Abstract
Caesarean delivery (C-section) has been increasing worldwide; however, many women from developing countries in Sub-Saharan Africa are deprived of these lifesaving services. This study aimed to explore the impact of certain socioeconomic factors, including respondent’s education, husband’s education, place of residence, and wealth index, on C-section delivery for women in Sub-Saharan Africa. We used pooled data from 36 demographic and health surveys (DHS) in Sub-Saharan Africa. Married women aged 15–49 years who have at least one child in the last five years were considered in this survey. After inclusion and excluding criteria, 234,660 participants were eligible for final analysis. Binary logistic regression was executed to determine the effects of selected socioeconomic factors. The countries were assembled into four sub-regions (Southern Africa, West Africa, East Africa, and Central Africa), and a meta-analysis was conducted. We performed random-effects model estimation for meta-analysis to assess the overall effects and consistency between covariates and utilization of C-section delivery as substantial heterogeneity was identified (I2 > 50%). Furthermore, the meta-regression was carried out to explain the additional amount of heterogeneity by country levels. We performed a sensitivity analysis to examine the effects of outliers in this study. Findings suggest that less than 15% of women in many Sub-Saharan African countries had C-section delivery. Maternal education (OR 4.12; CI 3.75, 4.51), wealth index (OR 2.05; CI 1.94, 2.17), paternal education (OR 1.71; CI 1.57, 1.86), and place of residence (OR 1.51; CI 1.44, 1.58) were significantly associated with the utilization of C-section delivery. These results were also consistent in sub-regional meta-analyses. The meta-regression suggests that the total percentage of births attended by skilled health staff (TPBASHS) has a significant inverse association with C-section utilization regarding educational attainment (respondent & husband), place of residence, and wealth index. The data structure was restricted to define the distinction between elective and emergency c-sections. It is essential to provide an appropriate lifesaving mechanism, such as C-section delivery opportunities, through proper facilities for rural, uneducated, impoverished Sub-Saharan African women to minimize both maternal and infant mortality.
Subject terms: Health care, Risk factors
Introduction
As the millennium development goals (MDGs) ended in 2015, the sustainable development goals (SDGs) emerged with a purpose to lessen the maternal mortality ratio (MMR) to less than 70 per 100,000 live births worldwide by 20301. With the enormous global attempt to restrain the threat of maternal and child death on account of the complicated pregnancy and delivery, maternal mortality is still unabated exclusively in the Sub-Saharan Africa (SSA) region2. The maternal mortality ratio is almost 14 times higher in developing countries than in developed countries worldwide, and the SSA region holds the maximum rates of maternal mortality3. Recently, it was projected that approximately 50% of total maternal mortality from pregnancy-related difficulties happened in Sub-Saharan Africa4. This high maternal mortality suggests the need to ensure evidence-based and high-quality maternal healthcare services, including advanced institutional delivery, skilled birth attendance, and standard approach utilization, such as caesarean section (C-section), to improve this crisis5.
To attain the goal three sustainable development goals, equality and equity inaccessibility to emergency obstetric care incorporating assisted vaginal delivery along with a safe C-section are tremendously crucial6. C-section is a surgical intervention designed to prevent or treat life-threatening maternal or foetal complications7. The potential to perform safe C-section delivery has been a significant improvement in obstetrics in the twentieth century8. Surgical deliveries are recommended exclusively in delivery complications where the health benefits of the intervention outweigh the risks9. However, there is no existence of standardized clinical algorithms for ascertaining the need for a C-section as the decision considers various factors and their changes over time. Consequently, if such a rate exists, which can be called ‘the optimal’ caesarean rate at the population level, it is unknown. A recent statement by the World Health Organization (WHO) on C-section calls for ‘every effort [to] be made to provide C-section to women in need, rather than striving to achieve a specific rate’10.
C-section has become a notable index of evaluating progress in emergency obstetric care and a medium to prevent complications during delivery and labour11. Accordingly, there is growing heed that C-section rates have typically been on the hike, regardless of race, medical condition, and gestational age, albeit unevenly. In developing countries, the C-section prevalence variation stretches from 2 to 39%12,13. According to the WHO, the developing world needed 3.2 million additional C-sections in 2008 while 6.2 million non-essential caesarean deliveries were performed elsewhere14. Global recognition over such upsurge has induced the WHO to recommend that C-section prevalence should not exceed 10–15%15. The previous evidence reveals that the prevalence of C-sections beyond 15% was not associated with reducing maternal and child mortality further16. An ecological study also deduced that in countries where the C-section rate was less than 15%, higher rates were analogous to the lower infant, neonatal, and maternal mortality rates17.
This is undoubtedly tough to narrate the role of C-section in poor-resource settings. Like the world at large, discrepancies exist in the C-section level in Sub-Saharan Africa (SSA) across varied socio-environmental and demographic factors, indicating inaccessibility to health care services18. Evidence shows that the low cost of C-sections is influencing people to prefer the C-section. A systematic review of the literature reveals that the C-section rate varies between 2 and 51% in SSA19,20. Another study stressing the aftermath of C-section in Africa noted that maternal mortality after caesarean delivery is 50 times higher than that of high-income countries and is driven by peripartum haemorrhage and anaesthesia complications21. The same study revealed that complications occurred in 17·4%, mainly were severe intraoperative and postoperative bleeding. Furthermore, maternal mortality was independently associated with a preoperative presentation of placenta praevia, placental abruption, ruptured uterus, antepartum haemorrhage and perioperative severe obstetric haemorrhage, or anaesthesia complications etc. Therefore, countries from SSA face a simultaneous double burden of both underuse and overuse of C-sections like the ‘too little, too late’ and ‘too much, too soon’ dichotomy perceived more extensively in delivery care11.
A previous study showed that the rate of C-section is consistently increasing due to diverse factors in many communities22. Women belonging to higher economic class with better education went through C-section more than women having a formal education and low economic level. Similarly, women who prefer private facilities over the government for delivery suffer more C-sections23. It is also well documented that women’s access to health care facilities with trained birth attendants (TBAs) together with sufficient drugs and supplies of other essentials significantly increased the likelihood of C-sections24,25. However, there is no denying that the additional burden to cover the associated expenses, i.e., medicines and emergency transports, on households could reduce the use of C-sections25,26. Therefore, maintaining the balanced use of C-sections is also very important for overuse, and less use of C-sections can lead to deleterious health outcomes27.
Several studies in the SSA region assessed the disparities among prevalence and influencing factors of C-section, its surgical site infections, and the effect of different government policies on C-section28–31. There are very few works that concentrate only on education, wealth, and place of residence that uses meta-analysis techniques using DHS data in the SSA region. This study identified the impact of these factors on the C-section delivery rate using meta-analysis techniques to estimate a more precise result in SSA.
Methods
Data source and extraction
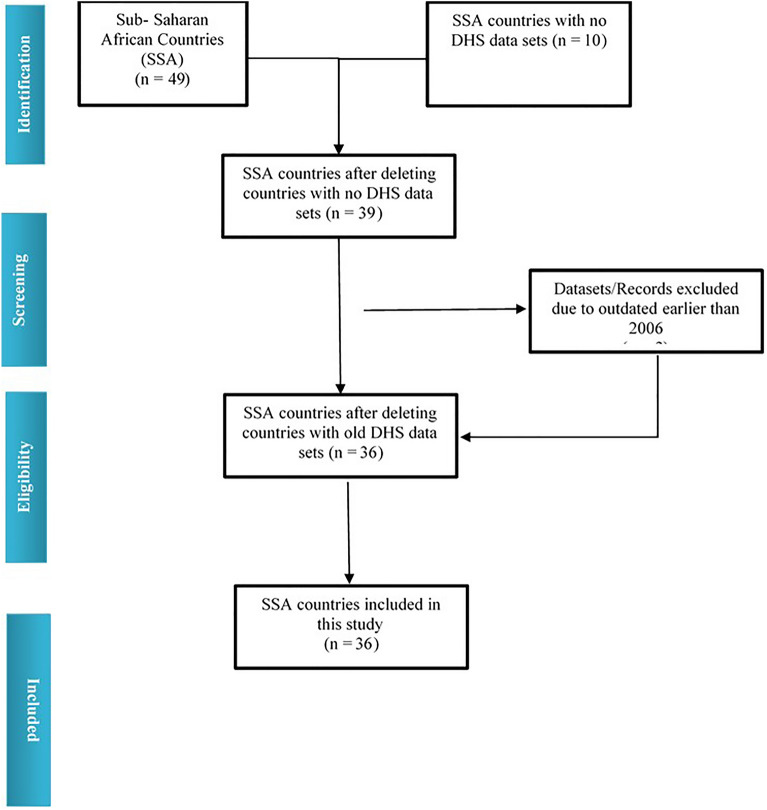
To collect Demographic and Health Survey (DHS) data, a cross-sectional study design is used for large nationally representative samples for every country. Information from the respondents was collected applying the same measures and similar questionnaires. In most of these surveys, a two-stage cluster sampling design with households in urban and rural strata has been used to choose the study respondents. Detailed information about the sampling and data collection methodology is available on the DHS websites32. The information utilized for this investigation was extracted from nationally representative secondary datasets of 36 developing countries (accessed in February 2021) from SSA33. The countries were Angola 2015–2016, Benin 2017–2018, Burkina Faso 2010, Burundi 2016–2017, Cameroon 2018, Chad 2014–2015, Comoros 2012, Congo Democratic Republic 2013–2014, Congo 2011–12, Cote d'Ivoire 2011–12, Eswatini 2006–2007, Ethiopia-2016, Gabon 2012, Gambia 2013, Ghana 2014, Guinea 2018, Kenya 2014, Lesotho 2014, Liberia 2013, Madagascar 2008–2009, Malawi 2015–2016, Mali 2018, Mozambique 2011, Namibia 2013, Niger 2012, Nigeria 2018, Rwanda 2014–2015, Sao Tome and Principe 2008–2009, Senegal 2010–2011, Sierra Leone 2019, South Africa 2016, Tanzania 2015–2016, Togo 2013–2014, Uganda 2016, Zambia 2018, Zimbabwe 2015. Married women of age 15–49 years having a minimum of 1 child during the last five years were considered in this survey. The DHS database contains information from 39 Sub-Saharan African countries (http://dhsprogram.com/data/available-datasets.cfm). We screened all the data set from SSA countries. We selected the data set from 2006 to 2021. We excluded 03 more countries before 2006. Finally, we have selected 36 SSA countries, where similar probability sampling was applied for data collection33 (Fig. 1). After excluding the missing cases, the participants from 36 SSA countries have been included in the study.
