Abstract
Objective:
To evaluate differences in long-term postretention changes between adolescents and adults.
Materials and Methods:
The sample included 96 subjects, 51 adolescents and 45 adults (14.2 ± 0.8 and 21.5 ± 6.8 years of age, respectively, at the end of treatment) retained for 3 years and followed approximately 16 years post treatment, who were randomly selected from two private practices. Prior to treatment, 38 and 58 had Class I and Class II malocclusions, respectively.
Results:
With the exception of adult midlines, all of the occlusal variables (overjet [0.50–0.77 mm], overbite [0.85–0.95 mm], the maxillary incisor irregularity [0.69–0.80 mm], the mandibular incisor irregularity [0.85–1.50 mm] and the PAR score [0.86–1.92 points]) showed significant increases over time. Adolescents consistently showed greater increases of the occlusal variables than adults, with mandibular incisor irregularity and the PAR index attaining statistically significant (P < .05) levels. Arch length and mandibular intercanine width showed statistically significant decreases over time in both groups; maxillary intercanine and intermolar widths did not change significantly. Overjet increased significantly more in Class II patients than in Class I patients, whereas Class I patients showed significantly greater decreases in mandibular intermolar width than Class II patients.
Conclusions:
Over the 16-year posttreatment period, adolescents showed significantly greater increases in mandibular incisor irregularity, and the PAR index than adults. Treated Class I patients demonstrated less increase in overjet and greater decreases in mandibular intermolar width than Class II patients.
Keywords: Postretention changes, Occlusion, Arch dimensions, Adults, Adolescents
INTRODUCTION
The goal of orthodontic treatment is to improve the patient's life by enhancing orofacial function and esthetics.1 Long-term postretention stability, which is the key to maintaining these goals, should be a primary objective of treatment. Even though teeth are properly aligned during treatment, they often change their positions after retention.2–4 Posttreatment crowding has been regularly observed, along with changes in overjet, overbite, arch length, and arch width.5–13 While postretention changes should be expected to occur, explanations for the changes are lacking. Most studies have reported little or no correlation between the treatment changes that occurred and the posttreatment changes.5,14–20
A number of studies indicate that posttreatment crowding may be related to the individuals' growth potential.10,12,21,22 In 1991, McReynolds and Little23 suggested that vertical growth could play an important role in determining the amount of posttreatment crowding that occurs. Harris and Vaden24 showed significantly greater posttreatment reductions in mandibular intercanine and intermolar widths in adolescents than in adults, but greater decreases in arch lengths among the adults. More recently, Driscoll-Gilliland et al25 showed that both treated and untreated subjects who underwent the greatest inferior growth displacement of the mandible and the greatest eruption of the mandibular incisors, also demonstrated the greatest amounts of posttreatment crowding.
On that basis, the primary purpose of the present study was to compare postretention occlusal and arch changes of adolescents and adults. Because younger patients have greater posttreatment vertical growth and associated eruptive potential, the primary hypothesis was that adolescents would undergo greater adverse changes than adults. Secondarily, the study compared the long-term stability of patients with treated Class I and Class II malocclusions.
MATERIALS AND METHODS
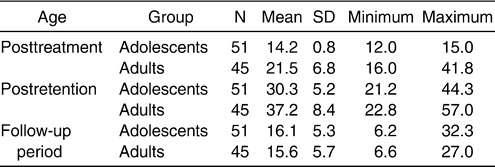
The sample consisted of 96 (81 extraction and 15 nonextraction) subjects who were randomly selected from two private practices. Subjects were selected based on: (1) the availability of long-term postretention (minimum of 6 year postretention) study casts, (2) permanent dentition (except third molars) at the start of treatment, and (3) the subjects' posttreatment age (adolescents who were less than 15 years of age and adults who were older than 16 years of age at posttreatment). The samples included 51 adolescents and 45 adults who were 14.2 ± 0.8 and 21.5 ± 6.8 years of age, respectively, at the end of treatment (Table 1). The adolescents and adults groups were followed for 16.3 ± 5.3 and 15.6 ± 5.7 years after treatment, respectively.
