Abstract
Purpose
Understanding which factors are important for healthcare decisions of patients with diabetes in clinical practice is important to personalise diabetes care strategies and tailor care plans to the individual. The main drivers for these healthcare decisions remain unclear. This study assessed which key factors are relevant for healthcare decisions during clinical consultations for patients with type 1 diabetes (T1DM) and type 2 diabetes (T2DM), according to healthcare professionals.
Materials and Methods
Annual diabetes reviews were performed as part of a trial assessing the impact of a consultation model facilitating person-centred diabetes care in six hospital outpatient clinics. After each consultation, we asked healthcare professionals to choose a maximum of three out of 20 factors that were most relevant for healthcare decisions about treatment goals and the professional support needed during the upcoming year. Factors were characterised as either person or disease-related. Percentages reflect the number of annual diabetes reviews in which the key factor was reported.
Results
Seventeen physicians and eight diabetes specialist nurses reported the key factors relevant for healthcare decisions in 285 annual diabetes reviews (T1DM n = 119, T2DM n = 166). Healthcare professionals most often reported quality of life (31.9%), motivation (27.0%) and diabetes self-management (25.6%), and to a lesser extent glycaemic control (24.2%), to be important for decisions about treatment goals. For decisions about the professional support needed during the upcoming year patient’s preferences (33.7%), diabetes self-management (33.3%), quality of life (27.0%) and motivation (25.6%) were most often considered relevant by healthcare professionals.
Conclusion
According to healthcare professionals, person-related factors such as quality of life, diabetes self-management and motivation are predominantly relevant for healthcare decisions about treatment goals and the professional support needed during the upcoming year.
Keywords: diabetes mellitus, person-centred, preferences, shared decision making
Introduction
The prevalence of diabetes and the complexity of diabetes healthcare are increasing worldwide.1–4 In 2021 diabetes affected approximately 537 million adults, resulting in diabetes-related healthcare costs of over 966 billion dollars per year.5 The growing number of potential treatment options, the expanding online diabetes community in which patients engage in diabetes related online activities, eg, blogs, discussion and support groups, video tutorials, podcasts and other offerings,6 and the rapid technological advances, are increasing the need for shared decision making and person-centred care strategies, putting even greater emphasis on the role patients have within the decision making process.7
Whilst the importance of person-centred care is increasingly acknowledged by major leading institutions like the ADA and EASD,8 diabetes care decisions are often still driven by biological outcomes such as HbA1c, lipid levels and blood pressure measurements, suggesting that disease-related factors such as glycaemic control, cardiovascular risk factors, complications of diabetes and comorbidities are considered most important in healthcare decisions. However, treatment success is not so much depending on disease-related factors, but predominantly on factors that influence the patient’s diabetes self-management behaviour, like the patient’s personal situation and attitudes towards diabetes, social context and psychological wellbeing, which are considered person-related factors.1,9–11 Understanding which factors predominantly drive patients in the process of decision making is crucial when striving towards person-centred diabetes care.12,13 Insight in the patient’s values, preferences and social context enables effective patient-clinician communication and increases the chance of patients and clinicians successfully partnering up in the process of shared decision making.12,14,15 Previous research has shown that engagement of patients and clinicians in shared decision making may result in increased therapy adherence and patient engagement.16–18 In addition, shared decision making helps patients and healthcare professionals to decide on the best available healthcare strategy, reflecting what matters to the patient while using the best available evidence.7 This way, person-centred diabetes care may improve diabetes-related healthcare outcomes on the long term.19
However, to date it remains unclear to what extent the patient’s desires, needs and values are recognised by healthcare professionals as vital factors driving healthcare decisions. Therefore, we assessed which person and disease-related factors were considered most relevant for healthcare decisions according to healthcare professionals, during annual diabetes reviews in patients with type 1 diabetes (T1DM) and type 2 diabetes (T2DM) in secondary care. Furthermore, with physicians and diabetes specialist nurses fulfilling different roles in diabetes care, we assessed differences between the key factors reported by physicians and diabetes specialist nurses and between the key factors considered relevant for patients with T1DM and T2DM.
Materials and Methods
Study Design and Setting
Trained healthcare professionals performed outpatient annual diabetes reviews in six hospital clinics in the Netherlands as part of a study assessing the effect of a consultation model promoting person-centred care.20 After every annual diabetes review we asked healthcare professionals to provide the three key factors that, in their perception, determined the patient’s healthcare decisions out of a fixed list of twenty factors. Healthcare decisions were divided in decisions about treatment goals for the upcoming year, focused on the patient’s needs and desires regarding their diabetes management, and decisions about the professional support needed during the upcoming year, focused on the external help patients wanted and needed from professionals to succeed. The list of potential key factors reflected the current knowledge and literature about relevant factors for care decisions and discussions of organised working groups,20,21 consisting of people with diabetes, healthcare professionals and scientists.