Figure 1.
PRISMA (preferred reporting items for systematic reviews and meta-analysis) flow diagram illustrating the process of identifying and including DHS datasets for the random effect meta-analysis.
Variables
The participants of this study were women who chose the C-section as delivery mode during their delivery; therefore, C-section delivery is the response variable. This response variable was categorized into two groups: those who had at least one C-section delivery were considered category ‘Yes’; those with no C-section were classified as ‘No’. For the logistic regression model, the independent variables include maternal education, paternal education, wealth index, place of residence. The categories of the place of residence (‘rural’, ‘urban’), respondent’s education (‘No education’, ‘Primary’, ‘Secondary’, ‘Higher’) and husband’s education (‘No education’, ‘Primary’, ‘Secondary’, ‘Higher’) remain same as it was in the BDHS data set. For the variable wealth index, were categorized it by adding poorer and poor to ‘poor’, middle as middle and rich, and richest to ‘rich’.
For the meta-analysis, we categorized parental education, including paternal and maternal, as ‘Educated’, merging primary, secondary, and higher education, and ‘Not educated’, including the not educated individuals. Wealth index was formulated into ‘Up to middle’ merging the poorest, poorer, and middle, whereas ‘Rich’ was constructed by combining richer and the richest. Place of residence the categories remained the same as it was found in the original dataset as rural and urban.
Moderator
Birth by skilled health staff is recommended by healthcare centres worldwide for a healthy pregnancy period and childbirth. Renowned health organizations train the health staff to ensure safe and convenient delivery34. As a result, these attendants could appropriately assess the delivery mode and provide pregnancy-related awareness throughout gestation. More precisely, they have superior knowledge of dietary intake and subsequent pregnancy-related complications and treatments, enabling them to avoid various health risks. They directly affect childbirth mode, pregnancy care, and pregnancy-related consciousness34. Besides, the total percentage of births attended by skilled health staff (TPBASHS) of a country could be utilized to estimate the effect size and identify additional sources of heterogeneity between C-section delivery and socioeconomic variables; however, meta-regression is scarce on this dimension.
Ethics declarations
The secondary source named Demographic Health Survey (DHS) was utilized to obtain the dataset. The only participant of the DHS program is human. We have got permission from https://dhsprogram.com/ to use the data through strict instructions and data confidentiality assurance. The DHS program has followed Helsinki Declaration (1964) ethical standards to assure ethical approval for each survey. The survey report from its website illustrates the entire survey information, including participants’ selection, sample size determination, ethical approval, sampling procedure, etc.
Consent to participate
Each selected participant in the survey sampling was sent an informed consent before beginning the interview. It is because of ensuring participants’ authorization and confidentiality in the survey.
Statistical analysis
We used statistical software SPSS V.23 (SPSS Inc. Chicago, USA) and R V.3.6.2 (Bell Laboratories, New Jersey, USA) to carry out the analysis. Binary logistic regression was executed using the key factors that impact C-section delivery using pooled data of 36 Sub–Saharan African countries35,36. We also applied meta-analysis techniques on the 36 DHS data from Sub –Saharan Africa37. Heterogeneity was assessed by enumerating values from I2 and p values among datasets38,39. We performed a random-effects model in the meta-analytical approach as significant heterogeneity was found by which we estimated DerSimonian and Laird's pooled effect40,41. The ‘leave-one-out’ sensitivity analysis was conducted to determine the effect of heterogeneity and outliers42. Forest plots were used to display 95% confidence interval (CI), 95% prediction interval, summary measure, and weight of each study for the most significant determinants43. The 95% prediction interval is used to estimate ranges that will define the expected effects for 95% of further studies. Subgroup analyses were applied to find out the regional difference of the influencing factors of C-section delivery across SSA countries.
Further, the authors deployed random-effects meta-regression with the total percentage of births attended by skilled health staff (TPBASHS) as a moderator in order to detect an extra amount of heterogeneity between C-section and socioeconomic variables, including education, place of residence, and wealth index. Test of moderator was performed by meta-regression to identify the significant influence of the moderator on effect size. The study is presented findings of meta-regression through scatterplot, executing in R Studio version 4.0.5. This study used ‘leave-one-country-out’ sensitivity analysis to assess the stability of the results and to examine whether one country had an excessive impact on the meta-analysis44. As a summary measure, we used Odds Ratio (OR), and all findings were weighted to handle bias due to under sampling and oversampling.
Patient and public involvement
We have used nationally representative Demographic and Health Survey (DHS) secondary data sets. for Sub-Saharan African countries, which were collected following rigorous rules by the authorities. That is why any kind of patient and public involvement was not applicable for this study.
Results
Table 1 shows the baseline characteristics for selected variables of 36 Sub-Saharan African countries. The proportion of delivery by caesarean section was lowest in Chad (1.3%); on the other hand, it was highest (24.5%) in South Africa among all countries.
Table 1.
Baseline characteristics table for selected variables for different countries.
