Abstract
Background:
The only treatment in patients developing liver failure is liver transplantation. According to the Ministry of Health, the number of patients waiting for a liver transplantation is 2141, the average waiting period for liver transplantation is approximately 5 years, and 15-18% of these patients lose their life while waiting for transplantation. In these patients, limitations in daily activities and depression–anxiety are commonly found. The aim of this study was to analyze life quality, depression symptoms, and existence of sexual functional disorders of patients waiting for liver transplantation.
Methods:
A total of 74 patients, who were registered in Başkent University Hospital between 2015 and 2018, were included into the study. Short Form-36, Beck Depression Inventory, and Arizona Sexual Experiences Scale were applied to 56 patients who approved study.
Results:
Most of the patients were male (64.3%), and the mean age was 46 (18-64). Short Form-36 scores were low in all patients. The mean Beck Depression Inventory score of patients was found as 18.4 ± 11.3, and they were suffering from moderate depressive symptoms. According to Arizona Sexual Experiences Scale, total mean scores of males was found as 16.3 ± 5.5, and for females, it was 19.5 ± 5.3 with a statistically significant difference (P < .05). It was found that sexual dysfunction mostly had moderate to mild.
Conclusion:
Depression and sexual dysfunction are common in patients with chronic liver diseases, and their life qualities deteriorate significantly. It is anticipated that evaluation of these patients in terms of psychological issues and sexual dysfunction will increase their quality of life during the organ waiting period and affect their well-being post-transplant.
Keywords: Quality of life, depression, sexual dysfunction, liver failure, liver transplantation
Introduction
Chronic diseases such as chronic liver disease negatively impact quality of life (QoL)1-3 Liver transplantation is the only option for patients with end-stage liver disease (ESLD). According to 2019 statistics from the Turkish Ministry of Health, 2141 patients are on the waiting list for liver transplantation (LT) in Turkey. The average waiting time for a suitable donor is currently about 5 years, and 15-18% of these patients die while waiting for transplantation.4 Patients with ESLD waiting for LT also experience health problems, as well as psychosocial issues and sexual dysfunction (SD).3
Important psychosocial factors that affect QoL are anxiety and depression. It has been shown in many studies that depression is seen in the majority of patients with ESLD, and the Beck Depression Inventory (BDI) scale is frequently used in the evaluation.3,5-8 Patients who suffer from these mental health conditions before LT report a lower QoL.3,5,6,9 In addition, these disorders are risk factors for mortality after LT.5,7 Several standard instruments are used to evaluate QoL, of which the short form-36 (SF-36) health survey is the most widely used.7 However, one drawback of the SF-36 is that it does not include subdomains related to sexual function.
Sexual function is a very important parameter in the evaluation of QoL, as it has been shown that SD in transplant patients is associated with increased depression and decreased QoL10-12; however, it is often not assessed in patients waiting for LT. The Arizona Sexual Experiences Scale (ASEX), a quick self-administered and easy-to-understand questionnaire developed to detect and monitor SD in depressed patients, is used to assess SD.13-15 Despite the potential impact of SD on QoL, insufficient information has been reported in patients awaiting LT.
It is critical to accurately identify and manage psychosocial problems and SD in patients and to optimize the QoL and transplant outcomes. Thus, this study evaluated the QoL and the presence of SD and depression in patients awaiting LT.
Materials and Methods
This was a cross‐sectional study. A total of 74 patients from Başkent University Ankara Hospital (Turkey), who were registered for LT on the list of the National Organ and Tissue Transplantation Coordination Center of Ministry of Health between 2015 and 2018, were examined. Prior to the study, informed consent was obtained from all patients. This study was approved by the Ethics Committee of Başkent University (Approval No. KA12/256) in accordance with the guidelines and the Declaration of Helsinki of 2013 on research involving human subjects. A total of 56 of 74 patients on the LT waiting list, who volunteered for the study and between 18 and 64 years of age, were included in the study. Demographic data of patients, etiology, duration of disease, and waiting time on the transplant list were recorded. In chronic liver disease, indices such as Child-Pugh and Model for End-Stage Liver Disease (MELD) score were used to express the severity of the disease.16 It was expressed as A, B, C in the Child-Pugh score, and a formula was calculated in the MELD score. The Child-Pugh and MELD scores were calculated from the patients’ records. The data were collected by face-to-face interviews between the physician and the patient using the following instruments: SF-36, BDI, and ASEX.
