Abstract
Radiocapitellar plica is a vestigial lateral portion of elbow synovial fold which may cause pain and snap in some cases.. Plica is a difficult and misleading diagnosis and it could be easily confused with a common lateral epicondylitis however, they are different conditions. Pathology full understanding and proper diagnosis is essential to achieve patient’s pain relief and functional recovery therefore, we reviewed the most relevant literature about radiocapitaller plica. The aim of this study is to provide the best and current concepts about: clinical evaluation, imaging findings and surgical treatments of radiocapitellar plica.(www.actabiomedica.it)
Keywords: radiocapitellar, plica, elbow, arthroscopy, lateral epicondylitis, synovial fold
Introduction
Lateral pain of the elbow might be a quite difficult diagnosis because its causes are multiple and imaging sometimes is not conclusive. Most patients complain about lateral pain, sometimes associated with popping, clicking or snapping (1, 2). The most common causes of epicondylalgia are: tennis elbow, inter-osseous nerve compression, muscular-cutaneous nerve entrapment, chondropathia of the humeral-radial joint. If a snap is present, the following diagnoses should be considered: medial triceps snap, posterolateral instability, loose bodies, unstable ulnar nerve, posterolateral plica. Lateral epicondylitis and synovial plica can be confused but the two conditions are different. The aim of this study is to review the most relevant literature about the radiocapitellar plica, reporting clinical tests, radiological findings for its diagnosis and the outcomes after surgical excision.
Historical Review
The “plica” was described for the first time in 1911 by Charpy and Nicolas as a meniscoid structure projecting into the radiohumeral joint from behind (fig.1) (3). In 1912 Poirer defined this structure as a “bourellet falciforme” that is interposed between the capitulum humeri and the radial head. Nonetheless in 1988, Clarke found a relationship between the presence of the plica and lateral elbow pain. Other authors confirmed that a hypertrophic plica can be a cause of lateral pain, demonstrating relief of symptoms after arthroscopic plica excision in 90% of patients (4-8).
Figure 1.
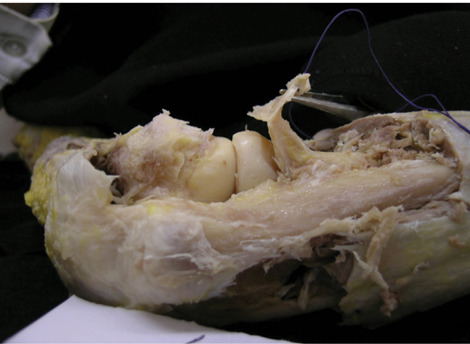
The “plica” is a synovial fold interposed between radial head and capitulum humeri.
Embryology
The elbow joint is divided in 3 rooms approximately until O’Rahilly stage 21 (53rd day of human development). At that time the cavitation of the elbow begins through the septa resorption. In O’Rahilly stage 23 it is possible to distinguish a triangulated shaped condensation of synovial mesenchyme that points toward the interior of the radio-humeral joint. In the 11th week this synovial fold fills the space between the humerus and the radial head. Thereafter, the synovial plica of the radial-humeral joint is an embryonal remnant of the cavitation of the septa (9). The presence of the plica as an embryonal remnant has been demonstrated in other joints such as in the knee, which was long described by several authors (10, 11).
Oztuna found a membranous structure which lies from the interfaced prominence of the radius to the scapholunate ligament and divides the wrist joint into two cavities. At weeks 11 and 12, the membranous structure underwent regression from dorsal to volar aspect; in some cases, a plica-like membranous structure may persist as a remnant of the fetal life (12). A synovial plication of capsule has been also described in the hip as a cause of bony erosion and pain, considering this structure being an embryonic relic (13). In the ankle, anatomical studies have found the plica in the distal tibiofibular joint. The triangular shaped synovial fold is sagittally oriented between the two bones in the posterior part of the joint. This structure is identified in the adult and even in the fetus (14-16). Codman and others authors showed that a plica may exist in the subacromial, subdeltoid and subcoracoid bursa. Funk et al. found the subacromial plica be a rare cause of the impingement syndrome (17-20).
Anatomy and Histology
Isogai et al. examined 40 embryos around their 28th week and found the presence of a plica circumferentially extended between the capitulum and radial head, in continuity distally with the annular ligament in all of them. Some authors subdivided this structure in anterior, lateral, posterolateral and lateral olecranon portions. A “circumferential synovial fold” in present in 2-12% of people (21, 23, 26, 27). The posterolateral radiocapitellar plica is almost ubiquitarian, and this is confirmed both from anatomic and from radiological studies (21-25). In the embryo, the plica was found to have a macroscopically homogeneous aspect with a fringed villus pattern, rather than showing a plicate pattern. In 34/40 embryos, the lateral portion was absent. Microscopically, the plica was formed from collagen fibers running along the longitudinal axis and was covered by a synovial layer. Chondroid metaplasia has not been reported, therefore it is not correct to consider it a meniscus, but rather a synovial fold. International literature agrees that the synovial fold must to be considered an embryonal remnant of the cavitation of the septa and is formed by fibroadiposus connective tissue covered by a layer of synovial tissue. In 2002 Duparc et al. claimed that “the absence of a fibrochondoid structure means this anatomical structure cannot be called a meniscus” (23). In addition to those studies, there are others case reports that describe elbow pain and/or snapping caused by a “real meniscus” composed by fibrocartilagineous tissue without synovial layer (23, 28, 29). Fabie et al. first described an humeroradial joint meniscus as cause of elbow stiffness in a 15-month-old infant. The surgical excision was successful. They interpreted this finding as a real pathological entity. This anatomopathological pattern is still controversial and should be further investigated (28). Isogai et al. confronted the morphology of the plica between embryos and adults both macroscopically and microscopically. The anterior portion of the plica in the adults was tighter and thinner. The posterior portion was hypertrophic and often covered by a multiple synovial layer. As regards the embryos, the lateral portion was only present in 6/40 specimens and likely to have two anatomopathological aspects: maybe developing either on a more distal plane to the anterior and posterior one, or maybe in continuity, on the same plane. They also described different plica pattern: villous, fringed, plicate and two intermediate patterns such as a villous-fringed and fringed plicated (21, 23, 28, 30-32). Mullet et al. published a morphologic classification of the radio-humeral synovial fold based on an arthroscopic anterior compartment view. He examined dynamically (flexion, extension, pronosupination) 30 patients affected by lateral epicondylitis and 34 paired cadaveric elbows. In type 1, the radial head was uncovered; in type 2, it was partially covered by the synovial fold which was not interposed in the joint; type 3, it was characterized by the presence of the radiocapitellar complex that obscured the radial head and impinged the joint. Type 4 was defined by the complete covering of the radial head and the tissue was extremely thickened and requiring wide debridement to allow the vision of the underling bone (33).
