Abstract
Background
Ultrasonography has become an essential tool for the evaluation and management of thyroid and parathyroid diseases. Its applications extend beyond neck endocrine conditions to a multitude of pathologies within the head and neck region.
Objectives
Our study aimed to: (1) provide a broad review of neck ultrasonography and key findings in neck endocrine diseases; (2) support skilled performance office-based diagnostic ultrasonography and its varied applications.
Materials and methods
A review of the current literature was supplemented with clinical examples of key ultrasonographic findings.
Results
Current applications and key findings of ultrasonography in the diagnosis and management of neck endocrine conditions are reviewed.
Conclusion
Ultrasonography is a fundamental component in the evaluation and management of neck endocrine diseases. The reader is encouraged to use this review to enhance office-based performance and application of ultrasonography.
Video online
The online version of this article contains 11 additional videos. They are provided to illustrate some of the dynamic aspects of US performance. The article and the videos are available online (10.1007/s00106-022-01162-0). The videos can be found in the article back matter as “Electronic Supplementary Material”.
Keywords: Imaging, Ultrasound, Head, Neck, Endocrine
Abstract
Hintergrund
Die Sonographie ist zu einem wesentlichen Instrument für die Beurteilung und Behandlung von Schilddrüsen- und Nebenschilddrüsenerkrankungen geworden. Ihre Anwendung geht über den Bereich endokriner Erkrankungen des Halses hinaus bis hin zu einer Vielzahl pathologischer Veränderungen in der Kopf-Hals-Region.
Ziel
Die vorliegende Studie zielte darauf ab, (1) einen umfassenden Überblick über die Halssonographie und die wesentlichen Befunde bei endokrinen Erkrankungen im Halsbereich zu geben; (2) die qualifizierte Durchführung der diagnostischen Sonographie in der Praxis und ihrer verschiedenen Anwendungen zu unterstützen.
Material und Methoden
Dazu wurde ein Überblick über die aktuelle Literatur ergänzt durch klinische Beispiele wesentlicher sonographischer Befunde.
Ergebnisse
Aktuelle Anwendungsbereiche und wesentliche sonographische Befunde in der Diagnose und Behandlung endokriner Erkrankungen werden besprochen.
Schlussfolgerung
Die Sonographie ist ein grundlegender Bestandteil bei der Beurteilung und Behandlung von endokrinen Erkrankungen im Halsbereich. Die vorliegende Übersicht soll dem Leser dazu dienen, die Durchführung und Anwendung der Sonographie in der Praxis zu verbessern.
Schlüsselwörter: Bildgebung, Ultraschall, Kopf, Hals, Endokrin
Ultrasound (US) has a well-established role in the diagnosis and management of conditions of the thyroid and parathyroid glands and has increasing relevance for nonendocrine neck conditions. Once under the purview of radiologists, US has become a central feature of clinical practice for many surgeons and endocrinologists. Its versatility, favorable safety profile, ability to deliver real-time imaging, and low cost compared to other radiologic modalities have contributed to its widespread adoption [1].
Background
Since the initial application of US to thyroid evaluation in the 1960s, US technology has undergone a remarkable evolution with significant improvements in imaging quality as well as the development of more compact and user-friendly equipment [2]. Modern US devices utilize a transducer that functions as both a transmitter and receiver for the production and detection of ultrasound waves. Underlying this is the piezoelectric effect, in which application of an alternating voltage to crystals embedded in the transducer causes their mechanical deformations and produces pulsed ultrasound waves. Optimized use of US technology and interpretation of US images requires a basic understanding of the underlying physics of US, including imaging artifacts produced by physical properties of US, which are outside the scope of this article.
While US has become most recognized for its role in the diagnostic evaluation and management of thyroid and parathyroid disease, US applications extend to a multitude of pathologies within the head and neck, including salivary gland disorders, adult and pediatric neck masses, and assessment of laryngeal function. Furthermore, US-guided diagnostic procedures include fine-needle aspiration and core-needle biopsy. These methods have similar diagnostic efficacy [3]; preference for one approach over the other is often reflective of regional pathology expertise. Therapeutic procedures such as botulinum toxin or other therapeutic injections, and ethanol or thermal tumor ablation, are additional applications predicated on skilled performance of diagnostic US.
The clinician’s adoption of office-based diagnostic US and US-guided procedures enables real-time dynamic interrogation and management of anatomy and disease, enhancing diagnostic and therapeutic capability. Moreover, US-guided fine-needle aspiration biopsy (FNAB) for cytopathology can expedite diagnosis and streamline triage to surgery. Imaging the extent and location of disease and its relationship to surrounding structures informs surgical planning. Having intimate familiarity with neck anatomy uniquely positions surgeons for successful US utilization.
Performing US in a consistent sequence guards against “tunnel vision”
Optimized use of office-based US involves applying a systematic approach to facilitate efficient and comprehensive evaluation. High-frequency (7–15 MHz) and thus high-resolution linear array transducers are ideal for neck US. Conducting an US examination in a consistent sequence guards against “tunnel vision” that may lead to missed pathology. Examination should include assessment of the central and lateral neck compartments in the transverse view (Videos 1–4); any lesions of interest are also imaged in the longitudinal view. Central compartment examination should include the thyroid (and parathyroid glands if clinically appropriate), laryngotracheal complex, esophagus, and central compartment lymph nodes, although the sensitivity of US for the detection of abnormal central neck nodes is limited when the thyroid is present [4]. In the lateral neck, scanning should extend from the clavicle to the mandible and mastoid. Sweeping the transducer along the carotid sheath encompasses the jugular chain of nodes in levels II–IV. Level V is evaluated by sweeping the transducer superiorly and inferiorly in sequential swaths from the posterior border of the sternocleidomastoid muscle to the trapezius. When managing thyroid cancer, the surgeon must ensure comprehensive US evaluation is performed so that relevant lateral cervical metastatic disease is not left undetected [5].
Thyroid ultrasonography
Familiarity with the appearance of the normal thyroid gland and its surrounding structures enables an appreciation of thyroid pathology. The normal thyroid gland in the low midline neck is readily identified by its homogeneous gray appearance (Fig. 1). The thyroid isthmus appears crescent-shaped as it courses over the trachea, whose hyperechoic cartilaginous rings contain an anechoic interior. The examiner may take note of a paramedian pyramidal lobe coursing cranially, as well as thyroglossal duct remnants most often found just superior or inferior to the hyoid bone. The overlying sternothyroid and sternohyoid muscles appear hypoechoic to the thyroid; the superficial layer of the deep cervical fascia investing the strap musculature appears as thin hyperechoic lines. The esophagus usually protrudes to the left of the trachea and appears as concentric hyperechoic rings (Fig. 1). The thymus is typically atrophic in adults but can be seen inferior to the thyroid in younger patients and appears hypoechoic with bright internal punctate reflectors, an appearance that can be mistaken for metastatic papillary thyroid carcinoma (PTC).
Fig. 1.