Instruments
Short Form-36:
Short Form-36 is one of the most widely used scales used to measure QoL. It was first developed by Ware and Sherbourne in 1992,17 and a validity and reliability study of the Turkish adaptation was conducted in 1999.18 The questionnaire is used in clinical trials, to evaluate individuals with chronic diseases, and in community health assessments. It is a self-evaluation questionnaire, consisting of 36 questions scored between 0 and 100: 0 indicates poor health and 100 indicates good health. The second question of the survey includes perception of change in health in the last 12 months; other questions are evaluated considering the last 4 weeks. The SF-36 consists of 8 subscales and measures health-related QoL domains: physical functioning, role physical (RP), role emotional (RE), bodily pain, general health (GH), vitality/energy/fatigue, social functioning, and mental health. Only one total score cannot be calculated. The summary measure of physical and mental dimensions, physical composite score (PCS), and mental composite score (MCS) are obtained by adding the scores from questions containing the subscales of the SF-36 QoL scale.17,18
Beck Depression Inventory:
The BDI was developed by Beck et al. in 1961 to measure the behavioral findings of depression in adolescents and adults. It is designed to measure the severity of depression, monitor changes with treatment, and identify disease.19 It is used frequently because it is easy for patients to fill out, has a simple language, and is easy to score. In addition, the correlation between BDI and other depression scales is quite high.20 The validity and reliability of this scale in Turkish have been confirmed.21 Depression-specific behaviors and symptoms are defined by a series of sentences, and each sentence is numbered from 0 to 3. It consists of 21 items, and the items are ranked from mild to severe. Patients are asked to mark the expression that best describes their current situation, and the result is obtained by summing the items. It is interpreted as 0-9 = minimal, 10-16 = mild, 17-29 = moderate, and 30-63 = severe.
Arizona Sexual Experiences Scale:
The ASEX is a self-reported scale consisting of 5 questions. It is designed to evaluate 5 main questions, each representing 1 domain: sexual drive, arousal, penile erection/vaginal lubrication, ability to reach orgasm, and orgasm satisfaction. Male and female forms of ASEX differ only in the question related to erection/wetting. This scale enables the rapid detection of SD.14 A Turkish validity and reliability study was done by Soykan.13 Each question is scored between 1 and 6. Low scores reflect improved sexual function, and high scores reflect SD, which is defined as a total ASEX score ≥ 19, any 1 item with a score ≥ 5 or any 3 items with a score ≥ 4.
Statistical Analysis
For descriptive statistics related to continuous data, we provided mean, standard deviation, median, minimum, maximum values for discrete data, and we present percentages. The Shapiro–Wilk test was used to analyze the normal distribution of the data. t-Test statistics was used to compare the normally distributed data between 2 groups, and the Mann–Whitney U test was used to compare the non-normally distributed data in 2 groups. The chi-square and Fisher’s exact tests were used for group comparisons (cross tables) of nominal variables. The relationship between scale scores was examined using Pearson’s correlation coefficient/Spearman’s rank correlation coefficient. Data analyses were performed with SPSS (version 21.0: IBM Corp., Armonk, NY, USA). P < .05 was considered statistically significant.
Results
Of the transplant candidates who participated in the study, 64.3% were males, and the mean age was 46.1 ± 13.6 years. The mean age was 46.6 ± 14.2 years for females, and there was no difference between the mean age of women and men (P = .905). The most common etiology (37.5% each) was hepatitis B virus and cryptogenic cirrhosis, and the vast majority of patients (64.3%) were in Child-Pugh class B. The median duration of the disease was 5 (1-13) years, and the median waiting time on the transplant list was 27 (1-31) months. Patients’ demographic and clinical data are presented in Table 1.
Table 1.
Patients’ Demographic and Clinical Data
| Mean ± Std | Median (Min-Max) | |
|---|---|---|
| Age | 46.3 ± 13.7 | 50.5 (18-64) |
| Disease duration (year) | 5.1 ± 3.1 | 5 (1-13) |
| Waiting time (month) | 22.8 ± 9.8 | 27 (1-31) |
| Child-Pugh score | 7.4 ± 1.6 | 7 (5-12) |
| MELD score | 13.3 ± 4.0 | 13 (7-25) |
| n | % | |
| Sex | ||
| Female | 20 | 35.7 |
| Male | 36 | 64.3 |
| Child-Pugh class | ||
| A | 14 | 25.0 |
| B | 36 | 64.3 |
| C | 6 | 10.7 |
| Etiology | ||
| HBV | 14 | 25.0 |
| HBV + HCC | 4 | 7.1 |
| HBV + HDV | 3 | 5.4 |
| HCV | 2 | 3.6 |
| Cryptogenic | 21 | 37.5 |
| Other | 12 | 21.4 |
Std, standard deviation; Min, minimum; Max, maximum; MELD, model for end-stage liver disease; HBV, hepatitis B virus; HDV, hepatitis delta virus; HCV, hepatitis C virus; HCC, hepatocellular carcinoma.