It is not fully understood incidence of radiocapitellar plica. Cadaveric studies and MRI findings outlined occurrence of synovial fold between 86-99% in asymptomatic individuals (21, 23, 35, 36). Authors reported symptomatic plica only in 7.2 – 8-7% of all elbow arthroscopy (6, 35, 36).
Etiopathogenesis
The presence of the lateral portion of the synovial fold in the adults has been interpreted like the result of mechanical stresses. The posterior portion of the plica falls in the radial-humeral joint at the maximum extension and covers the posterior half of the radial head that in such a position is not articulated with the capitulum. In flexion, the posterior portion of the plica covers the capitulum humeri, keeping it covered by a film of synovial liquid. The anterior portion plays a limited mechanical role and covers the radial head in extension, probably because of the tension of the joint capsule. The lateral portion is in continuity with the articular surface of the lateral ulnar collateral ligament (LUCL). Some studies showed the relationship between the annular ligament and the radiocapitellar synovial fold: it is contiguous with the radiocapitellar joint capsule and distinct from the annular ligament, and belongs to the lateral epicondyle enthesis. When the forearm is in pronation, the epicondyloid muscles and the lateral ligamentous complex keep the radial-humeral joint in tension and stretch the structure that is tight between the radial head and capitulum laterally. Therefore, the lateral epicondylitis may be a pathology that involves not only the extensor origin and the joint capsule, but also the underling anatomical structures, like the synovial fold. Moreover, symptoms of epicondylitis can be caused by both the pathology of the extensor enthesis and the impingement of synovial fold (34).
Literature is still controversial: Rhyou and Kim reported that plica’s excision do not decrease pain in lateral epicondylitis and according to Lee (1) plica resection is not helpful in typical elbow pain (1, 37).
The radial head and the plica have a movement described as a mutual piston-like by Kim: in extension, the plica covers the radial head slipping proximally, while in flexion, the plica snaps distally and uncovers the radial head. This movement may be the cause of the plica hypertrophy, of its fibrotic and erythematous aspect and it is the rational of the clinical tests for the diagnosis of the symptomatic synovial fold and of which portion is more involved (34,37-39). Moreover, the snap can cause abrasion over the cartilage surface of the radial head and capitellum (92,8% and 21,4%, respectively, in Antuna and O’Driscoll’s patient series) and chondromalacia (6). Steiner et al. noted that early detection and treatment of hypertrophic symptomatic plica can decrease incidence of cartilage damage due to mechanical degeneration (40). This theory is supported by comparison of two patient series: in Antuna and O’Driscoll patient’s series the incidence of cartilage abrasion is high (92,8%), in Steinert et al. patient’s series is 33%. This is probably due to the shorter time in symptoms onset and surgical treatment (mean 13 months in Antuna and O’Driscoll series, mean 7,8 months in Steiner et al. series). However, this conclusion should consider the different number of patients observed: 14 (Antuna and O’Driscoll) vs 3 (Steiner et al.) (6, 40).
Diagnosis
The pathology can occur at any age and patients generally complain about a lateral pain that can be associated to either clicking or snapping. In history, possible previous trauma or joint overload due to repetitive work or sport activities are reported to be present. The snap can be felt on the lateral side of the joint flexing the elbow from 90 to 110 degrees. Typically, the snap is perceived around 90° if the plica is hypertrophic; if the synovial fold is present but its volume is reduced, the snap is felt around 120° of flexion. Some authors describe a clicking in full extension and supination of the joint. The mechanical symptoms can be inconstant: in some patient series, the snap is identified to be present in 58% of patients, in some other series in 100%. The pain is on the lateral side of the elbow, more posteriorly than the epicondyle. The symptoms can be reproduced fingering the anconeus soft spot. A mild lack of extension can be observed (1, 6-8).
Clinical Test
Flexion-Pronation Test
Antuna and O’Driscoll described the flexion-pronation test. The examiner puts his thumb on the lateral side of the radial-humeral joint and transmits a mild pressure. The forearm is held in pronation and the elbow in extension. In this position the external portion of the plica lies inside of the radial-humeral joint. Keeping the pressure on the radial-humeral joint, the examiner bends the elbow. Around 90 degrees, a snap is perceived under the thumb, that can be painful for the patient. In this position, the plica snaps outside the joint. The positivity of this test leads to diagnosis of lateral plica (fig.2) (6).
Figure 2.

Flexion-pronation test for detecting lateral plica.
