Abstract
INTRODUCTION:
Knowledge about cancer, treatment, and likely treatment outcomes is critically important for decision-making regarding adherence to the treatment. Hence, it seems imperative to find out the attitude and belief of cancer patients to determine the efficacy of cancer diagnostic and treatment available along with assessing the efficacy of prevention. The purpose of this study was to determine the level of knowledge, belief, and attitude of cancer patients who came to our facility.
MATERIALS AND METHODS:
The present study was a descriptive cross-sectional study which was conducted at All India Institute of Medical Sciences, Rishikesh, from July 2020 to December 2020. One hundred fifty-six newly diagnosed cancer patients were recruited. The participants were provided with a validated 44 key questionnaire divided into four different categories including the sociodemographic profile, knowledge, belief, and attitude subheading. Mean, frequency, percentage, and Chi-square test were calculated to do data analysis using SPSS version 23.0.
RESULTS:
Out of the total of 156 newly diagnosed cancer patients, only 130 patients provided responses so the overall response rate was 84.3%. Most of cancer patients had moderately adequate knowledge (79 [60.5%]), poor belief (111 [86%]), and neutral attitude (69 [54%]) regarding cancer. The Chi-square test revealed a link between educational level and cancer knowledge (P = 0.01). Males showed a more positive attitude than females, and this difference was statistically significant (P = 0.02).
CONCLUSIONS:
Cancer patients need to be made more aware of the red flag signs of cancer and improvise their attitude toward cancer. Cancer care programs should not only involve cancer patients but also involve their caregivers because the understanding of family members is of utmost importance to fight this disease.
Keywords: Cancer, cancer screening, cancer's attitude, cancer's belief, cancer's knowledge
Introduction
Cancer is a leading cause of morbidity and mortality in developed countries.[1,2,3] Cancer has also been found out to be one of the leading causes of death worldwide, accounting for nearly 10 million deaths in 2020.[4] Knowledge about cancer, treatment, and likely treatment outcomes is critically important for decision-making regarding adherence to prescribed therapy.[5] It has been also found that cultural and social beliefs of the patient toward their illness influence perceptions about the meaning of an illness, the useful types of treatment, and the likely outcome of health behaviors related to the prevention and control of the disease.[6] Furthermore, knowledge and perception toward cancer have been found to significantly impact help-seeking in patients and adherence to treatment.[7,8] However, late diagnosis and treatment remain are significant barriers to improving outcomes, which, in turn, is a cause of poor knowledge less likely to seek treatment.[9] As a result, it appears necessary to analyze the efficacy of knowledge about various cancer diagnostic and therapeutic options among cancer patients, as well as the efficacy of knowledge about various cancer preventative measures among the general public, if possible.[10] The purpose of this study was to assess the knowledge, belief, and attitude of cancer patients who were visiting hospital.
Materials and Methods
Study design and setting
This study was a descriptive cross-sectional study was conducted at All India Institute of Medical Sciences, (AIIMS), Rishikesh, from July 2020 to December 2020.
Study participant and sampling
One hundred and fifty-six newly diagnosed cancer patients who were visiting oncology outpatient department were recruited after giving explaining about the study. Written informed consent was obtained from each study participant and anonymity and confidentially of each study participant was maintained during the study. Ethical approval for this study was obtained from the Institutional Ethical Committee (AIIMS/IEC/20/210).
Cancer patients who were newly diagnosed cancer, who were over the age of 18 years, and could read and write Hindi were included in this study. Cancer patients who experienced a recurrence of cancer and were on follow-up treatment were excluded from the study.
Data collection tool and technique
Data collection tools consist of a total of 44 items which were included in a total of 4 sections. Section-I included questions related to sociodemographic profile of study participants. Section-II included questions related to knowledge, Section-III included questions related to attitude, and Section-IV included questions related to belief about cancer. Each question was scored into a binary system, i.e., 0 – no or 1 – yes according to information provided by participants. Scoring criteria for knowledge were ranged from 0% to 35% inadequate, 36%–75% moderately adequate, and 75%–100% adequate knowledge; belief scoring ranged from 0% to 50% poor belief and 51%–100% good belief; attitude scoring ranged from 0% to 33% unfavorable, 34%–70% neutral and 70%–100% favorable attitude (negative statements were reverse-scored) for cancer prevention.
