Abstract
Background:
Unscheduled care is used increasingly during the last year of life by people known to have significant palliative care needs.
Aim:
To document the frequency and patterns of use of unscheduled healthcare by people in their last year of life and understand the experiences and perspectives of patients, families and professionals about accessing unscheduled care out-of-hours.
Design:
A mixed methods, multi-stage study integrating a retrospective cohort analysis of unscheduled healthcare service use in the last year of life for all people dying in Scotland in 2016 with qualitative data from three regions involving service users, bereaved carers and general practitioners.
Setting:
Three contrasting Scottish Health Board regions and national datasets for the whole of Scotland.
Results:
People who died in Scotland in 2016 (n = 56,407) had 472,360 unscheduled contacts with one of five services: telephone advice, primary care, ambulance service, emergency department and emergency hospital admission. These formed 206,841 individual continuous unscheduled care pathways: 65% starting out-of-hours. When accessing healthcare out-of-hours, patients and carers prioritised safety and a timely response. Their choice of which service to contact was informed by perceptions and previous experiences of potential delays and whether the outcome might be hospital admission. Professionals found it difficult to practice palliative care in a crisis unless the patient had previously been identified.
Conclusion:
Strengthening unscheduled care in the community, together with patient and public information about how to access these services could prevent hospital admissions of low benefit and enhance community support for people living with advanced illness.
Keywords: After-hours care, unscheduled care, palliative care, terminal care, advance care planning, anticipatory care planning
What is already known about this subject?
People living at home with advanced progressive illness require well-coordinated services at all times of the day and night.
Early identification for generalist palliative care support and care planning in the community can improve outcomes but requires effective information sharing across services.
People with palliative care needs are high users of unscheduled care in the last months of life.
What does this paper add?
People dying with advanced organ failure accessed unscheduled community health services less often than people with cancer or frailty.
The organisation of unscheduled healthcare services is poorly understood, and current care pathways could be used more effectively in line with patient preferences.
Early identification of those requiring palliative care informs and enhances their unscheduled care; resources should be available to enable routine proactive identification.
What are the implications for practice, theory or policy?
Better resourcing of unscheduled community services for people identified for palliative care support in the community will provide safer, more responsive and cost-effective care.
Rapid access to unscheduled care via effective NHS telephone services and out-of-hours primary care assessment can reduce unwarranted ambulance calls, attendances at emergency departments and hospital admissions.
Public education should encourage and support patients and carers living with advanced illness to access the unscheduled care best suited to their needs.
Routine clinical datasets for most NHS unscheduled care services lack a variable to record patients in the community identified for palliative care.
Background
Unscheduled care is used increasingly during the last year of life by people known to have significant health-related suffering. However, most of this group are not identified prospectively for a palliative care approach. Management by busy urgent care services can lack coordination and tends to focus on urgent physical problems. 1 Avoidable hospital admissions may result. Safe and effective care 24 hours a day is a priority to enable people with palliative care needs to live safely in the community. However, palliative care integration into unscheduled care services remains challenging2–4 People at home need rapid and efficient access to urgent and emergency healthcare. Patients can opt to contact ambulance services at any time but unscheduled care in the community varies according to whether routine primary care services are open (in-hours) or closed (out-of-hours). Reviews of out-of-hours services have identified people with palliative care needs as a key group requiring improved services. 5
The World Health Organisation 6 called for early identification in primary care of people with advanced illnesses to facilitate timely palliative care. Palliative care includes proactive care planning and improves care coordination and integration with unscheduled care.7,8 Even in economically developed countries, identification of most people for this palliative approach only happens in the last months to weeks of life.9–12 People with ‘health-related suffering due to severe illness’ 13 have unpredictable episodes of deterioration before dying and depend increasingly on unscheduled care services. 14
In the UK in 2005, a new GP contract transferred responsibility for out-of-hours primary care from individual GPs and practices to local Health authorities deploying designated unscheduled primary care services for their region or area. This means that unscheduled care services are different during ‘in-hours’ (8–6 am weekdays) and out-of-hours (the rest of the time plus public holidays). During in-hours, unscheduled care in the community is provided by the patient’s usual GP surgery while during out-of-hours it is handled by a dedicated phone line (called NHS24 in Scotland and NHS Direct in the rest of the UK) and Primary Care out-of-hours hubs to which patients can be referred by the phone. Secondary care unscheduled services consisting of ambulance services, hospital emergency departments, and emergency hospital admission are available at all times. Patients may also have access to other 24/7 advice services depending on what health issues they have, where they live or whether they are registered with a hospice. If a person experiences a health crisis during out-of-hours they (or someone acting for them) may face complicated decisions about which service to call and the ramifications of so-doing. In this study we aimed to explore retrospectively which unscheduled care services had been used during the last year of life as well as prospectively asking current users about their experiences and why they made their decisions.
Methods
Design
We addressed the research question of which unscheduled healthcare services people used in their last year of life and their decision-making about accessing such care. To do this, we combined a quantitative, retrospective cohort analysis of national clinical datasets for all people dying in Scotland in 2016 with multi-perspective, qualitative research into lived experiences of accessing unscheduled NHS services from service users and professionals. We adopted an exploratory, multistage method 15 drawing on our previous study of care coordination for people towards the end of life. 16 Quantitative and qualitative data gathering were undertaken in parallel with emerging findings from each utilised to refine further analyses of both datasets. We followed the GRAMMS protocol for reporting mixed methods research and therefore we integrated and described our findings holistically rather than separating them according to the data collection method. 17 The principal investigators (Boyd, Murray) worked closely with the project lead researcher (Mason) to ensure consistent integration of the findings and full compliance with all data management procedures. The project steering group provided clinical, service management and policy expertise; with ongoing public-patient involvement (PPI) capturing lay and service user perspectives.
