Abstract
Background:
The purpose of this meta-analysis is to appraise the efficacy and safety of delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage (PTGBD) versus emergency laparoscopic cholecystectomy (ELC) for acute cholecystitis.
Methods:
The kinds of literature were searched by Web of Science, PubMed, OVID, Cochrane Library, and EMBASE between the year 2000 and 2019. RevMan 5.3 was used for meta-analysis.
Results:
Seventeen studies with 2135 participants were included in our study. Compared with the ELC group, delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage group (PTGBD group) had a significant better effect in intraoperative bleeding (P = .002), conversion rate to open surgery (P = .02), postoperative complications (P < .00001), bile leakage (P = .01), bile duct injury (P = .02), and wound infection (P = .02). There was no significant difference between the two groups in operative time (P= 32), postoperative hospital stay (P = .30), and intraperitoneal hemorrhage (P = .39). PTGBD group had a significantly longer overall hospital stay than the ELC group (P < .00001).
Conclusion:
Compared with the ELC group, the PTGBD group has several advantages, including bile duct injury, intraoperative bleeding, bile leakage, conversion rate to open surgery, postoperative complications, and wound infection. The only drawback in the PTGBD group is to lengthen the total hospital stay.
Keywords: Acute cholecystitis, laparoscopic cholecystectomy, percutaneous transhepatic gallbladder drainage, meta-analysis
Introduction
Acute cholecystitis (AC) is distension and chemical or bacterial inflammation of the gallbladder that results from obstruction of the cystic duct, usually by a gallstone.1 An increase in the incidence of AC has been reported in recent years.2 It is one of the most common diseases in the emergency department. Based on refinements in laparoscopic technique and increased surgical experience, laparoscopic cholecystectomy (LC) has replaced the traditional open cholecystectomy (OC), and become a standard therapy of cholecystitis, especially for chronic disease. For the treatment of AC, there has been controversy over the advantages of emergency LC (ELC) versus delayed surgery after gallbladder drainage, like percutaneous transhepatic gallbladder drainage (PTGBD).3-5 In 1980, PTGBD was first introduced by Radder.6 Because it has the advantages of causing minimal injury, lower complication rate, and being a simple procedure with rapid symptom relief,7 PTGBD has been widely performed as a safer substitute for ELC. There have been a lot of arguments about the safety and efficacy between PTGBD + LC and ELC for AC. The purpose of this study is to compare the outcome of delayed LC after PTGBD to ELC.
Materials and Methods
Search Strategy
We conduct this study according to the Preferred Reporting Items for Systematic Review and Meta-analysis statement. Related articles were searched by two authors in Web of Science, PubMed, OVID, Cochrane Library, and EMBASE using the following keywords: “percutaneous transhepatic gallbladder drainage,” “laparoscopic cholecystectomy,” “acute cholecystitis.” All studies were published between the years 2000 and 2019. Languages were limited to English and Chinese.
Inclusion Criteria:
(1) All patients were diagnosed with AC; (2) the PTGBD group received PTGBD before LC; (3) the ELC group underwent emergency LC without PTGBD; and (4) the PTGBD group had no severe complication during and after PTGBD.
Exclusion Criteria:
(1) Patients diagnosed with chronic cholecystitis or gallbladder cancer; (2) incomplete data; (3) duplicate studies; (4) based on animals or non-human samples and (5) case reports or reviews.
Data Extraction
Two reviewers separately performed the search, then reviewed the titles, abstracts, and full texts of all studies and extracted the following data from each eligible study. The following data were collected from each study: author, publication year, patient’s characteristic, study type, inclusion and exclusion criteria, number of subjects, and the evaluation index included operative time (minutes), intraoperative bleeding (mL), postoperative and overall hospital stay (days), conversion rate to open surgery, and postoperative complications, including bile duct injury, bile leakage, intraperitoneal hemorrhage, and wound infection.
Quality Assessment
The quality of RCT was measured by the modified Jadad method. Studies awarded four or more points were considered high-quality studies. The quality of non-randomized studies was assessed by the Newcastle–Ottawa scale (NOS),8 and more than seven stars were defined as high quality, 4–6 stars as medium quality, and <4 stars as low quality.
Statistical analysis
RevMan 5.3 was used for meta-analysis. Heterogeneity among the studies was analyzed by the Chi-square test and I 2 test. P < .05 and I 2 > 50% were considered as statistically significant heterogeneity and a random-effects model was selected. Otherwise, a fixed-effects model was selected. Dichotomous data were calculated by odds ratio (OR) and 95% confidence interval (95% CI), whereas continuous data were calculated by mean difference (MD) and 95% CI. A probability value of P < .05 was considered statistically significant. A funnel plot was used to assess publication bias.