Table 1.
Posttreatment and Postretention Ages (in Years) Along With the Duration of the Follow-up Period (Which Includes a Maximum of 3 Years of Retention)
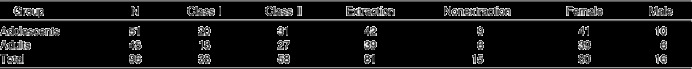
The sample included 38 individuals with Class I malocclusions and 58 individuals with Class II malocclusions, diagnosed based on molar and canine relationships (Table 2). Most (81) of the patients were treated with extractions and standard edgewise mechanics; the 15 nonextraction patients were treated with the Alexander Discipline prescription. All patients were retained with a fixed canine-to-canine bonded lower retainer and a maxillary Hawley retainer for approximately 3 years.
Table 2.
Sample Sizes Based on Class of Malocclusion, Extractions/Nonextraction, and Sex
The mandibular and maxillary arches were measured using digital calipers accurate to .01 mm. Twelve variables were measured, including the following:
Incisor irregularity: the summed displacement of the anatomical contact points of the six anterior teeth in both the upper and lower arches.26
Overjet: the horizontal distance from the labial surface of the maxillary central incisors to the labial surface of the mandibular central incisors, measured parallel with the occlusal plane.
Overbite: the amount of vertical overlap of the maxillary and mandibular central incisors measured perpendicular to the occlusal plane; open bite was assigned a negative value.
Intercanine width: the distance between the cusp tips or estimated cusp tips in patients with wear facets.
Intermolar width: the distance between the centroids of the occlusal surfaces of the first permanent molars.
PAR index: the sum of the scores of 11 individual components, including alignment of maxillary and mandibular anterior segments, maxillary/mandibular and right/left buccal segments, right and left buccal occlusion, overjet, overbite, and centerline.27
Arch length: the sum of the right and left distances between the mesial contact points of the first permanent molars and the interproximal contact point of the central incisors or the midpoint between the central incisors' contacts, if spaced.
Midline deviation: the difference between maxillary and mandibular incisor midlines.
Replicate analyses were performed after several months on 20 randomly chosen records. Paired t-tests showed no significant systematic errors. The method errors ranged from 0.08 mm (overjet) to 0.45 mm (PAR index).
Statistical Analyses
The skewness and kurtosis statistics indicated normal distributions for all measures except the PAR components. Changes over time were evaluated using paired t-tests. Posttreatment changes for the larger extraction sample were compared to the smaller nonextraction sample using the nonparametric Mann-Whitney U-test. The adolescents and adults were compared using t-tests. Age group differences in the PAR components were evaluated using the Mann-Whitney U-test.
RESULTS
Of the 12 measures evaluated, only the posttreatment changes of mandibular intermolar width showed significant (P = .025) differences between the extraction (−0.25 ± 1.0 mm) and nonextraction (0.36 ± 0.8 mm) subsamples.
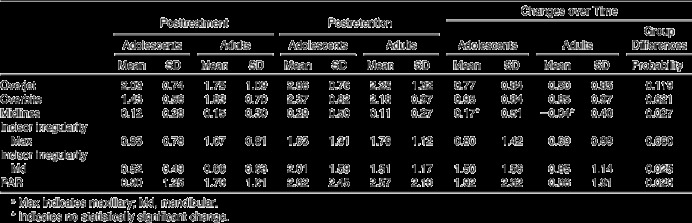
With the exception of midlines, all of the occlusal variables of the adolescents and adults showed significant changes between posttreatment and postretention (Table 3). Adolescents consistently showed greater increases than adults. Changes in mandibular incisor irregularity (1.50 vs 0.85 mm) and the PAR index (1.92 vs 0.86) were significantly greater in adolescents than in adults. Mann-Whitney U-tests showed that the group differences in the PAR index were primarily due to overall maxillary crowding (P = .016).
