Abstract
Background
Higher postoperative quadriceps function has been positively associated with surgical outcomes after anterior cruciate ligament reconstruction (ACLR). However, the impact of autograft harvest and/or a concomitant meniscal procedure on the recovery of quadriceps strength is not well defined.
Purpose
To describe postoperative recovery of quadriceps strength following ACLR related to autograft selection, meniscal status, and sex.
Study Design
Retrospective Cohort.
Methods
One hundred and twenty-five participants who underwent ACLR with either a hamstring tendon (HT), bone-patellar tendon-bone (BPTB) or quadriceps tendon (QT) autograft were included. At postoperative months 3, 6 and 9, each participant completed an isometric quadriceps strength testing protocol at 90-degrees of knee flexion. Participants’ quadriceps average peak torque (Q-AvgPKT), average peak torque relative to body weight (Q-RPKT), and calculated limb symmetry index (Q-LSI) were collected and used for data analysis. Patients were placed in groups based on sex, graft type, and whether they had a concomitant meniscal procedure at the time of ACLR. At each time point, One-way ANOVAs, independent samples t-test and chi-square analyses were used to test for any between-group differences in strength outcomes.
Results
At three months after ACLR, Q-RPKT was significantly higher in those with the HT compared to the QT. At all time points, males had significantly greater Q-RPKT than females and HT Q-LSI was significantly higher than BPTB and QT. A concomitant meniscal procedure at the time of ACLR did not significantly affect Q-LSI or Q-RPKT at any testing point.
Conclusion
This study provides outcomes that are procedure specific as well as highlights the objective progression of quadriceps strength after ACLR. This information may help better-define the normal recovery of function, as well as guide rehabilitation strategies after ACLR.
Level of Evidence
3
Keywords: quadriceps, strength, isometric, meniscus, anterior cruciate ligament reconstruction
INTRODUCTION
Anterior cruciate ligament reconstruction (ACLR) is the primary surgical procedure for restoring anatomic knee stability after an anterior cruciate ligament injury. Despite improvements in ACLR indications, techniques, and postoperative rehabilitation,1–3 a large proportion of patients continue to report long-term reductions in physical function.4 Stronger and more symmetrical quadriceps strength has consistently been associated with better surgical outcomes.5–12 Prior ACLR studies have highlighted a positive correlation between higher quadriceps strength and improved knee function within the surgical limb, as well as a reduced risk of recurrent knee injuries.12–15 In reference to long-term joint health after ACLR, poor postoperative quadriceps function may be an intervening risk factor in the development of post-traumatic osteoarthritis within the knee.16,17
There are a number of considerations for ACLR graft harvest selection with each option having advantages and disadvantages, but research is limited on graft specific objective performance outcomes. Bone-patellar tendon-bone autograft (BPTB) has been reported as the superior graft choice for athletes,18,19 but carries an increased risk of patellar fracture,20 kneeling difficulty,21 and anterior knee pain.19,22–24 Compared to the BPTB, the hamstring tendon (HT) autograft may produce fewer graft harvest site complications,25 but yield an increase prevalence of joint laxity and delayed graft maturation.26–28 More recently, outcomes for the quadriceps tendon (QT) autograft have been reported to be comparable to the BPTB and HT autograft,22,24,29 but the QT produces significantly less initial quadriceps weakness than the BPTB autograft.23 Current evidence suggests no significant difference in graft failure rates between BPTB, HT and QT autografts, 19,24 but studies have suggested graft-specific impairments in muscle function after ACLR, to which the recovery of postoperative quadriceps strength is partially dictated by graft selection itself.30–32 Specifically, ACLR with a BPTB may produce larger reductions in quadriceps function, require more time to recover quadriceps strength, and be slower to achieve rehabilitation milestones compared to the HT autograft or an allograft procedure.33
The above observations are paralleled by research highlighting persistent impairments in quadriceps function at longer-term follow up, independent of graft type.17,34–37 Regardless of graft selection for ACLR, higher postoperative quadriceps strength at mid-term follow-up has been consistently correlated with better knee function at longer-term follow up.38–40 Although greater quadriceps strength may facilitate a better ACLR outcome10,11, the majority of these studies have reported the between-limb, level of quadriceps strength-symmetry as the outcome of interest rather than the actual quadriceps strength relative to the participants’ body weight.41 The quadriceps limb symmetry index (Q-LSI) approach to quantifying muscle strength assumes the non-surgical limb’s strength-value is an adequate benchmark from which to compare the reconstructed knee’s muscles. Most of the recent literature has reported that athletes achieve a Q-LSI anywhere between 73% and 95% at their time of return to activities, which has been measured both isometrically and isokinetically.5,11,13,41–43
However, data published by Chung et al37 has highlighted the fact unilateral ACL injury can produce reductions in muscle strength within the uninjured limb, and suboptimal muscle function is still present at the time of return to sport. For this reason, the use of Q-LSI without consideration of the individual’s relative strength levels when assessing functional status should be questioned. To the authors’ knowledge, two studies to date have investigated the ability of Q-LSI and relative strength values to predict patient-reported knee function.44,45 Kuenze et al44 suggest an isometric relative quadriceps strength value ≥ 3.00 newton-meters/kilogram (Nm/kg) is an acceptable indicator of good patient-reported knee function 2.5 years after ACLR, whereas a Q-LSI ≥ 84.7% is less indicative of higher outcome scores. With similar methods, Pietrosimone et al45 established an isokinetic relative quadriceps strength value of >3.10 Nm/kg as a good indicator of higher patient reported outcome at three years post ACLR.
