Abstract
Objectives
Older adults are at high risk for complications from coronavirus disease 2019 (COVID-19). Health guidelines recommend limiting physical contact during the pandemic, drastically reducing opportunities for in-person social exchange. Older adults are also susceptible to negative consequences from loneliness, and the COVID-19 pandemic has likely exacerbated this age-related vulnerability.
Methods
In 107 community-dwelling older individuals (65–90 years, 70.5% female) from Florida, the United States, and Ontario, Canada, we examined change in loneliness over the course of the pandemic after implementation of COVID-19-related physical distancing guidelines (March–September 2020; T1–T5; biweekly concurrent self-report) using multilevel modeling. We also explored gender differences in loneliness during the early phase of the COVID-19 pandemic at both data collection sites.
Results
Consistent across the 2 sites, levels of loneliness remained stable over time for the full sample (T1–T5). However, our exploratory moderation analysis suggested gender differences in the trajectory of loneliness between the United States and Canada, in that older men in Florida and older women in Ontario reported an increase in loneliness over time.
Discussion
Leveraging a longitudinal, binational data set collected during the early phase of the COVID-19 pandemic, this study advances understanding of stability and change in loneliness among a North American sample of individuals aged 65 and older faced with the unique challenges of social isolation. These results can inform public health policy in anticipation of future pandemics and highlight the need for targeted intervention to address acute loneliness among older populations.
Keywords: Aging, Gender, Longitudinal, Physical distancing, Social isolation
Loneliness refers to the subjective perception of social isolation or the felt difference between desired and perceived levels of social connection (Luhmann & Hawkley, 2016). Although loneliness rates typically stabilize with age (Hawkley & Cacioppo, 2007), mental and physical consequences of loneliness become more severe in late adulthood (e.g., for functional decline and mortality; Cornwell & Waite, 2009; Dahlberg, 2021; Perissinotto et al., 2012; Tyrrell & Williams, 2020), which highlights the importance of assessing loneliness across development, including adulthood and aging.
At the onset of the coronavirus disease 2019 (COVID-19) pandemic in North America in March 2020, public health safety protocols (e.g., physical distancing of at least 2 m/6 ft; limited social gathering) were implemented to reduce viral spread (Detsky & Bogoch, 2020; Schuchat, 2020). Though physical distancing is effective and necessary for reducing spread of infection (Kucharski et al., 2020), COVID-19 safety protocols also placed pressures to dramatically reduce in-person social activities.
Older adults have disproportionately the greatest risk for hospitalization and severe complications after contracting COVID-19 (Centers for Disease Control and Prevention, 2020). This paired with the increased vulnerability of older adults to experience social isolation and loneliness due to age-related declines in functional status (Shankar et al., 2017) as well as the limited opportunities for social interaction brought on by the COVID-19 pandemic catalyzed multiple lines of investigation on the impact of the COVID-19 pandemic on loneliness in this population.
To date, findings on loneliness among older adults during the COVID-19 pandemic are mixed, but largely point to an increase in loneliness early in the pandemic (Dahlberg, 2021). For example, several recent studies saw an initial, though small, increase in loneliness among older adults early on (e.g., in the United States: Krendl & Perry, 2021, effect size d = 0.32; in the Netherlands: van Tilburg et al., 2020, effect size d = 0.21 for social loneliness, but see Luchetti et al., 2020, in the United States, effect size d = 0.14). In contrast, however, a study utilizing large international cohorts from Denmark, France, the Netherlands, and the United Kingdom found that participants younger than 30 experienced greater loneliness in March–July 2020 than adults aged 30–60 and 60 and older (Varga et al., 2021). Additionally, findings from the Health and Retirement Study in the United States showed that, compared to responses made in 2016, there was no significant within-person change in digital isolation or loneliness among older adults, although physical distancing and social isolation increased with the pandemic (Peng & Roth, 2021).
