Abstract
Objective: We aimed to evaluate the perspective of the Turkish Thoracic Society (TTS) members regarding institutional preparedness, in terms of administrative measures and availability of personal protective equipment (PPE), in the first and third months of the coronavirus disease 2019 (COVID-19) pandemic in Turkey.
Material and Methods: A 22-item online survey was e-mailed between the first and third months to TTS members, and participants’ responses were evaluated.
Results: The number of participants was 295 in the first survey and 141 in the second. In the second survey, the percentage of answers implying availability increased in all 18 control measures, 16 of which were statistically significant. However, there were still less than half of the respondents who reported the availability of psychological and behavioral support and some PPE, including respirators, facial protectors, goggles, and gowns. Statistical significance was observed for provision of a waiting area (P = .008), rooms for aerosol-generating procedures (P = .042), and special wards for patients with suspected or definite COVID-19 (P < .001); testing healthcare workers (HCWs) with a history of contact with a COVID-19 case (P < .001); and surveillance of symptomatic HCWs (P = .048), between tertiary vs. primary and secondary healthcare facilities in the first survey, but provision of special wards (P = .002) and supply for aprons (P = .027) in the second survey.
Conclusion: Our results showed an improvement in control measures in the third month of the pandemic. However, the persistent low availability of psychological and behavioral support and several items of PPE pointed out the need for action. Considering the health and safety of HCWs, the control measures should be actively monitored and deficiencies eliminated.
Keywords: COVID-19, occupational safety and health, healthcare workers’ health, personal protective equipment
MAIN POINTS
An improvement in control measures was demonstrated in the third month of the pandemic. However, persistently low availability of psychological and behavioral support and some PPE pointed out the need for action.
The significant difference in the level of control measures between tertiary vs. primary and secondary healthcare facilities in the first month was mostly diminished in the third month.
For the health and safety of healthcare workers, the level of control measures should be actively monitored and deficiencies eliminated.
Introduction
The coronavirus disease 2019 (COVID-19) emerged at the end of 2019, spread worldwide, and was declared as a pandemic by the World Health Organization on March 11, 2020.1 COVID-19 is mainly transmitted via respiratory droplets; aerosols generated during coughing, sneezing, laughing, or speaking aloud are other possible sources. Depending on its severity, the disease might involve the lungs and lead to pneumonia, respiratory failure, acute respiratory distress syndrome, and mortality.2
Since the initial phases of the pandemic, the healthcare workers (HCWs) have been a part of the frontline.3 The growing number of HCWs who contracted COVID-19 and lost their lives has also been documented by the research, which has pointed out the increased risk for HCWs compared to the general population.4 That risks have been evaluated according to principles of occupational safety and health, including measures to control them, and both national and global guidelines have been published.5-9
Despite rapidly developed guideline recommendations, control measures have failed to varying degrees in most countries, particularly at the initial phase.10 The domain of chest diseases being one of the essential medical specialties during the pandemic due to the above mentioned characteristics of the disease, HCWs practicing in this field have also encountered that failure globally, including in Turkey, where the first COVID-19 case was diagnosed on March 11, 2020.11 In this study, we aimed to evaluate the perspective of members of the Turkish Thoracic Society (TTS), one of the foremost societies for HCWs working in the field of chest diseases in Turkey, regarding institutional preparedness in terms of administrative measures and availability of personal protective equipment (PPE), in the first and third months of the pandemic.
MATERIAL AND METHODS
Survey
A 22-item survey was prepared. There were 4 items covering age, sex, specialty, and type of healthcare facility. The remaining 18 multiple choice items were based on the “Guidance on Preparing Workplaces for COVID-19” published by the United States of America Department of Labor Occupational Safety and Health Administration (OSHA).9 Of those, 9 questions relating to the administrative measures covered the following: provision of a waiting area, special rooms for aerosol-generating procedures, special wards for patients with suspected or definite COVID-19, displaying signs on use of facial masks, testing HCWs with a history of contact with a COVID-19 case, surveillance of symptomatic HCWs, paid leave for high-risk HCWs (e.g., HCWs with chronic diseases, pregnant or nursing HCWs), occupational safety and health training on COVID-19, and psychological and behavioral support for job stress. Nine questions concerned supplies of soap, hand sanitizer with at least 60 degrees of ethyl alcohol, and PPE, namely disposable gloves, surgical mask, respirator, facial protector, goggles, apron, and gown. The multiple choice answers to questions about administrative measures and supplies for soap or hand sanitizer included “don’t know, no, partially, and yes”, depending on the question. The multiple choice answers for questions on PPE included “don’t know, no, partially, a few PPE per shift, supplied with an upper limit, supplied whenever required.” The survey and the study protocol were approved by the the Ethics Board for Non-interventional Health Research of the last author’s institution (Decision No. 2020/125).
