Abstract
Background: The communication of the diagnosis of breast cancer induces to the patient a strong psychological trauma. Radiologists are at the forefront of communicating, either for a biopsy or the probable diagnosis of malignancy. This is a complex task, which requires the knowledge and application of correct “communicative models”, among which the SPIKES protocol represents a fundamental reference.
Design and methods: 110 patients, with a history of breast cancer, filled out a questionnaire consisting of six questions: five aimed at defining communication compliance with the SPIKES protocol, the sixth, consisting of six feelings, aimed at the knowledge of the next emotional state.
Results: Regarding compliance with various “strategic points” of the SPIKES protocol, questionnaires show that 70% of patients reported no omissions, while the remaining 30% reported omissions relatively to perception (56%), emotions (23%), setting (13%), knowledge (6%) and invitation (2%). The results showed the existence of a correlation between the final emotional state and the correct application of the SPIKES protocol; in fact, patients who reacted with a positive final emotional state-reported greater adherence to the strategic points of the SPIKES protocol.
Conclusions: In healthcare, knowing the communicative compliance of a team in giving “bad news” is fundamental, especially in breast cancer. The SPIKES protocol is recognized by the Literature as a fundamental reference able to affect “positively” the emotional state of patients. The proposed questionnaire is a valid tool to identify the weak points of communication and related criticalities, to improve clinical practice.
Significance for public health.
The attention of the scientific community is often focused on analyzing the pathologies that afflict the human being, and more frequently there is a tendency to overshadow what is the interpersonal relationship with the patient, which is what underlies the trust relationship that must necessarily be established between doctors and patients to facilitate a correct diagnostic and therapeutic process. In this study, we tried to understand what the weaknesses of our approach may be to breast cancer diagnosis communication, to improve our communication skills and offer a better service. We propose an easily reproducible protocol aimed at highlighting the criticalities of an extremely delicate process that every Breast Team must face daily.
Key words: Bad news, patient communication, breast cancer, breast imaging
Introduction
The incidence of breast cancer is the main cause of death in women between the ages of 40 and 55 and is constantly growing, knowing no geographical limits; this is due both to the increase in life expectancy and the adoption of Western lifestyles also in developing countries.1 The diagnosis of breast cancer has a high emotional impact, as it undermines the integrity of a woman, leading to a dissociation between mind and body and a sense of transition from “I can” to “I can’t”. The moment of diagnosis is therefore a traumatic event that gives rise to feelings of anger, producing effects on the psyche and the physical.2 Hence the importance of proper pre-diagnostic - diagnostic communication, to minimize the emotional impact on the patient.
In contrast to what happened in the ‘50s and ‘60s, today it is considered fundamental to correct communication of the actual diagnosis, it is understood that by the doctor there must be adequate expertise in dealing with bad news. From a general point of view, we can define as bad news “any information that, with a negative effect, seriously influences the vision of the future life”. Bad news should always be understood from the perspective of the recipient and it is not possible to estimate the impact without knowing the expectations and the degree of understanding of the receiver.3 In the case of breast cancer, the negative consequences of diagnosis communication are closely linked to a number of factors ranging from fear of death to a sense of shame, from fear of pain to concern for body change, including loss of physical attractiveness. 4 The radiologist doctor is asked to communicate both the suspect and the confirmation of a diagnosis of breast cancer; it is deduced the need for multiple skills and adequate training on communication. 5-10 From the foregoing, it is necessary to identify tools that allow a self-assessment, systematic and periodic, of the communicative compliance of a team, in order to study the criticalities and to improve, more and more, the communicative potential.
The aim of our work was to test a questionnaire aimed at assessing, retrospectively, the Compliance of a team of Radiologists in communicating the diagnosis of breast cancer and to identify critical issues in the communicative process, in order to improve information procedures. The team of medical radiologists, senologists, whose compliance in giving correct information has been verified is composed of 3 radiologists in service near the section of Senology for a minimum of six years.
Design and methods
At the Institute of Radiology of the Maggiore Hospital in Novara, an anonymous questionnaire, with obligatory multiple choice, is prepared to be submitted to patients operated for at least five years for breast cancer and who had completed the therapeutic process; 110 patients were enlisted, aged between 40 and 90 years.
The design of the study and the questionnaire were approved by the Ethics Committee of the EC Study 129/20. The questionnaire included six questions, divided into two groups of questions: The first group tested the adequacy of the information with respect to the SPIKES protocol;4-6-7 the second was aimed at identifying the state of mind of the patient in the period following the communication of the diagnosis.
Subsequently, the data deriving from the two groups of questions were cross-referenced in order to verify the complicity and the possible criticality of the communicative appropriateness of the team of radiology senologists.