Extension-Supination Test
The examiner puts his thumb on the arthroscopic soft spot, on the posterior side of the radial-humeral joint. The forearm is held in supination. The physician extends the elbow from a flexed position. In the last degrees the plica engages the radial-humeral articulation, if is hypertrophic a portion of the plica (except its free margin) remains outside the joint. With the pressure of the thumb the posterior portion of the plica is pushed inside the radial-humeral joint but in complete extension it pushed outside because his volume. This produces a snap that is perceived under the thumb and leads to diagnosis of posterior plica (6, 8) (fig.3).
Figure 3.

Extension-supination test to detect posterior plica
Posterolateral Radiocapitellar Plica Test
In 2019 Park et all. described a new physical test outlined 83.3% sensibility and 87.5% specificity, tough patient sample size was small and study was conducted retrospectively. The examiner puts his thumb at the posterolateral aspect of radiocapitellar joint and the elbow is extended in the starting position; grasp the wrist with other examiner’s hand and turn the patient’s forearm into a pronated position. Manual compression force on radiocapitellar joint is maintained and the elbow is flexed. The presence of tenderness must be checked. The test must be considered positive if the pain that occurs at low flexion angle is significantly decreased at more than 90° of flexion (41).
Differential Diagnosis
Tennis elbow: Physical examination shows tenderness 1 cm anteriorly and distally to lateral epicondyle. Pain is reproduced by the following tests:
- “Chair test”: the patient is asked to lift a chair with the affected hand (forearm in pronation and wrist in palmar flexion) (42).
- Middle finger resisted extension test: pain on resisted extension of the middle finger at the metacarpophalangeal joint when the elbow is in full extension (43, 44).
- Mill’s test: passive stretch of extensor tendons produced by full elbow extension, forearm pronation, wrist palmar flexion and ulnar deviation of the hand.
- Cozen test: resisted wrist extension (45)
- Posterior interosseous nerve compression: Radial tunnel syndrome (RTS) causes symptoms that mimic others pathologies. The patient complains about pain like a “shooting” along the lateral side of the elbow irradiating to the back of the wrist and the thumb or the opposite. If the symptoms are reproduced by pressing the point of maximum tenderness along the course of radial nerve, this is considered a positive confirmatory test. This point is generally around 6 cm distally to lateral epicondyle (46, 47). Other tests are:
- Pain on resisted supination of the forearm
- Injection with 1% lidocaine and 40 mg of triamcinolone in the site of maximal tenderness along the course of radial nerve. If the injection relieves the pain, the test is confirmatory (48).
- Middle finger resisted extension test: the test is conducted with the elbow in extension. The pain is provoked by tightening the fascia of extensor carpi radialis brevis and it is positive both in lateral epicondylitis and radial tunnel syndrome (43, 45).
EMG is normal. Ultrasound of the area in which the nerve enters the Frohse arcade can show reduction in anteroposterior dimension of the nerve on longitudinal scans and no change in transverse section (47).
Musculocutaneous nerve entrapment: The symptoms of this syndrome are pain and dysesthesias (described as “burning” sensation) on the lateral side of the forearm. Physical examination shows tenderness lateral to the biceps tendon, loss of extension if the forearm is pronated, hyperesthesia in the radial side of the forearm. The nerve is purely sensory, then there is no loss of motory function (49, 50).
Chondropathia of the humeral-radial joint: Chondromalacia can be concomitant with the radiohumeral plica. O’Driscoll reported 13 observations of radial head erosion in 14 patients who underwent arthroscopic plica excision. This finding is correlated with the mechanical abrasion of the snapping plica over the radial head (6) Symptoms of chondropathia of the humeral-radial joint are not specific: end range of motion pain, loss of motion, crepitus and tenderness at the lateral aspect of the elbow. In patients who have more advanced cartilage changes, symptoms are more evident: catching, clicking, locking (if loose bodies or loose cartilage flaps are present) (51, 52).
Medial triceps snap: The snap is perceived medially, over the medial epicondyle, when the elbow is flexed (actively or passively) to more than 90° degrees (around 110°) (53, 54).
Unstable ulnar nerve: in this pathology the snap can be correlated to ulnar neuropathy. The snap is typically felt around 90° degrees of elbow flexion, over the medial epicondyle. If a snapping of the medial head of the triceps is also present, during clinical examination the ulnar nerve dislocates around 90 degrees and the triceps around 110 degrees (54).
Posterolateral instability (PLRI): The posterolateral rotatory instability is caused by an acute or chronic deficiency of the ulnar part of lateral collateral ligament of the elbow (LUCL). The patient complains recurrent clicking or locking on the lateral side of the joint. The diagnosis can be made through history (previous trauma or surgery for lateral epicondylitis, elbow dislocation) and mainly by clinical examination.
The most sensitive test is the lateral pivot-shift apprehension test: the patient is supine and the arm is overhead. Supination and valgus moment with axial compression is applied during flexion: the elbow subluxates around 40-70 degrees of flexion. With this maneuver, it is possible to reproduce the patient’s symptoms (if he is relaxed enough) with the patient reacting with an apprehension response (55, 56). Other tests for PLRI are the following:
- Posterolateral rotatory drawer test: it is similar to the Lachmann test of the knee. Holding the humerus with one hand, use the other hand to keep the forearm in supination and pull it dorsally away from the humerus. The test is positive if the radius and ulna subluxate, leaving a dimple in the skin behind the radial head (57).
- Tabletop relocation test: the patient is asked to hold the lateral edge of the table with his affected arm (to keep the forearm in supination). Then he is asked to flex the elbow. If PLRI is present an apprehension response is elicited around 40 degrees of flexion. Symptoms are relieved if the examiner keeps the radial head reduced with his thumb during the maneuver (58).
- Chair sign: the patient is asked to stand up from a sitting position, pushing on the seat and keeping the forearm supinated (59).