Key factors were classified to be either person or disease-related. We considered age, ethnicity, level of education, stage of life, quality of life, lifestyle, pregnancy (wish), illness perception, motivation, patient’s preferences, self-management knowledge and skills, self-efficacy and opportunities for development, and social context to be person-related factors. Glycaemic control, cardiovascular risk factors, complications of diabetes, comorbidity, duration of diabetes, hereditary factors, use of medication and results of previous treatments were considered disease-related factors.
Patients with T1DM and T2DM were eligible for participation if they fulfilled the following inclusion criteria: age ≥ 18 years, sufficient language comprehension and ability to complete questionnaires. All patients provided written informed consent prior to participation. According to the Medical Ethical Committee of the University Medical Centre of Utrecht official approval of this study was not required under the Medical Research Involving Human Subjects Act (WMO).22 This study was conducted in accordance with the guidelines of the Declaration of Helsinki.
Participants
Prior to the annual diabetes review patients completed a questionnaire on age, sex, ethnicity, marital status, education, employment status, illness duration, family history of diabetes, diabetes-related complications and comorbidity. Furthermore, they filled out the Patient Activation Measure (PAM-13), a questionnaire consisting of 13 items assessing knowledge, skills and confidence for self-management.20,23 PAM-13 scores range from 0 to 100, with higher PAM-13 scores indicating a better ability of patients to manage their health. Data on type of diabetes, HbA1c, lipids, blood pressure and BMI were retrieved from electronic health records.
Implementation of the Consultation Model
Both physicians and diabetes specialist nurses were trained to use the consultation model and were educated about person and disease-related factors that may influence healthcare decisions, the principles of shared decision making, and dealing with disagreement. After two face-to-face training sessions (two hours per session) they applied the consultation model during the annual diabetes review. The consultation model consisted of four steps: 1) discussing person and disease-related factors that influence decisions about treatment goals and the professional support needed during the upcoming year together with the patient; 2) setting person and disease-related goals together; 3) discussing treatment options to reach the goals and making the decision; 4) assessing the professional support needed.20 Whether this step-wise approach was followed during the annual diabetes review and which topics were addressed depended on the actual situation of the patient and was not protocolled. After the annual diabetes review healthcare professionals were asked to indicate which factors they considered to be most relevant for this individual patient in decisions about treatment goals and decisions about the professional support needed during the upcoming year out of a list of twenty potential factors (Supplementary Figure 1). A minimum of zero and maximum of three factors could be chosen to be relevant for both decisions about treatment goals and the professional support needed during the upcoming year. The factors reported were considered to be of equal importance.
Statistical Analysis
Comparisons between characteristics of patients with T1DM and T2DM and physicians and diabetes specialist nurses were performed using chi square tests for categorical data and independent t-tests for continuous data. PAM-scores were transformed into a standardised activation score ranging from 0 to 100.23 Missing outcome data were handled using multiple imputation, to prevent reduction in statistical power and biased results due to patient exclusion.
Consultation time was compared between physicians and diabetes specialist nurses using independent t-tests. We calculated the frequency of person and disease-related factors reported by healthcare professionals for both decisions about treatment goals and the professional support needed during the annual diabetes reviews. Percentages reflect the number of annual diabetes reviews in which the factor was reported. Tests of proportions were used to assess differences between the total number of key factors stated and the frequency of each key factor between physicians and diabetes specialist nurses and patients with T1DM and T2DM. For each key factor a mixed-effects logistic regression analysis was performed, separately for patients with T1DM and T2DM, assessing the association between the factor reported and patient characteristics, with the type of healthcare professional as random factor. Mixed-effects ordinal logistic regression analyses were performed, with the type of diabetes and the type of healthcare professional as random factors, to assess the associations between the number of factors reported for decisions about treatment goals and the professional support needed during the upcoming year and patient characteristics, applicability of the consultation model, gathered insight in the patient’s situation and setting of goals at the end of the annual diabetes review.
A p-value <0.05 was considered statistically significant. Data analyses were performed using STATA intercooled version 14.2 (StataCorp LLC, Texas, USA).
Results
Study Population and Consultation
In total 119 patients with T1DM and 166 patients with T2DM were included in the study. Patients with T1DM had a mean PAM-score of 62.5 (± 15.6) compared to 59.2 (± 12.6) for patients with T2DM. Table 1 shows the baseline characteristics of the participating patients.