Results
Base Characteristic
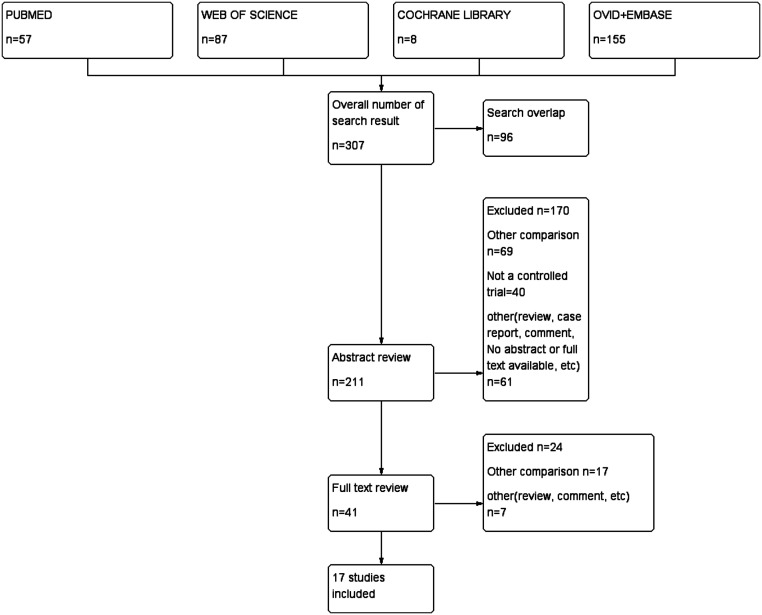
A total of 307 studies were identified, 96 studies were excluded after duplicate removal by EndNote. After examining the titles and abstracts, we excluded 170 articles because of the following reasons: Other comparison (n = 69), not a controlled trial (n = 40), case report (n = 22), guideline and consensus (n = 8), and others (n = 31). Twenty-four studies were excluded after full-text article review for the following reasons: Other comparison (n = 17) and others (n = 7). Finally, 17 articles2,7,9-23 were enrolled for analysis, including 2135 patients, 938 patients in the PTGBD group, and 1197 patients in the ELC group (Figure 1). The characteristics and baseline demographic data of the patients are listed in Table 1.
Figure 1.
Flow diagram of study screening and inclusion.
Table 1.
Characteristics of the Included Studies
| First Author | Year | Study Design | Total Cases | No. of Patients (PTGBD: ELC) | Included Outcomes | Quality |
|---|---|---|---|---|---|---|
| Jia | 2018 | Retrospective | 86 | 38:48 | a,b,c,d,e,f,g,h,i,j | 8 |
| Lee | 2017 | Retrospective | 85 | 44:41 | a,c,d,e,f, | 6 |
| Jung | 2017 | Retrospective | 294 | 128:166 | a,c,d,e,f,g,i | 6 |
| Ahmed | 2017 | RCT | 150 | 75:75 | a,b,e,f,g,h,i,j | 5 (Jadad) |
| Ni | 2015 | Retrospective | 59 | 26:33 | a,b,d,e,f | 6 |
| Na | 2015 | Retrospective | 116 | 39:77 | c,d,e,f,g,h | 7 |
| Hu | 2015 | RCT | 70 | 35:35 | a,b,c,e,f,g,i,j | 4 (Jadad) |
| Uchiyama | 2013 | Retrospective | 21 | 5:16 | a,b,c,d,e,f,j | 6 |
| Choi | 2012 | Retrospective | 103 | 40:63 | a,b,d,e,f,g,i | 6 |
| Kim | 2011 | Retrospective | 244 | 97:147 | a,c,d,e,f | 6 |
| Kim | 2009 | Retrospective | 133 | 73:60 | e,f,g,j | 8 |
| Kim | 2008 | Retrospective | 99 | 37:62 | a,c,d,e,f,g,i,j | 6 |
| Tsumura | 2004 | Retrospective | 133 | 60:73 | a,b,c,e,f,g,h,j | 6 |
| Chikamori | 2002 | Retrospective | 40 | 31:9 | a,c,d,e,g,h,i,j | 8 |
| Kim | 2018 | Retrospective | 325 | 131:194 | a,c,d,e,f,g,i | 6 |
| Yu | 2017 | Prospective | 86 | 36:50 | a,c,e,f,g,h,i | 9 |
| Karakayali | 2014 | Prospective | 91 | 43:48 | a,c,e,f,g,h,j | 8 |
Included outcomes: a, operative time; b, intraoperative bleeding; c, postoperative hospital stay; d, overall hospital stay; e, conversion rate to open surgery; f, postoperative complications; g, bile leakage; h, bile duct injury; i, intraperitoneal hemorrhage; j, wound infection.
Meta-Analysis Results
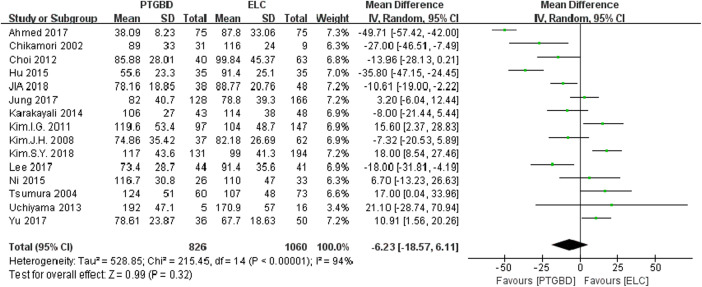
Operative Time:
The operative time was reported in 15 studies. Significant heterogeneity was found (P < .00001, I² = 94%). Therefore, the random-effects model was adopted, and there was no significant difference between the PTGBD group and ELC group [MD = –6.23, 95% CI (−18.57 to 6.11), P = .32] (Figure 2).
