Abstract
Background:
Currently, there is no consensus on patient selection for ambulatory laparoscopic cholecystectomy (LC). This study is a systematic review of previously published patient selection for ambulatory LC.
Methods:
A comprehensive search was done in PubMed, Web of Science, Embase and Google Scholar Database up to March 2020 to summarise previously reported medical or surgical selection criteria used for inclusion and exclusion of patients, as well as successful same-day discharge rates and readmission rate after discharge.
Results:
Fifty-nine studies with a total of 13,219 patients were included in this systematic review. In total, the median same-day discharge rate was 90% (range: 63%–99.4%), and median readmission rate was 2.22% (range: 0%–16.9%). The most considered medical criteria were American Society of Anesthesiologists classification I and II, age <70, and body mass index <35. Surgical criteria varied greatly. The top three accessible exclusion variables were (1) common bile duct stones, cholangitis, or jaundice (27 publications, 45.8%); (2) history of abdominal surgery (12 publications, 20.3%) and (3) history of pancreatitis (9 publications, 15.3%).
Conclusion:
The results of the current study showed the variable patient selection in different centres, the medical aspect criteria may be expanded under adequate pre-anaesthetic assessment and preparation and the surgical aspect criteria should include more laboratory or imaging parameters to ensure the surgical safety.
Keywords: Ambulatory surgical procedures, laparoscopic cholecystectomy, systematic review
INTRODUCTION
Laparoscopic cholecystectomy (LC) is the most used surgical procedure for symptomatic gallstones globally.[1] In comparison with open surgery, LC has been extensively accepted for its advantages of less invasiveness, post-operative pain, hospitalisation and recovery time.[2,3,4,5]
In the early 1990s, some surgeons introduced the safety and feasibility of the performing of LC in ambulatory settings.[6,7] Until now, ambulatory LC has not been extensively accepted, especially in developing regions. The main reticence is the concern of possible misdetection of the appearance of any vital complications during the post-operative period. Therefore, basic principles are necessary for determining the ambulatory process and ensuring the highest probability of success with the utmost safety for candidate patients. Nevertheless, currently, there are still no widely recognised patient selection criteria for ambulatory LC in the surgical community.
We conducted this systematic review to summarise previously reported selection criteria for ambulatory LC.
METHODS
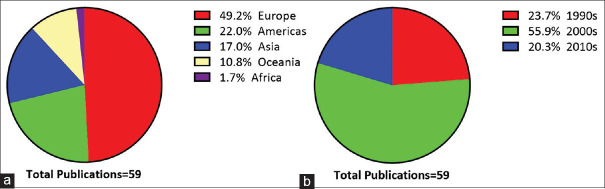
Following the PRISMA guidelines, a comprehensive search was done in PubMed, Web of Science, Embase and Google Scholar Database up to March 2020 for all accessible publications to summarise the previously reported patient's selection criteria for ambulatory LC. We used the search terms (“Cholecystectomy, Laparoscopic” [Mesh] AND “Ambulatory Surgical Procedures”[Mesh]) to identify all potential records. We also included extra studies in relevant references. Following exclusion criteria were used: (1) published not in English; (2) not original research; (3) paediatric studies; (4) research in other topics, such as nursing, anaesthesiology or ecology; (5) full-text unavailable; and (6) no patient's selection criteria provided. The PRISMA flow chart is presented in Figure 1.
Figure 1.
PRISMA flow diagram for literature inclusion
After the stepwise exclusion investigation, from all available publications, we extracted the following data: the author's name, study regions, publication years, sample size, successful same-day discharge rates, readmission rate after discharge and medical or surgical selection criteria used for the inclusion and exclusion of patients.
RESULTS
As demonstrated in Figure 1, 290 potentially available publications were included following the identification and implementation strategies. Two hundred and thirty-one records were excluded per the exclusion criteria listed in Figure 1. Eventually, 59 studies were included in this systematic review.
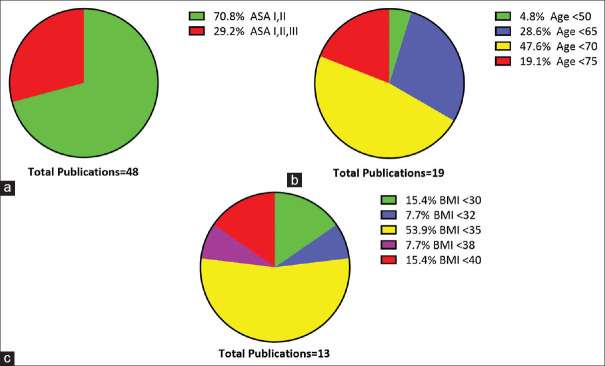
Altogether, the patient's selection criteria were provided in 59 publications, including 13219 patients. Most of the studies were performed in Europe and the Americas. In contrast, only ten studies, including 1444 patients, were analysed in the Asian area. The majority of the studies were published from 2000 to 2009 [Figure 2]. In total, the median same-day discharge rate was 90% (range: 63%–99.4%), and median readmission rate was 2.22% (range: 0%–16.9%).
Figure 2.