Previous studies have used a single assessment (Parlapani et al., 2020) or a comparison of two or three time points to assess change in loneliness related to the COVID-19 pandemic (Fuller & Huseth-Zosel, 2021; Krendl & Perry, 2021; Luchetti et al., 2020; Peng & Roth, 2021; van Tilburg et al., 2020; but see Varga et al., 2021). However, whether loneliness was maintained or varied throughout the pandemic remains uncertain. Uncertain, fast-evolving dynamics during the pandemic resulted in various “phases” of response at both the societal (e.g., physical distancing and stay-at-home orders, waves of infection, and mortality rates; Unruh et al., 2021) and individual (e.g., adherence/fatigue) levels and make it particularly relevant to examine loneliness over time as this public health crisis unfolded. That is, more frequent sampling throughout the early phase of the pandemic is needed to fully characterize these dynamics in loneliness during the COVID-19 epoch.
Taken together, current published findings suggest that jurisdictional factors, including duration and severity of physical distancing restrictions, may have played a role in determining the psychological impacts of social isolation on older adults during the COVID-19 pandemic (Varga et al., 2021). To investigate this possibility, we measured loneliness in two jurisdictions, and Florida, the United States and Ontario, Canada. While official timelines for physical distancing restrictions were similar across Florida and Ontario, individual adherence to these guidelines (Coroiu et al., 2020; Pedersen & Favero, 2020; Seiter & Curran, 2021) and health care system demands/accessibility likely differed (Unruh et al., 2021). Direct comparison of responses to physical distancing and stay-at-home orders between multiple nations is currently limited (but see Varga et al., 2021).
To address this gap, we leveraged a binational data set from a North American sample of older adults (65+ years old) collected during the earlier months of the COVID-19 pandemic (March–September 2020) using a microlongitudinal design (i.e., via biweekly online assessments). The present study design was geared toward assessing change in loneliness during the COVID-19 pandemic with higher temporal resolution to capture the rapidly evolving nature of this time. Our main hypothesis was that loneliness among older adults would increase over the course of the pandemic as physical distancing restrictions persisted, and that loneliness levels among older adults would be similar across jurisdictions. In addition, some recent studies reported higher loneliness in older women than older men during the pandemic (Savage et al., 2021; Wickens et al., 2021). Given this initial evidence of gender differences in loneliness during the COVID-19 pandemic, we explored a moderation effect of gender in the loneliness trajectory over time during the early phase of the pandemic. We expected that older women compared to older men would show a greater increase in loneliness along with the progression of the pandemic.
Method
Participants
A total of 107 older adults (65–90 years) from two North American sites participated in this study: 57 participants from Gainesville, FL (M = 73.09 years, SD = 5.03, 75.4% female) and 50 from Toronto, ON (M = 73.54 years, SD = 5.97, 66% female). This community sample of older adults was a convenience sample available for this data collection at the start of the COVID-19 pandemic through a well-coordinated collaboration between the United States and the Canada site.
Participants were recruited through existing research cohorts at the University of Florida, Gainesville, and York University, Toronto, supplemented with word-of-mouth and online posts/media advertisements. Table 1 summarizes sample-descriptive information for the total sample and by site; Supplementary Tables 1–3 detail study attrition.
Table 1.
Descriptive Information for the Total Sample and by Site
| Florida | Ontario | Total | |
|---|---|---|---|
| Sample size | 57 | 50 | 107 |
| Female (%) | 75.4 | 66.0 | 71.0 |
| Age (M, SD) | 73.09, 5.03 | 73.54, 5.97 | 73.30, 5.47 |
| Education (M, SD) | 16.71, 2.95 | 16.20, 2.69 | 16.21, 2.75 |
| Income (%) | |||
| Category 1 | 21.1 | 22.0 | |
| Category 2 | 49.1 | 50.0 | |
| Category 3 | 19.3 | 22.0 | |
| TICS (M, SD) | 35.65, 2.32 | 37.68, 4.20 | |
| Household size (median [25%, 75% percentile]) | 2 [2, 2] | 2 [2, 2] | 2 [1, 2] |
Notes: Age and education are reported in years. In Florida, income category 1: <$24,999, income category 2: $25,000–$99,999, and income category 3: >$100,000; in Ontario: income category 1: <$39,999, income category 2: $40,000–$99,999, and income category 3: >100,000. The Telephone Interview for Cognitive Status (TICS) used in Florida has a theoretical range from 0 to 41 (Brandt et al., 1988); the TICS used in Ontario has a theoretical range from 0 to 50 (Welsh et al., 1993). Household size was measured by the number of people in the household. Information about education was missing from one participant in Florida; income information was missing from six participants in Florida and three participants in Ontario. The two samples did not significantly differ in gender distribution, age, education, or household size.