Figure 2.
Forest plot of the operative time between the PTGBD group and the ELC group.
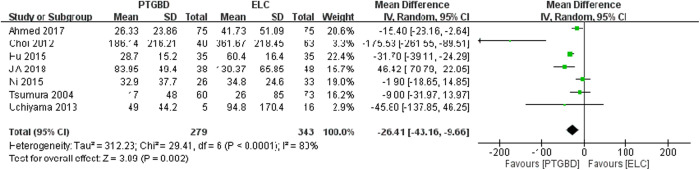
Intraoperative Bleeding:
Data for intraoperative bleeding was provided in seven studies. High heterogeneity was observed (P < .0001, I² = 80%). Therefore, the random-effects model was used. The meta-analysis showed that the amount of intraoperative bleeding in the PTGBD group was lower than the ELC group, and the difference was significant [MD = −26.41, 95% CI (−43.16 to –9.66), P = .002] (Figure 3).
Figure 3.
Forest plot of the intraoperative bleeding between the PTGBD group and the ELC group.
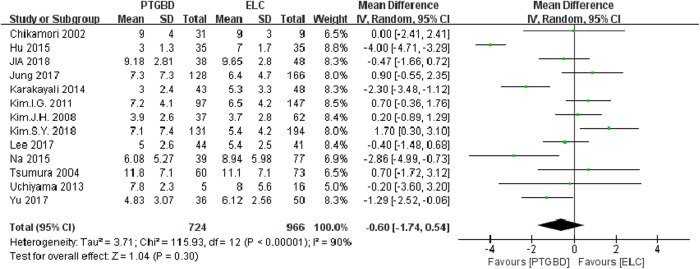
Postoperative Hospital Stay:
Thirteen studies reported the postoperative hospital stay. Due to the high heterogeneity (P < .00001, I² = 90%), the random-effects model was used, and no significant difference was found [MD = −0.60, 95% CI (−1.74 to 0.54), P = .30] (Figure 4).
Figure 4.
Forest plot of the postoperative hospital stay between the PTGBD group and the ELC group.
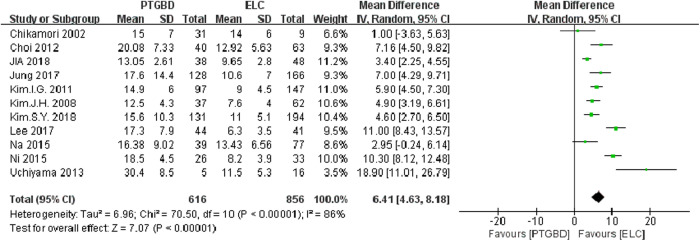
Overall Hospital Stay:
The overall hospital stay was reported in 11 studies. Heterogeneity among studies was high (P < .00001, I² = 86%), therefore the random-effects model was used. The results showed that the overall hospital stay in the PTGBD group was significantly longer than the ELC group [MD = 6.41, 95% CI (4.63 to 8.18), P <.00001] (Figure 5).
Figure 5.
Forest plot of the overall hospital stay between the PTGBD group and the ELC group.
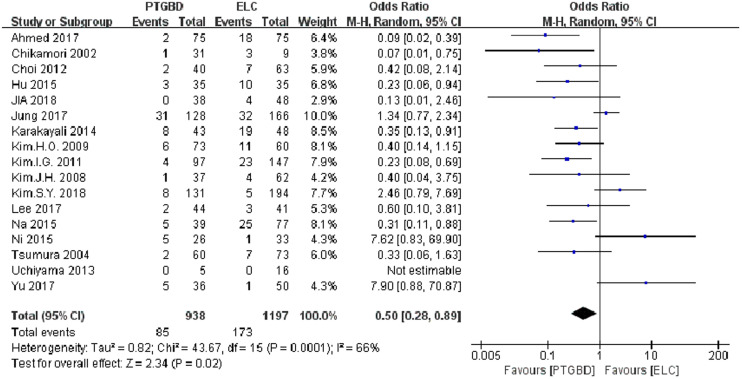
Conversion Rate to Open Surgery:
The conversion rate to open surgery was reported in all 17 studies, reporting the comparison of the conversion rate to open surgery between the PTGBD group and the ELC group. Significantly high heterogeneity was observed (P =.0001, I² = 66%), thus the random-effects model was used. The meta-analysis showed that the conversion rate to open surgery in the PTGBD group was significantly lower than the ELC group [OR = 0.50, 95% CI (0.28 to 0.89), P = .02] (Figure 6).
Figure 6.
Forest plot of the conversion rate to open surgery between the PTGBD group and the ELC group.
