Abstract
Smartphone applications are increasingly being used to measure gait due to their portability and cost-effectiveness. Important reliability metrics are not available for most of these devices. The purpose of this article was to evaluate the test-retest reliability and concurrent validity of spatiotemporal gait using the novel Gait Analyzer smartphone application compared to the Tekscan Strideway. Healthy participants (n=23) completed 12 trials of 10-meter walking, at two separate time points, using Gait Analyzer and while walking across the Tekscan Strideway. The results suggest excellent test-retest reliability for the Gait Analyzer and good test-retest reliability for the Tekscan Strideway for both velocity and cadence. At both time points, these devices were moderately to strongly correlated to one another for both velocity and cadence. These data suggest that the Gait Analyzer and Tekscan Strideway are reliable over time and can comparably calculate velocity and cadence.
Introduction
Health care providers and researchers are progressively using smartphone applications for remote assessment due to their cost effectiveness, portability, and ability to reduce potential barriers for patients’ involvement in research.1,2 These advancements in technology allow for monitoring of various health outcomes in austere and non-laboratory settings. In the realm of biomechanics, gait applications have been actively used since early 2011 to track diseases/injuries3,4,5,6,7,8, functionality in older adults9,10, and to track physical activity (i.e. running).11,12 While the gold standard for gait assessments continues to be motion capture and pressure mat technology1, wearable sensors and smartphone applications continue to advance in order to reduce the time and resources required for gait assessments.14,15
Pressure mat systems similar to the Gaitrite or Tekscan® Strideway continue to demonstrate excellent ability to quantify spatiotemporal gait.13,14 These systems vary from full length mats13, linked configurable tile systems16 and in-soles.17 They are generally considered extremely reliable on repeat administration18 and have been used in numerous assessments of pathological gait.3,4,5,6 While they provide advantages over motion capture, these systems are generally limited to the half-life of the particular sensors (i.e. the more it is used, the less sensitive and accurate it becomes), the available sensing area, additional equipment requirements, and trained personnel to use the technology. Thus, wearable sensors and smartphone applications are attempting to provide truly cost effective and portable methods of gait assessment.
Wearable sensors vary in price based on the capabilities of each system and can range from $300 to >$20,000 in price. While the price of the wearable system has a wide range, the ease of use does as well. Systems can range from having a participant place a phone system in a pocket or pouch, to having multiple placements of sensors on differing parts of the body 19,20,21. For simple at-home measurements of gait, smartphone applications continue to dominate the market given the ability to directly download the application on the individual participants’ smartphone. Modern smartphones with appropriate accelerometers are used by nearly 45% of the world’s population23 and can be carried in numerous positions on the body to accurately track gait.24,21 One particular smartphone application, Gait Analyzer25 created by Control One LLC, has been used with moderate success to analyze gait of pathological and older adult populations.6,26,25,10 This application has high intrarater and interrater reliability24 and sufficient validity when compared to motion capture.24 However, it is lacking any test-retest reliability statistics to support its use over time. It is critical to understand the reliability of accelerometer-based smartphone applications as they have been suggested for use as a viable at-home measurement tool to track longitudinal decline of Facioscapulohumeral muscular dystrophy and other pathologies.3 In addition, to the authors’ best knowledge, no known data exists comparing the Gait Analyzer to gait mat systems. In some clinical scenarios these measurement tools have become more common compared to the gold standard, motion capture and other gait walkways, which can be expensive and requires more personnel to run. Thus, understanding how smartphone applications may relate to gait mat systems is important to continue to build confidence in these devices for clinicians and researchers.
The purpose of this article is to evaluate the test-retest reliability and concurrent validity of spatiotemporal gait using the novel Gait Analyzer smartphone application compared to the Tekscan Strideway. It is hypothesized that both devices will demonstrate acceptable test-retest reliability and concurrent validity for both gait velocity and cadence in a non-pathological population. It is the aim of this research to provide basic evidence that the Gait Analyzer can be used to assess spatiotemporal gait over time. In the future, the gait analysis tracking ability can be used for possible upcoming clinical trials that are relying on gait performance as a marker for disease progression.
