Abstract
Objective:
To determine the shear bond strength (SBS) and microleakage of metal brackets bonded with two different adhesives when a resin coat and the adhesive were light-cured separately or simultaneously.
Materials and Methods:
Eighty stainless steel brackets were bonded to the enamel of extracted premolars, 40 with Transbond Plus adhesive (group 1) and 40 with Transbond XT (group 2). Each group was subdivided into four equal subgroups; a, b, c, and d. Brackets in subgroups a and b were bonded with the adhesive without coating. For brackets in subgroup c, Ortho-Choice Ortho-Coat was applied and cured after curing of the adhesive, while the coat was applied and cured with the adhesive for brackets in subgroup d. The specimens were immersed in a 2% methylene blue dye. After debonding, the teeth and brackets were examined with a stereomicroscope. The data were subjected to a two-way analysis of variance (ANOVA), Duncan multiple range test, and Pearson correlation.
Results:
Both adhesives had comparable SBS. Curing of the coat after curing of the adhesive showed significantly higher SBS than other protocols. There was no significant difference in SBS of the adhesives without coating and with curing of the coat and adhesive simultaneously. Application of the coat significantly reduced microleakage. There was a significant negative relationship between SBS and microleakage.
Conclusions:
SBS was significantly improved with curing of the coat and adhesive separately, while it was not adversely affected when the coat and adhesive were cured simultaneously. Using the coat with either protocol significantly reduced the microleakage.
Keywords: Bond strength, Microleakage, Resin coat, Metal brackets
INTRODUCTION
Bracket bonding with light-cured composite material has become increasingly popular in orthodontics. Its popularity is based on clinically acceptable bond strength and technical ease of application.1 However, enamel decalcification (white spot lesion) around and under the bracket base is a significant problem, particularly in patients with poor oral hygiene.2 Enamel decalcifications have been reported in as many as 50% of teeth treated with bonded orthodontic brackets and in up to 50% of patients.3,4
Microleakage around orthodontic brackets increases the risk of decalcification. It occurs irrespective of the curing method, type of adhesive, and bracket type used.5–8 Upon curing, shrinkage of composite adhesive may cause a gap between the adhesive material and enamel surface leading to microleakage, thus facilitating the formation of white-spot lesions under the bracket surface area. A gap of 10 µm width was detected at the adhesive-enamel junction around the bracket base, within which oral fluids leak and bacterial accumulation was consistently observed.9 The organic acids produced by bacteria in dental plaque surrounding fixed appliances lead to demineralization, which occurs when the pH of the oral environment favors diffusion of calcium and phosphate ions out of enamel.10
Previous studies11,12 have shown the effects of microleakage on the durability of bonding. The enamel-adhesive interfaces exhibit more microleakage than the adhesive-bracket interfaces, accompanied with low bond strength.12,13 However, James et al5 could not demonstrate any correlation between microleakage and bond strength. In addition to microleakage, the rough surface of the remaining adhesive on the enamel surface provides sites for the rapid attachment and growth of oral microorganisms.14,15 These findings show that, in the presence of poor oral hygiene, the bonding adhesive may present a risk for enamel demineralization during orthodontic treatment.
In an attempt to overcome the demineralization associated with bonded brackets, a low dose of fluoride application could be used. Fluoride can be applied through self-administration or professional means.16 Self-administration methods, such as fluoride mouth rinses and tooth pastes, are efficient for reducing white spot lesions, but patient's cooperation is essential.16 Professional means of fluoride application included fluoride-releasing bonding agents, fluoridated elastomeric ligature ties and fluoride varnish.17–20 Coating with a resin veneer has been described as a valuable method to protect enamel against caries. However, this approach requires complex operative procedures.21 A caries-protective adhesive patch, applied in combination with the orthodontic brackets, seals the enamel adjacent to the bracket base and reduces the risk of leakage and decalcification.22 In addition, good adhesive flash removal is essential in reducing the amount of plaque accumulation.15,23
A color change adhesive was developed that possesses a different color from tooth enamel. It changes its color after polymerization, so it allows easier removal of excess before curing. More recently, a fluoride-releasing, light-cured resin coat was introduced. It is used to coat the borders of the bracket base, adhesive margin, and the surrounding enamel in order to reduce microleakage and collection of food and bacteria around and under the brackets. This coating exhibited no adverse effect on bond strength of bonded metal brackets.24 The present study was conducted to evaluate the effect of modifying the application protocol of a fluoride-releasing light-cured resin coat on bond strength and microleakage of metal orthodontic brackets bonded with two different adhesives.
