Abstract
Objective
The Canadian 24-hour movement guidelines for children and youth recommend a minimum of 60 min/day of moderate-to-vigorous physical activity, no more than 2 h/day of recreational screen time, and 8–11 h/night of sleep depending on age. The objective of this study was to examine the associations of meeting combinations of these recommendations with self-rated physical and mental health.
Methods
This study used data from the 2017 (n = 5739) and 2019 (n = 6960) cycles of the Ontario Student Drug Use and Health Survey (OSDUHS), a biennially repeated cross-sectional study of Ontario students in grades 7 through 12. Multivariable ordered logistic regression models were adjusted for age, gender, ethnoracial background, subjective socio-economic status, and body mass index z-scores.
Results
Similar patterns were seen in the 2017 and 2019 samples. Compared with meeting none of the recommendations, meeting different combinations of recommendations in the 2019 sample was associated with positive self-rated physical and mental health. A dose–response gradient between the number of recommendations met and self-rated physical (p < 0.001) and mental (p < 0.001) health was observed, with meeting one (AOR: 1.82; 95% CI: 1.58–2.09), two (AOR: 3.54; 95% CI: 2.98–4.22), or three recommendations (AOR: 6.34; 95% CI: 4.46–9.02) being increasingly associated with positive self-rated physical health compared with meeting none; and meeting one (AOR: 1.51; 95% CI: 1.33–1.71), two (AOR: 2.70; 95% CI: 2.31–3.17), or three recommendations (AOR: 3.58; 95% CI: 2.57–4.98) being increasingly associated with positive self-rated mental health compared with meeting none.
Conclusion
Meeting the 24-hour movement guidelines is associated with better self-rated physical and mental health among adolescents.
Keywords: Physical activity, Screen time, Sleep, Physical health, Mental health, Youth
Résumé
Objectif
Les Directives canadiennes en matière de mouvement sur 24 heures pour les enfants et les jeunes recommandent un minimum de 60 min par jour d’activité physique d’intensité moyenne à élevée, un maximum de 2 heures par jour de temps de loisir devant un écran et de 8 à 11 heures de sommeil selon l’âge. L’objectif de cette étude était d’examiner les associations entre l’adoption d’une combinaison de ces recommandations et l’autoévaluation de la santé physique et mentale.
Méthode
Cette étude s’est appuyée sur les données tirées des cycles de 2017 (n = 5 739) et de 2019 (n = 6 960) du Sondage sur la consommation de drogues et la santé des élèves de l’Ontario (SCDSEO), un sondage transversal réalisé tous les deux ans auprès d’élèves de la 7e à la 12e année en Ontario. Les modèles de régression logistique multivariés ont été ajustés en ce qui a trait à l’âge, au genre, aux antécédents ethnoraciaux, au statut socioéconomique subjectif et aux scores-z de l’indice de masse corporelle.
Résultats
Des tendances similaires ont été observées dans les échantillons de 2017 et de 2019. L’adoption d’une combinaison des recommandations parmi l’échantillon de 2019, comparativement au fait de ne se conformer à aucune d’elles, était associée à une autoévaluation positive de la santé physique et mentale. Un gradient dose-réponse entre le nombre de recommandations adoptées et l’autoévaluation de la santé physique (p < 0,001) et mentale (p < 0,001) a été observé. L’adoption d’une (RCa : 1,82; IC de 95% : 1,58 à 2,09), de deux (RCa : 3,54; IC de 95% : 2,98 à 4,22) ou de trois recommandations (RCa : 6,34; IC de 95% : 4,46 à 9,02) était étroitement associée à une autoévaluation positive de la santé physique, comparativement au fait de ne se conformer à aucune d’elles; et l’adoption d’une (RCa : 1,51; IC de 95% : 1,33 à 1,71), de deux (RCa : 2,70; IC de 95% : 2,31 à 3,17) ou de trois recommandations (RCa : 3,58; IC de 95% : 2,57 à 4,98) était étroitement associée à une autoévaluation positive de la santé mentale, comparativement au fait de ne se conformer à aucune d’elles.
Conclusion
La conformité aux directives en matière de mouvement sur 24 heures est associée à une meilleure autoévaluation de la santé physique et mentale chez les adolescents.
Mots-clés: Activité physique, temps d’écran, sommeil, santé physique, santé mentale, jeunes
Introduction
The Canadian 24-hour movement guidelines for children and youth are evidence-based guidelines that provide integrated guidance on the amount of physical activity, screen time, and sleep duration that should be achieved for better health (Tremblay et al., 2016). These guidelines recommend that children and youth get at least 60 min/day of moderate-to-vigorous physical activity (vigorous physical activities and muscle and bone strengthening activities should each be incorporated at least 3 days per week), engage in light physical activities for several hours per day, spend no more than 2 h/day in recreational screen time, and sleep for 9 to 11 h/night (children aged 5 to 13 years) or 8 to 10 h/night (youth aged 14 to 17 years), with consistent bed and wake-up times (Tremblay et al., 2016). Meeting these guidelines has been associated with improved indicators of social, physical, and mental health (Carson et al., 2017; Janssen et al., 2017; Saunders et al., 2016). Recent research has also shown that meeting the Canadian 24-hour movement guidelines is associated with less mental health problems among adolescents, such as psychological distress, suicidality, aggressive behaviours, and substance use (Sampasa-Kanyinga et al., 2020a, 2020b, 2020c, 2020d). However, no studies have examined the link between meeting the 24-hour movement guidelines and a more global measure of self-perception of health, such as self-rated health.