Geographical (a) and temporal distributions (b) of included publications
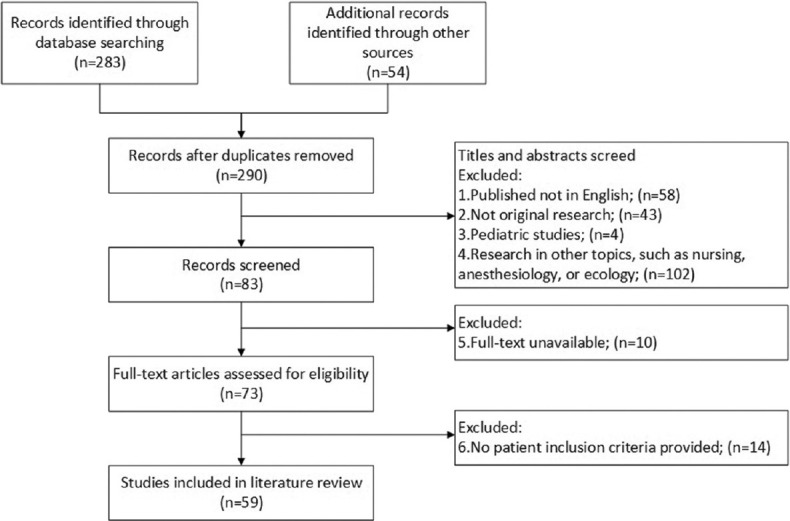
Regarding the medical factors, the American Society of Anesthesiologists (ASA) Physical Status Classification was the most popular variable to identify the suitability of candidate patients (48 publications, 81.4%). Of the 48 publications that used the ASA classification, most (34 publications, 70.8%) restricted the candidate patients within ASA I and II; 14 studies relaxed the criteria to ASA III [Figure 3]. Age was also usually considered; 28 (47.5%) articles had the limitations of age, but only 19 of them defined the upper age limit; others just required the patients to be adults. Sixty-five and seventy were frequently adopted in most articles [Figure 3]. Twenty-seven (45.8%) studies clearly stated that the common bile duct (CBD) should be in absolute normal status in pre-operative evaluations. Twenty-four (40.7%) studies excluded the patients with ongoing or previous acute cholecystitis. In contrast, some research did not consider acute cholecystitis as a limiting factor. Body mass index (BMI) was also commonlypted for selection in 13 articles, and three other studies avoided obese patients by weight only. In the 13 studies that used BMI, 35 was the common cut-off value [Figure 3].
Figure 3.
American Society of Anaesthesiologists classification (a), age upper limit (b), and Body mass index (c) cut-off values used in previous publications
Concerning the surgical factors, the top three accessible exclusion variables were (1) CBD stones, cholangitis or jaundice (27 publications, 45.8%); (2) history of abdominal surgery (12 publications, 20.3%) and (3) history of pancreatitis (9 publications, 15.3%). All detailed information was summarised in Supplementary Table 1.
Supplementary Table 1.
Detailed selection criteria extracted from 59 included publications
| Author and years | Region | Patients number | Selection criteria | Discharge rate (%) | Readmission rate (%) |
|---|---|---|---|---|---|
| Qu et al. (2019)[1] | China | 42 | ASA ≤ SAn 18 <age <50, BMI <30, no AC, no atrophic cholecystitis, no intrahepatic gallbladder, no previous abdominal surgery, no cardiopulmonary comorbidities, no diabetes | 97.6 | 0 |
| Gregori et al. (2018)[2] | Italy | 730 | No cardiopulmonary comorbidities | 85.7 | 3.4 |
| Abet et al. (2017)[3] | France | 102 | ASA ≤ SA, age ≥ ge, no choledocholithiasis, no substance abuse, no antecedents of gastro-duodenal ulcers, no immune suppression, no need of analgesics, no ongoing pregnancy. No conversion to open | 98.0 | 3.2 |
| Tandon et al. (2016)[4] | UK | 571 | ASA ≤ SAI | 78.0 | 11.7 |
| Mattila et al. (2015)[5] | Finland | 169 | ASA ≤ SA, 18 <age <65, BMI <35, no AC, no choledocholithiasis, no previous abdominal surgery, no NSAIDs allergy. No previous pancreatitis. Normal liver function tests | 87.0 | 4.0 |
| Al-Qahtani et al.[6] | Kingdom of Saudi Arabia | 487 | ASA ≤ SA, AGE ≥ GE, BMI <35, no AC, no thickening gallbladder wall, no previous abdominal surgery, normal liver function tests. Normal liver function test, no thickening gallbladder wall, no insulin-dependent diabetes or epilepsy, no ongoing pregnancy, no upper respiratory tract infection, or uncontrolled hypertension | 95.0 | n.a. |
| Salleh et al. (2015)[7] | Malaysia | 29 | ASA ≤ SA, age <75, BMI <30, no AC, no chronic cholecystitis, no choledocholithiasis, no thickening gallbladder wall. No dilated CBD | n.a. | n.a. |
| Brescia et al. (2013)[8] | Italy | 400 | ASA ≤ SA, age <70, BMI <35, no AC, no atrophic cholecystitis, no choledocholithiasis. No previous jaundice, mental healthy | 96.7 | n.a. |
| Gelmini et al. (2013)[9] | Italy | 43 | ASA ≤ SAl 18 <age <70, BMI <35, no AC, no choledocholithiasis, no previous abdominal surgery, no coagulopathy | 86.1 | 2.3 |
| Khan et al. (2012)[10] | Bangladesh | 210 | ASA ≤ SA, no choledocholithiasis, no morbid obesity | 97.6 | 0 |
| Seleem et al. (2011)[11] | Egypt | 210 | ASA ≤ SA, no AC, no conversion to open | n.a. | n.a. |
| Akoh et al. (2011)[12] | UK | 258 | ASA ≤ SAI, no AC, no choledocholithiasis | 69.0 | 5.0 |
| Briggs et al. (2009)[13] | UK | 106 | ASA ≤ SA, BMI <38, no choledocholithiasis, no previous abdominal surgery, no previous ERCP, no previous PNOV | 84.0 | 1.8 |
| Lledó et al. (2008)[14] | Spain | 410 | ASA ≤ SAI, no choledocholithiasis | 89.8 | 1.5 |
| Chang and Tan (2008)[15] | Singapore | 50 | Normal liver function tests | 92.4 | 4.0 |
| Psaila et al. (2008)[16] | UK | 176 | Weight >120 kg, no asthmatic, no NSAIDs allergy | 85.8 | 4.0 |
| Bona et al. (2007)[17] | Italy | 250 | ASA ≤ SAI, age >18, no choledocholithiasis | 82.4 | n.a. |
| Rathore et al. (2007)[18] | UK | 164 | ASA ≤ SAI, no choledocholithiasis, no previous pancreatitis, normal-sized CBD | 86.0 | 3.6 |
| Proske et al. (2007)[19] | France | 211 | ASA ≤ SA, age <75, no coagulopathy, no sleep apnea | 82.0 | 0 |
| Topal et al. (2007)[20] | Belgium | 117 | ASA ≤ SA, 16 <age <75, no AC, no choledocholithiasis, no coagulopathy | 94.0 | 4.3 |
| Victorzon et al. (2007)[21] | Finland | 567 | ASA ≤ SA, BMI <35 | 63.0 | 2.0 |
| Sherigar et al. (2006)[22] | UK | 198 | ASA ≤ SAI, no AC, no previous abdominal surgery | 88.4 | 2.0 |