Methods
Participants
Twenty-three healthy recreationally active (30 minutes of exercise a day for at least 3 days a week) collegiate students participated in this study (13 female; avg. age = 21±2 years, avg. weight = 90.01±15.5 kg, avg. leg length = 98.4±3.2 cm). All participants completed a brief questionnaire that requested age, sex, and medical history. Participants were excluded if they reported a concussion diagnosis, neurological disorders, any lower extremity disorders that may influence gait, along with any existing lower extremity injury within the past six months. All participants provided written informed consent to the study procedure, which was approved by the University’s Institutional Review Board, prior to enrollment into the study.
Procedures
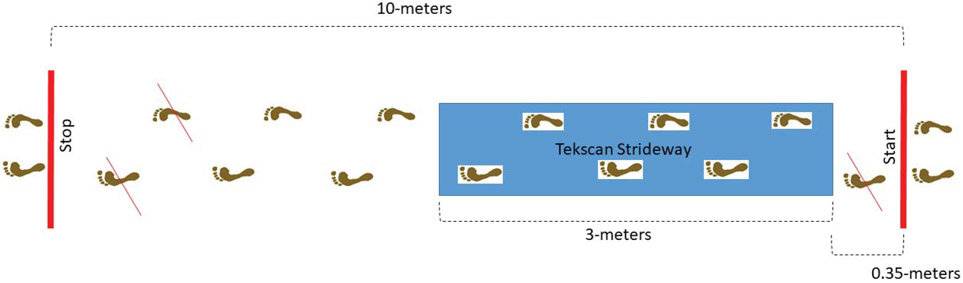
Participants reported at two separate time points, one week apart (average time 7 days). Participants body weight (kg) and leg length (cm) (greater trochanter to medial malleoli) were measured and used for appropriate calibration of the Tekscan Strideway (30Hz, Boston, MA). The Tekscan Strideway is comprised of a series of linked tiles (5 tiles; 0.65 x 3.0 meter sensing area, with a spatial accuracy of 0.968 sensels/cm2) (see Figure 1) that were used to assess gait kinematics across vertical, anteroposterior (AP) and mediolateral directions. Each Tekscan Strideway tile was calibrated to the participant’s weight using single leg vertical ground reaction force. Once the Tekscan Strideway was calibrated, an LGK40 phone with the application “Gait Analyzer” was placed into a running belt (Rino Valley Running Belt Waist Pack) secured directly onto the participants’ lumbar spine (closest to L5). Participants were then instructed to walk in a 10-meter, straight line for a total of 12 (down and back, six times) trials with a three second pause at the end of each 10-meter walk for the phone to record one “bout”. For three of the 10 meters, the Tekscan Strideway continuously collected gait information on a step-by-step basis.
Figure 1:
Walking diagram for data collection, participants walked 10-meters in total for 12 consecutive trials using the Gait Analyzer application and directly through the Tekscan Strideway. Once the person reached the stop area, they waited 10 seconds, then turned around and walked back to the start position. During the analysis the first step from the start position and last two steps were removed to reduce gait initiation and termination. The same steps were removed consistently regardless of walking direction (right to left or left to right).
Data Analysis
The “Gait Analyzer” application provided real-time gait spatiotemporal computations, with results saved to a tab-delimited file on the phone following completion of each walking trial. Online calculations of step time, step length, gait velocity, and cadence, were computed as previously described.24 Specifically, tri-axial accelerations, which were collected at the smartphone’s maximum sampling frequency (Android: SENSOR_DELAY_FASTEST; 95-105 Hz range), were resampled to 100 Hz, to ensure a constant sampling rate. The tri-axial acceleration data were filtered using a 4th order low-pass Butterworth filter with a 20Hz cutoff frequency, and anteroposterior (AP) accelerations further filtered using a 4th order low-pass Butterworth filter with a 20Hz cutoff frequency. Heel strikes were identified based on positive peaks in the AP direction, with step time (ST) calculated as the time difference between these steps. The step length (SL) was computed as
| (Eq 1) |
where h is the change in vertical position and l is the participant’s leg length. The change in vertical position was calculated by double integrating the vertical acceleration, and subsequently filtering the result using a 4th order high-pass Butterworth filter with a 0.1 Hz cutoff frequency to remove integration drift across each step cycle. Step velocity (SV) across each step I was computed as
| (Eq 2) |
with gait reported as the average step velocity across all steps. Cadence was computed as the quotient of the number of steps and the total trial time, in units of steps/min.