Setting
The retrospective cohort analysis was conducted using Scottish national datasets for people who died over a 12-month period starting from 1st January 2016. The prospective qualitative study was conducted in 2019 in three regions of Scotland chosen purposively to provide a mix of rural, urban and metropolitan locations with a total combined population of around 2,300,000. Each region consisted of the area administered by one Scottish Health Board.
Population, sampling and recruitment
The population for the retrospective cohort study consisted of all people aged 18 or over who died in Scotland during 2016. Three Scottish national datasets – National Records of Scotland (NRS) deaths, Hospital Admissions, and the Scottish Unscheduled Care Datamart (UCD) – provided a complete record of unscheduled healthcare over the last 12 months of life for each person in the study cohort. 14 Records were excluded for people under the age of 18 or if they had corrupted or incomplete data.
To understand current perspectives and experiences of service users with advanced, progressive illness, we conducted qualitative research in the three diverse regions. Research-active GP practices agreed to approach patients on their palliative care register or those with a care planning record such as an advance/anticipatory care plan or an electronic urgent care record (known as a ‘Key Information Summary’). The practice staff gained consent for a researcher to contact potential participants. The researchers discussed the study and obtained formal consent from all recruited patients and their carers. We conducted a purposive, maximum variation sample of service users with a wide range of illnesses and a mix of gender and age. The GP practices were chosen to ensure a diverse mixture of socio-economic demography.
To recruit participants for the focus groups, we worked with hospices in each Health Board region. The hospice staff identified potential participants and made initial contact. Formal consent was obtained by the researchers. Two focus groups were held with hospice outpatients, one with a pre-existing group of women with cancer, and two were with bereaved carers’ groups. We anticipated reaching data saturation with around 50 participants 18 although we anticipated that the diversity of our intended sample might require more.
Data collection
Quantitative data collection, linkage and analyses were all conducted within a secure data haven by a senior data scientist (Kerssens) from the Public Health Scotland Data and Intelligence Service. Data from the three national datasets were cleaned, validated and linked entirely within the safe haven ready for analysis. No unprocessed or identifiable data were shared with the rest of the project team. The project data management plan specified that we only collect data needed to answer the research question.
Qualitative data was generated through fieldwork conducted by the two project researchers (Mason, Laidlaw). Laidlaw focussed on the largest health board area while Mason conducted fieldwork in the other two. All interviews and focus groups with patients and carers were conducted in person while interviews with health professionals were primarily by telephone. The interviews and focus groups were conducted with a semi-structured topic guide designed in consultation with our own PPI group members and approved by the research ethics committee. All fieldwork was recorded with an encrypted digital recorder and participant identifier codes used to maintain confidentiality. Transcription was shared between the project administrator and a University of Edinburgh accredited independent transcriber. The project researchers checked each transcript and fully de-identified it. Any personal information for each participant was stored separately in an encrypted folder on the University server.
Data analysis
Quantitative data analyses
The primary analysis for the national data sets consisted of three elements. Firstly we used the ICD10 codes 19 present in the national register of deaths for the underlying cause of death to impute an ‘illness trajectory’ 20 for each person in our cohort using a methodology developed by a co-investigator (Moine 21 ) for his PhD research.
Secondly we needed to identify each service used in the dataset. The Unscheduled Care Dataset (UCD) provided details for the five unscheduled NHS services in Scotland: NHS24 (the Scottish NHS telephone advice service), primary care out-of-hours services provided by GPs and community nurses, the Scottish ambulance service, hospital emergency departments and emergency hospital admissions. A unique aspect of the UCD is that it links connected service uses together into ‘Continuous Unscheduled Care Pathways’ (CUPs). A CUP consists of one more service uses that occur within 24 hours of each other; this aims to capture the fact that multiple services may be involved in managing a single, ongoing episode of care. A CUP was defined as ‘in-hours’ if started between 9 am–5 pm on weekdays that were not a public holiday. All other CUPs were defined as ‘out-of-hours’. As a CUP was defined by the start point, an out-of-hours CUP could span both in and out-of-hours periods over several days. For example, a person who called NHS24 for advice overnight, and then had an out-of-hours GP visit at home followed by an ambulance transfer to hospital the next morning experienced one out-of-hours CUP.
Finally, individual service use was compared using Chi square tests for categorical variables including demography, and multiple logistic regression analysed multivariate associations. A health economist (Stoddart) from the Edinburgh Clinical Trials unit used a pricing dictionary to impute standard service costs. The core project team worked closely with the data scientist and economist through scheduled, regular meetings to review the quantitative data findings and guide further analyses based on emerging qualitative findings from the interviews and focus groups. We have reported the quantitative methods and findings in detail elsewhere. 14
Qualitative data analysis
The qualitative data underwent a thematic analysis. Transcripts were imported into the software package NVivo 11 and a process of exploratory, in-vivo coding 22 guided by the project’s research question was conducted in parallel with the fieldwork and quantitative data collection. The project researchers (BM, SL) coded their own transcripts then read each other’s coding. A sample of transcripts and initial coding were reviewed by PPI members then the steering group. The emergent coding frameworks were then reviewed and combined. The iterative process and cross-checking gave us confidence that we had reached data saturation once new codes stopped emerging. 23 When reporting quotes, we have removed identifiable details.