| Country name | Respondent’s education n (%) | Wealth Index n (%) | Husband’s Education n (%) | Place of Residence n (%) | Delivery by caesarean (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Not educated | Educated | Up to middle | Rich | Not educated | Educated | Urban | Rural | No | Yes | |
| Angola 2015–16 | 1491 (26.3) | 4169 (73.7) | 3508 (62.0) | 2152 (38.0) | 1115 (19.7) | 4545 (80.3) | 3550(62.7) | 2110(37.3) | 5411 (95.6) | 249 (4.4) |
| Benin 2017–18 | 5262 (66.3) | 2676 (33.7) | 4937 (62.2) | 3000 (37.8) | 4358 (54.9) | 3580 (45.1) | 2989 (37.7) | 4948 (62.3) | 7478 (94.2) | 460 (5.8) |
| Burkina Faso 2010 | 8558 (83.3) | 1717 (16.7) | 6409 (62.4) | 3866 (37.6) | 8325 (81.0) | 1950 (19.0) | 1881 (18.3) | 8394 (81.7) | 10,043 (97.7) | 233 (2.3) |
| Burundi 2016–17 | 3676 (47.2) | 4119 (52.8) | 4960 (63.6) | 2835 (36.4) | 3012 (38.6) | 4783 (61.4) | 713 (9.1) | 7083 (90.9) | 7341 (94.2) | 455 (5.8) |
| Cameroon, 2018 | 1544 (30.1) | 3593 (69.9) | 3368 (65.6) | 1769 (34.4) | 1251 (24.4) | 3886 (75.6) | 2238 (43.6) | 2899 (56.4) | 4950 (96.3) | 188 (3.7) |
| Chad 2014–15 | 6820 (66.8) | 3391 (8.8) | 6362 (62.3) | 3849 (37.7) | 5986 (58.6) | 4224 (41.4) | 2005 (19.6) | 8206 (80.4) | 10,260 (98.7) | 137 (1.3) |
| Comoros, 2012 | 848 (43.6) | 1098 (56.4) | 1248 (64.1) | 698 (35.9) | 725 (37.3) | 1221 (62.7) | 568 (29.2) | 1378 (70.8) | 1732 (89.0) | 214 (11.0) |
| Congo Democratic Republic, 2013–14 | 1894 (18.7) | 8245 (81.3) | 6577 (64.9) | 3562 (35.1) | 786 (7.8) | 9353 (92.2) | 3121 (30.8) | 7018 (69.2) | 9561 (94.3) | 578 (5.7) |
| Congo, 2011–12 | 317 (6.3) | 4741 (93.7) | 3148 (62.2) | 1910 (37.8) | 171 (3.4) | 4887 (96.6) | 3265 (64.5) | 1794 (35.5) | 4741 (93.7) | 318 (6.3) |
| Cote d'Ivoire, 2011–12 | 2892 (65.9) | 1497 (34.1) | 2876 (65.5) | 1513 (34.5) | 2352 (53.6) | 2037 (46.4) | 1663 (37.9) | 2726 (62.1) | 4264 (97.1) | 125 (2.9) |
| Eswatini, 2006–07 | 132 (10.3) | 1146 (89.7) | 773 (60.5) | 505 (39.5) | 176 (13.8) | 1102 (86.2) | 293 (22.9) | 985 (77.1) | 1167 (91.3) | 111 (8.7) |
| Ethiopia-2016 | 4474 (63.3) | 2592 (36.7) | 4559 (64.5) | 2507 (35.5) | 3346 (47.4) | 3720 (52.6) | 872 (12.3) | 6194 (87.7) | 6903 (97.7) | 163 (2.3) |
| Gabon, 2012 | 194 (7.5) | 2389 (92.5) | 1562 (60.5) | 1021 (39.5) | 204 (7.9) | 2379 (92.1) | 2212 (85.6) | 371 (14.4) | 2274 (88.0) | 309 (12.0) |
| Gambia 2013 | 2947 (59.8) | 1979 (40.2) | 2999 (60.9) | 1927 (39.1) | 3042 (61.7) | 1884 (38.3) | 2411 (48.9) | 2515 (51.1) | 4808 (97.6) | 118 (2.4) |
| Ghana, 2014 | 1035 (28.1) | 2645 (71.9) | 2220 (60.3) | 1460 (39.7) | 807 (21.9) | 2873 (78.1) | 1687 (45.8) | 1993 (54.2) | 3169 (86.1) | 511 (13.9) |
| Guinea, 2018 | 3902 (77.9) | 1105 (22.1) | 3312 (66.2) | 1694 (33.8) | 3653 (73.0) | 1353 (27.0) | 1407 (28.1) | 3600 (71.9) | 4854 (97.0) | 152 (3.0) |
| Kenya, 2014 | 654 (10.6) | 5541 (89.4) | 3592 (58.0) | 2604 (42.0) | 502 (8.1) | 5693 (91.9) | 2400 (38.7) | 3796 (61.3) | 5640 (91.0) | 556 (9.0) |
| Lesotho, 2014 | 19 (0.8) | 2231 (99.2) | 1345 (59.8) | 905 (40.2) | 297 (13.2) | 1953 (86.8) | 648 (28.8) | 1602 (71.2) | 2017 (89.6) | 233 (10.4) |
| Liberia, 2013 | 1710 (44.6) | 2124 (55.4) | 2534 (66.1) | 1300 (33.9) | 918 (23.9) | 2916 (76.1) | 1961 (51.1) | 1873 (48.9) | 3675 (95.9) | 159 (4.1) |
| Madagascar, 2008–09 | 1845 (23.2) | 6096 (76.8) | 5155 (64.9) | 2786 (35.1) | 1733 (21.8) | 6208 (78.2) | 960 (12.1) | 6981 (87.9) | 7808 (98.3) | 134 (1.7) |
| Malawi, 2015–16 | 1367 (12.4) | 9643 (87.6) | 6987 (63.5) | 4023 (36.5) | 1089 (9.9) | 9921 (90.1) | 1590 (14.4) | 9420 (85.6) | 10,316 (93.7) | 693 (6.3) |
| Mali, 2018 | 4466 (73.0) | 1650 (27.0) | 3855 (63.0) | 2261 (37.0) | 4511 (73.7) | 1606 (26.3) | 1222 (20.0) | 4895 (80.0) | 5929 (96.9) | 188 (3.1) |
| Mozambique, 2011 | 2545 (36.4) | 4439 (63.6) | 4521 (64.7) | 2463 (35.3) | 1801 (25.8) | 5183 (74.2) | 1897 (27.2) | 5087 (72.8) | 6694 (95.9) | 290 (4.1) |
| Namibia, 2013 | 138 (7.5) | 1708 (92.5) | 1121 (60.8) | 724 (39.2) | 224 (12.1) | 1622 (87.9) | 994 (53.9) | 851 (46.1) | 1552 (84.1) | 294 (15.9) |
| Niger, 2012 | 6636 (85.1) | 1165 (14.9) | 4721 (60.5) | 3080 (39.5) | 6387 (81.9) | 1414 (18.1) | 1062 (13.6) | 6739 (86.4) | 7674 (98.4) | 127 (1.6) |
| Nigeria, 2018 | 9263 (45.8) | 10,970 (54.2) | 12,975 (64.1) | 7258 (35.9) | 7335 (36.2) | 12,899 (63.8) | 7922 (39.2) | 12,311 (60.8) | 19,590 (96.8) | 643 (3.2) |
| Rwanda 2014–15 | 822 (15.2) | 4588 (84.8) | 3521 (65.1) | 1889 (34.9) | 919 (17.0) | 4491 (83.0) | 897 (16.6) | 4514 (83.4) | 4709 (87.0) | 701 (13.0) |
| Sao Tome and Principe, 2008–09 | 9263 (45.8) | 10,970 (54.2) | 12,975 (64.1) | 7258 (35.9) | 7335 (36.2) | 12,899 (63.8) | 7922 (39.2) | 12,311 (60.8) | 19,590 (96.8) | 643 (3.2) |
| Senegal, 2010–11 | 4804 (71.6) | 1910 (28.4) | 4277 (63.7) | 2436 (36.3) | 5033 (75.0) | 1681 (25.0) | 2586 (38.5) | 4128 (61.5) | 6258 (93.2) | 456 (6.8) |
| Sierra Leone, 2019 | 3404 (58.7) | 2399 (41.3) | 3899 (67.2) | 1904 (32.8) | 3232 (55.7) | 2571 (44.3) | 1960 (33.8) | 3843 (66.2) | 5565 (95.9) | 237 (4.1) |
| South Africa, 2016 | 28 (2.2) | 1280 (97.8) | 826 (63.1) | 482 (36.9) | 47 (3.6) | 1262 (96.4) | 962 (73.5) | 347 (26.5) | 988 (75.5) | 321 (24.5) |
| Tanzania, 2015–16 | 1166 (20.5) | 4516 (79.5) | 3560 (62.7) | 2122 (37.3) | 752 (13.2) | 4930 (86.8) | 1569 (27.6) | 4112 (72.4) | 5284 (93.0) | 398 (7.0) |
| Togo, 2013–14 | 1832 (40.4) | 2708 (59.6) | 2755 (60.7) | 1785 (39.3) | 1196 (26.3) | 3344 (73.7) | 1653 (36.4) | 2886 (63.6) | 4223 (93.0) | 317 (7.0) |
| Uganda, 2016 | 860 (10.7) | 7152 (89.3) | 4956 (61.9) | 3056 (38.1) | 517 (6.5) | 7495 (93.5) | 1749 (21.8) | 6263 (78.2) | 7438 (92.8) | 574 (7.2) |
| Zambia, 2018 | 512 (9.6) | 4795 (90.4) | 3352 (63.2) | 1954 (36.8) | 322 (6.1) | 4985 (93.9) | 1965 (37.0) | 3342 (63.0) | 5012 (94.5) | 294 (5.5) |
| Zimbabwe, 2015 | 50 (1.2) | 4113 (98.8) | 2444 (58.7) | 1718 (41.3) | 54 (1.3) | 4109 (98.7) | 1345 (32.3) | 2818 (67.7) | 3899 (93.7) | 264 (6.3) |
Table 2 shows that the respondent from an urban area is 1.51 (OR 1.51; CI 1.44, 1.58) times more likely to use C-section delivery than the respondents forms rural areas. Respondents with high education were 4.12 times (OR 4.12; CI 3.75, 4.51) more likely to use C-section delivery than the respondents with no education. A respondent with a higher educated husband was 1.71 times (OR 1.71; CI 1.57, 1.86) more likely to use C-section delivery than the respondent with a not educated husband. A wealthy family respondent was 2.05 times (OR 2.05; CI 1.94, 2.17) more likely to use C-section delivery than a respondent from a low-income family.
Table 2.