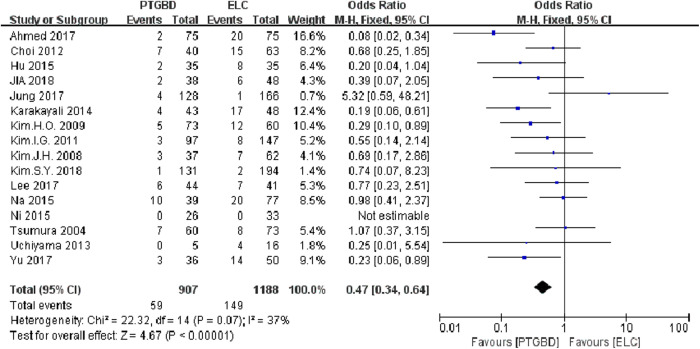
Postoperative Complications:
A total of 16 studies reported postoperative complications. There was no significant heterogeneity between these studies (P = .07, I² = 37%), therefore, the fixed-effects model was used. Compared to the ELC group, the PTGBD group had significantly lesser postoperative complication [OR=0.47, 95% CI (0.34 to 0.64), P < .00001] (Figure 7).
Figure 7.
Forest plot of the postoperative complications between the PTGBD group and the ELC group.
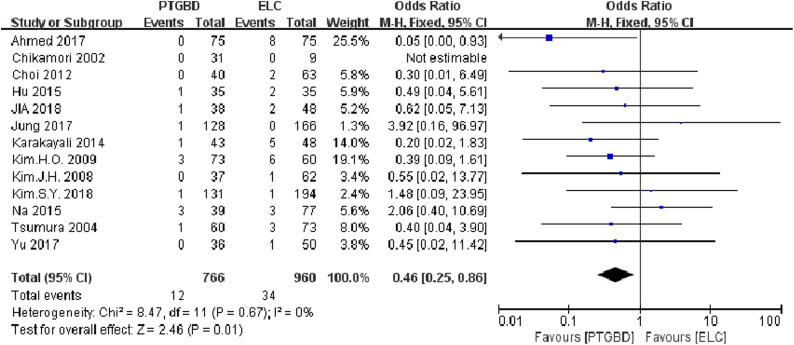
Bile Leakage:
The bile leakage was reported in 13 studies. Compared to the ELC group, the PTGBD group had a lesser bile leakage [OR = 0.46, 95% CI (0.25 to 0.86), P = .01] in the fixed-effects model (P =.67, I² = 0%) (Figure 8).
Figure 8.
Forest plot of the bile leakage between the PTGBD group and the ELC group.
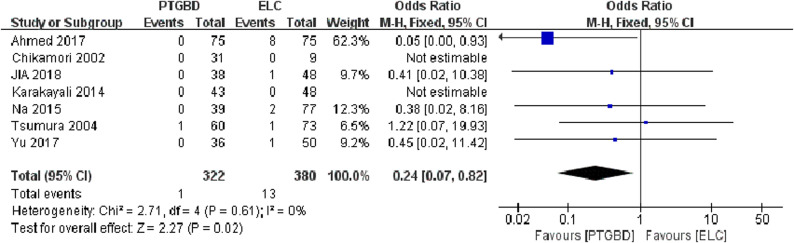
Bile Duct Injury:
Seven studies reported the bile duct injury and showed that the PTGBD group had a lesser bile duct injury than the ELC group [OR = 0.24, 95% CI (0.07 to 0.82), P = .02]. There was no heterogeneity observed (P = 0.61, I² = 0%), thus the fixed-effects model was used (Figure 9).
Figure 9.
Forest plot of the bile duct injury between the PTGBD group and the ELC group.
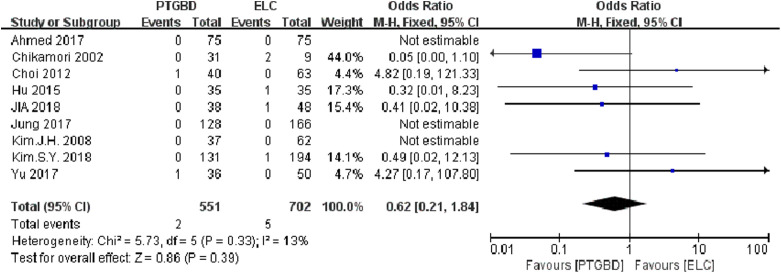
Intraperitoneal Hemorrhage:
The intraperitoneal hemorrhage was reported in nine studies. There was no significant difference in intraperitoneal hemorrhage between the two groups [OR = 0.62, 95% CI (0.21 to 1.84), P = .39]. There was no significant heterogeneity observed (P = .33, I² = 13%), thus the fixed-effects model was used (Figure 10).
Figure 10.
Forest plot of the intraperitoneal hemorrhage between the PTGBD group and the ELC group.