Self-rated health is a subjective, multi-dimensional indicator of one’s health status as impacted by physical, psychological, and social functioning (Leidy et al., 1999). In younger age groups, self-rated health is more dependent on health behaviours as opposed to health problems (Krause & Jay, 1994), thus making self-rated health a somewhat different construct in children/adolescents than in adults. The measure may therefore be more representative of health as an enduring self-concept rather than a fleeting assessment of health at present (Boardman, 2006). Indeed, the World Health Organization (WHO) considers self-rated health a more appropriate measure of adolescent health than traditional morbidity and mortality measures (Currie et al., 2009). Self-rated health is often used in health surveys to assess health-related quality of life. A study specific to combinations of the Canadian 24-hour movement guidelines found that meeting more recommendations was associated with better health-related quality of life in children, as measured by a 10-question survey (Sampasa-Kanyinga et al., 2017). However, the association between meeting the 24-hour movement guidelines and health-related quality of life in adolescents is largely unknown.
Research has shown that individual movement behaviours are associated with self-rated health. A recent systematic review and meta-analysis study demonstrated consistent findings of better self-rated health observed in children and adolescents who reported 2 h or less of daily recreational screen time and those who reported higher levels of physical activity (Zhang et al., 2020). Moreover, self-rated health can be further partitioned into self-rated physical and mental health (Boak et al., 2017; Statistics Canada, 2013). For example, Herman et al. (2015) found that adolescents exceeding 2 h of daily recreational screen time had 30% greater odds of suboptimal self-reported health (defined here as self-perceiving health as good, fair, or poor, as opposed to optimal health, defined as excellent or very good perceptions), and 30–50% greater odds of suboptimal self-reported mental health. Shorter sleep duration has also been found to be associated with poorer self-rated health in various age groups, including adolescents, young adults, and adults (Geiger et al., 2012; Štefan et al., 2017; Yeo et al., 2019).
To our knowledge, the association between different combinations of physical activity, screen time, and sleep duration with self-rated health or self-rated physical or mental health as single-item global health questions has yet to be explored. This is particularly important for two reasons. First, physical activity, screen time, and sleep duration are codependent (Chaput et al., 2014), and it is necessary to get a better understanding of the combined influence of movement behaviours on self-rated physical or mental health. Second, the use of a global health status assessment of physical and mental health could be essential to capture adolescents’ well-being beyond consideration of specific health problems (Krause & Jay, 1994; Vingilis et al., 2002). While it should not serve as a replacement for objective and specific measures of physical illness and morbidity, self-rated health has been associated with mortality and physical and psychological health status, exhibiting its potential use as a screening tool (Gallagher et al., 2016; Lorem et al., 2020; Williams et al., 2017). Furthermore, studying the relationship between movement behaviours and self-rated health with physical and mental health as distinct entities can provide insight into the roles that combinations of movement behaviours may separately play in different aspects of health perception by adolescents.
Thus, the purpose of this study was to examine the association between meeting combinations of the 24-hour movement guidelines for physical activity, recreational screen time, and sleep duration and self-rated physical and mental health in adolescents in the 2017 and 2019 cycles of the Ontario Student Drug Use and Health Survey (OSDUHS). The 2017 and 2019 samples were examined separately to examine whether the findings would be consistent across these two cycles. We hypothesized that (1) adherence to the 24-hour movement guidelines would be associated with better self-rated physical and mental health; and (2) adherence to a greater number of recommendations (3 > 2 > 1 > 0) would be more strongly associated with better self-rated physical and mental health among adolescents.
Methods
Data
Cross-sectional data were derived from the 2017 and 2019 cycles of the OSDUHS, a biennial representative province-wide survey of students in grades 7 through 12 (aged 11 to 20 years or over) in publicly funded schools across Ontario, Canada (Boak et al., 2017, 2020). The survey has been ongoing since 1977 to monitor students’ drug use, mental health, physical health, gambling, bullying, and other risk behaviours, as well as to identify risk and protective factors. The OSDUHS employs a stratified two-stage cluster design (school, class). Participation in the survey is anonymous and voluntary. Students completed a self-administered paper-and-pencil questionnaire during a regularly scheduled classroom period. In the 2017 cycle, the survey sampled 11,435 students in grades 7 through 12 from 52 school boards, 214 schools, and 764 classrooms (Boak et al., 2017). The student participation rate was 61%. Students were lost due to absenteeism (12%) and parental refusal or unreturned consent forms (27%) (Boak et al., 2017). In the 2019 cycle, the survey included 14,142 students in grades 7 through 12 from 47 school boards, 263 schools, and 992 classrooms (Boak et al., 2020). The student participation rate was 59%. Students were lost due to absenteeism (12%) and parental refusal or unreturned consent forms (29%) (Boak et al., 2020). The rates of student participation were above average for a student survey that required active consent from a parent or guardian (Courser et al., 2009). Analyses were restricted to the random half samples who completed the A version of the questionnaire, which included a question on self-reported mental health (N = 6364 and 7617 for the 2017 and 2019 data, respectively). Greater details about the survey design and methods are described elsewhere (Boak et al., 2017, 2020). The 2017 and 2019 OSDUHS protocols were approved by the Research Ethics Boards at the Centre for Addiction and Mental Health and York University, as well as the school board research review committees. All subjects gave their signed assent in addition to parentally signed consent for those aged under 18 years before they participated in the study.
Measures
Dependent variable
Self-reported physical and mental health constitute the dependent variables. Similar measures are widely used in national (Statistics Canada, 2013) and international population-based surveys, such as the Centers for Disease Control (CDC)’s Youth Risk Behavior Survey (YRBS) (Centers for Disease Control and Prevention, n.d.) and the Health Behaviour in School-aged Children study (HBSC) (Currie et al., 2009), and have shown good psychometric properties among children and adolescents.
Self-reported physical health was assessed using the following question: “How would you rate your physical health?”. Response options included excellent, very good, good, fair, and poor. Response options ranging from 1 (excellent) to 5 (poor) were reverse coded and treated as an ordinal variable so that higher scores indicate positive self-reported physical health.
Self-reported mental health was measured using the following question: “How would you rate your mental or emotional health?”. Response options included excellent, very good, good, fair, and poor. Response options ranging from 1 (excellent) to 5 (poor) were reverse coded and treated as an ordinal variable so that higher scores indicate positive self-reported mental health.
