Abstract
Background:
The treatment of distal femur fractures represents a challenging task. General and local factors, including bone quality, articular surface involvement, fracture comminution, associated soft tissue injuries and ultimately fixation system, all play a role in the final clinical outcome. Current surgical approaches often undermine patellar vascularization and integrity of the extensor apparatus, not guaranteeing sufficient visualization of the medial condyle. This technical note presents the efficacy and safety of a new surgical technique to address distal femoral fractures.
Methods:
The original “swashbuckler” surgical approach was modified in order to obtain a better visualization of the lateral and medial femoral condyles without affecting the knee extensor mechanism and the anastomotic arterial supply of the patella. This modified surgical approach was utilized in a consecutive series of patients presenting with a AO Foundation/Orthopaedic Trauma Association (AO/OTA) 33 distal femur or periprosthetic fracture of the knee. The last follow-up functional outcome was recorded according to Sanders scoring system.
Results:
Twelve patients with a mean age of 67, 8 years were included in this series. The same, modified “swashbuckler” surgical approach was applied in all cases. Multiple internal fixation techniques, including a single lateral plate, a combination of a lateral and medial plate, a single lateral plate associated with lag screws, were used to obtain a satisfactory stabilization of the fracture site. All patients were reviewed at a minimum one-year follow up (median 15 months): all patients returned to their previous life style or work activity; average Sanders Score was 34.9. No major intraoperative or postoperative complications were recorded.
Conclusions:
The modified swashbuckler approach allows anatomical reduction and appropriate fixation with a theoretically reduced severance of the blood supply to the patella and preserves the integrity of extensor mechanism. (www.actabiomedica.it)
Keywords: distal femur fracture, swashbuckler approach, open reduction internal fixation
Background
The treatment of distal femur fractures represents a challenging task, as the outcome is influenced by numerous factors: bone quality, patient’s age, articular surface involvement, presence of small fragments, fixation system and associated soft tissue injuries, all play a role in the final clinical result (1, 2). Traditionally, obtaining an anatomical reduction is a priority that must be achieved without compromising the soft tissues and knee vascularization [3]. In addition to classical fractures, trauma surgeons are often asked to treat complex distal femur periprosthetic fractures or other complicated cases, such as non-unions or malunions. Different strategies have been described to solve these challenges, as the choice of an adequate surgical approach represents the first step to achieve satisfying reduction and fixation (4, 5).
The aim of this study is to present a modification of the classical “swashbuckler” approach to the distal femur, highlighting its main features when compared to the other approaches and presenting the clinical results in a retrospective case series (6).
Methods
All patients aged 18 years and older who presented with a distal femoral fracture at the first author Institution between January 2017 and December 2019 were potentially eligible for study. We retrospectively queried our institutional surgical procedures and outpatient consultation database. Only patients with distal femoral fracture who underwent open reduction and internal fixation (ORIF) through a modified “swashbuckler” approach were included. The pre-operative radiologic images of all the eligible patients were obtained from the Picture Archiving and Communication System (PACS, GE Healthcare, USA) and examined in at least two standard projections (anteroposterior and lateral views of the distal femur and knee); a computerized tomography (CT) scan allowing 3D reconstruction was performed in all cases. There were no differences in the surgical approach between different surgeons. We did not perform any damage control procedure and all procedures were performed in a single-stage setting. The fracture type was classified according to the AO Foundation/Orthopaedic Trauma Association (AO/OTA) classification system (7). Periprosthetic fractures of the distal femur were classified according to the Lewis and Rorabeck Classification (8). Patient characteristics at the time of fracture were obtained from hospital files, including data on age, gender, weight, risk factors and comorbidities. Patients were followed for a minimum of 12 months postoperatively. Each follow up (FU) visit consisted of an outpatient consultation with a careful clinical and radiological examination (two weight-bearing anteroposterior and lateral radiographic projections of the distal femur including the knee) at an interval of 1, 3, 6, 12 months postoperatively and thereafter depending on the need of further control. Knee range of motion (ROM) at the last follow-up was recorded and results grouped into 4 sets: less than 90°, between 90° and 100°, between 101° and 119° and finally greater than 120°. Clinical outcomes and complications, such as infections, implant failure, osteolysis, bone collapse, skin necrosis, knee stiffness and quadriceps hypotrophic changes were all recorded. The final outcome was classified according to the functional evaluation scoring system described by Sanders et al (9): this scoring system takes into consideration the functional performance of patients as well as rate of fatigue failure of the construct after fixation of distal femur fractures; the outcome was defined as excellent (36 - 40 points), good (26 - 35 points), fair (16 - 25 points) and poor (0 - 15 points).