MATERIALS AND METHODS
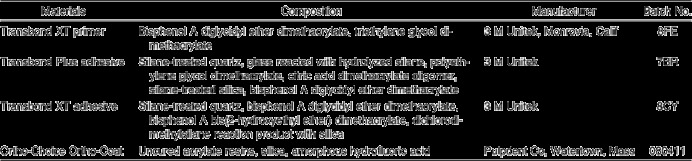
Eighty recently extracted human maxillary first premolars with no visible enamel defects, restorations, or caries were collected, cleaned, and stored in a 0.1 aqueous thymol solution. They were polished with pumice and rubber cups. They were randomly divided into two equal groups. Standard twin edgewise metal orthodontic brackets (American Orthodontics, Sheboygan, Wis) were used in this study with an average base area of 11.85 mm2. The brackets were bonded to the enamel of the buccal surfaces of the teeth using either Transbond Plus color change adhesive (3 M Unitek, Monrovia, Calif) for group 1 or Transbond XT adhesive (3 M Unitek) for group 2. Bonding procedures were performed according to manufacturer's instructions. Each group was further subdivided into four equal subgroups; a, b, c, and d (10 specimens each). Two of the subgroups were bonded with the adhesive without coating while the other two were bonded and then coated with a fluoride-releasing light-cured resin (Ortho-Choice Ortho-Coat, Pulpdent, Watertown, Mass) using two different application protocols. A description of the materials used is presented in Table 1.
Table 1.
Materials Used in the Study
Bonding and Coating Procedures
For all specimens in groups 1 and 2, enamel surfaces were etched with 37% phosphoric acid gel (Ivoclar, Vivadent, Schaan, Liechtenstein) for 30 seconds, thoroughly rinsed with an oil-free air-water spray for 15 seconds and dried with oil-free compressed air. A thin coat of Transbond XT primer was applied on the etched enamel.
For subgroups 1a and 1b, Transbond Plus adhesive paste was applied to the base of the bracket and pressed firmly onto the tooth. For subgroups 2a and 2b, Transbond XT adhesive was used. For both adhesives, the excess was removed from around the base of the bracket, and the adhesive was light-cured (Megalux, Mega-Physik Dental, Germany) on each interproximal side for 10 seconds.
For subgroups 1c and 2c, similar procedures were followed as in subgroups 1a and 1b and 2a and 2b, respectively. After curing the adhesives, the fluoride-releasing resin coat was applied around the bracket base and the surrounding enamel margins. The coat was light-cured from the mesial and distal sides for 20 seconds.
For subgroups 1d and 2d, similar procedures were followed as in subgroups 1c and 2c, respectively, but the resin coat was applied immediately after removing the excess adhesive (before curing of the adhesive). Both the adhesive and the coat were cured together for 20 seconds from the mesial and distal sides.
After bonding, the specimens were stored in distilled water at 37 ± 1°C for 4 weeks. Next, all of the specimens were thermocycled 500 times between two water baths held at 5°C and 55°C with a dwell time of 30 seconds in each bath. The teeth in all groups were embedded in autopolymerizing acrylic resin (Duracryl, SpofaDental-Praha) poured in plastic rings, with the buccal surface up. Specimens in all groups were immersed in a 2% methylene blue dye for 24 hours except specimens in subgroups 1a and 2a. These specimens were prepared to study the effect of dye immersion on bond strength for each adhesive.