Analytical integration
Initially we had planned to create a thematic framework from the quantitative data analysis which would be used to create a framework analysis for the qualitative research. 24 Unfortunately, the length of time needed to conduct ethical review and then access and clean the data made this impossible. Consequently, after input from the steering group, we adopted an exploratory, multistage model 13 instead. This enabled us to use the emerging qualitative findings to guide the quantitative analysis and vice versa.
A stakeholder workshop using a world café method of feedback and discussion was held once results from both datasets were available and had been integrated by the research team. 25 This enabled service providers, commissioners and clinicians from unscheduled healthcare services to respond to the composite findings. Feedback from the stakeholder workshop was incorporated as data.
Ethical issues
Permission to access and link data from the Scottish Public Benefit and Privacy Panel (PBPP) for health and social care (reference 1516-0483) and approval from SE Scotland Research Ethics Committee 2 (reference 17/SS/0127) were gained. Although no issues were raised by either approval process, it was a lengthy procedure which led us to revise our data integration method. Scotland has been a pioneer in enabling effective data linkage of national datasets for health and social care research in a safe and ethical manner.
Results
This integrated, mixed method approach enabled us to quantify and describe patterns of unscheduled care use whilst also generating a thick description of experiences of accessing unscheduled healthcare and the decisions service users made when faced with a health crisis. From an epistemological standpoint we approached an understanding of out-of-hours care as socially constructed, 26 meaning that there is an ‘objectively real’ set of services but how people understand and use them is complex and emergent. A central element of the findings relates to the concept of Continuous Unscheduled Care Pathways (CUPs). A CUP consists of a linked set of services associated with a single health crisis so we present extended quotes from some participants that summarise or narrate all or part of a CUP associated with their experiences of unscheduled care.
Of the 56,407 people who died in Scotland in 2016, 49% were male (n = 27,534) and 51% female (n = 28,873); 18% were aged 18–64 (n = 10,325), 49% were aged 65–84 (n = 27,419) and 33% were 85 or older (n = 18,863). Among the cohort, 91% (n = 51,169) died with a pre-existing long-term condition: 28% from cancer (n = 15,902), 38% from organ failure (n = 21,244), 25% from frailty (n = 14,023), and 9% died from other causes (n = 5238). Thus over 90% of people were potential candidates for a palliative care approach. For ease of reading, percentages reported in the text have been rounded to whole figures while they are reported to one decimal place in tables.
For the qualitative research, we recruited 58 participants in total. We held five focus groups with a total of 19 participants (three with patients, two with bereaved carer) and semi-structured interviews with 21 patients, nine linked family carers, a bereaved carer, and eight linked GPs. The stakeholder workshop involved 18 participants.
Through integrating the qualitative, quantitative and workshop data, we identified three themes that combined to build an understanding of patient-carer journeys through unscheduled healthcare during the last 12 months of life. Although our focus is on services provided out-of-hours, unscheduled health care is a round the clock activity and out-of-hours provision is understood within that wider context.
Theme 1: Accessing unscheduled and out-of-hours NHS services
The cohort of people who died in Scotland in 2016 had 472,360 unscheduled care service contacts with the five NHS services during their last 12 months of life; 95% of them had at least one contact (Table 1).
Table 1.
Number (and percentage) of patients (18+) with contacts in the last year of life in Scotland 2016 for patients dying with cancer, organ failure or frailty.
| All | NHS 24 telephone advice (%) | Primary care out-of-hours (%) | Scottish ambulance service (%) | Emergency department attendance (%) | Emergency hospital admission (%) | |
|---|---|---|---|---|---|---|
| Total | 56,407 | 33,656 (59.7) | 30,161 (53.5) | 41,678 (73.9) | 35,383 (62.7) | 42,253 (74.9) |
| Cause of death | ||||||
| Cancer | 15,902 | 10,074 (63.4) | 9783 (61.5) | 11,569 (72.8) | 9857 (62.0) | 14,039 (88.3) |
| Organ failure | 21,244 | 11,888 (56.0) | 9678 (56.0) | 16,770 (78.9) | 13,851 (65.2) | 15,559 (73.2) |
| Frailty | 14,023 | 9258 (66.0) | 8654 (66.0) | 9509 (67.8) | 8262 (58.9) | 9314 (66.4) |
People with frailty, compared to other illness groups, used NHS 24 and primary care out-of-hours more and the other services less. People with organ failure used ambulance services and emergency departments most, but NHS24 and primary care out-of-hours the least. People with cancer had more hospital admissions per patient than individuals with other illnesses. These contacts linked into 206,841 CUPs (Continuous Unscheduled Care Pathways). Of those, 65% (n = 133,980) started out-of-hours, 28% (58,157) in-hours, and 7% (n = 14,704) were not known. Table 2 shows the initial CUP element by whether it occurred in or out of hours. The majority of work in the out-of-hours period was undertaken by the two primary care services: NHS24 and primary care out-of-hours. More ambulance calls happened in the in-hours period despite the out-of-hours period being twice as long.