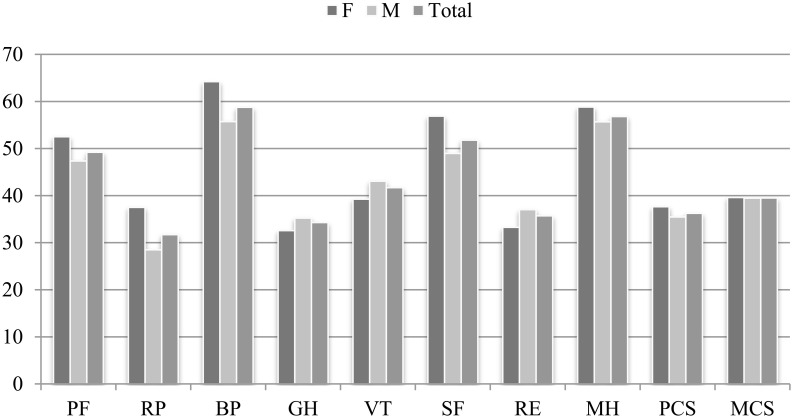
Because the SF-36 scale does not have a single total result, the values of all subgroups, summary of the 2 main items, and the results of the SF-36 scale in men and women are shown in Figure 1. There were no differences between female and male scores of the SF-36 scale (P > .05). There was no relationship between the disease duration, MELD and Child-Pugh scores or the subscale scores of the SF-36 scale. A positive correlation was found between age and GH subscale scores (r = 0.288, P < .05). No correlation was found between the other subscale scores.
Figure 1.
Short Form-36 scores of females, males, and total. PF, physical functioning; RP, role physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role emotional; MH, mental health; PCS, physical composite score; MCS, mental composite score.
The BDI results showed that 76.8% of the LT candidates suffer from depression. Most of the patients (37.5%) had moderate BDI scores. Moderate depression was detected in 7 females (35.0%) and 14 males (38.9%); 25.0% had mild depression symptom and 14.3% showed signs of severe depression. There were no differences between female and male BDI results (P > .05) (Table 2).
Table 2.
Patients’ BDI Results
| n | Mean ± Std | Statistics* | P | |
|---|---|---|---|---|
| BDI | ||||
| Female | 20 | 18.3 ± 13.2 | X2 = 0.291 | 1.000 |
| Male | 36 | 18.2 ± 10.9 | ||
| Minimal | 13 | 4.2 ± 2.6 | ||
| Mild | 14 | 13 ± 1.6 | ||
| Moderate | 21 | 22.7 ± 3.6 | ||
| Severe | 8 | 38.4 ± 8.4 | ||
*Fisher’s exact test; Std, standard deviation.
There were no relationships among patient age, disease duration, MELD score, and BDI score (P > .05). However, a positive correlation was found between Child-Pugh score and BDI (r = 0.323, P < .05). Patients with higher depressive score on the BDI scale showed lower scores in all evaluated QoL items in the SF-36. A negative correlation was found between BDI scores and scores of the SF-36 scale (P = .000), with the exception of the RE scores.