- Push-up sign: this is an active apprehension test. The patient is asked to lift himself from the floor, from a flexed elbow position, forearm supinated and arms abducted to greater than the shoulder width (59).
Loose bodies: Typical symptoms are swelling, pain and locking. The locking symptoms are inconstant and variable. Sometimes a mobile mass is palpable on the back of the elbow. Diagnosis can be frequently achieved by radiologic examination (60, 61).
Imaging
Imaging could be a useful tool in diagnosing plica alongside with a careful clinical examination.
X-rays role has some limitations for plica diagnosis in order to exclude some other elbow pain’s causes as well as ultrasonographic examination may play some role, however the sensitivity is different if the synovial fold is anterior (96%), posterior (94%) or lateral (67%) (62). Magnetic Resonance Imaging (MRI) is the most reliable diagnostic tool for plica. Some studies analyzed the thickness of radiocapitellar plica: it is considered hypertrophic and possible cause of elbow pain if it is 3 mm thick or more (1). Husarik et al. noted that in a series of 60 asymptomatic patients, thickness of the plica never exceeds 3.1 mm. In 2018 Hyun et al. reported a mean thickness of 3.7 mm on coronal MRI and a mean thickness of 3.4 mm on sagittal images and also the mean length was increased (1, 2, 24). Choi et al. demonstrated dimensions of posterolateral plica were 7.0mm mediolateral and 7.4 mm sagittal in symptomatic patients while 3.8mm and 4.7mm in asymptomatic patients (35).
Nonetheless, results are still controversial. Vahlensieck et al. used MRI to study and dissect 42 elbows: he found the plica in all specimens, but only in 24% of them MRI enabled identifying the plica (fig.4 a,b) (35). In O’Driscoll’s patient series only in 1 case MRI showed an annular ligament mild edema (6 patients underwent MRI examination) (6). Other authors detected the plica in a 12-year-old boy using a microscopic coil MRI, that enabled the visualization of small structures (63). The use of arthrographic MRI (gd-DTPA) is suggested by Huang in his case report, but in Kim’s patient series, the gadolinium-enhanced MRI detected the synovial fold only in 25% of cases (8, 29). MRI is always recommended when suspected radial head or capitulum chondromalacia and for differential diagnosis among causes of lateral elbow pain. Notably it is important to differentiate between true osseous and chondral erosion of capitellum and “pseudodefect of capitellum” described by Rosenberg (64, 65). Capitellum pseudodefect is on MRI the area of conjunction between cartilage surface of capitellum and cortical bone of lateral epicondyle and must be considered a normal finding. In 2010 Kang et al. underlies the usefulness of double contrast arthrography under fluoroscopic control to detect plica and study dynamically plica snapping (66).
Figure 4.
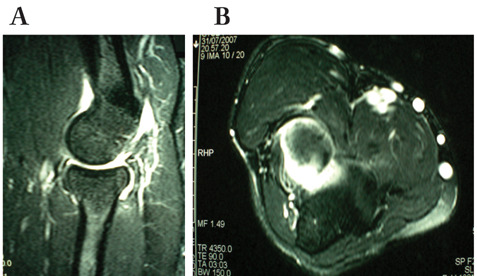
MRI showing posterolateral plica in sagittal view (a) and axial view (b)
MRI and CT arthrography could have an emerging role to better identify a thickened plica, even if a normal plica on MRI does not exclude the possibility to be symptomatic (41). We have studied one case of posterolateral pain with clinical suspicion of plica by CT. The 2D reconstructions on the coronal, axial and sagittal planes and the 3D reconstruction were performed. CT showed the presence of two small-size ossifications on the posterolateral margin of the radial head (fig 5, a,b). An arthroscopic debridement of the plica was performed and two small loose bodies were found under the plica, in the inner side of the annular ligament (fig.6, fig.7).
Figure 5.
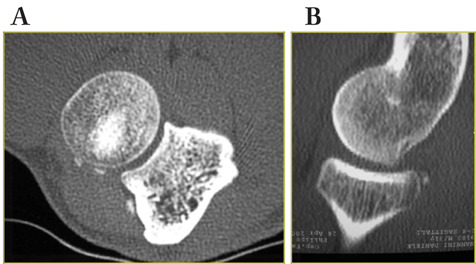
On CT scan loose bodies behind the radial head can be localized in axial (a) and sagittal view (b)
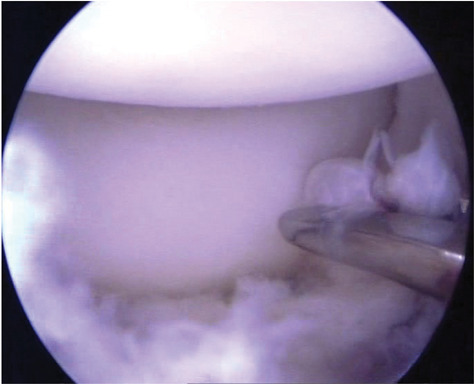
Figure 6.
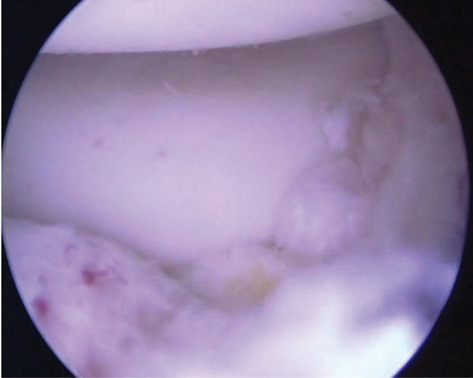
Arthroscopic visualization of loose bodies from posterolateral portal
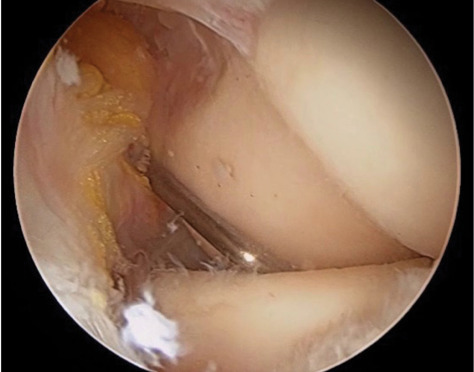
Figure 7.