Gait velocity and cadence were calculated automatically by the Tekscan Strideway using each consecutive footfall. Gait velocity were computed based on the total gait distance travelled divided by the total trial time. Cadence was calculated as the total number of steps taken per minute based on the overall footfall. The Tekscan Strideway was not synced to the gait app which required manual evaluation and independent evaluation of each dataset. In order to limit any gait initiation and termination, the first and last two steps of each trial were manually removed from both devices to obtain steady state gait (see Figure 1). All 12 trials were ensemble averaged and further analyzed.
Statistical Analysis
All dependent variables (gait velocity and cadence) were examined for normalcy and to determine if influence skewness exists. None of the variables for both devices were non-parametric. Thus, intra-class correlation coefficients (ICC) were used to assess the test-retest reliability of the phone application and Tekscan Strideway between both time points for gait velocity and cadence. Using intraclass correlation coefficient, retest reliability was determined as ICC ≥ 0.9 = excellent, 0.9 > ICC ≥ 0.75 = good, 0.75 > ICC ≥ 0.5 = moderate, ICC ≥ 0.5 = poor, 0.5 > ICC = unacceptable.29 Pearson’s product correlation coefficients were used to determine the concurrent validity between gait velocity and cadence calculated by each device (phone and Tekscan Strideway) with > 0.10 = negligible, 0.10-0.39 = weak, 0.40-0.69 = moderate, 0.70-0.89 = strong, 0.90-1.0 = very strong.30 All statistical analysis were run in Statistical Package for the Social Sciences (SPSS IBM, Armonk, NY 2020, Version 27).
Results
At both testing time points, the Tekscan Strideway calculated a higher velocity and cadence when compared to the phone (see Table 1 and 2).
Table 1.
Mean, standard deviation and intra-class correlation coefficient for velocity using the phone application and the Tekscan Strideway at each time point.
| Velocity (meters/ second) | ICC (95% CI) | |
|---|---|---|
| T1 Phone | 1.12 ± 0.25 | |
| T2 Phone | 1.12 ± 0.13 | 0.77 (0.47 to 0.91) |
| T1 Tekscan Strideway | 1.27 ± 0.20 | |
| T2 Tekscan Strideway | 1.31 ± 0.17 | 0.90 (0.74 to 0.95) |
Note: T1=time point 1, T2=time point 2, ICC = intra-class correlation coefficient, CI = confidence interval
Table 2.
Mean, standard deviation with intra-class correlation coefficient for cadence using the phone application and the Tekscan Strideway at each time point.
| Cadence (steps/ minute) | ICC (95% CI) | |
|---|---|---|
| T1 Phone | 105.93 ± 6.68 | |
| T2 Phone | 107.83 ± 7.68 | 0.94 (0.74 to 0.97) |
| T1 Tekscan Strideway | 109.30 ± 5.99 | |
| T2 Tekscan Strideway | 111.21 ± 7.55 | 0.87 (0.68 to 0.94) |
Note: T1=time point 1, T2=time point 2, ICC = intra-class correlation coefficient, CI = confidence interval
Gait Velocity and Cadence Test-retest Reliability
The results of the ICC observed a good test-retest reliability (ICC = 0.77; 95% CI = 0.47 to 0.91) for Gait Analyzer velocity (see Figure 2a) and an excellent test retest reliability (ICC = 0.90; 95% CI = 0.74 to 0.95) for Tekscan Strideway velocity (see Figure 2b) between Time 1 and Time 2 (see Table 1). These data suggest that gait velocity for both the Gait Analyzer and the Tekscan Strideway are between good and excellent (as previously defined) across two time points separated by 7-days.