Description of the modified swashbuckler approach
The patient was placed supine onto a radiolucent table with a roll beneath the knee in order to maintain a flexion of approximately 30° of both hip and knee. A radiolucent bump was also placed under the ipsilateral buttock to avoid excessive external rotation of the lower limb. In order to prevent quadriceps medial retraction and avoid ischemic damage to the tissues, no tourniquet was used (8). Starting at the lateral aspect of the tibial tuberosity, a blunt incision, which maintained a distance of about 2 cm from the lateral border of the patellar tendon, was made first; at the base of the patella, the incision deviated slightly, aiming for the posterior depression of the vastus lateralis until it reached the anterolateral aspect of the thigh, about 5 fingerbreadths from the patella (Figure 1); the incision continued along thigh anterolateral aspect as proximal as needed. Subsequently, the approach was addressed from its proximal to its distal sections. The incision was first extended deep to the quadriceps fascia, which was incised, exposing the quadriceps muscle belly. The iliotibial band was then bluntly separated from the vastus lateralis muscle and retracted laterally. The lateral intermuscular septum, which separates the anterior and posterior compartments of the thigh, usually relates directly to the iliotibial band distally at the level of the patella: a blunt dissection was used to divide the septum from the vastus lateralis until the anterolateral aspect of femoral shaft is exposed and visualized according to the surgeon’s need. After the vastus lateralis has been detached from the lateral intermuscular septum, Hohmann retractors were used to displace the quadriceps muscle medially and to expose distal femur. The superior lateral geniculate artery was identified before it joins the anastomotic lateral circle and was ligated. The distal extension of the subcutaneous dissection must be performed carefully and precisely to minimize the disruption of the patellar arterial supply. Parapatellar arthrotomy is performed at least 2 cm from the lateral patellar margin in order to preserve the integrity of the peripatellar vascular anastomotic ring (Figure 2). The integrity of the lateral descending and the transverse infrapatellar artery are thought to be pivotal in maintaining patellar vascularization on both sides of the anastomotic ring. The lateral inferior geniculate artery, which crosses the surgical incision perpendicularly at the height of the lateral meniscus, was always ligated. We recommend preserving, if possible, the anterior tibial recurrent artery which usually crosses the surgical field at the height of the tibial tuberosity, in order to maintain a better vascularization of the peripatellar anastomotic ring (9, 10). If a wider visualization of the medial side of the distal femur is required, the vastus intermedius muscle could be stripped from the femoral anterior cortex, as there are no attachments distally (Figure 3). The last step to increase exposure of the medial condyle was to bend the knee few degrees in association with a medial sliding of the extensor apparatus in order to avoid unnecessary stress at the fracture site. Adductor magnus and biceps femoris brevis muscles usually remained intact at the posterior aspect of the femur, as there is no need to further expose both these structures. A retractor is usually useful to move the patella medially. Before skin suture, the retinaculum is closed with absorbable sutures with special attention not to damage the lateral circulatory anastomosis of the patellar network.
Figure 1.
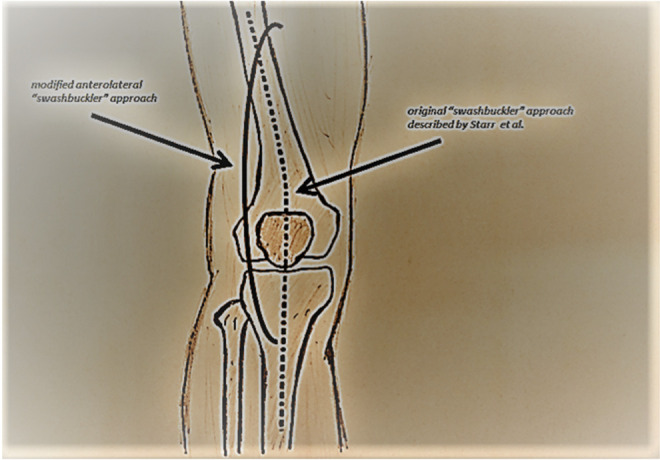
Modified anterolateral swashbuckler approach: a smooth curve incision which distally maintains a distance of about 2 cm from the lateral border of the patellar tendon.
Figure 2.
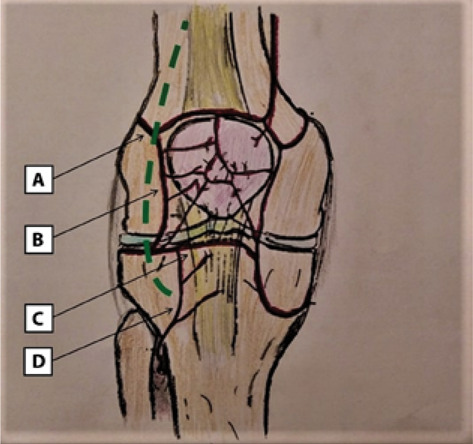
a. Lateral Superior Genicular Artery; b. Lateral Ascending Parapatellar Artery; c. Trasverse Infrapatellar Artery; d. Anterior Tibial Reccurent Artery. The superior lateral geniculate artery is ligated, whereas the lateral ascending artery, the transverse infrapatellar and the anterior tibial recurrent artery should be preserved.