| Kasem et al. (2006)[23] | UK | 150 | ASA ≤ SA, BMI <35, blood pressure <160/90 mmHg, no previous abdominal surgery, normal liver function tests, no previous anaesthetic complications, no previous difficult intubation. no previous severe AC | 99.4 | 0 |
| Metcalfe et al. (2006)[24] | Australia | 33 | ASA ≤ SAtrage >18 | 75.8 | 6.1 |
| Johansson et al. (2006)[25] | Sweden | 52 | ASA ≤ SAd 18 <age <70, no AC, no choledocholithiasis, no previous abdominal surgery, no previous pancreatitis | 92.0 | 0 |
| Kaman et al. (2005)[26] | India | 106 | ASA ≤ SA, age <70 | 95.2 | n.a. |
| Jain et al. (2005)[27] | UK | 269 | ASA ≤ SA, BMI <32 | 95.0 | 2.0 |
| Chok et al. (2004)[28] | Hong Kong, China | 73 | ASA ≤ SAg age <70 | 88.0 | 2.7 |
| Vuilleumier and Halkic (2004)[29] | Switzerland | 136 | ASA ≤ SA, no previous jaundice, no anaesthetic contraindication | 98.0 | n.a. |
| Fassiadis et al. (2004)[30] | UK | 100 | ASA ≤ SA, age <70, no AC, no morbid obesity, normal liver function tests | 99.0 | 1.0 |
| Skattum et al. (2004)[31] | Norway | 1060 | ASA ≤ SA0, mental health, no AC, no cholangitis, no pancreatitis | 92.9 | 6.6 |
| Leeder et al. (2004)[32] | UK | 154 | BMI <40, no cardiopulmonary comorbidity | 85.7 | 0.7 |
| Ammori et al. (2003)[33] | UK | 140 | ASA ≤ SA, 18 <age <75, no morbid obesity, no AC, no thickening gallbladder wall, no choledocholithiasis, no previous abdominal surgery, no previous constipation or abdominal pain | 84.0 | 1.4 |
| Bal et al. (2003)[34] | India | 313 | ASA ≤ SA, age <65, mental health | 92.0 | 3.0 |
| Blatt and Chen (2003)[35] | Australia | 41 | ASA ≤ Sat | 80.0 | 2.4 |
| Maggiore (2002)[36] | Italy | 71 | ASA ≤ SAly age <75, no gallbladder neoplasia | 88.7 | 16.9 |
| Lau and Brooks (2002)[37] | US | 200 | ASA ≤ SA, no adverse anaesthetic history, no significant comorbidities, operation time <90 min, no uncorrectable coagulopathy and diffuse intraperitoneal sepsis | 95.5 | 3.0 |
| Lau and Brooks (2002)[38] | US | 888 | ASA ≤ SA, no adverse anaesthetic history, no significant comorbidities, operation time <90 min | 96.8 | n.a. |
| Curet et al. (2002)[39] | US | 43 | Age >18, no AC, mental healthy | 86.0 | 0 |
| Siu et al. (2001)[40] | Hong Kong, China | 60 | ASA ≤ SA, no choledocholithiasis, no thickening gallbladder wall, no contracted gallbladder. No previous AC, abdominal surgery, cholangitis, or pancreatitis | 90.0 | 1.7 |
| Lau and Brooks (2001)[41] | US | 731 | ASA ≤ SA, no adverse anaesthetic history, no significant comorbidities, operation time <90 min | 96.6 | n.a. |
| Bringman et al. (2001)[42] | Sweden | 100 | ASA ≤ SA, no previous choledocholithiasis or pancreatitis, normal liver function tests. No CBD dilatation | 88.0 | n.a. |
| Richardson et al. (2001)[43] | US | 847 | ASA ≤ SAI, not extremely age | 76.0 | 4.0 |
| Young and Connell (2001)[44] | Australia | 14 | ASA ≤ SAtrage <50 | 95.0 | n.a. |
| Fleming et al. (2000)[45] | Australia | 45 | ASA ≤ SAtrno choledocholithiasis, no coagulopathy, no previous jaundice or pancreatitis. No CBD dilatation | 82.3 | 2.2 |
| Voyles and Boyd (1999)[46] | US | 100 | Age <65, normal liver enzymes, CBD diameter ≤ 5 mm | 74.0 | n.a. |
| Hollington et al. (1999)[47] | Australia | 67 | ASA ≤ SAtrano previous abdominal surgery | 89.6 | 3.0 |
| Kumar et al. (1999)[48] | India | 74 | ASA ≤ SAiaage <65 | 92.0 | 5.4 |
| Fleisher et al. (1999)[49] | US | 96 | ASA ≤ SA999age >18 | 96.9 | n.a. |
| Keulemans et al. (1998)[50] | Netherlands | 40 | ASA ≤ SAheage ≤ geheno AC, no choledocholithiasis, no calcified gallbladder, no previous abdominal surgery | 92.0 | 0 |
| Voitk (1997)[51] | Canada | 85 | ASA III and IV, or age >70 | 72.0 | 8.2 |
| 430 | ASA I and II, and age <70 | 88.0 | 2.0 | ||
| Voyles and Berch (1997)[52] | US | 605 | Age <65, no choledocholithiasis, no previous abdominal surgery | 92.0-98.0 | 0.2 |
| Narain and DeMaria (1997)[53] | US | 60 | ASA ≤ SA97no common bile duct dilatation, coagulopathy, pregnancy, or cirrhosis | 97.0 | 5.0 |
| Mjåland et al. (1997)[54] | Norway | 200 | ASA ≤ SAI, mental health | 94.0 | 8.0 |
| Lam et al. (1997)[55] | US | 213 | No AC, no clinically significant pain, normal leukocyte count, normal liver function test, no cardiopulmonary comorbidities | 97.0 | n.a. |
| Singleton et al. (1996)[56] | Australia | 40 | ASA ≤ SAtrano previous surgery, cholecystitis, jaundice, or pancreatitis | 82.5 | n.a. |
| Smith et al. (1994)[57] | Canada | 98 | No elderly, no significant commodities | 80.6 | 1.0 |
| Farha et al. (1994)[58] | US | 55 | No AC, no jaundice, CBD diameter <1 cm, no cardiopulmonary comorbidities | 90.0 | 1.8 |
| Stephensona et al. (1993)[59] | UK | 15 | ASA ≤ SA99age <70, BMI <35, no AC, no chronic cholecystitis. No previous jaundice. Mental healthy | 80.0 | n.a. |
n.a.: Not available, ASA: American society of anesthesiologist physical status classification, BMI: Body mass index, AC: Acute cholecystitis, CBD: Common bile duct, UK: The United Kingdom, US: The United States, NSAIDs: Nonsteroidal anti-inflammatory drugs, ERCP: Endoscopic retrograde cholangiopancreatography, PONV: Postoperative nausea and vomiting
DISCUSSION
As per the suggested guidelines from the British Association of Day Surgery in 2019, the patient's selection criteria should fall into three major aspects: social, medical and surgical.[8] The present study summarised all previously reported medical or surgical selection criteria used for ambulatory LC.