Arthroscopic vision of plica from posterolateral portal.
Treatment
The treatment of the posterolateral synovial fold contemplates as a first step rest, change in activities, physical therapy and drugs administration such as NSAID, steroid injections and supervised physiotherapy (1, 8, 40). If conservative treatment fails, an arthroscopic procedure should be performed. The visualization of the articular space must be complete. The plica must be inspected on both the anterior and posterior sides (fig.8a). The best vision is obtained from the posterolateral portal using a 30° scope. The posterior portion of the plica can be resected putting the working instruments (motorized instruments: 3,5 mm shaver; knife, forceps) in the soft spot portal (fig.8b). The excision of the plica anterior portion may be obtained watching from the anteromedial portal and working with a shaver or back cutting instruments from the anterolateral portal and/or the soft spot portal. In the latter case, the instrument crosses the joint from the back to the front (fig.9). The back-cut instruments are useful most of all to ablate the lateral portion of the plica sometimes presenting a tent-like shape, thus making it difficult to ablate it from the anterolateral portal.
Figure 8a.
Arthroscopic vision of plica from posterolateral portal.
Figure 8b.
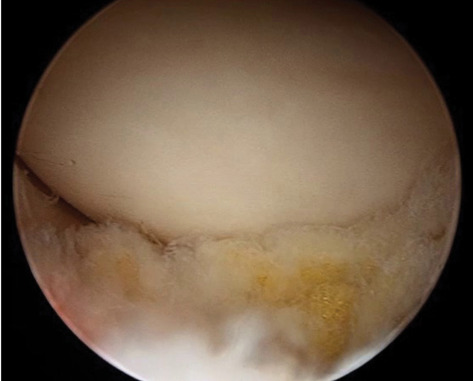
Vision after plica resection, from the same portal.
Figure 9.

Arthroscopic elbow instruments in soft-spot portal and arthroscope in antero-medial portal.
To date results about arthroscopic excision of the plica have limitations, with small cohorts and no validating score system. Authors reported excellent functional outcomes after arthroscopic treatment and focused rehabilitation (8, 68, 69). Brahe Pedersen et al. reported a case series of 64 arthroscopic plica resection, they reported improved functional outcomes at 22-months follow-up in 52% of patients who underwent surgery (69). Lee et al. noted that all patient decreased their pain and improved extension deficit after surgery (1). Though, further studies are needed to detect long term functional outcome of surgical treatment.
Conclusions
Radiohumeral synovial plica can be easily misdiagnosed for several reasons: multiple causes of elbow lateral pain and ubiquitarian presence of the radial-humeral joint synovial fold. The diagnosis can be achieved accurately, through clinical tests and careful patient examinations considering differential diagnoses. Imaging could be a useful support for diagnosis associated to clinical exam. We still have limited significative results about treatment both conservative and surgical, long term-result is still lack in literature. Despite several studies, there is not a full understanding of embryological development, size cut-off and pathological evolution. So far, we can conclude that accurate clinical examination and MRI imaging play a leading role in diagnosis as well as arthroscopic plica debridement has shown optimal functional and clinical outcome on short term.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- Lee HI, Koh KH, Kim JP, Jaegal M, Kim Y, Park MJ. Prominent synovial plicae in radiocapitellar joints as a potential cause of lateral elbow pain: clinico-radiologic correlation. J Shoulder Elbow Surg. 2018 Aug;27(8):1349–1356. doi: 10.1016/j.jse.2018.04.024. [DOI] [PubMed] [Google Scholar]
- Steinert AF, Goebel S, Rucker A, Barthel T. Snapping elbow caused by hypertrophic synovial plica in the radiohumeral joint: a report of three cases and review of literature. Arch Orthop Trauma Surg. 2010 Mar;130(3):347–51. doi: 10.1007/s00402-008-0798-0. [DOI] [PubMed] [Google Scholar]
- Charpy A, Nicolas A. Traite d’Anatomie Humaine. Ancient Maison Delahaye L. Battaille et Cie Editors, Paris. 1911:700–716. [Google Scholar]
- Poirier P, Charpy A, Nicolas A. Traite d’anatomie humaine. vol.1. Ancient Maison Delahaye L. Battaille et Cie Editors, Paris. 1912 [Google Scholar]
- Clarke RP. Symptomatic, lateral synovial fringe (plica) of the elbow joint. Arthroscopy. 1988;4(2):112–6. doi: 10.1016/s0749-8063(88)80077-x. [DOI] [PubMed] [Google Scholar]
- Antuna SA, O’Driscoll SW. Snapping plicae associated with radiocapitellar chondromalacia. Arthroscopy. 2001 May;17(5):491–5. doi: 10.1053/jars.2001.20096. [DOI] [PubMed] [Google Scholar]
- Ruch DS, Papadonikolakis A, Campolattaro RM. The posterolateral plica: a cause of refractory lateral elbow pain. J Shoulder Elbow Surg. 2006 May-Jun;15(3):367–70. doi: 10.1016/j.jse.2005.08.013. [DOI] [PubMed] [Google Scholar]