Contact Procedure
The first and second surveys were started between April 3, 2020 and May 8, 2020, respectively. The link to the surveys was sent via e-mail to 6107 members in April and 6108 members in May. The first survey was kept open for 1 week, without any reminders. However, the second survey was kept open for 1 month, considering coincidence with the month of Ramadan and the holiday for Eid, and 4 reminders were sent to the members.
Statistical Analysis
All statistical analyses were performed using IBM SPSS for Windows V.22.0 (IBM Corp., Armonk, NY). Descriptive statistics were presented as mean ± standard deviation (SD) or median and minimum–maximum for continuous variables, and as number and percentage for categorical variables. The normal distribution for continuous variables was evaluated using the Shapiro–Wilk and Kolmogorov–Smirnov tests. The Mann–Whitney U-test was used for intergroup comparison of continuous variables that did not follow a normal distribution. The chi-square test was used for comparison of categorical variables. The answers of “yes” for the questions related to administrative measures and “supplied whenever required” for the questions related to PPE were accepted as the availability of the measure and compared with any other answers. The healthcare facilities were grouped as tertiary hospital (e.g., research and training hospital, state university hospital, private university hospital), secondary hospital (e.g., state hospital and private hospital), and primary healthcare facility (e.g., tuberculosis dispensary and other primary healthcare facilities). For all comparisons, the level of statistical significance was set at P < .05.
Results
The number of participants was 295 in the first survey and 141 in the second survey, 57 (40.4%) of whom reported that they had already responded to the first survey. Comparing participants’ characteristics between the first and second surveys revealed no statistically significant difference (Table 1). Most participants were females and chest disease specialists, and more than half of the participants in both surveys worked in a research and training hospital or a state university hospital.
Table 1.
The Characteristics of Study Participants
| First Survey (N = 295) | Second Survey (N = 141) | P | |
|---|---|---|---|
| Age, years, median (minimum-maximum) | 44 (24-63) | 45 (25-69) | .274 |
| Female sex, n (%) | 184 (62.4) | 92 (65.2) | .560 |
| Specialty, n (%) | .401 | ||
| Chest diseases | 193 (65.4) | 96 (68.1) | |
| Thoracic surgery | 13 (4.4) | 4 (2.8) | |
| Pediatrics | 14 (4.7) | 11 (7.8) | |
| Other | 75 (25.4) | 30 (21.3) |
|
| Type of the healthcare facility, n (%) | .243 | ||
| Research and training hospital | 77 (26.1) | 35 (24.8) | |
| State university hospital | 71 (24.1) | 48 (34.0) | |
| State hospital | 66 (22.4) | 27 (19.1) | |
| Private hospital | 45 (15.3) | 19 (13.5) | |
| Private university hospital | 11 (3.7) | 7 (5.0) | |
| Tuberculosis dispensary | 5 (1.7) | 1 (0.7) | |
| Other primary healthcare facilities | 20 (6.8) | 4 (2.8) |
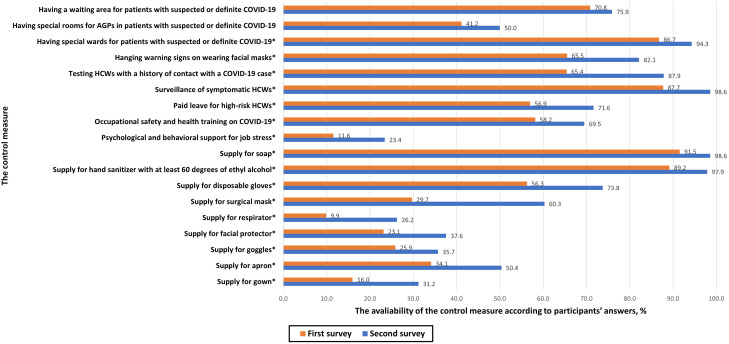
The answers to the questions on the level of the control measures were compared between the 2 surveys. The percentages of answers of “yes” to the questions related to administrative measures or “supplied whenever required” to the questions related to PPE were increased in all 18 items (Figure 1). The improvement was statistically significant for all measures except regarding provision of a waiting area and rooms for aerosol-generating procedures (P values are given in Table 2). In the first survey, less than half of the respondents reported the availability of rooms for aerosol-generating procedures, psychological and behavioral support, and all PPE except disposable gloves. Of those, the level of availability of psychological and behavioral support, respirators, facial protectors, goggles, and gowns were still less than 50% in the second survey.