Results of the BLR model using pooled data of 36 Sub-Saharan African countries.
| Variables | AOR | p value | 95% CI for AOR | OR | p value | 95% CI for OR | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | |||||
| Place of residence | ||||||||
| Rural (ref) | ||||||||
| Urban | 1.51 | < 0.000 | 1.44 | 1.58 | 2.99 | < 0.000 | 2.88 | 3.11 |
| Respondent’s education | ||||||||
| No Education (ref) | ||||||||
| Primary | 1.65 | < 0.000 | 1.55 | 1.76 | 2.23 | < 0.000 | 2.11 | 2.36 |
| Secondary | 2.02 | < 0.000 | 1.89 | 2.16 | 3.82 | < 0.000 | 3.62 | 4.04 |
| Higher | 4.12 | < 0.000 | 3.75 | 4.51 | 11.07 | < 0.000 | 10.32 | 11.87 |
| Husband’s education | ||||||||
| No Education (ref) | ||||||||
| Primary | 1.49 | < 0.000 | 1.39 | 1.596 | 2.19 | < 0.000 | 2.06 | 2.33 |
| Secondary | 1.42 | < 0.000 | 1.33 | 1.528 | 3.16 | < 0.000 | 2.98 | 3.34 |
| Higher | 1.71 | < 0.000 | 1.57 | 1.862 | 6.88 | < 0.000 | 6.44 | 7.35 |
| Wealth index | ||||||||
| Poor (ref) | ||||||||
| Middle | 1.32 | < 0.000 | 1.24 | 1.41 | 1.66 | < 0.000 | 1.56 | 1.77 |
| Rich | 2.05 | < 0.000 | 1.94 | 2.17 | 4.04 | < 0.000 | 3.85 | 4.23 |
AOR adjusted odds ratio, CI confidence interval, OR odds ratio; ref reference category.
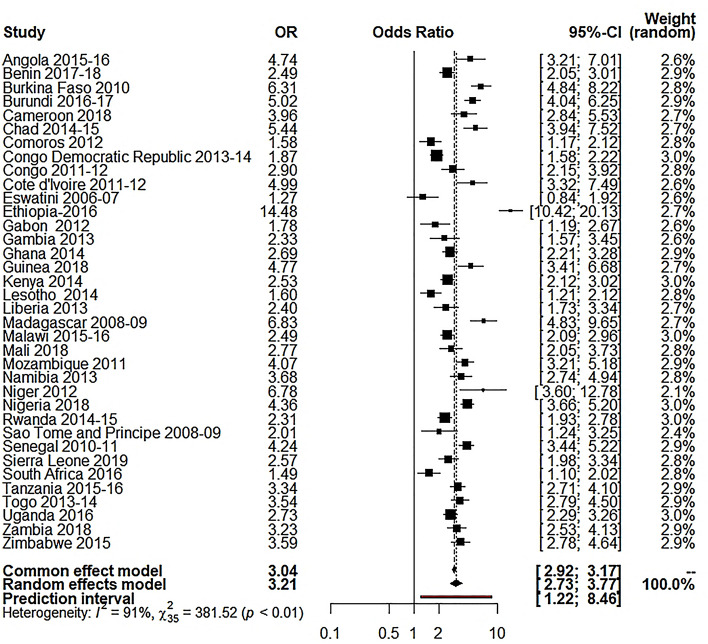
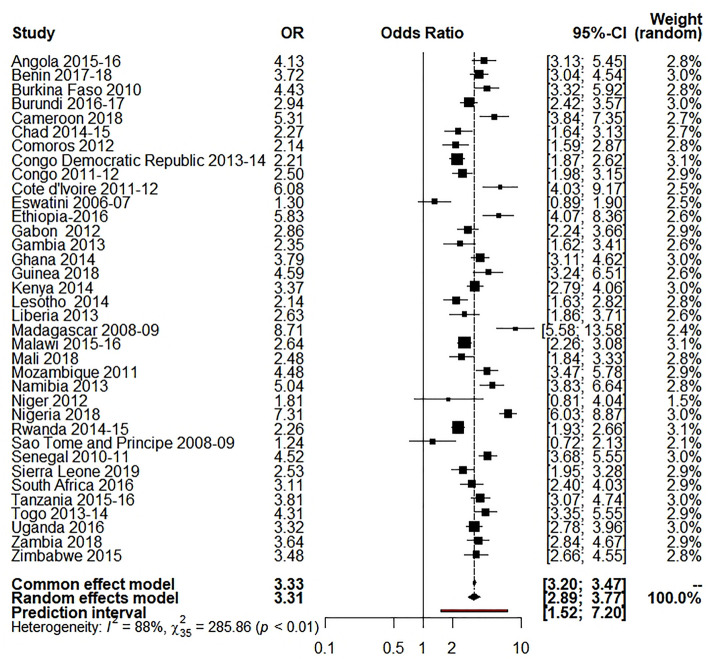
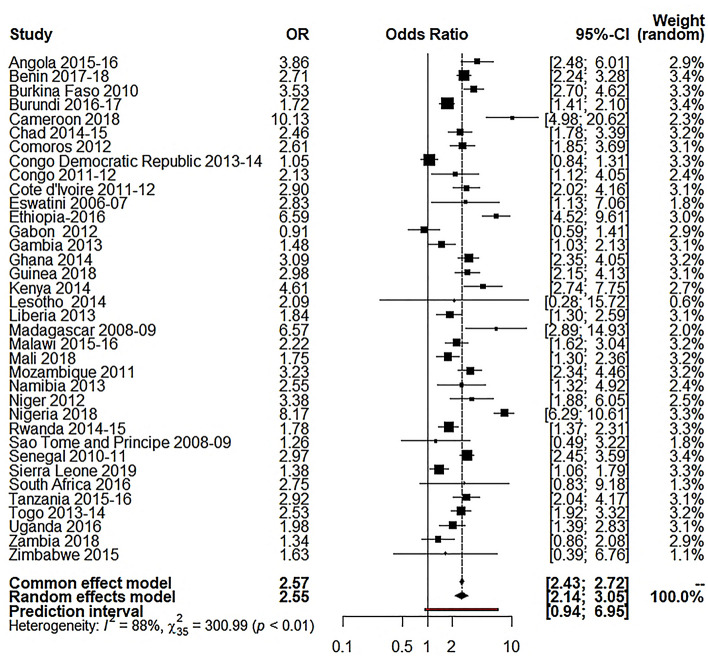
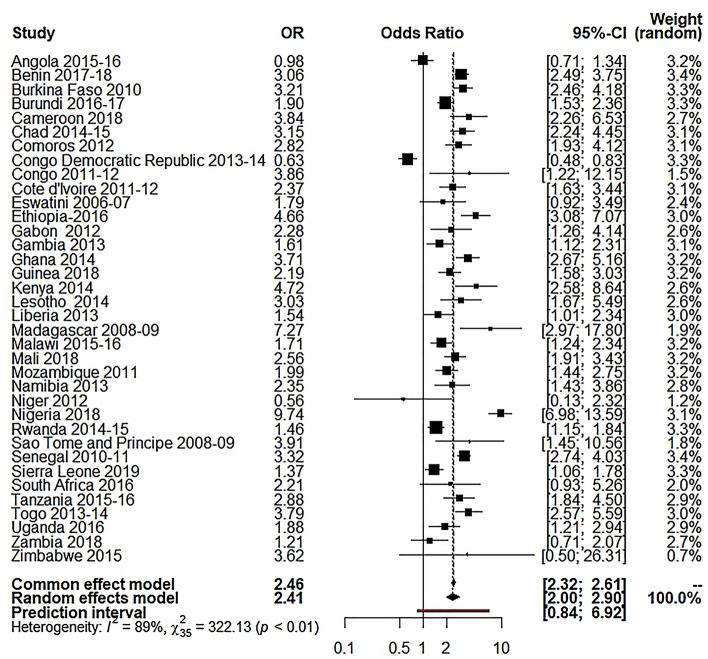
Our study used the random-effects model as the study showed high between-study variations (heterogeneity). Table 3 shows the results of random effect model estimation results of 36 Sub-Saharan African countries, and Table 4 shows the summary effect of different explanatory variables. For respondent’s education, the overall OR was 2.55 (95% CI 2.14 to 3.05; p 0.0001; 95% PI: 0.94 to 6.95), meaning the educated respondents were 155% more likely to use caesarian section delivery than the illiterate respondents. About 85.5% of the variation (I2 = 85.5%) was found for this variable. For husband’s education, the overall OR was 2.41 (95% CI 2.00 to 2.90; p 0.0001; 95% PI: 0.84 to 6.92), meaning the respondents with educated husbands were 141% more likely to use C-section delivery than the respondents with illiterate husband (I2 = 89.3%). For the place of residence, the overall OR was 3.21 (95% CI 2.73 to 3.77; p 0.0001; 95% PI: 1.22 to 8.46), which reveals the utilization of C-section delivery was 221% higher to the individuals who came from urban areas compared to those who were from rural settings (I2 90.8%,). For wealth index, I2 was 87.8%, where the overall OR was 3.31 (95% CI 2.89 to 3.77; p 0.0001; 95% PI: 1.52 to 7.20), which reveals that the utilization of C-section delivery was 231% higher for the individuals from rich families compared to the respondents from low-income families.