The data were collected in a 110 x 8 matrix with the following variables (Table 1):
Sequence number
Patient’s age
5 closed questionnaire replies related to the application of the different moments of the SPIKES protocol
1 indicator of the patient’s state of mind after the information
The closed answers related to the SPIKES4,6,7 protocol concerned the application or not of the following steps (Table 2):
Setting
Perception
Invitation
Emotions
Knowledge
Strategy
Of the six steps, of which the protocol is constituted, the first four concern the information that the doctor must provide and receive in order to establish the will of the patient to be informed or not and the relative modalities. The fifth concerns the empathic behavior of the doctor and his ability to relate to the patient, while the sixth concerns the planning of therapy.
Table 1.
Multiple choice questionnaire, divided into two parts: the first aimed at investigating the correct implementation of the SPIKE protocol, the second identifying the state of mind of the patients at the end of the interview.
| Question | Yes | No | ||
|---|---|---|---|---|
| (Tick the box corresponding to the chosen option) | ||||
| 1 | Was the diagnosis communicated to you in a calm and peaceful environment? | |||
| 2 | Were you asked what you knew about your illness and how much did you want to be informed? | |||
| 3 | Did the doctor use simple and understandable terminology to communicate the diagnosis? | |||
| 4 | Was the doctor able to understand your reaction and identify the reasons of greatest concern? | |||
| 5 | Did the doctor leave room for your questions and check the understanding of what was explained? | |||
| 6 | How did you feel when you left the clinic? | |||
| Panic | ||||
| Anguish and fear | ||||
| Depression and sadness | ||||
| Anxiety and uncertainty about the future | ||||
| Anxiety but with confidence for the future | ||||
| Peace of mind and confidence 26 for the future |
Table 2.
Six points SPIKES protocol representation and their implementation.
| SPIKES protocol | Practical implication |
|---|---|
| Setting | • Arrange for privacy |
| • Proactively manage time constraints | |
| • Make eye contact | |
| • Silence phone | |
| Perception | • Use open-ended questions to understand patient’s perception of the medical situation |
| • “What do you understand about the course of your illness to this point?” | |
| Invitation | • Ask patient how much they want to know |
| • Get permission to disclose bad news | |
| Knowledge | • Share information about diagnosis and prognosis; give information in small chunks and periodically check patient’s under |
| standing | |
| Empathize with emotions | • Watch for signs of emotions |
| • Identify the emotion and the reason for it | |
| • Respond empathically | |
| Strategy | • Plan a strategy for the future |
The indicator of the state of mind of the patient assumed the following feelings:
Panic
Anguish and fear
Depression and sadness
Anxiety and uncertainty for the future
Anxiety but with confidence in the future
Serenity and confidence in the future
In the first phase a pre statistical analysis was carried out to evaluate the frequency distribution of some variables:
Distribution of attendance by age groups
Frequency distribution of omission reports with respect to different SPIKES protocol steps
Frequency distribution of states of mind after diagnosis communication.
Subsequently, the original sample of 110 cases analyzed was divided into two sub-groups: the first included all patients who reported negative moods in the questionnaire between 1 and 4 (panic, anxiety and fear, depression and sadness, anxiety and uncertainty for the future); in the second were included positive moods between 5 or 6 (anxiety but with confidence in the future, serenity and confidence in the future).
Starting from the state of mind of the patients it has been correlated to the respect of the various points indicated in the protocol spikes, in order to identify which strategic points, during the communication, have been omitted and/or neglected.
The proportions in which omissions in the application of the different moments of the protocol were reported in the two subgroups, were elaborated with the T-Student Test to ascertain the existence of statistically significant differences, assuming a normal distribution.
Results
The questionnaire was submitted to 110 patients with an average age of 62.4 (Figure 1). Relative to the age range, 66% of patients were included in the 50-80 average range, the time window in which breast cancer is the main cause of death, 12% of patients in the range of 40-49 years, 28% in the range of 50-59 years, 25% in the range 60-69 years, 23% in the 70-79 years group, 9% in the range 80-89 years and the 3% of patients were over 90 years old. As regards the assessment of the responses provided on the proper implementation of the SPIKES protocol, these showed that 70% of the patients interviewed indicated that they had not found any omissions at the time of the diagnosis communication.
In the remaining 30% of cases, there was an omission of the various steps suggested in the SPIKE protocol, related to perception 56% of the reports, to emotions in 23%, to setting in 13%, to knowledge in 6% and to invitation in 2% (Figure 2). After the announcement of the diagnostic suspect, the news generated a feeling of anxiety associated with confidence in the future in 26% of patients, a feeling of serenity and confidence in 21% of anguish and fear in 20%, of panic and anxiety associated with uncertainty in the future in 15%, while of sadness in 2% (Figure 3).
