Abstract
OBJECTIVE:
Benign Paroxysmal Positional Vertigo (BPPV) as the most common vestibular disorder can affect the quality of life. This study aimed to compare the effectiveness of the half somersault maneuver (HSM) as a treatment to that of the Epley maneuver (EM) as a clinical-based treatment in subjects with PC-BPPV.
Methods:
In this randomized study, 43 participants with unilateral posterior canal BPPV were recruited. The experimental group received the HSM, whereas the control group received the EM. All participants were asked to fill in the Vestibular Rehabilitation Benefit Questionnaire (VRBQ), Dizziness Handicap Inventory (DHI), and Vertigo Symptom Scale (VSS) questionnaires at pretreatment and at 48 hours, 1 week, and 1 month post-treatment. The severity of residual dizziness was determined by the visual analog scale (VAS) weekly for up to 4 weeks after treatment. The success rate and the recurrence rate were assessed after the 3-month follow-up.
Results:
The differences between the results of pretreatment and post-treatment questionnaires for both groups were significant. However, the differences were not significant between the 2 groups for the DHI scores, the total, dizziness, motion-provoked dizziness, and symptom subscale scores of the VRBQ, and the anxiety subscale scores of the VSS. There were significant differences between the 2 groups for VAS, the total VSS and vertigo subscale scores, and the VRBQ anxiety subscale scores.
Conclusion:
Even though both maneuvers are significantly effective in the treatment of PC-BPPV, subjects in the HSM group reported more improvement in terms of psychometric symptoms and residual dizziness compared to the EM group.
Keywords: BPPV, Epley maneuver, half somersault maneuver, canalith repositioning maneuver
Introduction
As one of the most common vestibular disorders, Benign Paroxysmal Positional Vertigo (BPPV), is described as short rotatory vertigo attacks that are triggered when the head position changes relative to gravity.1 BPPV has been diagnosed as approximately 15% of all balance disorders, and 17% to 42% of all causes of vertigo. It is caused by free-floating endolymph particles (otoconia) that have detached from the utricle and are displaced in the semicircular canals.2,3 The resulting vertigo is often accompanied by elevated anxiety and signs of emotional disturbance.4 Furthermore, it can impact a patient’s quality of life with a reduction in activities of daily living and frequent falls.1 Vertigo experienced in BPPV responds well to treatment.
The best practice in treating BPPV is the Canalith Repositioning Procedure (CRP), and depending on the affected canals, different maneuvers have been described.5 Almost 85% to 95% of cases of BPPV arise in the posterior semicircular canal (PC-BPPV).6 To treat PC-BPPV, the Epley and Semont maneuvers are commonly used, with nearly similar success rates.7 The Epley maneuver (EM) as a CRP is most used to treat PC-BPPV for an effective outcome.8 Even though the EM can remove the particles successfully, it may be associated with mild but negative outcomes such as fainting and nausea as well as a change to horizontal canal BPPV.9 Foster et al. (2012) proposed another treatment called Half Somersault Maneuver (HSM) that can clear the detached particles from the posterior semicircular canal, with fewer side effects.7 According to Foster (2012), the first stage in performing the EM is similar to the Dix Hallpike (DH) maneuver and causes ampullofugal movements that contribute to the sensation of vertigo and nystagmus which may be severe enough to induce uncomfortable symptoms such as vomiting. Conversely, in the initial step of the HSM, the particle movement is against the direction of fluid movement and has an inhibitory effect (ampullopetal movement). Consequently, it reduces the symptoms of dizziness and nausea experienced by the patients.
Foster et al. (2012) assessed the efficacy of the EM versus the HSM as a home-based exercise. In their study, the severity of the dizziness, the nystagmus intensity during the exercise, and treatment failures after a 6-month follow-up were evaluated. Their results showed that nystagmus intensity was significantly reduced in the EM group compared to the HSM group, initially. However, induced dizziness during the HSM was remarkably lower compared to the EM, and treatment failure was more frequent in the EM.7 In another study, Paramasivan Mani et al. (2019) used the Dizziness Handicap Inventory (DHI) questionnaire to compare the effectiveness of the EM and HSM with the Brandt–Daroff exercise in patients with PC-BPPV and showed greater success in reducing the perceived handicap by self-application of HSM with the Brandt–Daroff exercise.10 Moreover, home-based treatment is a cost-effective and time-saving approach to recommend for patients with recurrent or continued BPPV who need additional maneuvers after the first clinical-based intervention.