Independent variables
Physical activity was measured using the following item: “On how many of the last 7 days were you physically active for at least 60 min each day. Please add up all the time you spent in any types of physical activity that increased your heart rate and made you breathe hard for some of the time (Some of the examples are brisk walking, running, rollerblading, biking, dancing, skateboarding, swimming, soccer, basketball, football). Please include both school and non-school activities”. Response options ranged from 0 to 7 days. For analysis, participants who responded “7 days” were considered as meeting the physical activity recommendation (Tremblay et al., 2016). Whereas, the remaining response options were collapsed to represent those who did not meet the physical activity recommendation.
Screen time was measured using the following item: “In the last 7 days, about how many hours a day, on average, do you spend watching TV/movies/videos, texting, playing video/computer games, emailing, or surfing the Internet in your free time?”. Participants who reported spending no more than 2 h/day of recreational screen time were considered as meeting the screen time recommendation (Tremblay et al., 2016). Those who reported screen time of more than 2 h/day were considered as not meeting the screen time recommendation.
Sleep duration was assessed using the following question: “On an average school night, how many hours of sleep do you get?”. Participants who reported a sleep duration falling within the recommended range (9–11 h/night for 11–13-year-olds; 8–10 h/night for 14–17-year-olds, or 7–9 h/night for those aged 18 years or older) were considered as meeting the sleep duration recommendation (Tremblay et al., 2016). Those who reported getting insufficient sleep were considered as not meeting the sleep duration recommendation.
Covariates
Covariates included age (in years), gender (determined by being boy or girl), ethnoracial background (including white, Black, East and Southeast Asian, South Asian, and Other), subjective socio-economic status (SES), and body mass index (BMI) z-score. Subjective SES was measured using the youth version of the MacArthur Scale of Subjective Social Status (Goodman et al., 2007). Minor modifications were made to the youth scale to assess the family’s place within society. The question was presented with a drawing of a ladder with 10 rungs that was described as follows: “Imagine this ladder below shows how Canadian society is set up. At the top of the ladder are people who are the ‘best off’ – they have the most money, the most education, and the jobs that bring the most respect. At the bottom are the people who are ‘worst off’ – they have the least money, little education, no job or jobs that no one wants. Now think about your family. Please check off the numbered box that best shows where you think your family would be on this ladder”. Students self-reported their body weight (kilograms) and height (metres). BMI (kilograms/metres2) was calculated and converted into z-scores following the WHO’s reference data (World Health Organization, 2011). Age, subjective SES, and BMI z-scores were treated as continuous variables, whereas gender and ethnoracial background were treated as categorical variables.
Data analysis
All analyses were conducted using STATA 16.0 and accounted for the complex survey sample design using Taylor series methods. Population weights were used to adjust for the unequal probability of selection. The characteristics of the study participants in the 2017 and 2019 OSDUHS were described via proportions, means, and medians. Given that separate two-way interactions between both independent variables and gender were not statistically significant for both outcomes in 2017 and 2019, analyzing boys and girls separately was not necessary. Ordered logistic regression analyses were used to examine the associations between the independent variables of (1) different combinations of meeting the physical activity, screen time, and sleep duration recommendations and (2) the number of recommendations met with the outcome variables of self-rated physical and mental health for both cycles of the survey. Multivariate models adjusted for age, gender, ethnoracial background, subjective SES, and body mass index z-score. Missing data were handled through listwise deletion, reducing the sample sizes by 9.8% and 9.4% for the 2017 and 2019 datasets, respectively. Participants with missing data were more likely to be boys in the 2017 and 2019 data. They were also more likely to be in lower grades and of Black ethnoracial background in the 2019 data.
Results
Descriptive characteristics of the sample are outlined in Table 1. Almost half of the 2017 and 2019 samples were girls, just over half identified themselves as white, and the average age of each sample was 15 years. In the 2017 sample, the prevalences of suboptimal self-rated physical and mental health were 40.4% and 46.8%, respectively. However, in the 2019 sample, the prevalences of suboptimal self-rated physical and mental health were 43.1% and 55.9%, respectively.
Table 1.
Descriptive characteristics of the study sample
| 2017 (N = 5739) |
2019 (N = 6960) |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Age (years) | ||||
| Mean (SD) | 15.2 | 1.8 | 15.2 | 1.8 |
| Gender | ||||
| Boys | 3293 | 49.0 | 49.4 | 49.4 |
| Girls | 2446 | 51.0 | 50.6 | 50.6 |
| Ethnoracial background | ||||
| White | 3319 | 54.0 | 3860 | 50.9 |
| Black | 479 | 12.0 | 556 | 9.5 |
| East/Southeast Asian | 508 | 8.1 | 855 | 14.0 |
| South Asian | 433 | 6.4 | 577 | 9.0 |
| Other | 1000 | 19.6 | 1112 | 16.7 |
| Subjective socio-economic status | ||||
| Mean (SD) | 6.9 | 1.7 | 6.9 | 1.7 |
| Body mass index z-score | ||||
| Mean (SD) | 0.3 | 1.2 | 0.3 | 1.1 |
| Physical activity | ||||
| Not meeting | 4510 | 78.1 | 5550 | 80.3 |
| Meeting | 1229 | 21.9 | 1410 | 19.7 |
| Screen time | ||||
| Not meeting | 3743 | 66.3 | 5115 | 75.5 |
| Meeting | 1996 | 33.8 | 1845 | 24.5 |
| Sleep duration | ||||
| Not meeting | 3830 | 67.3 | 4570 | 65.9 |
| Meeting | 1909 | 32.7 | 2390 | 34.1 |
| Number of recommendations met | ||||
| Zero | 2248 | 39.9 | 3013 | 44.5 |
| One | 2134 | 36.9 | 2526 | 36.2 |
| Two | 1071 | 18.2 | 1144 | 15.8 |
| Three | 286 | 5.0 | 277 | 3.5 |
| Self-rated physical healtha | ||||
| Median | 4 | 4 | ||
| Self-rated mental healtha | ||||
| Median | 4 | 3 | ||
Data are shown as count and percentage unless otherwise indicated
SD, standard deviation
a This variable was measured on a 5-point ordinal scale so that higher scores indicate a positive measure
Figure 1 displays the prevalence of participants in the 2017 (Venn diagram A) and 2019 (Venn diagram B) cycles of the OSDUHS who met recommendations for movement behaviours. Overall, meeting all three recommendations was reported by 5.0% of the sample in 2017 and by 3.5% of the sample in 2019. Not meeting any recommendation was reported by 39.9% of the sample in 2017 and by 44.5% of the sample in 2019.