Figure 2:
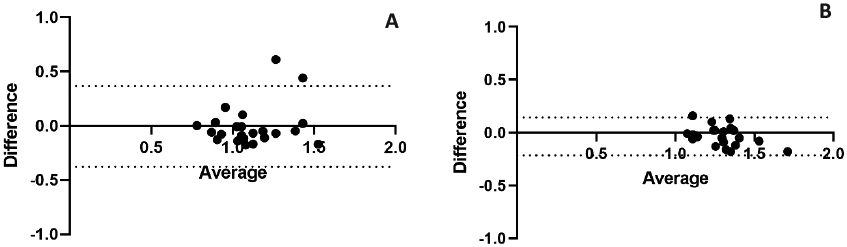
Bland Altman plots displaying the mean difference from time 1 to time 2 for A) Gait Analyzer and B) Tekscan Strideway gait velocity.
The results of the ICC observed an excellent test retest reliability (ICC = 0.94; 95% CI = 0.74 to 0.97) for the Gait Analyzer cadence (see Figure 3a) and a good test retest reliability (ICC= 0.87; CI= 0.68 to 0.94) for the Tekscan Strideway cadence (see Figure 3b) between T1 and T2 (see Table 2). These data suggest that gait cadence for both the Gait Analyzer and the Tekscan Strideway are good to excellent across two time points separated by 7-days.
Figure 3:
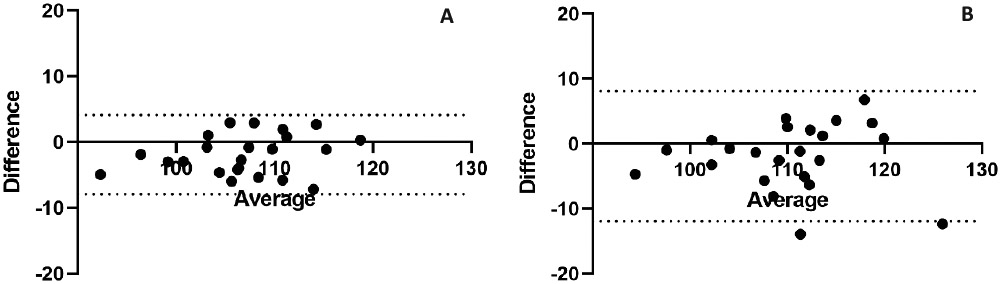
Bland Altman plots displaying the mean difference from time 1 to time 2 for A) Gait Analyzer and B) Tekscan Strideway gait cadence.
Gait Velocity and Cadence Concurrent Validity
The results of the Pearson’s r observed a positive moderate correlation between the phone application and Tekscan Strideway when comparing gait velocity (r = 0.59; r2 = .35; p = 0.003) at T1 and a positive strong correlation between the Gait Analyzer and Tekscan Strideway when comparing gait velocity (r = 0.74; r2 = 0.55; p < 0.001) at T2. The results of the Pearson’s r observed a very strong positive correlation between the Gait Analyzer and Tekscan Strideway when comparing gait cadence (r = 0.90; r2 = 0.80; p < 0.001) at T2 and a positive moderate correlation between the Gait Analyzer and Tekscan Strideway when comparing gait cadence (r = 0.57; r2 = 0.3; p = .005) at T2. These result suggest the Gait Analyzer and Tekscan Strideway gait velocity and cadence calculations are moderately to very strongly correlated at both time points.