The potential for inconsistency in quadriceps strength and muscle recovery exists after ACLR, necessitates more detailed reporting of strength outcomes which are specific to the ACLR procedure. Few studies comment on the progression of quadriceps strength relative to the participant’s body weight,46–50 but these studies are limited to only reporting isokinetic data and lack procedure-specific comparisons. Specifically, no study has presented the progression of isometric quadriceps strength within a population of BPTB, HT, and QT autografts at 3, 6, and 9 months after ACLR. Studies with this level of procedure-specific detail can help better define the normal recovery of quadriceps strength after ACLR. Therefore, the purpose of this study was to describe postoperative recovery of quadriceps strength following ACLR related to autograft selection, meniscal status, and sex.
MATERIALS AND METHODS
Between September 2018 and May 2020, 125 competitive and recreational athletes who underwent an ACLR procedure were included in this study; 85% of the participants were involved in either Level I or II cutting, pivoting, jumping, and lateral movement.51 Participants were included if they had undergone ACLR with either a HT, BPTB or QT autograft. Patients who underwent ACLR with a concomitant meniscal repair or meniscectomy were also included. Those with meniscectomies were included in the non-meniscus group for analysis due to lack of weight bearing and range of motion restrictions. Exclusion criteria included those having undergone a contralateral ACLR, a revision ACLR; having a multi-ligament knee injury or graft harvest from the contralateral limb; or any previous knee surgeries on either limb. The study was conducted under institutional review board approval (Advarra, 08.19.2019 NS_HAUS). All testing procedures were explained to each participant and an informed consent document was signed prior to testing. Parental consent and youth assent were obtained for all participants under the age of 18 years. All data was collected at the Training HAUS Sports Science Lab at Twin Cities Orthopedics (Eagan, MN).
All participants underwent quadriceps strength testing between three and nine months after ACLR. Participants completed testing at three separate time points within 1.5 months of their 3, 6 and 9-month postoperative date. For three month testing, no participants were tested earlier than 2.4 months after ACLR. Isometric quadriceps strength tests were all performed using an isokinetic dynamometer (Biodex Medical Systems, Inc., Shirley, NY). Due to the varying postoperative precautions present during the early stages of recovery after an ACLR, isometric contractions at 90-degrees where utilized to test quadriceps strength instead of an isokinetic protocol.20,27,45,52,53
Before testing, participants were taken through a dynamic warm-up led by a physical therapist, athletic trainer or sports performance coach. For strength testing, participants were seated with the knee positioned so that the lateral femoral epicondyle aligned with the dynamometer’s axis of rotation. Thigh, waist, and two chest straps were used to secure the participant to the chair. The dynamometer’s force-arm was secured superior to the lateral malleolus of the ankle. Each participant completed a warm-up protocol on the dynamometer consisting of four, isokinetic knee extensions through a self-selected range of motion. For isometric testing, the knee was positioned at 90-degrees of flexion and all participants were asked to apply as much force as possible against the fixed arm of the dynamometer throughout the duration of the test. One maximal voluntary isometric contraction (MVIC) torque for the quadriceps, recorded in Nm, was completed against the arm of the dynamometer; this was done to practice the subsequent isometric strength test. Three, MVICs were completed for five-seconds in duration, with a 30-second rest interval in between each repetition. For all participants, testing was completed on the non-surgical limb first, followed by testing of the surgical limb. The average of the three peak torque values was calculated (Q-AvgPKT) and normalized to body mass in kilograms (Q-RPKT). Q-LSI was calculated at each time point utilizing Q-AvgPKT with the following equation: (Q-AvgPKT surgical limb/ Q-AvgPKT non-surgical limb) x 100. The variables used in analysis were Q-RPKT and Q-LSI.
An a priori power analysis was completed for three independent groups, a medium effect size and a power of 0.80. For the data set to be adequately powered, a total sample size of 115 patients would be needed with a minimum of 15 patients within each group. Kolmogorov-Smirnov and Shapiro-Wilk tests were used to confirm normality within the collected data set for this study. When applicable, one-way ANOVAs, as well as independent samples t-tests and chi-square tests were used to determine mean differences between the three groups. Statistical analyses were performed with SPSS version 24 (IBM Corp., Armonk, NY, USA), and significance was set at p < 0.05.
RESULTS
Patient demographics are presented in Table 1. Procedure-specific quadriceps strength variables, organized by postoperative time point, are presented in Table 2. The testing protocol used in this study did not result in any surgical complications when implemented as early as three months after ACLR, suggesting an isometric testing protocol on an isokinetic dynamometer is a safe and clinically reasonable way to assess quadriceps strength during the early stages of rehabilitation after ACLR. At postoperative months 3, 6 and 9, quadriceps Q-LSI was found to be significantly higher in patients who had undergone ACLR with the HT autograft than with the BPTB and QT (p< .001). At three months after ACLR, Q-RPKT was found to be significantly higher in those with the HT compared to the QT (p<.05). There were no significant differences in Q-RPKT between graft types at six and nine months after ACLR. At all three postoperative time points, males had significantly greater Q-RPKT than females (p<.01) but no differences in Q-LSI was observed between sexes. Compared to those who received an isolated ACLR procedure, no significant difference in Q-LSI or Q-RPKT was found in those with a concomitant meniscal procedure at the time of ACLR.