Table 2.
Starting point of each CUP for patients (18+) in the last year of life in Scotland 2016 by CUP start time (in-hours or out-of-hours).
| First CUP element | In-hours | Out-of-hours | Unknown | Total |
|---|---|---|---|---|
| NHS 24 | 5203 | 70,743 | 75,946 | |
| Primary care out-of-hours | 1514 | 27,275 | 28,789 | |
| Scottish ambulance service | 37,061 | 22,408 | 59,469 | |
| Hospital emergency department attendance | 12,737 | 10,185 | 22,922 | |
| Emergency hospital admission | 978 | 13,489* | 14,467 | |
| First CUP element unknown | 1496 | 2146 | 362 | 4004 |
| Total | 56,515 | 131,589 | 13,489 | 205,597** |
A direct hospital admission does not have a time stamp just date information. This means in-hours and out-of-hours admissions cannot be differentiated on weekdays.
1,244 CUPs have not been counted in this table. 695 started with a mental health admission (not analysed in this paper) and the rest contained inconsistencies or missing elements and are not included in Table 2.
Qualitative results indicated that someone caring for the patient often made the initial contact. Unless the acute episode caused the person to be unconscious or unable to communicate, there was dialogue and sometimes a prolonged discussion before deciding which service, if any, to access.
The person who called was my son, because . . .he feels responsible. . . I don’t really want him to call the doctor, we have a sort of argument about it. . . but he wants to protect himself by calling the doctor if he’s not quite sure what to do.
(Interview, female patient with heart failure, son present)
The telephone call initially was a little bit difficult because. . . the first thing you’ve got to go through is demonstrating proof that you are the next of kin and have the individual’s authority to talk on their behalf before you can actually get to discuss the problem.
(Interview, bereaved male carer of wife with cancer)
People preferred to wait for their GP surgery to re-open. Otherwise, the decision was between ‘calling the doctor’ or ‘calling an ambulance’ with general reluctance to start a process leading to hospital admission.
If I phone an ambulance they’re duty bound to take you to the nearest hospital, and I didn’t want to go to that hospital. (Interview, male carer of wife with cancer)
Service users made decisions based on perceived problems with out-of-hours services. A common belief was that the NHS24 telephone service asked many questions and involved long waits for a call back.
I’ve never used it yet [NHS24] but I’ve heard there’s a lot of carry on with it you know. You’ve got to wait, and then phoning you back, and all the rest of it.
(Interview, female patient with multiple organ failure, no carer present)
Some practices had a ‘named doctor’ system and/or an enhanced telephone service for patients identified as being seriously ill. Service users valued this as it helped them avoid out-of-hours services, where possible. Likewise, some participants receiving oncology treatments, had access to a 24-h helpline.
I don’t have to phone a GP because I’ve got a helpline number, so I phone the helpline number direct and they deal with it. So even if it is out-of-hours I never have to go through 111 [NHS24].
(Interview, female with lung cancer having palliative chemotherapy, spouse present)
Some patients and family members had social networks of contacts with knowledge or experience of the system which helped them determine the best point of access.
I’ve got a family that would come down and take me to hospital, or something like that, because I don’t really know how the system’s working at night time.
(Interview, female with multi-organ failure, no carer present)
A younger male with liver failure illustrated the complexity around accessing unscheduled care. He tried not to call NHS24 but his neighbour called an ambulance that took him to hospital. Low self-worth due to alcohol dependency informed his decision-making and he worried about wasting professionals’ time. He did not regard himself as needing palliative care because his ‘life’s not ending”’. The following extended quote illustrates the nuances of his experience and understanding of accessing NHS services.
My liver is goosed. . . . So it’s just a matter of time before I’ll be back in the hospital again, I reckon. . . .
The only time I would phone [NHS24] is if I wasn’t well and it would really need to be quite bad for me to phone them up. If not, I usually try and hack it ‘til the morning.
I kind of don’t want to waste their time, I thought it [episode of severe abdominal pain and collapse] might have just been a daft wee thing right. I didn’t think it was going to be as bad. That’s why I would have left it until the morning.
. . .but, no they wanted me in the hospital. I’m no’ going to argue with a guy with an ambulance. He says I have to go into hospital, okey-doke! I waited till I was in a bad state. . . .
I’m a bit funny about phoning [NHS24], I feel as if my illness is due to my own self, right? Nobody forced me to drink, I just ended up getting addicted to it. And, it’s just, my life has just been fuckin’ drink. Nae hope. Nae nothin’.
I don’t know what [palliative care] is. All I know is it’s end of life. I’m only 49. My life’s not ending yet. I’m not ready. I see myself as more of a burden.