Table 3.
Posttreatment and Postretention Occlusal Dimensions (mm, except for PAR) of Adolescent and Adult Patientsa
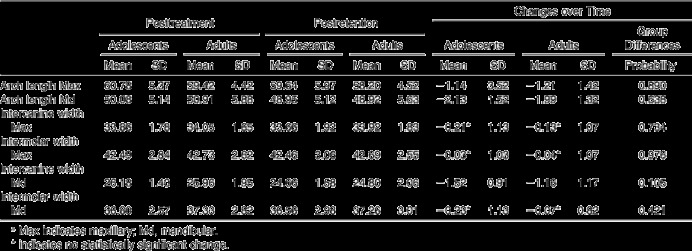
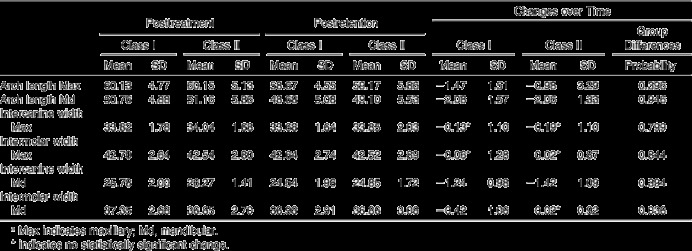
Three of the arch dimensions, including maxillary intercanine width and the two intermolar widths, did not change significantly over the 16-year follow-up period for either group (Table 4). Mandibular arch lengths decreased approximately twice as much as maxillary arch lengths. Mandibular intercanine widths also decreased. Posttreatment changes in arch dimensions were not significantly different between adolescents and adults.
Table 4.
Posttreatment and Postretention Arch Dimensions (mm) of Adolescent and Adult Patientsa
Generally, patients with Class I and Class II malocclusions showed similar posttreatment changes. Differences that occurred during the follow-up period were limited to overjet and mandibular intermolar width (Tables 5 and 6). Overjet increased significantly (P = .001) more in Class II malocclusions than in Class I malocclusions, whereas Class I malocclusions showed significantly (P = .036) greater decreases in mandibular intermolar width than Class II malocclusions.
Table 5.
Posttreatment and Postretention Occlusal Dimensions (mm, except for PAR) of Subjects Who Presented With Class I and Class II Malocclusiona
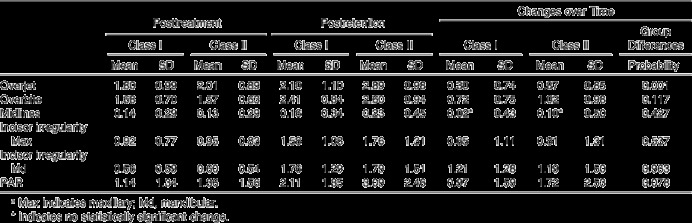
Table 6.
Posttreatment and Postretention Arch Dimensions (mm) of Subjects Who Presented With Class I and Class II Malocclusiona
DISCUSSION
Incisor irregularity increased after treatment for both adolescents and adults, with greater increases in the mandible than in the maxilla. Previous studies have consistently shown greater posttreatment increases in mandibular incisor irregularity than in maxillary incisor irregularity.7,9,10 With the exception of Vaden et al,10 the posttreatment increase in maxillary irregularity over the 16-year follow-up period was less than previously reported.7,9 Importantly, mandibular incisor irregularity increased approximately 1.2 mm, which tends to be at the low end of the values previously reported (Figure 1), including both extraction and nonextraction cases. Approximately 90.5% of the patients had mandibular incisor irregularity less than 3.5 mm, which has become the de facto standard for clinical acceptability, 16 years posttreatment (Table 3).
Figure 1.