Procedure
Data reported here are a subset of variables collected in a larger longitudinal, cross-national investigation on the social, psychological, and health-related effects of acute social isolation related to COVID-19 physical distancing in older adults. The larger project comprises additional measures (e.g., lifestyle, substance use), but this report is restricted to variables directly related to the research questions addressed here. Data for this report were collected during March–September 2020. The study protocol was approved by the Institutional Review Board at each participating site.
After informed consent, participants completed an online survey through Qualtrics that comprised a retrospective self-report assessment that took place during the pandemic but was with reference to the time prior to the implementation of physical distancing restrictions (T0). Approximately a day later, participants completed the first of five biweekly self-report assessments in reference to their experiences during the pandemic (T1–T5; i.e., each referring to the two previous weeks, respectively, during the pandemic). Given the close temporal proximity of the T0 and T1 assessments and the acquisition of T0 data after and not before onset of the COVID-19 pandemic, methodological features that could have resulted in reporting biases, we only analyzed T1–T5 measures for this report (i.e., microlongitudinal change in self-reported loneliness during the pandemic). Results pertaining to T0 are reported in Supplementary Materials. Participants were compensated for completion of the online assessments (equivalent to 5–15 USD per assessment depending on the site).
Measures
This study evolved out of the unique circumstances of the COVID-19 pandemic. An adapted version of the revised 20-item UCLA Loneliness Scale (Russell et al., 1980), a measure of subjective feelings of loneliness and social isolation, was completed at each time point (see Supplementary Materials for individual items). Participants rated items on a 10-point Likert-type scale, ranging from 1 = Never to 10 = Always. Averaged scores across items (reverse-scored as applicable) were used to represent loneliness, with higher scores indicating greater self-reported loneliness.
Analysis
We used multilevel modeling techniques implemented in Stata 16.1. Leveraging T1–T5 data, we examined change in loneliness during the pandemic, with Site (categorical: 1 = Florida, 2 = Ontario) as a between-subject variable and Duration as a within-subject variable. Participants were enrolled on a continuing basis; therefore, we used Duration to capture the time since implementation of pandemic-related physical distancing by calculating the days between March 17, 2020 (i.e., when a U.S. Coronavirus task force news briefing recommended shelter in place and in Ontario a state of emergency was declared) and when a participant completed a given assessment.
In the exploratory analysis, we added Gender (categorical: 0 = Men, 1 = Women) and its interactions with the other predictors (e.g., Duration, Site, Duration-by-Site) in the model to determine the moderating role of gender in a longitudinal change in loneliness during the pandemic at the two study sites. Retrospectively reported prior loneliness at T0 served as a covariate in both models. Furthermore, we estimated interindividual variability in average self-reported loneliness by including the random effect of the intercept. Wald tests determined significance (see Supplementary Materials for sensitivity analysis).