Depending on the emotional state “ positive or negative “ after receiving the news, the patients were finally included in two cohorts: the first, included 52 patients with manifested “ positive emotional state” marked by feelings of serenity and confidence, even in a natural anxious context. The second included 58 patients with manifested “negative emotional state “ marked by feelings of panic, fear, depression, anxiety and uncertainty for the future. In the context of each cohort, compliance with the various steps of the SPIKES protocol (Figure 4) has been verified. Regarding patients with manifested “ positive emotional state” the various steps of the SPIKES protocol were respected in the following percentages: setting 98%, perception 81%, invitation 100%, knowledge 96%, and emotions 94%. Regarding patients with manifested “ negative emotional state “ the various steps of the SPIKES protocol were respected in the following percentages: setting 87%, perception 62%, invitation 93%, knowledge 90% ed emotions 78%. The differences between the proportions of the cases reported in the two cohorts, related to the five steps of the protocol, subjected to significance tests with normal distribution assumptions of the standardized variable, were all significant at the level of 0.05 except for the one associated with K (knowledge) pass.
Figure 1.

Our sample demographic distribution.
Figure 2.

Percentage of failure to implement the various steps of SPIKE protocol.
Figure 3.
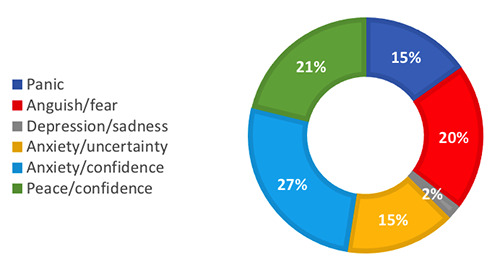
Patients' emotional state after the diagnosis communication.
Figure 4.

SPIKE protocol application frequency.
Discussion
The assessment of the compliance of a team in communicating bad health news involves careful work that has its times; in fact, we wonder if the evaluation should be subject to immediate verification or whether it should be evaluated over time. The retroactivity of the information could represent a limit of our work, but it is out of the question that the proposition of a questionnaire in the immediate is conditioned by the state of mind of the patients. Therefore, in our work, we preferred to propose it later, when the emotional state is controlled and the judgment by patients is more objective. The choice of assessing the compliance of a team and not of the individual professional could in fact represent a limit of this work; being the first experience and considered the teamwork, supported by years of joint work and sharing, in this preliminary work we have aimed at developing group compliance and not individual professional compliance. In our experience, from the analysis of the questionnaires submitted to our patient sample, a correlation has been demonstrated between the emotional state of the patients and the application of the SPIKES protocol. Patients who have shown emotional states of panic, fear, depression, anxiety and uncertainty have reported, more frequently than patients characterized by greater serenity and confidence, the omission of some steps of the SPIKES protocol. In particular, the main deficiencies were identified, with regard to perception, which consists in understanding the patient’s ideas about the disease and its readiness to be informed, and the emotions, the empathic management of the patient’s emotional reaction.
With regard to compliance with the perception step (reported by 82% of patients with “positive emotional state” against 62% of patients with “negative emotional state”), it should be stressed that the doctor should ask before informing.11 It is appropriate to explore what the patient already perceives of the clinical situation and verify the realistic measure of perception or whether negation mechanisms are put in place.12 These aspects are essential to weigh the information, in the form and to the extent that it needs to be given, on the basis of the awareness expressed by the patient. As for compliance with the emotions step it was reported in 94 % of patients with “positive emotional state” compared to 78% of patients with “negative emotional state”. Emotional reactions can be different, and the doctor cannot limit himself to an automatic and instantaneous reassurance but must adapt his response to each patient, based on observation of the emotions expressed by the patient and identification of the thoughts associated with them. This is done through dialogue and the formulation of targeted questions, which will therefore allow the doctor to respond with empathy, showing his participation in the life of the patient.13-15
The patient who can express his concerns in the presence of an attentive and empathetic doctor feels understood and supported, the other way around will develop a sense of generalized anxiety that interferes negatively with the therapeutic path.14,16-18 The respect of emotion and perception have represented, in our cases, the elements of greatest communicative weakness The existence of a significant difference in the application of the SPIKES protocol between the two cohorts, does not necessarily imply the existence of a cause and effect relationship between, for example, the lower empathic charge offered by the doctor and the state of panic and fear of the patients, but it indicates a direction in which to direct attention to improve the effects of communication on the emotional state of the patient. The communication of the diagnosis is not a moment but a process, a sequence that aims to correctly inform the patient, to form a therapeutic alliance between doctor and patient. In the case of breast cancer, the radiologist accompanies the patient in this process, from the suspicion of the disease to confirmation of the diagnosis. The knowledge and application of the various steps suggested by the SPIKES protocol allow the doctor to establish in a correct way the most suitable methods, language, and timing to carry out diagnosis communication, empathetically with the patient for proper therapy planning. However, the guidelines are not always sufficient to fulfill this task comprehensively; it is, therefore, important that the doctor can try to train himself in the communicative field, dealing with the available literature, with experts, and with his working environment. In order to investigate the real communication skills of a breast therapy team, the experience gained, thanks to a dedicated questionnaire, has allowed verification of the data emerged, identifying and discussing the major issues.