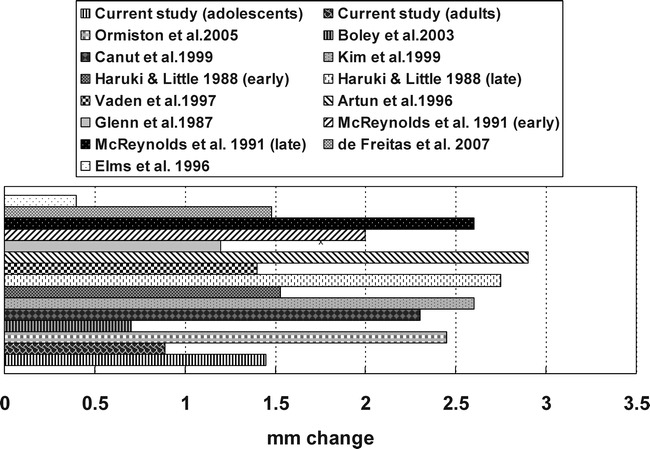
Posttreatment mandibular incisor irregular changes (all studies except Haruki and Little30 pertain to growing adolescents).
The PAR index showed a posttreatment increase of 1.39 points, which was also less than previously reported for long-term follow-up of treated cases.16,28,29 Adolescents showed greater posttreatment increases in their PAR scores than adults, which may be related to the fact that adults had higher posttreatment PAR scores. While crowding measured with the PAR scores and crowding measured using incisor irregularity are related, they might be expected to differ because the PAR scores include the posterior arch segments.
Even though posttreatment mandibular irregularity increased only minimally, the changes were significantly more in adolescents than in adults. The increases were approximately two times greater in adolescents than in adults (1.50 mm vs 0.85 mm). In contrast, Haruki and Little30 showed greater posttreatment increases in the irregularity index (2.75 mm vs 1.53 mm) among adolescents who started treatment at 13.3 years of age compared with those who started treatment at 11.2 years of age. The differences between studies may be related to the leeway space available in their younger sample.
In contrast, the crowding differences observed between adults and children were probably related to vertical growth differences and associated eruption differences. It has been previously reported that patients with the greatest posttreatment increases in lower and total posterior facial heights also demonstrated the greatest increases in crowding.23 In 2001, Driscoll-Gilliland et al25 who longitudinally followed posttreatment sample and a matched sample of untreated subjects, showed that the amounts of crowding that occurred were related to vertical mandibular growth and dental eruption. The subjects who showed the greatest growth and eruption displayed the greatest increases in crowding. Since the adolescents in the present study finished treatment at approximately 14.2 years of age and were retained for approximately 3 years, many might be expected to have had considerable growth potential after retention. Vertical growth31–38 and crowding39,40 have been shown to continue well into the 20s. This implies that it might be prudent to retain adolescent patients longer than is normally recommended, and retention should be continued through the early and mid 20s.
Posttreatment overjet increased significantly more in Class II than in Class I malocclusions. Glenn et al12 and Uhde et al41 reported results consistent with the present study. While Class I and Class II patients have not been previously compared, overjet has been shown to increase, although sometimes not significantly, after treatment.7,9,10,14,16,42,43
The current study Class II malocclusions also showed greater increases in the PAR scores than in Class I malocclusions, but the differences were not statistically significant. Based on the less stable subjects in their sample (ie, those with a postretention PAR score greater than 10), Ormiston et al16 noted significantly more unstable Class II than Class I patients 14.4 years after treatment. Consistent with the present findings, Birkeland et al28 found no significant differences in the posttreatment changes of the PAR scores between Class I and II patients. The Class I patients in the present study showed significantly greater decreases in mandibular intermolar width than Class II patients. Although they did not provide statistical comparisons, De La Cruz et al44 and Glenn et al12 also showed greater posttreatment decreases in mandibular intermolar widths among Class I patients than among Class II patients.
CONCLUSIONS
Long-term posttreatment (16 years) and postretention (13 years) changes included small but definite increases in overjet, overbite, maxillary irregularity, mandibular irregularity, and the PAR index, as well as decreases in arch length, mandibular intercanine width, and mandibular intermolar width.