Regarding the medical aspect, ASA grading, age and BMI are the three most considered variables in previous publications. With the development of modern anaesthesiology, higher ASA and age seem to carry no increased risk of post-operative risk.[9,10] In 1997, Voitk also reported that ambulatory cholecystectomy is safe for the high-risk patient (ASA III and IV, or age >70).[11] Recently, Gregori et al. proved the safety of ambulatory LC in obese patients with a similar outcome in non-obese patients.[12] The British Association of Day Surgery also suggested that obesity itself is not a contraindication to the ambulatory procedure.[8] In addition, obese patients may even benefit from early mobilisation in the ambulatory procedure.[13,14] Thus, we may suggest that, with adequate pre-anaesthetic assessment and preparation, elder or obese patients with stable medical conditions could be considered as candidates for ambulatory LC. More evidence for this opinion is needed.
In the surgical aspect, the patients with a high risk of severe post-operative complications should be excluded. Even though LC has experienced four decades of development, the difficulty of LC varies greatly, mainly depending on the inflammation degree of the gallbladder and the anatomy of the Calot's triangle.[15] Inadequate pre-operative evaluation often leads the serious complications such as iatrogenic bile duct injuries and post-operative bleeding. Hence, we highly suggest that the candidate patient should be carefully evaluated regarding the gallbladder inflammation and potential anatomical variation. According to our review, many researchers excluded the patients with acute cholecystitis, history of pancreatitis or abdominal surgery or clinical suspicion of CBD stones.[16,17,18,19,20,21,22,23] In contrast, some other studies also reported acceptable outcomes with those patients.[24,25,26,27,28] Besides, abnormal laboratory tests, as well as thickening gallbladder wall in ultrasonography has been well known to be risk factors predicting complex operation.[29,30,31,32] However, only a few studies considered them as patient's selection criteria.[33,34,35] We, therefore, propose more studies to validate the efficiency of these quantitative and objective parameters in patient selection. In addition, the intraoperative situation should also be considered for the timely interruption of the ambulatory procedure. Previous studies have shown that prolonged operation could predict the inabilities of ambulatory discharge.[36,37] Thus, we recommended that unexpected difficult operation should be considered as an exclusion criterion.
CONCLUSION
The results of the current study showed the variable patient selection in different centres, the medical aspect criteria may be expanded under adequate pre-anaesthetic assessment and preparation and the surgical aspect criteria should include more laboratory or imaging parameters to ensure surgical safety.
Financial support and sponsorship
Institutional Research Funding of The First Affiliated Hospital of Chengdu Medical College (CYFY-GQ20).
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank the Department of Technology of our centre for administrative and financial support (CYFY-GQ20).
REFERENCES
- 1.Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: Cholelithiasis and cancer. Gut Liver. 2012;6:172–87. doi: 10.5009/gnl.2012.6.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reynolds W., Jr The first laparoscopic cholecystectomy. JSLS. 2001;5:89–94. [PMC free article] [PubMed] [Google Scholar]
- 3.Schirmer BD, Edge SB, Dix J, Hyser MJ, Hanks JB, Jones RS. Laparoscopic cholecystectomy.Treatment of choice for symptomatic cholelithiasis. Ann Surg. 1991;213:665–76. doi: 10.1097/00000658-199106000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy.The new ‘gold standard’? Arch Surg. 1992;127:917–21. doi: 10.1001/archsurg.1992.01420080051008. [DOI] [PubMed] [Google Scholar]
- 5.Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, et al. Tokyo guidelines 2018: Surgical management of acute cholecystitis: Safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos) J Hepatobiliary Pancreat Sci. 2018;25:73–86. doi: 10.1002/jhbp.517. [DOI] [PubMed] [Google Scholar]
- 6.Reddick EJ, Olsen DO. Outpatient laparoscopic laser cholecystectomy. Am J Surg. 1990;160:485–7. doi: 10.1016/s0002-9610(05)81009-8. [DOI] [PubMed] [Google Scholar]
- 7.Topal B, Peeters G, Verbert A, Penninckx F. Outpatient laparoscopic cholecystectomy: Clinical pathway implementation is efficient and cost effective and increases hospital bed capacity. Surg Endosc. 2007;21:1142–6. doi: 10.1007/s00464-006-9083-x. [DOI] [PubMed] [Google Scholar]
- 8.Bailey CR, Ahuja M, Bartholomew K, Bew S, Forbes L, Lipp A, et al. Guidelines for day-case surgery 2019: Guidelines from the Association of Anaesthetists and the British Association of Day Surgery. Anaesthesia. 2019;74:778–92. doi: 10.1111/anae.14639. [DOI] [PubMed] [Google Scholar]
- 9.Ansell GL, Montgomery JE. Outcome of ASA III patients undergoing day case surgery. Br J Anaesth. 2004;92:71–4. doi: 10.1093/bja/aeh012. [DOI] [PubMed] [Google Scholar]