Table 1. Participant Demographicsa.
| Demographic | Measure |
|---|---|
| Sex | Female: 74 Male: 51 |
| Age (y) | 18.52 (5.08) |
| Height (m) | 1.71 (0.09) |
| Weight (kg) | 69.57 (14.37) |
| Testing Time Post-Op (months) | Early: 3.48 (0.57) Mid: 6.37 (0.61) Late: 9.23 (0.64) |
| Sport Levels51 | Level I: 97 Level II: 23 Level III: 5 |
| Limb Involved | Right: 51 Left: 74 |
| Graft Type | BPTB: 87 HT: 21 QT: 17 |
| Meniscal Involvement | Yes: 45 No: 80 |
aValues are presented as mean (SD) or number
BPTB = bone-patellar tendon-bone, HT = hamstring tendon, QT = quadriceps tendon
Table 2. Mean Values of Strength & Symmetry over Stages of Rehabilitation, all data presented mean (SD).
| 3 month | 6 month | 9 month | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Non-Surgical Q-RPKT (Nm/kg) | Surgical Q-RPKT (Nm/kg) | Q-LSI (%) | Non-Surgical Q-RPKT (Nm/kg) | Surgical Q-RPKT (Nm/kg) | Q-LSI (%) | Non-Surgical Q-RPKT (Nm/kg) | Surgical Q-RPKT (Nm/kg) | Q-LSI (%) | |
| BPTB | 87 | 2.75 (0.60) | 1.64 (0.50) | 60% (0.13) | 2.88 (0.68) | 2.12 (0.59) | 74% (0.13) | 2.93 (0.67) | 2.46 (0.66) | 84% (0.14) |
| HT | 21 | 2.41 (0.42) | 1.83 (0.42) | 76% (0.12) | 2.45 (0.46) | 2.25 (0.54) | 92% (0.13) | 2.74 (0.54) | 2.61 (0.59) | 96% (0.16) |
| QT | 17 | 2.63 (0.69) | 1.39 (0.67) | 52% (0.17) | 2.79 (0.61) | 1.87 (0.70) | 67% (0.20) | 2.85 (.044) | 2.24 (0.78) | 77% (0.19) |
| p value | p=.059 | p=.035† | p<.001‡§ | p=.025* | p=.146 | p<.001‡§ | p=.443 | p=.237 | p<.001†§ | |
| Meniscus | 45 | 2.77 (0.57) | 1.72 (0.40) | 63% (0.13) | 2.85 (0.63) | 2.16 (0.49) | 76% (0.14) | 2.94 (0.56) | 2.49 (0.60) | 85% (0.15) |
| No Meniscus | 80 | 2.62 (0.59) | 1.59 (0.58) | 60% (0.60) | 2.76 (0.67) | 2.09 (0.68) | 76% (0.17) | 2.86 (0.64) | 2.44 (0.73) | 85% (0.17) |
| p value | p=.170 | p=.185 | p=.285 | p=.463 | p=.545 | p=.999 | p=.485 | p=.697 | p=.999 | |
| Male | 51 | 2.94 (0.61) | 1.88 (0.58) | 64% (0.15) | 3.15 (0.70) | 2.42 (0.69) | 77% (0.16) | 3.18 (0.61) | 2.78 (0.74) | 87% (0.16) |
| Female | 74 | 2.49 (0.50) | 1.47 (0.41) | 60% (0.14) | 2.55 (0.50) | 1.9 (0.45) | 75% (0.16) | 2.68 (0.52) | 2.23 (0.54) | 84% (0.16) |
| p value | p<.001 | p<.001 | p=.130 | p<.001 | p<.001 | p=.494 | p<.001 | p<.001 | p=.305 | |
* Statistically significant difference between BPTB & HT (p< 0.05), † Statistically significant difference between HT & QT (p< 0.05), ‡ Statistically significant difference between HT & QT (p< 0.001), §Statistically significant difference between BPTB & HT (p< 0.0001), Q-RPKT = quadriceps average peak torque normalized to body mass, Q-LSI = quadriceps limb symmetry index, BPTB = bone-patellar tendon-bone, HT = hamstring tendon, QT = quadriceps tendon
DISCUSSION
The purpose of this study was to describe the postoperative recovery of quadriceps strength after ACLR. Before determining the clinical significance of any findings, the reader must first acknowledge the observed distribution of quadriceps strength within the cohort. At all three testing points, those receiving the BPTB and QT autografts for ACLR presented with a wider distribution of Q-LSI values than was observed in the HT group (Figure 1. d-f).
Figure 1a-f. Quadriceps Relative Peak Torque and Limb Symmetry Index Frequency Distribution by Graft Type: 3, 6 and 9 month postoperative. (a-c RPKT; d-f LSI).
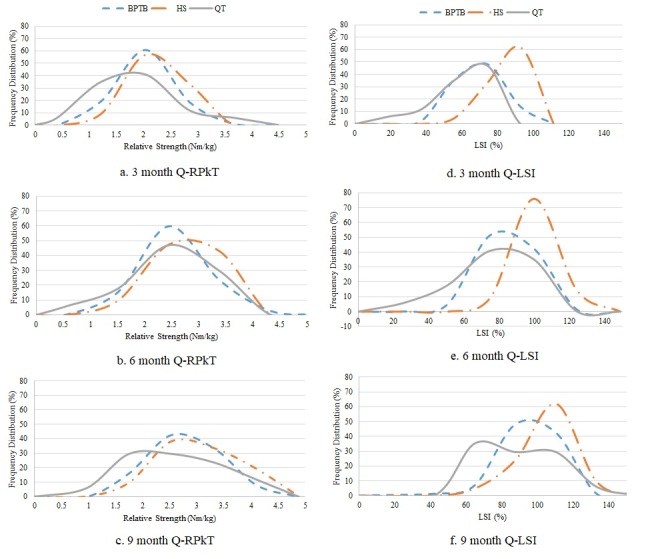
Additionally, those receiving the BPTB autograft tended to have a more consistent improvement in Q-LSI throughout the postoperative testing period, which is reflected in the higher absolute BPTB frequency-distribution percentages compared to the QT autograft at the six and nine month testing points. Collectively, these observations suggest that at three months after ACLR, a larger distribution in Q-LSI may be expected in those receiving the BPTB or QT for ACLR, compared to the HT autograft.