Theme 2: Use and experiences of NHS out-of-hours services
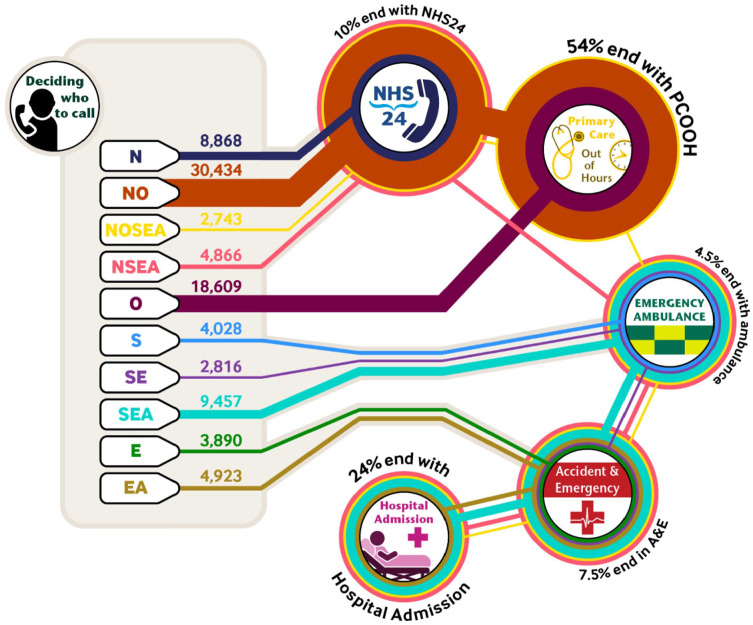
Of the cohort, 95% (n = 53,667) had at least one CUP in their last year. Most out-of-hours CUPs began with NHS 24 and were managed by telephone advice and/or primary care out-of-hours (73%), with 54% ending in primary care. Those beginning with an ambulance call usually led to secondary care via the emergency department; hospital admission occurring in 60% of cases. Figure 1 illustrates the ten most common CUPs starting out-of-hours, how patients move through services, and the numbers ending an episode with each service. The size of a service circle is proportionate to the total number of contacts with that service.
Figure 1.
Ten most common Continuous Unscheduled Pathways (CUPs) started out of hours showing point of access and pathway.
A patient with breast cancer exemplified the lived experience of an extended CUP (depicted as NOSEA in Figure 1). Initially, she and her husband disagreed until her husband finally called NHS24. The five unscheduled care services worked together, managing an acute situation safely, rapidly and effectively. The patient clearly appreciated this.
I couldn’t keep anything down. . . . I hadn’t even the strength to stand up or do anything. . . . When [Carer] got worried he thought this is gone far enough, and decided to phone out of hours. . .
When the doctor eventually did come out, he didn’t waste any time and he just said, I’m going down to the car and I’ll phone an ambulance. . . So he obviously could see it was more serious than I thought . . ...the ambulance arrived, and that was really quite a quick, a quick thing. . .
The emergency admissions unit. . . I was taken in there and they just examined you, asked a few questions, and they gave me an anti-sickness injection. . . So I was there overnight and then the next day, I was moved up the stairs to one of the wards. But yeah, everything went quite smoothly, so it did, from being taken in.
Integrating the quantitative and qualitative data show the complexity of interconnected journeys and how they interfaced with in-hours primary care and the cancer treatment helpline. A bereaved carer described calling NHS24 due to his experience of previous infections. Although this CUP began out-of-hours, it concluded in-hours with the carer choosing to speak to a familiar GP to avoid an admission. The carer valued the coordination and responsiveness of the services, and his ability to tailor use to the needs and wishes of his wife.
. . .this chest infection caused a temperature spike of up to about 37.8 or 9. . . I phoned NHS24, and they asked me a number of questions about (wife’s) symptoms. But my wife at that point was happy enough with more paracetamol and said to me, leave it alone, don’t worry about it. . .
. . .the following day, the cancer nurse that we had, we phoned her, and what [cancer nurse] was interested in was the temperature readings, and then she said, if you want you can bring her into the [unit].
I phoned our doctor surgery. . . and had an appointment for my wife forty minutes later. The doctor just said bring her in, and I’ll see her right then. . . [GP] just prescribed some generic antibiotic, something just to ease this, which it did. . . ..but what I did was phone her back the following day, [my wife] was beginning to feel a lot better, thanks very much, the temperature’s come down, she’s not clammy or sweaty the way she was.
So, it worked well. . ..the whole circle there, flowed and worked well.
Theme 3: Outcomes and learning
Figure 1 demonstrates two major patterns in the use of out-of-hours unscheduled care. One began and ended in primary care, and the other mostly resulted in an ambulance transfer to hospital. Importantly, service users not professionals made the initial access decision. Once people experienced an episode of unscheduled healthcare, they adapted their behaviour to their preferred outcome.
I have been very reluctant, to go back into [Hospital X]. And I have found the out-of-hours doctors extremely helpful in explaining why I should go in, and it not influencing me unduly, so that I can make a very informed decision
(Interview, female with cancer, carer present)
. . .with her mother a few years before, we often were up in Accident & Emergency sitting there all night. When you had that fall. . . I phoned the practice and the receptionist said you’d better get an ambulance. Other times I’ve gone through NHS24 and they’ve called the ambulance.
(Interview, male, carer for his mother who has heart failure)
Only one NHS unscheduled care dataset (primary care out-of-hours) recorded information indicating a patient had been identified for care planning or palliative care. Of all primary care out-of-hours contacts (N = 28,265), 58% (n = 17,527) had a palliative care Read code and/or a Scottish electronic care summary (KIS). (Table 3) People with cancer and those living in a care home were the most likely to be identified, compared to people dying with organ failure living at home. None of the routine datasets captured involvement of specialist palliative care for advice or urgent hospice admission. Patients and carers did not see specialist palliative care as an option for support out-of-hours.