Discussion
The purpose of this article was to assess the test-retest reliability and concurrent validity of a novel smartphone application measuring velocity and cadence of gait when compared to a commonly used pressure mat system. The results suggest the Gait Analyzer smartphone application provides a good reliability while the Tekscan Strideway has acceptable to good reliability for both velocity and cadence, respectively. Across the two time points, the devices were related for both velocity and cadence, however, this relationship varied from moderate to strong. The major implication of the study is that users of either device, Gait Analyzer or Tekscan Strideway, can feel relatively confident that gait velocity and cadence will be reliably and accurately measured. These data are important as smartphone applications are becoming more common to assess gait remotely in order to reduce the travel time and cost of attending in-person assessments.
The gait velocity measured by the Gait Analyzer were lower than normal ranges (≈1.2 m/s)32, yet similar to other research using accelerometers (≈1.1 m/s)9. The major differences in the calculated gait velocity compared to other normative data, could be the lack of a calibration trial to determine the most appropriate step length values for each participant. This could cause a possible increase and/or decrease in overall velocity by artificially decreasing the total distance traveled. Secondly, the data collection included a single step of gait initiation (see Figure 1). Any non-steady state gait data will reduce the overall average velocity for the trial.32,34 The Tekscan Strideway gait velocity was comparable to prior research31,34, was faster than the Gait Analyzer and slightly increased between time points. The increase could be due to a simple learning effect; however, this was not reflected in the Gait Analyzer. The difference between the two devices could be explained by the disparity in measurement distance available for calculating spatiotemporal gait. The Tekscan Strideway had a total of 3-meters of active sensing and the velocity is calculated by the total gait distance travelled divided by the total trial time, rather than using SL or ST. An additional reason for the disparity between devices may also be due to the difference in algorithms that are being used in each device to calculate the measurements that are being studied.
Cadence, the number of steps taken in a one-minute period, has an average of 100 steps/minute in healthy individuals between 21 and 40 years of age.35 Both devices were above 100 steps/minute and slightly increased (≈2 steps/minute) from T1 to T2. This can be attributed to a general increase in how many steps were accomplished per trial at each session. In addition, both devices were slightly lower than prior research using accelerometers36 while the Tekscan Strideway had a higher cadence when compared to the Gait Analyzer (≈Δ4 steps/minute). This could again be due to the total amount of distance available for calculating spatiotemporal gait by device. Both devices were reliable for measuring cadence over time and were related to one another.
Limitations
The overall population sample size and age of the participants limits the ability to generalize to a broader population. Future research should replicate these results in older adult and pathological gait populations to ensure the data remains valid and reliable when impairments are introduced to the study. This increase of signal noise will test the reliability of this study as well as create a more in-depth understanding of the population where gait impairments are the most common. The second limitation is the possible learning effect that occurred between T1 and T2. When participants returned for the second time, they may have recalled how to perform the tasks which included where to turn in the laboratory and the amount of time pausing before turning around to complete the task in the opposite direction. This recall can lead to an increase in comfort and overall increase in walking speed or pace in which the trial was complete. The average of the cadence and velocity is directly correlated to the number of steps and the speed at which those steps were taken, this can cause different outcomes at time point one and two because of the change in average speed after steps are removed (see Figure 1). The change in speed may also be due to a learning effect in which the participants became more comfortable in the lab leading to a faster completion of the task, and increase speed of steps taken. Third, due to size constraints of the laboratory, the participants started 0.35-meters away from the Tekscan Strideway. This led to a single footfall of gait initiation being included in the overall analysis which may have altered the overall velocity and cadence calculations. Lastly, the lack of a calibration for the Gait Analyzer application may have reduced the overall capabilities of the device. Future development on this application should include a calibration trial.
Conclusion
This study indicates that the novel smartphone application, Gait Analyzer, and the Tekscan Strideway are reliable over time for the measurement of gait velocity and cadence. Furthermore, both devices were related to one another and are somewhat comparable to normative data. Users can feel relatively comfortable that either device will reliably measure gait velocity and cadence over time along with being related to one another. These data are important as smartphone applications are becoming more common to assess gait remotely in order to reduce the travel time and cost of attending in-person assessments. Future research should address the limitations of this study alongside assessing the Gait Analyzer in clinical populations.