Results
Change in Self-Reported Loneliness During Physical Distancing Restrictions (T1–T5)
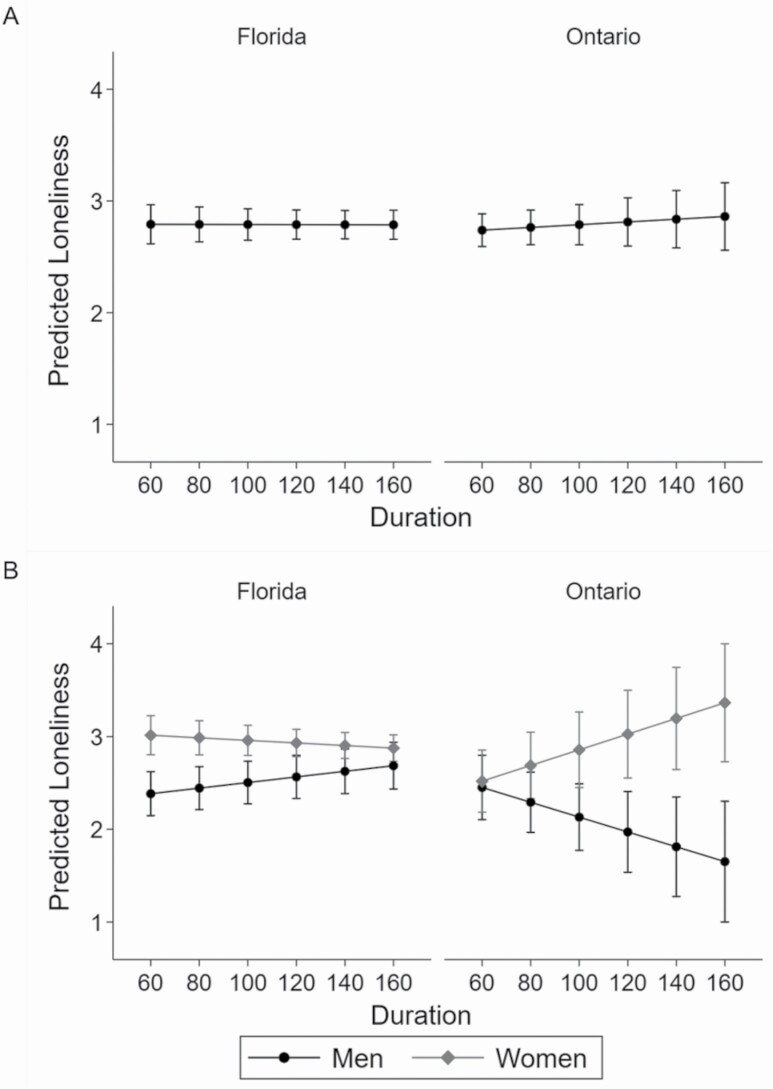
Neither the Duration (χ 2(1) < 0.01, p = .97, Cohen’s f2 < 0.001) nor Site (χ 2(1) = 0.29, p = .59, Cohen’s f2 < 0.001) main effects nor their interaction (χ 2(1) = 0.32, p = .57, Cohen’s f2 = 0.002) were significant. This finding suggests that self-reported loneliness did not change across the duration of COVID-19-related physical distancing restrictions (March–September 2020) at the two sites (Figure 1A).
Figure 1.
Longitudinal change in self-reported loneliness during the pandemic (T1–T5, biweekly) by Site (A) and by Site and Gender (B). The theoretical range of loneliness is from 1 to 10, with higher scores indicating greater self-reported loneliness. Duration indicated the number of days between March 17, 2020 and when a participant completed a given assessment. Error bars represent 83% confidence intervals to facilitate group-difference comparison (Austin & Hux, 2002).
The Duration × Site × Gender interaction was significant (χ 2(1) = 11.75, p = .001, Cohen’s f2 = 0.03). Following up, we observed a significant Duration × Gender interaction in the Florida (χ 2(1) = 6.84, p = .01, Cohen’s f2 = 0.02) and the Ontario (χ 2(1) = 6.98, p = .01, Cohen’s f2 = 0.06) samples. While older women in Florida (χ 2(1) = 0.93, p = .34, Cohen’s f2 = 0.01) reported no change in loneliness over the course of T1–T5, older men in Florida reported an increase in loneliness (χ 2(1) = 6.73, p = .01, Cohen’s f2 = 0.06). In contrast, older women in Ontario showed an increase in reported loneliness over time (χ 2(1) = 4.89, p = .03, Cohen’s f2 = 0.06), while older men in Ontario reported no change (χ 2(1) = 2.60, p = .11, Cohen’s f2 = 0.07; Figure 1B).
Discussion
This brief report leverages longitudinal self-reports collected during March–September 2020 across a binational sample of older adults aged 65 and older to determine the impact of COVID-19-related acute social isolation due to physical distancing on loneliness. While some previous findings demonstrated an initial rise in loneliness among older adults (Krendl & Perry, 2021; Seifert & Hassler, 2020), our data support that self-reported loneliness among older adults in regions within the United States and Canada stabilized over a period of 10 weeks during the pandemic (T1–T5).
Our finding is consistent with results from a study by Luchetti et al. (2020), which found that loneliness among older adults in the United States remained stable in the month following the implementation of pandemic-related “stay-at-home” orders in mid-March 2020. Our work adds to these previous findings by including binational, longitudinal assessments covering nearly the full first wave of the COVID-19 pandemic and two sites in North America (i.e., Florida and Ontario). We used a microlongitudinal design (i.e., biweekly assessments) for a fine-grained evaluation of loneliness during the pandemic (see also Saltzman et al., 2020). Furthermore, our multilevel modeling approach specifically allowed for the determination of both within- and between-subject variability over time.