Table 3.
Random-effects model estimation of odds ratio for different variables on 36 selected Sub- Saharan African countries.
| Country(s) | Wealth index OR [95% CI] | Respondent’s education OR [95% CI] | Husband’s education OR [95% CI] | Place of residence OR [95% CI] |
|---|---|---|---|---|
| Angola 2015–2016 | 4.13 [3.13; 5.45] | 3.86 [2.48; 6.01] | 0.98 [0.71; 1.34] | 4.74 [3.21; 7.01] |
| Benin 2017–2018 | 3.72 [3.04; 4.54] | 2.71 [2.24; 3.28] | 3.06 [2.49; 3.75] | 2.49 [2.05; 3.01] |
| Burkina Faso 2010 | 4.43 [3.32; 5.92] | 3.53 [2.70; 4.62] | 3.21 [2.46; 4.18] | 6.31 [4.84; 8.22] |
| Burundi 2016–2017 | 2.94 [2.42; 3.57] | 1.72 [1.41; 2.10] | 1.90 [1.53; 2.36] | 5.02 [4.04; 6.25] |
| Cameroon 2018 | 5.31 [3.84; 7.35] | 10.13 [4.98; 20.62] | 3.84 [2.26; 6.53] | 3.96 [2.84; 5.53] |
| Chad 2014–2015 | 2.27 [1.64; 3.13] | 2.46 [1.78; 3.39] | 3.15 [2.24; 4.45] | 5.44 [3.94; 7.52] |
| Comoros 2012 | 2.14[1.59; 2.87] | 2.61 [1.85; 3.69] | 2.82 [1.93; 4.12] | 1.58 [1.17; 2.12] |
| Congo Democratic Republic 2013–2014 | 2.21 [1.87; 2.62] | 1.05 [0.84; 1.31] | 0.63 [0.48; 0.83] | 1.87 [1.58; 2.22] |
| Congo 2011–2012 | 2.50 [1.98; 3.15] | 2.13 [1.12; 4.05] | 3.86 [1.22; 12.15] | 2.90 [2.15; 3.92] |
| Cote d'Ivoire 2011–2012 | 6.08 [4.03; 9.17] | 2.90 [2.02; 4.16] | 2.37 [1.63; 3.44] | 4.99 [3.32; 7.49] |
| Eswatini 2006–2007 | 1.30 [0.89; 1.90] | 2.83 [1.13; 7.06] | 1.79 [0.92; 3.49] | 1.27 [0.84; 1.92] |
| Ethiopia-2016 | 5.83 [4.07; 8.36] | 6.59 [4.52; 9.61] | 4.66 [3.08; 7.07] | 14.48 [10.42; 20.13] |
| Gabon 2012 | 2.86 [2.24; 3.66] | 0.91 [0.59; 1.41] | 2.28 [1.26; 4.14] | 1.78 [1.19; 2.67] |
| Gambia 2013 | 2.35 [1.62; 3.41] | 1.48 [1.03; 2.13] | 1.61 [1.12; 2.31] | 2.33 [1.57; 3.45] |
| Ghana 2014 | 3.79 [3.11; 4.62] | 3.09 [2.35; 4.05] | 3.71 [2.67; 5.16] | 2.69 [2.21; 3.28] |
| Guinea 2018 | 4.59 [3.24; 6.51] | 2.98 [2.15; 4.13] | 2.19 [1.58; 3.03] | 4.77 [3.41; 6.68] |
| Kenya 2014 | 3.37 [2.79; 4.06] | 4.61 [2.74; 7.75] | 4.72 [2.58; 8.64] | 2.53 [2.12; 3.02] |
| Lesotho 2014 | 2.14 [1.63; 2.82] | 2.09 [0.28; 15.72] | 3.03 [1.67; 5.49] | 1.60 [1.21; 2.12] |
| Liberia 2013 | 2.63 [1.86; 3.71] | 1.84 [1.30; 2.59] | 1.54 [1.01; 2.34] | 2.40 [1.73; 3.34] |
| Madagascar 2008–09 | 8.71 [5.58; 13.58] | 6.57 [2.89; 14.93] | 7.27 [2.97; 17.80] | 6.83 [4.83; 9.65] |
| Malawi 2015–16 | 2.64 [2.26; 3.08] | 2.22 [1.62; 3.04] | 1.71 [1.24; 2.34] | 2.49 [2.09; 2.96] |
| Mali 2018 | 2.48 [1.84; 3.33] | 1.75 [1.30; 2.36] | 2.56 [1.91; 3.43] | 2.77 [2.05; 3.73] |
| Mozambique 2011 | 4.48 [3.47; 5.78] | 3.23 [2.34; 4.46] | 1.99 [1.44; 2.75] | 4.07 [3.21; 5.18] |
| Namibia 2013 | 5.04 [3.83; 6.64] | 2.55 [1.32; 4.92] | 2.35 [1.43; 3.86] | 3.68 [2.74; 4.94] |
| Niger 2012 | 1.81 [0.81; 4.04] | 3.38 [1.88; 6.05] | 0.56 [0.13; 2.32] | 6.78 [3.60; 12.78] |
| Nigeria 2018 | 7.31 [6.03; 8.87] | 8.17 [6.29; 10.61] | 9.74 [6.98; 13.59] | 4.36 [3.66; 5.20] |
| Rwanda 2014–15 | 2.26 [1.93; 2.66] | 1.78 [1.37; 2.31] | 1.46 [1.15; 1.84] | 2.31 [1.93; 2.78] |
| Sao Tome and Principe 2008–09 | 1.24 [0.72; 2.13] | 1.26 [0.49; 3.22] | 3.91 [1.45; 10.56] | 2.01 [1.24; 3.25] |
| Senegal 2010–11 | 4.52 [3.68; 5.55] | 2.97 [2.45; 3.59] | 3.32 [2.74; 4.03] | 4.24 [3.44; 5.22] |
| Sierra Leone 2019 | 2.53 [1.95; 3.28] | 1.38 [1.06; 1.79] | 1.37 [1.06; 1.78] | 2.57 [1.98; 3.34] |
| South Africa 2016 | 3.11 [2.40; 4.03] | 2.75 [0.83; 9.18] | 2.21 [0.93; 5.26] | 1.49 [1.10; 2.02] |
| Tanzania 2015–2016 | 3.81 [3.07; 4.74] | 2.92 [2.04; 4.17] | 2.88 [1.84; 4.50] | 3.34 [2.71; 4.10] |
| Togo 2013–2014 | 4.31 [3.35; 5.55] | 2.53 [1.92; 3.32] | 3.79 [2.57; 5.59] | 3.54 [2.79; 4.50] |
| Uganda 2016 | 3.32 [2.78; 3.96] | 1.98 [1.39; 2.83] | 1.88 [1.21; 2.94] | 2.73 [2.29; 3.26] |
| Zambia 2018 | 3.64 [2.84; 4.67] | 1.34 [0.86; 2.08] | 1.21 [0.71; 2.07] | 3.23 [2.53; 4.13] |
| Zimbabwe 2015 | 3.48 [2.66; 4.55] | 1.63 [0.39; 6.76] | 3.62 [0.50; 26.31] | 3.59 [2.78; 4.64] |
| 87.8% [84.1; 90.6] | 88.5% [85.1; 91.1] | 89.3% [86.2; 91.7] | 90.8% [88.3; 92.8] | |
| 0.1140 | 0.2268 | 0.2780 | 0.1644 | |
| 95% PI | [1.52; 7.20] | [0.94; 6.95] | [0.84; 6.92] | [1.22; 8.46] |
OR odds ratio, CI confidence interval, PI prediction interval.
Table 4.
Random-effects model estimation (summary effect) for different variables on 36 selected Sub- Saharan African countries.
| Variables | Random effects model | |||
|---|---|---|---|---|
| OR | p value | 95% CI | ||
| Lower bound | Upper bound | |||
| Respondent’s education | 2.55 | 0.0001 | 2.14 | 3.05 |
| Husband’s education | 2.41 | 0.0001 | 2.00 | 2.90 |
| Place of residence | 3.21 | 0.0001 | 2.73 | 3.77 |
| Wealth index | 3.31 | 0.0001 | 2.89 | 3.77 |
OR odds ratio, CI confidence interval.
Table 5 and Fig. 2 show that place of residence significantly affected the C-section delivery concerning the region in SSA countries. For instance, women who lived in urban areas were more likely to utilize C-section delivery in the East Africa region (OR 3.56, p < 0.01, I2 = 94%) than the other regions of SSA countries. Figure 3 and Table 5 show that the respondents from a rich family background were more likely to take C-section delivery. The West Africa region has the highest tendency of C-section (OR 3.66, p < 0.01, I2 = 87%) than the other SSA regions.
Table 5.