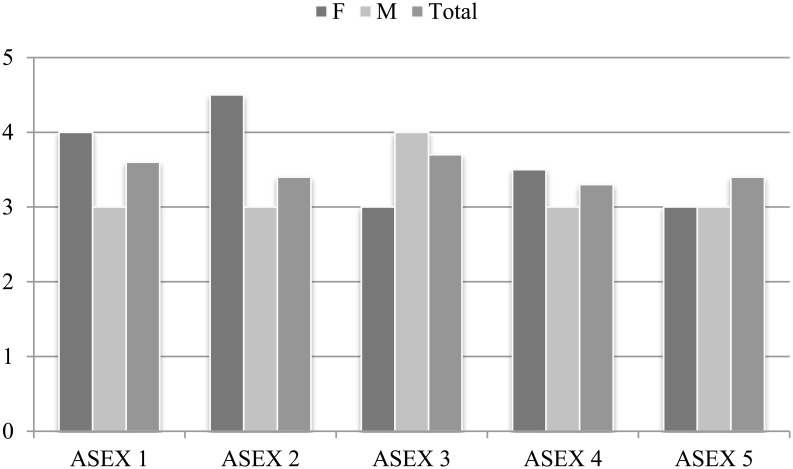
Regarding ASEX, two 18 year-old patients did not complete this scale. Arizona Sexual Experiences Scale evaluation was made for each question as ASEX 1, 2, 3, 4, 5 and ASEX total score. The mean ± Std values of these scores were 3.59 ± 1.57, 3.44 ± 1.49, 3.72 ± 1.50, 3.26 ± 1.35, 3.37 ± 1.19, and 17.39 ± 5.96, respectively. The total mean ASEX scores of females and males were 19.56 ± 5.34 and 16.31 ± 5.47, respectively, with a statistically significant difference between scores (P < .05). The total ASEX score of females was significantly higher than that of males. The results are illustrated in Figure 2. Sexual drive, arousal, and ability to reach orgasm were more common in female patients, and penile erectile dysfunction was the most common SD in male patients.
Figure 2.
Arizona Sexual Experiences Scale scores. F, female; M, male.
There was no correlation between MELD score and total ASEX score (r = −0.234, P = .089). However, a positive correlation was found between the BDI and total ASEX score (r = 0.614, P = .000), and a negative correlation was found between 2 main items of the SF-36 (PCS and MCS) and total ASEX score (r = −0.410, P = .002; r = −0.357, P = .008; respectively). For total ASEX score as the dependent variable in the regression model, where independent variables were MELD score, BDI, PCS, and MCS, the determining factors were MELD score and BDI (r² = 0.492, F = 11.884, P = .000). When the other variables were kept constant, the MELD score increased by 1 point for every 0.4-point decrease in ASEX score, and the BDI increased by 1 point for every 0.3-point decrease in ASEX score (P < .05, for all) (Table 3).
Table 3.
Multiple Regression Results for ASEX
| Parameter | B | Std. Error | 95 % CI | P | |
|---|---|---|---|---|---|
| MELD Score | −0.358 | 0.145 | −0.649 | −0.067 | .017 |
| BDI | 0.339 | 0.070 | 0.198 | 0.480 | .000 |
| Waiting time | 0.106 | 0.059 | −0.013 | 0.225 | .081 |
| PCS | 0.008 | 0.069 | −0.131 | 0.146 | .912 |
| MCS | 0.031 | 0.070 | −0.109 | 0.172 | .654 |
MELD, model for end-stage liver disease; BDI, Beck Depression Inventory; PCS, physical composite score; MCS, mental composite score; Std. Error, standard error
A statistical significance of P > .05 is highlighted in bold.
SD was found in 26 (48.1%) patients. There were no differences between the SD rates of females and males (P > .05) (Table 4). In addition, the mean age of those with and without SD was 48.2 ± 13.6 and 46.5 ± 12.09, respectively, and no effect of age on SD (p=0.630) was found.
Table 4.
Distribution of SD by Sex According to ASEX
| Female, n (%) | Male, n (%) | Statistics* | P | |
|---|---|---|---|---|
| ASEX - SD | ||||
| Negative | 8 (44.4) | 20 (55.6) | X2 = 0.593 | .441 |
| Positive | 10 (55.6) | 16 (44.4) |
*Fisher’s exact test; ASEX, Arizona Sexual Experiences Scale; SD, sexual dysfunction.
There was a statistically significant difference between MELD scores and BDI results of patients with SD (P < .05; P < .001; respectively). The scores of patients with SD were significantly lower than those of patients without SD. Beck Depression Inventory scores of patients with SD were significantly higher than those without SD. While there was no difference in the duration of the disease in patients with and without SD (P > 0.05), it was observed that the waiting time on the transplant list was longer in patients with SD (P = .015) (Table 5).
Table 5.