- Kim DH, Gambardella RA, Elattrache NS, Yocum LA, Jobe FW. Arthroscopic treatment of posterolateral elbow impingement from lateral synovial plicae in throwing athletes and golfers. Am J Sports Med. 2006 Mar;34(3):438–44. doi: 10.1177/0363546505281917. [DOI] [PubMed] [Google Scholar]
- Mérida-Velasco JA, Sánchez-Montesinos I, Espín-Ferra J, Mérida-Velasco JR, Rodríguez-Vázquez JF, Jiménez-Collado J. Development of the human elbow joint. Anat Rec. 2000 Feb 1;258(2):166–75. doi: 10.1002/(SICI)1097-0185(20000201)258:2<166::AID-AR6>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- De Mot P, Brys P, Samson I. Non perforated septum supra-patellaris mimicking a soft tissue tumour. JBR-BTR. 2003 Sep-Oct;86(5):262–4. [PubMed] [Google Scholar]
- Dupont JY. Synovial plicae of the knee. Controversies and review. Clin Sports Med. 1997 Jan;16(1):87–122. doi: 10.1016/s0278-5919(05)70009-0. [DOI] [PubMed] [Google Scholar]
- Oztuna V, Coşkun B, Polat A, Kuyurtar F. El bileği ekleminin fetal dönemdeki gelişimi [The development of the wrist joint in the fetal period] Acta Orthop Traumatol Turc. 2003;37(3):254–60. [PubMed] [Google Scholar]
- Hélénon C, Bergevin H, Aubert JD, Lebreton C, Hélénon O. Le repli synovial supra-cervical de la hanche [Plication of the hip synovium above the femur neck] J Radiol. 1986 Oct;67(10):737–40. [PubMed] [Google Scholar]
- Bartonícek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. 2003 Nov-Dec;25(5-6):379–86. doi: 10.1007/s00276-003-0156-4. [DOI] [PubMed] [Google Scholar]
- Doskocil M. Distální spojení tibie a fibuly není jen syndesmóza [The distal connection of the tibia and fibula is not just a syndesmosis] Sb Lek. 1988 Jan;90(1):1–7. [PubMed] [Google Scholar]
- Kelikian H, Kelikian AS. Disorders of the ankle. Saunders Ed. Philadelphia; 1952. pp. 1–91. [Google Scholar]
- Codman EA. The shoulder. Todd, Boston; 1934. [Google Scholar]
- Strizak AM, Danzig L, Jackson DW, Resnick D, Staple T. Subacromial bursography. An anatomical and clinical study. J Bone Joint Surg Am. 1982 Feb;64(2):196–201. [PubMed] [Google Scholar]
- Bunker T, Wallace WA. Shoulder Arthroscopy. Martin Dunitz, London; 1991. [Google Scholar]
- Funk L, Levy O, Even T, Copeland SA. Subacromial plica as a cause of impingement in the shoulder. J Shoulder Elbow Surg. 2006 Nov-Dec;15(6):697–700. doi: 10.1016/j.jse.2006.03.009. [DOI] [PubMed] [Google Scholar]
- Isogai S, Murakami G, Wada T, Ishii S. Which morphologies of synovial folds result from degeneration and/or aging of the radiohumeral joint: an anatomic study with cadavers and embryos. J Shoulder Elbow Surg. 2001 Mar-Apr;10(2):169–81. doi: 10.1067/mse.2001.112956. [DOI] [PubMed] [Google Scholar]
- Mercer SR, Bogduk N. Intra-articular inclusions of the elbow joint complex. Clin Anat. 2007 Aug;20(6):668–76. doi: 10.1002/ca.20467. [DOI] [PubMed] [Google Scholar]
- Duparc F, Putz R, Michot C, Muller JM, Fréger P. The synovial fold of the humeroradial joint: anatomical and histological features, and clinical relevance in lateral epicondylalgia of the elbow. Surg Radiol Anat. 2002 Dec;24(5):302–7. doi: 10.1007/s00276-002-0055-0. [DOI] [PubMed] [Google Scholar]
- Husarik DB, Saupe N, Pfirrmann CW, Jost B, Hodler J, Zanetti M. Ligaments and plicae of the elbow: normal MR imaging variability in 60 asymptomatic subjects. Radiology. 2010 Oct;257(1):185–94. doi: 10.1148/radiol.10092163. [DOI] [PubMed] [Google Scholar]
- Awaya H, Schweitzer ME, Feng SA, Kamishima T, Marone PJ, Farooki S, Trudell DJ, Haghighi P, Resnick DL. Elbow synovial fold syndrome: MR imaging findings. AJR Am J Roentgenol. 2001 Dec;177(6):1377–81. doi: 10.2214/ajr.177.6.1771377. [DOI] [PubMed] [Google Scholar]
- Koh S, Morris RP, Andersen CL, Jones EA, Viegas SF. Ultrasonographic examination of the synovial fold of the radiohumeral joint. J Shoulder Elbow Surg. 2007 Sep-Oct;16(5):609–15. doi: 10.1016/j.jse.2006.10.019. [DOI] [PubMed] [Google Scholar]
- Aguililla Liñan JM, Miguel Pérez MI, Palau González J, Möller Parera I, Martinoli C. A Comprehensive Review of Radiohumeral Synovial Plicae for a Correct Clinical Interpretation in Intractable Lateral Epicondylitis. Curr Rev Musculoskelet Med. 2020 Aug;13(4):385–390. doi: 10.1007/s12178-020-09636-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabié F, Brouchet A, Accadbled F, Verhaegue L, de Gauzy JS, Cahuzac JP. Does the meniscus exist in the elbow joint in children? Surg Radiol Anat. 2003 Apr;25(1):73–5. doi: 10.1007/s00276-002-0094-6. [DOI] [PubMed] [Google Scholar]