Highlights:
Data suggest that the Gait Analyzer and Tekscan Strideway are reliable over time and can comparably calculate velocity and cadence
At time point one and time point two, the devices were moderately to strongly correlated to one another for both velocity and cadence
The novel smartphone application may be used to collect reliable gait data for those in the future possibly in at-home locations
Acknowledgements
The authors would like to thank the Neuromechanics Lab staff for their continued efforts on this project. The research team would like to thank our volunteers for participating in this study. We would like to thank Madison Taylor and Vincentia Owusu-Amankonah for their help with data collection and processing. This study was funded by P20GM103650.
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
CReDIT Author Statement
Conceptualization – Marie Kelly, Nicholas Murray
Methodology – Marie Kelly, Ryan Wuebbles, Nicholas Murray
Software – Vipul Lugade
Validation – Daniel Cipriani
Formal analysis – Daniel Cipriani, Marie Kelly
Investigation – Marie Kelly, Nicholas Murray
Resources – Nicholas Murray, Peter Jones
Data Curation – Marie Kelly
Writing – Original Draft – Marie Kelly, Peter Jones, Ryan Wuebbles, Vipul Lugade, Daniel Cipriani, Nicholas Murray
Writing – Review and Editing – Marie Kelly, Nicholas Murray
Supervision – Nicholas Murray
Project Administration – Marie Kelly
Funding Acquisition – Nicholas Murray, Peter Jones, Ryan Wuebbles
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Vella MA, Li H, Reilly PM, Raza SS. Unlocked yet untapped: The ubiquitous smartphone and utilization of emergency medical identification technology in the care of the injured patient. Surg Open Sci. 2020;2(3):122–126. Published 2020 Apr 12. doi: 10.1016/j.sopen.2020.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiechmann W, Kwan D, Bokarius A, Toohey SL. There's an App for That? Highlighting the Difficulty in Finding Clinically Relevant Smartphone Applications. West J Emerg Med. 2016;17(2):191–194. doi: 10.5811/westjem.2015.12.28781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abou L, Peters J, Wong E, Akers R, Dossou MS, Sosnoff JJ, Rice LA. Gait and Balance Assessments using Smartphone Applications in Parkinson's Disease: A Systematic Review. J Med Syst. 2021. Aug;45(9) 87. doi: 10.1007/s10916-021-01760-5. PMID: 34392429; PMCID: PMC8364438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Omberg L, Chaibub Neto E, Perumal TM, et al. Remote smartphone monitoring of Parkinson's disease and individual response to therapy. Nature Biotechnology. 2021. Aug. DOI: 10.1038/s41587-021-00974-9. PMID: 34373643. [DOI] [PubMed] [Google Scholar]
- 5.Fréchette Guillaume R., Lizzeri Alessandro, and Salz Tobias. 2019. "Frictions in a Competitive, Regulated Market: Evidence from Taxis." American Economic Review, 109 (8): 2954–92.DOI: 10.1257/aer.20161720 [DOI] [Google Scholar]
- 6.Howell DR, Seehusen CN, Wingerson MJ, Wilson JC, Lynall RC, Lugade V. Reliability and Minimal Detectable Change for a Smartphone-Based Motor-Cognitive Assessment: Implications for Concussion Management. J Appl Biomech. 2021. Jul 13; 1–8. PMID: 34257159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marziyeh Ghoreshi Beyrami S, Ghaderyan P. A robust, cost-effective and non-invasive computer-aided method for diagnosis three types of neurodegenerative diseases with gait signal analysis. Measurement. 2020;156:107579.doi: 10.1016/j.measurement.2020.107579 [DOI] [Google Scholar]