The current study aimed to compare the effectiveness of the HSM as a treatment to that of the EM as a clinical-based treatment in subjects with PC-BPPV. This includes home-based treatment with HSM. The author’s premise was to investigate the possibility and success of recommending a home-based, self-applied intervention instead of performing multiple EMs at the clinic.
Methods
Participants
All participants were selected with unilateral PC-BPPV according to the AAO-HNS (2017) clinical practice guideline on BPPV,9 from April to September 2019 at AmirAlam hospital. After their medical history was recorded, participants underwent otoscopy, tympanometry, pure-tone audiometry, and the full VNG test battery. All participants had normal pure-tone thresholds (less than 25 dBHL) at speech frequencies, and none of them had a history of the neurological or otological disease, head trauma, or alcohol/drug abuse.11 All subjects who diagnosed positive for horizontal canal BPPV (HC-BPPV) in the supine roll test were excluded from the study. The participants had to be able to correctly perform the HSM and EM, Therefore, the subjects complaining about knee, neck, and back injuries were not included in the study.7 All procedures in this study received the approval of the research board of Iran University of Medical Sciences. Ethical code: IR.IUMS.REC.1397.1134. All subjects signed a written consent form to actively participate in the study. They were matched for age and randomly assigned to 2 study groups. The control group received the EM (n = 26) and the experimental group was treated with the HSM (n = 17). A total of 6 participants (3 in each group) did not fully cooperate in follow-up, and were excluded from the analyses.
Procedures
The EM was performed based on AAO-HNS 2017 clinical practice guideline on BPPV.9 The EM was performed as a single maneuver per session by the main investigator in the outpatient clinic. If the symptoms of BPPV persisted or recured, the subjects had to return to the hospital. All subjects were reassessed by the DH test and the supine roll test after a week and a month following the first visit. The HSM was also exactly performed according to Foster’s definition as follows, by an example for right-sided BPPV: “While kneeling, the head is quickly tipped upward and back. Next, the somersault position is assumed, with the chin tucked as far as possible toward the knee. After that, the head is turned about 45° toward the right shoulder, to face the right elbow. Then, maintaining the head at 45°, the head is raised to the back/shoulder level. Eventually, maintaining the head at 45°, the head is raised to the fully upright position. After each position change, any dizziness is allowed to subside before moving into the next position; if there is no dizziness, the position should be held for 15 seconds.”7 To make sure that the experimental group correctly performed the HSM, they had to do it at the hospital first under the supervision of the main investigator. Afterward, HSM was performed by the subjects at home if the symptoms of PC-BPPV persisted. We also recoreded a video that showed how to do the maneuver and sent it to the subjects. Moreover, all subjects were monitored through phone interviews.
Outcome Measures
Successful treatment was defined as the absence of positional vertigo and torsional nystagmus in the DH test. The validated Persian versions of the DHI, Vestibular Rehabilitation Benefit Questionnaire (VRBQ), and Vertigo Symptom Scale (VSS)12-14 were administered by personally interviewing the participants before treatment, and phone interview at 48 hours (48h), 1 week (1w), and 1 month (1m) after treatment to track the individuals’ symptoms. The DHI consists of 25 items and 3 subscales: physical (DHI-P), functional (DHI-F), and emotional (DHI-E).12 The VRBQ has 22 questions and 5 subsets: dizziness (VRBQ-D), anxiety (VRBQ-A), symptoms (VRBQ-S), quality of life (VRBQ-Q), and motion-provoked dizziness (VRBQ-M).14 The VSS includes 2 versions (Long and short). The short form (VSS-SF) includes 15 items and the long version consists of 34 items and 2 subscales: the vertigo scale (VSS‑VER) and the anxiety and autonomic symptom scale (VSS‑AA).13, 15 Furthermore, the authors assessed the severity of residual dizziness by devising a visual analog scale (VAS), weekly for up to 4 weeks after treatment. The VAS is a tool to measure the intensity of the subjective complaints and the severity of residual dizziness after treatment. This tool was scaled from 0 (best condition) to 10 (worst condition) lines. The rate of recurrence of BPPV was assessed for up to 3 months after the first visit.