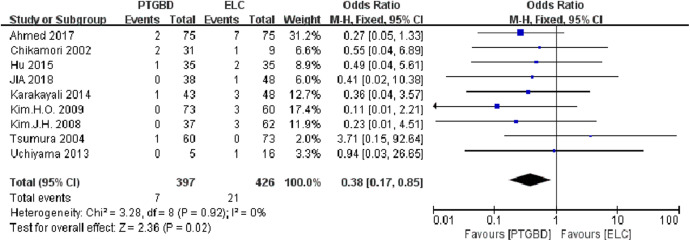
Wound Infection:
The wound infection was reported in nine studies. Compared to ELC group, PTGBD group had a lesser wound infection [OR = 0.38, 95% CI (0.17 to 0.85), P = .02] in the fixed-effects model (P = .92, I² = 0%) (Figure 11).
Figure 11.
Forest plot of the wound infection between the PTGBD group and the ELC group.
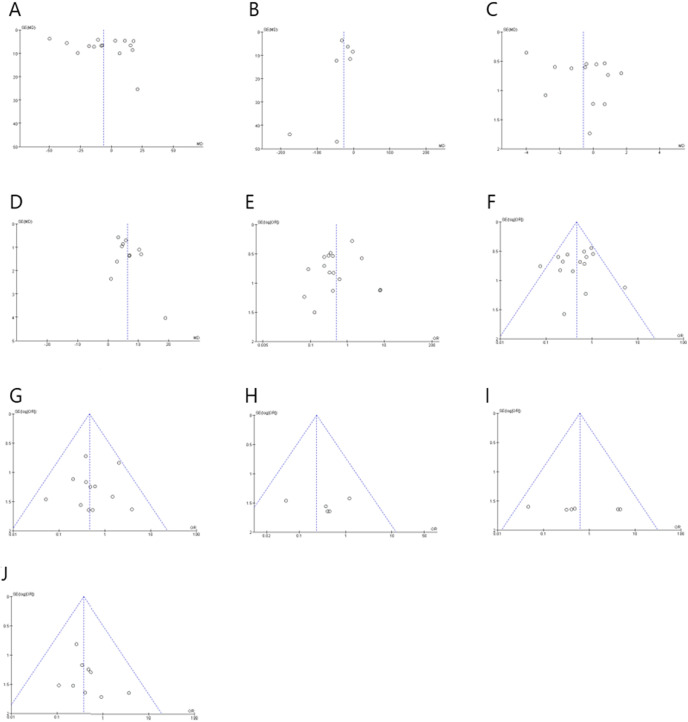
Publication Bias:
Funnel plots were constructed for each outcome and used to assess the publication bias (Figure 12).
Figure 12.
The funnel plots of each outcome. A, operative time; B, intraoperative bleeding; C, postoperative hospital stay; D, overall hospital stay; E, conversion rate to open surgery; F, postoperative complications; G, bile leakage; H, bile duct injury; I, intraperitoneal hemorrhage; J, wound infection.
Discussion
Acute cholecystitis is an inflammatory gallbladder disease that results from the bacterial invasion and obstruction of the cystic duct. Acute cholecystitis is one of the most common reasons for emergency surgical admission.24 In the past, AC was a contraindication to LC because of severe adhesion or difficult exposure of the gallbladder triangle. Especially, in elderly AC patients with other life-threatening comorbidities, LC can lead to high morbidity of up to 41% and mortality of up to 4.5% during the acute phase.25,26 With the increase in laparoscopic experience and the improvement in the laparoscopic devices and instruments, LC has become the standard treatment for AC.27 However, we sometimes experience difficulty during LC because of inflammation with severe fibrosis, dense adhesions, or tissue friability near the triangle of the gallbladder. These can increase postoperative complications, such as bile duct injury, bile leakage, Intraperitoneal hemorrhage, bowel injury, and other complications.
In 1980, PTGBD was first introduced by Radder,6 since then, it has become an emergency replacement procedure for high-risk AC. PTGBD is performed as a simple procedure, which can lessen pain to the patients, with low requirement for advanced equipment, high efficiency, and fast recovery.28-31 Hu et al.13 consider that PTGBD not only decompresses gallbladder swelling and prevents gallbladder perforation, but also improves local circulation and controls local infection. High-risk patients can undergo an operation after PTGBD without the increase of postoperative morbidity. This was in agreement with some researchers. They32 found that the success rate of percutaneous gallbladder drainage was almost 100% and the symptom remission rate reached from 78% to 100%. However, the morbidity rate and the mortality rate merely ranged from 3% to 13% and 0% to 11%, respectively. Compared with OC in critical patients, it has been considered as a less invasive operation with low mortality and morbidity.33,34 As most AC is caused by obstruction of bile outflow because of a gallstone, PTGBD cannot solve the problem. Hence, PTGBD has been used as a bridge to an elective cholecystectomy.
Based on our meta-analysis, there was no significant difference between PTGBD group and ELC group for operative time [MD = −6.23, 95% CI (−18.57 to 6.11), P = .32], postoperative hospital stay [MD = −0.60, 95% CI (−1.74 to 0.54), P = .30], intraperitoneal hemorrhage [OR = 0.62, 95% CI (0.21 to 1.84), P = .39]. This result was possibly associated with that in some reports patients in the PTGBD group had worse general condition and disease severity than patients in the ELC group, such as the proportion of ASA grade 3-4 and the proportion of severe AC patients.