Figure 1.
The comparision of the avaliability of the control measures according to participants’ answers between first and second surveys. *The statistical significance. AGP, aerosol generating procedure; COVID-19, coronavirus disease 2019; HCW, healthcare worker.
Table 2.
The Comparision of the Avaliability of the Control Measures According to Participants’ Answers Between First and Second Surveys
| First Survey, n/N (%) | Second Survey, n/N (%) | P* | |
|---|---|---|---|
| Having a waiting area for patients with suspected or definite COVID-19 | 209/295 (70.8) | 107/141 (75.9) | .270 |
| Having special rooms for aerosol-generating procedures in patients with suspected or definite COVID-19 | 121/294 (41.2) | 70/140 (50.0) | .083 |
| Having special wards for patients with suspected or definite COVID-19 | 255/294 (86.7) | 133/141 (94.3) | .017 |
| Displaying signs on use of facial masks | 192/293 (65.5) | 115/140 (82.1) | <.001 |
| Testing HCWs with a history of contact with a COVID-19 case | 193/295 (65.4) | 123/140 (87.9) | <.001 |
| Surveillance of symptomatic HCWs | 257/293 (87.7) | 138/140 (98.6) | <.001 |
| Paid leave for high-risk HCWs (e.g., HCWs with chronic diseases, pregnant or nursing HCWs) | 168/295 (56.9) | 101/141 (71.6) | .003 |
| Occupational safety and health training on COVID-19 | 171/294 (58.2) | 98/141 (69.5) | .023 |
| Psychological and behavioral support for job stress | 34/294 (11.6) | 33/141 (23.4) | .001 |
| Supply of soap | 270/295 (91.5) | 139/141 (98.6) | .004 |
| Supply of hand sanitizer with at least 60 degrees of ethyl alcohol | 263/295 (89.2) | 138/141 (97.9) | .002 |
| Supply of disposable gloves | 166/295 (56.3) | 104/141 (73.8) | <.001 |
| Supply of surgical mask | 87/293 (29.7) | 85/141 (60.3) | <.001 |
| Supply of respirator | 29/294 (9.9) | 37/141 (26.2) | <.001 |
| Supply of facial protector | 68/294 (23.1) | 53/141 (37.6) | .002 |
| Supply of goggles | 76/294 (25.9) | 50/140 (35.7) | .034 |
| Supply of apron | 100/293 (34.1) | 71/141 (50.4) | .001 |
| Supply of gown | 47/294 (16.0) | 44/141 (31.2) | <.001 |
*Bold values indicate statistical significance. n, number of participants answering “yes” to the questions related to administrative measures and “supplied whenever required” for the questions related to personal protective equipment (PPE); N, number of participants responding to the relevant question; COVID-19, coronavirus disease 2019.
HCW, healthcare worker.
The level of measures was also compared between tertiary vs. primary and secondary healthcare facilities (Table 3). In the first survey, statistical significance was observed for several administrative measures, including provision of a waiting area (P = .008), rooms for aerosol-generating procedures (P = .042), and special wards for patients with suspected or definite COVID-19 (P < .001); testing HCWs with a history of contact with a COVID-19 case (P < .001), and surveillance of symptomatic HCWs (P = .048). In the second survey, only the provision of special wards for patients with suspected or definite COVID-19 and the supply of aprons were significantly different (P-values were .002 and .027, respectively).
Table 3.