Statistical Analysis
Statistical analysis was performed by SPSS (SPSS V.23; Chicago, United States). The data for 43 participants (17 experimental, and 26 for control groups) were included in the analyses. According to the normal distribution of the data, the mixed ANOVA was used at a significance level of P < .05. Partial Eta-Squared was also calculated.
Results
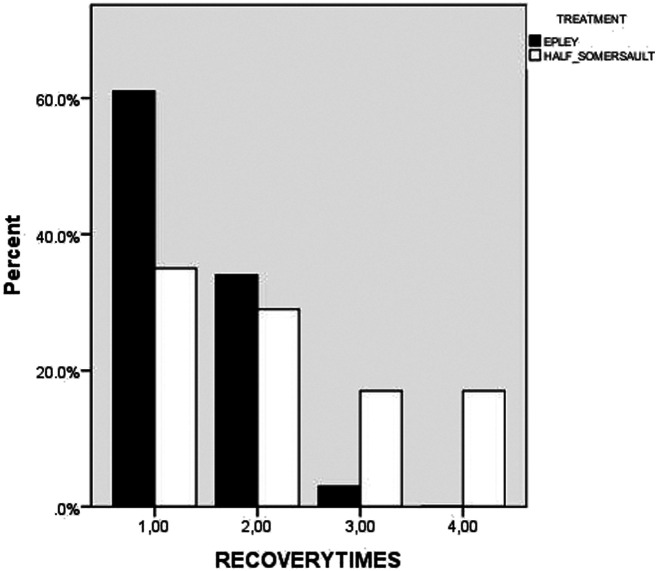
A total of 43 participants (30 women and 13 men), aged 31-60 years (mean ± SD = 52.18 ± 8.16), participated in this study. The total and subscale scores of the DHI, VSS, and VRBQ questionnaires at pretreatment, and 48 hours, 1 week, and 1 month after treatment are shown in Table 1. Table 2 shows the VAS scores completed weekly up to 1 month after treatment in both groups. There were significant differences (P < .0001) between pretreatment and post-treatment in the total and subscale scores of all questionnaires in each of the groups, and it was significant in each step with respect to the pervious. However, the differences between the 2 groups for the total and subscale of the DHI scores (DHI-TOTAL, DHI-P, DHI-E, and DHI-F) were not statistically significant (P = .119, P = .944, P = .059, P = .111, respectively). Figure 1 shows the total, the physical, functional, and emotional subscales of the DHI scores at pretreatment and at 48 hours, 1 week, and 1 month post-treatment in both groups. The total VSS and vertigo subscale scores at pretreatment and at 48 hours, 1 week, and 1 month post-treatment are shown in Figure 2 (P = .045, P = .038, respectively). These differences between the 2 groups were significant. Figure 2 shows the anxiety and autonomic subscales, and the short-version VSS scores at pretreatment and at 48 hours, 1 week, and 1 month post-treatment in both groups. No significant difference was observed between the HSM group and the EM group (P = 0.060, P = 0.128, respectively). Figure 3 represents the total, dizziness, motion-provoked dizziness, and symptom subscales of the VRBQ scores at pretreatment and at 48 hours, 1 week, and 1 month post-treatment in both groups. The differences between the 2 groups were not statistically significant (P = 0.086, P = 0.054, P = 0.330, P = 0.260, respectively). Scores for anxiety and quality of life subscales of the VRBQ scores were significantly less for the HSM group (P = .015, P = .023) (Figure 3). Moreover, for the residual dizziness, a significant difference was seen in the VAS scores in the HSM group compared to the EM group (P < 0.0001), as shown in Table 2. In each of the groups, there were significant differences between the first (VAS 1w) and second stage (VAS 2w), and between the second (VAS 2w) and third (VAS 3w) stage (P < 0.001, P = 0.009, respectively). However, it was not significant between the third (VAN 3w) and fourth (VAS 4w) stage (P = 1.00). Figure 4 shows the successful treatment rate (disappearance of nystagmus and vertigo) after 4 maneuvers in both HSM & EM groups. As depicted in Figure 4, most of the patients in the EM group were successfully treated after 2 maneuvers (61% after the first maneuver), and only 1 patient needed the third maneuver. However, the successful treatment rate was lower in the HSM group. In the study, 35% of HSM patients were treated successfully after the first maneuver, whereas 29% needed second maneuvers, 17% needed third, and 17% needed fourth maneuvers for the complete resolution of vertigo and nystagmus. Meanwhile, the recurrence rate of symptoms was lower in the HSM group (5%) compared to the EM group (11%) which was not significant. None of these subjects with recurrent BPPV were positively diagnosed with HC-BPPV. Partial Eta-Squared is shown in Tables 1and 2, shown for all variables between the 2 study groups. It was between 0.34 and 0.87 in each of the groups.
