nursing 2017;24:61–8. [Google Scholar]
- 49. Christensen SS, Frostholm L, Ørnbøl E, et al. Changes in illness perceptions mediated the effect of cognitive behavioural therapy in severe functional somatic syndromes. J Psychosom Res 2015;78(4):363–70. [DOI] [PubMed] [Google Scholar]
- 50. Weingarden H, Renshaw KD, Wilhelm S, et al. Anxiety and shame as risk factors for depression, suicidality, and functional impairment in body dysmorphic disorder and obsessive compulsive disorder. J Nerv Ment Dis 2016;204(11):832–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gilbert P. The evolution of social attractiveness and its role in shame, humiliation, guilt and therapy. Br J Med Psychol 1997;70 (Pt 2):113–47. [DOI] [PubMed] [Google Scholar]
- 52. Lewis M. The role of the self in shame. Social Research: An International Quarterly 2003;70:1181–204. [Google Scholar]
- 53. Wicks S, Berger Z, Camic PM. It’s how I am. it’s what I am. it’s a part of who I am: A narrative exploration of the impact of adolescent-onset chronic illness on identity formation in young people. Clin Child Psychol Psychiatry 2019;24(1):40–52. [DOI] [PubMed] [Google Scholar]
- 54. Rüsch N, Lieb K, Bohus M, et al. Self-stigma, empowerment, and perceived legitimacy of discrimination among women with mental illness. Psychiatr Serv 2006;57(3):399–402. [DOI] [PubMed] [Google Scholar]
- 55. Watson AC, Corrigan P, Larson JE, et al. Self-stigma in people with mental illness. Schizophr Bull 2007;33(6):1312–8. [DOI] [PMC free article] [PubMed] [Google Scholar]