Abstract
Bradycardia is rare in children and may be asymptomatic or cause fatigue or discomfort leading to syncope. It may be a warning sign of underlying pathology. A check-up for a cardiac or extra-cardiac organic cause should be performed. We report the case of an 8-year-old child admitted to the emergency room for bradycardia with a sino-atrial block that caused syncope. The assessment has objectified a brain tumor. We will discuss the different mechanisms that can explain the occurrence of bradycardia during a brain tumor, and the specificities of the management.
Keywords: Brain tumor, bradycardia, vagal hyperactivity, intracranial hypertension.
Résumé :
La bradycardie est rare chez les enfants et peut être asymptomatique ou provoquer une fatigue ou un malaise conduisant à une syncope. Elle peut être un signe d'alerte d'une pathologie sous-jacente. Un bilan à la recherche d'une cause organique cardiaque ou extra-cardiaque doit être réalisé. Nous rapportons le cas d'un enfant de 8 ans admis aux urgences pour une bradycardie avec un bloc sino-atrial à l'origine d'une syncope, le bilan a objectivé une tumeur cérébrale, nous allons discuter les différents mécanismes qui peuvent expliquer la survenue de bradycardie lors d'une tumeur cérébrale, et les particularités de la prise en charge.
Mots clés: tumeur cérébrale, bradycardie, hyperactivité vagale, hypertension intracrânienne
Introduction
Bradycardia is defined by a heart rate below 60 beats per minute, It can be physiological in the athletic or elderly subject, as it can be secondary to an underlying cardiac pathology (sinus node anomaly, conduction disorder) or extracardiac such as a metabolic disorder or dysthyroidism, or after taking some medicines (betablocker, bradycardia calcium channel blockers). It can also be related to neurological causes as seen in the reported case 1 .
We will discuss through this clinical case, the different neurological causes that can lead to bradycardia.
Clinical case
Eight-year-old child with no specific pathological history, admitted to the emergency department for significant fatigability for one week. The child didn’t report any chest pain, dyspnea, neurological or infectious signs.
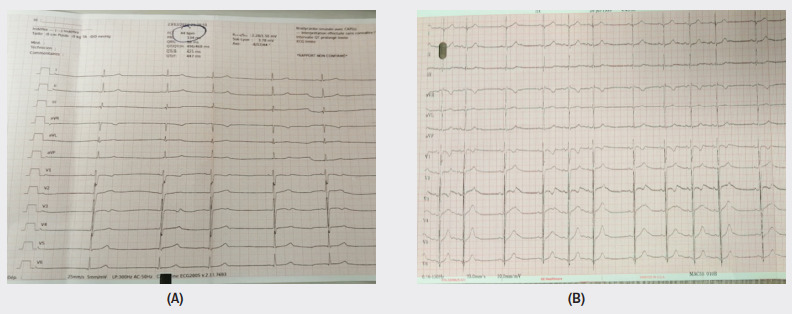
On clinical examination, he was conscious, his conjunctiva was well colored, apyretic (T=36,5°C), his heart rate was 43 beats per minute with a blood pressure of 120/60 mmHg. His cardiovascular examination has shown regular bradycardia without any audible murmur or signs of heart failure. The neurological examination was normal. No motor or sensory deficit was observed, no meningeal stiffness and reflexes were preserved. Blood tests were normal (blood glucose, hemoglobin, thyroid blood tests, blood ionogram, magnesemia, and serum calcium), infectious check-up was negative. The electrocardiogram revealed an atrial sinus block 2/1 with a heart rate at 43 beats per minute A deep breathing test was performed (Figure 1 ). An acceleration of the heart rate with a variability of 65% was found, and vagal hyperactivity was detected. The echocardiography was normal. The patient was hospitalized for clinical monitoring.
First electrocardiogram (A) showing an atrial sinus block 2/1 (calibration 25mm/s, 5mm/mV) and Second ECG (B) after deep breating (calibration 25mm/s, 10mm/mV).
During his hospitalization, he had sinus bradycardia at 35 beats per minute with syncopal unconsciousness of a few seconds. The post-syncopal clinical examination was unchanged. A few hours later, he made an abnormal movement with his lower lip.
Given this evolution, a brain scanner was performed to eliminate an intracranial cause. It revealed an expansive supra-tentorial intra-ventricular right process with hydrocephalus and signs of intracranial hypertension (Figure 2 ). The patient was transferred to the neurosurgery department and an external ventricular shunt was emergently performed. A brain magnetic resonance imaging showed a 22.5/42/32 mm right ventricular expansive process of lobulated contours blowing into the left ventricle (Figure 2 ).
Brain scanner (A,B) and brain magnetic resonance imaging (B) showing right intra ventricular expansive process (arrow) with hydrocephalus.

We planned to perform a lumpectomy. Unfortunately, the patient presented with severe bradycardia and profuse sweating followed by a drop in blood pressure and asystole that could not be recovered despite resuscitation measures.
Discussion
Brain tumors may manifest as headaches, seizures, clinical signs of intracranial hypertension (nausea, vomiting, visual disturbances), or motor deficit. Cardiac manifestations of brain tumors are non-specific, with a few rare cases of bradycardia described in the literature as warning signs 2 . Many investigations done allowed us to understand the mechanisms of bradycardia of so-called central origin (in the case of a brain tumor or haematoma, or a spinal cord tumor, or during neurosurgery) 3 .