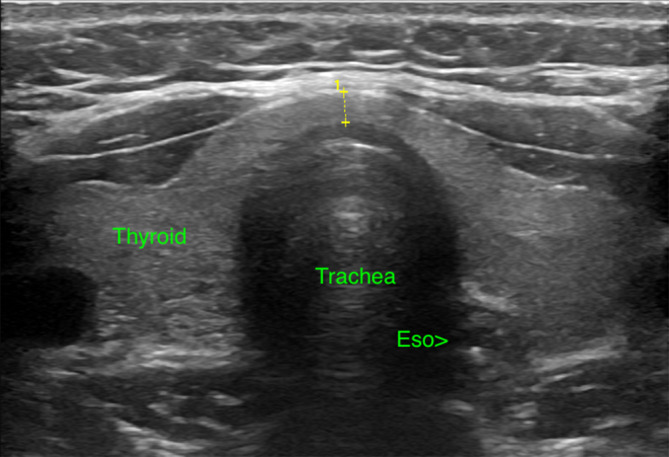
Normal thyroid gland with homogeneous gray appearance; midline transverse view. Cursors indicate isthmus, eso esophagus
The thymus is typically atrophic in adults and not readily seen on US
The relatively superficial position and soft tissue composition of the thyroid make it well-suited to US examination. An US evaluation can confirm the presence of a nodule, objectively characterize a nodule’s size, location, and appearance, assess for benign or suspicious features, and evaluate for the presence of other thyroid nodules or cervical lymphadenopathy [6]. Nodule characteristics that should be evaluated to assess risk of malignancy include echogenicity, composition, shape, margins, presence of calcifications, and associated lymphadenopathy.
Echogenicity
The echogenicity of a nodule is characterized relative to the appearance of normal thyroid tissue and the adjacent neck muscles [7]. Hypoechoic nodules are darker than normal thyroid; most malignancies are hypoechoic but hypoechogenicity is not specific for malignancy, as many benign nodules are hypoechoic, especially mildly so [6]. Rather, nodules that are moderately to markedly hypoechoic have an increased likelihood of being malignant [7, 8]. Isoechoic nodules have similar echogenicity to normal thyroid; hyperechoic nodules appear brighter than normal thyroid. Isoechoic and hyperechoic nodules are less likely to be malignant although when proven to be malignant are often of the follicular-type (follicular carcinoma, Hürthle cell carcinoma, follicular variant of PTC; [9–11]).
Composition
A nodule may be solid, cystic, or a combination, referred to as “predominantly solid” or “predominantly cystic.” Malignant nodules are more often solid in composition. Nodules that have an internal microcystic appearance comprising more than 50% of the volume of the nodule are termed “spongiform” and are characteristically benign, as are purely cystic nodules [12, 13].
Shape
A growth pattern demonstrating a “taller-than-wide” appearance (defined as an anteroposterior [AP] diameter that exceeds the transverse [T] diameter when imaging the thyroid in the transverse plane) is predictive of malignancy [14–18]. The basis for this finding is not well understood, although it has been proposed to relate to how normal versus cancerous nodules grow along tissue planes [8]. More recent analysis of shape in the transverse plane has highlighted its susceptibility to intra-observer and inter-observer variability and proposed the use of a slightly higher AP/T ratio or a multilevel rather than binary variable to improve specificity for malignancy without losing diagnostic performance [18, 19].
Margins
Evaluating the interface of a nodule with the surrounding thyroid parenchyma and thyroid capsule is important for stratifying risk of malignancy. Smooth and well-defined margins are reassuring, whereas irregular, spiculated, or infiltrative margins suggest malignancy. Importantly, nodules with irregular or infiltrative margins should be differentiated from nodules with indistinct margins that are difficult to discern from surrounding thyroid, as the latter is not associated with increased risk of malignancy [20].
Calcifications
Several types of calcifications can be seen in both benign and malignant nodules (Fig. 2). Microcalcifications are small (< 1 mm) echogenic foci that are highly associated with malignancy, usually PTC, with a specificity of over 90% [21–23]. The term “punctate echogenic foci” (PEF) has recently supplanted the term “microcalcifications” owing to the fact that not all such foci are calcifications (e.g., they can represent colloid, amyloid, or other granulomatous or reflective material). Macrocalcifications are coarse calcifications (> 1 mm) demonstrating posterior acoustic shadowing that occurs when all US waves are reflected back, unable to penetrate the calcium deposit. When coexistent with microcalcifications, coarse calcifications are highly associated with thyroid cancer, but their presence alone is not consistently associated with malignancy [22–24]. Peripheral rim calcifications, or “eggshell calcifications,” may be seen in both benign and malignant nodules; however, the presence of an “interrupted” rim calcification caused by tumor extruding through the calcification should raise concern for malignancy [25, 26].
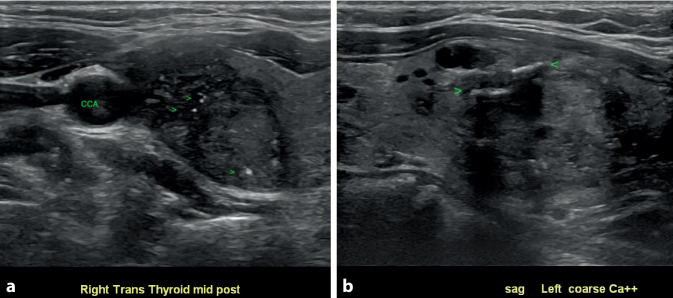
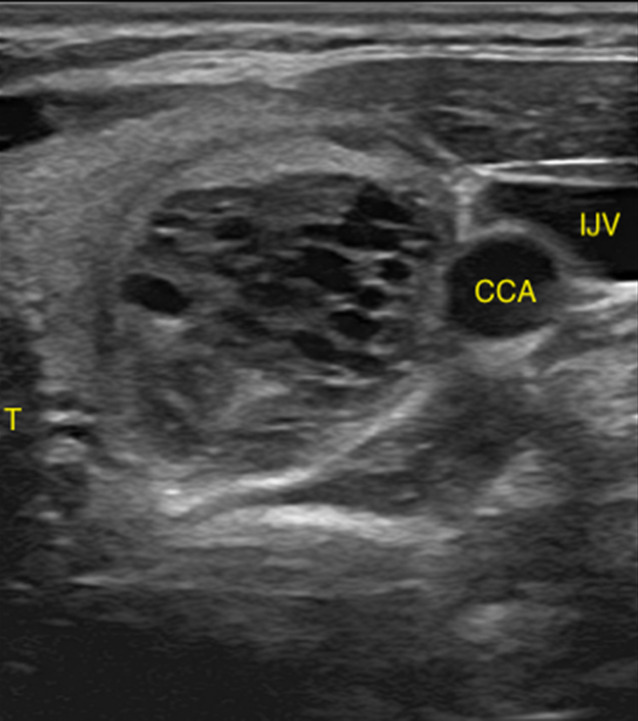
Fig. 2.
Calcifications can be small (< 1 mm) echogenic foci, as in this papillary thyroid carcinomas (a arrowheads, CCA common carotid artery), or coarse (> 1 mm) enough to cause posterior acoustic shadowing as in this benign multinodular goiter (b, arrowheads)
Associated lymphadenopathy
The neck compartments should be evaluated for the presence of abnormal lymph nodes, since locoregional metastatic disease is common in thyroid cancer [6]. Notably, detection of abnormal paratracheal nodes can be difficult in the presence of the thyroid gland. By contrast, the sensitivity of US for the detection of lateral neck metastasis is high, up to 93% in thyroid malignancy, with a specificity of up to 84% [4, 27]. The finding of suspicious nodes may influence the decision to perform lymph node FNAB, which may be accomplished in lieu of thyroid biopsy.
