Abstract
Among people with ST-segment elevation myocardial infarction (STEMI), high alexithymia was associated with delay to hospital arrival. High alexithymia could be a determinant of early death in the long term after STEMI. People with STEMI who participated in a survey in 2011, was tested about the state of life in 2021. The sample was divided into two cohorts (cut-off: TAS- 20≥61 in 2011). The relationship between possible death occurred and having high alexithymia was calculated by comparing the mortality after 10 years in the two cohorts through the Cox’ proportional hazard model. Status in life was verified on 39.3% of the sample. No differences were found regarding age, sex, high alexithymia between individuals on whom it was possible to verify the state in life and in whose it was not. In 2021, among people having high alexithymia in 2011, a higher risk of early death was found (RR=5.75, CI 95% 1.116-29.637).
Significance for public health.
Among people with ST-segment elevation myocardial infarction (STEMI), high alexithymia is associated with delay to hospital arrival. High alexithymia could be a determinant of early death in the long term after STEMI. Although the results of this study are preliminary, they highlight a relevant prognostic factor, alexithymia, in relation to the long-term course of post-myocardial infarction, condition responsible for more than 7 million deaths each year. As known, alexithymia may be improved with adequate interventions of recognized efficacy. This means that a significant proportion of early deaths among people with previous STEMI could be avoided through an adequate intervention on alexithymia.
Key words: Alexithymia, STEMI, cardiology, death risk
Introduction
A study published over ten years ago found that, in people coming to hospital for ischemic acute heart attack (acute myocardial infarction with ST segment elevation, STEMI), a high score on the Toronto Alexithymia Scale (TAS-20),1 was associated with an excessive delay from time of the first onset of symptoms of hearth attack to hospital arrival and treatment.2 This result found further confirmation in systematic reviews with meta-analyses3,4 and in a new study conducted by the same group on a larger sample size and with more restrictive inclusion criteria.5As known the time between early acute myocardial infarction (AMI) symptoms and the arrival in a hospital for seeking care is a crucial factor for survival. An early reperfusion limits the necrosis of the myocardial tissue and if reperfusion does not occur within two hours from symptoms onset, survival decreases drastically.6
As reported by the most recent contributions,7 alexithymia is a cognitive deficit in emotional processing that could not allow to properly differentiate bodily sensations (thus signals of illness) from affects’ arousal, with restricted imaginal activity. As one of the most relevant elements related to time to reperfusion treatment is the patient’s decision to delay seeking care, it is intuitive that having strong alexithymia traits can determine indecision, difficulty in recognizing the severity of the symptoms8 and therefore can be associated with the delay and with the probability of survival from the acute episode.
The studies conducted so far have examined patients who survived an acute myocardial infarction during the first days after hospitalization and intervention. However, if the alexithymia traits can cause a delay in seeking treatment, it is also possible that it can have a negative effect in the post-infarct course. This could happen both because people with alexithymia may not adequately cope with a new myocardial infarction (relevant for the course and not rare), with angina attacks (relevant for the course and frequent) but also because it is known that alexithymia can negatively influence the course and treatment of anxiety and depressive disorders,9,10 that typically impairs outcome after AMI. Our study hypothesis is thus that a high alexithymia, measured immediately after hospitalization at the time of an acute STEMI, could be a determinant of early death in the long term.
Design and methods
The study was conducted on a cohort of 83 people with STEMI who had participated in the previously mentioned survey in 2011 that was aimed at investigating the association between alexithymia and delay in calling for help2 using the TAS-20 for measuring of alexithymia.
In 2021, the state of life of these people was verified based on the allowed contacts on the clinical documentation. Each medical record contained a telephone number of a family member or friend who could be asked for information. This number had been provided by the same patient who had given consent for a possible contact. Given the current privacy law, this was the only number that could be contacted. In case the number was changed (and often it was) or no one answered, it was not possible to conduct further investigations.
The interviewers gave comprehensive information by phone about health and state in life of the patient if a relatives/friend was traceable. The whole sample of traced people was divided into two cohorts according to the alexithymia scores reported in the previous study based on the predefined cut-off of TAS-20 ≥61 which identifies people with high alexithymia.