Fig. 1.
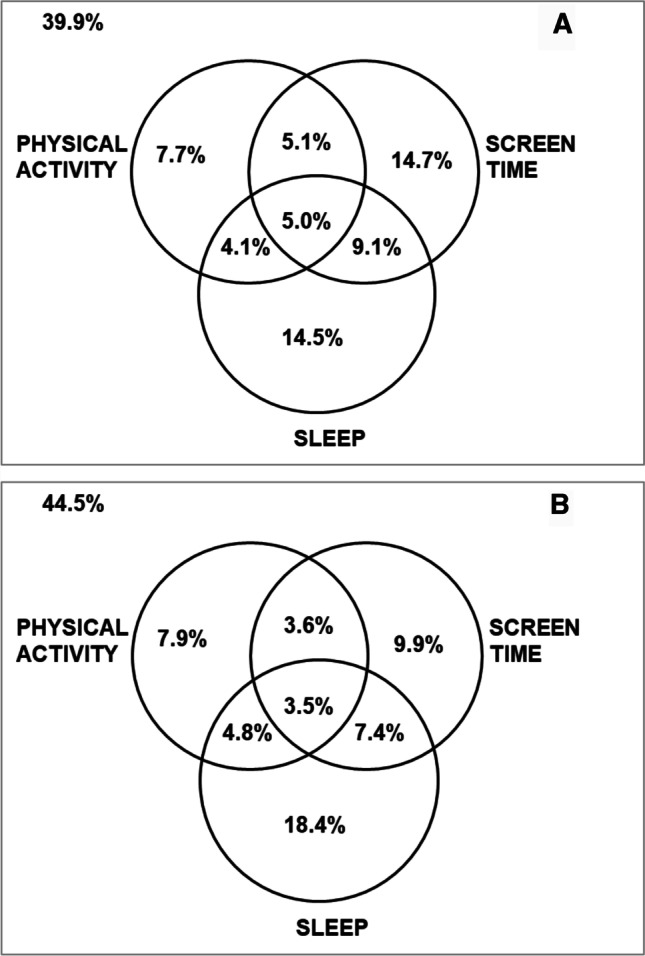
Venn diagram showing the prevalence of students who meet the physical activity, screen time, and sleep duration recommendations, their combinations, and those who meet none of the 3 recommendations in the total study sample in 2017 (panel A, N = 5739) and 2019 (panel B, N = 6960)
Results of univariable and multivariable ordered logistic regression analyses examining the associations between meeting combinations of the physical activity, screen time, and sleep duration recommendations with self-rated physical and mental health are outlined in Table 2. Findings showed that in the 2017 sample, meeting all 3 recommendations and different intermediate combinations of the recommendations were all associated with positive self-reported physical health. The same pattern was observed for self-reported mental health, except meeting the screen time recommendation only, which was not associated with this outcome (AOR = 1.33; 95% CI: 0.97 – 1.81). However, in the 2019 sample, meeting different combinations of recommendations was all associated with positive self-reported physical health and self-reported mental health.
Table 2.
Ordered logistic regression examining the associations of movement behaviour combinations with self-reported physical and mental health
| Self-rated physical healtha | Self-rated mental healtha | |||
|---|---|---|---|---|
| Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
|
| 2017 (N = 5739) | ||||
| Meeting none | 1 | 1 | 1 | 1 |
| Only physical activity | 4.39 (3.02 – 6.38) | 3.75 (2.81 – 4.99) | 2.39 (1.89 – 3.01) | 1.88 (1.56 – 2.28) |
| Only screen time | 2.02 (1.62 – 2.51) | 1.74 (1.42 – 2.14) | 1.31 (0.98 – 1.75) | 1.33 (0.97 – 1.81) |
| Only sleep duration | 1.76 (1.37 – 2.25) | 1.39 (1.10 – 1.76) | 2.22 (1.59 – 3.09) | 1.99 (1.40 – 2.83) |
| Physical activity + screen time | 8.33 (4.63 – 14.99) | 5.81 (3.14 – 10.75) | 3.78 (2.70 – 5.30) | 2.58 (1.72 – 3.86) |
| Physical activity + sleep duration | 10.00 (6.82 – 14.69) | 6.50 (4.38 – 9.65) | 7.69 (4.75 – 12.43) | 4.92 (3.18 – 7.62) |
| Screen time + sleep duration | 3.89 (2.77 – 5.47) | 2.91 (1.92 – 4.39) | 5.12 (3.72 – 7.04) | 4.47 (3.20 – 6.25) |
| Physical activity + screen time + sleep duration | 19.92 (11.94 – 33.22) | 12.78 (6.97 – 23.41) | 5.92 (4.42 – 7.93) | 3.84 (2.69 – 5.48) |
| 2019 (N = 6960) | ||||
| Meeting none | 1 | 1 | 1 | 1 |
| Only physical activity | 3.66 (2.75 – 4.86) | 3.24 (2.42 – 4.33) | 1.51 (1.20 – 1.91) | 1.42 (1.11 – 1.79) |
| Only screen time | 1.86 (1.50 – 2.31) | 1.75 (1.44 – 2.12) | 1.26 (1.03 – 1.54) | 1.20 (1.00 – 1.43) |
| Only sleep duration | 1.78 (1.54 – 2.04) | 1.50 (1.29 – 1.75) | 2.13 (1.80 – 2.51) | 1.96 (1.65 – 2.34) |
| Physical activity + screen time | 6.61 (4.81 – 9.09) | 5.50 (3.90 – 7.76) | 2.46 (1.82 – 3.32) | 2.16 (1.61 – 2.91) |
| Physical activity + sleep duration | 5.87 (4.50 – 7.67) | 4.55 (3.43 – 6.03) | 4.45 (3.38 – 5.86) | 3.75 (2.84 – 4.96) |
| Screen time + sleep duration | 3.32 (2.67 – 4.13) | 2.56 (2.07 – 3.17) | 3.76 (3.05 – 4.65) | 3.17 (2.55 – 3.93) |
| Physical activity + screen time + sleep duration | 9.86 (6.94 – 14.00) | 6.49 (4.55 – 9.25) | 6.01 (4.29 – 8.43) | 4.40 (3.20 – 6.04) |
Models are adjusted for age, gender, ethnoracial background, subjective socio-economic status, and body mass index z-score
OR, odds ratio; CI, confidence interval
a This variable was measured on a 5-point ordinal scale so that higher scores indicate a positive measure
Results of ordered logistic regression analyses examining the association between the number of movement behaviour recommendations met and self-reported physical and mental health in the 2017 and 2019 samples are summarized in Table 3. We documented a dose–response gradient between the number of guideline recommendations met (3 vs. 2 vs. 1 vs. none) and both outcome variables of self-reported physical health (p < 0.001) and self-reported mental health (p < 0.001) in both the 2017 and 2019 samples (Table 3). These findings suggest that an increase in the number of recommendations met is associated with more positive self-reported physical and mental health. Meeting all three recommendations showed the strongest association with positive self-reported physical health and self-reported mental health compared with meeting two or one recommendation(s).