Table 1.
Patient Characteristics
| T1DM | T2DM | P-value | |
|---|---|---|---|
| N | 119 | 166 | |
| Age (years)* | 47.0 (13.5) | 64.0 (10.1) | <0.001 |
| Female gender† | 58.6 | 44.6 | 0.024 |
| Ethnicity† | 0.71 | ||
| Caucasian | 92.8 | 91.6 | |
| Other | 7.2 | 8.4 | |
| Marital status† | 0.70 | ||
| Married or cohabitating | 72.1 | 69.9 | |
| Single | 27.9 | 30.1 | |
| Education level† | <0.001 | ||
| Low | 9.9 | 30.5 | |
| Intermediate | 42.3 | 46.8 | |
| High | 47.8 | 22.7 | |
| Employment status† | <0.001 | ||
| Having a job | 63.0 | 27.6 | |
| PAM-13* | 62.5 (15.6) | 59.2 (12.6) | 0.057 |
| Duration of diabetes (years)* | 24.5 (14.5) | 18.9 (10.0) | <0.001 |
| Number of comorbid conditions* | 1.2 (1.6) | 2.4 (2.0) | <0.001 |
| Family history of diabetes† | 48.7 | 66.2 | 0.004 |
| Glucose-lowering medication† | |||
| None | 0 0 | 1.2 | 0.30 |
| Metformin | 5.0 | 47.6 | <0.001 |
| SGLT-2 inhibitors | 0 | 1.8 | 0.20 |
| Sulfonylurea derivatives | 0 | 7.2 | <0.01 |
| DPP-4 inhibitors | 0 | 0.6 | 0.46 |
| GLP-1 receptor antagonists | 1.7 | 3.0 | 0.53 |
| Basal insulin only | 1.1 | 21.6 | <0.001 |
| Basal-bolus insulin injection regimen | 43.3 | 58.1 | <0.05 |
| Insulin pump therapy | 54.4 | 12.8 | <0.001 |
| HbA1c* | 0.34 | ||
| mmol/mol Hb | 63.6 (11.4) | 62.0 (14.6) | |
| % | 8.0 (1.0) | 7.8 (1.3) | |
| Systolic blood pressure (mmHg)* | 132.0 (16.0) | 141.3 (19.9) | <0.001 |
| Diastolic blood pressure (mmHg)* | 77.6 (9.5) | 78.3 (11.9) | 0.61 |
| LDL cholesterol (mmol/l)* | 1.13 (0.35) | 1.13 (0.42) | 1.0 |
| HDL cholesterol (mmol/l)* | 0.80 (0.25) | 0.58 (0.22) | <0.001 |
| Total cholesterol (mmol/l)* | 2.02 (0.45) | 1.99 (0.51) | 0.60 |
| Body Mass Index (kg/m2)* | 26.2 (4.2) | 31.9 (6.4) | <0.001 |
Notes: *Mean (± SD). †%. P-values <0.05 are considered statistically significant.
Abbreviations: SC, Secondary Care; T1DM, Type 1 diabetes mellitus; T2DM, Type 2 diabetes mellitus; PAM-13, Patient Activation Measure-13, with a higher score indicating more knowledge, skill and confidence for self-management of one’s health or chronic condition; SGLT-2, sodium glucose co-transporter; DPP-4, dipeptidyl peptidase-4; GLP-1, glucagon-like peptide 1; LDL, low density lipoprotein; HDL, high density lipoprotein.
Healthcare consultations were performed by 17 physicians and 8 diabetes specialist nurses in six hospital outpatient clinics. Physicians had a mean age of 50.5 (± 9.2) years and 41% of the physicians was female. Diabetes specialist nurses had a mean age of 48.7 (± 2.6) years and 75% of the nurses was female. In 66.0% of patients the annual diabetes review was performed by a physician. Of all the consultations 67.7% was performed within 25 minutes. This was more often the case for physician-led than for nurse-led consultations (p<0.001).