Our preliminary experience suggests the need for a systematic and/or periodic verification, through questionnaires, eventually customized, aimed at improving and optimizing communicative accomplices, which are an integral part of good clinical practice.
References
- 1.Siegel RL, Miller KD, Fuchs H, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin 2021:71:7-33. [DOI] [PubMed] [Google Scholar]
- 2.Del Piccolo L. [La comunicazione della diagnosi di tumore al paziente e ai familiari: linee guida].[Article in Italian]. Recenti Prog Med 2007;98:271-8. [PubMed] [Google Scholar]
- 3.Baile WF, Kudelka AP, Beale EA, et al. Communication skills training in oncology: Description and preliminary outcomes of work-shops on breaking bad news and managing patient reactions to illness. Cancer 1999;86:887-97. [PubMed] [Google Scholar]
- 4.Adler DD, Riba MB, Eggly S. Breaking bad news in the breast imaging setting. Acad Radiol 2009;16:130. [DOI] [PubMed] [Google Scholar]
- 5.Buckman R. Breaking bad news: Why is it so difficult? BMJ 1984;288:1597-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buckman R. How to break bad news: A guide for health professionals. Baltimore: Johns Hopkins Press; 1992. [Google Scholar]
- 7.Baile WF, Buckman R, Lenzi R, et al. SPIKES: A six-step protocol for delivery bad news—Application to the patient with cancer. Oncologist 2000;5:302-11. [DOI] [PubMed] [Google Scholar]
- 8.Leydon GM, Boulton M, Moynihan C, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ 2000;320:909-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barnett MM. Effect of breaking bad news on patients’ perceptions of doctors. J R Soc Med 2002;95:343-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mills ME, Sullivan K. The importance of information giving for patients newly diagnosed with cancer: a review of the literature. J Clin Nurs 1999;8:631-42. [DOI] [PubMed] [Google Scholar]
- 11.Gorniewicz J, Floyd M, Krishnan K, et al. Breaking bad news to patients with cancer: A randomized control trial of a brief communication skills training module incorporating the stories and preferences of actual patients. Patient Educ Couns 2017;100:655-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zøylner IA, Lomborg K, Christiansen PM, Kirkegaard P. Surgical breast cancer patient pathway: Experiences of patients and relatives and their unmet needs. Health Expect 2019;22:262-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ptacek JT, Eberhardt TL. Breaking bad news: a review of the literature. JAMA 1996;276:496–502. [PubMed] [Google Scholar]
- 14.Harvey JA, Cohen MA, Brenin DR, et al. Breaking bad news: a primer for radiologists in breast imaging. J Am Coll Radiol 2007;4:800-8. [DOI] [PubMed] [Google Scholar]
- 15.van Vliet LM, Francke AL, Meijers MC, et al. The use of expectancy and empathy when communicating with patients with advanced breast cancer; an observational study of clinician- patient consultations. Front Psychiatry 2019;10:464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cao W, Qi X, Yao T, et al. How doctors communicate the initial diagnosis of cancer matters: cancer disclosure and its relationship with patients’ hope and trust. Psychooncology 2017;26:640-8. [DOI] [PubMed] [Google Scholar]
- 17.Boisserie-Lacroix M, Duguey-Cachet O, Stadelmaier N, et al. Establishment of a consultation to announce the results of a breast biopsy. Diagn Interv Imaging 2014;95:595-9. [DOI] [PubMed] [Google Scholar]
- 18.Westendorp J, Stouthard J, Meijers MC, et al. The power of clinician- expressed empathy to increase information recall in advanced breast cancer care: an observational study in clinical care, exploring the mediating role of anxiety. Patient Educ Couns 2021;104:1109-15. [DOI] [PubMed] [Google Scholar]