Figure 3.
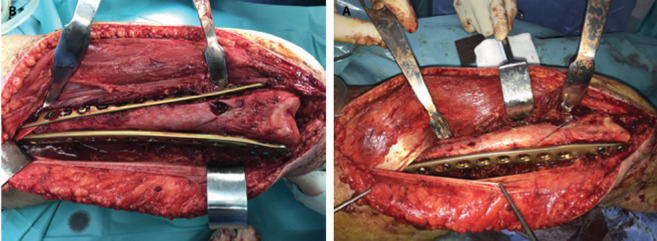
The vastus intermedius is stripped from the femoral anterior cortex.
Postoperative management
A single daily dose of low-molecular-weight heparin12 hours after the operation was administered as a prophylaxis to prevent deep venous thrombosis of lower extremities. No hemovac drain was placed in any joint. The skin stitches were removed two weeks after the procedure or later if the surgical wound has not healed. Our standard protocol includes toe touch weight bearing for the first 4 weeks, then partial weight bearing (15-20 kg) for the following 2 weeks, and, finally, full weight bearing was allowed 6-8 weeks post-operatively. In patients number 7, 9, 10 and 12 (Table 1), partial weight-bearing was prolonged to 6 weeks due to the advanced age. A knee brace was not used in this series; ROM exercises were recommended starting from postop day 1. During hospitalization, patients underwent two, 50 minutes physiotherapy sessions each day. Patients aged 65 years or older were discharged to a nursing facility, while younger patients were discharged at home. All patients underwent physiotherapy outpatient sessions after discharge.
Table 1.
Injury characteristics of the patients.
| Case | Age (Years) | Gender | Diagnosis | Treatment | Follow-up (months) | Major complications | Sanders Scoring System |
|---|---|---|---|---|---|---|---|
| 1 | 18 | M | AO 33 C1 | Lateral plate | 24 | None | 40 |
| 2 | 64 | F | AO 33 B2 | Media plate & lag screws | 20 | None | 37 |
| 3 | 66 | F | LR 2 | Lateral & medial plate | 16 | Anterior Knee Pain | 34 |
| 4 | 36 | M | AO 33 A3 | Lateral & medial plate | 14 | None | 40 |
| 5 | 72 | F | AO 33 B2 | Media plate & lag screws | 12 | None | 36 |
| 6 | 74 | F | AO 33 A3 | Lateral plate | 20 | None | 33 |
| 7 | 90 | F | LR 2 | Lateral & medial plate | 12 | Anterior Knee Pain | 34 |
| 8 | 82 | F | AO 33 C3 | Lateral & medial plate | 12 | None | 37 |
| 9 | 90 | F | AO 33 A3 | Lateral & medial plate | 12 | None | 28 |
| 10 | 88 | F | LR2 | Media plate & lag screws | 12 | None | 34 |
| 11 | 45 | F | AO 33 A3 | Lateral plate | 12 | None | 35 |
| 12 | 89 | F | AO 33 A2 | Lateral & medial plate | 13 | None | 30 |
Results
The demographic data are illustrated in Table 2. Two males and ten females with a mean age of 67,8 (18 ~90) years were included in our study. All were closed fractures. The median delay from injury to surgical procedure was 2,8 (1~6) days. None of the patients had any neurological or vascular deficit at the time of admission. After a median follow-up of 14,9 (12~24) months, all patients regained their activities of daily living. No cases of major complications as infections, plate breakage or loosening, varus collapse, bone reabsorption were recorded. Three patients were treated with lateral plating, three patients with medial plating and lag screws and 6 patients with dual-plating (lateral and medial) of the distal femur. Two patients who sustained a periprosthetic fracture complained of anterior knee pain since their first FU consultation: during further investigation, it appeared that both patients had anterior knee pain previous to the traumatic event, as a complication of the original total knee arthroplasty (TKA) procedure. All incisions were healed at the time of final FU. The postoperative joint function was rated according to the functional evaluation scoring system described by Sanders (9): 4 cases were rated excellent, 8 cases good, no cases had a fair or poor score. The mean score was 34,8 points (30 ~40). Among the patients, 7 had maximal flexion of more than 120°, 5 patients had flexion between 90° and 120°, no patient showed a flexion below 90°.
Table 2.