This study’s findings also suggest individuals receiving the HT autograft for ACLR may exhibit a greater Q-LSI throughout the postoperative rehabilitation period, compared to those receiving the BPTB and QT autografts. This finding is not a novel contribution to the ACLR literature, as prior studies have reported graft-specific reductions in muscle strength after ACLR. Fischer et al54 reported a difference in muscle strength between the HT and the QT autografts used for ACLR, to which a similarly higher level of Q-LSI was observed in those with the HT compared to the QT. Considering this, this study’s findings further suggest that graft harvest site is a relevant functional consideration for Q-LSI after ACLR, as graft specific impairments in quadriceps symmetry between limbs may be expected with the BPTB and QT autografts, compared to the HT.
At three months after ACLR, this study suggests individuals receiving the HT may expect a statistically greater level of Q-RPKT than those receiving the QT autograft. BPTB Q-RPKT was less than HT and greater than QT, but these differences were not statistically different. These decreased Q-RPKT values in QT and BTB may be present due to graft harvest from the knee extensor mechanics resulting in decreased tendon capacity. At postoperative months six and nine, no between-graft differences in Q-RPKT were found between any of the three autograft types (Table 2). Prior research has suggested any between-graft differences in quadriceps strength may only be clinically distinguishable during the early phases of rehabilitation after ACLR;55 a notion which these findings support. These findings may support the idea that factors other than graft harvest site are responsible for relative strength values not reaching previously reported values for higher outcomes by nine months.44,45 Further research is needed to assess the relevance and relationship of Q-RPKT to the timing of return-to-sport (RTS) and graft rupture rates.
The statistically lower Q-LSI values observed after ACLR with the BPTB and QT, compared to the HT autograft, may be partially explained by the body’s protective response to donor site morbidity. Previously published biomechanical research has highlighted a 25% and 34% relative reduction in the absolute tensile strength of the patellar and quadriceps tendons after autograft harvest, respectively.56 It also appears having a concomitant meniscal procedure at the time of ACLR does not impact Q-RPKT or Q-LSI levels, and although males presented with a greater Q-RPKT than females, sex did not significantly impact Q-LSI levels. Collectively, these findings may suggest the low Q-LSI observed with the BPTB and QT, and Q-RPKT with the QT autograft at three months, is partially due to trauma to the extensor mechanism during graft harvest rather than any additional meniscal procedure at the time of ACLR.
When discussing RTS after ACLR, recent authors have shown that only 65% of athletes return to their pre-injury level of sports participation.57 An improved understanding of the contextual factors associated with RTS has shown a greater subjective report of knee function is positively correlated with an improving likelihood of an athlete returning to their pre-injury level of sport.58 Prior research has highlighted a positive relationship between greater Q-LSI and patient reported knee function, but fewer studies have investigated the relationship between Q-RPKT and subjective knee function. Kuenze et al44 reported an isometric relative strength cut-off value of ≥ 3.00 Nm/kg may be a more sensitive predictor of good patient-reported knee function in recreational athletes than Q-LSI. This however, was collected in recreational individuals beyond traditional time points of returning to sport. The majority of this current study’s population participated in Level I/II sports with 52% of HT, 22% of BPTB and 35% of QT achieving the previously mentioned Q-RPKT ≥ 3.00Nm/kg by the nine month post-surgery time point (Figure 1. a-c). These findings suggest that at nine months after ACLR, a relatively low proportion of this cohort achieved the level of Q-RPKT that may be assumed to present with a high self-report of knee function.
Smith et al33 have previously highlighted a discrepancy between subjective reporting of knee function and objective functional status within a cohort of athletes after ACLR. Athletes who had an ACLR with the BPTB were slower to achieve rehabilitation milestones and functional criteria than those with the HT or allograft, but no statistical, between-graft differences were observed in the subjective reporting of knee function. However, it is important to note that Smith et al33 used Q-LSI, rather than Q-RPKT, to quantify quadriceps function, and therefore, inferences from their study on the relationship between Q-RPKT and subjective knee function within this cohort is not directly comparable.
Q-LSI is commonly used as an objective outcome within the RTS decision-making process. Considering this, HT autografts consistently had more individuals testing ≥ 90% Q-LSI at all three testing points, with less variability in strength testing scores than the BPTB and QT autografts. This finding, alone, may be useful to clinicians when implementing criteria-based rehabilitation for an athlete. For instance, a medical team may elect to more closely monitor the progression of quadriceps strength throughout the postoperative rehabilitation period for athletes undergoing ACLR with the BPTB or QT compared to the HT, as well as implement a longer and more specific quadriceps strengthening program. Lastly, the procedure-specific Q-LSI and Q-RPKT values within this study may be used as normative data for clinicians to cross-reference when implementing criteria-based rehabilitation after ACLR for those returning to Level I and II sports, as well as recreational athletes returning to activity.