Data analysis was done using IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp. IBM Corp. Written informed consent was obtained from each study participant after proper explanation about the study. The questionnaires were available in the bilingual language, English and Hindi, whichever was preferred by cancer patients. The interviewees were assured of the confidentiality of the data and that this would have no impact on their treatment.
Sociodemographic profile was analyzed using mean, frequency, and percentage. Association between sociodemographic variables and knowledge, belief, and attitude was determined using Chi-square test at level of 0.05.
Results
Sociodemographic profile of patients
A total of 156 newly diagnosed patients of cancer were provided with the questionnaire, out of which 130 provided with all answers, and 26 were excluded because they filled <50% of responses. Hence, the overall response rate was 83.3%. The age of participants ranged from 24 to 67 years (mean 49.4 ± 1.24). There were 67 (52%) female respondents and 63 (48%) male respondents. Seventy-three (56%) patients were residing in urban areas. One hundred twenty (92%) patients were married. Education level was up to primary school in 53 (41%) patients and 33 (25%) patients were graduate and above [Table 1].
Table 1.
Sociodemographic details of patients (n=130)
| Variables | Options | Frequency (%) |
|---|---|---|
| Age (years) | 24-67 (49.4±1.24) | |
| <50 | 63 (48) | |
| >50 | 67 (52) | |
| Gender | Male | 63 (48) |
| Female | 67 (52) | |
| Residence | Urban | 73 (56) |
| Rural | 57 (44) | |
| Marital status | Single | 9 (7) |
| Married | 120 (92) | |
| Widow | 1 (1) | |
| Educational level | Primary | 53 (41) |
| High school | 16 (12) | |
| Senior secondary | 28 (22) | |
| Graduate | 15 (11) | |
| Postgraduate | 18 (14) | |
Knowledge about cancer among patients
Forty-seven (36%) believed that cancer is an old age disease. Only forty-nine (38%) patients were aware of the warning signs of cancer. One hundred thirteen (90%) patients had the acquaintance that smoking and alcohol have a causative association with cancer. Forty-one (31.5%) patients knew regarding the role of dietary factors in cancer. Thirty (23%) patients had a perception that cancer is a communicable disease. Furthermore, 35 (27%) had a familiarity that cancer runs in families and 95 (73%) said it was not a genetic disease. Thirty-six (27.6%) patients alleged that biopsy causes the spread of cancer. One hundred fifteen (88.5%) patients were aware that surgery, radiation therapy, or chemotherapy are the treatment modalities for cancer. Regarding cure of cancer, 19 (14.6%) assumed it is curable in all stages, 38 (29.2%) never, and 71 (55%) that cure depends on stage so is sometimes curable. Whether chemotherapy or radiation therapy was painful management strategies, 42 (32.3%) responded with an answer, yes, but 67.7% suggested that these treatments were not painful. Whether screening for cancer leads to early detection of cancer, 42 (32.3%) had responded no, but the majority (67.7%) had the opinion that it will lead to early detection. On scoring, 2 (1.55), 79 (60.5%), and 49 (38%) had inadequate knowledge, moderately adequate knowledge, and adequate knowledge, respectively.
Belief about cancer among patients
Fifty-seven (43.8%) patients believed that they had cancer because of their physical status and 49 (37.6%) believed that they acquired this disease because of their family issues. One hundred four (80%) patients had a lot of worries about cancer and believed that they will develop complications of cancer even after treatment and will eventually die because of it. One hundred seven (82.3%) patients were frightful suffering from cancer. Sixty-six (50.7%) patients believed that suffering from cancer will ruin their relationships. One hundred and eighteen (90.7%) patients reported that they ate a balanced diet but still suffered from cancer.