Comparison of Age, MELD Score, Child-Pugh Score, BDI Score and Disease Duration of Patients With and Without SD
| SD (–) (n = 28) | SD (+) (n = 26) | Statistics* | P | |
|---|---|---|---|---|
| Mean ± Std | Mean ± Std | |||
| Age | 46.5 ± 12.1 | 48.2 ± 13.6 | U = 315.0 | .396 |
| Child-Pugh score | 7.8 ± 1.8 | 7.2 ± 1.4 | U = 305.0 | .294 |
| MELD score | 14.67 ± 4.2 | 12.2 ± 3.5 | U = 241.5 | .033 |
| BDI | 12.2 ± 8.0 | 24.62 ± 12.0 | U = 140.0 | .000 |
| Disease duration (year) | 5.8 ± 3.4 | 4.3 ± 2.8 | U = 266.0 | .086 |
| Waiting time (month) | 19.7 ± 10.3 | 26.2 ± 8.4 | U = 229.5 | .015 |
* Mann–Whitney U test; SD, sexual dysfunction; Std, standard deviation; MELD, model for end-stage liver disease; BDI, Beck Depression Inventory.
A statistical significance of P > .05 is highlighted in bold.
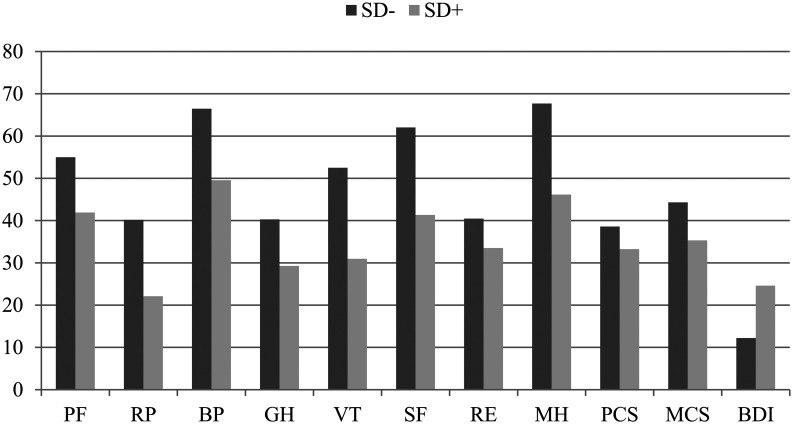
There was a statistically significant difference between PCS and MCS scores of patients with and without SD (P < .05). The scores of both were significantly lower in patients with SD. There were no differences in RP, GH, and RE scores between patients with and without SD (P > .05) (Figure 3).
Figure 3.
Beck Depression Inventory and SF-36 scores. PF, physical functioning; RP, role physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role emotional; MH, mental health; PCS, physical composite score; MCS, mental composite score; SD, sexual dysfunction.
According to logistic model created with independent variables that affected SD, only MELD score and BDI results were significant. The MELD score and BDI were associated with SD. A 1-point increase in MELD was associated with a 1.3-fold decrease in SD, and a 1-point increase in BDI score was associated with a 1.2-fold increase in SD (Table 6).
Table 6.
Independent Risk Factors Affecting SD and Multivariate Logistic Regression Results
| Parameter | B | Std. Error | OR | 95% CI | P | |
|---|---|---|---|---|---|---|
| MELD score | −0.275 | 0.110 | 1.317 | 1.061 | 1.633 | .012 |
| BDI | 0.161 | 0.046 | 1.174 | 1.072 | 1.286 | .001 |
MELD, model for end-stage iver Disease; BDI, Beck Depression Inventory; SD, sexual dysfunction; OR, odds ratio.
A statistical significance of P > .05 is highlighted in bold.