Strengths of this study include the standardization of data collection; testing of participants at multiple testing periods; and the direct comparison of quadriceps strength between the HT, BPTB, and QT autografts for ACLR. However, this study has several limitations worth mentioning. (1) This study was a retrospective analysis of prospectively collected data, and therefore, subject to the innate limitations of a retrospective study design. (2) Wide age-range within this cohort may make it difficult to extrapolate the normative data to more specific populations, such as young athletes returning to sport. (3) Participants were recruited from a single metropolitan city, making the possibility of a regional bias reflected within the study’s outcomes. (4) ACLR procedures were completed by 36 different surgeons; specific postoperative rehabilitation protocols, number of therapy visits, quality of rehabilitation, variance in surgical techniques and supplemental training was not standardized or described. (5) Weight bearing status was not taken into account for the meniscus repair group. (6) Lastly, a relatively low number of ACLR procedures with the QT and HT, compared to the BPTB, were completed within this cohort.
CONCLUSION
The results of this study outline isometric quadriceps strength progression specific to graft type, sex and meniscal involvement. Q-LSI was significantly greater in HT compared to BPTB and QT graft types at all three time points. Q-RPKT for QT was significantly lower than HT at 3-months, postoperatively. At all time points, males presented with significantly greater Q-RPKT than females, but sex did not significantly impact Q-LSI. Lastly, receiving a concomitant meniscal procedure at the time of ACLR did not statistically impact Q-RPKT or Q-LSI. The strength data found within this paper can be used to better understand the recovery of quadriceps strength after ACLR, as well as be used to optimize the rehabilitation plan of care based on surgical procedure. Future analysis on this population from subsequent testing sessions at later time points and evaluation of self-reported function will further provide additional insight into isometric quadriceps strength progression following ACLR.
CONFLICTS OF INTEREST
The authors report no conflicts of interest.
Acknowledgments
ACKNOWLEDGEMENTS
We thank the Twin Cities Orthopedics surgeons and physical therapists who referred their patients to be participants in this study. We also acknowledge Becky Stone McGaver for her contribution to this work.
References
- “ACL surgery: when to do it?”. Musahl Volker, Diermeier Theresa, de SA Darren, Karlsson Jon. 2020Knee Surgery, Sport Traumatol Arthrosc. 28(7):2023–2026. doi: 10.1007/s00167-020-06117-y. [DOI] [PubMed] [Google Scholar]
- Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. van Melick Nicky, van Cingel Robert E. H., Brooijmans Frans, Neeter Camille, van Tienen Tony, Hullegie Wim, Nijhuis-van der Sanden Maria W. G. Dec 1;2016 British Journal of Sports Medicine. 50(24):1506 LP–1515. doi: 10.1136/bjsports-2015-095898. [DOI] [PubMed] [Google Scholar]
- Return to sports after anterior cruciate ligament injury: Neither surgery nor rehabilitation alone guarantees success-it is much more complicated. Thomeé R., Waldén M., Hägglund M. 2015British Journal of Sports Medicine. 49(22):1422. doi: 10.1136/bjsports-2015-094793. [DOI] [PubMed] [Google Scholar]
- Anterior cruciate ligament injury after more than 20 years: I. Physical activity level and knee function. Tengman E., Brax Olofsson L., Nilsson K. G., Tegner Y., Lundgren L., Häger C. K. 2014Scandinavian Journal of Medicine and Science in Sports. 24(6):e491–500. doi: 10.1111/sms.12212. [DOI] [PubMed] [Google Scholar]
- Assessment of quadriceps/hamstring strength, knee ligament stability, functional and sports activity levels five years after anterior cruciate ligament reconstruction. Seto J. L., Orofino A. S., Morrissey M. C., Medeiros J. M., Mason W. J. 1988The American journal of sports medicine. 16(2):170–180. doi: 10.1177/036354658801600215. [DOI] [PubMed] [Google Scholar]
- Extensor mechanism function after patellar tendon graft harvest for anterior cruciate ligament reconstruction. Rosenberg T. D., Franklin J. L., Baldwin G. N., Nelson K. A., Reider B. 1992American Journal of Sports Medicine. 20(5):519–526. doi: 10.1177/036354659202000506. [DOI] [PubMed] [Google Scholar]
- The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. Wilk K. E., Romaniello W. T., Soscia S. M., Arrigo C. A., Andrews J. R. 1994Journal of Orthopaedic and Sports Physical Therapy. 20(2):60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]
- Arthroscopy-assisted anterior cruciate ligament reconstruction using patellar tendon substitution: two- to four-year follow-up results. Bach Bernard R., Jones Greg T., Sweet Fred A., Hager Cheryl A. 1994The American Journal of Sports Medicine. 22(6):758–767. doi: 10.1177/036354659402200606. [DOI] [PubMed] [Google Scholar]
- Objective factors affecting overall subjective evaluation of recovery after anterior cruciate ligament reconstruction. Muneta T, Seklya I, Ogiuchi T, Yagishita K, Yamamoto H, Shinomiya K. Oct;1998 Scandinavian Journal of Medicine & Science in Sports. 8(5):283–289. doi: 10.1111/j.1600-0838.1998.tb00484.x. [DOI] [PubMed] [Google Scholar]