Table 3.
Number (%) of patients (18+) who contacted PCOOH having been identified for care planning or palliative care in the last year of life in Scotland in 2016 by cause of death and place of residence (N = 28,265).
| Cause of death | Lived at home |
Lived in institution (mostly care homes) |
||
|---|---|---|---|---|
| Number | % identified | Number | % identified | |
| Cancer | 9289 | 67.4 | 558 | 73.8 |
| Organ failure | 8213 | 42.1 | 1513 | 71.6 |
| Frailty | 5128 | 54.8 | 3564 | 75.1 |
| Total | 22,630 | 55.4 | 5635 | 74.0 |
‘Various’ and ‘External’ causes of death are not shown.
GPs confirmed the value of starting an electronic urgent care record (Key Information Summary or KIS) and sharing it with all NHS unscheduled care services. Challenges included identifying patients, time taken to collate clinical information, keeping information updated and involvement/consent from patients.
He has no KIS. . . Disaster! If he was on the Gold Standard Framework he would have had a KIS. I think we’re all aware that his situation is difficult. He’s just someone that’s probably fallen through the cracks because he doesn’t shout loudly. (Interview, GP)
The KIS’s give me a constant feeling of guilt and I aspire to complete them. There’s five aspects of a KIS which is useful, but because of the amount of work that we’re doing at the moment, we’re really, really stretched, so it comes as a bit of a Cinderella task. (Interview, GP)
Co-ordination and communication between primary care teams and NHS unscheduled care services or specific helplines was challenging. GPs were keen to know their summaries had been used by other services.
. . .so she obviously used the cancer hotline on the 28th. I’ve got nothing after that to tell me what happened. She must have been assessed up there at the [hospital], but, difficult to know. . . Yeah, it bypasses us. (Interview GP)
. . .when people are seen in casualty, it says relevant information gleaned from KIS, so, you know, clearly it is being looked at, which I suppose was our worry, having done this work, who looks at it. (Interview, GP)
The stakeholder workshop looked at service pressures and improvements to out-of-hours care in the last year of life. Prior identification and an accessible, updated electronic care plan (KIS) was seen as important for effective triage by the NHS telephone advice service. Enabling other key professionals to update these care plans alongside primary care teams was highly recommended. High workload demands on primary care in-hours and out-of-hours meant primary care professionals struggled at times to deliver proactive care planning and timely assessment of patients that could potentially avoid hospital admissions.
Discussion
Main findings
Unscheduled NHS services were used by around 95% of people in Scotland during their last year of life. Over 60% of unscheduled care pathways started in the out-of-hours period: mostly by contacting the NHS telephone advice service. The most common out-of-hours care pathway, especially for frail people and care home residents, began and ended in primary care, and this was the preference of many service users. If an ambulance was called, 60% of those care pathways ended with a hospital admission.
Each episode of unscheduled healthcare was initiated by a patient or carer (or care home staff) who decided when and where to start the journey. Initial choices about how to access urgent care was a key factor in determining the final outcome. Public perceptions of ways to seek help in an emergency and personal experiences of encounters with unscheduled care services shaped their decision-making processes.
Service users described the stress of having to repeat information and long waits for a return call. Effective triage informed by an existing electronic care plan was the ideal situation for all involved. Professionals confirmed that this required reliable systems for identifying patients at risk of a health crisis, and uploading timely information to give effective access to care plans for all unscheduled care services. However, identification of people at risk of deteriorating acutely or dying in the next year was relatively difficult: especially for people with organ failure at high risk of hospital admission. The absence of routine data to drive service improvements in all but the community out-of-hours dataset was evident. Except for people currently receiving cancer treatment, no service users perceived they had enhanced access to out-of-hours care. Very few people regarded themselves as receiving or needing ‘palliative’ care. There was little understanding of the concept of future care planning.
Strengths and limitations
A major strength of this mixed methods study is its comprehensive integration of data from the five Scottish NHS unscheduled care service datasets with interviews and focus groups involving patients, families and professionals. Linking data for individual episodes and interconnected pathways of care though unscheduled healthcare services with population data provided a detailed overall picture of the unscheduled care system from a Scottish population perspective. The study included perspectives of patients, carers and bereaved carers and involved people dying from all illnesses.
The major limitation for this project is that we did not have access to national in-hours unscheduled primary care data for this 2016 cohort. Social care is vital for many people living at home in the last year of life, so a further limitation is that we did not include social care datasets. Although the Unscheduled Care Datamart did include information about admissions to mental health wards, we did not include it in this study. Some people accessed primary care out-of-hours services directly and these contacts may have included community-based services such as the Marie Curie nursing service but this could not be quantified. Our national dataset integration and analysis may not be transferrable to countries without a universal national health care system that combines primary and secondary care.
Comparison with other studies
Unscheduled care research has focussed previously on emergency department attendance and people with cancer.27–29 This study included all NHS unscheduled healthcare services and people who died from any underlying cause. Cohort studies using large administrative datasets are being used increasingly to measure healthcare systems outcomes and screen populations with serious illness for palliative care and care planning.30,31 Building on our qualitative research in Scotland from 10 years ago, 32 this study captured in detail the challenges patients and carers faced when contacting unscheduled care.