Adolescents showed significantly greater posttreatment increases of mandibular incisor irregularity and the PAR index than adults, despite the fact that the vast majority of cases had clinically acceptable incisor irregular at the end of the postretention phase.
Class I patients showed significantly less long-term posttreatment increases in overjet and greater decreases in mandibular intermolar width than Class II patients.
REFERENCES
- 1.Graber T. M, Vanarsdall R. L, Vig K. W. L, editors. Orthodontics Current Principles and Techniques 4th ed. St Louis, Mo: Elsevier Mosby; 2005. p. 4. [Google Scholar]
- 2.Bresolin D, Shapiro P. A, Shapiro G. G, Chapko M. K, Dassel S. Mouth breathing in allergic children: its relationship to dentofacial development. Am J Orthod. 1983;83:334–340. doi: 10.1016/0002-9416(83)90229-4. [DOI] [PubMed] [Google Scholar]
- 3.Mills J. R. E. A long-term assessment of the mechanical retroclination of the lower incisors. Angle Orthod. 1967;37:165–174. doi: 10.1043/0003-3219(1967)037<0165:ALAOTM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Graber T. M. Postmortens in post-treatment adjustment. Am J Orthod. 1966;52:331–352. doi: 10.1016/0002-9416(66)90151-5. [DOI] [PubMed] [Google Scholar]
- 5.Freitas K. M. S, Freitas M. R, Henriques J. F. C, Pinzan A, Janson G. Postretention relapse of mandibular anterior crowding in patients treated without mandibular premolar extraction. Am J Orthod Dentofacial Orthop. 2004;125:480–487. doi: 10.1016/j.ajodo.2003.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Boley J. C, Mark J. A, Sachdeva R. C. L, Buschang P. H. Long-term stability of Class I premolar extraction treatment. Am J Orthod Dentofacial Orthop. 2003;124:277–287. doi: 10.1016/s0889-5406(03)00448-7. [DOI] [PubMed] [Google Scholar]
- 7.Canut J. A, Arias S. A long-term evaluation of treated Class II division 2 malocclusions: a retrospective study model analysis. Eur J Orthod. 1999;21:377–386. doi: 10.1093/ejo/21.4.377. [DOI] [PubMed] [Google Scholar]
- 8.Little R. M. Stability and relapse of mandibular anterior alignment: University of Washington studies. Semin Orthod. 1999;5:191–204. doi: 10.1016/s1073-8746(99)80010-3. [DOI] [PubMed] [Google Scholar]
- 9.Kim T. W, Little R. M. Postretention assessment of deep overbite correction in Class II Division 2 malocclusion. Angle Orthod. 1999;69:175–186. doi: 10.1043/0003-3219(1999)069<0175:PAODOC>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Vaden J. L, Harris E. F, Gardner R. L. Z. Relapse revisited. Am J Orthod Dentofacial Orthop. 1997;111:543–553. doi: 10.1016/s0889-5406(97)70291-9. [DOI] [PubMed] [Google Scholar]
- 11.Little R. M, Riedel R. A, Årtun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988;93:423–428. doi: 10.1016/0889-5406(88)90102-3. [DOI] [PubMed] [Google Scholar]
- 12.Glenn G, Sinclair P. M, Alexander R. G. Nonextraction orthodontic therapy: posttreatment dental and skeletal stability. Am J Orthod Dentofacial Orthop. 1987;92:321–328. doi: 10.1016/0889-5406(87)90333-7. [DOI] [PubMed] [Google Scholar]