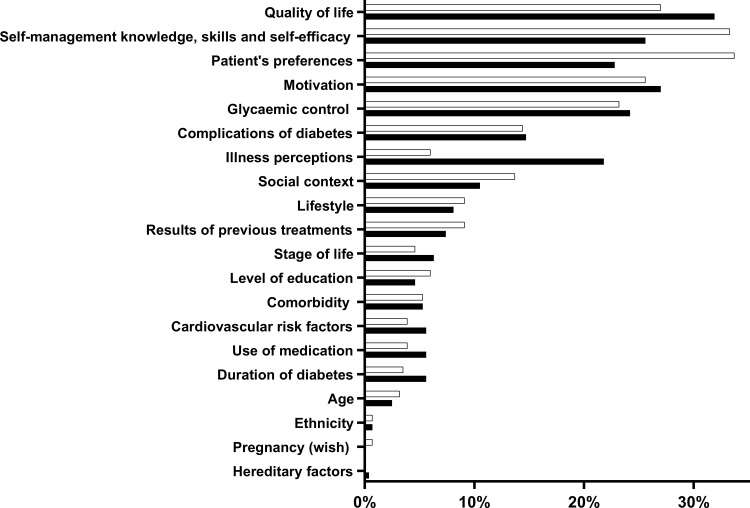
Key Factors for Decisions About Treatment Goals
Overall, quality of life (31.9% of annual diabetes reviews), motivation (27.0%), self-management knowledge and skills, self-efficacy and opportunities for development (25.6%) and glycaemic control (24.2%) were the key factors most often reported by healthcare professionals to be important for decisions about treatment goals (Figure 1).
Figure 1.
Person and disease-related factors relevant for healthcare decisions for patients T1DM and T2DM, according to healthcare professionals. After the consultation healthcare professionals indicated the most important factors (max. three factors) determining decisions about treatment goals and the professional support needed during the upcoming year. Bars represent the percentage of annual diabetes reviews in which each factor was reported by healthcare professionals for decisions about treatment goals (black bars) and the professional support needed (white bars).
A similar distribution was found in patients with T1DM, however, in patients with T2DM quality of life (34.9%), motivation (27.7%), patient’s preferences (27.7%) and self-management knowledge and skills, self-efficacy and opportunities for development (26.5%) were reported to be the most important factors for decisions about treatment goals (Table 2).
Table 2.
Person and Disease-Related Factors Reported by Healthcare Professionals to Influence Healthcare Decisions About Treatment Goals for the Upcoming Year
| Factors Provided | ||||
|---|---|---|---|---|
| Overall | T1DM | T2DM | P-value | |
| Quality of life | 31.9 | 27.7 | 34.9 | 0.20 |
| Motivation | 27.0 | 26.1 | 27.7 | 0.76 |
| Self-management knowledge and skills, self-efficacy and opportunities for development | 25.6 | 24.4 | 26.5 | 0.69 |
| Glycaemic control | 24.2 | 24.4 | 24.1 | 0.95 |
| Patient’s preferences | 22.8 | 16.0 | 27.7 | 0.020* |
| Illness perceptions | 21.8 | 18.5 | 24.1 | 0.26 |
| Complications of diabetes | 14.7 | 12.6 | 16.3 | 0.39 |
| Social context | 10.5 | 9.2 | 11.4 | 0.55 |
| Lifestyle | 8.1 | 7.6 | 8.4 | 0.81 |
| Results of previous treatments | 7.4 | 4.2 | 9.6 | 0.085 |
| Stage of life | 6.3 | 5.9 | 6.6 | 0.81 |
| Duration of diabetes | 5.6 | 5.9 | 5.4 | 0.86 |
| Use of medication | 5.6 | 4.2 | 6.6 | 0.38 |
| Cardiovascular risk factors | 5.6 | 4.2 | 6.6 | 0.38 |
| Comorbidity | 5.3 | 2.5 | 7.2 | 0.079 |
| Level of education | 4.6 | 5.9 | 3.6 | 0.36 |
| Age | 2.5 | 1.7 | 3.0 | 0.23 |
| Ethnicity | 0.7 | 0.0 | 1.2 | 0.48 |
| Hereditary factors | 0.4 | 0.8 | 0.0 | 0.25 |
| Pregnancy (wish) | 0.0 | 0.0 | 0.0 | - |
Notes: Person-related factors are in bold. Percentages represent the number of annual diabetes reviews in which the factor was reported (total n=285, T1DM n=119, T2DM n=166). *Significant difference between patients with T1DM and T2DM.
Abbreviations: T1DM, Type 1 diabetes mellitus; T2DM, Type 2 diabetes mellitus.
Patient’s preferences was more often reported as a key factor of importance for patients with T2DM than for patients with T1DM (T1DM: 16.0%; T2DM: 27.7% of annual diabetes reviews, p=0.020) (Table 2).
Key Factors for Decisions About Professional Support
For decisions about the professional support needed during the upcoming year, healthcare professionals considered patient’s preferences (33.7% of annual diabetes reviews), self-management knowledge and skills, self-efficacy and opportunities for development (33.3%), quality of life (27.0%) and motivation (25.6%) to be the most important factors overall (Table 3).