Debonding Procedures and Assessment of Microleakage
Shear bond strength (SBS) testing was carried out for all groups using a universal testing machine (Lloyed, Type 500, Lloyed Instrument, England). The specimens were subjected to a shear load at a crosshead speed of 2 mm/min until failure. The load was applied under the incisal wings of each bonded bracket and parallel to the long axis of each mounted tooth. The load required to dislodge each bracket was recorded in newtons, and the shear bond strength was calculated in MPa by dividing the load by the cross-sectional area of the bracket base.
After debonding, the teeth and brackets were examined under 20× magnification with a stereomicroscope (Olymbus SZ 60, Japan) to evaluate microleakage as well as the mode of failure. Microleakage was assessed by measuring the deepest dye penetration (mm) on the tooth surfaces at right angle to the bracket margin and bracket base.5 The mode of bond failure was determined on the basis of the amount of adhesive remaining on the tooth using the adhesive remnant index (ARI). The ARI has a range of 0 (no adhesive left on the enamel surface) to 3 (all adhesive left on the enamel surface). Less than 50% of the adhesive left on the enamel is 1, while more than 50% of adhesive left on the enamel is 2.
Statistical Analysis
The mean SBS (MPa), microleakage (mm), and standard deviations were calculated for all groups. The data were subjected to a two-way analysis of variance (ANOVA) and Duncan multiple range test. Pearson correlation coefficient was used to describe the relationship between microleakage and bond strength. The chi-square test was used to determine significant differences in the ARI scores. Significance for all statistical tests was predetermined at P < .05.
RESULTS
The two-way ANOVA results of bond strength are presented in Table 2. There was no significant difference in SBS between the two adhesives (P = .8648). On the other hand, there was a significant difference in SBS in each adhesive based on the application protocols of the resin coat (P < .0001). There was no significant interaction between the type of adhesive and application protocols (P = .8135). Mean SBS, standard deviations (MPa), and results of the Duncan multiple range test for both adhesives are expressed in Table 3. A graphical presentation of these values is shown in Figure 1. For both adhesives, dye immersion of specimens bonded without coating exhibited no significant effect on SBS (P > .05). Curing of the resin coat and the adhesive separately showed significantly higher values compared with the other application protocols (P < .05). There was no significant difference (P > .05) in SBS of the adhesives without coating and with curing of the coat and adhesive simultaneously.
Table 2.
Two-Way Analysis of Variance Showing the Effect of Type of Adhesive and Application Protocols of the Resin Coat on Shear Bond Strength

Table 3.
Mean Shear Bond Strengths, Standard Deviations, and Results of the Duncan Multiple Range Test of the Two Adhesives Without Coating and With Coating Using Two Application Protocols
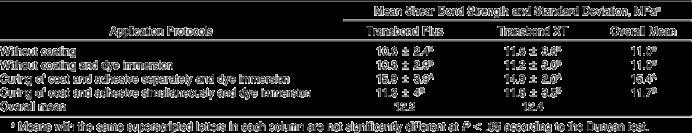
Figure 1.
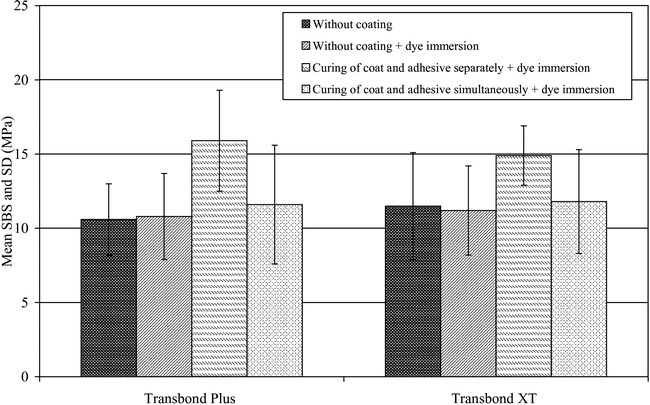
Mean shear bond strength ± SD in MPa of the studied adhesives without coating and with coating using two application protocols.
