Editor,
Intravascular tissue sampling may be percutaneous, endovascular, or surgical [1]. Small-volume transvenous biopsies have been described using 5.5- and 7-French biopsy forceps [1]. Small volume sampling, however, may result in lower diagnostic yields and be limited by crush artifact. The ClotTriever thrombectomy system (Inari Medical; Irvine, CA) has been used for the extraction of large-volume thrombotic and embolic materials in peripheral and central veins [2]. This report describes the results of histopathologic analysis on specimens collected via ClotTriever-mediated thrombectomy. Institutional review board approval was obtained for preparation of this report.
Twenty-six consecutive patients (14 males, 12 females; mean age 54.4 ± 15.3 years) underwent ClotTriever-mediated thrombectomy for symptomatic venous thrombosis with endovascular tissue samples sent for pathologic analyses. Twenty-three patients presented with swelling, fifteen with pain, two with fever, and one with respiratory failure. Fifteen patients underwent thrombectomy of the inferior vena cava or lower extremity deep veins, and eleven patients underwent thrombectomy of the thoracic central veins or upper extremity deep veins. Technical success, described as extraction of intravascular materials adequate for desired pathologic and/or microbiologic analysis, was obtained in all patients. There were no intraprocedural adverse events. Of the removed samples, seventeen were benign (i.e., bland thrombus of various chronicity), seven were malignant, and two were infectious. Malignancies included non-small cell adenocarcinoma from lung primary (n = 2), EBV + large B-cell lymphoma (n = 1), papillary thyroid carcinoma (n = 1) [3], acute T-cell lymphoblastic leukemia (n = 1), follicular lymphoma (n = 1), and colorectal adenocarcinoma (n = 1) [4]. Infections were due to Staphylococcus aureus (n = 2). 2/7 of malignant thrombus samples demonstrated enhancement on computed tomography (CT) or magnetic resonance-based imaging studies within thirty days of the thrombectomy procedures. Clinical success, described as resolution of presenting systems, was achieved in all patients.
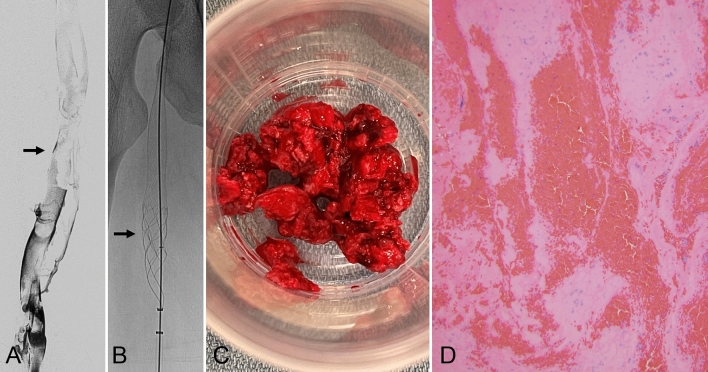
Benign Pathology Example
A 25-year-old man with coronavirus-19 infection presented with left lower extremity swelling and pain. CT, venous duplex ultrasound, and lower extremity venography (Fig. 1A) showed acute deep venous thrombosis extending from the left popliteal vein to the iliocaval confluence. He underwent left lower extremity thrombectomy using the thrombectomy device (Fig. 1B), followed by stent reconstruction of the left common iliac vein with a 16 mm × 80 mm Abre (Medtronic; Dublin, Ireland) venous stent. Histopathologic analysis demonstrated bland thrombus with early organization (Fig. 1C, D), confirming benign venous occlusive disease.
Fig. 1.
25-year-old man with acute left lower extremity swelling. A Ascending venography of the left lower extremity demonstrating acute deep venous thrombosis (black arrow). B ClotTriever (black arrow) thrombectomy of the left lower extremity was performed. C Photograph of thrombus. D Hematoxylin and eosin-stained section, 100 × magnification, showing alternating zones of red blood cells and fibrin, typical of thrombus
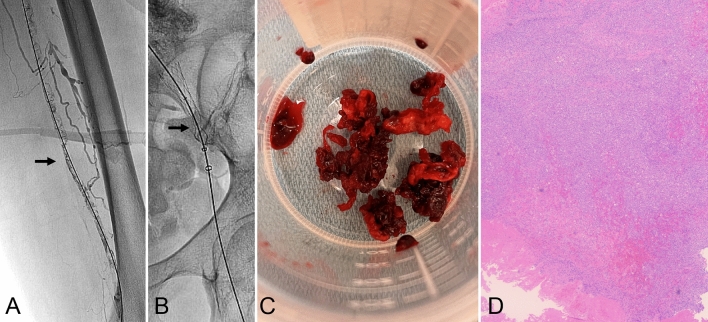
Malignant Pathology Example
A 65-year-old woman with diffuse large B cell lymphoma, in remission, presented with left leg swelling. Computed tomography and lower extremity venography (Fig. 2A) demonstrated left pelvic sidewall lymphadenopathy resulting in compression of the left common iliac and external iliac veins with associated deep venous thrombosis in the pelvis and thigh. She underwent left lower extremity thrombectomy using the thrombectomy device (Fig. 2B), followed by stent reconstruction with a 14-mm × 80-mm Abre (Medtronic) venous stent and a 12-mm × 90-mm Wallstent (Boston Scientific; Marlborough, MA). Histopathologic analysis revealed sheets of EBV + B-cells consistent with relapsed large B cell lymphoma (Fig. 2C, D).