The sensitivity of US in detecting lateral neck metastasis is high
The correlation of US features with risk of malignancy has led several professional groups, including the American Thyroid Association (ATA), American College of Radiology (ACR), European Thyroid Association (ETA), and Korean Society of Thyroid Radiology (KSThR), to develop tiered scoring systems for stratifying risk and establishing size cutoffs for FNAB recommendation [6, 28–30]. These guidelines focus on the presence or patterns of sonographic characteristics and are similar but nonidentical in their classification systems. Malignancy risk estimates based on sonographic appearance are closely aligned between the systems but size thresholds for biopsy differ. Since no single US finding represents a sine qua non for thyroid cancer, it is the pattern or constellation of features that informs risk classification. The ACR Thyroid Imaging and Reporting Data System (TIRADS) quantifies risk by assigning points to individual features, with more suspicious features being assigned additional points; risk level is determined by summation of points for a given nodule. The ATA classification system, EU-TIRADS, and K‑TIRADS do not use a point system but similarly categorize risk based on the presence of select features. These systems have enhanced the consistency and universality of thyroid ultrasound reporting, while continuing to undergo modification to improve their specificity and sensitivity. An international/global TIRADS system is currently under development [31].
While US characteristics of thyroid nodules do not provide sufficient specificity to diagnose malignancy or malignancy type, US nonetheless may offer insight into the nature of the pathology at hand, and stratify risk to aid in decision-making regarding biopsy, complementary imaging, management, and surveillance. An advanced US practitioner should be able to appreciate the characteristic findings of specific malignant pathologies, discussed in the sections that follow.
Papillary thyroid carcinoma
The US features typical of PTC include a solid, hypoechoic lesion with microcalcifications or PEF (Figs. 2a and 3a). Microcalcifications are highly specific for PTC, and are favored to represent psammoma bodies [32] (tiny laminated, spherical collections of calcium which appear as tiny bright foci)—a histopathologic feature considered pathognomonic for PTC—or, less often, crystalline colloid. Cystic components may be present within a solid lesion. Margins are irregular or lobulated and taller-than-wide morphology is often present. Doppler examination is inconsistent but may reveal disorganized hypervascularity.
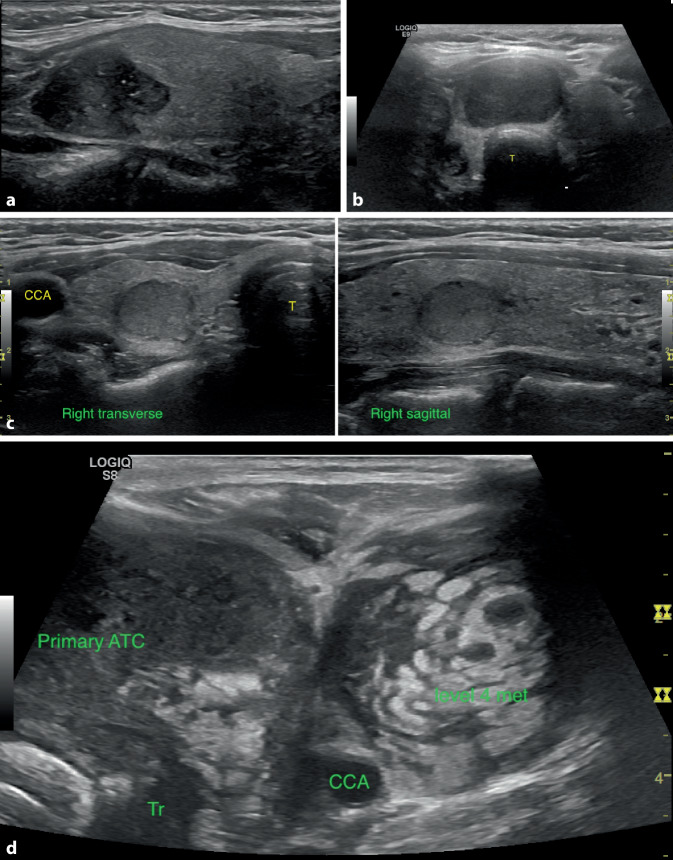
Fig. 3.
a Papillary Thyroid carcinoma. Solid, hypoechoic lesion with microcalcifications or PEF and lobulated margins (right sagittal view). b Follicular neoplasms are typically solid, and can be hyperechoic, isoechoic, or hypoechoic like this follicular carcinoma (midline transverse view of isthmus nodule; T trachea). c Medullary thyroid carcinoma appears solid and hypoechoic but cannot be distinguished from other neoplasms on ultrasound alone (right transverse and sagittal views, CCA common carotid artery; T trachea). d Anaplastic thyroid carcinoma is typically large, hypoechoic and heterogeneous, infiltrating, and associated with lymph node metastases (left transverse view; ATC anaplastic thyroid carcinoma, Tr trachea, CCA common carotid artery, level 4 met = lymph node metastasis in left lateral neck)
Follicular carcinoma
Follicular neoplasms, both benign and malignant, are typically solid, and can be hyperechoic, isoechoic, or hypoechoic lesions (Fig. 3b), the latter sometimes with a halo—a rim of decreased echoes around the nodule. Cystic components and calcifications are rare. Hypervascularity is common and FNAB samples are often bloody.
Hürthle cell carcinoma
The US characteristics of Hürthle cell carcinomas are similar to follicular neoplasms. These tumors tend to be solid with hypoechoic and hyperechoic components. An irregular border may sometimes be seen. Neither calcifications nor a halo is typically present.
Medullary thyroid carcinoma
The US appearance of medullary thyroid carcinoma (MTC) shares some features of PTC. Medullary thyroid carcinoma appears solid and hypoechoic and frequently has PEF representing both amyloid deposition and calcification (Fig. 3c). These foci may also appear within affected lymph nodes. Doppler examination may reveal disorganized hypervascularity.
Anaplastic thyroid carcinoma
The US findings of anaplastic thyroid carcinoma include a markedly hypoechoic lesion infiltrating the entire thyroid lobe with areas of necrosis or ill-defined calcifications (Fig. 3d). Involved lymph nodes may also exhibit necrotic changes. Invasion into surrounding vessels or soft tissue is often seen.
Lymphoma
The US appearance of lymphoma varies and may include a focal lesion within a lobe or diffuse abnormality involving the entire gland. The involved tissue is usually heterogeneous and hypoechoic and may be mistaken for anaplastic carcinoma. Posterior enhancement of the gland may be seen, owing to differences in acoustic impedance with the surrounding soft tissues. Associated lymph nodes appear large, round, hypoechoic, and hypervascular.
The thyroid is prone to developing multiple, often coalescent nodules
Thyroid US can aid in the diagnosis of benign thyroid diseases through evaluation of glandular size, echotexture, nodularity, and vascularity. Characteristic features may be seen in some conditions described in the following sections.
Chronic lymphocytic thyroiditis
The US findings of chronic lymphocytic thyroiditis, or Hashimoto’s thyroiditis, include patchy poorly defined hypoechoic areas resulting from accumulation of lymphoid tissue. Inflammatory changes alter thyroid architecture and generate heterogeneity and the appearance of “pseudonodules,” or hyperechoic and poorly demarcated regions sometimes separated by hyperechoic septations. Vascularity may be increased early and decreased late in the disease course. In later stages, the atrophied gland appears shrunken and imparts a “honeycomb” appearance. Central neck adenopathy may be prominent as a result of increased local immune activity and may be difficult to distinguish from small malignant lymphadenopathy.
Graves’ disease
The US features of Graves’ disease include diffuse thyroid enlargement, a thickened thyroid isthmus, heterogeneous hypoechogenicity, and hypervascularity. The hypoechoic appearance corresponds with increased vascular flow, increased cellularity, and lymphocytic infiltration [33]. Increased flow is also noted through the inferior thyroid artery.