The overall hospital stay in PTGBD group was significantly longer than ELC group [MD = 6.41, 95% CI (4.63 to 8.18), P < .00001]. Percutaneous transhepatic gallbladder drainage group patients had longer hospital stay than ELC group because PTGBD group patients needed to be hospitalized much longer or even twice to complete the entire therapy. This might be the only drawback in the PTGBD group.
The intraoperative bleeding of the PTGBD group was significantly lower than the ELC group [MD = −26.41, 95% CI (−43.16 to −9.66), P = .002]. The conversion rate to open surgery was significantly lower in the PTGBD group than the ELC group [OR = 0.50, 95% CI (0.28 to 0.89), P = .02]. Postoperative complications in the PTGBD group were significantly lesser than the ELC group [OR = 0.47, 95% CI (0.34 to 0.64), P < .00001]. There was a significant increase in incidence of bile leakage [OR = 0.46, 95% CI (0.25 to 0.86), P = .01], bile duct injury [OR = 0.24, 95% CI (0.07 to 0.82), P = 0.02] and wound infection [OR = 0.38, 95% CI (0.17 to 0.85), P = .02] in ELC group.
Some asymmetric was seen in the funnel plots, which identified the presence of publication bias. Significant heterogeneity was observed in some results too. The reason may be surgical experience, surgical instruments, the proportion of ASA grade 3 and 4, severity grading of acute cholecystitis, and different discharge standards. The different interval from PTGBD to LC is another important factor that causes heterogeneity. The best time of delayed LC after PTGBD has been controversial until now. The optimal time of delayed LC differs among various centers based on their experience and policy.11 Jia et al.35 suggested that patients who underwent LC within 5 days after PTGBD had significantly lesser operating time, blood loss, postoperative peritoneal drainage time, postoperative oral intake time, and postoperative complications compared to those who underwent LC more than 5 days. Another study36 showed that the SI group, LC performed within 216 hours after PTGBD, had significantly longer operative time, more postoperative complications, except surgical site infection, and higher rates of necrosis/abscess formation and adhesions around the gallbladder neck than LI group, LC performed more than 216 hours after PTGBD. Therefore, it requires more studies, especially well-designed, large, randomized controlled studies, to confirm the best time of delayed LC after PTGBD.
Perform PTGBD before LC has several benefits. First, PTGBD is a simple, less invasive, high-efficiency procedure, especially for high-risk AC patients who are not suitable for LC. Second, PTGBD is a useful procedure for LC because it not only decompresses the gallbladder distention but also attenuates the gallbladder wall and inflammation.10 Last, after PTGBD, scheduled LC can be performed when the patient’s condition stabilized.
This meta-analysis has some limitations, such as the sample size was too small in the intraoperative bleeding analysis, most of the articles in our study were retrospective studies, heterogeneity in some results, etc. These might have affected the results. Therefore, well-designed, large, multicenter, high-quality, randomized controlled articles should be performed to verify the results.
Conclusions
This study indicates that, although the operative time, postoperative hospital stay and intraperitoneal hemorrhage did not differ significantly between the two groups, patients in the PTGBD group had better outcomes, such as intraoperative bleeding, conversion rate to open surgery, postoperative complications, bile duct injury, bile leakage, and wound infection, than those in ELC group. The only drawback in PTGBD group is to lengthen total hospital stay.
Funding Statement
The authors declared that this study has received no financial support.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: N/A.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – S.C.; Design - S.C.; Supervision - X.M.; Resource - S.C., X.M.; Materials - S.C., X.M.; Data Collection and/or Processing - S.C., X.M.; Analysis and/or Interpretation - S.C., X.M.; Literature Search - S.C.; Writing - S.C., X.M.; Critical Reviews - X.M.
Acknowledgments: The authors thanks all colleagues of the Department of General Surgery and Oncology for clinical suggestions and commenting the manuscript.
Conflict of Interest: The authors have declared that no conflicts of interest exist.