Table 1.
Summary of the Questionnaire Results (Mean ± SD)
| Partial Eta Squared | Control Group | Experimental Group | Questionnaires | ||||||
| 1 month | 1 week | 48 hours | Pre-test | 1 month | 1 week | 48 hours | Pre-test | ||
| 0.058 | 6.38 ± 6.24 | 12.84 ± 10.38 | 28.61± 18.11 | 56.69 ± 18.34 | 3.76 ± 5.09 | 10.52 ± 12.76 | ±13.89 20.64 | 48.58 ± 14.94 | DHI_Total |
| 0.061 | 3.46 ± 3.92 | 6.69 ± 4.99 | 13.61 ± 7.87 | 22.61 ± 7.34 | 1.41 ± 2.20 | 4.58 ± 6.19 | 6.39 ± 10.23 | 20.82 ± 7.48 | DHI_F |
| 0.000 | 1.69 ± 0.69 | 3.00 ± 4.00 | 8.30 ± 6.56 | 20.38 ± 5.30 | 1.52 ± 3.77 | 3.94 ± 4.87 | 6.73 ± 7.41 | 19.76 ± 3.59 | DHI_P |
| 0.084 | 3.21 ± 1.76 | 3.23 ± 4.66 | 6.92 ± 6.93 | 13.69 ± 9.44 | 0.70 ± 2.11 | 2.00 ± 4.30 | 4.30 ± 3.05 | 8.00 ± 6.32 | DHI_E |
| 0.094 | 4.96 ± 4.72 | 8.53 ± 6.53 | 16.57 ± 8.50 | 21.26 ± 9.85 | 2.29 ± 1.31 | 5.52 ± 3.93 | 6.04 ± 10.64 | 18.05 ± 6.94 | VSS_Total |
| 0.044 | 2.00 ± 1.61 | 4.19 ± 3.29 | 9.38 ± 4.72 | 12.03 ± 4.41 | 0.94 ± 1.08 | 3.29 ± 3.49 | 6.23 ± 4.45 | 11.94 ± 5.20 | VSS_VER |
| 0.084 | 3.38 ± 3.56 | 4.38 ± 4.07 | 7.19 ± 5.25 | 9.34 ± 7.38 | 1.47 ± 1.00 | 2.94 ± 1.95 | 2.64 ± 4.47 | 5.88 ± 2.44 | VSS_AA |
| 0.056 | 2.34 ± 2.26 | 5.00 ± 3.33 | 10.42 ± 4.20 | 12.26 ± 3.93 | 1.35 ± 1.25 | 3.58 ± 2.95 | 7.41 ± 3.58 | 12.64 ± 3.46 | VSS_SF |
| 0.070 | 5.50 ± 6.13 | 11.50 ± 8.32 | 26.76 ± 12.20 | 59.80 ± 13.99 | 3.88 ± 4.78 | 10.82 ± 11.89 | 13.50 ± 19.88 | 51.70 ± 14.05 | VRBQ_Total |
| 0.039 | 1.83 ± 1.61 | 3.38 ± 2.45 | 7.11 ± 2.77 | 9.84 ± 2.11 | 0.94 ± 1.24 | 2.82 ± 2.81 | 5.05 ± 2.68 | 10.29 ± 2.61 | VRBQ_D |
| 0.137 | 1.30 ± 1.61 | 1.88 ± 2.12 | 2.84 ± 2.76 | 3.30 ± 2.89 | 0.52 ± 0.62 | 0.64 ± 0.78 | 0.94 ± 1.34 | 1.29 ± 1.49 | VRBQ_A |
| 0.023 | 0.42 ± 1.23 | 1.15 ± 2.66 | 4.73 ± 4.74 | 19.96 ± 4.41 | 1.00 ± 1.69 | 3.47 ± 4.43 | 4.87 ± 5.29 | 19.29 ± 3.98 | VRBQ_M |
| 0.031 | 3.26 ± 3.35 | 6.42 ± 5.23 | 14.69 ± 7.42 | 33.07 ± 6.27 | 2.35 ± 2.69 | 6.82 ± 7.11 | 11.41 ± 7.76 | 30.88 ± 6.49 | VRBQ_S |
| 0.119 | 2.30 ± 3.03 | 5.23 ± 4.27 | 12.76 ± 6.86 | 28.07 ± 10.77 | 1.41 ± 2.52 | 3.88 ± 5.85 | 8.47 ± 7.33 | 20.23 ± 8.59 | VRBQ_Q |
Table 2.