- Knee-extension torque variability and subjective knee function in patients with a history of anterior cruciate ligament reconstruction. Goetschius John, Hart Joseph M. 2016Journal of Athletic Training. 51(1):22–27. doi: 10.4085/1062-6050-51.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Age, gender, quadriceps strength and hop test performance are the most important factors affecting the achievement of a patient-acceptable symptom state after ACL reconstruction. Cristiani Riccardo, Mikkelsen Christina, Edman Gunnar, Forssblad Magnus, Engström Björn, Stålman Anders. Feb 22;2020 Knee Surgery, Sports Traumatology, Arthroscopy. 28(2) doi: 10.1007/s00167-019-05576-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Single-legged hop test as predictors of self-reported knee function after ACL reconstruction. Logerstedt David, Grindem Hege, Lynch Andrew, Eitzen Ingrid. 2013The American journal of sports medicine. 40(July 2012):2348–2356. doi: 10.1177/0363546512457551.Single-legged. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. Schmitt Laura C., Paterno Mark V., Hewett Timothy E. 2012Journal of Orthopaedic and Sports Physical Therapy. 42(9):750–759. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Kyritsis Polyvios, Bahr Roald, Landreau Philippe, Miladi Riadh, Witvrouw Erik. Aug;2016 British Journal of Sports Medicine. 50(15):946–951. doi: 10.1136/bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. Grindem Hege, Snyder-Mackler Lynn, Moksnes Håvard, Engebretsen Lars, Risberg May Arna. Jul 1;2016 British Journal of Sports Medicine. 50(13):804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Chaudhari Ajit M.W., Briant Paul L., Bevill Scott L., Koo Seungbum, Andriacchi Thomas P. 2008Medicine and Science in Sports and Exercise. 40(2):215–222. doi: 10.1249/mss.0b013e31815cbb0e. [DOI] [PubMed] [Google Scholar]
- Noyes Frank R., Barber-Westin Sue. ACL Injuries in the Female Athlete. Springer Berlin Heidelberg; Risks of future joint arthritis and reinjury after ACL reconstruction; pp. 67–93. [DOI] [Google Scholar]
- Superior return to sports rate after patellar tendon autograft over patellar tendon allograft in revision anterior cruciate ligament reconstruction. Keizer Michèle N.J., Hoogeslag Roy A.G., van Raay Jos J.A.M., Otten Egbert, Brouwer Reinoud W. Feb 1;2018 Knee Surgery, Sports Traumatology, Arthroscopy. 26(2):574–581. doi: 10.1007/s00167-017-4612-9. [DOI] [PubMed] [Google Scholar]
- Bone–patellar tendon–bone versus hamstring tendon autografts for primary anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Schuette Hayden B, Kraeutler Matthew J, Houck Darby A, McCarty Eric C. Nov;2017 5(11):2325967117736484. doi: 10.1177/2325967117736484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fractures associated with patellar ligament grafts in cruciate ligament surgery. Christen B., Jakob R. P. 1992Journal of Bone and Joint Surgery - Series B. 74(4):617–619. doi: 10.1302/0301-620x.74b4.1624526. [DOI] [PubMed] [Google Scholar]
- A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Laxdal Gauti, Kartus Jüri, Hansson Leif, Heidvall Mats, Ejerhed Lars, Karlsson Jon. 2005Arthroscopy - Journal of Arthroscopic and Related Surgery. doi: 10.1016/j.arthro.2004.09.014. [DOI] [PubMed]
- Is quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Cavaignac Etienne, Coulin Benoit, Tscholl Philippe, Nik Mohd Fatmy Nik, Duthon Victoria, Menetrey Jacques. 2017American Journal of Sports Medicine. 45(6):1326–1332. doi: 10.1177/0363546516688665. [DOI] [PubMed] [Google Scholar]
- Comparison of short-term biodex results after anatomic anterior cruciate ligament reconstruction among 3 autografts. Hughes Jonathan D., Burnham Jeremy M., Hirsh Angela, Musahl Volker, Fu Freddie H., Irrgang James J., Lynch Andrew D. 2019Orthopaedic Journal of Sports Medicine. 7(5):1–7. doi: 10.1177/2325967119847630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone–patellar tendon–bone and hamstring-tendon autografts. Mouarbes Dany, Menetrey Jacques, Marot Vincent, Courtot Louis, Berard Emilie, Cavaignac Etienne. 2019American Journal of Sports Medicine. 47(14):3521–3540. doi: 10.1177/0363546518825340. [DOI] [PubMed] [Google Scholar]
- A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Pinczewski Leo A., Lyman Jeffrey, Salmon Lucy J., Russell Vivianne J., Roe Justin, Linklater James. 2007American Journal of Sports Medicine. 35(4):564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- Knee flexor strength recovery following hamstring tendon harvest for anterior cruciate ligament reconstruction: a systematic review. Ardern Clare, Webster Kate. 2009Orthopedic Reviews. 1(2) doi: 10.4081/or.2009.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamstring strength recovery after hamstring tendon harvest for anterior cruciate ligament reconstruction: a comparison between graft types. Ardern Clare L., Webster Kate E., Taylor Nicholas F., Feller Julian A. 2010Arthroscopy - Journal of Arthroscopic and Related Surgery. 26(4):462–469. doi: 10.1016/j.arthro.2009.08.018. [DOI] [PubMed] [Google Scholar]