Benign thyroid nodules
Most nodules are nonneoplastic, hyperplastic, or adenomatous nodules, consisting of follicular cells and colloid. Aggregates of colloid have a characteristic US appearance as bright echogenic foci with reverberation artifact in which echogenic lines of decreasing width appear posterior to the reflector. This so-called comet-tail sign distinguishes colloid from microcalcifications or other PEF. Spongiform appearance, as discussed earlier, is characteristic of benign nodules (Fig. 4). Follicular adenomas are benign neoplasms that present as homogeneous hyper-, iso-, or hypoechoic well-encapsulated round lesions, often with a halo sign distinguishing them from normal surrounding thyroid tissue. Nodules that are purely cystic are nearly uniformly benign and FNAB is not indicated, as nondiagnostic rates are high. Cystic lesions with a solid component requiring biopsy should undergo US guidance for any FNAB to ensure sampling of the solid component.
Fig. 4.
Benign spongiform nodule in the left thyroid lobe (transverse view). CCA common carotid artery, IJV internal jugular vein, T trachea
Multinodular goiter
The thyroid is highly prone to developing multiple, often coalescent nodules, and the primary goal in the evaluation of multinodular goiter is to identify whether there are any suspicious outliers within a gland full of otherwise benign change (Video 5). With increasing gland size comes decreasing accuracy of measurement. One should consider complementary cross-sectional imaging to more fully evaluate thyroid extent and impact, especially if substernal extension is suspected.
Parathyroid ultrasonography
High-resolution US is extremely useful for localizing abnormal parathyroid glands in patients with hyperparathyroidism. The success of US localization depends on the experience (and arguably, the motivation) of the examiner, with sensitivities for correct side and quadrant localization that exceed the performance of sestamibi scanning [34, 35]. In addition to its lower cost and ease of use, office-based US offers greater anatomic detail for preoperative planning, facilitating performance of focused parathyroidectomy. Furthermore, it allows for identification of coexistent thyroid pathology that may be managed concurrently.
Normal parathyroid glands are difficult to identify on US, owing to their small size and subtle US characteristics [36]. A recent investigation suggests that normal parathyroid glands can in fact sometimes be seen on US as small oval homogeneously hyperechoic structures ([37]; Fig. 5a). By contrast, abnormal hypercellular parathyroid glands characteristically appear as hypoechoic well-circumscribed ovoid structures (Fig. 5b), although a variety of shapes may be seen and the degree of hypoechogenicity may be variable. Parathyroid adenomas typically have a polar blood vessel that terminates near the capsule in the gland; its identification can be useful in differentiating a parathyroid adenoma from reactive lymphadenopathy, which is characterized by the presence of a hyperechoic fatty hilum [38]. Hyperplastic parathyroid glands similarly appear as hypoechoic ovoid structures; hyperplastic glands identified in the setting of longstanding secondary or tertiary hyperparathyroidism may demonstrate nodularity that gives the appearance of irregular borders. Calcifications within the gland may also be seen [38].
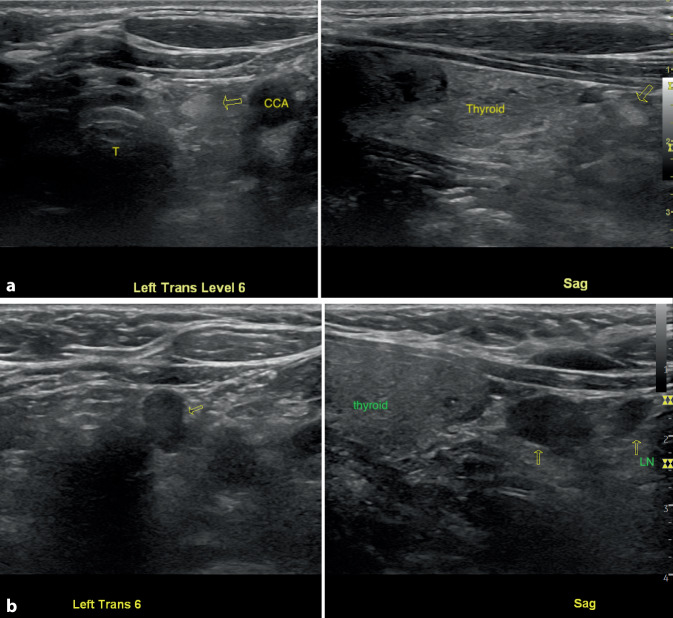
Fig. 5.
a Normal parathyroid glands are sometimes detectable, appearing as small oval homogeneously hyperechoic structures (left inferior parathyroid gland, transverse and sagittal views, open arrows). T trachea, CCA common carotid artery. b Hypercellular parathyroids (both adenomas and hyperplastic glands) usually appear as hypoechoic well-circumscribed ovoid structures (left inferior parathyroid adenoma, transverse and sagittal view). LN adjacent benign lymph node
Skilled localization of abnormal parathyroid glands is predicated on knowledge of parathyroid embryologic development. The superior parathyroid glands develop from the fourth branchial pouch and are usually located on the posterior aspect of the thyroid gland near the cricothyroid joint, dorsal to the recurrent laryngeal nerve (RLN). By contrast, the inferior parathyroid glands develop from the third branchial pouch, travel with the thymus, and have a relatively longer and more variable path of migration inferiorly. The inferior parathyroid glands may be located at the level of the inferior thyroid lobe on the anterior or posterolateral surface, along the thyrothymic ligament or within the thymic tongue at the thoracic inlet. The inferior parathyroid glands are situated ventral to the RLN. Notably, because the inferior and superior glands cross paths during embryologic migration, the inferior gland may be located cranial to the superior gland or the two glands may be found in close proximity [39].
Ectopic parathyroid glands result from abnormalities of embryologic migration. Failure of the inferior gland to descend may result in a location within the submandibular triangle or carotid sheath. On the other hand, failure of the inferior parathyroid gland to separate from the thymus may result in a location within the chest, often within the retrosternal thymus [40]. Ectopic superior parathyroid glands may be found above the superior pole of the thyroid, near the carotid artery, in the retropharyngeal/retroesophageal space, or even within the pyriform sinus [41]. Both inferior and superior parathyroid glands may be intrathyroidal in their location. Enlarged superior parathyroid glands may descend into the upper mediastinum through a combination of gravity, favorable tissue planes, and swallowing movements thought to contribute to downward displacement [42]. Importantly, these overly descended superior glands retain their dorsal relationship to the RLN, which may lead to inadvertent RLN injury if the surgeon fails to recognize the superior origin of the gland. The inferior thyroid artery or posterior surface of the carotid artery approximate the plane of the RLN; taking notice of the depth of the adenoma candidate relative to these structures on US examination can alert the surgeon to this possibility.
When localizing enlarged parathyroid glands, the examiner initially directs attention to the regions posterior and inferior to the thyroid gland between the carotid artery and the trachea; the transducer should be tilted at the sternal notch to examine the superior mediastinum. Scanning should be undertaken in a transverse plane (Video 6); longitudinal imaging should be used to interrogate structures of interest and assess craniocaudal position (Video 7). Depth, frequency, and focal adjustments may be made on the US system to optimize imaging of deeper planes. When an enlarged gland is not identified in an expected location, ectopia should be considered. However, ectopic glands located within the retropharyngeal or retroesophageal space may be difficult to visualize, as US waves do not pass through the air-filled structures that lie anterior to these spaces. Similarly, ectopic glands located behind bone within the chest cannot be visualized with neck US.