The two-way ANOVA results of microleakage (Table 4) indicated that there was no significant difference between the two adhesives (P = .5677). On the other hand, there was a significant difference in each adhesive based on the application protocols of the resin coat (P < .0001). There was no significant interaction between the type of adhesive and application protocols (P = .3291). Mean microleakage, standard deviations in millimeters, and results of the Duncan multiple range test for both adhesives are expressed in Table 5. A graphical presentation of these values is shown in Figure 2. In both adhesives, applying the adhesive without coating showed significantly higher microleakage values compared with either of the coating protocols (P < .05). Curing of the resin coat and the adhesive separately exhibited the lowest microleakage values. No significant difference (P > .05) was found in microleakage between specimens in which the coat and adhesive were cured separately and that in which the coat and adhesive were cured simultaneously.
Table 4.
Two-way Analysis of Variance Showing the Effect of Type of Adhesive and Application Protocols of the Resin Coat on Microleakage
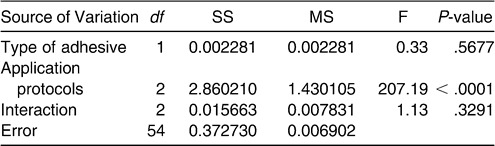
Table 5.
Mean Microleakage, Standard Deviations, and Results of the Duncan Multiple Range Test of the Two Adhesives After 24 Hours Dye Immersion
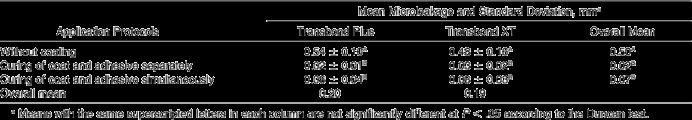
Figure 2.
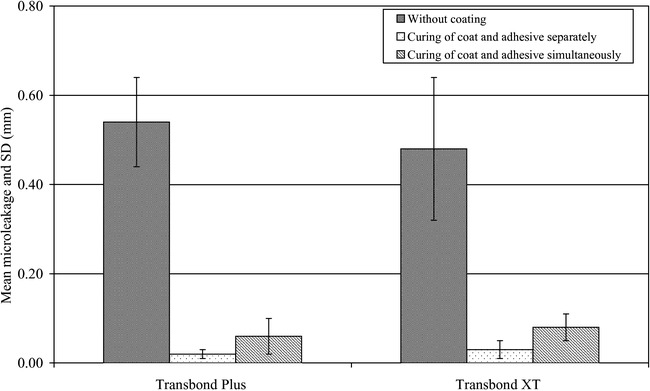
Mean microleakage ± SD in mm of the studied adhesives without coating and with coating using two application protocols.
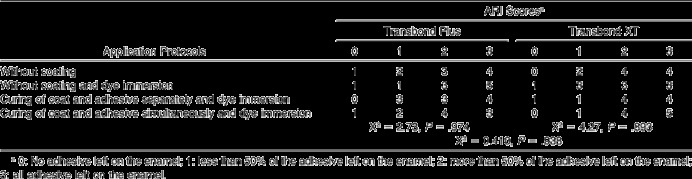
In general, correlation analysis between microleakage and SBS indicated a significantly negative relationship (r = −0.318, P < .05). Within each adhesive, correlation coefficient values were −0.376 and −0.247 for Transbond Plus and Transbond XT, respectively. The results of chi-square test (Table 6) indicated that for both adhesives, bond failure occurred most frequently at the adhesive-enamel interface (most of the adhesive left on the enamel). No significant difference was found in ARI scores between the two adhesives as well as within each adhesive using different application protocols of the resin coat.