Discussion
Most patients with ESLD have difficulty performing physical activities, have limited social lives, and sometimes experience fatigue and depression due to the disease. Due to uncertainties about the future, they have difficulty dealing with the disease and their QoL is affected. It is thought that as the disease duration increases, patients experience more deterioration of their QoL as they have to experience the limitations of having chronic disease for a longer period of time.22,23 Cadaveric organ transplantation is insufficient in Turkey, which prolongs the waiting period for transplantation, leading to deterioration of patients’ QoL and even causing patients to lose their lives. The wait time for transplantation is generally a very stressful period that negatively affects QoL.23-25 These patients suffer from problems in their work performance, social life, and sexual function. As a result, patients often isolate themselves from the community, which contributes to a lower QoL.23 Most patients listed for LT have ESLD associated with a marked decrease in their QoL and psychosocial well-being.24
Patients with chronic diseases have a low QoL. Although a healthy sex life is also part of the QoL, sexual function is generally neglected when evaluating QoL, although it significantly decreases in patients with liver failure, usually due to depression and sexual SD.2,8,10,12 The effects of ESLD on sexual functions are complex and are often ignored in the context of chronic disease and transplantation assessment. A previous study reported that SD can continue after transplantation in both men and women.12
In this study, we found marked SD, which has not been previously found in patients with hepatic impairment. We also documented depression and QoL deterioration. We attributed depression and anxiety to the negative effects of the chronic disorder. Moreover, there is a known relationship between depression–anxiety and SD. While women often have decreased libido and arousal, men mostly have erectile dysfunction.11,26 In logistic regression analyses, depression was associated with SD, which increased by 1.2-fold with a 1-point increase in BDI score. Sexual dysfunction is a multifactorial condition that is influenced by psychogenic, physical, and social factors.15,27,28 Sexual dysfunction in men and women in chronic liver disease is complicated because it is caused by many different factors such as drug–alcohol use, changes in the hypothalamic–pituitary–gonadal axis, and social and psychological problems arising from the transplantation process.15,28,29 The liver plays an important role in the metabolism of sex hormones and the optimization of gonadal function. Therefore, it is stated that SD in those with ESLD, hyperestrogenism, and decreased testosterone in men, and suppression of the hypothalamic–pituitary–gonadal axis in women are the main factors.27,28 However, epidemiological data are relatively insufficient, and studies do not have sufficient homogeneity. Psychological status appears to play a key role in SD after liver transplantation. Post-liver transplant depression is the main risk factor for SD in both male and female patients.10 The results of our study also indicate that SD is related to a decrease in QoL as well as depression and anxiety.
Although some studies have reported that there is no correlation between MELD score and QoL,15,30 others have described a trend toward high anxiety scores and high post-transplant QoL due to low MELD scores.8,23,31 Benzing et al.8 found that the knowledge of having a life-threatening disease and the need for LT lead to higher levels of anxiety and depression and poor QoL. In this study, although no correlation was found between MELD score and the scales, the MELD score was associated with ASEX scores in regression analyses: as the MELD score increases, the ASEX score decreases. Accordingly, QoL can be increased by improving SD before LT when the health of patients with low MELD scores is less impaired.
Patients on the LT waiting list with a higher depression score were associated with a significant decrease in QoL. However, half of the patients had SD. In our study, we accepted 19 as cut-off value in ASEX scoring, which is internationally accepted. In another study conducted in our country, patients with chronic renal failure and undergoing hemodialysis, the ASEX score cut-off value of the scale was evaluated as 11.18 This give rise to thought about the possibility of higher than what is available rate of having SD in our patients.
It appears that SD and depression affect each other. The data presented here suggest that adequate management of depressive symptoms in the early period may treat SD and increase QoL. In addition, maintaining the QoL together with the patient’s sexual life may be a protective factor in the development of depressive symptoms throughout the waiting period of the transplant. Although SD is thought to improve in many patients with the recovery of hormonal disruptions associated with chronic liver disease after transplantation,28 the effect of LT on SD is still unclear.10 Our findings suggest that patients waiting on the LT list should routinely question their sexual function, which plays an important role in determining the QoL. Thus, they can make a positive contribution to the pre-transplant and even post-transplant treatment of these patients.
With this important finding regarding the ASEX scores and the clinical SD occurrence in our patients on the LT waiting list, an important limitation of our study was the lack of the post-transplant reevaluation of the same cohort of patients. Undoubtfully, if performed, this evaluation surely would have added a great value to this study. It was not possible because of the really long and sometimes exhausting waiting durations on the transplant list in our country.
In conclusion, depression and SD are associated with a significant decrease in QoL of patients waiting for LT. Since sexual function is one of the factors in the evaluation of QoL, it is clear that the sexual function of patients waiting on the transplant list should also be considered. Detecting and controlling the SD of patients in the early period will be effective in increasing both pre-transplant and post-transplant QoL. Although depression is among the causes of SD, its coexistence is also common. Therefore, we believe that informing health professionals in terms of taking sexual history and being aware of the potential causes of SD and evaluating them for depression at each follow-up during the waiting period for transplantation will be important factors in increasing the QoL of patients with ESLD. Adequate management of depressive symptoms can improve QoL and SD. Increasing the QoL of patients will both positively affect the course of the disease and will contribute to the adaptation of the patients to treatment. National studies on sexual function in liver transplant candidates and recipients and studies evaluating the long-term consequences of transplantation on sexual function in men and women affected by chronic liver disease are limited. Therefore, future research on this subject is required.
Funding Statement
The authors declared that this study has received no financial support.