Mean ± SD VAS Scores in Both Groups
| Partial Eta-Squared | Control Group | Experimental Group | VAS Scores | ||||||
| Fourth Week | Third Week | Second Week | First Week | Fourth Week | Third Week | Second Week | First Week | ||
| 0.363 | 0.88 ± 1.14 | 1.07 ± 1.44 | 1.88 ± 1.55 | 4.23 ± 1.53 | 0.35 ± 1.05 | 0.17 ± 0.52 | 0.29 ± 0.98 | 1.52 ± 1.62 | |
Figure 1.
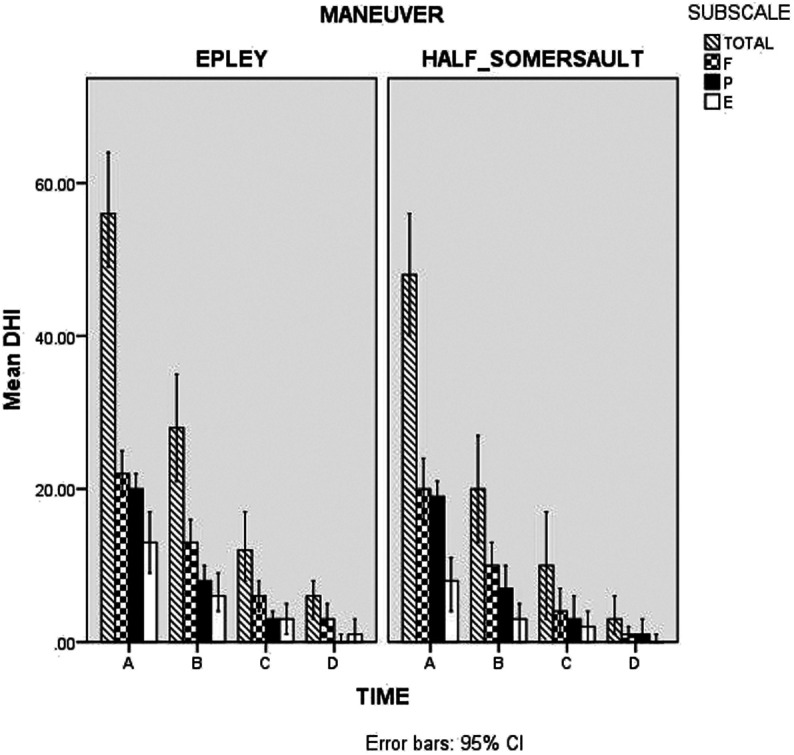
DHI scores in both groups.: Total (total), F (functional), P (physical) and E (emotional) subscales of DHI scores respectively from the left side to the right side at A (pretreatment), B (48-hours post-treatment), C (1-week post-treatment) and D (1-month post-treatment).
Figure 2.