- The effect of open- versus closed-kinetic-chain exercises on anterior tibial laxity, strength, and function following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Perriman Alyssa, Leahy Edmund, Semciw Adam Ivan. 2018Journal of Orthopaedic & Sports Physical Therapy. 48(7):552–566. doi: 10.2519/jospt.2018.7656. [DOI] [PubMed] [Google Scholar]
- Quadriceps recovery after anterior cruciate ligament reconstruction with quadriceps tendon versus patellar tendon autografts. Hunnicutt Jennifer L., Gregory Chris M., McLeod Michelle M., Woolf Shane K., Chapin Russell W., Slone Harris S. Apr 1;2019 Orthopaedic Journal of Sports Medicine. 7(4) doi: 10.1177/2325967119839786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: Comparison between bone-patellar tendon-bone and hamstring tendon autografts. Lautamies Riitta, Harilainen Arsi, Kettunen Jyrki, Sandelin Jerker, Kujala Urho M. 2008Knee Surgery, Sports Traumatology, Arthroscopy. 16(11):1009–1016. doi: 10.1007/s00167-008-0598-7. [DOI] [PubMed] [Google Scholar]
- The influence of graft choice on isokinetic muscle strength 4-24 months after anterior cruciate ligament reconstruction. Xergia Sofia A., McClelland Jodie A., Kvist Joanna, Vasiliadis Haris S., Georgoulis Anastasios D. 2011Knee Surgery, Sports Traumatology, Arthroscopy. 19(5):768–780. doi: 10.1007/s00167-010-1357-0. [DOI] [PubMed] [Google Scholar]
- Quadriceps tendon grafts does not cause patients to have inferior subjective outcome after anterior cruciate ligament (ACL) reconstruction than do hamstring grafts: a 2-year prospective randomised controlled trial. Lind Martin, Nielsen Torsten Grønbech, Soerensen Ole Gade, Mygind-Klavsen Bjarne, Faunø Peter. 2020British Journal of Sports Medicine. 54(3):183–187. doi: 10.1136/bjsports-2019-101000. [DOI] [PubMed] [Google Scholar]
- Athletes with bone-patellar tendon-bone autograft for anterior cruciate ligament reconstruction were slower to meet rehabilitation milestones and return-to-sport criteria than athletes with hamstring tendon autograft or soft tissue allograft. Smith Angela Hutchinson, Capin Jacob J., Zarzycki Ryan, Snyder-Mackler Lynn. 2020Journal of Orthopaedic and Sports Physical Therapy. 50(5):259–266. doi: 10.2519/jospt.2020.9111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Neeter Camille, Gustavsson Alexander, Thomeé Pia, Augustsson Jesper, Thomeé Roland, Karlsson Jon. 2006Knee Surgery, Sports Traumatology, Arthroscopy. 14(6):571–580. doi: 10.1007/s00167-006-0040-y. [DOI] [PubMed] [Google Scholar]
- Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. de Jong Suzanne N, van Caspel Danny R, van Haeff Michiel J, Saris Daniël B.F. Jan;2007 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 23(1):21.e1–21.e11. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: How many actually meet recommended return-to-sport criterion cutoffs? Toole Allison R., Ithurburn Matthew P., Rauh Mitchell J., Hewett Timothy E., Paterno Mark V., Schmitt Laura C. 2017Journal of Orthopaedic and Sports Physical Therapy. 47(11):825–833. doi: 10.2519/jospt.2017.7227. [DOI] [PubMed] [Google Scholar]
- Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament injury? Chung Kyu Sung, Ha Jeong Ku, Yeom Cheol Hyun, Ra Ho Jong, Lim Jin Woo, Kwon Min Soo, Kim Jin Goo. Dec 12;2015 The American Journal of Sports Medicine. 43(12):3013–3021. doi: 10.1177/0363546515606126. [DOI] [PubMed] [Google Scholar]
- Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. Wojtys Edward M., Huston Laura J. 2000American Journal of Sports Medicine. 28(3):336–344. doi: 10.1177/03635465000280030901. [DOI] [PubMed] [Google Scholar]
- Relationship between muscle volume and muscle torque of the hamstrings after anterior cruciate ligament reconstruction. Konishi Yu, Fukubayashi Toru. Jan;2010 Journal of Science and Medicine in Sport. 13(1):101–105. doi: 10.1016/j.jsams.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Deficits in quadriceps strength and patient-oriented outcomes at return to activity after ACL reconstruction. Lepley Lindsey K. May 20;2015 Sports Health: A Multidisciplinary Approach. 7(3):231–238. doi: 10.1177/1941738115578112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Abrams Geoffrey D., Harris Joshua D., Gupta Anil K., McCormick Frank M., Bush-Joseph Charles A., Verma Nikhil N., Cole Brian J., Bach Bernard R. 2014Orthopaedic Journal of Sports Medicine. doi: 10.1177/2325967113518305. [DOI] [PMC free article] [PubMed]
- The utility of limb symmetry indices in return-to-sport assessment in patients with bilateral anterior cruciate ligament reconstruction. Zwolski Christin, Schmitt Laura C, Thomas Staci, Hewett Timothy E, Paterno Mark V. Aug;2016 The American Journal of Sports Medicine. 44(8):2030–2038. doi: 10.1177/0363546516645084. [DOI] [PubMed] [Google Scholar]
- Young athletes after anterior cruciate ligament reconstruction cleared for sports participation: how many actually meet recommended return-to-sport criteria cutoffs? Toole Allison R., Ithurburn Matthew P., Rauh Mitchell J., Hewett Timothy E., Paterno Mark V., Schmitt Laura C. Oct 7;2017 Journal of Orthopaedic & Sports Physical Therapy. :1–27. doi: 10.2519/jospt.2017.7227. [DOI] [PubMed]