References
- 1. . Halpin V. Acute cholecystitis. BMJ Clin Evid. 2014;2014:0411. [PMC free article] [PubMed] [Google Scholar]
- 2. . Jia B, Liu K, Tan L, Jin Z, Liu Y. Percutaneous transhepatic gallbladder drainage combined with laparoscopic cholecystectomy versus emergency laparoscopic cholecystectomy in acute complicated cholecystitis: comparison of curative efficacy. Am Surg. 2018;84(3):438–442.. 10.1177/000313481808400331) [DOI] [PubMed] [Google Scholar]
- 3. . Patterson EJ, McLoughlin RF, Mathieson JR, Cooperberg PL, MacFarlane JK. An alternative approach to acute cholecystitis. Percutaneous cholecystostomy and interval laparoscopic cholecystectomy. Surg Endosc. 1996;10(12):1185–1188.. 10.1007/s004649900275) [DOI] [PubMed] [Google Scholar]
- 4. . Van Steenbergen W, Rigauts H, Ponette E.et al. Percutaneous transhepatic cholecystostomy for acute complicated calculous cholecystitis in elderly patients. J Am Geriatr Soc. 1993;41(2):157–162.. 10.1111/j.1532-5415.1993.tb02051.x) [DOI] [PubMed] [Google Scholar]
- 5. . Watanabe Y, Sato M, Abe Y.et al. Preceding PTGBD decreases complications of laparoscopic cholecystectomy for patients with acute suppurative cholecystitis. J Laparoendosc Surg. 1996;6(3):161–165.. 10.1089/lps.1996.6.161) [DOI] [PubMed] [Google Scholar]
- 6. . Radder RW. Ultrasonically guided percutaneous catheter drainage for gallbladder empyema. Diagn Imaging. 1980;49(6):330–333.. [PubMed] [Google Scholar]
- 7. . Ni Q, Chen D, Xu R, Shang D. The efficacy of percutaneous transhepatic gallbladder drainage on acute cholecystitis in high-risk elderly patients based on the Tokyo guidelines: a retrospective case-control study. Med. 2015;94(34):e1442. 10.1097/MD.0000000000001442) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. . Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605.. 10.1007/s10654-010-9491-z) [DOI] [PubMed] [Google Scholar]
- 9. . Lee R, Ha H, Han YS.et al. Percutaneous transhepatic gallbladder drainage followed by elective laparoscopic cholecystectomy for patients with moderate to severe acute cholecystitis. Med. 2017;96(44):e8533. 10.1097/MD.0000000000008533) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. . Jung BH, Park JI. Impact of scheduled laparoscopic cholecystectomy in patients with acute cholecystitis, following percutaneous transhepatic gallbladder drainage. Ann Hepatobiliary Pancreat Surg. 2017;21(1):21–29.. 10.14701/ahbps.2017.21.1.21) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. . El-Gendi A, El-Shafei M, Emara D. Emergency versus delayed cholecystectomy after percutaneous transhepatic gallbladder drainage in Grade II acute cholecystitis patients. J Gastrointest Surg. 2017;21(2):284–293.. 10.1007/s11605-016-3304-y) [DOI] [PubMed] [Google Scholar]
- 12. . Na BG, Yoo YS, Mun SP.et al. The safety and efficacy of percutaneous transhepatic gallbladder drainage in elderly patients with acute cholecystitis before laparoscopic cholecystectomy. Ann Surg Treat Res. 2015;89(2):68–73.. 10.4174/astr.2015.89.2.68) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. . Hu YR, Pan JH, Tong XC.et al. Efficacy and safety of B-mode ultrasound-guided percutaneous transhepatic gallbladder drainage combined with laparoscopic cholecystectomy for acute cholecystitis in elderly and high-risk patients. BMC Gastroenterol. 2015;15:81. 10.1186/s12876-015-0294-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. . Uchiyama H, Shirabe K, Yoshizumi T.et al. Verification of our therapeutic criterion for acute cholecystitis: “perform a subemergency laparoscopic cholecystectomy when a patient is judged to be able to tolerate general anesthesia”--the experience in a single community hospital. Fukuoka Igaku Zasshi = Hukuoka Acta Medica. 2013;104(10):339–343.. [PubMed] [Google Scholar]
- 15. . Choi JW, Park SH, Choi SY, Kim HS, Kim TH. Comparison of clinical result between early laparoscopic cholecystectomy and delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage for patients with complicated acute cholecystitis. Korean J Hepatobiliary Pancreat Surg. 2012;16(4):147–153.. 10.14701/kjhbps.2012.16.4.147) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. . Kim IG, Kim JS, Jeon JY.et al. Percutaneous transhepatic gallbladder drainage changes emergency laparoscopic cholecystectomy to an elective operation in patients with acute cholecystitis. J Laparoendosc Adv Surg Tech A. 2011;21(10):941–946.. 10.1089/lap.2011.0217) [DOI] [PubMed] [Google Scholar]
- 17. . Kim HO, Ho Son B, Yoo CH, Ho Shin J. Impact of delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage for patients with complicated acute cholecystitis. Surg Laparosc Endosc Percutan Tech. 2009;19(1):20–24.. 10.1097/SLE.0b013e318188e2fe) [DOI] [PubMed] [Google Scholar]
- 18. . Kim JH, Kim JW, Jeong IH.et al. Surgical outcomes of laparoscopic cholecystectomy for severe acute cholecystitis. J Gastrointest Surg. 2008;12(5):829–835.. 10.1007/s11605-008-0504-0) [DOI] [PubMed] [Google Scholar]