- 10.Aldwinckle RJ, Montgomery JE. Unplanned admission rates and postdischarge complications in patients over the age of 70 following day case surgery. Anaesthesia. 2004;59:57–9. doi: 10.1111/j.1365-2044.2004.03560.x. [DOI] [PubMed] [Google Scholar]
- 11.Voitk AJ. Is outpatient cholecystectomy safe for the higher-risk elective patient? Surg Endosc. 1997;11:1147–9. doi: 10.1007/s004649900557. [DOI] [PubMed] [Google Scholar]
- 12.Gregori M, Miccini M, Biacchi D, de Schoutheete JC, Bonomo L, Manzelli A. Day case laparoscopic cholecystectomy: Safety and feasibility in obese patients. Int J Surg. 2018;49:22–6. doi: 10.1016/j.ijsu.2017.11.051. [DOI] [PubMed] [Google Scholar]
- 13.Servin F. Ambulatory anesthesia for the obese patient. Curr Opin Anaesthesiol. 2006;19:597–9. doi: 10.1097/ACO.0b013e328010cb78. [DOI] [PubMed] [Google Scholar]
- 14.Members of the Working Party, Nightingale CE, Margarson MP, Shearer E, Redman JW, Lucas DN, et al. Peri-operative management of the obese surgical patient 2015: Association of Anaesthetists of Great Britain and Ireland Society for Obesity and Bariatric Anaesthesia. Anaesthesia. 2015;70:859–76. doi: 10.1111/anae.13101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hussain A. Difficult laparoscopic cholecystectomy: Current evidence and strategies of management. Surg Laparosc Endosc Percutan Tech. 2011;21:211–7. doi: 10.1097/SLE.0b013e318220f1b1. [DOI] [PubMed] [Google Scholar]
- 16.Sherigar JM, Irwin GW, Rathore MA, Khan A, Pillow K, Brown MG. Ambulatory laparoscopic cholecystectomy outcomes. JSLS. 2006;10:473–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Qu JW, Xin C, Wang GY, Yuan ZQ, Li KW. Feasibility and safety of single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy in an ambulatory setting. Hepatobiliary Pancreat Dis Int. 2019;18:273–7. doi: 10.1016/j.hbpd.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Mattila A, Mrena J, Kautiainen H, Nevantaus J, Kellokumpu I. Day-care laparoscopic cholecystectomy with diathermy hook versus fundus-first ultrasonic dissection: A randomized study. Surg Endosc. 2016;30:3867–72. doi: 10.1007/s00464-015-4691-y. [DOI] [PubMed] [Google Scholar]
- 19.Al-Qahtani HH, Alam MK, Asalamah S, Akeely M, Ibrar M. Day-case laparoscopic cholecystectomy. Saudi Med J. 2015;36:46–51. doi: 10.15537/smj.2015.1.9738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brescia A, Gasparrini M, Nigri G, Cosenza UM, Dall’Oglio A, Pancaldi A, et al. Laparoscopic cholecystectomy in day surgery: Feasibility and outcomes of the first 400 patients. Surgeon. 2013;11(Suppl 1):S14–8. doi: 10.1016/j.surge.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Seleem MI, Gerges SS, Shreif KS, Ahmed AE, Ragab A. Laparoscopic cholecystectomy as a day surgery procedure: Is it safe.– An Egyptian experience? Saudi J Gastroenterol. 2011;17:277–9. doi: 10.4103/1319-3767.82584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh DR, Joshi MR, Koirala U, Shrestha BR, Shrestha S, Gautam B. Early experience of day care surgery in Nepal. JNMA J Nepal Med Assoc. 2010;49:191–4. [PubMed] [Google Scholar]
- 23.Akoh JA, Watson WA, Bourne TP. Day case laparoscopic cholecystectomy: Reducing the admission rate. Int J Surg. 2011;9:63–7. doi: 10.1016/j.ijsu.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Rathore MA, Andrabi SI, Mansha M, Brown MG. Day case laparoscopic cholecystectomy is safe and feasible: A case controlled study. Int J Surg. 2007;5:255–9. doi: 10.1016/j.ijsu.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Briggs CD, Irving GB, Mann CD, Cresswell A, Englert L, Peterson M, et al. Introduction of a day-case laparoscopic cholecystectomy service in the UK: A critical analysis of factors influencing same-day discharge and contact with primary care providers. Ann R Coll Surg Engl. 2009;91:583–90. doi: 10.1308/003588409X432365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang SK, Tan WB. Feasibility and safety of day surgery laparoscopic cholecystectomy in a university hospital using a standard clinical pathway. Singapore Med J. 2008;49:397–9. [PubMed] [Google Scholar]
- 27.Psaila J, Agrawal S, Fountain U, Whitfield T, Murgatroyd B, Dunsire MF, et al. Day-surgery laparoscopic cholecystectomy: Factors influencing same-day discharge. World J Surg. 2008;32:76–81. doi: 10.1007/s00268-007-9225-x. [DOI] [PubMed] [Google Scholar]
- 28.Maggiore D. Outpatient laparoscopic cholecystectomy: A reality. JSLS. 2002;6:369–71. [PMC free article] [PubMed] [Google Scholar]
- 29.Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, et al. Tokyo guidelines 2018: Diagnostic criteria and severity grading of acute cholecystitis (with videos) J Hepatobiliary Pancreat Sci. 2018;25:41–54. doi: 10.1002/jhbp.515. [DOI] [PubMed] [Google Scholar]
- 30.Raman SR, Moradi D, Samaan BM, Chaudhry US, Nagpal K, Cosgrove JM, et al. The degree of gallbladder wall thickness and its impact on outcomes after laparoscopic cholecystectomy. Surg Endosc. 2012;26:3174–9. doi: 10.1007/s00464-012-2310-8. [DOI] [PubMed] [Google Scholar]