Table 6.
Frequency Distribution and Results of the Chi-square Analysis of the Adhesive Remnant Index (ARI) of the Studied Adhesives
DISCUSSION
In the present investigation, aging of the specimens for 4 weeks and thermocycling were performed as the hypothesis was based on the microleakage after some service life in the mouth. For each adhesive, all aged specimens were immersed in the dye and then tested for bond strength with the exception of specimens of subgroups 1a and 2a. These two subgroups were used as control for each adhesive in order to study the effect of the dye on bond strength. The results revealed no significant effect of the dye on bond strength.
The results of the current study showed that both adhesives had comparable bond strength. This may be attributed to the close similarity in their chemical composition (Table 1), application procedures, as well as using the same etchant and primer. For both adhesives, curing of the resin coat and adhesive simultaneously showed an increase in SBS that was not significant, while curing of the resin coat and adhesive separately exhibited a significant increase. This could be due to increase in irradiation time of the adhesive from 20 seconds in the former to 40 seconds in the latter. The increase in curing time may enhance polymerization as it increases degree of conversion (DC) from monomer to polymer. These observations are in agreement with another study,25 which stated that bond strength increased proportionally with increase of irradiation time up to 40 seconds. It was reported that the efficiency of light-cure bracket bonding mainly depends on the energy absorbed by light-cured composite, which depends on energy density of the light. Energy density is the product of power density and curing time.26
Concurrently, it was documented that greater light energy generally results in increased flexural strength and fracture toughness, which usually correlate with greater bond strength.27 The finding of the present study agreed with a previous study24 suggesting that applying fluoride-releasing resin coating after curing of the adhesive had no adverse effect on bond strength. However, no significant increase in bond strength was obtained in that study compared with the present study.
In the current study, both adhesives without coating exhibited significantly high values of microleakage. This could be attributed to the differences in the linear thermal coefficients of expansion of enamel, metal brackets, and the adhesive systems. Metal brackets contract and expand more than enamel or the adhesives, producing microgaps between the bracket and the adhesive and causing leakage of oral fluids and bacteria beneath the brackets.28,29 A fluoride-releasing resin coat applied in either protocol produced a significant reduction in microleakage. This probably occurred because the resin coat may act as a barrier around the bracket and the adhesive edges, which prevents entry of the dye beneath the bracket. In addition, it may absorb some of the shrinkage that occurred during curing of the adhesive.
Several factors affect bond strength of brackets, such as adhesive system used, composite composition, photopolymerization type, and exposure time. Although not evidence-based in orthodontics, microleakage may also contribute to the bond strength. The finding of the present study indicated a significant negative correlation between bond strength and microleakage, which disagreed with the results obtained by James et al,5 who stated that no correlation was found between microleakage and bond strength. With respect to the ARI scores, most of the adhesive remained on the enamel surfaces of the specimens in all groups, without coating and with coating using either protocol. Although there was a change in bond strength, the nonsignificant change in the ARI scores revealed that mode of failure of bonded brackets depends not only on bond strength of the adhesive but also on many other factors.30 These findings indicated that resin coat had an unnoticeable effect on the ARI scores of both adhesives.
CONCLUSIONS
Both adhesives showed comparable SBS.
Curing of the resin coat and adhesive separately produced a significant improvement in SBS.
Curing of the resin coat and adhesive simultaneously did not adversely affect SBS, which makes it successfully save chair-side time.
Use of the resin coat with either protocol exhibited a significant reduction in microleakage.
There was a negative correlation between SBS and microleakage.