Table 3.
Person and Disease-Related Factors Reported by Healthcare Professionals to Influence Healthcare Decisions About the Professional Support Needed During the Upcoming Year
| Factors Provided | ||||
|---|---|---|---|---|
| Overall | T1DM | T2DM | P-value | |
| Patient’s preferences | 33.7 | 27.7 | 38.0 | 0.070 |
| Self-management knowledge and skills, self-efficacy and opportunities for development | 33.3 | 39.5 | 28.9 | 0.062 |
| Quality of life | 27.0 | 16.8 | 34.3 | 0.0010* |
| Motivation | 25.6 | 27.7 | 24.1 | 0.49 |
| Glycaemic control | 23.2 | 26.1 | 21.1 | 0.32 |
| Complications of diabetes | 14.4 | 10.9 | 16.9 | 0.15 |
| Social context | 13.7 | 10.1 | 16.3 | 0.13 |
| Lifestyle | 9.1 | 5.0 | 12.0 | 0.043* |
| Results of previous treatments | 9.1 | 5.0 | 12.0 | 0.043* |
| Illness perceptions | 6.0 | 2.5 | 8.4 | 0.038* |
| Level of education | 6.0 | 8.4 | 4.2 | 0.14 |
| Comorbidity | 5.3 | 1.7 | 7.8 | 0.023* |
| Stage of life | 4.6 | 4.2 | 4.8 | 0.81 |
| Cardiovascular risk factors | 3.9 | 2.5 | 4.8 | 0.32 |
| Use of medication | 3.9 | 2.5 | 4.8 | 0.32 |
| Duration of diabetes | 3.5 | 5.0 | 2.4 | 0.24 |
| Age | 3.2 | 0.8 | 4.8 | 0.056 |
| Ethnicity | 0.7 | 0.0 | 1.2 | 0.23 |
| Pregnancy (wish) | 0.7 | 0.8 | 0.6 | 0.84 |
| Hereditary factors | 0.0 | 0.0 | 0.0 | - |
Notes: Person-related factors are in bold. Percentages represent the number of annual diabetes reviews in which the factor was reported (total n=285, T1DM n=119, T2DM n=166). *Significant difference between patients with T1DM and T2DM.
Abbreviations: T1DM, Type 1 diabetes mellitus; T2DM, Type 2 diabetes mellitus.
Small, but distinct differences were found between the key factors reported for patients with T1DM and T2DM. For patients with T1DM self-management knowledge and skills, self-efficacy and opportunities for development (39.5%), patient’s preferences (27.7%), motivation (27.7%) and glycaemic control (26.1%) were considered most important (Table 3). For patients with T2DM healthcare professionals reported patient’s preferences (38.0%), quality of life (34.3%), self-management knowledge and skills, self-efficacy and opportunities for development (28.9%) and motivation (24.1%) to be most important (Table 3).
The key factors quality of life (T1DM: 16.8%; T2DM: 34.3%, p=0.0010), lifestyle (T1DM: 5.0%; T2DM: 12.0%, p=0.043), results of previous treatments (T1DM: 5.0%; T2DM: 12.0%, p=0.043), illness perceptions (T1DM: 2.5%; T2DM: 8.4%, p=0.038) and comorbidities (T1DM: 1.7%; T2DM: 7.8% of, p=0.023) were all considered to be of more importance for patients with T2DM in decisions about the professional support needed during the upcoming year, than for patients with T1DM (Table 3).
Key Factors Reported by Healthcare Professionals
Healthcare professionals indicated the key factors relevant for decisions about treatment goals and about the professional support needed in respectively 81.8% and 80.7% of the annual diabetes reviews. Diabetes specialist nurses more often reported key factors than physicians (treatment goals: physicians: 73.9%; nurses: 94.8%, p<0.001, professional support needed: physicians: 73.4%; nurses: 94.8%, p<0.001). No differences were found in the number of key factors reported by physicians or diabetes specialist nurses between patients with T1DM and T2DM.
For decisions about treatment goals, diabetes specialist nurses more often reported the key factors glycaemic control (nurses: 43.2%; physicians: 14.4%, p<0.001), quality of life (nurses: 41.2%; physicians: 27.1%, p=0.016), cardiovascular risk factors (nurses: 11.3%; physicians: 2.7%, p=0.003) and results of previous treatments (nurses: 12.4%; physicians: 4.8%, p=0.020) to be of importance, compared to physicians (Supplementary Table 1). Physicians more often indicated social context to play an important role (nurses: 5.2%; physicians: 13.3%, p=0.035) (Supplementary Table 1).