The Comparision of the Avaliability of the Control Measures According to Participants’ Answers Between Primary and Secondary Versus Tertiary Healthcare Facilities in the First and Second Surveys
| First Survey | Second Survey | |||||
|---|---|---|---|---|---|---|
| Primary and Secondary HCFs, n/N (%) | Tertiary HCFs, n/N (%) | P* | Primary and Secondary HCFs, n/N (%) | Tertiary HCFs, n/N (%) | P* | |
| Having a waiting area for patients with suspected or definite COVID-19 | 86/136 (63.2) | 123/159 (77.4) | .008 | 36/51 (70.6) | 71/90 (78.9) | .268 |
| Having special rooms for aerosol-generating procedures in patients with suspected or definite COVID-19 | 47/135 (34.8) | 74/159 (46.5) | .042 | 21/50 (42.0) | 49/90 (54.4) | .158 |
| Having special wards for patients with suspected or definite COVID-19 | 99/135 (73.3) | 156/159 (98.1) | <.001 | 44/51 (86.3) | 89/90 (98.9) | .002 |
| Displaying signs on wearing facial masks | 92/135 (68.1) | 100/158 (63.3) | .383 | 42/51 (82.4) | 73/89 (82.0) | .961 |
| Testing HCWs with a history of contact with a COVID-19 case | 71/136 (52.2) | 122/159 (76.7) | <.001 | 42/51 (82.4) | 81/89 (91.0) | .131 |
| Surveillance of symptomatic HCWs | 112/134 (83.6) | 145/159 (91.2) | .048 | 49/50 (98.0) | 89/90 (98.9) | .671 |
| Paid leave for high-risk HCWs (e.g., HCWs with chronic diseases, pregnant or nursing HCWs) | 70/136 (51.5) | 98/159 (61.6) | .079 | 38/51 (74.5) | 63/90 (70.0) | .568 |
| Occupational safety and health training on COVID-19 | 81/135 (60.0) | 90/159 (56.6) | .556 | 35/51 (68.6) | 63/90 (70.0) | .865 |
| Psychological and behavioral support for job stress | 12/135 (8.9) | 22/159 (13.8) | .186 | 11/51 (21.6) | 22/90 (24.4) | .698 |
| Supply of soap | 128/136 (94.1) | 142/159 (89.3) | .139 | 50/51 (98.0) | 89/90 (98.9) | .682 |
| Supply of hand sanitizer with at least 60 degrees of ethyl alcohol | 125/136 (91.9) | 138/159 (86.8) | .159 | 49/51 (96.1) | 89/90 (98.9) | .266 |
| Supply of disposable gloves | 75/136 (55.1) | 91/159 (57.2) | .719 | 38/51 (74.5) | 66/90 (73.3) | .879 |
| Supply of surgical mask | 42/135 (31.1) | 45/158 (28.5) | .623 | 35/51 (68.6) | 50/90 (55.6) | .127 |
| Supply of respirator | 15/135 (11.1) | 14/159 (8.8) | .509 | 17/51 (33.3) | 20/90 (22.2) | .150 |
| Supply of facial protector | 35/135 (25.9) | 33/159 (20.8) | .295 | 23/51 (45.1) | 30/90 (33.3) | .166 |
| Supply of goggles | 36/135 (26.7) | 40/159 (25.2) | .768 | 22/50 (44.0) | 28/90 (31.1) | .127 |
| Supply of apron | 50/135 (37.0) | 50/158 (31.6) | .332 | 32/51 (62.7) | 39/90 (43.3) | .027 |
| Supply of gown | 23/135 (17.0) | 24/159 (15.1) | .651 | 17/51 (33.3) | 27/90 (30.0) | .681 |
*Bold values indicate statistical significance. n, number of participants answering yes” to the questions related to administrative measures and “supplied whenever required” to the questions related to personal protective equipment (PPE); N, number of participants responding to the relevant question; COVID-19, coronavirus disease 2019.
HCF, healthcare facility; HCW, healthcare worker.
Discussion
The present study investigated the level of control measures in the first and third months of the pandemic at the healthcare facilities where TTS members worked, via online surveys. In all 18 control measures surveyed, the percentages of answers implying the availability increased, 16 of which were also statistically significant. However, the availability of psychological and behavioral support and some PPE, including respirators, facial protectors, goggles, and gowns, still has been reported by less than half of the respondents during the second survey. Although several measures differed significantly between tertiary vs. primary and secondary healthcare facilities in the first survey, only the provision of special wards for patients with suspected or definite COVID-19 and supply of aprons were significantly different in the second survey.