Sub-group analysis for different factors.
| Variables | Central Africa | West Africa | East Africa | Southern Africa | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | p value | OR (95%CI) | p value | OR (95%CI | p value | OR (95%CI | p value | |
| Place of residence | 3.14 [2.24; 4.43] | < 0.01 89% | 3.45 [2.85; 4.18] | < 0.01 84% | 3.56 [2.76; 4.60] | < 0.01 94% | 1.84 [1.15; 2.97] | < 0.01 89% |
| Wealth index | 2.92 [2.25; 3.79] | < 0.01 86% | 3.66 [2.95; 4.55] | < 0.01 87% | 3.46 [2.93; 4.09] | < 0.01 85% | 2.60 [1.55; 4.35] | < 0.01 92% |
| Respondent’s education | 2.26 [1.37; 3.72] | < 0.01 82% | 2.64 [2.01; 3.47] | < 0.01 91% | 2.65 [2.03; 3.47] | < 0.01 84% | 2.63 [1.64; 4.22] | < 0.01 0.00% |
| Husband’s education | 2.08 [1.20; 3.62] | < 0.01 92% | 2.70 [2.01; 3.63] | < 0.01 91% | 2.37 [1.85; 3.04] | < 0.01 78% | 2.35 [1.73; 3.21] | < 0.01 0.00% |
Q heterogenic statistic, I2 Between study variation, OR odds ratio, CI confidence interval.
Figure 2.
Forest plot for the place of residence.
Figure 3.
Forest plot for wealth index.
Figure 4 indicates that the respondent’s education significantly influenced the C-section delivery in SSA countries. For instance, educated women were more likely to utilize C-section delivery in the East Africa region (OR 2.65, p < 0.01, I2 = 84%) than the other regions of SSA countries. In Fig. 5, it is clear that the husband’s education significantly influenced the utilization of C-sections across the SSA countries. Results indicated that the respondents with educated husbands were more prone to use C-section delivery in West Africa (OR 2.71, < 0.01, I2 = 91%).
Figure 4.
Forest plot for respondent’s education.
Figure 5.
Forest plot for husband’s education.
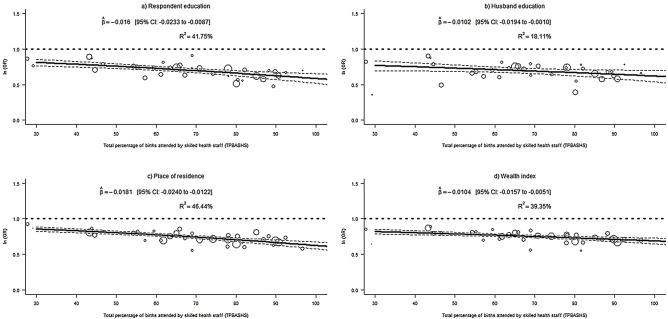
Tests of moderator for educational attainment, residence, and wealth index are exhibited in Table 6. The findings reveal that these tests are statistically significant for all socioeconomic variables. Consequently, TPBASHS has a significant influence on the countries’ effect size and could significantly explain the extra amount of heterogeneity for all four variables.
Table 6.
Output of test of moderator for different variables on 36 selected Sub- Saharan African countries.
| Variables | Respondent education | Husband education | Place of residence | Wealth index |
|---|---|---|---|---|
| Moderator | TPBASHS | TPBASHS | TPBASHS | TPBASHS |
| Estimate | 18.55 | 4.70 | 37.09 | 14.55 |
| P-value | < 0.0001 | 0.0302 | < 0.0001 | 0.0001 |
TPBASHS total percentage of births attended by skilled health staff.
Figure 6 shows the odds of C-section utilization to determine the influence of TPBASHS in all 36 countries from the Sub-Saharan African sub-continent. A significant negative association is observed between TPBASHS and C-section delivery for all four socioeconomic variables. For respondent educational attainment and accommodation, the estimated value of TPBASHS were -0.0160 (95% CI − 0.0233 to − 0.0087; R2 = 41.75%) and − 0.0181 (95% CI − 0.0240 to − 0.0122; R2 = 46.44%). The findings also include that 41.75% (respondent education) and 46.44% (place of residence) of variation in true effect sizes could be explained by TPBASHS.
Figure 6.
Meta-regressions of C-section delivery and socio-economic factors, (a) respondent education: TPBASHS (b) husband education: TPBASHS (c) place of residence: TPBASHS (d) wealth index: TPBASHS.
Discussion
Over past decades, an uncertain increase in C-section rate is occurring. Education, wealth, and residence were strongly associated with the utilization of C-section in the SSA regions. The current study was more informative in providing the rate and association of C-section delivery with education, wealth, and place of residence as compared to that of previous findings. In the current study, the highest caesarean rate was found in Latin America and the Caribbean regions (40.5%), followed by Northern America (32.3%), Oceania (31.1%), Europe (25%), Asia (19.2%), and Africa (7.3%). This trend is increasing worldwide, especially in Egypt, Turkey, Dominican Republic, Georgia, and China, except for two countries (Guinea and Nigeria). The C-section rate decreased in Zimbabwe. These different rates of C-section in different countries showed that it was varying widely among the SSA countries, while WHO recommends that it should be 5–15%45. Dikete et al. reported that C-section rate in sub-Saharan Africa was 14 to 24%, which showed variation from the current study46. Bonsaffoh et al. reported a higher level of C-section rate i.e., 46%, as compared to current findings47. Betran et al. reported a study similar to the present finding in which 18.6% of all births occurred by C-section. In that previous finding, the highest caesarean rate was in Latin America, Caribbean regions, and Northern America (42.9%) followed by northern Africa (27.8%), Africa (7.3%), Saharan Africa (3.5%). Sanni et al. reported a study dissimilar to the present study in which the public health care centres rate of C-section was 3% in Burana and 15.6% in Ghana. While the private health care centers were having a C-section rate of 0% and 64% in Sao tome and Rwanda48.
A metanalysis on 36 different countries of sub-Saharan showed that 41.75%, 18.11%, 46.44%, and 36.35% of the C-section deliveries occur due to respondent education, husband education, place of residence, and wealth index, respectively. The BLR model and meta-analysis revealed that parents’ education is a crucial factor that is the reason behind the increased rate of C-sections. Educated respondents are more likely to use C-section delivery compared to respondents with no education. Regarding the association of C-section rate with education, the current study showed similarity with many of the previous studies except a few ones. Majid et al. (2019) presented a study in Iran that showed that the probability of utilizing the C-section is higher among educated women than women having lower education49. Arendt et al. (2017), Feng et al. (2020), Nababan et al. (2018), and Divyamol et al. (2016) also indicated that an increase in maternal education level leads to C-section delivery as educated women make their own decision regarding delivery, and they, in general, prefer C-section delivery50–53. However, previous findings of Epistein et al., Lee et al., and Mumtaz et al. reported that the educated women prefer C-section as the level of pain is lower, and they believe it is safer and interferes less with the workload, leisure time, and socially more prestigious than the normal vaginal delivery49,54,55. Another study by Long et al. (2015) showed that the overall OR for paternal education also showed that husbands with education are more likely to use C-section delivery than husbands with no education. The result delivered a similar statement from the BLR model and was consistent with previous studies56. A study reported by Bandori et al. showed exception. It showed that high education is not always positively associated with the likelihood of having the C-section. Therefore, in South Korea, the negative association between education and C-section rate has also been seen in the literature. The reason for this exception is that the education is also providing information on health-promoting behaviour, more educated women have more knowledge about the risk of unnecessary C-sections57–59.
The second determent highlighted by this study was the place of residence that plays an essential role in the increased C-section rate. The utilization of C-section delivery is higher to individuals from urban areas, whereas the rate is comparatively lower to individuals from rural settings. Similar to the current study, a previous study reported by Bahadori et al. (2013) showed that the women from rural areas had less chance to utilize the C-section delivery than women from urban areas57. Another study showed similarity with the current study by describing the prevalence of C-sections rates ranging from 4.6% to 12.2% for urban areas, whereas the prevalence of C-section rate ranging from 1.6% to 3.9% for rural areas60. The findings of this study are also in line with the previous studies, which suggest that the prevalence of C-sections in urban areas is significantly higher than those in rural areas. Maybe women who live in rural areas have fewer delivery mode options, awareness, and limited financial resources58,61,62. Based on 80 demographic and health surveys conducted in 26 countries in Southern Asia and SSA, a study reported by Cavallaro et al. (2013) revealed that women from urban areas were more likely to utilize the C-section delivery than rural women59. Availability, accessibility, and affordability of C-sections in urban areas women are more than the rural women, more private C-section facilities and higher women employment rate in urban areas could be the reasons behind the high caesarean rate in urban areas compared to rural areas63,64.