Table 3.
Ordered logistic regression examining the associations of number of movement behaviour recommendations met with self-reported physical and mental health
| Self-rated physical healtha | Self-rated mental healtha | |||
|---|---|---|---|---|
| Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
|
| 2017 (N = 5739) | ||||
| None | 1 | 1 | 1 | 1 |
| One | 2.22 (1.90 – 2.59) | 1.84 (1.59 – 2.14) | 1.83 (1.44 – 2.31) | 1.75 (1.32 – 2.31) |
| Two | 5.72 (4.95 – 6.61) | 4.05 (3.39 – 4.83) | 5.06 (4.11 – 6.23) | 4.17 (3.36 – 5.17) |
| Three | 19.29 (11.51 – 32.31) | 12.23 (6.62 – 22.59) | 5.85 (4.36 – 7.85) | 4.77 (3.44 – 6.62) |
| p-trend | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| 2019 (N = 6960) | ||||
| None | 1 | 1 | 1 | 1 |
| One | 2.07 (1.81 – 2.38) | 1.82 (1.58 – 2.09) | 1.71 (1.50 – 1.94) | 1.51 (1.33 – 1.71) |
| Two | 4.53 (3.83 – 5.37) | 3.54 (2.98 – 4.22) | 3.02 (3.02 – 4.27) | 2.70 (2.31 – 3.17) |
| Three | 9.69 (6.84 – 13.75) | 6.34 (4.46 – 9.02) | 4.26 (4.26 – 8.35) | 3.58 (2.57 – 4.98) |
| p-trend | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Models are adjusted for age, gender, ethnoracial background, subjective socio-economic status, and body mass index z-score
OR, odds ratio; CI, confidence interval
a This variable was measured on a 5-point ordinal scale so that higher scores indicate a positive measure
Discussion
This cross-sectional study used a representative school-based sample of Ontario students in grades 7 through 12 to examine the associations of meeting different combinations of movement behaviour recommendations, including physical activity, screen time, and sleep duration with self-rated physical and mental health. Collectively, our results indicated that meeting the 24-hour movement guidelines and different combinations of movement behaviour recommendations were associated with positive self-reported physical and mental health. We found a dose–response gradient between the number of guideline recommendations met and both outcome measures of self-reported physical and mental health, whereby an increase in the number of recommendations met is associated with more positive self-reported physical and mental health. Meeting all three recommendations showed the strongest association with positive self-reported physical health and self-reported mental health compared with meeting two or one recommendation(s). The findings were consistent across the 2017 and 2019 samples.
Our results are somewhat consistent with those from previous studies indicating that meeting the physical activity, screen time, and sleep duration recommendations is associated with better self-reported health or self-reported physical and mental health (Geiger et al., 2012; Herman et al., 2015; Štefan et al., 2017; Yeo et al., 2019; Zhang et al., 2020). However, our findings extend those from previous studies by examining different combinations of meeting the 24-hour movement behaviours recommendations. To the best of our knowledge, this is the first study to demonstrate that meeting the 24-hour movement guidelines is associated with optimal self-rated physical and mental health. Indeed, research has shown that movement behaviours are codependent (Chaput et al., 2014). Therefore, examining these associations in the context of the integrated guidelines is deemed more appropriate.
Results from this study indicated that the associations with meeting different combinations of movement behaviour recommendations were similar for both self-rated physical and mental health. Furthermore, the associations between the number of guidelines met and self-rated mental health were irrespective of which movement behaviours were met. However, previous research has found different patterns between specific physical and mental health outcomes in their associations with movement behaviours. Contrary to findings that physical activity is the most important determinant of physical health (World Health Organization, 2020), recent studies that have examined the associations between meeting the 24-hour movement guidelines and specific mental health problems, such as psychological distress, suicidality, aggressive behaviours, and substance use, have found that meeting the sleep duration and screen time recommendations are associated with mental health outcomes, whereas meeting the physical activity recommendation is not (Sampasa-Kanyinga et al., 2020a, 2020b, 2020c, 2020d). A similar pattern was also documented in two longitudinal studies examining the associations of meeting the 24-hour movement guidelines with negative (i.e., depressive symptoms) and positive (i.e., flourishing) mental health indicators in a sample of Canadian adolescents (Faulkner et al., 2020; Patte et al., 2020). It is possible that the global measures of self-rated physical and mental health dilute the effects of different movement behaviours, and thus mask possible differences between specific health problems. Our findings provide further support that the single self-reported global measures are framed on different factors beyond health problems, such as personal, socio-environmental, behavioural, and psychological factors (Krause & Jay, 1994; Vingilis et al., 2002).