Neck ultrasonography
As noted in the previous section, US may be applied to the evaluation and management of many conditions that extend beyond the endocrine glands of the neck. The full scope of US applications cannot be covered here; instead, some additional applications beyond the thyroid and parathyroid glands related to the management of neck endocrine disease are discussed.
Lymph node evaluation
For patients with known or suspected thyroid cancer, US remains the most important imaging modality; its application should include assessment of the cervical lymph nodes to guide the need for compartment-based nodal dissection (Videos 8, 9). The sensitivity of ultrasound for detecting metastatic disease varies in the literature, and is highly operator-dependent, but is generally higher in the lateral neck (53–100%) than in the central neck (5–68%), in large part because the thyroid obstructs the contents of the central neck [4, 27, 43]. Ultrasound is especially useful in the surveillance setting, where absence of the thyroid allows for improved visualization of the central compartment [4, 44]. Overall, the specificity of US for detecting recurrent metastatic thyroid cancer is quite high, at 93% in the central neck and 84% in the lateral neck [27].
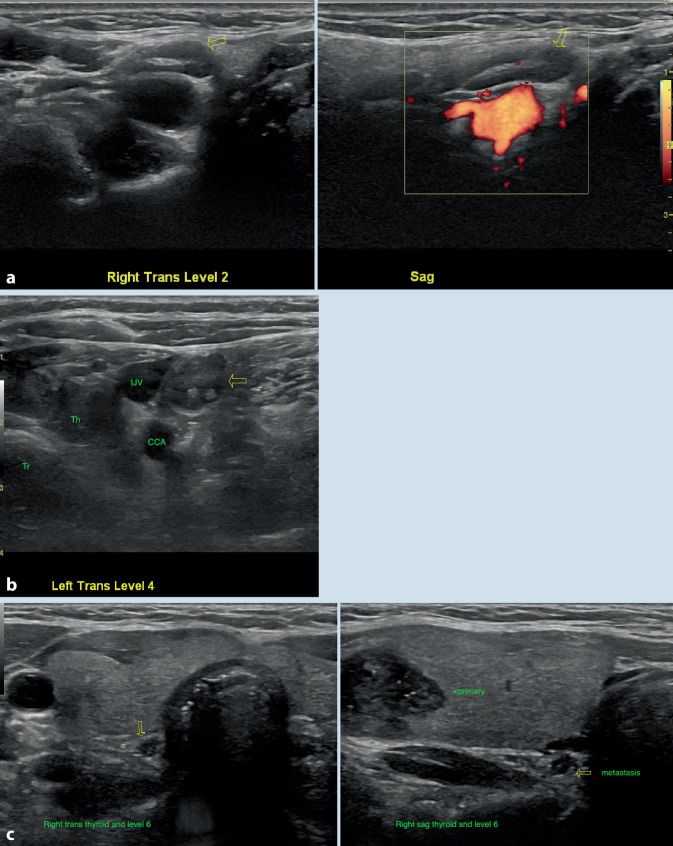
Lymph nodes are assessed for their size, shape, number, echogenicity, composition, margins, and presence or absence of a fatty hilum. Malignant nodes are often identified by their large size, with a short-axis measurement greater than 10–15 mm generally considered suspicious [45]. However, size alone should not determine the level of suspicion, as many reactive nodes will exceed this width, especially in the jugulodigastric region. Malignant nodes are typically rounded, in contrast to benign nodes that generally appear as a flattened, ovoid, elongated structures (Fig. 6). Nodes that are multiple or matted or demonstrate necrotic or cystic change or the presence of microcalcifications should raise concern for malignancy. Similarly, nodes that demonstrate irregular borders suggestive of extranodal extension into surrounding soft tissues are suggestive of malignancy. It should be noted that benign lymph nodes have smooth but more subtle borders than malignant nodes, whose borders are sharp. The sharp border is the result of tumor replacing normal nodal and fatty tissue, which creates a greater difference in the acoustic impedance between the node and adjacent tissue [46].
Fig. 6.
a Benign ovoid level 2 lymph node with central hyperechoic linear hilum (left panel, transverse view) and minimal superimposed hilar flow on power Doppler (right panel, sagittal view). b By contrast, rounded lymph node with metastatic papillary thyroid carcinoma, lacking visible hilum, with irregular margins and internal echogenic material (arrow). Tr trachea, Th thyroid with primary tumor, CCA common carotid artery, IJV internal jugular vein. c Although central compartment metastases are more difficult to detect in the presence of the thyroid gland, nodal metastases can be suspected when small rounded nodules are seen adjacent to the thyroid, such as in this case of papillary thyroid carcinoma (same patient as in Fig. 3a)
US is the most important imaging modality for patients with thyroid cancer
The presence or absence of a visible hilum can help to distinguish benign from suspicious nodes. The fatty hilum carries the blood supply of the node and appears as a central hyperechoic linear structure within a benign hypoechoic node. Use of color or power Doppler reveals a hilar vascular pattern, or no flow at all, in benign nodes. When nodal architecture is disrupted and angiogenesis occurs due to tumor, the hilum may be destroyed and vascularity becomes disordered and diffuse. As such, the presence of a clear echogenic hilum is highly sensitive in predicting benign cytology upon FNAB ([47]; Video 10).
Salivary gland ultrasonography
The superficial anatomic location of the major salivary glands is well-suited for US evaluation [48]; experienced clinicians can frequently examine and interpret findings without the need for more costly cross-sectional imaging modalities such as computed tomography (CT) or magnetic resonance imaging (MRI). Moreover, US may be used to evaluate the full spectrum of salivary gland pathology, including infectious, inflammatory, neoplastic, and calculous disease.
Normal salivary glands have a homogeneous echotexture that is similar to the normal thyroid gland. The parotid gland lies anterior to the ear and sternocleidomastoid muscle, overlying the mandible and masseter muscle. It is divided into superficial and deep lobes by the facial nerve that cannot be visualized on US, although the retromandibular vein serves as a landmark that approximates its location. The deep lobe of the parotid is only partially visible due to the acoustic shadow of the overlying mandible. Normal lymph nodes are commonly seen within the superficial lobe; these nodes typically do not exceed 5–6 mm in size, appear round to oval, and contain a prominent hyperechoic hilum [49]. The submandibular gland lies within the submandibular triangle where it wraps around the posterior border of the mylohyoid muscle. The posterior aspect of the submandibular gland may lie in close apposition to the tail of the parotid gland. Unlike the parotid gland, the submandibular gland does not contain intraglandular nodes; rather the nodes in level I are contained within the surrounding fat and connective tissue. The parotid and submandibular ducts cannot be visualized normally but may be appreciated proximal to an obstruction, or with administration of sialogogues that cause them to dilate [49]. The sublingual glands are located on the floor of the mouth, cranial to the mylohyoid muscle between the mandible laterally and the geniohyoid muscle medially. The sublingual gland may be difficult to distinguish from the adjacent submandibular gland that extends into the sublingual space.
The salivary glands are commonly affected by the administration of radioactive iodine (RAI) in the treatment of well-differentiated thyroid cancer, with up to two thirds of patients experiencing RAI-induced sialadenitis [50, 51]. Initial pain and swelling associated with salivary duct constriction may occur; later development of chronic sialadenitis is marked by parenchymal destruction and fibrosis as well as fatty degeneration and atrophy [51, 52]. Ultrasonographic features of RAI-induced sialadenitis include decreased glandular size, coarse echotexture with decreased echogenicity, and lobulated margins [52]. Notably, these changes may not correlate with the degree of xerostomia experienced [53].