General information of the patients.
| Item | |
|---|---|
| Gender (male/female) | 2/10 |
| Mean age (years) | 67,8 |
| Fracture region (left/right) | 6/6 |
| Injury cause | |
| Vehicular accidents | 2 |
| Fall injuries | 10 |
| AO/OTA classification: 33 | |
| A2 | 1 |
| A3 | 4 |
| B2 | 1 |
| C1 | 2 |
| C3 | 1 |
| Rorabeck-Lewis classification of supracondylar periprosthetic femoral fracture (Type II) | 3 |
Discussion
This study showed that the modification of the classical “swashbuckler approach” has allowed for an appropriate internal fixation of distal femoral fractures: the rate of complications, related to the surgical approach, was very low.
Displaced or comminuted distal femur fractures require anatomic reduction of the articular surface since literature agrees that articular incongruity leads to poor outcomes (10). Due to the combination of an increased life expectancy and younger patients undergoing TKA, periprosthetic fractures of the distal femur are no longer a rare event. According to a recent study, up to 5% of primary total knee arthroplasty patients and up to 30% of revision patients will suffer a periprosthetic fracture (11). A recent danish study has identified an annual 8.7/100,000 incidence of distal femur fractures; a rapid increase in incidence has been demonstrated over the age of 60, predominantly in the female gender (12).
In order to achieve an anatomic, intra-articular reduction at the fracture site, the surgeon must be able to fully visualize and address the proximal end of the knee joint. Historically, the direct lateral access proposed by Marcy et al. in 1947 has represented the gold standard in a distal femoral fracture scenario (13). Unfortunately, this approach lacks the visualization of the entire medial condyle and trochlea as well as the severance of multiple perforating arteries: its association with a medial parapatellar incision can be tempting but the soft tissue vascularization is usually exposed to a high risk of necrosis; moreover, its proximal extension is laborious and time wasting. The Olerud approach usually guarantees good visualization, but the current authors believe that a prolonged post-operative immobilization, typically following that surgical approach, is not recommended for an elderly patient (14). Nevertheless, tibial tuberosity osteotomy (TTO) ensures wide intercondylar visualization but the integrity of the extensor apparatus is essential for early weight-bearing and early mobilization (14, 15). Similarly to the current authors, Starr et al claimed that their version of the “swashbuckler approach” allowed for wide visualization of the distal femur without damaging the extensor apparatus (6). Dugan et al. reported poor knee ROM after this approach was applied to a series of patients; interestingly, Khalil and Ayoub reported multiple complications, including infections, non-unions, delayed tibial tuberosity osteotomy healing, in several young patients who have sustained 33-C3 fractures (16, 17). On the other side, a TTO is useful in a periprosthetic fracture scenario but several authors, in this clinical situation, reported severe complications (18-20). Beltran et al. proposed a “minimally invasive” version of the classical “swashbuckler approach”: this modification significantly reduced the length of the skin incision and the extension of the quadriceps stripping from the meta-diaphyseal bone; the current authors consider a good visualization of the metadiaphyseal portion as necessary to obtain a satisfactory fracture reduction and subsequent fixation (21). On the other side, the current authors use the access proposed by Beltran et al. for the treatment of Hoffa fractures, because of its minimally invasiveness and good joint visualization. Several case reports and case series have confirmed the validity of the “swashbuckler approach” as proposed by Starr et al. (3, 22-24).
The main drawback of the “swashbuckler approach” in all its modified versions is the inclusion of a lateral parapatellar arthrotomy which may undermine the lateral supply to the anastomotic patellar ring [25]. In fact, recent literature has identified poor vascularization as one of the etiologies of postoperative anterior knee pain as well as patellar necrosis and stress fractures (26-30). The current authors developed a modification of the “Swashbuckler approach” with the primary intention of not reducing blood flow to the patella while maintaining the ability to mobilize the extensor mechanism and gain access to the medial condyle. Lazaro et al in their cadaveric study, defined patellar anastomotic ring “safety margins” while performing a knee arthrotomy: they found that a tissue cuff greater than 15 mm, both medially and laterally, ensured the patellar blood supply not be damaged. Based on these findings, the current authors decided to perform the arthrotomy with a minimum 2 cm margin (31). This choice did not lead to a reduction in the mobility of the extensor apparatus allowing the surgeon to perform a dual-plate osteosynthesis when indicated (Figures 4, 5, 6). In light of recent literature, internal fixation with a medial and lateral plate appears to be the gold standard in the treatment of distal femur fractures in the elderly population, which may benefit from early loading and mobilization in terms of lower mortality, inferior morbidity and overall better function (1, 32-38). On the other side, if a TKA will be subsequently indicated, the surgeon could decide whether to perform a more familiar medial approach or a lateral one, not being excessively afraid of ischemic complications involving the patella and the adjacent soft tissues. The current authors made the same considerations with an inverse temporal order regarding dual-plating of periprosthetic fractures. Knowing that the anastomotic circle has been interrupted from the medial side, the authors were able to safely visualize and instrument the entire fracture by incising laterally, keeping the previously described arthrotomy margin (31).
Figure 4.