Excessive duration of recreational screen time is known to be associated with negative health outcomes among adolescents, such as poorer body composition, higher cardiometabolic risk, behavioural problems, and mental health problems (Carson et al., 2016). Research has also shown that excessive screen time in childhood and adolescence is prospectively associated with poor mental health outcomes (Allen & Vella, 2015; Babic et al., 2017; Grontved et al., 2015). Surprisingly, our results showed that meeting the screen time recommendation only was associated with self-reported mental health in the 2019 sample, but not in 2017. Our findings are somewhat consistent with those from Faulkner et al. (2020), who found that meeting the screen time recommendation was not associated with an increase in flourishing in a sample of Canadian adolescents. Contrary to the latest study, the proportion of those meeting the screen time recommendation could not explain the observed differences because it dropped from 33.8% in the 2017 sample to 24.5% in the 2019 sample. It is possible that other factors, such as change over time in the pattern of screen time use and/or sample characteristics, explain the observed differences.
The use of 24-hour movement guidelines in public health is an important change in how we view movement behaviours. The fact that physical activity, sedentary behaviour, and sleep add up to 24 hours suggests that time-use displacements are important to consider when designing interventions that may impact health. For example, the benefits of physical activity may not be the same if the activity is done at the expense of sleep (bad trade-off) or sedentary behaviour (good trade-off). Similarly, the health benefits of physical activity would vary based on the intensity of the activity performed (Goldfield et al., 2011). For example, Parfitt et al. (2009) found that children accumulating high levels of very light activity report higher levels of anxiety and depression and lower levels of global self-worth, while children accumulating high levels of vigorous activity report lower levels of anxiety and higher levels of global self-worth. Future studies should continue to explore the interconnections among movement behaviours and how it influences health outcomes to better inform policy and practice.
The current study has several methodological strengths. First, it is an empirical study with a large sample size and an acceptable response rate for a school-based survey requiring parental or guardian active consent (Courser et al., 2009). Second, samples from two survey cycles (i.e., 2017 and 2019) were examined separately, thus offering opportunity to document consistency of the observed associations across the cycles. Third, the dose–response analysis provided evidence of proportionality in the association between the number of movement behaviour recommendations met and self-rated physical and mental health. Finally, the analyses adjusted for several potential confounders, allowing for a clearer interpretation of the main findings.
This study also has limitations worth mentioning. First, causality assumptions should not be made because of the cross-sectional nature of the data. There is also a possibility of reverse causation if participants with suboptimal self-rated physical and mental health are less likely to meet the 24-hour movement behaviour guidelines. Second, data were based on self-reports and may be subject to recall or desirability biases. However, self-reported measures of movement behaviours have shown good validity in comparison with accelerometry measures among children and adolescents (Lubans et al., 2011; Nascimento-Ferreira et al., 2016; Schmitz et al., 2004; Scott et al., 2015). Measures of recreational screen time have also demonstrated good psychometric properties in this age group. Third, the present study did not include other aspects of the 24-hour movement guidelines, such as muscle and bone strengthening activities and light physical activities (not available). Future studies that include these components are needed to replicate our findings.
Conclusion
Despite limitations, results from the present study provide further support for the Canadian 24-hour movement guidelines by showing that meeting the guidelines is associated with better self-rated physical and mental health. This has important public health implications due to the modifiable nature of physical activity, screen time, and sleep duration, particularly given the low rate of adherence to the Canadian 24-hour movement guidelines among adolescents. Our findings provide an important venue to promote adolescent well-being. All stakeholders, including public health authorities, health service providers, schools, parents, and adolescents themselves should be aware of these associations and the need to encourage adolescents to meet the Canadian 24-hour movement guidelines.
Contributions to knowledge
What does this study add to existing knowledge?
Previous research that has examined the relationships between movement behaviours (i.e., physical activity, screen time, and sleep duration) and self-reported physical and mental health has considered the movement behaviours individually and in isolation of each other, ignoring the interconnections between these behaviours.
What are the key implications for public health interventions, practice, or policy?
Results of this study showed that meeting the 24-hour movement guidelines and different combinations of movement behaviour recommendations were associated with positive self-reported physical and mental health.
There was a dose–response gradient between the number of guideline recommendations met and both outcome measures of self-reported physical and mental health, with meeting all 3 recommendations showing the strongest associations with positive self-reported physical and mental health compared with meeting two or one recommendation(s).
Acknowledgements
The Ontario Student Drug Use and Health Survey is an initiative of the Centre for Addiction and Mental Health that is funded by the ongoing support of the Ontario Ministry of Health and Long-Term Care, along with targeted funding from various provincial agencies.
Author contributions
All the authors contributed to the study conception and design. Data analysis was performed by HS. All the authors interpreted results. The first draft of the manuscript was written by HS and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Data availability
Our data cannot be made available in the manuscript, the supplemental files or a public repository due to the Centre for Addiction and Mental Health’s and The Ontario Public and Catholic School Board’s institutional Research Ethics Board agreements. Readers, however, may contact to request the public data file underlying the findings of this study by contacting the Centre for Addiction and Mental Health at info@camh.ca.
Code availability
Code is available upon request from the corresponding author.
Declarations
Ethics approval
Ethics approval was granted by the Research Ethics Boards at the Centre for Addiction and Mental Health, the school board research review committees, and York University. The study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Consent to participate
Informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Allen MS, Vella SA. Screen-based sedentary behaviour and psychosocial well-being in childhood: Cross-sectional and longitudinal associations. Mental Health and Physical Activity. 2015;9:41–47. doi: 10.1016/j.mhpa.2015.10.002. [DOI] [Google Scholar]
- Babic MJ, Smith JJ, Morgan PJ, Eather N, Plotnikoff RC, Lubans DR. Longitudinal associations between changes in screen-time and mental health outcomes in adolescents. Mental Health and Physical Activity. 2017;12:124–131. doi: 10.1016/j.mhpa.2017.04.001. [DOI] [Google Scholar]
- Boak, A., Hamilton, H. A., Adlaf, E. M., & Mann, R. E. (2017). Drug use among Ontario students, 1977–2017: Detailed findings from the Ontario Student Drug Use and Health Survey (OSDUHS) (CAMH Research Document Series No. 46). Toronto, ON: Centre for Addiction and Mental Health.