Assessment of vocal fold mobility
Perioperative assessment of vocal fold function is regarded as an essential component of care in thyroid and parathyroid surgery [6, 54–57]. The US assessment of vocal fold mobility, when compared with the gold standard of fiberoptic laryngoscopy, has a reported sensitivity and specificity for detecting motion abnormalities ranging of 53.8–93.3% and 50.5–97.8%, respectively [58–60]. Adequate assessment of vocal fold mobility may be obtained in patients with favorable anatomy; gender and age impact successful visualization such that older men are often more difficult to image due to the shape and calcification of the thyroid cartilage [55, 60]. Further, US assessment may have special utility in resource-limited settings where laryngoscopy is not available. Its use has also become relevant during the COVID-19 pandemic where aerosol-generating procedures such as laryngoscopy pose potential infectious risk to clinicians [61].
US assessment may have special utility in resource-limited settings
The technique for laryngeal evaluation involves placement of a linear transducer with ample gel at the vertical midpoint of the thyroid cartilage or inferior to it in the cricothyroid region with the transducer angled superiorly. Reducing frequency to the 7–8-MHz range improves sound penetration. Vocal fold abduction and adduction are best visualized during respiration (Video 11). Assessment during phonation is difficult due to laryngeal movement, but maneuvers such as breath-holding and whistling may facilitate evaluation. The true vocal folds appear as hypoechoic muscle with a fine hyperechoic line at the free mucosal edge. The false vocal folds contain fatty connective tissue and appear hyperechoic; similarly, the arytenoid cartilages are hyperechoic and may be assessed for symmetry and movement.
Practical conclusion
Ultrasound (US) has an essential role in the management of thyroid and parathyroid disease with applications that extend to a multitude of pathologies within the neck.
Expertise in the use of US is gained through repetitious practice in the clinical setting; familiarity with normal anatomy is imperative for thorough and accurate performance of diagnostic US.
Recently, there has been growing interest in interventional US procedures, including ablation procedures to treat conditions of the thyroid.
It is important to recognize that safe and successful execution of these procedures is predicated on skilled performance of diagnostic US and familiarity with normal sonographic head and neck anatomy.
The clinician who builds a strong foundation of diagnostic US in all of its varied applications will be well-positioned to incorporate interventional procedures into practice.
Supplementary Information
Video 1: Transverse sweep through central (level 6) and lateral neck: Right central neck.
Video 2: Left central neck. A separate sweep through the midline central neck should extend from the foramen cecum/base of tongue to the sternum.
Video 4: Left lateral neck sweeps, beginning inferiorly, reveal scattered benign-appearing lymph nodes and normal salivary gland parenchyma at the superior limits.
Video 5: Multinodular goiter with coalescent, predominantly solid nodules. Transverse descending sweep through left lobe; note compressed and posteriorly displaced trachea.
Video 6: Parathyroid examination: Transverse sweep descending through thyroid and level 6 reveals an inferior parathyroid adenoma, in this case superficial to the inferior pole of the thyroid.
Video 7: Longitudinal/sagittal sweep is used to confirm findings and assess craniocaudal position (and observing patient during swallowing can further delineate parathyroid adenoma candidate).
Video 8: Transverse sweep through left level 6 in this patient with chronic lymphocytic thyroiditis and papillary thyroid carcinoma reveals abnormal thyroid and lymph nodes, even including a portion of a malignant lymph node lateral to carotid sheath.
Video 9: Transverse sweep through left levels 3 and 2 in a different patient with papillary thyroid carcinoma, demonstrating multiple metastatic nodes, some with cystic change.
Video 10: US-guided fine-needle aspiration biopsy (FNAB) of a small metastatic lymph node lacking a visible hilum. Note refraction (appearance of bending) and reverberation (needle tip step-off) artifacts of 25-gauge needle.
Video 11: Laryngeal ultrasound. Symmetrical vocal fold abduction and adduction seen during respiration and soft phonation.
Declarations
Conflict of interest
M. D. Russell and L. A. Orloff declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Footnotes

Scan QR code & read article online
References
- 1.Kangelaris GT, Kim TB, Orloff LA. Role of ultrasound in thyroid disorders. Otolaryngol Clin North Am. 2010;43(6):1209–1227. doi: 10.1016/j.otc.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Armstrong WB, Haidar YM. The history of head and neck ultrasonography. In: Orloff LA, editor. Head and neck ultrasonography: essential and extended applications. 2. Plural Publishing; 2017. [Google Scholar]
- 3.Cengiz AB, Tansuker HD, Gul R, Emre F, Demirbas T, Oktay MF. Comparison of preoperative diagnostic accuracy of fine needle aspiration and core needle biopsy in parotid gland neoplasms. Eur Arch Otorhinolaryngol. 2021;278(10):4067–4074. doi: 10.1007/s00405-021-07022-x. [DOI] [PubMed] [Google Scholar]
- 4.Hwang HS, Orloff LA. Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope. 2011;121(3):487–491. doi: 10.1002/lary.21227. [DOI] [PubMed] [Google Scholar]
- 5.Shalaby M, Hadedeya D, Lee GS, Toraih E, Kandil E. Impact of surgeon-performed ultrasound on treatment of thyroid cancer patients. Am Surg. 2020;86(9):1148–1152. doi: 10.1177/0003134820945229. [DOI] [PubMed] [Google Scholar]
- 6.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JY, Na DG, Yoon SJ, Gwon HY, Paik W, Kim T, et al. Ultrasound malignancy risk stratification of thyroid nodules based on the degree of hypoechogenicity and echotexture. Eur Radiol. 2020;30(3):1653–1663. doi: 10.1007/s00330-019-06527-8. [DOI] [PubMed] [Google Scholar]
- 8.Kim E-K, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002;178(3):687–691. doi: 10.2214/ajr.178.3.1780687. [DOI] [PubMed] [Google Scholar]
- 9.Jeh S, Jung SL, Kim BS, Lee YS. Evaluating the degree of conformity of papillary carcinoma and follicular carcinoma to the reported ultrasonographic findings of malignant thyroid tumor. Korean J Radiol. 2007;8(3):192–197. doi: 10.3348/kjr.2007.8.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim DS, Kim J, Na DG, Park S-H, Kim E, Chang K-H, et al. Sonographic features of follicular variant papillary thyroid carcinomas in comparison with conventional papillary thyroid carcinomas. J Ultrasound Med. 2009;28(12):1685–1692. doi: 10.7863/jum.2009.28.12.1685. [DOI] [PubMed] [Google Scholar]