Our finding of stability in loneliness among older adults over the course of the pandemic is, in fact, quite consistent with evidence around the hedonic treadmill model. According to this theory, a person’s momentary well-being is affected by current life events, but only temporarily, after which it typically returns to its previous state (i.e., hedonic neutrality; Diener et al., 2006). In line with this theoretical account and our own findings, other recent studies found stability in subjective well-being (Shavit et al., 2021) as well as psychological distress levels (Daly & Robinson, 2021) over the course of the COVID-19 pandemic. Furthermore, recent work suggests that older adults experienced lower levels of anxiety/depression (González-Sanguino et al., 2020) and more positive affect (Klaiber et al., 2021) than younger adults during the pandemic (Vahia et al., 2020). However, direct comparisons across age cohorts using a microlongitudinal design would be necessary in the future to confirm this interpretation.
Living situation, finances, and other interindividual differences, such as gender, can also moderate the effects of COVID-19-related loneliness (Seifert & Hassler, 2020). We observed a gender-by-site interaction on the longitudinal trajectory of loneliness, in that older men (but not women) in Florida and older women (but not men) in Ontario reported increased loneliness as the pandemic unfolded in its early phase. The literature generally supports that older women experience greater feelings of loneliness than older men (Savage et al., 2021; Wickens et al., 2021). In contrast, a recent European study suggested that men and women did not generally differ in COVID-19-related loneliness (Parlapani et al., 2020). Stigma and social influence contribute to gender differences in self-reported loneliness (Borys & Perlman, 1985) and may have interacted with cultural differences in our binational sample. Also, there is evidence that both older adults and women were more adherent to physical distancing restrictions (Coroiu et al., 2020; Lin et al., 2021), which needs to be further examined as possibly underlying age and gender differences in self-reported loneliness during the pandemic.
Some work has demonstrated commonalities between the United States and Canada in terms of individual and interpersonal barriers and facilitators of physical distancing adherence (Coroiu et al., 2020; Taylor et al., 2020). Experiences of loneliness were among the greatest threats to adherence to physical distancing guidelines, with older adults and women being the most compliant groups (Coroiu et al., 2020). Another binational sample (the United States and Canada) showed that the strongest predictor for experiencing distress during social isolation and excessive avoidance were beliefs over the dangerousness of the coronavirus (Taylor et al., 2020). Thus, physical distancing adherence is a dynamic process dependent on various individual factors, including one’s reactions to loneliness and perceptions of the dangerousness of the virus. Future examination of additional individual factors, such as level of worry about COVID-19 (Taylor et al., 2020) or living situation (e.g., alone vs. not; Parlapani et al., 2020; rural vs. nonrural; Fuller & Huseth-Zosel, 2021), may further elucidate longitudinal change in loneliness associated with the COVID-19 pandemic by gender and region.
However, our analysis was limited in its ability to draw firm conclusions about the moderating role of gender on longitudinal change in loneliness across the early phase of the COVID-19 pandemic, due to the size and gender distribution of the convenience sample (e.g., 75.4% female in Florida and 66% female in Ontario). Future research will benefit from a larger, more gender-balanced sample.
The longer-term impact of physical distancing and other safety protocols, beyond the first few pandemic months, is unclear. Continued longitudinal investigation will increase understanding of the evolving health burden associated with loneliness in aging and during future public health crises. This work will benefit from the use of objective observational measures (e.g., geolocation tracking and/or ecological momentary assessment) and qualitative interviews (Fuller & Huseth-Zosel, 2021) to complement self-report questionnaires. Assessment of attitudes toward the pandemic, risk perception, and adherence to safety protocols are especially needed as they may influence levels of physical contact with others. For example, among individuals in the United States and Canada, high fear responses to COVID-19 predicted both increased rates of general distress and distress associated with social isolation (Taylor et al., 2020).