Having a specific treatment or care plan, or an ‘end-of-life’ diagnosis can be a first class ticket to more personalised care. People who lack this are potentially disadvantaged. 33 We found people with organ failure were less often identified for proactive care coordination in primary care. Canadian research showed that a palliative care approach in primary care was associated with less emergency department visits and acute admissions in patients with chronic organ failure.30,31
The frustrations experienced by service users when asked to repeat similar information, and professionals’ concerns about lack of information can be mitigated by having an electronic care summary available to all unscheduled care services. 34 Reviews of electronic care coordination systems show that these were strongly associated with more care being delivered at home. 4 Electronic care coordination systems need to record, review and share a care plan that aligns with what matters most to our sickest patients.35,36 Emergency treatment and care planning and targetted unscheduled care delivery based on predictive algorithms using data from many sources including routine national datasets can help minimise potentially preventable hospitalisations. 33
In a previous paper relating to this study, we reported costs of providing unscheduled NHS care in the community of under 4% of total unscheduled care costs despite primary care handling most out-of-hours calls. 14 Resourcing primary care and social care to manage more people who need urgent care is likely to be highly cost-effective and greatly valued by patients and their carers. 37 The WHO affirms that primary care and hospital-based care should together take a population-based planning approach, and that care should be delivered in the community, if possible. 38
Conclusions
Patients and carers prioritised safety and a timely response when accessing healthcare out-of-hours and during a health crisis. Care in the community was much preferred unless hospitalisation would be of overall benefit. Experience increased confidence and ability to navigate the health systems to meet people’s needs, but the first call may be as important as the last. Targetted patient-public information about how to access unscheduled care for people living with advanced illness coupled with proactive identification and care planning in the community are needed. Timely identification is a pre-requisite for effective anticipatory care planning and should be shared by primary and secondary care teams. To do this, the absence of coding for patients in the community identified for care planning and palliative care in all but one routine dataset should be rectified, and data capture extended to include social care and specialist palliative care.
Developments in electronic care coordination systems should facilitate data entry by all key professionals caring for a patient and offer people a patient portal to record their own priorities and wishes. Rapid access to unscheduled care via effective NHS telephone services, and primary care assessment where needed can reduce unwarranted attendances at emergency departments and hospital admissions for people at risk of needing emergency treatment and care. Better resourcing of unscheduled community services available to people with any advanced illness will provide safer, more responsive and cost-effective care.
Acknowledgments
The authors wish to acknowledge the work of Nicole Brun, project administrator, the support of the eDRIS team (National Service Scotland) for their involvement of obtaining approvals, provisioning and linking the data and the participants in interviews, focus groups and the project workshop.
Footnotes
Authorship: All listed authors assert that they:
(i) Made a substantial contribution to the concept or design of the work; or acquisition, analysis or interpretation of data,
(ii) Drafted the article or revised it critically for important intellectual content,
(iii) Approved the version to be published,
(iv) Have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Data sharing: More information (including de-identified data tables and topic guides) is available from the corresponding author on reasonable request.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Marie Curie and Chief Scientist Office Scotland, combined grant MCRGS-07-16-37.
ORCID iDs: Bruce Mason  https://orcid.org/0000-0002-9304-3362
https://orcid.org/0000-0002-9304-3362
Scott A Murray  https://orcid.org/0000-0002-3819-2912
https://orcid.org/0000-0002-3819-2912
Anne Finucane  https://orcid.org/0000-0002-3056-059X
https://orcid.org/0000-0002-3056-059X
References
- 1. Murtagh FE, Bausewein C, Verne J, et al. How many people need palliative care? A study developing and comparing methods for population-based estimates. Palliat Med 2014; 28(1): 49–58. [DOI] [PubMed] [Google Scholar]
- 2. Best S, Tate T, Noble B, et al. Research priority setting in palliative and End of life care: the James Lind approach consulting patients. BMJ Support Palliat Care 2015; 5(1): 102.1–10102. [Google Scholar]
- 3. Henson LA, Higginson IJ, Gao W. What factors influence emergency department visits by patients with cancer at the end of life? Analysis of a 124,030 patient cohort. Palliat Med 2018; 32(2): 426–438. [DOI] [PubMed] [Google Scholar]
- 4. Leniz J, Weil A, Higginson IJ, et al. Electronic palliative care coordination systems (EPaCCS): a systematic review. BMJ Support Palliat Care 2020; 10(1): 68–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. The Scottish Government. Pulling together: transforming urgent care for the people of Scotland. Edinburgh: The Scottish Government, 2015. [Google Scholar]
- 6. World Health Organization. Integrating palliative care and symptom relief into primary health care. Geneva, Switzerland: WHO, 2018. [Google Scholar]
- 7. Daveson BA, Harding R, Shipman C, et al. The real-world problem of care coordination: a longitudinal qualitative study with patients living with advanced progressive illness and their unpaid caregivers. PLoS One 2014; 9(5): e95523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Murray SA, Kendall M, Mitchell G, et al. Palliative care from diagnosis to death. BMJ 2017; 356: j878. [DOI] [PubMed] [Google Scholar]