- 11.Lee SK, Rho BH, Woo S-K. Hürthle cell neoplasm: correlation of gray-scale and power Doppler sonographic findings with gross pathology. J Clin Ultrasound. 2010;38(4):169–176. doi: 10.1002/jcu.20684. [DOI] [PubMed] [Google Scholar]
- 12.Bonavita JA. Sonographic patterns of benign thyroid nodules. AJR Am J Roentgenol. 2012;198(1):W102–103. doi: 10.2214/AJR.11.7737. [DOI] [PubMed] [Google Scholar]
- 13.Durante C, Grani G, Lamartina L, Filetti S, Mandel SJ, Cooper DS. The diagnosis and management of thyroid nodules: a review. JAMA. 2018;319(9):914–924. doi: 10.1001/jama.2018.0898. [DOI] [PubMed] [Google Scholar]
- 14.Alexander EK, Marqusee E, Orcutt J, Benson CB, Frates MC, Doubilet PM, et al. Thyroid nodule shape and prediction of malignancy. Thyroid. 2004;14(11):953–958. doi: 10.1089/thy.2004.14.953. [DOI] [PubMed] [Google Scholar]
- 15.Cappelli C, Castellano M, Pirola I, Gandossi E, De Martino E, Cumetti D, et al. Thyroid nodule shape suggests malignancy. Eur J Endocrinol. 2006;155(1):27–31. doi: 10.1530/eje.1.02177. [DOI] [PubMed] [Google Scholar]
- 16.Cappelli C, Pirola I, Cumetti D, Micheletti L, Tironi A, Gandossi E, et al. Is the anteroposterior and transverse diameter ratio of nonpalpable thyroid nodules a sonographic criteria for recommending fine-needle aspiration cytology? Clin Endocrinol (Oxf) 2005;63(6):689–693. doi: 10.1111/j.1365-2265.2005.02406.x. [DOI] [PubMed] [Google Scholar]
- 17.Moon HJ, Kwak JY, Kim E-K, Kim MJ. A taller-than-wide shape in thyroid nodules in transverse and longitudinal ultrasonographic planes and the prediction of malignancy. Thyroid. 2011;21(11):1249–1253. doi: 10.1089/thy.2010.0372. [DOI] [PubMed] [Google Scholar]
- 18.Mattingly AS, Noel JE, Orloff LA. A closer look at “taller-than-wide” thyroid nodules: examining dimension ratio to predict malignancy. Otolaryngol Head Neck Surg. 2021 doi: 10.1177/01945998211051310. [DOI] [PubMed] [Google Scholar]
- 19.Grani G, Lamartina L, Ramundo V, Falcone R, Lomonaco C, Ciotti L, et al. Taller-than-wide shape: a new definition improves the specificity of TIRADS systems. Eur Thyroid J. 2020;9(2):85–91. doi: 10.1159/000504219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seo H, Na DG, Kim J-H, Kim KW, Yoon JW. Ultrasound-based risk stratification for malignancy in thyroid nodules: a four-tier categorization system. Eur Radiol. 2015;25(7):2153–2162. doi: 10.1007/s00330-015-3621-7. [DOI] [PubMed] [Google Scholar]
- 21.Moon W-J, Jung SL, Lee JH, Na DG, Baek J-H, Lee YH, et al. Benign and malignant thyroid nodules: US differentiation—multicenter retrospective study. Radiology. 2008;247(3):762–770. doi: 10.1148/radiol.2473070944. [DOI] [PubMed] [Google Scholar]
- 22.Kwak JY, Han KH, Yoon JH, Moon HJ, Son EJ, Park SH, et al. Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology. 2011;260(3):892–899. doi: 10.1148/radiol.11110206. [DOI] [PubMed] [Google Scholar]
- 23.Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002;87(5):1941–1946. doi: 10.1210/jcem.87.5.8504. [DOI] [PubMed] [Google Scholar]
- 24.Kobaly K, Kim CS, Langer JE, Mandel SJ. Macrocalcifications do not alter malignancy risk within the American thyroid association sonographic pattern system when present in non-high suspicion thyroid nodules. Thyroid. 2021;31(10):1542–1548. doi: 10.1089/thy.2021.0140. [DOI] [PubMed] [Google Scholar]
- 25.Park YJ, Kim J-A, Son EJ, Youk JH, Kim E-K, Kwak JY, et al. Thyroid nodules with macrocalcification: sonographic findings predictive of malignancy. Yonsei Med J. 2014;55(2):339–344. doi: 10.3349/ymj.2014.55.2.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ohmori N, Miyakawa M, Ohmori K, Takano K. Ultrasonographic findings of papillary thyroid carcinoma with Hashimoto’s thyroiditis. Intern Med. 2007;46(9):547–550. doi: 10.2169/internalmedicine.46.1901. [DOI] [PubMed] [Google Scholar]
- 27.Zhao H, Li H. meta-analysis of ultrasound for cervical lymph nodes in papillary thyroid cancer: diagnosis of central and lateral compartment nodal metastases. Eur J Radiol. 2019;112:14–21. doi: 10.1016/j.ejrad.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Russ G, Bonnema SJ, Erdogan MF, Durante C, Ngu R, Leenhardt L. European thyroid association guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults: the EU-TIRADS. Eur Thyroid J. 2017;6(5):225–237. doi: 10.1159/000478927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, et al. ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS committee. J Am Coll Radiol. 2017;14(5):587–595. doi: 10.1016/j.jacr.2017.01.046. [DOI] [PubMed] [Google Scholar]
- 30.Shin JH, Baek JH, Chung J, Ha EJ, Kim J-H, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean society of thyroid radiology consensus statement and recommendations. Korean J Radiol. 2016;17(3):370–395. doi: 10.3348/kjr.2016.17.3.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoang JK, Middleton WD, Tessler FN. Update on ACR TI-RADS: successes, challenges, and future directions, from the AJR special series on radiology reporting and data systems. AJR Am J Roentgenol. 2021;216(3):570–578. doi: 10.2214/AJR.20.24608. [DOI] [PubMed] [Google Scholar]
- 32.Hong MJ, Noh B-J, Na DG, Paik W. Histopathological correlation of punctate echogenic foci on ultrasonography in papillary thyroid carcinoma. J Clin Ultrasound. 2022;50(1):49–57. doi: 10.1002/jcu.23107. [DOI] [PubMed] [Google Scholar]
- 33.Hegedüs L. Thyroid ultrasonography as a screening tool for thyroid disease. Thyroid. 2004;14(11):879–880. doi: 10.1089/thy.2004.14.879. [DOI] [PubMed] [Google Scholar]
- 34.Steward DL, Danielson GP, Afman CE, Welge JA. Parathyroid adenoma localization: surgeon-performed ultrasound versus sestamibi. Laryngoscope. 2006;116(8):1380–1384. doi: 10.1097/01.mlg.0000227957.06529.22. [DOI] [PubMed] [Google Scholar]
- 35.Gurney TA, Orloff LA. Otolaryngologist-head and neck surgeon-performed ultrasonography for parathyroid adenoma localization. Laryngoscope. 2008;118(2):243–246. doi: 10.1097/MLG.0b013e31815a9e9d. [DOI] [PubMed] [Google Scholar]
- 36.Ha TK, Kim DW, Jung SJ. Ultrasound detection of normal parathyroid glands: a preliminary study. Radiol Med. 2017;122(11):866–870. doi: 10.1007/s11547-017-0792-0. [DOI] [PubMed] [Google Scholar]
- 37.Cohen SM, Noel JE, Puccinelli CL, Orloff LA. Ultrasound identification of normal parathyroid glands. OTO Open. 2021;5(4):2473974X211052857. doi: 10.1177/2473974X211052857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shindo M. Parathyroid ultrasonography. In: Orloff LA, editor. Head and neck ultrasonography: essential and extended applications. 2. Plural Publishing; 2017. pp. 137–153. [Google Scholar]
- 39.Palestini N. Surgical anatomy of the parathyroid glands. In: Gasparri G, Camandona M, Palestini N, editors. Primary, secondary and tertiary hyperparathyroidism: diagnostic and therapeutic updates. Springer; 2015. [Google Scholar]
- 40.Pradhan R, Agarwal A, Lombardi CP, Raffaelli M. Applied embryology of the thyroid and parathyroid glands. In: Randolph GW, editor. Surgery of the thyroid and parathyroid glands. 3. Elsevier; 2021. pp. 15–25.e4. [Google Scholar]