REFERENCES
- 1.Greenlaw R, Way D. C, Galil K. A. An in vitro evaluation of a visible light-cured resin as an alternative to conventional resin bonding systems. Am J Orthod Dentofacial Orthop. 1989;96:214–220. doi: 10.1016/0889-5406(89)90458-7. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell L. Decalcification during orthodontic treatment with fixed appliances: an overview. Br J Orthod. 1992;19:199–205. doi: 10.1179/bjo.19.3.199. [DOI] [PubMed] [Google Scholar]
- 3.Gorelick L, Geiger A. M, Gwinnett A. J. Incidence of white spot formation after banding and bonding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 4.Travess H, Roberts-Harry D, Sandy J. Orthodontics. Part 6: Risks in orthodontic treatment. Br Dent J. 2004;196:71–77. doi: 10.1038/sj.bdj.4810891. [DOI] [PubMed] [Google Scholar]
- 5.James J. W, Miller B. H, English J. D, Tadlock L. P, Buschang P. H. Effects of high speed curing devices on shear bond strength and microleakage of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2003;123:555–561. doi: 10.1067/mod.2003.S0889540602000197. [DOI] [PubMed] [Google Scholar]
- 6.Arıkan S, Arhun N, Arman A, Cehreli S. B. Microleakage beneath ceramic and metal brackets photopolymerized with LED or conventional light curing units. Angle Orthod. 2006;76:1035–1040. doi: 10.2319/110905-392. [DOI] [PubMed] [Google Scholar]
- 7.Ramoglu S. I, Uysal T, Ulker M, Ertas H. Microleakage under ceramic and metallic brackets bonded with resin-modified glass ionomer. Angle Orthod. 2009;79:138–143. doi: 10.2319/102607-508.1. [DOI] [PubMed] [Google Scholar]
- 8.Ulker M, Uysal T, Ramoglu S. I, Ertas H. Microleakage under orthodontic brackets using high-intensity curing lights. Angle Orthod. 2009;79:144–149. doi: 10.2319/111607-534.1. [DOI] [PubMed] [Google Scholar]
- 9.Sukontapatipark W, El-Agroudi M. A, Selliseth N. J, Thunold K, Selvig K. A. Bacterial colonization associated with fixed orthodontic appliances. A scanning electron microscopy study. Eur J Orthod. 2001;23:475–484. doi: 10.1093/ejo/23.5.475. [DOI] [PubMed] [Google Scholar]
- 10.O'Reilly M. M, Featherstone J. D. Demineralization and remineralization around orthodontic appliances: an in vivo study. Am J Orthod Dentofacial Orthop. 1987;92:33–40. doi: 10.1016/0889-5406(87)90293-9. [DOI] [PubMed] [Google Scholar]
- 11.Kubo S, Yokota H, Sata Y, Hayashi Y. Microleakage of self-etching primers after thermal and load cycling. Am J Dent. 2001;14:163–169. [PubMed] [Google Scholar]
- 12.Celiberti P, Lussi A. Use of a self-etching adhesive on previously etched intact enamel and its effect on sealant microleakage and tag formation. J Dent. 2005;33:163–171. doi: 10.1016/j.jdent.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 13.Uysal T, Ulker M, Ramoglu S. I, Ertas H. Microleakage under metallic and ceramic brackets bonded with orthodontic self-etching primer systems. Angle Orthod. 2008;78:1089–1094. doi: 10.2319/100507-481.1. [DOI] [PubMed] [Google Scholar]
- 14.Weitman R. T, Eames W. B. Plaque accumulation on composite surfaces after various finishing procedures. J Am Dent Assoc. 1975;91:101–106. doi: 10.14219/jada.archive.1975.0294. [DOI] [PubMed] [Google Scholar]
- 15.Armstrong D, Shen G, Petocz P, Darendeliler A. Excess adhesive flash upon bracket placement. Angle Orthod. 2007;77:1101–1108. doi: 10.2319/081506-334.1. [DOI] [PubMed] [Google Scholar]