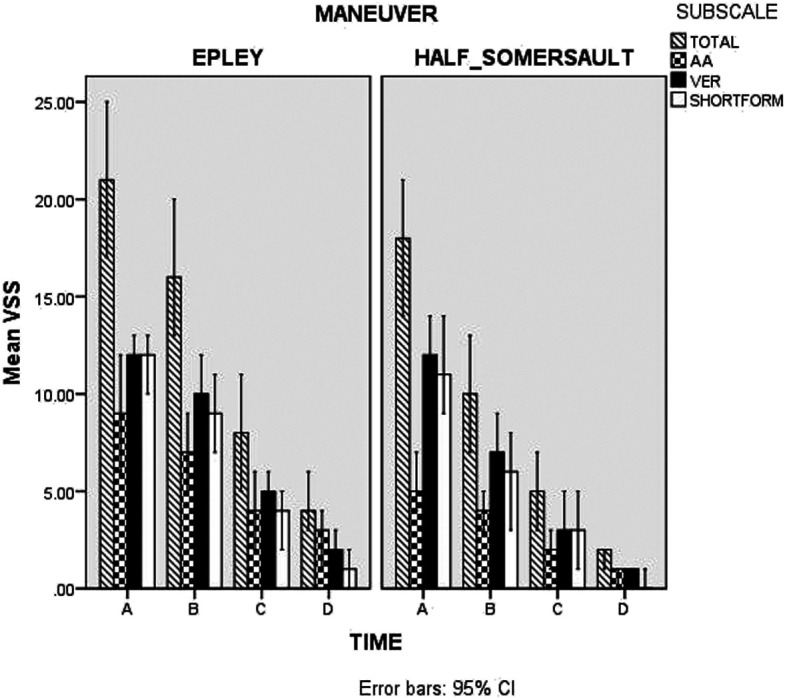
VSS scores in both groups: Total (total), AA (anxiety and autonomic symptom), VER (Vertigo) subscale and SHOERTFORM (short version) VSS score respectively from the left side to the right side at A (pretreatment), B (48 hours post-treatment), C (1-week post-treatment) and D (1-month post-treatment).
Figure 3.
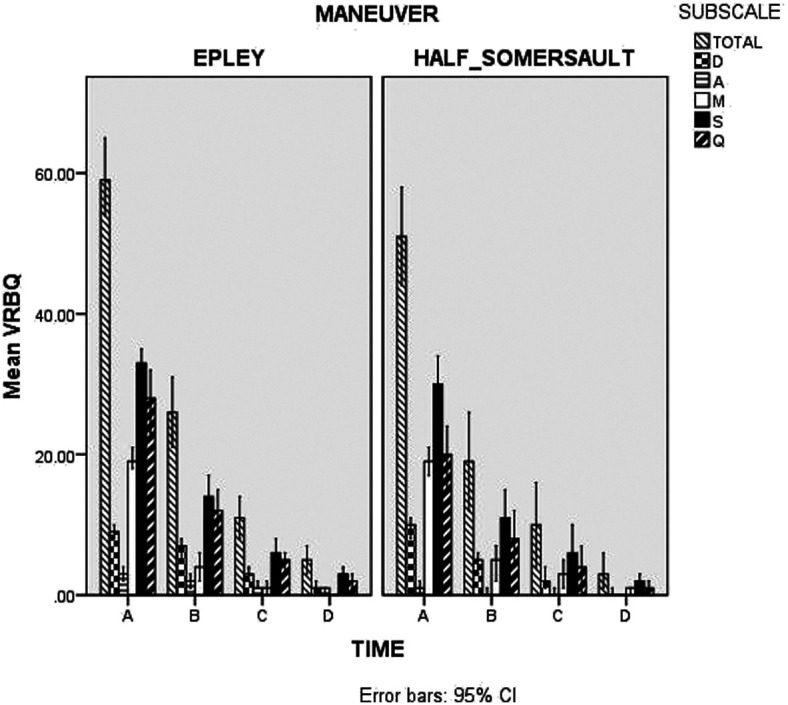
VRBQ scores in both groups: Total (total), D (dizziness), A (anxiety), M (motion provoked dizziness), S (symptoms), and Q (quality of life) subscale VRBQ scores respectively from the left side to the right side at A (pretreatment), B (48 hours post-treatment), C (1week post-treatment) and D (1-month post-treatment).
Figure 4.
Successful treatment rate in HSM & EM groups.