- Huang GS, Lee CH, Lee HS, Chen CY. A meniscus causing painful snapping of the elbow joint: MR imaging with arthroscopic and histologic correlation. Eur Radiol. 2005 Dec;15(12):2411–4. doi: 10.1007/s00330-005-2685-1. [DOI] [PubMed] [Google Scholar]
- Kobayashi M. A morphological and histological study on elbow-joint: part I [in Japanese with English abstract] Med J Kagoshima Univ. 1957;9:321–35. [Google Scholar]
- Stingl J, Gruber V, Koudela K, Marecek M. Arrangement of the joint capsule in the radiohumeral part of the elbow joint (author’s transl) Acta Chir Orthop Traumatol Cech. 1978 Feb;45(1):24–9. [PubMed] [Google Scholar]
- Sato T, Kikuchi S, Yosida J. Anatomical study of the plica sy-novialis of the elbow [in Japanese] J Jpn Orthop Assoc. 1992;66:S1349. [Google Scholar]
- Mullett H, Sprague M, Brown G, Hausman M. Arthroscopic treatment of lateral epicondylitis: clinical and cadaveric studies. Clin Orthop Relat Res. 2005 Oct;439:123–8. doi: 10.1097/01.blo.0000176143.08886.fe. [DOI] [PubMed] [Google Scholar]
- Tsuji H, Wada T, Oda T, Iba K, Aoki M, Murakami G, Yamashita T. Arthroscopic, macroscopic, and microscopic anatomy of the synovial fold of the elbow joint in correlation with the common extensor origin. Arthroscopy. 2008 Jan;24(1):34–8. doi: 10.1016/j.arthro.2007.07.020. [DOI] [PubMed] [Google Scholar]
- Choi SH, Ji SK, Lee SA, Park MJ, Chang MJ. Magnetic resonance imaging of posterolateral plica of the elbow joint: Asymptomatic vs. symptomatic subjects. PLoS One. 2017 Jun 16;12(6):e0174320. doi: 10.1371/journal.pone.0174320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubiatowski P, Wałecka J, Dzianach M, Stefaniak J, Romanowski L. Synovial plica of the elbow and its clinical relevance. EFORT Open Rev. 2020 Sep 30;5(9):549–557. doi: 10.1302/2058-5241.5.200027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim PT, Isogai S, Murakami G, Wada T, Aoki M, Yamashita T, Ishii S. The lateral collateral ligament complex and related muscles act as a dynamic stabilizer as well as a static supporting structure at the elbow joint: an anatomical and experimental study. Okajimas Folia Anat Jpn. 2002 Aug;79(2-3):55–61. doi: 10.2535/ofaj.79.55. [DOI] [PubMed] [Google Scholar]
- Meyers AB, Kim HK, Emery KH. Elbow plica syndrome: presenting with elbow locking in a pediatric patient. Pediatr Radiol. 2012 Oct;42(10):1263–6. doi: 10.1007/s00247-012-2407-1. [DOI] [PubMed] [Google Scholar]
- Bartz B, Tillmann B, Schleicher A. Stress in the human elbow joint. II. Proximal radio-ulnar joint. Anat Embryol (Berl) 1984;169(3):309–18. doi: 10.1007/BF00315636. [DOI] [PubMed] [Google Scholar]
- Steinert AF, Goebel S, Rucker A, Barthel T. Snapping elbow caused by hypertrophic synovial plica in the radiohumeral joint: a report of three cases and review of literature. Arch Orthop Trauma Surg. 2010 Mar;130(3):347–51. doi: 10.1007/s00402-008-0798-0. [DOI] [PubMed] [Google Scholar]
- Park KB, Kim SJ, Chun YM, Yoon TH, Choi YS, Jung M. Clinical and diagnostic outcomes in arthroscopic treatment for posterolateral plicae impingement within the radiocapitellar joint. Medicine (Baltimore) 2019 May;98(18):e15497. doi: 10.1097/MD.0000000000015497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner RC. Tennis elbow: diagnosis, pathology and treatment. Nine severe cases treated by a new reconstructive operation. Clin Orthop Relat Res. 1970 Sep-Oct;72:248–53. [PubMed] [Google Scholar]
- Lister GD, Belsole RB, Kleinert HE. The radial tunnel syndrome. J Hand Surg Am. 1979 Jan;4(1):52–9. doi: 10.1016/s0363-5023(79)80105-7. [DOI] [PubMed] [Google Scholar]
- Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br. 1972 Aug;54(3):499–508. [PubMed] [Google Scholar]
- Cozen Lewis N. Office orthopedics. Thomas Publisher, Springfield; 1974. [Google Scholar]
- Colozza A, Mencarani C, Fontana M, Ducati A, Staffa G. Peripheal nerve entrapment syndromes at the Elbow. In: Porcellini G, Rotini R, Stignani Kantar S, et al., editors. The elbow: Principles of Surgical Treatment and Rehabilitation. 1st edition. London: Springer Nature; 2018. [Google Scholar]
- Kotnis NA, Chiavaras MM, Harish S. Lateral epicondylitis and beyond: imaging of lateral elbow pain with clinical-radiologic correlation. Skeletal Radiol. 2012 Apr;41(4):369–86. doi: 10.1007/s00256-011-1343-8. [DOI] [PubMed] [Google Scholar]
- Sarhadi NS, Korday SN, Bainbridge LC. Radial tunnel syndrome: diagnosis and management. J Hand Surg Br. 1998 Oct;23(5):617–9. doi: 10.1016/s0266-7681(98)80015-6. [DOI] [PubMed] [Google Scholar]