- Boak, A., Elton-Marshall, T., Mann, R. E., & Hamilton, H. A. (2020). Drug use among Ontario students, 1977–2019: Detailed findings from the Ontario Student Drug Use and Health Survey (OSDUHS). Toronto, ON: Centre for Addiction and Mental Health.
- Boardman, J. D. (2006). Self-rated health among U.S. adolescents. Journal of Adolescent Health, 38(4), 401–408. 10.1016/j.jadohealth.2005.01.006. [DOI] [PMC free article] [PubMed]
- Carson V, Hunter S, Kuzik N, Gray CE, Poitras VJ, Chaput J-P, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Applied Physiology, Nutrition, and Metabolism. 2016;41(6):S240–S265. doi: 10.1139/apnm-2015-0630. [DOI] [PubMed] [Google Scholar]
- Carson V, Chaput J-P, Janssen I, Tremblay MS. Health associations with meeting new 24-hour movement guidelines for Canadian children and youth. Preventive Medicine. 2017;95:7–13. doi: 10.1016/j.ypmed.2016.12.005. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (n.d.). YRBSS - Questionnaires 2017. Available at: http://www.cdc.gov/healthyyouth/data/yrbs/questionnaires.htm. Accessed March 7, 2021.
- Chaput JP, Carson V, Gray CE, Tremblay MS. Importance of all movement behaviors in a 24 hour period for overall health. International Journal of Environmental Research and Public Health. 2014;11(12):12575–12581. doi: 10.3390/ijerph111212575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courser MW, Shamblen SR, Lavrakas PJ, Collins D, Ditterline P. The impact of active consent procedures on nonresponse and nonresponse error in youth survey data: Evidence from a new experiment. Evaluation Review. 2009;33(4):370–395. doi: 10.1177/0193841X09337228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie C, Nic Gabhainn S, Godeau E. The Health Behaviour in School-aged Children: WHO Collaborative Cross-National (HBSC) study: Origins, concept, history and development 1982–2008. International Journal of Public Health. 2009;54(Suppl 2):131–139. doi: 10.1007/s00038-009-5404-x. [DOI] [PubMed] [Google Scholar]
- Faulkner G, Weatherson K, Patte K, Qian W, Leatherdale ST. Are one-year changes in adherence to the 24-hour movement guidelines associated with flourishing among Canadian youth? Preventive Medicine. 2020;139:106179. doi: 10.1016/j.ypmed.2020.106179. [DOI] [PubMed] [Google Scholar]
- Gallagher JE, Wilkie AA, Cordner A, Hudgens EE, Ghio AJ, Birch RJ, et al. Factors associated with self-reported health: Implications for screening level community-based health and environmental studies. BMC Public Health. 2016;16:640. doi: 10.1186/s12889-016-3321-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiger SD, Sabanayagam C, Shankar A. The relationship between insufficient sleep and self-rated health in a nationally representative sample. Journal of Environmental and Public Health. 2012;2012:518263. doi: 10.1155/2012/518263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldfield GS, Henderson K, Buchholz A, Obeid N, Nguyen H, Flament MF. Physical activity and psychological adjustment in adolescents. Journal of Physical Activity and Health. 2011;8(2):157–163. doi: 10.1123/jpah.8.2.157. [DOI] [PubMed] [Google Scholar]
- Goodman E, Huang B, Schafer-Kalkhoff T, Adler NE. Perceived socioeconomic status: A new type of identity that influences adolescents’ self-rated health. Journal of Adolescent Health. 2007;41(5):479–487. doi: 10.1016/j.jadohealth.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grontved A, Singhammer J, Froberg K, Moller NC, Pan A, Pfeiffer KA, et al. A prospective study of screen time in adolescence and depression symptoms in young adulthood. Preventive Medicine. 2015;81:108–113. doi: 10.1016/j.ypmed.2015.08.009. [DOI] [PubMed] [Google Scholar]
- Herman KM, Hopman WM, Sabiston CM. Physical activity, screen time and self-rated health and mental health in Canadian adolescents. Preventive Medicine. 2015;73:112–116. doi: 10.1016/j.ypmed.2015.01.030. [DOI] [PubMed] [Google Scholar]
- Krause NM, Jay GM. What do global self-rated health items measure? Medical Care. 1994;32(9):930–942. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- Leidy NK, Revicki DA, Genesté B. Recommendations for evaluating the validity of quality of life claims for labeling and promotion. Value Health. 1999;2(2):113–127. doi: 10.1046/j.1524-4733.1999.02210.x. [DOI] [PubMed] [Google Scholar]
- Lorem G, Cook S, Leon DA, Emaus N, Schirmer H. Self-reported health as a predictor of mortality: A cohort study of its relation to other health measurements and observation time. Scientific Reports. 2020;10(1):4886. doi: 10.1038/s41598-020-61603-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubans DR, Hesketh K, Cliff DP, Barnett LM, Salmon J, Dollman J, et al. A systematic review of the validity and reliability of sedentary behaviour measures used with children and adolescents. Obesity Reviews. 2011;12(10):781–799. doi: 10.1111/j.1467-789X.2011.00896.x. [DOI] [PubMed] [Google Scholar]
- Nascimento-Ferreira MV, Collese TS, de Moraes ACF, Rendo-Urteaga T, Moreno LA, Carvalho HB. Validity and reliability of sleep time questionnaires in children and adolescents: A systematic review and meta-analysis. Sleep Medicine Reviews. 2016;30:85–96. doi: 10.1016/j.smrv.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Parfitt G, Pavey T, Rowlands AV. Children’s physical activity and psychological health: The relevance of intensity. Acta Paediatrica. 2009;98(6):1037–1043. doi: 10.1111/j.1651-2227.2009.01255.x. [DOI] [PubMed] [Google Scholar]