Fig. 2.
65-year-old woman with a history of diffuse large B-cell lymphoma, thought to be in remission, presented left leg swelling. A Ascending venography showing acute deep venous thrombosis (black arrow). B Fluoroscopic spot image of the coring element of the ClotTriever device (black arrow) at the level of the external iliac vein. C Photograph of the gross specimen following thrombectomy. D Hematoxylin and eosin-stained slides (4 × magnification) demonstrating thrombus with foci consisting of sheets of large, atypical lymphocytes. The cells stained positive by PAX5 (B cell marker) and EBER for EBV (images not shown), consistent with involvement of the thrombus by EBV + large B cell lymphoma
Infectious Pathology Example
A 26-year-old man with end-stage renal disease on hemodialysis via a left internal jugular vein tunneled central venous catheter presented with fever and was found to have methicillin-susceptible Staphylococcus aureus bacteremia. Prompt catheter removal and nafcillin intravenous antibiotic therapy failed to resolve the bacteremia. Computed tomography and upper extremity venography (Fig. 3A) demonstrated thrombi within the left brachiocephalic vein and superior vena cava. In an effort to provide source control for his persistent bacteremia, the patient underwent thrombectomy using the thrombectomy device (Fig. 3B). Thrombus culture yielded Staphylococcus aureus, matching prior blood cultures (Fig. 3C, D). Blood cultures drawn on day one following thrombectomy showed no growth.
Fig. 3.
A 26-year-old man with persistent bacteremia. A Central venography was performed through left brachial vein access demonstrating filling defects in the left brachiocephalic and superior vena cava (black arrow). B Fluoroscopic spot image demonstrating the coring element of the ClotTriever device (black arrow) deployed in the central portion of the superior vena cava. C Photograph of the ClotTriever immediately following initial thrombectomy with friable, purulent material. D Hematoxylin and eosin-stained section, 100 × magnification, showing intermixed blood and fibrin with some macrophage infiltrate in the upper left, likely representing features of very early organization
ClotTriever-mediated thrombectomy has been approved for the treatment of venous thrombosis [2–4]. It may prove difficult to differentiate benign, malignant, and infectious thrombi on imaging alone, and conventional percutaneous needle biopsy may lead to non-diagnostic sampling or injury to the adjacent neurovascular structures. This report demonstrates that large-volume specimens obtained via the thrombectomy device may provide diagnostic information regarding benign, malignant, or infectious etiologies with no additional time, materials, or risks. Additionally, while catheter-directed thrombolysis of septic thrombophlebitis may be contraindicated for the fear of overwhelming sepsis, the thrombectomy device may offer both diagnostic and therapeutic benefits via en bloc extraction of the infected thrombi with lower risk of dissemination or endotoxin release. Further studies are warranted to establish the effectiveness of ClotTriever-mediated sampling as the primary modality for endovascular biopsy.
Acknowledgements
Institutional review board approval was obtained for preparation of this report. There are no additional acknowledgements.
Declarations
Conflicts of interest
E.J.M. is a scientific advisor and speaker for Biogen. J.F.B.C. is a consultant and speaker for Inari Medical, Guerbet, C. R. Bard, Argon Medical Devices, Boston Scientific, and NXT Biomedical. None of the other authors have identified a conflict of interest.
Human or Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sherk WM, Khaja MS, Majdalany BS, Saad WE, Udager AM, Cooper KJ, Williams DM. Transvenous biopsy in the diagnosis of intravascular or perivascular neoplasm: a single-center retrospective analysis of 36 patients. J Vasc Interv Radiol. 2019;30(1):54–60. doi: 10.1016/j.jvir.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Benarroch-Gampel J, Pujari A, Aizpuru M, Rajani RR, Jordan WD, Crawford R. Technical success and short-term outcomes after treatment of lower extremity deep vein thrombosis with the ClotTriever system: a preliminary experience. J Vasc Surg Venous Lymphat Disord. 2020;8(2):174–181. doi: 10.1016/j.jvsv.2019.10.024. [DOI] [PubMed] [Google Scholar]
- 3.Bertino FJ, Shin DS, Monroe EJ, Siu JJ, Tenen CC, Chick JFB. Thrombectomy of malignant thoracic central venous occlusive disease using inari ClotTriever system. J Vasc Interv Radiol. 2021;32(9):1398–1400. doi: 10.1016/j.jvir.2021.05.018. [DOI] [PubMed] [Google Scholar]
- 4.Shin DS, Abad-Santos M, Bertino FJ, Monroe EJ, Ricciotti R, Chick JFB. Percutaneous extraction of colorectal cancer metastasis involving inferior vena cava using inari clottriever thrombectomy system. Clin Imag. 2022;82:100–102. doi: 10.1016/j.clinimag.2021.11.010. [DOI] [PubMed] [Google Scholar]