- 13.Little R. M, Wallen T, Riedel R. Stability and relapse of mandibular anterior alignment: first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod. 1981;80:349–365. doi: 10.1016/0002-9416(81)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Erdinc A. E, Nanda R. S, Isiksal E. Relapse of anterior crowding in patients treated with extraction and nonextraction of premolars. Am J Orthod Dentofacial Orthop. 2006;129:775–784. doi: 10.1016/j.ajodo.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Nett B. C, Huang G. J. Long-term posttreatment changes measured by the American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2005;127:444–450. doi: 10.1016/j.ajodo.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 16.Ormiston J. P, Huang G. J, Little R. M, Decker J. D, Seuk G. D. Retrospective analysis of long-term stable and unstable orthodontic treatment outcomes. Am J Orthod Dentofacial Orthop. 2005;128:568–574. doi: 10.1016/j.ajodo.2004.07.047. [DOI] [PubMed] [Google Scholar]
- 17.Wood M, Lee D, Crawford E. Finishing occlusion, degree of stability and the PAR index. Aust Orthod J. 2000;16:9–15. [PubMed] [Google Scholar]
- 18.Lenz G. J, Woods M. G. Incisal changes and orthodontic stability. Angle Orthod. 1999;69:424–432. doi: 10.1043/0003-3219(1999)069<0424:ICAOS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Paquette D. E, Beattie J. R, Johnston L. E. A long-term comparison of nonextraction and premolar extraction and edgewise therapy in “borderline” Class II patients. Am J Orthod Dentofacial Orthop. 1992;102:1–14. doi: 10.1016/0889-5406(92)70009-Y. [DOI] [PubMed] [Google Scholar]
- 20.Schulaf R. J, Allen R. W, Walters R. D, Dreskin M. The mandibular dental arch: part I, lower incisor position. Angle Orthod. 1977;47:280–287. doi: 10.1043/0003-3219(1977)047<0280:TMDAPI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Schudy G. F. Posttreatment craniofacial growth: its implications in orthodontic treatment. Am J Orthod. 1974;65:39–57. [Google Scholar]
- 22.Gardner R. A, Harris E. F, Vaden J. L. Postorthodontic dental changes: a longitudinal study. Am J Orthod Dentofacial Orthop. 1998;114:582–587. doi: 10.1016/s0889-5406(98)70178-7. [DOI] [PubMed] [Google Scholar]
- 23.McReynolds D. C, Little R. M. Mandibular second premolar extraction-postretention evaluation of stability and relapse. Angle Orthod. 1991;61:133–144. doi: 10.1043/0003-3219(1991)061<0133:MSPEPE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Harris E. F, Vaden J. L. Posttreatment stability in adult and adolescent orthodontic patients: a cast analysis. Int J Adult Orthodon Orthognath Surg. 1994;9:19–29. [PubMed] [Google Scholar]
- 25.Driscoll-Gilliland J, Buschang P. H, Behrents R. G. An evaluation of growth and stability in untreated and treated subjects. Am J Orthod Dentofacial Orthop. 2001;120:588–597. doi: 10.1067/mod.2001.118778. [DOI] [PubMed] [Google Scholar]
- 26.Little R. M. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod Dentofacial Orthop. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 27.Richmond S, Shaw W. C, O'Brien K. D, Buchanan I. B, Jones R, Stephens C. D, Roberts C. T, Andrews M. The development of the PAR Index (Peer Assessment Rating): reliability and validity. Eur J Orthod. 1992;14:125–139. doi: 10.1093/ejo/14.2.125. [DOI] [PubMed] [Google Scholar]
- 28.Birkeland K, Furevik J, Boe O. E, Wisth P. J. Evaluation of treatment and post-treatment changes by the PAR Index. Eur J Orthod. 1997;19:279–288. doi: 10.1093/ejo/19.3.279. [DOI] [PubMed] [Google Scholar]
- 29.de Freitas K. M. S, Janson G, de Freitas M. R, Pinzan A, Henriques J. F. C, Pinzan-Vercelino C. R. M. Influence of the quality of the finished occlusion on postretention occlusal relapse. Am J Orthod Dentofacial Orthop. 2007;132:428.e9–428.e14. doi: 10.1016/j.ajodo.2007.02.051. [DOI] [PubMed] [Google Scholar]