- Patte KA, Faulkner G, Qian W, Duncan M, Leatherdale ST. Are one-year changes in adherence to the 24-hour movement guidelines associated with depressive symptoms among youth? BMC Public Health. 2020;20(1):793–793. doi: 10.1186/s12889-020-08887-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampasa-Kanyinga H, Standage M, Tremblay MS, Katzmarzyk PT, Hu G, Kuriyan R, et al. Associations between meeting combinations of 24-h movement guidelines and health-related quality of life in children from 12 countries. Public Health. 2017;153:16–24. doi: 10.1016/j.puhe.2017.07.010. [DOI] [PubMed] [Google Scholar]
- Sampasa-Kanyinga H, Chaput JP, Goldfield GS, Janssen I, Wang J, Hamilton HA, et al. 24-hour movement guidelines and suicidality among adolescents. Journal of Affective Disorders. 2020;274:372–380. doi: 10.1016/j.jad.2020.05.096. [DOI] [PubMed] [Google Scholar]
- Sampasa-Kanyinga, H., Chaput, J. P., Goldfield, G. S., Janssen, I., Wang, J., Hamilton, H. A., et al. (2020b). The Canadian 24-Hour Movement Guidelines and Psychological Distress among Adolescents: Les Directives canadiennes en matiere de mouvement sur 24 heures et la detresse psychologique chez les adolescents. Canadian Journal of Psychiatry, 706743720970863.10.1177/0706743720970863 [DOI] [PMC free article] [PubMed]
- Sampasa-Kanyinga H, Colman I, Goldfield GS, Janssen I, Wang J, Hamilton HA, et al. Associations between the Canadian 24 h movement guidelines and different types of bullying involvement among adolescents. Child Abuse and Neglect. 2020;108:104638. doi: 10.1016/j.chiabu.2020.104638. [DOI] [PubMed] [Google Scholar]
- Sampasa-Kanyinga H, Colman I, Goldfield GS, Janssen I, Wang J, Tremblay MS, et al. 24-hour movement behaviors and internalizing and externalizing behaviors among youth. Journal of Adolescent Health. 2020 doi: 10.1016/j.jadohealth.2020.09.003. [DOI] [PubMed] [Google Scholar]
- Saunders TJ, Gray CE, Poitras VJ, Chaput J-P, Janssen I, Katzmarzyk PT, et al. Combinations of physical activity, sedentary behaviour and sleep: Relationships with health indicators in school-aged children and youth. Applied Physiology, Nutrition, and Metabolism. 2016;41(6):S283–S293. doi: 10.1139/apnm-2015-0626. [DOI] [PubMed] [Google Scholar]
- Schmitz KH, Harnack L, Fulton JE, Jacobs DR, Jr, Gao S, Lytle LA, et al. Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. Journal of School Health. 2004;74(9):370–377. doi: 10.1111/j.1746-1561.2004.tb06632.x. [DOI] [PubMed] [Google Scholar]
- Scott JJ, Morgan PJ, Plotnikoff RC, Lubans DR. Reliability and validity of a single-item physical activity measure for adolescents. Journal of Paediatrics and Child Health. 2015;51(8):787–793. doi: 10.1111/jpc.12836. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. (2013). Canadian Community Health Survey (CCHS): User Guide 2012 and 2011–2012 Microdata Files (p. 100). Statistics Canada.
- Štefan L, Juranko D, Prosoli R, Barić R, Sporiš G. Self-reported sleep duration and self-rated health in young adults. Journal of Clinical Sleep Medicine. 2017;13(7):899–904. doi: 10.5664/jcsm.6662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay MS, Carson V, Chaput JP, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Applied Physiology, Nutrition, and Metabolism. 2016;41(6 Suppl 3):S311–327. doi: 10.1139/apnm-2016-0151. [DOI] [PubMed] [Google Scholar]
- Vingilis ER, Wade TJ, Seeley JS. Predictors of adolescent self-rated health. Canadian Journal of Public Health. 2002;93(3):193–197. doi: 10.1007/BF03404999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, G., Di Nardo, F., & Verma, A. (2017). The relationship between self-reported health status and signs of psychological distress within European urban contexts. European Journal of Public Health, 27(suppl_2), 68–73. doi:10.1093/eurpub/ckx008. [DOI] [PubMed]
- World Health Organization. (2011). WHO Anthro (version 3.2.2) and macros. World Health Organization, Geneva, Switzerland.
- World Health Organization. (2020). Physical activity. Fact sheet. World Health Organization; Geneva, Switzerland. Available at: https://www.who.int/news-room/fact-sheets/detail/physical-activity. Last accessed: March 19, 2021.
- Yeo SC, Jos AM, Erwin C, Lee SM, Lee XK, Lo JC, et al. Associations of sleep duration on school nights with self-rated health, overweight, and depression symptoms in adolescents: Problems and possible solutions. Sleep Medicine. 2019;60:96–108. doi: 10.1016/j.sleep.2018.10.041. [DOI] [PubMed] [Google Scholar]
- Zhang T, Lu G, Wu XY. Associations between physical activity, sedentary behaviour and self-rated health among the general population of children and adolescents: A systematic review and meta-analysis. BMC Public Health. 2020;20(1):1343. doi: 10.1186/s12889-020-09447-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Our data cannot be made available in the manuscript, the supplemental files or a public repository due to the Centre for Addiction and Mental Health’s and The Ontario Public and Catholic School Board’s institutional Research Ethics Board agreements. Readers, however, may contact to request the public data file underlying the findings of this study by contacting the Centre for Addiction and Mental Health at info@camh.ca.
Code is available upon request from the corresponding author.