- Davidson JJ, Bassett FH 3rd, Nunley JA 2nd. Musculocutaneous nerve entrapment revisited. J Shoulder Elbow Surg. 1998 May-Jun;7(3):250–5. doi: 10.1016/s1058-2746(98)90053-2. [DOI] [PubMed] [Google Scholar]
- Dinah AF, Patel VR. An unusual cause of lateral elbow pain. J Shoulder Elbow Surg. 2007 Mar-Apr;16(2):e1–3. doi: 10.1016/j.jse.2005.08.008. [DOI] [PubMed] [Google Scholar]
- McLaughlin RE 2nd, Savoie FH 3rd, Field LD, Ramsey JR. Arthroscopic treatment of the arthritic elbow due to primary radiocapitellar arthritis. Arthroscopy. 2006 Jan;22(1):63–9. doi: 10.1016/j.arthro.2005.10.013. [DOI] [PubMed] [Google Scholar]
- Krijnen MR, Lim L, Willems WJ. Arthroscopic treatment of osteochondritis dissecans of the capitellum: Report of 5 female athletes. Arthroscopy. 2003 Feb;19(2):210–4. doi: 10.1053/jars.2003.50052. [DOI] [PubMed] [Google Scholar]
- Dreyfuss U, Kessler I. Snapping elbow due to dislocation of the medial head of the triceps. A report of two cases. J Bone Joint Surg Br. 1978 Feb;60(1):56–7. doi: 10.1302/0301-620X.60B1.627579. [DOI] [PubMed] [Google Scholar]
- Spinner RJ, Goldner RD. Snapping of the medial head of the triceps and recurrent dislocation of the ulnar nerve. Anatomical and dynamic factors. J Bone Joint Surg Am. 1998 Feb;80(2):239–47. doi: 10.2106/00004623-199802000-00011. [DOI] [PubMed] [Google Scholar]
- O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991 Mar;73(3):440–6. [PubMed] [Google Scholar]
- O’Driscoll SW. Elbow instability. Hand Clin. 1994 Aug;10(3):405–15. [PubMed] [Google Scholar]
- Kinast C. “Differentialdiagnostik bei ellbogengelenksblockierungen-die subluxationsstressaufnahmetechnik” Hefte Unfallheilkd. 1986;181:339–341. [Google Scholar]
- Arvind CH, Hargreaves DG. Tabletop relocation test: a new clinical test for posterolateral rotatory instability of the elbow. J Shoulder Elbow Surg. 2006 Nov-Dec;15(6):707–8. doi: 10.1016/j.jse.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Regan W, Lapner PC. Prospective evaluation of two diagnostic apprehension signs for posterolateral instability of the elbow. J Shoulder Elbow Surg. 2006 May-Jun;15(3):344–6. doi: 10.1016/j.jse.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Atsatt R. “Loose bodies in the elbow joint: an unusual location and form”. J Bone Joint Surg Am. 1933;1008:15–9. [Google Scholar]
- Mueller T, Barthel T, Cramer A, Werner A, Gohlke F. Primary synovial chondromatosis of the elbow. J Shoulder Elbow Surg. 2000 Jul-Aug;9(4):319–22. doi: 10.1067/mse.2000.106744. [DOI] [PubMed] [Google Scholar]
- Koh S, Morris RP, Andersen CL, Jones EA, Viegas SF. Ultrasonographic examination of the synovial fold of the radiohumeral joint. J Shoulder Elbow Surg. 2007 Sep-Oct;16(5):609–15. doi: 10.1016/j.jse.2006.10.019. [DOI] [PubMed] [Google Scholar]
- Vahlensieck M, Wiche U, Schmidt HM. Plica humeroradialis: Inzidenz und MR-tomographische Darstellbarkeit [Humeroradial plica: frequency and visualization on MRI] Rofo. 2004 Jul;176(7):959–64. doi: 10.1055/s-2004-813301. [DOI] [PubMed] [Google Scholar]
- Fukase N, Kokubu T, Fujioka H, Iwama Y, Fujii M, Kurosaka M. Usefulness of MRI for diagnosis of painful snapping elbow. Skeletal Radiol. 2006 Oct;35(10):797–800. doi: 10.1007/s00256-005-0940-9. [DOI] [PubMed] [Google Scholar]
- Rosenberg ZS, Beltran J, Cheung YY. Pseudodefect of the capitellum: potential MR imaging pitfall. Radiology. 1994 Jun;191(3):821–3. doi: 10.1148/radiology.191.3.8184072. [DOI] [PubMed] [Google Scholar]
- Kang ST, Kim TH. Lateral sided snapping elbow caused by a meniscus: two case reports and literature review. Knee Surg Sports Traumatol Arthrosc. 2010 Jun;18(6):840–4. doi: 10.1007/s00167-010-1076-6. [DOI] [PubMed] [Google Scholar]
- Rajeev A, Pooley J. Arthroscopic resection of humeroradial synovial plica for persistent lateral elbow pain. J Orthop Surg (Hong Kong) 2015 Apr;23(1):11–4. doi: 10.1177/230949901502300103. [DOI] [PubMed] [Google Scholar]
- Park KB, Kim SJ, Chun YM, Yoon TH, Choi YS, Jung M. Clinical and diagnostic outcomes in arthroscopic treatment for posterolateral plicae impingement within the radiocapitellar joint. Medicine (Baltimore) 2019 May;98(18):e15497. doi: 10.1097/MD.0000000000015497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brahe Pedersen J, Kristensen PK, Mønsted P, Thillemann TM. Short-term results after arthroscopic resection of synovial plicae in the radiohumeral joint: a case series of 64 procedures. SICOT J. 2017;3:42. doi: 10.1051/sicotj/2017021. [DOI] [PMC free article] [PubMed] [Google Scholar]