- 8.Ghaderyan P, Fathi G. Inter-limb time-varying singular value: A new gait feature for parkinson’s disease detection and stage classification. Measurement. 2021;177:109249. doi: 10.1016/j.measurement.2021.109249 [DOI] [Google Scholar]
- 9.Lugade V, Kuntapun J, Prupetkaew P, Boripuntakul S, Verner E, Silsupadol P. Three-Day Remote Monitoring of Gait Among Young and Older Adults Using Participants' Personal Smartphones [published online ahead of print, 2021 Aug 4]. J Aging Phys Act. 2021;1–8. doi: 10.1123/japa.2020-0353 [DOI] [PubMed] [Google Scholar]
- 10.Prupetkaew P, Lugade V, Kamnardsiri T, Silsupadol P. Cognitive and visual demands, but not gross motor demand, of concurrent smartphone use affect laboratory and free-living gait among young and older adults. Gait Posture. 2019;68:30–36. doi: 10.1016/j.gaitpost.2018.11.003 [DOI] [PubMed] [Google Scholar]
- 11.Benson LC, Clermont CA, Bošnjak E, Ferber R. The use of wearable devices for walking and running gait analysis outside of the lab: A systematic review. Gait Posture. 2018;63:124–138. doi: 10.1016/j.gaitpost.2018.04.047 [DOI] [PubMed] [Google Scholar]
- 12.Eades MT, Tsanas A, Juraschek SP, Kramer DB, Gervino E, Mukamal KJ. Smartphone-recorded physical activity for estimating cardiorespiratory fitness. Sci Rep. 2021;11(1):14851. Published 2021 Jul 21. doi: 10.1038/s41598-021-94164-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanko RM, Laende EK, Strutzenberger G, et al. Assessment of spatiotemporal gait parameters using a deep learning algorithm-based markerless motion capture system. J Biomech. 2021;122:110414. doi: 10.1016/j.jbiomech.2021.110414 [DOI] [PubMed] [Google Scholar]
- 14.Roggio F, Ravalli S, Maugeri G, et al. Technological advancements in the analysis of human motion and posture management through digital devices. World J Orthop. 2021;12(7):467–484. Published 2021 Jul 18. doi: 10.5312/wjo.v12.i7.467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng N, Barrentine SW. Biomechanics and motion analysis applied to sports. Phys Med Rehabil Clin N Am. 2000;11(2):309–322. [PubMed] [Google Scholar]
- 16.Murray NG, Moran R, Islas A, et al. Sport-related concussion adopt a more conservative approach to straight path walking and turning during tandem gait. Journal of Clinical and Translational Research. 2021. doi: 10.18053/jctres.07.202104.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hegde N, Zhang T, Uswatte G, et al. The Pediatric SmartShoe: Wearable Sensor System for Ambulatory Monitoring of Physical Activity and Gait. IEEE Trans Neural Syst Rehabil Eng. 2018;26(2):477–486. doi: 10.1109/TNSRE.2017.2786269 [DOI] [PubMed] [Google Scholar]
- 18.Donisi L, Pagano G, Cesarelli G, Coccia A, Amitrano F, D'Addio G. Benchmarking between two wearable inertial systems for gait analysis based on a different sensor placement using several statistical approaches. Measurement. 2021;173:108642. doi: 10.1016/j.measurement.2020.108642 [DOI] [Google Scholar]
- 19.Liu T, Inoue Y, Shibata K. Development of a wearable sensor system for quantitative gait analysis. Measurement. 2009;42(7):978–988. doi: 10.1016/j.measurement.2009.02.002 [DOI] [Google Scholar]
- 20.Palermo E, Rossi S, Marini F, Patanè F, Cappa P. Experimental evaluation of accuracy and repeatability of a novel body-to-sensor calibration procedure for inertial sensor-based gait analysis. Measurement. 2014;52:145–155. doi: 10.1016/j.measurement.2014.03.004 [DOI] [Google Scholar]
- 21.Zhang Z, Xie L. Adaptive body movement system for wearable IOT instruments based on matrix vector parameter estimation. Measurement. 2021;169:108350. doi: 10.1016/j.measurement.2020.108350 [DOI] [Google Scholar]