For decisions about the support needed during the upcoming year, diabetes specialist nurses more often reported glycaemic control (nurses: 40.2%; physicians: 14.4%, p<0.001), cardiovascular risk factors (nurses: 7.2%; physicians: 2.1%, p=0.034) and results of previous treatments (nurses: 14.4%; physicians: 6.4%, p=0.026) to be important, compared to physicians (Supplementary Table 2). Level of education however, was more often mentioned by physicians to be of importance (nurses: 1.0%; physicians: 8.5%, p=0.011) (Supplementary Table 2).
Association Between Patient Characteristics and Reported Key Factors
Healthcare professionals reported a mean of 2.31 (SD1.18) factors for decisions about treatment goals and a mean of 2.27 (SD 1.20) factors for decisions about the professional support needed during the upcoming year per consultation. No difference was found between the number of factors reported for patients with T1DM and patients with T2DM.
For patients with T1DM more key factors were indicated when patients were older (treatment goals: OR 1.06, p=0.013, professional support: OR 1.07, p=0.004), had a shorter illness duration (treatment goals: OR 0.95, p=0.023, professional support: OR 0.95, p=0.025) or when they received a high education (professional support: OR 4.2, p=0.058). When patients with T1DM already suffered from comorbidities, complications was more often considered key for healthcare decisions (treatment goals: OR 2.25, 95% CI: 1.24; 4.08, p=0.008, professional support OR 1.72, 95% CI: 1.04; 2.84, p=0.034) (Supplementary Tables 3 and 4). For patients with T1DM that received a high level of education, motivation (OR 3.65, 95% CI 1.32; 10.05, p=0.012) and social context (OR 28.9, 95% CI: 1.50; 558, p=0.026) were considered to play an important role in decisions about the professional support needed during the upcoming year (Supplementary Table 4).
For patients with T2DM, more factors were indicated when patients were female (treatment goals: OR 4.9, p=0.009, professional support OR 4.9, p=0.011). When patients had a higher BMI, motivation was more often indicated as a key factor for decisions about treatment goals (OR 1.10, 95% CI: 1.03; 1.18, p=0.007), whilst quality of life and illness perceptions were considered less important (quality of life: OR 0.93, 95% CI: 0.86–0.99, p=0.049, illness perceptions: OR 0.92, 95% CI: 0.84–0.99, p=0.044) (Supplementary Table 5). Furthermore, when patients were older, glycaemic control was less often considered important for decisions about the professional support needed during the upcoming year (OR 0.95, 95% CI: 0.90; 0.99, p=0.027), whilst the patient’s age, stage of life and comorbidity were considered more important (age: OR 1.40, 95% CI: 1.04–1.87, p=0.027; stage of life: OR 1.24, 95% CI: 1.01–1.53, p=0.045; comorbidity: OR 1.11, 95% CI: 1.00–1.24, p=0.049) (Supplementary Table 6).
Discussion
Our study shows that, whilst traditionally biological outcomes are often used to measure care performance and are presumed to be of major importance for healthcare decisions, healthcare professionals considered person-related factors most important for the decision making process. Quality of life, motivation, self-management knowledge and skills, self-efficacy and opportunities for developments and patient’s preferences in particular were indicated as vital factors for healthcare decisions. This suggests that the focus during the decision making process predominantly lies on the patient’s capacities, preferences and needs rather than on biological outcomes, and that healthcare professionals attempt to tailor care decisions to the individual.
Some distinct differences could be found between the factors reported for patients with T1DM and T2DM. These differences might reflect the characteristics of the pathophysiology of the two diseases, with T1DM being an autoimmune disease occurring independently of lifestyle and BMI and T2DM being strongly associated to a sedentary lifestyle and obesity.