- 19. . Tsumura H, Ichikawa T, Hiyama E.et al. An evaluation of laparoscopic cholecystectomy after selective percutaneous transhepatic gallbladder drainage for acute cholecystitis. Gastrointest Endosc. 2004;59(7):839–844.. 10.1016/s0016-5107(04)00456-0) [DOI] [PubMed] [Google Scholar]
- 20. . Chikamori F, Kuniyoshi N, Shibuya S, Takase Y. Early scheduled laparoscopic cholecystectomy following percutaneous transhepatic gallbladder drainage for patients with acute cholecystitis. Surg Endosc. 2002;16(12):1704–1707.. 10.1007/s00464-002-9004-6) [DOI] [PubMed] [Google Scholar]
- 21. . Kim SY, Yoo KS. Efficacy of preoperative percutaneous cholecystostomy in the management of acute cholecystitis according to severity grades. Korean J Intern Med. 2018;33(3):497–505.. 10.3904/kjim.2016.209) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. . Yu HB, Song HL, Pan BJ.et al. Is it safe to give laparoscopic cholecystectomy (LC) treatment of acute cholecystitis in senile patients 3 months after percutaneous transhepatic gallbladder drainage (PTGD)? A case-control study. Int J Clin Exp Med. 2017;10(9):13766–13771.. [Google Scholar]
- 23. . Karakayali FY, Akdur A, Kirnap M.et al. Emergency cholecystectomy vs percutaneous cholecystostomy plus delayed cholecystectomy for patients with acute cholecystitis. Hepatobiliary Pancreat Dis Int. 2014;13(3):316–322.. 10.1016/s1499-3872(14)60045-x) [DOI] [PubMed] [Google Scholar]
- 24. . Elsharif M, Forouzanfar A, Oaikhinan K, Khetan N. Percutaneous cholecystostomy... why, when, what next? A systematic review of past decade. Ann R Coll Surg Engl. 2018;100(8):1–14.. 10.1308/rcsann.2018.0150) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. . Chok KS, Chu FS, Cheung TT.et al. Results of percutaneous transhepatic cholecystostomy for high surgical risk patients with acute cholecystitis. ANZ J Surg. 2010;80(4):280–283.. 10.1111/j.1445-2197.2009.05105.x) [DOI] [PubMed] [Google Scholar]
- 26. . Kortram K, van Ramshorst B, Bollen TL.et al. Acute cholecystitis in high risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy (Chocolate trial): study protocol for a randomized controlled trial. Trials. 2012;13:7. 10.1186/1745-6215-13-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. . Pezzolla A, Lattarulo S, Borrello G.et al. The acute cholecystitis: the operative timing for the laparoscopic approach. Ann Ital Chir. 2007;78(6):475–480.. [PubMed] [Google Scholar]
- 28. . Tian H, Xia M, Zhang S, Li J, Liu J. Acute calculous cholecystitis associated with hepatic artery pseudoaneurysm after percutaneous transhepatic gallbladder drainage in a diabetic patient. Chin Med J. 2014;127(17):3192–3194.. [PubMed] [Google Scholar]
- 29. . Zhao XQ, Dong JH, Jiang K, Huang XQ, Zhang WZ. Comparison of percutaneous transhepatic biliary drainage and endoscopic biliary drainage in the management of malignant biliary tract obstruction: a meta-analysis. Dig Endosc. 2015;27(1):137–145.. 10.1111/den.12320) [DOI] [PubMed] [Google Scholar]
- 30. . Fujita T, Tanabe M, Takahashi S, Iida E, Matsunaga N. Percutaneous transhepatic hybrid biliary endoprostheses using both plastic and metallic stents for palliative treatment of malignant common bile duct obstruction. Eur J Cancer Care. 2013;22(6):782–788.. 10.1111/ecc.12088) [DOI] [PubMed] [Google Scholar]
- 31. . Komatsu S, Tsukamoto T, Iwasaki T.et al. Role of percutaneous transhepatic gallbladder aspiration in the early management of acute cholecystitis. J Dig Dis. 2014;15(12):669–675.. 10.1111/1751-2980.12198) [DOI] [PubMed] [Google Scholar]
- 32. . Melloul E, Denys A, Demartines N, Calmes JM, Schäfer M. Percutaneous drainage versus emergency cholecystectomy for the treatment of acute cholecystitis in critically ill patients: does it matter? World J Surg. 2011;35(4):826–833.. 10.1007/s00268-011-0985-y) [DOI] [PubMed] [Google Scholar]
- 33. . Famulari C, Macri A, Galipo S.et al. The role of ultrasonographic percutaneous cholecystostomy in treatment of acute cholecystitis. Hepato-Gastroenterology. 1996;43(9):538–541.. [PubMed] [Google Scholar]
- 34. . Hatzidakis AA, Prassopoulos P, Petinarakis I.et al. Acute cholecystitis in high-risk patients: percutaneous cholecystostomy vs conservative treatment. Eur Radiol. 2002;12(7):1778–1784.. 10.1007/s00330-001-1247-4) [DOI] [PubMed] [Google Scholar]
- 35. . Jia B, Liu K, Tan L.et al. Evaluation of the safety and efficacy of percutaneous transhepatic gallbladder drainage combined with laparoscopic cholecystectomy for treating acute complicated cholecystitis. Am Surg. 2018;84(1):133–136.. 10.1177/000313481808400134) [DOI] [PubMed] [Google Scholar]
- 36. . Inoue K, Ueno T, Nishina O.et al. Optimal timing of cholecystectomy after percutaneous gallbladder drainage for severe cholecystitis. BMC Gastroenterol. 2017;17(1):71. 10.1186/s12876-017-0631-8) [DOI] [PMC free article] [PubMed] [Google Scholar]