Attitude about cancer among patients
Regarding attitude about cancer, marking was done on the Likert scale, 69 (54%) patients had a neutral attitude, 52 (40%) had a favorable attitude, and 9 (6%) had an unfavorable attitude toward cancer. Overall, most of cancer patients had moderately adequate knowledge (79 [60.5%]), poor belief (111 [86%]), and neutral attitude (69 [54%]) regarding cancer. Figure 1 shows the combined scores for knowledge, belief, and attitude of patients toward cancer.
Figure 1.
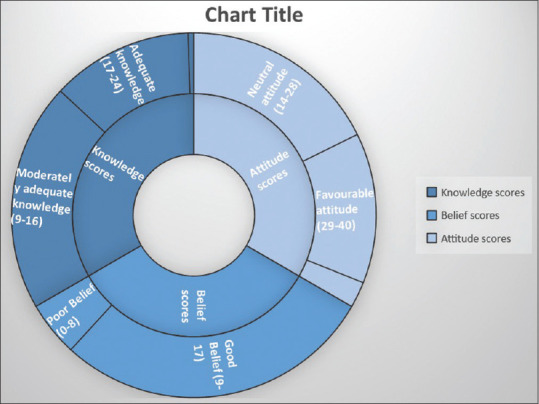
Scores for knowledge, belief, and attitude of patients toward cancer
Association of knowledge, belief, and attitude with sociodemographic variables
Patients residing in urban areas had adequate knowledge about cancer and it was statistically significant (P = 0.04). Furthermore, there was an association of educational level (graduate and postgraduate) with knowledge about cancer (P = 0.01). Males had a favorable attitude compared to females and it was statistically significant (P = 0.02). There was no statistically significant association of belief with any of the variables [Table 2].
Table 2.
Association of knowledge, belief, and attitude with sociodemographic variables
| Variables | Options | Knowledge | Belief | Attitude | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| IA | MA | AK | Chi value | PB | GB | Chi value | UA | NA | FA | Chi value | ||
| Age (years) | <50 | 1 | 35 | 27 | 0.49 | 9 | 54 | 0.91 | 6 | 35 | 22 | 0.34 |
| >50 | 1 | 44 | 22 | 10 | 57 | 3 | 34 | 30 | ||||
| Gender | Male | 2 | 37 | 24 | 0.33 | 8 | 55 | 0.54 | 1 | 33 | 29 | 0.04* |
| Female | 0 | 42 | 25 | 11 | 56 | 8 | 36 | 23 | ||||
| Residence | Urban | 0 | 40 | 33 | 0.04* | 11 | 62 | 0.86 | 7 | 44 | 22 | 0.02* |
| Rural | 2 | 39 | 16 | 8 | 49 | 2 | 25 | 30 | ||||
| Marital status | Single | 0 | 7 | 2 | 0.58 | 3 | 6 | 0.24 | 0 | 7 | 2 | 0.47 |
| Married | 2 | 72 | 46 | 16 | 104 | 9 | 61 | 50 | ||||
| Widow | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | ||||
| Educational level | Primary | 1 | 39 | 13 | 0.01* | 7 | 46 | 0.72 | 1 | 26 | 26 | 0.07 |
| High school | 0 | 8 | 8 | 1 | 15 | 0 | 8 | 8 | ||||
| Senior secondary | 1 | 19 | 08 | 5 | 23 | 3 | 15 | 10 | ||||
| Graduate | 0 | 3 | 12 | 2 | 13 | 1 | 10 | 4 | ||||
| Postgraduate | 0 | 10 | 8 | 4 | 14 | 4 | 10 | 4 | ||||
IA=Inadequate knowledge, MA=Moderately adequate knowledge, AK=Adequate knowledge, PB=Poor belief, GB=Good belief, UA=Unfavorable attitude, NA=Neutral attitude, FA=Favorable attitude
Discussion
During the past few decades, notions about cancer have changed remarkably due to advancements in diagnostics and management options. There has been an emphasis on cancer control programs and health education for screening and early diagnosis. This study was done to get an idea about the knowledge, belief, and attitude of patients toward cancer and identify the requirement of further health education.