- 31.Sakuramoto S, Sato S, Okuri T, Sato K, Hiki Y, Kakita A. Preoperative evaluation to predict technical difficulties of laparoscopic cholecystectomy on the basis of histological inflammation findings on resected gallbladder. Am J Surg. 2000;179:114–21. doi: 10.1016/s0002-9610(00)00248-8. [DOI] [PubMed] [Google Scholar]
- 32.Jessica Mok KW, Goh YL, Howell LE, Date RS. Is C-reactive protein the single most useful predictor of difficult laparoscopic cholecystectomy or its conversion.A pilot study? J Minim Access Surg. 2016;12:26–32. doi: 10.4103/0972-9941.158963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lam D, Miranda R, Hom SJ. Laparoscopic cholecystectomy as an outpatient procedure. J Am Coll Surg. 1997;185:152–5. doi: 10.1016/s1072-7515(97)00041-0. [DOI] [PubMed] [Google Scholar]
- 34.Salleh AA, Affirul CA, Hairol O, Zamri Z, Azlanudin A, Hilmi MA, et al. Randomized controlled trial comparing daycare and overnight stay laparoscopic cholecystectomy. Clin Ter. 2015;166:e165–8. doi: 10.7417/CT.2015.1848. [DOI] [PubMed] [Google Scholar]
- 35.Ammori BJ, Davides D, Vezakis A, Martin IG, Larvin M, Smith S, et al. Day-case laparoscopic cholecystectomy: A prospective evaluation of a 6-year experience. J Hepatobiliary Pancreat Surg. 2003;10:303–8. doi: 10.1007/s00534-002-0807-6. [DOI] [PubMed] [Google Scholar]
- 36.Wu Q, Fu N, Chen W, Jin X, He L, Mo C, et al. Risk factors for patient selection in ambulatory laparoscopic cholecystectomy: A single-centre experience. J Minim Access Surg. 2021 doi: 10.4103/jmas.JMAS_25_21. Online ahead of print. Doi: 10.4103/jmas.JMAS_25_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lau H, Brooks DC. Predictive factors for unanticipated admissions after ambulatory laparoscopic cholecystectomy. Arch Surg. 2001;136:1150–3. doi: 10.1001/archsurg.136.10.1150. [DOI] [PubMed] [Google Scholar]
REFERENCES
- 1.Qu JW, Xin C, Wang GY, Yuan ZQ, Li KW. Feasibility and safety of single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy in an ambulatory setting. Hepatobiliary Pancreat Dis Int. 2019;18:273–7. doi: 10.1016/j.hbpd.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 2.Gregori M, Miccini M, Biacchi D, de Schoutheete JC, Bonomo L, Manzelli A. Day case laparoscopic cholecystectomy:Safety and feasibility in obese patients. Int J Surg. 2018;49:22–6. doi: 10.1016/j.ijsu.2017.11.051. [DOI] [PubMed] [Google Scholar]
- 3.Abet E, Orion F, Denimal F, Brau-Weber AG, de Kerviler B, Jean MH, et al. Interest of using ropivacaine for outpatient laparoscopic cholecystectomy: Prospective randomized trial. World J Surg. 2017;41:687–92. doi: 10.1007/s00268-016-3797-2. [DOI] [PubMed] [Google Scholar]
- 4.Tandon A, Sunderland G, Nunes QM, Misra N, Shrotri M. Day case laparoscopic cholecystectomy in patients with high BMI: Experience from a UK centre. Ann R Coll Surg Engl. 2016;98:329–33. doi: 10.1308/rcsann.2016.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mattila A, Mrena J, Kautiainen H, Nevantaus J, Kellokumpu I. Day-care laparoscopic cholecystectomy with diathermy hook versus fundus-first ultrasonic dissection: A randomized study. Surg Endosc. 2015;30:3867–72. doi: 10.1007/s00464-015-4691-y. [DOI] [PubMed] [Google Scholar]
- 6.Al-Qahtani HH, Alam MK, Asalamah S, Akeely M, Ibrar M. Day-case laparoscopic cholecystectomy. Saudi Med J. 2015;36:46–51. doi: 10.15537/smj.2015.1.9738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salleh AA, Affirul CA, Hairol O, Zamri Z, Azlanudin A, Hilmi MA, et al. Randomized controlled trial comparing daycare and overnight stay laparoscopic cholecystectomy. Clin Ter. 2015;166:e165–8. doi: 10.7417/CT.2015.1848. [DOI] [PubMed] [Google Scholar]
- 8.Brescia A, Gasparrini M, Nigri G, Cosenza UM, Dall'Oglio A, Pancaldi A, et al. Laparoscopic cholecystectomy in day surgery: Feasibility and outcomes of the first 400 patients. Surgeon. 2013;11(Suppl 1):S14–8. doi: 10.1016/j.surge.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Gelmini R, Franzoni C, Saviano M. Day surgery laparoscopic cholecystectomy: Initial experience in 43 consecutive patients. Ann Ital Chir. 2013;84:631–6. [PubMed] [Google Scholar]
- 10.Khan MH, Khan AW, Aziz MM, Rabbi MA. Day case laparoscopic cholecystectomy: Experience at the Bangabandhu Sheikh Mujib Medical University. Mymensingh Med J. 2012;21:485–9. [PubMed] [Google Scholar]
- 11.Seleem MI, Gerges SS, Shreif KS, Ahmed AE, Ragab A. Laparoscopic cholecystectomy as a day surgery procedure: Is it safe?–An Egyptian experience. Saudi J Gastroenterol. 2011;17:277–9. doi: 10.4103/1319-3767.82584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akoh JA, Watson WA, Bourne TP. Day case laparoscopic cholecystectomy: Reducing the admission rate. Int J Surg. 2011;9:63–7. doi: 10.1016/j.ijsu.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Briggs CD, Irving GB, Mann CD, Cresswell A, Englert L, Peterson M, et al. Introduction of a day-case laparoscopic cholecystectomy service in the UK: A critical analysis of factors influencing same-day discharge and contact with primary care providers. Ann R Coll Surg Engl. 2009;91:583–90. doi: 10.1308/003588409X432365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lledó JB, Planells M, Espí A, Serralta A, García R, Sanahuja A. Predictive model of failure of outpatient laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2008;18:248–53. doi: 10.1097/SLE.0b013e31816de922. [DOI] [PubMed] [Google Scholar]