The relationship between the dependent variable (possible death occurred) and having high alexithymia was calculated by comparing the mortality at 10 years in the two cohorts (exposed and not exposed to high alexithymia) through Kaplan-Meier analysis and the proportional hazard model of Cox, using as covariables age (continued) and gender. The study was conducted after approval by the independent ethics committee of the University Hospital of Cagliari in accordance with the Helsinki agreements and national and European Union laws on privacy.
Results
The status in life was verify of only on 33 people (39.3% of the whole sample). However, a comparison according to age, sex and number of people with TAS score <61 between the group of individuals on whom it was possible to verify the state in life (n=33) and the group in which it doesn’t (N=50), showed no difference in the two groups (Table 1). In people on whom it was possible to verify the state in life, the Table 2 show the condition of been alive in September 2021 in the cohort of those having high score at TAS 20 in 2011 and those do not, the comparison found a higher risk of early death in the group with previous high alexithymia [Log Rank Mantel-Cox = 6.899, 1 df, p=0.009; RR=5.75 (CI 95% 1.116-29.637)], the result is coherent with that calculated with Kaplan- Meier analysis which results is shown in Figure 1.
Discussion
The strict European laws on the respect of privacy and the fact that having operated in the record of an emergency unit that did not follow the patients over time allowed to verify the status in life among only 39.3% of the whole sample. This is an obvious limitation of our study, even if the sample of people whose life we have been able to ascertain does not differ for important determinants of possible death (including the frequency of people with high alexithymia) from the sample of people not traced.
The results of this study, however, are so relevant that they can set our study as a milestone towards future research. In fact, our results highlight a relevant prognostic factor, alexithymia, in relation to the long-term course of post-myocardial infarction, condition responsible for more than 7 million deaths each year.11 The percental of death due to a fist myocardial infarction is estimated to be 23% before the arrive to hospital for care, 4.1% during hospitalization;12 9.8 % during the first year after hospital discharge13 and 5% per year in each subsequent year.11 After 15 years from acute event, cumulative mortality can reach 70%. The outcome worsened in case of a second myocardial infarction.11 These figures explain the public health relevance of our data should it be confirmed.
Figure 1.
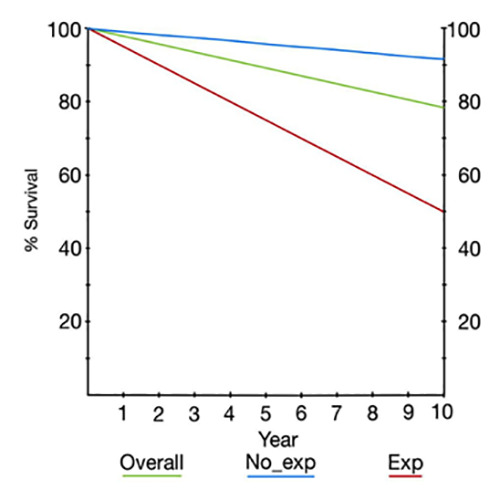
Survive analysis in the overall cohort and in exposed and not expose to high alexithymia.
Table 1.
Comparison between individuals on whom it was possible or not to verify the state in life.
Table 2.
Been alive in September 2021 in the two cohorts.
| Cohort | Total n | Deaths on September 2021 | Incidence /10 years x 100 |
|---|---|---|---|
| Exposed to high alexithymia in 2011 | 10 | 5 | 50.0 |
| Not exposed to high alexithymia in 2011 | 23 | 2 | 8.7 |
| Overall | 33 | 7 | 21.2 |
Log Rank (Mantel-Cox) =6.899, 1 df, p=0.009, RR=5.75 (CI 95% 1.116-29.637); c2 with Yates correction = 4.858, RR=5.75 (CI 95% 1.116-29.637).
As known alexithymia may be improved with adequate interventions of recognized efficacy.14,15 This means that, if our data were confirmed, a significant proportion of early deaths could be avoided through an adequate intervention on alexithymia.
Although our data, as affirmed before, are preliminary, our study lays the foundation for prospective multicenter studies in which to confirm our hypothesis. The study also lays the basis for the possibility of the privacy managers, to agree of a more extensive investigation through further methods of verifying the status in life (for example, requesting the registry offices of the municipalities of residence). This type of methodology is, in fact, granted only in cases of proven importance by the so-called privacy guarantors according to the diction of the European law and this study provides the necessary clinical evidence. On the other hand, it would be possible, but not ethically correct, to conduct verification studies in countries with less restrictive rules on the verification of life status in scientific studies.