Current findings may not reflect the experiences of more vulnerable aging populations, including individuals with cognitive impairment/dementia, in assisted living, with lower household income, with depression, or racial/ethnic minorities (Dahlberg, 2021; Vahia et al., 2020); nor do they speak to impacts on health-related behaviors (e.g., greater substance use, reduced physical activity), highlighting the need for more targeted longitudinal investigations. Building from these early findings, and recognizing the links between loneliness, cognitive decline, and neurodegenerative disease risk (Lara et al., 2019), determination of the impacts of acute loneliness on brain health in later life is urgently needed (Spreng & Bzdok, 2021). Furthermore, a more detailed analysis of how older adults fostered social connections during this period of limited in-person interactions (e.g., via technology use; Van Orden et al., 2021) as well as research extending across the full unfolding of the pandemic, and phase-locked to shifting public health directives, will be fruitful to examine the experience of loneliness within and between different phases of the pandemic (e.g., before and after executive orders limiting social gatherings).
In conclusion, the present study incorporated data from two sites (the United States and Canada) providing an international comparison of loneliness among older adults to the growing literature on the mental and social effects of the COVID-19 pandemic in North America. To our knowledge, these findings provide the first precise sampling of loneliness experiences among older adults during the early phases of the COVID-19 pandemic in a binational sample. These data emphasize the importance of considering both jurisdictional as well as interindividual factors (e.g., gender, region) in evaluating the psychological impacts of public health policies in older adulthood.
Supplementary Material
Acknowledgments
The authors would like to thank the volunteers for their participation in this study. The authors would also like to acknowledge Eliany Perez and Kevin Chi for help with study implementation and data collection logistics as well as Sarah Peeling and Julia Cochran for help with the literature search.
Funding
This work was supported by the National Institute on Aging of the National Institutes of Health grants 1R01AG057764 (to N. C. Ebner and R. N. Spreng) and R01AG068563 (to R. N. Spreng); the Natural Science and Engineering Research Council of Canada Discovery grant (to G. Turner); the University of Florida Substance Abuse Training Center in Public Health from the National Institute on Drug Abuse of the National Institutes of Health under award number T32DA035167 (to M. Horta). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of Interest
None declared.
Data Availability
The study was not preregistered. The data and analytic syntax are available at OSF (https://osf.io/2vdsh/?view_only=db9b4c7903c94a198f7369df97de60ae).
References
- Austin, P. C., & Hux, J. E. (2002). A brief note on overlapping confidence intervals. Journal of Vascular Surgery, 36(1), 194–195. [DOI] [PubMed] [Google Scholar]
- Borys, S., & Perlman, D. (1985). Gender differences in loneliness. Personality and Social Psychology Bulletin, 11(1), 63–74. doi: 10.1177/0146167285111006 [DOI] [Google Scholar]
- Brandt, J., Spencer, M., & Folstein, M. (1988). The telephone interview for cognitive status. Neuropsychiatry, Neuropsychology, and Behavioral Neurology, 1(2), 111–117. [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Centers for Disease Control and Prevention.https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html
- Cornwell, E. Y., & Waite, L. J. (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50(1), 31–48. doi: 10.1177/002214650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coroiu, A., Moran, C., Campbell, T., & Geller, A. C. (2020). Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLoS One, 15(10), e0239795. doi: 10.1371/journal.pone.0239795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlberg, L. (2021). Loneliness during the COVID-19 pandemic. Aging & Mental Health, 25(7), 1161–1164. doi: 10.1080/13607863.2021.1875195 [DOI] [PubMed] [Google Scholar]
- Daly, M., & Robinson, E. (2021). Psychological distress and adaptation to the COVID-19 crisis in the United States. Journal of Psychiatric Research, 136, 603–609. doi: 10.1016/j.jpsychires.2020.10.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detsky, A. S., & Bogoch, I. I. (2020). COVID-19 in Canada: Experience and response. Journal of the American Medical Association, 324(8), 743–744. doi: 10.1001/jama.2020.14033 [DOI] [PubMed] [Google Scholar]