- 15.Chang SK, Tan WB. Feasibility and safety of day surgery laparoscopic cholecystectomy in a university hospital using a standard clinical pathway. Singapore Med J. 2008;49:397–9. [PubMed] [Google Scholar]
- 16.Psaila J, Agrawal S, Fountain U, Whitfield T, Murgatroyd B, Dunsire MF, et al. Day-surgery laparoscopic cholecystectomy: Factors influencing same-day discharge. World J Surg. 2008;32:76–81. doi: 10.1007/s00268-007-9225-x. [DOI] [PubMed] [Google Scholar]
- 17.Bona S, Monzani R, Fumagalli Romario U, Zago M, Mariani D, Rosati R. Outpatient laparoscopic cholecystectomy: A prospective study of 250 patients. Gastroenterol Clin Biol. 2007;31:1010–5. doi: 10.1016/s0399-8320(07)78322-7. [DOI] [PubMed] [Google Scholar]
- 18.Rathore MA, Andrabi SI, Mansha M, Brown MG. Day case laparoscopic cholecystectomy is safe and feasible: A case controlled study. Int J Surg. 2007;5:255–9. doi: 10.1016/j.ijsu.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Proske JM, Dagher I, Revitea C, Carloni A, Beauthier V, Labaille T, et al. Day-case laparoscopic cholecystectomy: Results of 211 consecutive patients. Gastroenterol Clin Biol. 2007;31:421–4. doi: 10.1016/s0399-8320(07)89403-6. [DOI] [PubMed] [Google Scholar]
- 20.Topal B, Peeters G, Verbert A, Penninckx F. Outpatient laparoscopic cholecystectomy: Clinical pathway implementation is efficient and cost effective and increases hospital bed capacity. Surg Endosc. 2007;21:1142–6. doi: 10.1007/s00464-006-9083-x. [DOI] [PubMed] [Google Scholar]
- 21.Victorzon M, Tolonen P, Vuorialho T. Day-case laparoscopic cholecystectomy: Treatment of choice for selected patients? Surg Endosc. 2007;21:70–3. doi: 10.1007/s00464-005-0787-0. [DOI] [PubMed] [Google Scholar]
- 22.Sherigar JM, Irwin GW, Rathore MA, Khan A, Pillow K, Brown MG. Ambulatory laparoscopic cholecystectomy outcomes. JSLS. 2006;10:473–8. [PMC free article] [PubMed] [Google Scholar]
- 23.Kasem A, Paix A, Grandy-Smith S, El-Hasani S. Is laparoscopic cholecystectomy safe and acceptable as a day case procedure? J Laparoendosc Adv Surg Tech A. 2006;16:365–8. doi: 10.1089/lap.2006.16.365. [DOI] [PubMed] [Google Scholar]
- 24.Metcalfe MS, Mullin EJ, Maddern GJ. Relaxation of the criteria for day surgery laparoscopic cholecystectomy. ANZ J Surg. 2006;76:142–4. doi: 10.1111/j.1445-2197.2006.03672.x. [DOI] [PubMed] [Google Scholar]
- 25.Johansson M, Thune A, Nelvin L, Lundell L. Randomized clinical trial of day-care versus overnight-stay laparoscopic cholecystectomy. Br J Surg. 2006;93:40–5. doi: 10.1002/bjs.5241. [DOI] [PubMed] [Google Scholar]
- 26.Kaman L, Verma GR, Sanyal S, Bhukal I. Relevance of day care laparoscopic cholecystectomy in a developing nation. Trop Gastroenterol. 2005;26:95–7. [PubMed] [Google Scholar]
- 27.Jain PK, Hayden JD, Sedman PC, Royston CM, O'Boyle CJ. A prospective study of ambulatory laparoscopic cholecystectomy: Training economic, and patient benefits. Surg Endosc. 2005;19:1082–5. doi: 10.1007/s00464-004-2170-y. [DOI] [PubMed] [Google Scholar]
- 28.Chok KS, Yuen WK, Lau H, Lee F, Fan ST. Outpatient laparoscopic cholecystectomy in Hong Kong Chinese –An outcome analysis. Asian J Surg. 2004;27:313–6. doi: 10.1016/S1015-9584(09)60058-0. [DOI] [PubMed] [Google Scholar]
- 29.Vuilleumier H, Halkic N. Laparoscopic cholecystectomy as a day surgery procedure: Implementation and audit of 136 consecutive cases in a university hospital. World J Surg. 2004;28:737–40. doi: 10.1007/s00268-004-7376-6. [DOI] [PubMed] [Google Scholar]
- 30.Fassiadis N, Pepas L, Grandy-Smith S, Paix A, El-Hasani S. Outcome and patient acceptance of outpatient laparoscopic cholecystectomy. JSLS. 2004;8:251–3. [PMC free article] [PubMed] [Google Scholar]
- 31.Skattum J, Edwin B, Trondsen E, Mjåland O, Raede J, Buanes T. Outpatient laparoscopic surgery: Feasibility and consequences for education and health care costs. Surg Endosc. 2004;18:796–801. doi: 10.1007/s00464-003-9180-z. [DOI] [PubMed] [Google Scholar]
- 32.Leeder PC, Matthews T, Krzeminska K, Dehn TC. Routine day-case laparoscopic cholecystectomy. Br J Surg. 2004;91:312–6. doi: 10.1002/bjs.4409. [DOI] [PubMed] [Google Scholar]
- 33.Ammori BJ, Davides D, Vezakis A, Martin IG, Larvin M, Smith S, et al. Day-case laparoscopic cholecystectomy: A prospective evaluation of a 6-year experience. J Hepatobiliary Pancreat Surg. 2003;10:303–8. doi: 10.1007/s00534-002-0807-6. [DOI] [PubMed] [Google Scholar]
- 34.Bal S, Reddy LG, Parshad R, Guleria R, Kashyap L. Feasibility and safety of day care laparoscopic cholecystectomy in a developing country. Postgrad Med J. 2003;79:284–8. doi: 10.1136/pmj.79.931.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blatt A, Chen S. Day-only laparoscopic cholecystectomy in a regional teaching hospital. ANZ J Surg. 2003;73:321–5. doi: 10.1046/j.1445-2197.2003.t01-1-02614.x. [DOI] [PubMed] [Google Scholar]