- 22.Wong JS, Jasani H, Poon V, Inness EL, McIlroy WE, Mansfield A. Inter- and intra-rater reliability of the GAITRite system among individuals with sub-acute stroke. Gait Posture. 2014;40(1):259–261. doi: 10.1016/j.gaitpost.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 23.O'Dea S. Number of smartphone users from 2016 to 2021. Statista. https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Published June 1, 2021. [Google Scholar]
- 24.Silsupadol P, Teja K, Lugade V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: Body, bag, belt, hand, and pocket. Gait Posture. 2017;58:516–522. doi: 10.1016/j.gaitpost.2017.09.030 [DOI] [PubMed] [Google Scholar]
- 25.Lugade V, Fortune E, Morrow M, Kaufman K (2014). Validity of using tri-axial accelerometers to measure human movement-part I: posture and movement detection. Med. Eng. Phys 36, 169–176. 10.1016/j.medengphy.2013.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly M, Taylor MR, Pavilionis P, et al. Analysis of mobile smartphone application for the assessment Of Facioscapulohumeral muscular Dystrophy (fshd) gait. Medicine & Science in Sports & Exercise. 2021;53(8S):137–137. doi: 10.1249/01.mss.0000760728.64290.b2 [DOI] [Google Scholar]
- 27.Silsupadol P, Prupetkaew P, Kamnardsiri T, Lugade V. Smartphone-Based Assessment of Gait During Straight Walking, Turning, and Walking Speed Modulation in Laboratory and Free-Living Environments. IEEE J Biomed Health Inform. 2020;24(4):1188–1195. doi: 10.1109/JBHI.2019.2930091 [DOI] [PubMed] [Google Scholar]
- 28.Silsupadol P, Teja K, Lugade V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: Body, bag, belt, hand, and pocket. Gait Posture. 2017;58:516–522. doi: 10.1016/j.gaitpost.2017.09.030 [DOI] [PubMed] [Google Scholar]
- 29.Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research [published correction appears in J Chiropr Med. 2017 Dec;16(4):346]. J Chiropr Med. 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schober P, Boer C, Schwarte LA. Correlation Coefficients: Appropriate Use and Interpretation. Anesth Analg. 2018;126(5):1763–1768. doi: 10.1213/ANE.0000000000002864 [DOI] [PubMed] [Google Scholar]
- 31.Oberg T, Karsznia A, Oberg K. Basic gait parameters: reference data for normal subjects, 10-79 years of age. J Rehabil Res Dev. 1993;30(2):210–223. [PubMed] [Google Scholar]
- 32.Gélat T, Pellec AL, Brenière Y. Evidence for a common process in gait initiation and stepping on to a new level to reach gait velocity. Exp Brain Res. 2006;170(3):336–344. doi: 10.1007/s00221-005-0214-8 [DOI] [PubMed] [Google Scholar]
- 33.Van Deventer KA, Seehusen CN, Walker GA, Wilson JC, Howell DR. The diagnostic and prognostic utility of the dual-task tandem gait test for pediatric concussion. J Sport Health Sci. 2021;10(2):131–137. doi: 10.1016/j.jshs.2020.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Godfrey A, Del Din S, Barry G, Mathers JC, Rochester L. Instrumenting gait with an accelerometer: a system and algorithm examination. Med Eng Phys. 2015;37(4):400–407. doi: 10.1016/j.medengphy.2015.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tudor-Locke C, Ducharme SW, Aguiar EJ, et al. Walking cadence (steps/min) and intensity in 41 to 60-year-old adults: the CADENCE-adults study. Int J Behav Nutr Phys Act. 2020;17(1):137. Published 2020 Nov 10. doi: 10.1186/s12966-020-01045-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Silsupadol P, Prupetkaew P, Kamnardsiri T, Lugade V. Smartphone-Based Assessment of Gait During Straight Walking, Turning, and Walking Speed Modulation in Laboratory and Free-Living Environments. IEEE J Biomed Health Inform. 2020;24(4):1188–1195. doi: 10.1109/JBHI.2019.2930091 [DOI] [PubMed] [Google Scholar]