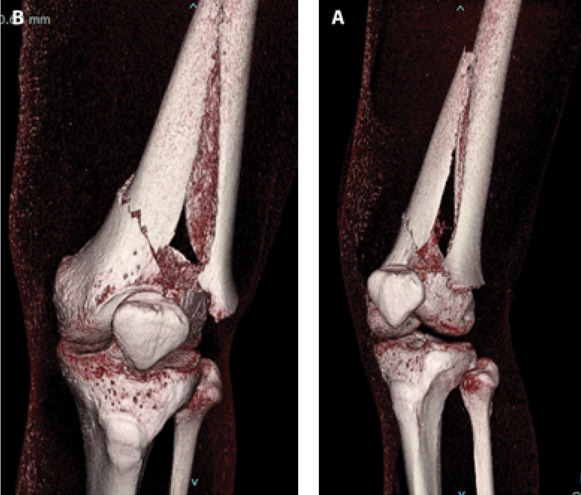
Male patient, 36 years old, AO 33 A3 type distal femur fracture according to the AO/OTA classification.
Figure 5.

X-rays one month after surgery. Double plating fixation of the distal femur.
Figure 6.

X-rays 12 months after surgery: the bone callus is visible with clear signs of fracture healing.
In the two years period examined in the current study, the authors did not routinely perform retrograde intramedullary nailing for AO/OTA 33 or LR type 2 fractures: they acknowledge that this surgical option has recently produced good results and it is currently practiced by the authors for LR type2 fractures when the femoral component presents an “open box” and in AO/OTA 33 A cases, often accompanied by a supplemental plate (39, 40). This study has several, major limitations: first, this is a retrospective case series, lacking of control subjects, with an average 14,9 months follow-up. The sample size is small in order to draw conclusions applicable to the general population. The main purpose of this study was to describe our surgical technique and gain information to generate hypotheses that lead to future, more focused studies of a stronger design. Although the patient population in the current study is heterogeneous regarding demographics and diagnosis, it reflects the two clusters that are most encountered in a standard, public, clinical practice: high-energy trauma in the younger population and low-energy trauma in the elderly. Different fixation options have been chosen in this series but all procedures had in common the goal of obtaining an anatomical reduction which was reached thanks to an effective visualization of the medial metadiaphyseal portion of the distal femur. Although the current authors did not encounter any difficulties in patellar mobilization during the surgical procedures, this finding needs to be verified and supported by future studies (41). In support of the authors conclusions, a large scale contrast-enhanced knee MRI study could be useful to verify the integrity of the peri-patellar circulation and a doppler ultrasound study could eventually verify the intra-patellar blood flow (42, 43). Another limitation of the current study is the difference in the skin incision location between the current authors and Starr et al. and by Beltran et al.: the current authors decided to make a skin incision 2 cm lateral to the patellar tendon; however, the current authors do not believe that this can constitute a substantial difference in comparison with the other authors, although it makes a subsequent medial knee incision more feasible (6, 21).
Conclusion
Fractures of the distal femur, whether on native bone or prosthetic implant, are increasing in number and their mortality is similar to the one of the proximal femur. The “modified Swashbuckler” approach allows anatomical reduction and appropriate fixation, preserves the integrity of the extensor mechanism and interferes minimally with the patellar vascularization.
The authors believe that this modified approach represents a solution to meet the modern demands for robust fixation and early mobilization without incurring in ischemic damage to the patella and the periarticular soft tissues.