Wealth status is another determinant of increased C-section. Wealthy families utilize C-sections more than low-income families, which is in line with current findings. Previous studies reported that the C-section tendency is more among women with a wealthy family background than women with low-income family background55,65–67, and the other study reveals that 12.3% of the rich women had a C-sections delivery compared to 1.7% of the poor women60. Different studies suggested that poor women in the developing world cannot afford this lifesaving procedure and give birth at home, which is another reason for wealthy family women's high caesarean delivery in SSA48,68,69. A data analysis based on over 20,000 births shows that women of higher socioeconomic backgrounds who had better access to antenatal services are the most likely to undergo a C-section70. However, the opposite trend has also been observed in developed countries, where higher education and economic status were protective against C-sections as awareness and knowledge of childbirth are expected to be high among this group of women71.
Strength and limitation
This study used a large sample size involving multiple nationally representative datasets from 36 countries in SSA to investigate the prevalence of C-sections in the sub-Sahara Africa region. We combined two methods: binary logistic regression and meta-analysis of 36 DHS data of Sub-Saharan African countries. The integrated findings enlarged the validity of the outcome of the research. We unfolded a new research approach by introducing this mixed-method design. Because of its extensive and acute quality, better knowledge and insights could be generated. Also, we applied subgroup analysis to find out the regional effect.
Nonetheless, the data lacks information relating to clinical indications for C-sections, as the data did not distinguish between elective and emergency C-sections. Also, the use of this information for decision-making and comparison should consider the cross-sectional nature of the data, which is inadequate to sufficiently establish causality. Another limitation is that for estimating OR from random-effects meta-analysis, we had to create 2 × 2 cross-tabulation for which each variable was categorized into two categories only. Moreover, a vast number of factors that could influence C-sections could not be included in our study because the DHS has very limited information on both supply- and demand-side variables regarding C-section.
Conclusion
The findings from the present study show that educated women and husbands, women residing in the urban area, and the wealthiest households are more likely to utilize C-section delivery in the Sub-Saharan region. Additionally, the higher percentage of births attended by skilled health staff of a country can significantly reduce the C-section delivery for variables educational attainment (respondent & husband), place of residence, and wealth index, exhibited by meta-regression. Although maternal, neonatal, and infant mortality and morbidity can be influenced by unnecessary C-sections, it can save women and their new-born lives in case of life-threatening pregnancy and childbirth-related complications. Therefore, our results suggest that strategies are needed to provide C-sections through proper facilities for rural, uneducated, impoverished Sub-Saharan African women to minimize maternal and infant mortality so that they can get access to the lifesaving procedure when necessary. Furthermore, the significant role of skilled health staff in the delivery period must be illustrated among pregnant women by health-related programs in each Sub-Saharan African country.
Supplementary Information
Acknowledgements
We would like to show our appreciation to the Demographic and Health Surveys (DHS) Program for offering data access used in this research. The authors also declare the following issues.
Author contributions
Conceptualization: M.A.I. Data curation: M.A.I., N.J.S. Formal analysis: M.A.I., N.J.S. Investigation: M.A.I., N.J.S. Methodology: M.A.I., N.J.S. Resources: M.A.I., N.J.S. Software: M.A.I. Supervision: M.A.I., M.T.H., S.M.S.I. Writing (Original draft preparation): M.A.I., N.J.S., M.T.H., A.J. Writing (Review & editing): M.A.I., N.J.S., M.T.H., A.J., A.M.N.R., S.M.S.I.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
Data are available at https://dhsprogram.com/.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Andre M. N. Renzahod and Sheikh Mohammed Shariful Islam.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-09567-1.
References
- 1.Desa U. Transforming Our World: The 2030 Agenda for Sustainable Development. United Nations; 2016. [Google Scholar]
- 2.Yaya S, Bishwajit G, Shah V. Wealth, education and urban–rural inequality and maternal healthcare service usage in Malawi. BMJ Glob. Health. 2016;1:e000085. doi: 10.1136/bmjgh-2016-000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alkema L, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. The Lancet. 2016;387:462–474. doi: 10.1016/S0140-6736(15)00838-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Batist J. An intersectional analysis of maternal mortality in Sub-Saharan Africa: A human rights issue. J. Glob. Health. 2019;9:010320. doi: 10.7189/jogh.09.010320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stanton C, Blanc AK, Croft T, Choi Y. Skilled care at birth in the developing world: progress to date and strategi es for expanding coverage. J. Biosoc. Sci. 2007;39:109. doi: 10.1017/S0021932006001271. [DOI] [PubMed] [Google Scholar]
- 6.Chu K, et al. Cesarean section rates and indications in sub-Saharan Africa: A multi-country study from Medecins sans Frontieres. PLoS ONE. 2012;7:e44484. doi: 10.1371/journal.pone.0044484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karanth L, Kanagasabai S, Abas AB. Maternal and foetal outcomes following natural vaginal versus caesarean section (c-section) delivery in women with bleeding disorders and carriers. Cochrane Database Syst. Rev. 2015 doi: 10.1002/14651858.CD011059.pub4. [DOI] [PubMed] [Google Scholar]
- 8.Todman D. A history of caesarean section: From ancient world to the modern era. Aust. N. Z. J. Obstet. Gynaecol. 2007;47:357–361. doi: 10.1111/j.1479-828X.2007.00757.x. [DOI] [PubMed] [Google Scholar]
- 9.Organization WH. WHO Recommendations Non-clinical Interventions to Reduce Unnecessary Caesarean Sections. World Health Organization; 2018. [PubMed] [Google Scholar]
- 10.Programme, W. H. O. H. R. (2015).
- 11.Miller S, et al. Beyond too little, too late and too much, too soon: A pathway towards evidence-based, respectful maternity care worldwide. The Lancet. 2016;388:2176–2192. doi: 10.1016/S0140-6736(16)31472-6. [DOI] [PubMed] [Google Scholar]
- 12.Shamshad B. Factors leading to increased cesarean section rate. Gomal J. Med. Sci. 2008;6:1–5. [Google Scholar]
- 13.Betrán AP, et al. Rates of caesarean section: Analysis of global, regional and national estimates. Paediatr. Perinat. Epidemiol. 2007;21:98–113. doi: 10.1111/j.1365-3016.2007.00786.x. [DOI] [PubMed] [Google Scholar]
- 14.Gibbons L, et al. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: Overuse as a barrier to universal coverage. World Health Rep. 2010;30:1–31. [Google Scholar]
- 15.Bailey P, Lobis S, Maine D, Fortney JA. Monitoring Emergency Obstetric Care: A Handbook. World Health Organization; 2009. [Google Scholar]
- 16.Omar AAA, Anza SHA. Frequency rate and indications of caesarean sections at Prince Zaid Bin Al Hussein Hospital-Jordan. JRMS. 2012;19:82–86. [Google Scholar]
- 17.Volpe FM. Correlation of Cesarean rates to maternal and infant mortality rates: An ecologic study of official international data. Rev. Panam. Salud Publica. 2011;29:303–308. doi: 10.1590/s1020-49892011000500001. [DOI] [PubMed] [Google Scholar]
- 18.Nilsen C, Østbye T, Daltveit AK, Mmbaga BT, Sandøy IF. Trends in and socio-demographic factors associated with caesarean section at a Tanzanian referral hospital, 2000 to 2013. Int. J. Equity Health. 2014;13:1–11. doi: 10.1186/s12939-014-0087-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dikete M, Coppieters Y, Trigaux P, Englert Y, Simon P. An analysis of the practices of caesarean section in sub-Saharan Africa: A summary of the literature. Arch. Community Med. Public Health. 2019;5:077–086. [Google Scholar]
- 20.Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst. Rev. 2015 doi: 10.1002/14651858.CD000166.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bishop D, et al. Maternal and neonatal outcomes after caesarean delivery in the African Surgical Outcomes Study: A 7-day prospective observational cohort study. Lancet Glob. Health. 2019;7:e513–e522. doi: 10.1016/S2214-109X(19)30036-1. [DOI] [PubMed] [Google Scholar]
- 22.Betrán AP, et al. The increasing trend in caesarean section rates: Global, regional and national estimates: 1990–2014. PLoS ONE. 2016;11:e0148343. doi: 10.1371/journal.pone.0148343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gebremedhin S. Trend and socio-demographic differentials of Caesarean section rate in Addis Ababa, Ethiopia: analysis based on Ethiopia demographic and health surveys data. Reprod. Health. 2014;11:1–6. doi: 10.1186/1742-4755-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCall SJ, et al. Trends, wealth inequalities and the role of the private sector in caesarean section in the Middle East and North Africa: A repeat cross-sectional analysis of population-based surveys. PLoS ONE. 2021;16(11):e0259791. doi: 10.1371/journal.pone.0259791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rahman S, et al. Effect of a package of integrated demand-and supply-side interventions on facility delivery rates in rural Bangladesh: Implications for large-scale programs. PLoS ONE. 2017;12:e0186182. doi: 10.1371/journal.pone.0186182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haider MR, et al. Ever-increasing Caesarean section and its economic burden in Bangladesh. PLoS ONE. 2018;13:e0208623. doi: 10.1371/journal.pone.0208623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Betrán AP, et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. The Lancet. 2018;392:1358–1368. doi: 10.1016/S0140-6736(18)31927-5. [DOI] [PubMed] [Google Scholar]
- 28.Yaya S, Uthman OA, Amouzou A, Bishwajit G. Disparities in caesarean section prevalence and determinants across sub-Saharan Africa countries. Glob. Health Res. Policy. 2018;3:19. doi: 10.1186/s41256-018-0074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chu K, Maine R, Trelles M. Cesarean section surgical site infections in sub-Saharan Africa: A multi-country study from Medecins Sans Frontieres. World J. Surg. 2015;39:350–355. doi: 10.1007/s00268-014-2840-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harrison MS, Goldenberg RL. Cesarean section in sub-Saharan Africa. Matern. Health Neonatol. Perinatol. 2016;2:1–10. doi: 10.1186/s40748-016-0033-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sway A, et al. Burden of surgical site infection following cesarean section in sub-Saharan Africa: A narrative review. Int. J. Women's Health. 2019;11:309. doi: 10.2147/IJWH.S182362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Program, T. D. https://dhsprogram.com/data/data-collection.cfm.