In the present study, 90% of patients were aware of smoking as a risk factor and it was similar to Berger et al. who also reported in their study that 90% of the patients were aware of this fact.[11] Only 38% of patients were aware of warning signs of cancer, it was slightly more than reported 25% in a study by Singh Mahendra et al.[12] The knowledge regarding dietary factors as a risk factor was 31.8% in the present study, similar to that reported by Lynes et al.[13] and Richards et al.[14] that awareness of cancer risk factors was low except for tobacco use. Twenty-three percent of patients had the notion that cancer is a communicable disease which was similar (21%) to that reported by Aweke et al.[15] against >50% reported by Gamage and Jayawardana.[16] Regarding knowledge about whether cancer can be cured or not, 14.6% of patients believed that cancer is curable, whereas 55% reported that cure depends on the stage of disease, in comparison to a study by Kumar et al. which reported 89.6% which was very high.[17]
Diagnosis of cancer invokes a feeling of uncertainty and fear in the minds of cancer patients, in the present study 80% of patients had a lot of worries about cancer and believed that they will develop complications of cancer even after treatment and will eventually die because of it. In the study by Gamage and Jayawardana[16] almost all patients reported a feeling of hopelessness and even the name of the word cancer caused anxiety and fear. Also Toon E[18] mentioned that only half of their study population desired to converse about their disease. Cancer leads to discouragement and fear in the minds of patients that they do not express their issues and also this might be a major factor for delayed presentation. Sharma et al.[19] mentioned in their study that >70% were not able to assess symptoms followed by fear and denial in 15.6% that they might be suffering from the dreadful disease. Therefore, fear, frightful attitude, lack of awareness of signs of cancer, and social stigma lead to negative attitude and belief toward cancer. Patients residing in urban areas and literacy levels had a positive impact on their knowledge toward cancer in the present study and it was similar to the study by Badihian et al.[20] and Kumar et al.[17] who showed that educational status influenced their dealing with diagnosis, management decision for cancer.
Also in the present study, males had a more positive attitude toward cancer than females, but it was in contrast to the study by Kumar et al.[17] Regarding the role of screening in early detection and diagnosis of cancer, in the present study, 67.7% of patients knew about screening which was in contrast to the study by Oswal et al. in which only 34% of patients knew about cancer screening.[21]
The present study revealed that 86% of the cancer patients had poor belief regarding cancer. As per the researchers there is paucity of studies on belief of cancer patients related to their diagnosis. Hence, the present study is imperative regarding the assessment of patient's knowledge for cancer warning signs, beliefs, and attitudes toward cancer because lack of information may further lead to delayed symptom appraisal and advanced stage presentation of any cancer, which indirectly will have an effect on cure rates.
Limitation and recommendation
The study's main limitations include its small sample size and high exclusion rate, both of which potentially lead to selection bias. Patients who did not volunteer to participate were not tracked, and it is possible that we only included the most motivated and well-informed patients. Nonetheless, the number of patients enrolled is higher than in previous cancer researches.
Conclusions
Given the rising incidence of cancer, a health awareness campaign needs to be adapted according to the issues of cancer patients. They need to be made more aware of the red flag signs of cancer and improvise their attitude toward cancer. Cancer care programs should not only involve cancer patients but also involve their caregivers because the understanding of family members is of utmost importance to fight this disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Authors acknowledge the efforts of Dr Bela Goyal, Dr Amit Sehrawat and Dr Deepak Sundriyal for validation of questionnare.
References
- 1.Nagai H, Kim YH. Cancer prevention from the perspective of global cancer burden patterns. J Thorac Dis. 2017;9:448–51. doi: 10.21037/jtd.2017.02.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3. [Last accessed on 25 September 2020]. Available from:https://www.cancer.gov/about-cancer/understanding/statistics .