Footnotes
Ethics Committee Approval: This study was approved by the Ethics Committee of Başkent University (Approval No. KA12/256) in accordance with the guidelines and the Declaration of Helsinki of 2013.
Informed Consent: Prior to the study, informed consent was obtained from all patients.
Peer Review: Externally peer-reviewed.
Author Contributions: Study Concept and design of the study: C.F., A.A., H.S.; Data acquisition: C.F., A.A., M.K.; Data analysis and interpretation: C.F., A.A., M.K., H.S.; Critical revisions for important intellectual content: H.S., S.Y., G.M., M.H.; Final approval of the version to be submitted: C.F., A.A., M.K., H.S., S.Y., G.M., M.H.
Conflict of Interest: The authors have no conflict of interest to declare.
References
- 1. . Aydemir O, Psikiyatrisi K-L, Kalitesi Y. Consultation-liaison psychiatry and quality of life. Turk Klin J Med Sci. 2006;47:85–88.. [Google Scholar]
- 2. . Orr JG, Homer T, Ternent L, et al. Health related quality of life in people with advanced chronic liver disease. J Hepatol. 2014;61(5):1158–1165.. 10.1016/j.jhep.2014.06.034) [DOI] [PubMed] [Google Scholar]
- 3. . Saracino RM, Jutagir DR, Cunningham A, et al. Psychiatric comorbidity, health-related quality of life, and Mental Health Service Utilization Among Patients Awaiting Liver Transplant. J Pain Symptom Manag. 2018;56(1):44–52.. 10.1016/j.jpainsymman.2018.03.001) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. .T. C. Organ Transplantation Coordination Statistics of the Ministry of Health. Available at: https://organkds.saglik.gov.tr/dss/publıc/wl_liver.aspx, Accessed January 10, 2018. [Google Scholar]
- 5. . Rogal SS, Dew MA, Fontes P, DiMartini AF. Early treatment of depressive symptoms and long-term survival after liver transplantation. Am J Transplant. 2013;13(4):928–935.. 10.1111/ajt.12164) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. . Febrero B, Ramírez P, Martínez-Alarcón L, et al. Quality of life and group psychological intervention in patients with cirrhosis on liver transplant waiting list. Transplant Proc. 2018;50(9):2626–2629.. 10.1016/j.transproceed.2018.04.013) [DOI] [PubMed] [Google Scholar]
- 7. . Dew MA, Rosenberger EM, Myaskovsky L, et al. Depression and anxiety as risk factors for morbidity and mortality after organ transplantation: a systematic review and meta-analysis. Transplantation. 2015;100(5):988–1003.. 10.1097/TP.0000000000000901) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. . Benzing C, Krezdorn N, Förster J, et al. Health-related quality of life and affective status in liver transplant recipients and patients on the waiting list with low MELD scores. HPB. 2016;18(5):449–455.. 10.1016/j.hpb.2016.01.546) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. . Corruble E, Barry C, Varescon I, et al. Report of depressive symptoms on waiting list and mortality after liver and kidney transplantation: a prospective cohort study. BMC Psychiatry. 2011;11:182-. 10.1186/1471-244X-11-182) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. . Burra P. Sexual dysfunction after liver transplantation. Liver Transpl. 2009;15(suppl 2):S50–S56.. 10.1002/lt.21899) [DOI] [PubMed] [Google Scholar]
- 11. . Onghena L, Develtere W, Poppe C, et al. Quality of life after liver transplantation: state of the art. World J Hepatol. 2016;8(18):749–756.. 10.4254/wjh.v8.i18.749) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. . Sorrell JH, Brown JR. Sexual functioning in patients with end-stage liver disease before and after transplantation. Liver Transpl. 2006;12(10):1473–1477.. 10.1002/lt.20812) [DOI] [PubMed] [Google Scholar]
- 13. . Soykan A. The reliability and validity of Arizona Sexual Experiences Scale in Turkish ESRD patients undergoing hemodialysis. Int J Impot Res. 2004;16(6):531–534.. 10.1038/sj.ijir.3901249) [DOI] [PubMed] [Google Scholar]
- 14. . McGahuey CA, Gelenberg AJ, Laukes CA, et al. The Arizona Sexual Experience Scale (ASEX): reliability and validity. J Sex Marital Ther. 2000;26(1):25–40.. 10.1080/009262300278623) [DOI] [PubMed] [Google Scholar]