Since the beginning of the pandemic, individual preparedness of HCWs (e.g., knowledge or attitude) and institutional preparedness of healthcare facilities (e.g., level of control measures) has been evaluated by various types of research. Of those, online surveys have played an important role, as physical distancing or stay-at-home orders would prevent face to face interviews. Other advantages include flexibility of the design and ease of repetition for the follow-up.
As the numbers of COVID-19 cases are growing, the researchers from both developed and developing countries evaluated institutional preparedness for the pandemic through online surveys. In Albano et al.’s12 study, nearly 60% of 2136 Italian radiologists declared that they worked safely during the pandemic, and 54.6% felt that their institutions protected them adequately. Paffenholz et al.13 analyzed the perception of the pandemic among 2827 German medical professionals who participated in an online survey between March 27, 2020 and April 11, 2020. The researchers analyzed subgroups according to location, type of medical profession, and type of healthcare facility, revealing statistically significant differences. The preventive measures were rated significantly worse by nurses and participants from ambulatory healthcare centers compared to doctors and participants from maximum-care hospitals, respectively. The PPE shortage was reported more in the ambulatory sector and in East German federal states. Smith et al.14 conducted a convenience-based internet survey of 5988 HCWs in Canada and demonstrated a significant relationship between the percentages of HCWs whose infection control procedure and PPE needs were met and their anxiety and depression symptoms. Alreshidi et al.15 evaluated responses of 1004 HCWs to a web-based survey conducted in Saudi Arabia between April 27, 2020 and May 3, 2020, and found the percentages of HCWs who appreciated various aspects of institutional preparedness for COVID-19 as high as 80-90%. Elhadi et al.’s16 study based on a cross-sectional survey among 1572 healthcare workers in Libya between February 26, 2020 and March 10, 2020 revealed that only less than 7% of participants received training on how to manage COVID-19 cases. Additionally, 47.3% of doctors and 54.7% of nurses who participated in the survey received adequate training on how to effectively use PPE. Hamal et al.17 assessed the COVID-19 readiness in government hospitals of Nepal according to 56 doctors’ responses to an online survey. The results showed that the measures for airborne isolation were found in 38.5% of central hospitals versus 8.3% of provincial hospitals. Moreover, 61.5% and 58.3% of participants working in central hospitals and provincial hospitals, respectively, had received practical training for wearing and removing PPE. Hakim et al.18 conducted an online survey in Pakistan between May 9, 2020 and June 5, 2020 and evaluated responses of 453 HCWs. Of these, 68.9% reported their perception for risk of COVID-19 transmission in their workplace as high.
During the pandemic, work-related psychosocial risks became much more important for HCWs. Pappa et al.19 evaluated the results of 13 relevant studies in their meta-analysis. They found the pooled prevalence of anxiety, depression, and insomnia as 23.2%, 22.8%, and 34.3%, respectively. However, our results demonstrated a very low level of psychological and behavioral support for participants at all types of healthcare facilities in both surveys. We think this aspect of control measures requires urgent action.
The supply and use of appropriate PPE have been among the most important aspects of occupational safety and health of HCWs during the pandemic. Liu et al. showed no COVID-19 in 420 healthcare professionals who worked 4- to 6-hour shifts for an average of 5.4 days a week and an average of 16.2 hours each week in intensive care units with appropriate PPE in Wuhan, China, where the COVID-19 emerged.20 Unfortunately, PPE supplies have not been used with such appropriate care in practice worldwide, particularly at the initial phases. Our results showed that less than 50% of participants of the second survey reported the availability of respirators, facial protectors, goggles, and gowns. Alreshidi et al.15 reported the percentages of HCWs declaring sufficient PPE in their units and hospitals as 68.5% and 58.7%, respectively. In Hakim et al.’s18 study, only 28.5% of 453 Pakistani HCWs reported adequate access to PPE versus 34.4% with no access. Of all PPE, only the supply for apron was significantly different between tertiary versus primary and secondary healthcare facilities, according to our second survey. In Hamal et al.’s17 study, higher availability of adequate facemask in central hospitals than provincial hospitals and local health centers was demonstrated. Similar to our study, Haji et al.21 evaluated PPE preparedness, including adherence to recommendations, training of HCWs, and PPE supplies, in Indian intensive care units through 2 phases of surveys. They reported varying PPE practice levels among states and private, government, and medical colleges and an improvement in PPE practice between the 2 phases of the survey. Kwan et al.22 investigated the PPE supplies with a different approach, including administrative measures and personnel education to control and manage the consumption and proper usage of PPE. They reported a significant decrease in PPE consumption rates.