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Tarrant SM, Balogh ZJ. The Global Burden of Surgical Management of Osteoporotic Fractures. World J Surg. 2020 Apr;44(4):1009–1019. doi: 10.1007/s00268-019-05237-y. doi: 10.1007/s00268-019-05237-y. PMID: 32047984. [DOI] [PubMed] [Google Scholar]
- Bogunovic L, Cherney SM, Rothermich MA, Gardner MJ. Biomechanical considerations for surgical stabilization of osteoporotic fractures. Orthop Clin North Am. 2013 Apr;44(2):183–200. doi: 10.1016/j.ocl.2013.01.006. doi: 10.1016/j.ocl.2013.01.006. PMID: 23544823. [DOI] [PubMed] [Google Scholar]
- Daroch MS, Vashisht D, Sreen S. Management of intra-articular fracture of distal femur with LCP and Lag screws in adults. Int J Res Med Sci. 2017;5(4):1434. doi: 10.18203/2320-6012.ijrms20171241. [Google Scholar]
- Ebraheim NA, Kelley LH, Liu X, et al. Periprosthetic Distal Femur Fracture after Total Knee Arthroplasty: A Systematic Review. Orthop Surg. 2015;7(4):297–305. doi: 10.1111/os.12199. doi: 10.1111/os.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Keudell A, Shoji K, Nasr M, Lucas R, Dolan R, Weaver MJ. Treatment Options for Distal Femur Fractures. J Orthop Trauma. 2016 Aug;30(Suppl 2):S25–7. doi: 10.1097/BOT.0000000000000621. doi: 10.1097/BOT.0000000000000621. PMID: 27441931. [DOI] [PubMed] [Google Scholar]
- Starr AJ, Jones AL, Reinert CM. The “swashbuckler”: a modified anterior approach for fractures of the distal femur. J Orthop Trauma. 1999 Feb;13(2):138–40. doi: 10.1097/00005131-199902000-00012. doi: 10.1097/00005131-199902000-00012. PMID: 10052790. [DOI] [PubMed] [Google Scholar]
- Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007 Nov-Dec;21(10 Suppl):S1–133. doi: 10.1097/00005131-200711101-00001. doi: 10.1097/00005131-200711101-00001. PMID: 18277234. [DOI] [PubMed] [Google Scholar]
- Rorabeck CH, Angliss RD, Lewis PL. Fractures of the femur, tibia, and patella after total knee arthroplasty: decision making and principles of management. Instr Course Lect. 1998;47:449–58. PMID: 9571446. [PubMed] [Google Scholar]
- Sanders R, Swiontkowski M, Rosen H, Helfet D. Double-plating of comminuted, unstable fractures of the distal part of the femur. J Bone Joint Surg Am. 1991 Mar;73(3):341–6. PMID: 2002071. [PubMed] [Google Scholar]
- A. P. Browner BD, Jupiter JB, Kretteck C. Principles of Internal Fixation. Skeletal Trauma: Basic Science, Management, and Reconstruction. 6th ed. Philadelphia, PA: Elsevier; 2020. [Google Scholar]
- Della Rocca GJ, Leung KS, Pape HC. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011 Jun;25(Suppl 2):S66–70. doi: 10.1097/BOT.0b013e31821b8c28. doi: 10.1097/BOT.0b013e31821b8c28. PMID: 21566478. [DOI] [PubMed] [Google Scholar]
- Elsoe R, Ceccotti AA, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop. 2018 Jan;42(1):191–196. doi: 10.1007/s00264-017-3665-1. doi: 10.1007/s00264-017-3665-1. Epub 2017 Nov 7. PMID: 29116356. [DOI] [PubMed] [Google Scholar]
- MARCY GH. The posterolateral approach to the femur. J Bone Joint Surg Am. 1947 Jul;29(3):676–8. PMID: 20253041. [PubMed] [Google Scholar]
- Olerud S. Operative treatment of supracondylar--condylar fractures of the femur. Technique and results in fifteen cases. J Bone Joint Surg Am. 1972 Jul;54(5):1015–32. PMID: 5057097. [PubMed] [Google Scholar]
- Khlopas A, Samuel LT, Sultan AA, Yao B, Billow DG, Kamath AF. The Olerud Extensile Anterior Approach for Complex Distal Femoral Fractures: A Systematic Review. J Knee Surg. 2021 Jul;34(8):822–827. doi: 10.1055/s-0039-3400954. doi: 10.1055/s-0039-3400954. Epub 2019 Nov 27. PMID: 31777034. [DOI] [PubMed] [Google Scholar]
- Dugan TR, Hubert MG, Siska PA, Pape HC, Tarkin IS. Open supracondylar femur fractures with bone loss in the polytraumatized patient - Timing is everything! Injury. 2013 Dec;44(12):1826–31. doi: 10.1016/j.injury.2013.03.018. doi: 10.1016/j.injury.2013.03.018. Epub 2013 Apr 16. PMID: 23601115. [DOI] [PubMed] [Google Scholar]