- Diener, E., Lucas, R. E., & Scollon, C. N. (2006). Beyond the hedonic treadmill: Revising the adaptation theory of well-being. The American Psychologist, 61(4), 305–314. doi: 10.1037/0003-066X.61.4.305 [DOI] [PubMed] [Google Scholar]
- Fuller, H. R., & Huseth-Zosel, A. (2021). Older adults’ loneliness in early COVID-19 social distancing: Implications of rurality. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 1–6. doi: 10.1093/geronb/gbab053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino, C., Ausín, B., Castellanos, M. Á., Saiz, J., López-Gómez, A., Ugidos, C., & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity, 87, 172–176. doi: 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley, L. C., & Cacioppo, J. T. (2007). Aging and loneliness: Downhill quickly? Current Directions in Psychological Science, 16(4), 187–191. doi: 10.1111/j.1467-8721.2007.00501.x [DOI] [Google Scholar]
- Klaiber, P., Wen, J. H., DeLongis, A., & Sin, N. L. (2021). The ups and downs of daily life during COVID-19: Age differences in affect, stress, and positive events. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), 30–37. doi: 10.1093/geronb/gbaa096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krendl, A. C., & Perry, B. L. (2021). The impact of sheltering in place during the COVID-19 pandemic on older adults’ social and mental well-being. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), 53–58. doi: 10.1093/geronb/gbaa110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucharski, A. J., Klepac, P., Conlan, A. J. K., Kissler, S. M., Tang, M. L., Fry, H., Gog, J. R., & Edmunds, W. J.; CMMID COVID-19 Working Group. (2020). Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: A mathematical modelling study. The Lancet. Infectious Diseases, 20(10), 1151–1160. doi: 10.1016/S1473-3099(20)30457-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara, E., Martín-María, N., De la Torre-Luque, A., Koyanagi, A., Vancampfort, D., Izquierdo, A., & Miret, M. (2019). Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Research Reviews, 52, 7–16. doi: 10.1016/j.arr.2019.03.002 [DOI] [PubMed] [Google Scholar]
- Lin, T., Harris, E. A., Heemskerk, A., Van Bavel, J. J., & Ebner, N. C. (2021). A multi-national test on self-reported compliance with COVID-19 public health measures: The role of individual age and gender demographics and countries’ developmental status. Social Science & Medicine (1982), 286, 114335. doi: 10.1016/j.socscimed.2021.114335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti, M., Lee, J. H., Aschwanden, D., Sesker, A., Strickhouser, J. E., Terracciano, A., & Sutin, A. R. (2020). The trajectory of loneliness in response to COVID-19. The American Psychologist, 75(7), 897–908. doi: 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luhmann, M., & Hawkley, L. C. (2016). Age differences in loneliness from late adolescence to oldest old age. Developmental Psychology, 52(6), 943–959. doi: 10.1037/dev0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parlapani, E., Holeva, V., Nikopoulou, V. A., Sereslis, K., Athanasiadou, M., Godosidis, A., Stephanou, T., & Diakogiannis, I. (2020). Intolerance of uncertainty and loneliness in older adults during the COVID-19 pandemic. Frontiers in Psychiatry, 11, 842. doi: 10.3389/fpsyt.2020.00842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng, S., & Roth, A. R. (2021). Social isolation and loneliness before and during the COVID-19 pandemic: A longitudinal study of U.S. adults older than 50. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 1–6, gbab068. doi: 10.1093/GERONB/GBAB068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perissinotto, C. M., Stijacic Cenzer, I., & Covinsky, K. E. (2012). Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine, 172(14), 1078–1083. doi: 10.1001/archinternmed.2012.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen, M. J., & Favero, N. (2020). Social distancing during the COVID-19 pandemic: Who are the present and future noncompliers? Public Administration Review, 80(5), 805–814. doi: 10.1111/PUAR.13240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, D., Peplau, L. A., & Cutrona, C. E. (1980). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39(3), 472–480. doi: 10.1037//0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Saltzman, L. Y., Hansel, T. C., & Bordnick, P. S. (2020). Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychological Trauma: Theory, Research, Practice and Policy, 12(S1), S55–S57. doi: 10.1037/tra0000703 [DOI] [PubMed] [Google Scholar]