- 4.Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941–53. doi: 10.1002/ijc.31937. [DOI] [PubMed] [Google Scholar]
- 5.Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86:304–14. doi: 10.4065/mcp.2010.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kahissay MH, Fenta TG, Boon H. Beliefs and perception of ill-health causation: A socio-cultural qualitative study in rural North-Eastern Ethiopia. BMC Public Health. 2017;17:124. doi: 10.1186/s12889-017-4052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samoil D, Kim J, Fox C, Papadakos JK. The importance of health literacy on clinical cancer outcomes: a scoping review. Ann Cancer Epidemiol. 2021;5:3. [Google Scholar]
- 8.Ouasmani F, Hanchi Z, Haddou Rahou B, Bekkali R, Ahid S, Mesfioui A. Determinants of patient delay in seeking diagnosis and treatment among moroccan women with cervical cancer. Obstet Gynecol Int. 2016;2016:4840762. doi: 10.1155/2016/4840762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. 2013;103:777–80. doi: 10.2105/AJPH.2012.301056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krzyszczyk P, Acevedo A, Davidoff EJ, Timmins LM, Marrero-Berrios I, Patel M, et al. The growing role of precision and personalized medicine for cancer treatment. Technology (Singap World Sci) 2018;6:79–100. doi: 10.1142/S2339547818300020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berger O, Grønberg BH, Loge JH, Kaasa S, Sand K. Cancer patients’ knowledge about their disease and treatment before, during and after treatment: A prospective, longitudinal study. BMC Cancer. 2018;18:381. doi: 10.1186/s12885-018-4164-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh Mahendra MR, Saini GL, Dewesh K, Shikha M. Knowledge, attitude and practices towards cancer among urban dwellers of Jodhpur, Rajasthan. Int J Res Health Sci. 2014;2:254–62. [Google Scholar]
- 13.Lynes K, Kazmi SA, Robery JD, Wong S, Gilbert D, Thaha MA. Public appreciation of lifestyle risk factors for colorectal cancer and awareness of bowel cancer screening: A cross-sectional study. Int J Surg. 2016;36:312–8. doi: 10.1016/j.ijsu.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Richards R, McNoe B, Iosua E, Reeder AI, Egan R, Marsh L, et al. Knowledge of evidence-based cancer risk factors remains low among New Zealand adults: Findings from two cross-sectional studies, 2001 and 2015. Asian Pac J Cancer Prev. 2017;18:2931–6. doi: 10.22034/APJCP.2017.18.11.2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aweke YH, Ayanto SY, Ersado TL. Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: Community-based cross-sectional study. PLoS One. 2017;12:e0181415. doi: 10.1371/journal.pone.0181415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gamage AU, Jayawardana PL. Knowledge of non-communicable diseases and practices related to healthy lifestyles among adolescents, in state schools of a selected educational division in Sri Lanka. BMC Public Health. 2017;18:64. doi: 10.1186/s12889-017-4622-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar S, Shaikh AJ, Khalid S, Masood N. Influence of patient's perceptions, beliefs and knowledge about cancer on treatment decision making in Pakistan. Asian Pac J Cancer Prev. 2010;11:251–5. [PubMed] [Google Scholar]
- 18.Toon E. “Cancer as the general population knows it”: Knowledge, fear, and lay education in 1950s Britain. Bull Hist Med. 2007;81:116–38. doi: 10.1353/bhm.2007.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma G, Gupta S, Gupta A, Kalyani VC, Rohilla KK, Sreejeev AT, et al. Identification of factors influencing delayed presentation of cancer patients. Int J Community Med Public Health. 2020;7:1705–10. [Google Scholar]
- 20.Badihian S, Choi EK, Kim IR, Parnia A, Manouchehri N, Badihian N, et al. Attitudes toward cancer and cancer patients in an Urban Iranian population. Oncologist. 2017;22:944–50. doi: 10.1634/theoncologist.2017-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oswal K, Kanodia R, Pradhan A, Nadkar U, Avhad M, Venkataramanan R, et al. Assessment of knowledge and screening in oral, breast, and cervical cancer in the population of the northeast region of India. JCO Glob Oncol. 2020;6:601–9. doi: 10.1200/JGO.19.00257. [DOI] [PMC free article] [PubMed] [Google Scholar]