The "Cushing's reflex" is characterized by the development of systemic hypertension, bradycardia and apnea secondary to an increase in intracranial pressure responsible for pressure and/or stretching of the brainstem. It is a protective and effective action of the brain that preserve an adequate cerebral perfusion pressure despite an increased intracranial pressure. It has been demonstrated that the haemodynamic features of classical Cushing’s response can be produced by electrical stimulation or distension of tissues within a thin strip of brain along the floor of the fourth ventricle in the rostral medulla and caudal pons. The efferent limb of the bradycardic response being the vagus nerve 4 . On the other hand, the elevation of intracranial pressure with the subsequent decrease of cerebral perfusion pressure significantly induced a vigorous cerebro-protective neuroendocrine system activation that can lead to the neurogenic stunned myocardium, which is defined as myocardial injury and dysfunction occurring after diverse types of acute brain injury as a result of imbalance of the autonomic nervous system 5 . Another cause that may explain bradycardia in brain tumors is its location. Cases of localization of tumors in the temporal or frontal lobe are associated with bradycardia 6 . Tumor location next to the regulatory heart centers (thalamus, hypothalamus and tonsil) may be accompanied by bradycardia 7 . A localization also in the posterior part of the cerebellum (sub-lobule IX-b of the cerebellar vermis) is associated with a decrease in sympathetic activity, responsible for bradycardia and hypotension 8 .
Epileptic seizures can also lead to changes in the autonomic nervous system. Tachycardia is the most common manifestation, but bradycardia and cardiac asystole may occasionally occur with temporal lobe seizures. Bradycardia and many other types of arrhythmias have also been described during episodes of focal or generalized epilepsy 8 . Other mechanisms described in the literature can also explain bradycardia such as trigeminocardiac Reflex 9 , ventricular catheter obstruction in cases of hydrocephalus or preganglionic sympathetic or parasympathic nerve fibers injury 10 .
Finally, all these mechanisms can coexist and lead to bradycardia as in the case of our patient, his tumor located in the right ventricle, with a large mass effect responsible for intracranial hypertension. He first presented bradycardia, with syncope, and then signs of vagal hyperactivity, with an epileptic seizure.
If bradycardia and signs of vagal hyperactivity is present with normal cardiac workup, further investigation is needed to find a central neurological cause, which may require urgent management.
Management of these patients include identification and treatment of the underlying cause of bradycardia, anti-cholinergics and if necessary cardiac pacing. Nevertheless, other causes of haemodynamic changes (i.e. anesthetic drugs, tumor manipulation) should also be considered and managed accordingly. We believe that this knowledge and understanding will help to identify the patients at risk and will also help in the management of neurosurgical patients with bradycardia 10 .
Conclusion
Bradycardia may be the only sign of a brain tumor with intracranial hypertension. It must lead us to perform an etiologic assessment with blood test, cardiac and also cerebral imaging, especially if there are other signs of vagal hyperactivity. Once diagnosed, the brain tumor must be urgently and effectively managed.
References
- Wung S F. Bradyarrhythmias: Clinical Presentation, Diagnosis, and Management. Crit Care Nurs Clin North Am. 2016;28(3):297–308. doi: 10.1016/j.cnc.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Kamil Ammar, Ghazzay Hazim. Journal of Medical Cases. 4. Vol. 9. Elmer Press, Inc.; 2018. Bradycardia as the First Sign of Brain Tumor: A Case Report; pp. 119–121. [DOI] [Google Scholar]
- Oppenheimer S. The anatomy and physiology of cortical mechanisms of cardiac control. Stroke. 1993;24:3–5. [PubMed] [Google Scholar]
- Dinallo S, Waseem M, Cushing Reflex StatPearls. Treasure; Island (FL. StatPearls Publishing; 2020. [Google Scholar]
- Nguyen Hoang, Zaroff Jonathan G. Current Neurology and Neuroscience Reports. 6. Vol. 9. Springer Science and Business Media LLC; 2009. Neurogenic stunned myocardium; pp. 486–491. [DOI] [PubMed] [Google Scholar]
- Park Ki-Hoon, Her Sung-Ho, Lee Jong-Min, Yoon Hee-Jeoung, Chin Jung-Yeon, Jeon Jun-Han, Park Ye-Lee, Do Kyong-Rock, Jung Yun-Hwa, Jin Seung-Won. Korean Circulation Journal. 9. Vol. 37. The Korean Society of Cardiology; 2007. Brain Tumor is a Rare Cause of both Bradycardia and Seizure; pp. 449–449. [DOI] [Google Scholar]
- Rehman H U, Atkin S L. Journal of the Royal Society of Medicine. 11. Vol. 92. SAGE Publications; 1999. Sleep disturbances and cardiac arrhythmia after treatment of a craniopharyngioma; pp. 585–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reifart Jörg, Tschernatsch Marlene, Hamm Christian W., Sperzel Johannes, Hain Andreas. BMC Cardiovascular Disorders. 1. Vol. 20. Springer Science and Business Media LLC; 2020. A case report of sinoatrial arrest caused by temporal lobe epilepsy in subclinical glioblastoma; pp. 30–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakil Husain, Wang Alick P., Horth Dillon A., Nair Saeda S., Reddy Kesava K.V. World Neurosurgery. Vol. 122. Elsevier BV; 2019. Trigeminocardiac Reflex: Case Report and Literature Review of Intraoperative Asystole in Response to Manipulation of the Temporalis Muscle; pp. 424–427. [DOI] [PubMed] [Google Scholar]
- Agrawal Amit, Timothy Jake, Cincu Rafael, Agarwal Trisha, Waghmare Lalit B. Clinical Neurology and Neurosurgery. 4. Vol. 110. Elsevier BV; 2008. Bradycardia in neurosurgery; pp. 321–327. [DOI] [PubMed] [Google Scholar]