- 30.Haruki T, Little R. M. Early versus late treatment of crowded first premolar extraction cases: postretention evaluation of stability and relapse. Angle Orthod. 1998;68:61–68. doi: 10.1043/0003-3219(1998)068<0061:EVLTOC>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.West K. S, McNamara J. A. Changes in the craniofacial complex from adolescence to midadulthood: a cephalometric study. Am J Orthod Dentofacial Orthop. 1999;115:521–532. doi: 10.1016/s0889-5406(99)70274-x. [DOI] [PubMed] [Google Scholar]
- 32.Bishara S. E, Treder J. E, Jakobsen J. R. Facial and dental changes in adulthood. Am J Orthod Dentofacial Orthop. 1994;106:175–186. doi: 10.1016/S0889-5406(94)70036-2. [DOI] [PubMed] [Google Scholar]
- 33.Behrents R. G. Growth in the Aging Craniofacial Skeleton. Ann Arbor, Mich: Center for Human Growth and Development, The University of Michigan; 1985. pp. 115–117. Craniofacial Growth Monograph Series; vol 17. [Google Scholar]
- 34.Sarnas K, Solow B. Early adult changes in the skeletal and soft-tissue profile. Eur J Orthod. 1980;2:1–12. [PubMed] [Google Scholar]
- 35.Forsberg C. M, Odenrick L. Changes on the relationship between the lips and the aesthetic line from eight years of age to adulthood. Eur J Orthod. 1979;1:265–270. doi: 10.1093/ejo/1.4.265. [DOI] [PubMed] [Google Scholar]
- 36.Kendrick G. S, Risinger H. L. Changes in the anteroposterior dimensions of the human male skull during the third and fourth decade of life. Anat Rec. 1967;159 doi: 10.1002/ar.1091590111. [DOI] [PubMed] [Google Scholar]
- 37.Bjork A. Variations in the growth pattern of the human mandible: longitudinal radiographic study by the implant method. J Dent Res. 1963;42:400–411. doi: 10.1177/00220345630420014701. [DOI] [PubMed] [Google Scholar]
- 38.Bjork A. Facial growth in man, studied with the aid of metallic implants. Acta Odontol Scand. 1955;13:9–34. doi: 10.3109/00016355509028170. [DOI] [PubMed] [Google Scholar]
- 39.Buschang P. H, Shulman J. D. Incisor crowding in untreated persons 15–50 years of age; United States, 1988–1994. Angle Orthod. 2003;73:502–508. doi: 10.1043/0003-3219(2003)073<0502:ICIUPY>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 40.Al Yami E. A, Kuijpers–Jagtman A. M, van 't Hof M. A. Stability of orthodontic treatment outcome: follow-up until 10 years postretention. Am J Orthod Dentofacial Orthop. 1999;115:300–304. doi: 10.1016/s0889-5406(99)70333-1. [DOI] [PubMed] [Google Scholar]
- 41.Uhde M. D, Sadowsky C, BeGole E. A. Long-term stability of dental relationships after orthodontic treatment. Angle Orthod. 1983;53:240–252. doi: 10.1043/0003-3219(1983)053<0240:LSODRA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 42.Årtun J, Garol J. D, Little R. M. Long-term stability of mandibular incisors following successful treatment of Class II, Division 1, malocclusions. Angle Orthod. 1996;66:229–238. doi: 10.1043/0003-3219(1996)066<0229:LTSOMI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 43.Elms T. N, Buschang P. H, Alexander R. G. Long-term stability of Class II, division 1, nonextraction cervical face-bow therapy: I. Model analysis. Am J Orthod Dentofacial Orthop. 1996;109:271–276. doi: 10.1016/s0889-5406(96)70150-6. [DOI] [PubMed] [Google Scholar]
- 44.De La Cruz R. A, Sampson P, Little R. M, Artun J, Shapiro P. A. Long-term changes in arch form after orthodontic treatment and retention. Am J Orthod Dentofacial Orthop. 1995;107:518–530. doi: 10.1016/s0889-5406(95)70119-2. [DOI] [PubMed] [Google Scholar]