- 41.Fukumoto A, Nonaka M, Kamio T, Kamura E, Ozu C, Baba S, et al. A case of ectopic parathyroid gland hyperplasia in the pyriform sinus. Arch Otolaryngol Head Neck Surg. 2002;128(1):71–74. doi: 10.1001/archotol.128.1.71. [DOI] [PubMed] [Google Scholar]
- 42.Thompson NW, Eckhauser FE, Harness JK. The anatomy of primary hyperparathyroidism. Surgery. 1982;92(5):814–821. [PubMed] [Google Scholar]
- 43.Al-Hilli Z, Strajina V, McKenzie TJ, Thompson GB, Farley DR, Richards ML. The role of lateral neck ultrasound in detecting single or multiple lymph nodes in papillary thyroid cancer. Am J Surg. 2016;212(6):1147–1153. doi: 10.1016/j.amjsurg.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 44.Lesnik D, Cunnane ME, Zurakowski D, Acar GO, Ecevit C, Mace A, et al. Papillary thyroid carcinoma nodal surgery directed by a preoperative radiographic map utilizing CT scan and ultrasound in all primary and reoperative patients. Head Neck. 2014;36(2):191–202. doi: 10.1002/hed.23277. [DOI] [PubMed] [Google Scholar]
- 45.Mao Y, Hedgire S, Harisinghani M. Radiologic assessment of lymph nodes in oncologic patients. Curr Radiol Rep. 2014;2(2):36. doi: 10.1007/s40134-013-0036-6. [DOI] [Google Scholar]
- 46.Iro H, Bozzato A, Zenk J. Atlas of head and neck ultrasound. Thieme; 2013. p. 399. [Google Scholar]
- 47.Rosário PWS, de Faria S, Bicalho L, Alves MFG, Borges MAR, Purisch S, et al. Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med. 2005;24(10):1385–1389. doi: 10.7863/jum.2005.24.10.1385. [DOI] [PubMed] [Google Scholar]
- 48.Bhatia KSS, Dai Y-L. Routine and advanced ultrasound of major salivary glands. Neuroimaging Clin N Am. 2018;28(2):273–293. doi: 10.1016/j.nic.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 49.Jecker P, Geisthoff UW, Meyer JE, Orloff LA. Salivary gland ultrasonography. In: Orloff LA, editor. Head and neck ultrasonography: essential and extended applications. 2. Plural Publishing; 2017. [Google Scholar]
- 50.Abdel Razek AAK, Mukherji S. Imaging of sialadenitis. Neuroradiol J. 2017;30(3):205–215. doi: 10.1177/1971400916682752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mandel SJ, Mandel L. Radioactive iodine and the salivary glands. Thyroid. 2003;13(3):265–271. doi: 10.1089/105072503321582060. [DOI] [PubMed] [Google Scholar]
- 52.Kim DW. Ultrasonographic features of the major salivary glands after radioactive iodine ablation in patients with papillary thyroid carcinoma. Ultrasound Med Biol. 2015;41(10):2640–2645. doi: 10.1016/j.ultrasmedbio.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 53.Soo Roh S, Wook Kim D, Jin Baek H. Association of xerostomia and ultrasonographic features of the major salivary glands after radioactive iodine ablation for papillary thyroid carcinoma. AJR Am J Roentgenol. 2016;207(5):1077–1081. doi: 10.2214/AJR.15.15776. [DOI] [PubMed] [Google Scholar]
- 54.Chandrasekhar SS, Randolph GW, Seidman MD, Rosenfeld RM, Angelos P, Barkmeier-Kraemer J, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol. Head Neck Surg. 2013;148(6):S1–37. doi: 10.1177/0194599813487301. [DOI] [PubMed] [Google Scholar]
- 55.Sinclair CF, Bumpous JM, Haugen BR, Chala A, Meltzer D, Miller BS, et al. Laryngeal examination in thyroid and parathyroid surgery: an American head and neck society consensus statement: aHNS consensus statement. Head Neck. 2016;38(6):811–819. doi: 10.1002/hed.24409. [DOI] [PubMed] [Google Scholar]
- 56.Musholt TJ, Clerici T, Dralle H, Frilling A, Goretzki PE, Hermann MM, et al. German association of endocrine surgeons practice guidelines for the surgical treatment of benign thyroid disease. Langenbecks Arch Surg. 2011;396(5):639–649. doi: 10.1007/s00423-011-0774-y. [DOI] [PubMed] [Google Scholar]
- 57.Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard BAG, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf) 2014;81:1–122. doi: 10.1111/cen.12515. [DOI] [PubMed] [Google Scholar]
- 58.Kandil E, Deniwar A, Noureldine SI, Hammad AY, Mohamed H, Al-Qurayshi Z, et al. Assessment of vocal fold function using transcutaneous laryngeal ultrasonography and flexible laryngoscopy. JAMA Otolaryngol. Head Neck Surg. 2016;142(1):74. doi: 10.1001/jamaoto.2015.2795. [DOI] [PubMed] [Google Scholar]
- 59.Wong K-P, Au K-P, Lam S, Lang BH-H. Lessons learned after 1000 cases of transcutaneous laryngeal ultrasound (TLUSG) with laryngoscopic validation: is there a role of TLUSG in patients indicated for laryngoscopic examination before thyroidectomy? Thyroid. 2017;27(1):88–94. doi: 10.1089/thy.2016.0407. [DOI] [PubMed] [Google Scholar]
- 60.Wong K-P, Lang BH-H, Chang Y-K, Wong KC, Chow FC-L. Assessing the validity of transcutaneous laryngeal ultrasonography (TLUSG) after thyroidectomy: what factors matter? Ann Surg Oncol. 2015;22(6):1774–1780. doi: 10.1245/s10434-014-4162-z. [DOI] [PubMed] [Google Scholar]
- 61.Noel JE, Orloff LA, Sung K. Laryngeal evaluation during the COVID-19 pandemic: transcervical laryngeal ultrasonography. Otolaryngol. Head Neck Surg. 2020;163(1):51–53. doi: 10.1177/0194599820922984. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1: Transverse sweep through central (level 6) and lateral neck: Right central neck.
Video 2: Left central neck. A separate sweep through the midline central neck should extend from the foramen cecum/base of tongue to the sternum.
Video 4: Left lateral neck sweeps, beginning inferiorly, reveal scattered benign-appearing lymph nodes and normal salivary gland parenchyma at the superior limits.
Video 5: Multinodular goiter with coalescent, predominantly solid nodules. Transverse descending sweep through left lobe; note compressed and posteriorly displaced trachea.
Video 6: Parathyroid examination: Transverse sweep descending through thyroid and level 6 reveals an inferior parathyroid adenoma, in this case superficial to the inferior pole of the thyroid.
Video 7: Longitudinal/sagittal sweep is used to confirm findings and assess craniocaudal position (and observing patient during swallowing can further delineate parathyroid adenoma candidate).
Video 8: Transverse sweep through left level 6 in this patient with chronic lymphocytic thyroiditis and papillary thyroid carcinoma reveals abnormal thyroid and lymph nodes, even including a portion of a malignant lymph node lateral to carotid sheath.
Video 9: Transverse sweep through left levels 3 and 2 in a different patient with papillary thyroid carcinoma, demonstrating multiple metastatic nodes, some with cystic change.
Video 10: US-guided fine-needle aspiration biopsy (FNAB) of a small metastatic lymph node lacking a visible hilum. Note refraction (appearance of bending) and reverberation (needle tip step-off) artifacts of 25-gauge needle.
Video 11: Laryngeal ultrasound. Symmetrical vocal fold abduction and adduction seen during respiration and soft phonation.