- Khalil Ael-S, Ayoub MA. Highly unstable complex C3-type distal femur fracture: can double plating via a modified Olerud extensile approach be a standby solution? J Orthop Traumatol. 2012 Dec;13(4):179–88. doi: 10.1007/s10195-012-0204-0. doi: 10.1007/s10195-012-0204-0. Epub 2012 Jun 26. PMID: 22733172; PMCID: PMC3506844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zonnenberg CB, Lisowski LA, van den Bekerom MP, Nolte PA. Tuberositas osteotomy for total knee arthroplasty: a review of the literature. J Knee Surg. 2010 Sep;23(3):121–9. doi: 10.1055/s-0030-1267472. doi: 10.1055/s-0030-1267472. PMID: 21329253. [DOI] [PubMed] [Google Scholar]
- Piedade SR, Pinaroli A, Servien E, Neyret P. Tibial tubercle osteotomy in primary total knee arthroplasty: a safe procedure or not? Knee. 2008 Dec;15(6):439–46. doi: 10.1016/j.knee.2008.06.006. doi: 10.1016/j.knee.2008.06.006. Epub 2008 Sep 4. PMID: 18771928. [DOI] [PubMed] [Google Scholar]
- Chun KC, Kweon SH, Nam DJ, Kang HT, Chun CH. Tibial Tubercle Osteotomy vs the Extensile Medial Parapatellar Approach in Revision Total Knee Arthroplasty: Is Tibial Tubercle Osteotomy a Harmful Approach? J Arthroplasty. 2019 Dec;34(12):2999–3003. doi: 10.1016/j.arth.2019.07.015. doi: 10.1016/j.arth.2019.07.015. Epub 2019 Jul 13. PMID: 31401038. [DOI] [PubMed] [Google Scholar]
- Beltran MJ, Blair JA, Huh J, Kirby JM, Hsu JR. Skeletal Trauma Research Consortium(STReC). Articular exposure with the swashbuckler versus a “Mini-swashbuckler” approach. Injury. 2013 Feb;44(2):189–93. doi: 10.1016/j.injury.2012.10.021. doi: 10.1016/j.injury.2012.10.021. Epub 2012 Dec 11. PMID: 23237603. [DOI] [PubMed] [Google Scholar]
- Harna B, Goel A, Singh P, Sabat D. Pediatric conjoint Hoffa’s fracture: An uncommon injury and review of literature. J Clin Orthop Trauma. 2017 Oct-Dec;8(4):353–354. doi: 10.1016/j.jcot.2016.12.001. doi: 10.1016/j.jcot.2016.12.001. Epub 2017 Jan 20. PMID: 29062218; PMCID: PMC5647619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R, Singh RB, Mahendra M. Functional Outcome of Isolated Hoffa Fractures Treated with Cannulated Cancellous Screw. Malays Orthop J. 2017 Jul;11(2):20–24. doi: 10.5704/MOJ.1707.016. doi: 10.5704/MOJ.1707.016. PMID: 29021874; PMCID: PMC5630046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta GK, Jacob RV. Demographic profile and functional outcome following fixation of distal femur fractures by locking compression plate. Int. Orthop Sci. 2020;6(1):79–82. doi: 10.22271/ortho.2020.v6.i1b.1843. [Google Scholar]
- DeBell H, Pinter Z, Pinto M, et al. Vascular supply at risk during lateral release of the patella during total knee arthroplasty: A cadaveric study. J Clin Orthop Trauma. 2019 Jan-Feb;10(1):107–110. doi: 10.1016/j.jcot.2017.11.009. doi: 10.1016/j.jcot.2017.11.009. Epub 2017 Nov 24. PMID: 30705542; PMCID: PMC6349579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noorpuri BS, Maqsood M. Osteonecrosis of the patella and prosthetic extrusion after total knee arthroplasty. J Arthroplasty. 2002 Aug;17(5):662–3. doi: 10.1054/arth.2002.33270. doi: 10.1054/arth.2002.33270. PMID: 12168185. [DOI] [PubMed] [Google Scholar]
- Putman S, Boureau F, Girard J, Migaud H, Pasquier G. Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res. 2019 Feb;105(1S):S43–S51. doi: 10.1016/j.otsr.2018.04.028. doi: 10.1016/j.otsr.2018.04.028. Epub 2018 Jul 7. PMID: 29990602. [DOI] [PubMed] [Google Scholar]
- Schüttrumpf JP, Behzadi C, Balcarek P, et al. Radiologically hyperdense zones of the patella seem to be partial osteonecroses subsequent to fracture treatment. J Knee Surg. 2013 Oct;26(5):319–26. doi: 10.1055/s-0032-1332805. doi: 10.1055/s-0032-1332805. Epub 2013 Jan 4. PMID: 23288779. [DOI] [PubMed] [Google Scholar]
- Sanchis-Alfonso V. Patellofemorale Schmerzen [Patellofemoral pain] Orthopade. 2008 Sep;37(9):835–6. 838–40. doi: 10.1007/s00132-008-1289-2. German. doi: 10.1007/s00132-008-1289-2. PMID: 18682915. [DOI] [PubMed] [Google Scholar]
- Baumgarten KM, Mont MA, Rifai A, Hungerford DS. Atraumatic osteonecrosis of the patella. Clin Orthop Relat Res. 2001 Feb;(383):191–6. doi: 10.1097/00003086-200102000-00021. doi: 10.1097/00003086-200102000-00021. PMID: 11210953. [DOI] [PubMed] [Google Scholar]