Funding Statement
Funding: This article has been developed within the framework of the Research Project financed with the resources of the P.O.R. SARDEGNA F.S.E. 2014-2020 - Axis III "Education and Training, Thematic Objective: 10, Specific Objective: 10.5, Action of the fi Partnership Agreement: 10.5.12 "Call for proposals for the funding of research projects – Year 2017".
References
- 1.Bressi C, Taylor GJ, Parker JDA, et al. Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: an Italian multicenter study. J Psychosom Res 1996;41:551–9. [DOI] [PubMed] [Google Scholar]
- 2.Carta MG, Sancassiani F, Pippia V, Bhat KM, et al. Alexithymia is associated with delayed treatment seeking in acute myocardial infarction. Psychother Psychosom 2013;82:190-2. [DOI] [PubMed] [Google Scholar]
- 3.Preti A, Sancassiani F, Cadoni F, Carta MG. Alexithymia affects pre-hospital delay of patients with acute myocardial infarction: meta-analysis of existing studies. Clin Pract Epidemiol Ment Health 2013;9:69-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sancassiani F, Montisci R, Preti A, et al. Surviving to acute myocardial infarction: The role of psychological factors and alexithymia in delayed time to searching care: A systematic review. J Clin Med 2021;10:3813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meloni L, Montisci R, Pippia V, et al. Alexithymia affects the time from symptom onset to calling the emergency system in STEMI patients referred for primary PCI. Int J Cardiol 201615;219:428-32. [DOI] [PubMed] [Google Scholar]
- 6.Giugliano RP, Braunwald E. TIMI Study Group: Selecting the best reperfusion strategy in ST-elevation myocardial infarction: it’s all a matter of time. Circulation 2003;108:2828–30. [DOI] [PubMed] [Google Scholar]
- 7.Taylor GJ, Bagby RM. Examining proposed changes to the conceptualization of the alexithymia construct: The way forward tilts to the past. Psychother Psychosom 2021;90:145-55. [DOI] [PubMed] [Google Scholar]
- 8.Rady A, Alamrawy RG, Ramadan I, El Raouf MA. Prevalence of alexithymia in patients with medically unexplained physical symptoms: A cross-sectional study in Egypt. Clin Pract Epidemiol Ment Health 2021;17:136-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abbass A, Town J, Holmes H, et al. Short-term psychodynamic psychotherapy for functional somatic disorders: A metaanalysis of randomized controlled trials. Psychother Psychosom 2020;89:363-70. [DOI] [PubMed] [Google Scholar]
- 10.Terock J, Janowitz D, Grabe HJ, et al. Alexithymia and psychotherapeutic treatment motivation: Main and interactional effects on treatment outcome. Psychother Psychosom 2017;86:185-6. [DOI] [PubMed] [Google Scholar]
- 11.Law MR, Watt HC, Wald NJ. The underlying risk of death after myocardial infarction in the absence of treatment. Arch Intern Med 2002;162:2405-10. [DOI] [PubMed] [Google Scholar]
- 12.Olivari Z, Steffenino G, Savonitto S, et al. The management of acute myocardial infarction in the cardiological intensive care units in Italy: the “Blitz 4 Qualità” campaign for performance measurement and quality improvement. Eur Heart J Acute Cardiovasc Care 2012;1:143-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rizzello V, Lucci D, Maggioni AP, et al. Clinical epidemiology, management and outcome of acute coronary syndromes in the Italian network on acute coronary syndromes (IN-ACS Outcome study). Acute Card Care 2012;14:71-80. [DOI] [PubMed] [Google Scholar]
- 14.Beresnevaite M: Exploring the benefits of group psychotherapy in reducing alexithymia in coronary heart disease patients: a preliminary study. Psychother Psychosom 2000;69:117-22. [DOI] [PubMed] [Google Scholar]
- 15.Ogrodniczuk JS, Joyce AS, Piper WE. Change in alexithymia in two dynamically informed individual psychotherapies. Psychother Psychosom 2013;82:61-3. [DOI] [PubMed] [Google Scholar]