Discussion
The main aim of the current study was to compare the effectiveness of the Half Somersault CRP treatment to the Epley as a clinical treatment for PC-BPPV in terms of resolution of psychometric symptoms and successful treatment rate. This included home-based HSM when the first HSM performed in the clinic failed to address the BPPV. This study demonstrated that both maneuvers are significantly effective in the treatment of PC-BPPV and can improve the symptoms of vertigo and anxiety, and the quality of life. Also, considering the results of the successful treatment rate, both maneuvers can lead to the disappearance of nystagmus in the subjects with PC-BPPV. Compared to the HSM, the EM was significantly more effective after 1 maneuver (disappearance of nystagmus and vertigo), therefore some individuals may need to perform additional HSMs for the treatment of BPPV at home. In this study, 17% of subjects needed to do 4 HSMs. Nonetheless, the participants in the HSM group experienced significantly lower residual dizziness than the EM group after performing the maneuver. According to the results, the total and vertigo subscale VSS scores, anxiety as well as quality of life subscale VRBQ scores were significantly lower for the HSM group. Furthermore, in this group, we noted that the dizziness subscale VRBQ, emotional subscale DHI, and the anxiety subscale VSS scores were lower compared to the EM group. Hence, the subjects in the HSM group reported more improvement in terms of the psychometric symptoms after receiving the maneuver compared to the EM group. Moreover, Foster et al. (2012) revealed that dizziness experienced during the HSM was significantly lower compared to the EM, and when the 2 maneuvers are used as a home treatment, the number of recurrences was higher for the EM compared to HSM. Conversion to HC-BPPV was observed only in the Epley group after the 6-month follow-up. Nevertheless, they reported that the EM was significantly effective in the reduction of nystagmus intensity with 2 maneuvers.7 The recurrence rate in the HSM group was lower than EM, though it did not reach the significance level. The Paramasivan Mani et al. study reported that home-based HSM+Brandt–Daroff exercise was more effective than the EM+Brandt–Daroff exercise in reducing the self-perceived handicap among patients with PC-BPPV at the end of 3 weeks.10 The current study suggests that HSM as a home-based treatment for PC-BPPV could be used to resolve the particles from the semicircular canals and improve the psychometric symptoms with more comfort for the patients, compared to outpatient delivery of the EM. With the ampullopetal movement in the HSM, as mentioned in the introduction section, the dizziness experienced by the patients during the HSM is less, and can be performed without assistance. Needless to say, performing the HSM could be difficult for patients with neck, knee, or back injuries.
The findings of this study have to be seen in light of some limitations that could be addressed in future research. The major limitation is that authors did not have access to validated BPPV-specific outcome measures in their native language. Future studies with more specific questionnaires on BPPV are recommended. The second limitation concerns the full vestibular testing including vHIT & VEMP to explore possible cryptogenic vestibular comorbidities. Considering the fact that BPPV is more common in females, future studies should be proposed to gender-match the participants. Moreover, a study that assesses these maneuvers in elderly patients is suggested.
Conclusion
The current study indicates that both exercises are effective in resolving the symptoms of PC-BPPV and that the Epley is more effective than the Half Somersault with one maneuver. However, the subjects in the Half Somersault group reported more improvement in the psychometric symptoms and residual dizziness after performing the maneuver. Also, the HSM is an easy exercise that individuals can perform at home to treat PC-BPPV.
Funding Statement
This study is supported by Iran University of Medical Science.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Iran University of Medical Sciences. Ethical code: IR.IUMS.REC.1397.1134.
Informed Consent: Informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – M.D.K., M.A.; Design – M.D.K., M.A.; Supervision – M.A.; Re-source – M.A., M.D.K., B.J.; Materials – M.A., M.D.K.; Data Collection and/or Pro-cessing –M.D.K., M.M.; Analysis and/or Interpretation –M.D.K., M.A., M.M., B.J.; Literature Search – M.D.K., M.A., M.M., B.J.; Writing – M.D.K., M.A.; Critical Reviews – M.D.K., M.A., M.M., B.J.
Acknowledgments: This study was part of a MSc. dissertation project in Audiology supported by the Iran University of Medical Sciences (Ethical code: IR.IUMS.REC.1397.1134).
Conflicts of Interest: The authors have no conflict of interest to declare.