- 15. . Lin CF, Juang YY, Wen JK, Liu CY, Hung CI. Correlations between sexual dysfunction, depression, anxiety, and somatic symptoms among patients with major depressive disorder. Chang Gung Med J. 2012;35(4):323–331.. 10.4103/2319-4170.106138) [DOI] [PubMed] [Google Scholar]
- 16. . Peng Y, Qi X, Guo X. Child-Pugh versus score for the assessment of prognosis in liver cirrhosis: a systematic review and meta-analysis of observational studies. Med. 2016;95(8):e2877. 10.1097/MD.0000000000002877) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. . Ware JE, Sherbourne CD.The Maryland Ornithological Society. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483.. 10.1097/00005650-199206000-00002) [DOI] [PubMed] [Google Scholar]
- 18. . Koçyiğit H, Aydemir O, Fişek G, et al. Kısa form-36 (SF-36)’nın Türkçe versiyonunun güvenilirliği ve geçerliliği. [Reliability and validity of the Turkish version of short form-36 (SF-36)]. İlaç Tedavi Derg. 1999;12:102–106.. [Google Scholar]
- 19. . Beck AT. A systematic investigation of depression. Compr Psychiatry. 1961;2:163–170.. 10.1016/s0010-440x(61)80020-5) [DOI] [PubMed] [Google Scholar]
- 20. . Kılınç S, Torun F. Türkiye’de klinikte kullanılan depresyon değerlendirme ölçekleri. Dirim Tıp Gazetesi. 2011;86:39–47.. [Google Scholar]
- 21. . Hisli N. Beck Depresyon Envanterinin gecerliligi uzerine bit calisma (A study on the validity of Beck Depression Inventory.). Psikhol Derg. 1988;6:118–122.. [Google Scholar]
- 22. . Gutteling J, Man R, Busschbach JJV, Darlington A-S. Health-related quality of life and psychological correlates in patients listed for liver transplantation. Hepatol Int. 2008;1:437–443.. 10.1007/s12072-007-9035-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. . Santos GG, Gonçalves LC, Buzzo N, et al. Quality of life, depression, and psychosocial characteristics of patients awaiting liver transplants. Transplant Proc. 2012;44(8):2413–2415.. 10.1016/j.transproceed.2012.07.046) [DOI] [PubMed] [Google Scholar]
- 24. . Goetzmann L, Wagner-Huber R, Klaghofer R, et al. Waiting for a liver transplant: psychosocial well-being, spirituality, and need for counselling. Transplant Proc. 2006;38(9):2931–2936.. 10.1016/j.transproceed.2006.08.171) [DOI] [PubMed] [Google Scholar]
- 25. . Jurado R, Morales I, Taboada D, et al. Coping strategies and quality of life among liver transplantation candidates. Psicothema. 2011;23(1):74–79.. [PubMed] [Google Scholar]
- 26. . Burra P, Germani G. Long-term quality of life for transplant recipients. Liver Transpl. 2013;19(suppl 2):S40–S43.. 10.1002/lt.23725) [DOI] [PubMed] [Google Scholar]
- 27. . Neong SF, Billington EO, Congly SE. Sexual dysfunction and sex hormone abnormalities in patients with cirrhosis: review of pathogenesis and management. Hepatology. 2019;69(6):2683–2695.. 10.1002/hep.30359) [DOI] [PubMed] [Google Scholar]
- 28. . Magro JTJ, Mendes KDS, Galvão CM. Sexual aspects of liver transplant candidates and recipients: evidence available in the literature. Rev Lat Am Enfermagem. 2018;26:e3033. 10.1590/1518-8345.2744.3033) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. . Burra P, Germani G, Masier A, et al. Sexual dysfunction in chronic liver disease: is liver transplantation an effective cure? Transplantation. 2010;89(12):1425–1429.. 10.1097/TP.0b013e3181e1f1f6) [DOI] [PubMed] [Google Scholar]
- 30. . Derck JE, Thelen AE, Cron DC, et al. Quality of life in liver transplant candidates: frailty is a better indicator than severity of liver disease. Transplantation. 2015;99(2):340–344.. 10.1097/TP.0000000000000593) [DOI] [PubMed] [Google Scholar]
- 31. . Togashi J, Sugawara Y, Akamatsu N, et al. Quality of life after adult living donor liver transplantation: a longitudinal prospective follow-up study. Hepatol Res. 2013;43(10):1052–1063.. 10.1111/hepr.12060) [DOI] [PubMed] [Google Scholar]