- Clinical thresholds for quadriceps assessment after anterior cruciate ligament reconstruction. Kuenze Christopher, Hertel Jay, Saliba Susan, Diduch David R., Weltman Arthur, Hart Joseph M. Feb;2015 Journal of Sport Rehabilitation. 24(1) doi: 10.1123/jsr.2013-0110. [DOI] [PubMed] [Google Scholar]
- Quadriceps strength predicts self-reported function post-ACL reconstruction. Pietrosimone Brian, Lepley Adam S., Harkey Matthew S., Luc-Harkey Brittney A., Troy Blackburn J., Gribble Phillip A., Spang Jeffrey T., Sohn David H. Sep 1;2016 Medicine and Science in Sports and Exercise. 48(9):1671–1677. doi: 10.1249/MSS.0000000000000946. [DOI] [PubMed] [Google Scholar]
- Quadriceps strength changes across the continuum of care in adolescent male and female athletes with anterior cruciate ligament injury and reconstruction. Goto Shiho, Garrison J. Craig, Hannon Joseph P., N. Grondin Angellyn, Bothwell James M., Wang-Price Sharon, Bush Curtis A., Papaliodis Dean N., Dietrich Lindsey N. 2020Physical Therapy in Sport. 46:214–219. doi: 10.1016/j.ptsp.2020.08.016. [DOI] [PubMed] [Google Scholar]
- Knee loading after ACL-R is related to quadriceps strength and knee extension differences across the continuum of care. Garrison J. Craig, Hannon Joseph, Goto Shiho, Kosmopoulos Victor, Aryal Subhash, Bush Curtis, Bothwell James M., Singleton Steven B. 2019Orthopaedic Journal of Sports Medicine. 7(10):1–8. doi: 10.1177/2325967119870155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longitudinal quadriceps strength recovery after anterior cruciate ligament reconstruction with hamstring autograft: patients stratified by preoperative quadriceps strength deficit. Ueda Yuya, Matsushita Takehiko, Shibata Yohei, Takiguchi Kohei, Kida Akihiro, Araki Daisuke, Kanzaki Noriyuki, Hoshino Yuichi, Ono Rei, Sakai Yoshitada, Kuroda Ryosuke. Jul 1;2020 Journal of Sport Rehabilitation. 29(5):602–607. doi: 10.1123/jsr.2018-0236. [DOI] [PubMed] [Google Scholar]
- Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Welling Wouter, Benjaminse Anne, Seil Romain, Lemmink Koen, Zaffagnini Stefano, Gokeler Alli. Dec 24;2018 Knee Surgery, Sports Traumatology, Arthroscopy. 26(12) doi: 10.1007/s00167-018-4916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timeline of gains in quadriceps strength symmetry and patient-reported function early after ACL reconstruction. Pottkotter Kristy A., Di Stasi Stephanie L., Schmitt Laura C., Magnussen Robert A., Paterno V. Mark, Flanigan David C., Kaeding Christopher C., Hewett Timothy E. 2020International Journal of Sports Physical Therapy. 15(6):995–1005. doi: 10.26603/ijspt20200995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fate of the ACL-injured patient: a prospective outcome study. Daniel Dale M., Stone Mary Lou, Dobson Barbara E., Fithian Donald C., Rossman David J., Kaufman Kenton R. 1994The American Journal of Sports Medicine. 22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- Reliability of knee extension and flexion measurements using the Con-Trex isokinetic dynamometer. Maffiuletti Nicola A., Bizzini Mario, Desbrosses Kevin, Babault Nicolas, Munzinger Urs. 2007Clinical Physiology and Functional Imaging. 27(6):346–353. doi: 10.1111/j.1475-097X.2007.00758.x. [DOI] [PubMed] [Google Scholar]
- Angle- and gender-specific quadriceps femoris muscle recruitment and knee extensor torque. Pincivero Danny M., Salfetnikov Yuliya, Campy Robert M., Coelho Alan J. Nov;2004 Journal of Biomechanics. 37(11) doi: 10.1016/j.jbiomech.2004.02.005. [DOI] [PubMed] [Google Scholar]
- Higher hamstring-to-quadriceps isokinetic strength ratio during the first post-operative months in patients with quadriceps tendon compared to hamstring tendon graft following ACL reconstruction. Fischer Felix, Fink Christian, Herbst Elmar, Hoser Christian, Hepperger Caroline, Blank Cornelia, Gföller Peter. Feb 21;2018 Knee Surgery, Sports Traumatology, Arthroscopy. 26(2):418–425. doi: 10.1007/s00167-017-4522-x. [DOI] [PubMed] [Google Scholar]
- Knee muscle strength after quadriceps tendon autograft anterior cruciate ligament reconstruction: systematic review and meta-analysis. Johnston Peta T., McClelland Jodie A., Feller Julian A., Webster Kate E. Sep 7;2021 Knee Surgery, Sports Traumatology, Arthroscopy. 29(9) doi: 10.1007/s00167-020-06311-y. [DOI] [PubMed] [Google Scholar]
- Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Adams Douglas J., Mazzocca Augustus D., Fulkerson John P. Jan;2006 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 22(1):76–79. doi: 10.1016/j.arthro.2005.10.015. [DOI] [PubMed] [Google Scholar]
- Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Ardern Clare L, Taylor Nicholas F, Feller Julian A, Webster Kate E. Nov;2014 British Journal of Sports Medicine. 48(21) doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction—not exactly a one-way ticket back to the preinjury level. Ardern Clare L. May 24;2015 Sports Health: A Multidisciplinary Approach. 7(3):224–230. doi: 10.1177/1941738115578131. [DOI] [PMC free article] [PubMed] [Google Scholar]