Despite person-centred care now being acknowledged as state-of-the-art medicine by leading associations like the ADA and EASD,8 research on factors that drive patients in the decision making process is sparse. Most research has been focused on factors that influence decisions made by healthcare professionals alone or the role of the clinical environment in which the decision making process takes place.24–26 There is one open ended interview assessing which factors drive patients’ healthcare decisions in which the researchers found that, according to healthcare professionals, healthcare decisions during clinical consultations often relied on perceived social, cognitive and psychological characteristics of the patient, including intellectual ability, motivation, quality of social support, lifestyle, anxiety levels and style of interaction.27 Physical symptoms and individual demographic characteristics were considered less important. These results support our findings, indicating person-related factors predominantly driving healthcare decisions rather than disease-related factors. A study about factors that influence the intensity of care for patients with T2DM, mainly treated in primary care, found that person-related factors predominantly influenced the intensity of care chosen, further underlining our findings.28
While our study provides important knowledge about the key factors that are valuable to address during clinical consultations, it must be taken into account that these key factors were reported by healthcare professionals after each annual diabetes review and not by the patient. Thus our data describe the healthcare professional’s viewpoint. It remains unclear whether the perspectives of the patients align with those of the healthcare professionals. Healthcare professionals that participated in this study were trained to explore the patient’s situation and which factors played an important role in the decision making process. This training may have helped healthcare professionals to identify factors relevant for healthcare decisions. During the training person and disease-related factors were presented to be of equal importance, preventing any bias towards the type of factor reported. The list of 20 key factors that was provided to the healthcare professional to choose from after each consultation reflects the current knowledge on person and disease-related factors that may play an important role in healthcare decisions and determine self-management. We did not assess any order effect. Additionally, there was no option to add other factors to this list or to further elaborate on the decision. The reasoning behind factors chosen remains a topic that needs to be investigated further.
Potential patient and healthcare professional bias, cannot be ruled out, although both patients and healthcare professionals did not receive any incentive for participation. Furthermore, this study was conducted in patients with type 1 and type 2 diabetes in secondary care. Whether our results are generalisable to other healthcare settings and patient populations remains to be investigated.
This study helps to clarify which factors are important drivers for healthcare decisions in secondary diabetes care. Healthcare professionals can benefit from this knowledge by being more aware of the important role that person-related factors may play in healthcare decisions during clinical consultations. Discussing these person-related factors openly and elaborately will help patients and healthcare professionals gain a better understanding of the situation and the patient’s needs and desires, which may increase the chance of building a solid partnership and deciding on care plans that fit the individual patient and their unique situation. This is expected to eventually improve healthcare outcomes.
In addition, our findings further emphasize the need to measure healthcare outcomes and quality of care in a different way. Currently healthcare systems and insurance companies still measure the quality of care by biological outcomes such as HbA1c, blood pressure and lipid levels, whilst our findings indicate that person-related factors such as quality of life are predominantly important for healthcare decisions.
Conclusions
In conclusion, whilst biomedical and disease-related factors are often presumed to be of major importance in diabetes care decisions, we now show that person-related factors are predominantly driving decisions in diabetes care, according to healthcare professionals. Exploring these person-related factors more elaborately during clinical consultations may help patients and healthcare professionals to successfully partner up in shared decision making and create care plans that reflect the patient’s needs and values, eventually improving healthcare outcomes.
Acknowledgments
The authors thank the physicians and diabetes specialist nurses, and the patients from the outpatient hospital clinics for participating in the study.
Funding Statement
This project is supported by a grant from the Innovation Fund of the Dutch Health Insurance Companies and a grant from the Dutch Diabetes Foundation.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author Contributions
G.E.H.M.R. H.A.v.V. and E.J.P.d.K. conceived and designed the study and were responsible for the coordination of the study and the acquisition of data. All authors contributed in the analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors have no potential competing interests relevant to this article.
References
- 1.Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008;31(12):2398–2403. doi: 10.2337/dc08-1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beverly EA, Brooks KM, Ritholz MD, Abrahamson MJ, Weinger K. Assessment of emotional struggles in type 2 diabetes: patient perspectives. Diabetes Care. 2012;35(8):e62. doi: 10.2337/dc12-0661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(12):2126–2140. doi: 10.2337/dc16-2053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wermeling PR, Gorter KJ, van Stel HF, Rutten GE. Both cardiovascular and non-cardiovascular comorbidity are related to health status in well-controlled type 2 diabetes patients: a cross-sectional analysis. Cardiovasc Diabetol. 2012;11(1):121. doi: 10.1186/1475-2840-11-121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Federation ID. IDF Diabetes Atlas 10th edition 2021. International Diabetes Federation. February 4, 2022. www.diabetesatlas.org. Accessed February 4, 2022.