- Savage, R. D., Wu, W., Li, J., Lawson, A., Bronskill, S. E., Chamberlain, S. A., Grieve, J., Gruneir, A., Reppas-Rindlisbacher, C., Stall, N. M., & Rochon, P. A. (2021). Loneliness among older adults in the community during COVID-19: A cross-sectional survey in Canada. BMJ Open, 11(4), e044517. doi: 10.1136/bmjopen-2020-044517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuchat, A. (2020). Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(18), 551–556. doi: 10.15585/MMWR.MM6918E2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifert, A., & Hassler, B. (2020). Impact of the COVID-19 pandemic on loneliness among older adults. Frontiers in Sociology, 5, 590935. doi: 10.3389/fsoc.2020.590935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seiter, J. S., & Curran, T. (2021). Social-distancing fatigue during the COVID-19 pandemic: a mediation analysis of cognitive flexibility, fatigue, depression, and adherence to CDC guidelines. 38(1), 68–78. doi: 10.1080/08824096.2021.1880385 [DOI] [Google Scholar]
- Shankar, A., McMunn, A., Demakakos, P., Hamer, M., & Steptoe, A. (2017). Social isolation and loneliness: Prospective associations with functional status in older adults. Health Psychology, 36(2), 179–187. doi: 10.1037/hea0000437 [DOI] [PubMed] [Google Scholar]
- Shavit, T., Sherman, A., & Aisenberg, D. (2021). The effects of the COVID-19 crisis on the subjective well-being of the Israeli population–monitored phase by phase. Current Psychology, 40, 1–8. doi: 10.1007/s12144-021-01594-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spreng, R. N., & Bzdok, D. (2021). Loneliness and neurocognitive aging. Advances in Geriatric Medicine and Research, 3(2), e210009. doi: 10.20900/AGMR20210009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S., Landry, C. A., Paluszek, M. M., & Asmundson, G. J. G. (2020). Reactions to COVID-19: Differential predictors of distress, avoidance, and disregard for social distancing. Journal of Affective Disorders, 277, 94–98. doi: 10.1016/j.jad.2020.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrrell, C. J., & Williams, K. N. (2020). The paradox of social distancing: Implications for older adults in the context of COVID-19. Psychological Trauma: Theory, Research, Practice and Policy, 12(S1), S214–S216. doi: 10.1037/tra0000845 [DOI] [PubMed] [Google Scholar]
- Unruh, L., Allin, S., Marchildon, G., Burke, S., Barry, S., Siersbaek, R., Thomas, S., Selina, R., Andriy, K., Alexander, M., Merkur, S., Webb, E., & Williams, G. A. (2021). A comparison of health policy responses to the COVID-19 pandemic in Canada, Ireland, the United Kingdom and the United States of America. Health Policy. doi: 10.1016/J.HEALTHPOL.2021.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahia, I. V., Jeste, D. V., & Reynolds, C. F.3rd. (2020). Older adults and the mental health effects of COVID-19. Journal of the American Medical Association, 324(22), 2253–2254. doi: 10.1001/jama.2020.21753 [DOI] [PubMed] [Google Scholar]
- Van Orden, K. A., Bower, E., Lutz, J., Silva, C., Gallegos, A. M., Podgorski, C. A., Santos, E. J., & Conwell, Y. (2021). Strategies to promote social connections among older adults during “social distancing” restrictions. The American Journal of Geriatric Psychiatry, 29(8), 816–827. doi: 10.1016/j.jagp.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Tilburg, T. G., Steinmetz, S., Stolte, E., van der Roest, H., & de Vries, D. H. (2020). Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76, e249–e255. doi: 10.1093/geronb/gbaa111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga, T. V., Bu, F., Dissing, A. S., Elsenburg, L. K., Bustamante, J. J. H., Matta, J., van Zon, S. K. R., Brouwer, S., Bültmann, U., Fancourt, D., Hoeyer, K., Goldberg, M., Melchior, M., Strandberg-Larsen, K., Zins, M., Clotworthy, A., & Rod, N. H. (2021). Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200,000 Western and Northern Europeans. The Lancet Regional Health—Europe, 2, 100020. doi: 10.1016/j.lanepe.2020.100020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh, K. A., Breitner, J. C., & Magruder-Habib, K. M. (1993). Detection of dementia in the elderly using telephone screening of cognitive status. Neuropsychiatry, Neuropsychology, & Behavioral Neurology, 6(2), 103–110. [Google Scholar]
- Wickens, C. M., McDonald, A. J., Elton-Marshall, T., Wells, S., Nigatu, Y. T., Jankowicz, D., & Hamilton, H. A. (2021). Loneliness in the COVID-19 pandemic: Associations with age, gender and their interaction. Journal of Psychiatric Research, 136, 103–108. doi: 10.1016/j.jpsychires.2021.01.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The study was not preregistered. The data and analytic syntax are available at OSF (https://osf.io/2vdsh/?view_only=db9b4c7903c94a198f7369df97de60ae).