The strength of the present study includes the evaluation of both administrative measures and availability of PPE, having a second survey to assess the trends, and the comparison of various types of health facilities where the participants worked. There are several limitations of this study. First, relatively low response rates were achieved in both surveys. The period for second survey coincided with the month of Ramadan and the holiday for Eid. To overcome this, the duration of the second survey maintained for longer than the first, and 4 reminders were also sent. Another reason might be the high workload of HCWs during the ongoing pandemic, which makes a low response rate understandable. As in any survey, personal factors might affect participants’ responses. The binary comparison of the answers might help overcome that situation by grouping answers, other than the answer implying the appropriate measures have been taken. Although our results reflected the level of control measures in healthcare facilities, the relationship between control measures and the COVID-19 prevalence in HCWs was not evaluated.
To conclude, our results showed an improvement in both administrative measures and PPE availability in the third month of the pandemic at the healthcare facilities where TTS members worked. However, low availability of psychological and behavioral support and several types of PPE, including respirators, facial protectors, goggles, and gowns, reported in the second survey, pointed out the need for action. In terms of the health and safety of healthcare workers, it is essential to actively monitor the level of administrative measures and supplies for PPE and to eliminate deficiencies during the pandemic.
Funding Statement
The author declared that this study has received no financial support.
Footnotes
Ethics Committee Approval: This study was approved by the the Ethics Board for Non-interventional Health Research of Düzce University, (Approval No: 2020/125).
Informed Consent: Verbal informed consent was obtained from the participants who agreed to take part in the study.
Peer Review: Externally peer-reviewed.
Author Contributions: Supervision – A.S., P.M.A.; Design – A.S., P.M.A., C.S.; Concept– A.S., Z.N.T, P.M.A.; Resources – A.S., Z.N.T., P.M.A., C.S.; Materials – C.S., A.S.; Data Collection and/or Processing – C.S., A.S., P.M.A.; Analysis and/or Interpretation – A.S., Z.N.T., P.M.A.; Literature Search – A.S., Z.N.T.; Writing Manuscript – A.S., Z.N.T.; Critical Review – P.M.A., C.S.
Acknowledgments: The authors thank the members of the Executive Committee of the Turkish Thoracic Society for their collaboration and support. The results of this study were presented as an oral presentation at the Turkish Thoracic Society’s 23rd Annual Congress (Virtual Congress, 15-18 October 2020).
Conflict of Interest: The author has no conflict of interest to declare.
References
- 1. Timeline of WHO’s response to COVID-19 2020. 2020. Available at: https://www.who.int/news-room/detail/29-06-2020-covidtimeline/. [Google Scholar]
- 2. Gandhi RT, Lynch JB, del Rio C. Mild or moderate Covid-19. N Engl J Med. 2020;383:1757–1766.. 10.1056/NEJMcp2009249) [DOI] [PubMed] [Google Scholar]
- 3. Koh D. Occupational risks for COVID-19 infection. Occup Med. 2020;70:3–5.. 10.1093/occmed/kqaa036) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nguyen LH, Drew DA, Graham MS. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475–e483.. 10.1016/S2468-2667(20)30164-X) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. European Centre for Disease Prevention and Control. Infection prevention and control for COVID-19 in healthcare settings – Third update. 2020. Available at: https://www.ecdc.europa.eu/sites/default/files/documents/Infection-prevention-control-for-the-care-of-patients-with-2019-nCoV-healthcare-settings_third-update.pdf. [Google Scholar]
- 6. Republic of Turkey Ministry of Family, Labour, and Social Services. [Fight with COVID-19 at workplaces]. 2020. Available at: https://ailevecalisma.gov.tr/covid19. [Google Scholar]
- 7. Republic of Turkey Ministry of Health. [Advices on personal protective equipment use against COVID-19 according to type of healthcare facility, duty and work activity]. 2020. Available at: https://covid19bilgi.saglik.gov.tr/depo/enfeksiyon-kontorl-onlemleri/KISISEL_KORUYUCU_EKIPMAN_KULLANIMI.pdf. [Google Scholar]