- 6.Litchman ML, Edelman LS, Donaldson GW. Effect of diabetes online community engagement on health indicators: cross-sectional study. JMIR Diabetes. 2018;3(2):e8. doi: 10.2196/diabetes.8603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruissen MM, Rodriguez-Gutierrez R, Montori VM, Kunneman M. Making diabetes care fit -are we making progress? Front Clin Diabetes Healthc. 2021;2. doi: 10.3389/fcdhc.2021.658817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.America Iomcoqohci. Crossing the quality chasm: a new health care system for the 21st century. Natl Acad Sci. 2001;57(3):120–121. [Google Scholar]
- 9.Weinger K, de Groot M, Cefalu WT. Psychosocial research and care in diabetes: altering lives by understanding attitudes. Diabetes Care. 2016;39(12):2122–2125. doi: 10.2337/dc16-2056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (Dawn) Study. Diab Med. 2005;22(10):1379–1385. doi: 10.1111/j.1464-5491.2005.01644.x [DOI] [PubMed] [Google Scholar]
- 11.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93(1):1–9. doi: 10.1016/j.diabres.2011.02.002 [DOI] [PubMed] [Google Scholar]
- 12.Tamhane S, Rodriguez-Gutierrez R, Hargraves I, Montori VM. Shared decision-making in diabetes care. Curr Diab Rep. 2015;15(12):112. doi: 10.1007/s11892-015-0688-0 [DOI] [PubMed] [Google Scholar]
- 13.Kunneman M, Branda ME, Hargraves I, Pieterse AH, Montori VM. Fostering choice awareness for shared decision making: a secondary analysis of video-recorded clinical encounters. Mayo Clin Proc Innov Qual Outcomes. 2018;2(1):60–68. doi: 10.1016/j.mayocpiqo.2017.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stiggelbout AM, Van der Weijden T, De Wit MP, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ (Clinical Research Ed). 2012;344:e256. doi: 10.1136/bmj.e256 [DOI] [PubMed] [Google Scholar]
- 15.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367. doi: 10.1007/s11606-012-2077-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weiner SJ, Schwartz A, Sharma G, et al. Patient-centered decision making and health care outcomes: an observational study. Ann Intern Med. 2013;158(8):573–579. doi: 10.7326/0003-4819-158-8-201304160-00001 [DOI] [PubMed] [Google Scholar]
- 17.Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8(5):410–417. doi: 10.1370/afm.1161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181(6):566–577. doi: 10.1164/rccm.200906-0907OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rutten G, Van Vugt H, de Koning E. Person-centered diabetes care and patient activation in people with type 2 diabetes. BMJ Open Diabetes Res Care. 2020;8(2):e001926. doi: 10.1136/bmjdrc-2020-001926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rutten GE, van Vugt HA, de Weerdt I, de Koning EJP. Implementation of a structured diabetes consultation model to facilitate a person-centered approach: results from a Nationwide Dutch Study. Diabetes Care. 2018;41(4):688–695. doi: 10.2337/dc17-1194 [DOI] [PubMed] [Google Scholar]
- 21.Quinn CC, Royak-Schaler R, Lender D, Steinle N, Gadalla S, Zhan M. Patient understanding of diabetes self-management: participatory decision-making in diabetes care. J Diabetes Sci Technol. 2011;5(3):723–730. doi: 10.1177/193229681100500327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Subjects CCoRIH. Medical scientific research and the WMO. Central Committee on Research Involving Human Subjects. Accessed September 24, 2019.
- 23.Health I. Patient Activation Measure (PAM) 13 License Materials. Portland: Insignia Health; 2016. [Google Scholar]
- 24.Scholl I, LaRussa A, Hahlweg P, Kobrin S, Elwyn G. Organizational- and system-level characteristics that influence implementation of shared decision-making and strategies to address them - a scoping review. Implement Sci. 2018;13(1):40. doi: 10.1186/s13012-018-0731-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alsulamy N, Lee A, Thokala P. Healthcare professionals’ views on factors influencing shared decision-making in primary health care centres in Saudi Arabia: a qualitative study. J Eval Clin Pract. 2022;28(2):235–246. doi: 10.1111/jep.13616 [DOI] [PubMed] [Google Scholar]
- 26.Baig AM, Humayaun A, Mehmood S, Akram MW, Raza SA, Shakoori T. Qualitative exploration of factors associated with shared decision-making in diabetes management: a health care provider’s perspective. Int J Qual Health Care. 2020;32(7):464–469. doi: 10.1093/intqhc/mzaa073 [DOI] [PubMed] [Google Scholar]
- 27.Lutfey KE, Campbell SM, Renfrew MR, Marceau LD, Roland M, McKinlay JB. How are patient characteristics relevant for physicians’ clinical decision making in diabetes? An analysis of qualitative results from a cross-national factorial experiment. Soc Sci Med. 2008;67(9):1391–1399. doi: 10.1016/j.socscimed.2008.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Vugt HA, Heijmans M, de Koning EJP, Rutten G. Factors that influence the intended intensity of diabetes care in a person-centred setting. Diab Med. 2020;37(7):1167–1175. doi: 10.1111/dme.14072 [DOI] [PubMed] [Google Scholar]