- 9. Tapsfield J, Hall C, Lunan C, et al. Many people in Scotland now benefit from anticipatory care before they die: an after death analysis and interviews with general practitioners. BMJ Support Palliat Care 2019; 9(4): e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Arias-Casais N, Garralda E, Rhee JY, et al. EAPC atlas of palliative care in Europe 2019. Vilvoorde, Belgium: EAPC Press, 2019. [Google Scholar]
- 11. Hopkins SA, Bentley A, Phillips V, et al. Advance care plans and hospitalized frail older adults: a systematic review. BMJ Support Palliat Care 2020; 10(2): 164–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tanuseputro P, Budhwani S, Bai YQ, et al. Palliative care delivery across health sectors: a population-level observational study. Palliat Med 2017; 31(3): 247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Radbruch L, De Lima L, Knaul F, et al. Redefining palliative care—a new consensus-based definition. J Pain Symptom Manag 2020; 60: 754–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mason B, Kerssens JJ, Stoddart A, et al. Unscheduled and out-of-hours care for people in their last year of life: a retrospective cohort analysis of national datasets. BMJ Open 2020; 10(11): e041888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. 3rd ed. Los Angeles; CA: SAGE Publications Inc, 2018. [Google Scholar]
- 16. Mason B, Epiphaniou E, Nanton V, et al. Coordination of care for individuals with advanced progressive conditions: a multi-site ethnographic and serial interview study. Br J Gen Pract 2013; 63(613): e580–e588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O’Cathain A, Murphy E, Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy 2008; 13(2): 92–98. [DOI] [PubMed] [Google Scholar]
- 18. Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods 2006; 18(1): 59–82. [Google Scholar]
- 19. World Health Organization. ICD10: International statistical Classification of diseases and related health problems version 10th revision. Geneva, Switzerland: WHO, 2010. [Google Scholar]
- 20. Murray SA, Kendall M, Boyd K, et al. Illness trajectories and palliative care. BMJ 2005; 330(7498): 1007–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moine S. How to better visualise the distribution of expected annual deaths in a “Standard” French GP surgery? Rebuilding the three main illness trajectories through a modified delphi study. Palliat Med 2016; 30: Abstract FC51. [Google Scholar]
- 22. Manning J. In Vivo coding. In: Matthes J. (ed.) The International Encyclopedia of Communication research methods. New York, NY: Wiley-Blackwell, 2017, pp.1–2, (Major Reference Works). [Google Scholar]
- 23. Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018; 52(4): 1893–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gale NK, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013; 13(1): 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. The World Cafe. The world cafe. http://www.theworldcafe.com/ (accessed 8 June 2020.)
- 26. Andrews T. What is social constructionism? Grounded theory. Rev An Int J 2012; 11(1): 1. [Google Scholar]
- 27. Mills S, Buchanan D, Guthrie B, et al. Factors affecting use of unscheduled care for people with advanced cancer: a retrospective cohort study in Scotland. Br J Gen Pract 2019; 69(689): e860–e868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mills SEE, Geneen LJ, Buchanan D, et al. Factors associated with unscheduled care use by cancer decedents: a systematic review with narrative synthesis. BMJ Support Palliat Care. Epub ahead of print 2020. October 13. DOI: 10.1136/bmjspcare-2020-002410 [DOI] [PubMed] [Google Scholar]
- 29. Worth A, Boyd K, Kendall M, et al. Out-of-hours palliative care: a qualitative study of cancer patients, carers and professionals. Br J Gen Pract J R Coll Gen Pract 2006; 56(522): 6–13. [PMC free article] [PubMed] [Google Scholar]
- 30. Quinn KL, Stukel T, Stall NM, et al. Association between palliative care and healthcare outcomes among adults with terminal non-cancer illness: population based matched cohort study. BMJ 2020; 370: m2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brown CR, Hsu AT, Kendall C, et al. How are physicians delivering palliative care? A population-based retrospective cohort study describing the mix of generalist and specialist palliative care models in the last year of life. Palliat Med 2018; 32(8): 1334–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mason BL, Donaldson AD, Epiphaniou E, et al. Coordination of care for people at risk of dying in the next 12 months: a multi-site prospective study and consensus seeking exercise. NIHR Health Services Research and Delivery Programme, London, 2013. [Google Scholar]
- 33. Martin CM, Sturmberg JP, Stockman K, et al. Anticipatory care in potentially preventable hospitalizations: making data sense of complex health journeys. Front Public Health 2019; 6(Jan): 376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Standing H, Patterson R, Lee M, et al. Information sharing challenges in end-of-life care: a qualitative study of patient, family and professional perspectives on the potential of an electronic palliative care co-ordination system. BMJ Open 2020; 10(10): e037483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lamas D, Panariello N, Henrich N, et al. Advance care planning documentation in electronic health records: current challenges and recommendations for change. J Palliat Med 2018; 21(4): 522–528. [DOI] [PubMed] [Google Scholar]
- 36. Resuscitation Council UK. ReSPECT: recommended summary plan for emergency care and treatment. https://www.resus.org.uk/respect (accessed 25 February 2021).
- 37. Luta X, Diernberger K, Bowden J, et al. Healthcare trajectories and costs in the last year of life: a retrospective primary care and hospital analysis. BMJ Support Palliat Care. Epub ahead of print 2 December 2020. DOI: 10.1136/bmjspcare-2020-002630 [DOI] [PubMed] [Google Scholar]
- 38. Reynolds TA, Guisset A-L, Dalil S, et al. Emergency, critical and operative care services for effective primary care. Bull World Health Organ 2020; 98(11): 728–728A. [DOI] [PMC free article] [PubMed] [Google Scholar]