References
- 1. Helminski J.O., Zee D.S., Janssen I., Hain T.C. Effectiveness of particle repositioning maneuvers in the treatment of benign paroxysmal positional vertigo: a systematic review. Phys Ther. 2010;90(5):663–678.. 10.2522/ptj.20090071) [DOI] [PubMed] [Google Scholar]
- 2. Nuti D., Masini M., Mandalà M. Benign paroxysmal positional vertigo and its variants. Handb Clin Neurol. 2016;137:241–256.. 10.1016/B978-0-444-63437-5.00018-2) [DOI] [PubMed] [Google Scholar]
- 3. Jilla A.M., Roberts R.A., Johnson C.E. Teaching patient-centered counseling skills for assessment, diagnosis, and management of benign paroxysmal positional vertigo. Semin Hear. Thieme Medical Publishers. 2018;39(1):52–66.. 10.1055/s-0037-1613705) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yardley L., Masson E., Verschuur C., Haacke N., Luxon L. Symptoms, anxiety and handicap in dizzy patients: development of the vertigo symptom scale. J Psychosom Res. 1992;36(8):731–741.. 10.1016/0022-3999(92)90131-k) [DOI] [PubMed] [Google Scholar]
- 5. Bressi F. et al. Vestibular rehabilitation in benign paroxysmal positional vertigo: reality or fiction?. Int J Immunopathol Pharmacol. SAGE Publications Sage UK 2017;30(2):113–122.. 10.1177/0394632017709917) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wegner I., Niesten M.E., van Werkhoven C.H., Grolman W. Rapid systematic review of the Epley maneuver versus vestibular rehabilitation for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2014;151(2):201–207.. 10.1177/0194599814534940) [DOI] [PubMed] [Google Scholar]
- 7. Foster C.A., Ponnapan A., Zaccaro K., Strong D. A comparison of two home exercises for benign positional vertigo: half Somersault versus Epley Maneuver. Audiol Neurotol Extra. 2012;2(1):16–23.. 10.1159/000337947) [DOI] [Google Scholar]
- 8. Sugita-Kitajima A., Sato S., Mikami K., Mukaide M., Koizuka I. Does vertigo disappear only by rolling over? Rehabilitation for benign paroxysmal positional vertigo. Acta oto-laryngol. 2010;130(1):84–88.. 10.3109/00016480902968086) [DOI] [PubMed] [Google Scholar]
- 9. Bhattacharyya N., Gubbels S.P., Schwartz S.R. et al. Clinical practice guideline: benign paroxysmal positional vertigo (update). Otolaryngol Head Neck Surg. 2017;156(suppl 3):S1–S47.. 10.1177/0194599816689667) [DOI] [PubMed] [Google Scholar]
- 10. Mani P. et al. Comparison of effectiveness of Epley’s maneuver and half-somersault exercise with Brandt-Daroff exercise in patients with posterior canal Benign Paroxysmal Positional Vertigo (pc-BPPV): a randomized clinical trial. Int. J. Health Sci. 2019;9(1):89–94.. [Google Scholar]
- 11. Dispenza F., Kulamarva G., De Stefano A. Comparison of repositioning maneuvers for benign paroxysmal positional vertigo of posterior semicircular canal: advantages of hybrid maneuver. Am J Otolaryngol. 2012;33(5):528–532.. 10.1016/j.amjoto.2011.12.002) [DOI] [PubMed] [Google Scholar]
- 12. Jafarzadeh S., Bahrami E., Pourbakht A., Jalaie S., Daneshi A. Validity and reliability of the Persian version of the dizziness handicap inventory. J Res Med Sci Off J Isfahan Univ Med Sci. 2014;19(8):769-775. [PMC free article] [PubMed] [Google Scholar]
- 13. Kamalvand A., Ghahraman M.A., Jalaie S. Development of the Persian version of the Vertigo Symptom Scale: validity and reliability. J Res Med Sci Off J Isfahan Univ Med Sci. 2017;22:58. 10.4103/jrms.JRMS_996_16) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moossavi A. et al. Development and assessment of validity and reliability of the Persian version of vestibular rehabilitation benefit questionnaire. Auditory Vestib Res. 2018;27(2):65–71.. [Google Scholar]
- 15. Kondo M., Kiyomizu K., Goto F. et al. Analysis of vestibular-balance symptoms according to symptom duration: dimensionality of the Vertigo Symptom Scale-short form. Health Qual Life Outcomes. 2015;13(1):4. 10.1186/s12955-015-0207-7) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a