- 36.Maggiore D. Outpatient laparoscopic cholecystectomy: A reality. JSLS. 2002;6:369–71. [PMC free article] [PubMed] [Google Scholar]
- 37.Lau H, Brooks DC. Contemporary outcomes of ambulatory laparoscopic cholecystectomy in a major teaching hospital. World J Surg. 2002;26:1117–21. doi: 10.1007/s00268-002-6264-1. [DOI] [PubMed] [Google Scholar]
- 38.Lau H, Brooks DC. Transitions in laparoscopic cholecystectomy: The impact of ambulatory surgery. Surg Endosc. 2002;16:323–6. doi: 10.1007/s00464-001-8114-x. [DOI] [PubMed] [Google Scholar]
- 39.Curet MJ, Contreras M, Weber DM, Albrecht R. Laparoscopic cholecystectomy. Surg Endosc. 2002;16:453–7. doi: 10.1007/s00464-001-8129-3. [DOI] [PubMed] [Google Scholar]
- 40.Siu WT, Leong HT, Law BK, Onsiong SM, Fung KH, Li AC, et al. Outpatient laparoscopic cholecystectomy in Hong Kong: Patient acceptance. Surg Laparosc Endosc Percutan Tech. 2001;11:92–6. [PubMed] [Google Scholar]
- 41.Lau H, Brooks DC. Predictive factors for unanticipated admissions after ambulatory laparoscopic cholecystectomy. Arch Surg. 2001;136:1150–3. doi: 10.1001/archsurg.136.10.1150. [DOI] [PubMed] [Google Scholar]
- 42.Bringman S, Anderberg B, Heikkinen T, Nyberg B, Peterson E, Hansen K, et al. Outpatient laparoscopic cholecystectomy. A prospective study with 100 consecutive patients. Ambul Surg. 2001;9:83–6. doi: 10.1016/s0966-6532(01)00076-2. [DOI] [PubMed] [Google Scholar]
- 43.Richardson WS, Fuhrman GS, Burch E, Bolton JS, Bowen JC. Outpatient laparoscopic cholecystectomy. Outcomes of 847 planned procedures. Surg Endosc. 2001;15:193–5. doi: 10.1007/s004640000301. [DOI] [PubMed] [Google Scholar]
- 44.Young J, O'Connell B. Recovery following laparoscopic cholecystectomy in either a 23 hour or an 8 hour facility. J Qual Clin Pract. 2001;21:2–7. doi: 10.1046/j.1440-1762.2001.00399.x. [DOI] [PubMed] [Google Scholar]
- 45.Fleming WR, Michell I, Douglas M. Audit of outpatient laparoscopic cholecystectomy. Universities of Melbourne HPB Group. Aust N Z J Surg. 2000;70:423–7. doi: 10.1046/j.1440-1622.2000.01840.x. [DOI] [PubMed] [Google Scholar]
- 46.Voyles CR, Boyd KB. Criteria and benchmarks for laparoscopic cholecystectomy in a free-standing ambulatory center. JSLS. 1999;3:315–8. [PMC free article] [PubMed] [Google Scholar]
- 47.Hollington P, Toogood GJ, Padbury RT. A prospective randomized trial of day-stay only versus overnight-stay laparoscopic cholecystectomy. Aust N Z J Surg. 1999;69:841–3. doi: 10.1046/j.1440-1622.1999.01713.x. [DOI] [PubMed] [Google Scholar]
- 48.Kumar A, Seenu V, Mohan N, Kaul A, Bhalla AP, Batra RK, et al. Initial experience with day case laparoscopic cholecystectomy at a tertiary care hospital in India. Natl Med J India. 1999;12:103–7. [PubMed] [Google Scholar]
- 49.Fleisher LA, Yee K, Lillemoe KD, Talamini MA, Yeo CJ, Heath R, et al. Is outpatient laparoscopic cholecystectomy safe and cost-effective?A model to study transition of care. Anesthesiology. 1999;90:1746–55. doi: 10.1097/00000542-199906000-00033. [DOI] [PubMed] [Google Scholar]
- 50.Keulemans Y, Eshuis J, de Haes H, de Wit LT, Gouma DJ. Laparoscopic cholecystectomy: Day-care versus clinical observation. Ann Surg. 1998;228:734–40. doi: 10.1097/00000658-199812000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Voitk AJ. Is outpatient cholecystectomy safe for the higher-risk elective patient? Surg Endosc. 1997;11:1147–9. doi: 10.1007/s004649900557. [DOI] [PubMed] [Google Scholar]
- 52.Voyles CR, Berch BR. Selection criteria for laparoscopic cholecystectomy in an ambulatory care setting. Surg Endosc. 1997;11:1145–6. doi: 10.1007/s004649900556. [DOI] [PubMed] [Google Scholar]
- 53.Narain PK, DeMaria EJ. Initial results of a prospective trial of outpatient laparoscopic cholecystectomy. Surg Endosc. 1997;11:1091–4. doi: 10.1007/s004649900537. [DOI] [PubMed] [Google Scholar]
- 54.Mjåland O, Raeder J, Aasboe V, Trondsen E, Buanes T. Outpatient laparoscopic cholecystectomy. Br J Surg. 1997;84:958–61. doi: 10.1002/bjs.1800840714. [DOI] [PubMed] [Google Scholar]
- 55.Lam D, Miranda R, Hom SJ. Laparoscopic cholecystectomy as an outpatient procedure. J Am Coll Surg. 1997;185:152–5. doi: 10.1016/s1072-7515(97)00041-0. [DOI] [PubMed] [Google Scholar]
- 56.Singleton RJ, Rudkin GE, Osborne GA, Watkins DS, Williams JA. Laparoscopic cholecystectomy as a day surgery procedure. Anaesth Intensive Care. 1996;24:231–6. doi: 10.1177/0310057X9602400215. [DOI] [PubMed] [Google Scholar]
- 57.Smith R, Kolyn D, Pace R. Outpatient laparoscopic cholecystectomy. HPB Surg. 1994;7:261–4. doi: 10.1155/1994/70629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Farha GJ, Green BP, Beamer RL. Laparoscopic cholecystectomy in a freestanding outpatient surgery center. J Laparoendosc Surg. 1994;4:291–4. doi: 10.1089/lps.1994.4.291. [DOI] [PubMed] [Google Scholar]
- 59.Stephenson BM, Callander C, Sage M, Vellacott KD. Feasibility of 'day case'laparoscopic cholecystectomy. Ann R Coll Surg Engl. 1993;75:249–51. [PMC free article] [PubMed] [Google Scholar]