- 16.Geiger A. M, Gorelick L, Gwinnett A. J, Griswold P. G. The effect of a fluoride program on white spot formation during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1988;93:29–37. doi: 10.1016/0889-5406(88)90190-4. [DOI] [PubMed] [Google Scholar]
- 17.Øgaard B, Rezk-Lega F, Ruben J, Arends J. Cariostatic effect of fluoride release from a visible light-curing adhesive for bonding of orthodontic brackets. Am J Orthod Dentofacial Orthop. 1992;101:303–307. doi: 10.1016/S0889-5406(05)80322-1. [DOI] [PubMed] [Google Scholar]
- 18.Wiltshire W. A. In vitro and in vivo fluoride release from orthodontic elastomeric ligature ties. Am J Orthod Dentofacial Orthop. 1999;115:288–292. doi: 10.1016/s0889-5406(99)70331-8. [DOI] [PubMed] [Google Scholar]
- 19.Gillgrass T. J, Creanor S. L, Foye R. H, Millett D. T. Varnish or polymeric coating for the prevention of demineralization? An ex vivo study. J Orthod. 2001;28:291–295. doi: 10.1093/ortho/28.4.291. [DOI] [PubMed] [Google Scholar]
- 20.Pascotto R. C, Navarro M. F, Capelozza Filho L, Cury J. A. In vivo effect of a resin-modified glass ionomer cement on enamel demineralization around orthodontic brackets. Am J Orthod Dentofacial Orthop. 2004;125:36–44. doi: 10.1016/s0889-5406(03)00571-7. [DOI] [PubMed] [Google Scholar]
- 21.Miwa H, Miyazawa K, Goto S, Kondo T, Hasegawa A. A resin veneer for enamel protection during orthodontic treatment. Eur J Orthod. 2001;23:759–767. doi: 10.1093/ejo/23.6.759. [DOI] [PubMed] [Google Scholar]
- 22.Schmidlin P. R, Schatzle M, Fischer J, Attin T. Bonding of brackets using a caries-protective adhesive patch. J Dent. 2008;36:125–129. doi: 10.1016/j.jdent.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 23.Eliades T, Eliades G, Brantley W. A. Microbial attachment on orthodontic appliances: I. Wettability and early pellicle formation on bracket materials. Am J Orthod Dentofacial Orthop. 1995;108:351–360. doi: 10.1016/s0889-5406(95)70032-3. [DOI] [PubMed] [Google Scholar]
- 24.Tuncer C, Tuncer B. B, Ulusoy C. Effect of fluoride-releasing light-cured resin on shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2009;135:14.e1–14.e6. doi: 10.1016/j.ajodo.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 25.Tetsu F, Shigeru H, Yosuke K. Effect of irradiation time on bond strength of metal brackets bonded with light-cured resin. Adhesive Dentistry. 2000;18:232–238. [Google Scholar]
- 26.Yoon T. H, Lee Y. K, Lim B. S, Kim C. W. Degree of polymerization of resin composites by different light sources. J Oral Rehabil. 2002;29:1165–1173. doi: 10.1046/j.1365-2842.2002.00970.x. [DOI] [PubMed] [Google Scholar]
- 27.Miyazaki M, Oshida Y, Moore B. K, Onose H. Effect of light exposure on fracture toughness and flexural strength of light cured composites. Dent Mater. 1996;12:328–332. doi: 10.1016/s0109-5641(96)80042-x. [DOI] [PubMed] [Google Scholar]
- 28.Callister W. D. Materials Science and Engineering An Introduction 2nd ed. New York, NY: John Wiley & Sons; 1991. pp. 738–739. [Google Scholar]
- 29.Van Noort R. Introduction to Dental Materials 1st ed. London, UK: Mosby; 1994. pp. 53–54. [Google Scholar]
- 30.O'Brien R. D, Watts D. C, Read M. J. F. Residual debris and bond strength—is there a relationship? Am J Orthod Dentofacial Orthop. 1988;94:222–230. doi: 10.1016/0889-5406(88)90031-5. [DOI] [PubMed] [Google Scholar]