- Lazaro LE, Cross MB, Lorich DG. Vascular anatomy of the patella: implications for total knee arthroplasty surgical approaches. Knee. 2014 Jun;21(3):655–60. doi: 10.1016/j.knee.2014.03.005. doi: 10.1016/j.knee.2014.03.005. Epub 2014 Apr 2. PMID: 24767718. [DOI] [PubMed] [Google Scholar]
- Peschiera V, Staletti L, Cavanna M, Saporito M, Berlusconi M. Predicting the failure in distal femur fractures. Injury. 2018 Nov;49(Suppl 3):S2–S7. doi: 10.1016/j.injury.2018.10.001. doi: 10.1016/j.injury.2018.10.001. PMID: 30415665. [DOI] [PubMed] [Google Scholar]
- Jennison T, Divekar M. Geriatric distal femoral fractures: A retrospective study of 30 day mortality. Injury. 2019 Feb;50(2):444–447. doi: 10.1016/j.injury.2018.10.035. doi: 10.1016/j.injury.2018.10.035. Epub 2018 Oct 31. PMID: 30442373. [DOI] [PubMed] [Google Scholar]
- Sain A, Sharma V, Farooque KVM, Pattabiraman K. Dual Plating of the Distal Femur: Indications and Surgical Techniques. Cureus. 2019 Dec 27;11(12):e6483. doi: 10.7759/cureus.6483. doi: 10.7759/cureus.6483. PMID: 31903313; PMCID: PMC6935741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg EL, Elis J, Steinberg Y, Salai M, Ben-Tov T. A double-plating approach to distal femur fracture: A clinical study. Injury. 2017 Oct;48(10):2260–2265. doi: 10.1016/j.injury.2017.07.025. doi: 10.1016/j.injury.2017.07.025. Epub 2017 Jul 25. PMID: 28768571. [DOI] [PubMed] [Google Scholar]
- Yaacobi E, Sanchez D, Maniar H, Horwitz DS. Surgical treatment of osteoporotic fractures: An update on the principles of management. Injury. 2017 Dec;48(Suppl 7):S34–S40. doi: 10.1016/j.injury.2017.08.036. doi: 10.1016/j.injury.2017.08.036. Epub 2017 Sep 4. PMID: 28882375. [DOI] [PubMed] [Google Scholar]
- Consigliere P, Iliopoulos E, Ads T, Trompeter A. Early versus delayed weight bearing after surgical fixation of distal femur fractures: a non-randomized comparative study. Eur J Orthop Surg Traumatol. 2019 Dec;29(8):1789–1794. doi: 10.1007/s00590-019-02486-4. doi: 10.1007/s00590-019-02486-4. Epub 2019 Jul 2. PMID: 31267203. [DOI] [PubMed] [Google Scholar]
- Larsen P, Ceccotti AA, Elsoe R. High mortality following distal femur fractures: a cohort study including three hundred and two distal femur fractures. Int Orthop. 2020 Jan;44(1):173–177. doi: 10.1007/s00264-019-04343-9. doi: 10.1007/s00264-019-04343-9. Epub 2019 May 12. PMID: 31081515. [DOI] [PubMed] [Google Scholar]
- Shin YS, Kim HJ, Lee DH. Similar outcomes of locking compression plating and retrograde intramedullary nailing for periprosthetic supracondylar femoral fractures following total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017 Sep;25(9):2921–2928. doi: 10.1007/s00167-016-4050-0. doi: 10.1007/s00167-016-4050-0. Epub 2016 Feb 20. PMID: 26897137. [DOI] [PubMed] [Google Scholar]
- Mirick Mueller GE. Nail-Plate Constructs for Periprosthetic Distal Femur Fractures. J Knee Surg. 2019 May;32(5):403–406. doi: 10.1055/s-0039-1683444. doi: 10.1055/s-0039-1683444. Epub 2019 Mar 27. PMID: 30919389. [DOI] [PubMed] [Google Scholar]
- Stevens JM, Clement ND, Macpherson G, Patton JT. Comparison of two extensile approaches to the knee: a cadaveric study evaluating quadriceps snip and extensile medial parapatellar approach. J Orthop. 2018 Mar 22;15(2):416–419. doi: 10.1016/j.jor.2018.03.023. doi: 10.1016/j.jor.2018.03.023. PMID: 29881167; PMCID: PMC5990209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholls RL, Green D, Kuster MS. Patella intraosseous blood flow disturbance during a medial or lateral arthrotomy in total knee arthroplasty: a laser Doppler flowmetry study. Knee Surg Sports Traumatol Arthrosc. 2006 May;14(5):411–6. doi: 10.1007/s00167-005-0703-0. doi: 10.1007/s00167-005-0703-0. Epub 2005 Nov 30. PMID: 16320014. [DOI] [PubMed] [Google Scholar]
- Rollick NC, Gadinsky NE, Klinger CE, Kubik JF, Dyke JP, Helfet DL, Wellman DS. The effects of dual plating on the vascularity of the distal femur. Bone Joint J. 2020 Apr;102-B(4):530–538. doi: 10.1302/0301-620X.102B4.BJJ-2019-1776. doi: 10.1302/0301-620X.102B4.BJJ-2019-1776. PMID: 32228080. [DOI] [PubMed] [Google Scholar]