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 34.Adegoke A, Van Den Broek N. Skilled birth attendance-lessons learnt. BJOG. 2009;116:33–40. doi: 10.1111/j.1471-0528.2009.02336.x. [DOI] [PubMed] [Google Scholar]
- 35.Hilbe JM. Logistic Regression Models. CRC Press; 2009. [Google Scholar]
- 36.Tranmer M, Elliot M. Binary logistic regression. Cathie Marsh for Census Surv. Res. 2008;20:3–43. [Google Scholar]
- 37.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol. Methods. 2006;11:193. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 38.Rücker G, Schwarzer G, Carpenter JR, Schumacher M. Undue reliance on I 2 in assessing heterogeneity may mislead. BMC Med. Res. Methodol. 2008;8:1–9. doi: 10.1186/1471-2288-8-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 41.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods. 2010;1:97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 42.Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: Proposed metrics and empirical evaluation. Int. J. Epidemiol. 2008;37:1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Verhagen A, Ferreira ML. Forest plots. J. Physiother. 2014;60:170–173. doi: 10.1016/j.jphys.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 44.Normand SLT. Meta-analysis: Formulating, evaluating, combining, and reporting. Stat. Med. 1999;18:321–359. doi: 10.1002/(sici)1097-0258(19990215)18:3<321::aid-sim28>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 45.Organization WH. WHO Statement on Caesarean Section Rates. World Health Organization; 2015. [Google Scholar]
- 46.Dikete M, et al. Variation of caesarean section rates in Sub-Saharan Africa: A literature review. J. Gynecol. Res. Obstet. 2019;5:042–047. [Google Scholar]
- 47.Adu-Bonsaffoh K, Obed SA, Seffah JD. Maternal outcomes of hypertensive disorders in pregnancy at Korle Bu Teaching Hospital, Ghana. Int. J. Gynecol. Obstet. 2014;127:238–242. doi: 10.1016/j.ijgo.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 48.Yaya S, Uthman OA, Amouzou A, Bishwajit G. Disparities in caesarean section prevalence and determinants across sub-Saharan Africa countries. Glob. Health Res. Policy. 2018;3:1–9. doi: 10.1186/s41256-018-0074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Azami-Aghdash S, Ghojazadeh M, Dehdilani N, Mohammadi M. Prevalence and causes of cesarean section in Iran: Systematic review and meta-analysis. Iran J. Public Health. 2014;43:545. [PMC free article] [PubMed] [Google Scholar]
- 50.Alimohamadian M, Shariat M, Mahmoodi M, Ramezanzadeh F. The survey of impact of pregnant women's request in selected cesarean. Payesh. 2003;2:133–139. [Google Scholar]
- 51.Murray SF. Relation between private health insurance and high rates of caesarean section in Chile: Qualitative and quantitative study. BMJ. 2000;321:1501–1505. doi: 10.1136/bmj.321.7275.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Epstein RM, Gramling RE. What is shared in shared decision making? Complex decisions when the evidence is unclear. Med. Care Res. Rev. 2013;70:94S–112S. doi: 10.1177/1077558712459216. [DOI] [PubMed] [Google Scholar]
- 53.Arendt E, Singh NS, Campbell OM. Effect of maternal height on caesarean section and neonatal mortality rates in sub-Saharan Africa: an analysis of 34 national datasets. PLoS ONE. 2018;13:e0192167. doi: 10.1371/journal.pone.0192167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Feng XL, Xu L, Guo Y, Ronsmans C. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull. World Health Organ. 2012;90:30–39A. doi: 10.2471/BLT.11.090399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nababan HY, et al. Trends and inequities in use of maternal health care services in Indonesia, 1986–2012. Int. J. Women's Health. 2018;10:11. doi: 10.2147/IJWH.S144828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Divyamol N, Raphael L, Koshy N. Caesarean section rate and its determinants in a rural area of South India. Int. J. Community Med. Public Health. 2016 doi: 10.18203/2394-6040.ijcmph20163370. [DOI] [Google Scholar]
- 57.Mumtaz S, Bahk J, Khang Y-H. Rising trends and inequalities in cesarean section rates in Pakistan: Evidence from Pakistan Demographic and Health Surveys, 1990–2013. PLoS ONE. 2017;12:e0186563. doi: 10.1371/journal.pone.0186563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bahadori F, Hakimi S, Heidarzade M. The trend of caesarean delivery in the Islamic Republic of Iran. East. Mediterr. Health J. 2013;19:67–70. [PubMed] [Google Scholar]
- 59.Cavallaro FL, et al. Trends in caesarean delivery by country and wealth quintile: cross-sectional surveys in southern Asia and sub-Saharan Africa. Bull. World Health Organ. 2013;91:914–922D. doi: 10.2471/BLT.13.117598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Long Q, Kempas T, Madede T, Klemetti R, Hemminki E. Caesarean section rates in Mozambique. BMC Pregnancy Childbirth. 2015;15:1–9. doi: 10.1186/s12884-015-0686-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Boatin AA, et al. Within country inequalities in caesarean section rates: Observational study of 72 low and middle income countries. BMJ. 2018;360:k55. doi: 10.1136/bmj.k55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liang J, et al. Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: Observational study of nearly seven million health facility births. BMJ. 2018;360:k817. doi: 10.1136/bmj.k817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khan MN, Islam MM, Shariff AA, Alam MM, Rahman MM. Socio-demographic predictors and average annual rates of caesarean section in Bangladesh between 2004 and 2014. PLoS ONE. 2017;12:e0177579. doi: 10.1371/journal.pone.0177579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rahman M, Shariff AA, Shafie A, Saaid R, Tahir RM. Determinants of caesarean risk factor in northern region of Bangladesh: a multivariate analysis. Iran J. Public Health. 2014;43:16. [PMC free article] [PubMed] [Google Scholar]
- 65.Ronsmans C, Holtz S, Stanton C. Socioeconomic differentials in caesarean rates in developing countries: A retrospective analysis. The Lancet. 2006;368:1516–1523. doi: 10.1016/S0140-6736(06)69639-6. [DOI] [PubMed] [Google Scholar]
- 66.Mohammaditabar S, Kiani A, Heidari M. The survey on tendencies of primiparous women for selecting the mode of delivery. J. Babol Univ. Med. Sci. 2009;11:54–59. [Google Scholar]
- 67.Béhague DP, Victora CG, Barros FC. Consumer demand for caesarean sections in Brazil: informed decision making, patient choice, or social inequality? A population based birth cohort study linking ethnographic and epidemiological methods. BMJ. 2002;324:942. doi: 10.1136/bmj.324.7343.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Montagu D, Yamey G, Visconti A, Harding A, Yoong J. Where do poor women in developing countries give birth? A multi-country analysis of demographic and health survey data. PLoS ONE. 2011;6:e17155. doi: 10.1371/journal.pone.0017155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bustreo F, Harding A, Axelsson H. Can developing countries achieve adequate improvements in child health outcomes without engaging the private sector? Bull. World Health Organ. 2003;81:886–895. [PMC free article] [PubMed] [Google Scholar]
- 70.Leone T, Padmadas SS, Matthews Z. Community factors affecting rising caesarean section rates in developing countries: An analysis of six countries. Soc. Sci. Med. 2008;67:1236–1246. doi: 10.1016/j.socscimed.2008.06.032. [DOI] [PubMed] [Google Scholar]
- 71.Begum T, et al. Indications and determinants of caesarean section delivery: Evidence from a population-based study in Matlab, Bangladesh. PLoS ONE. 2017;12:e0188074. doi: 10.1371/journal.pone.0188074. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available at https://dhsprogram.com/.