- 8. Republic of Turkey Ministry of Health. [Guideline on COVID-19 (SARS-CoV-2 infection)]. 2020. Available at: https://covid19bilgi.saglik.gov.tr/depo/rehberler/COVID-19_Rehberi.pdf?type=file. [Google Scholar]
- 9. U.S. Department of Labor Occupational Safety and Health Administration. Guidance on preparing workplaces for COVID-19. 2020. Available at: https://www.osha.gov/Publications/OSHA3990.pdf. [Google Scholar]
- 10. Burki T. Global shortage of personal protective equipment. Lancet Infect Dis. 2020;20:785–786.. 10.1016/S1473-3099(20)30501-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Anatolian Agency. [The Minister of Health declared the first diagnosed case of COVID-19]. 2020. Available at: https://www.aa.com.tr/tr/koronavirus/saglik-bakani-koca-turkiyede-ilk-koronavirus-vakasinin-goruldugunu-acikladi/1761466. [Google Scholar]
- 12. Albano D, Bruno A, Bruno F. Impact of coronavirus disease 2019 (COVID-19) emergency on Italian radiologists: a national survey. Eur Radiol. 2020;30:6635–6644.. 10.1007/s00330-020-07046-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Paffenholz P, Peine A, Hellmich M. Perception of the 2020 SARS-CoV-2 pandemic among medical professionals in Germany: results from a nationwide online survey. Emerg Microbes Infect. 2020;9:1590–1599.. 10.1080/22221751.2020.1785951) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Smith PM, Oudyk J, Potter G, Mustard C. The association between the perceived adequacy of workplace infection control procedures and personal protective equipment with mental health symptoms: a cross-sectional survey of Canadian health-care workers during the COVID-19 pandemic. [l'association entre le caractère adéquat perçu des procédures de contrôle des infections Au travail et de l'équipement de protection personnel pour les symptômes de santé mentale. Un sondage transversal des travailleurs de la santé canadiens durant la pandémie COVID-19]. Can J Psychiatry. 2021;66:17–24.. 10.1177/0706743720961729) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alreshidi NM, Haridi HK, Alaseeri R. Assessing healthcare workers' knowledge, emotions and perceived institutional preparedness about COVID-19 pandemic at Saudi hospitals in the early phase of the pandemic. J Public Health Res. 2020;9:1936. 10.4081/jphr.2020.1936) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Elhadi M, Msherghi A, Alkeelani M. Assessment of healthcare workers' levels of preparedness and awareness regarding COVID-19 infection in low-resource settings. Am J Trop Med Hyg. 2020;103:828–833.. 10.4269/ajtmh.20-0330) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hamal PK, Pokhrel N, Pandey D, Malla P, Lamsal R. Perspective of doctors for COVID-19 pandemic readiness in government hospitals of Nepal. J Nepal Health Res Counc. 2020;18:166–171.. 10.33314/jnhrc.v18i2.2811) [DOI] [PubMed] [Google Scholar]
- 18. Hakim M, Khattak FA, Muhammad S. Access and use experience of personal protective equipment among frontline healthcare workers in pakistan during the COVID-19 emergency: a cross-sectional study. Health Secur. 2021;19:140–149.. 10.1089/hs.2020.0142) [DOI] [PubMed] [Google Scholar]
- 19. Pappa S, Ntella V, Giannakas T. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907.. 10.1016/j.bbi.2020.05.026) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liu M, Cheng SZ, Xu KW. Use of personal protective equipment against coronavirus disease 2019 by healthcare professionals in wuhan, china: cross sectional study. BMJ. 2020;369:m2195. 10.1136/bmj.m2195) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Haji JY, Subramaniam A, Kumar P, Ramanathan K, Rajamani A. State of personal protective equipment practice in Indian intensive care units amidst COVID-19 pandemic: a nationwide survey. Indian J Crit Care Med. 2020;24:809–816.. 10.5005/jp-journals-10071-23550) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kwan WM, Mok CK, Kwok YT. Bundled interventions for consumption management and monitoring of personal protective equipment in COVID-19 pandemic in Hong Kong local hospitals. BMJ Open Qual. 2020;9:e000990. 10.1136/bmjoq-2020-000990) [DOI] [PMC free article] [PubMed] [Google Scholar]