Abstract
Objective
Adults in food-insecure households will often sacrifice their own nutritional needs so that children are fed first. This shielding may protect children from malnutrition, but its links to mental health and well-being have not been closely examined. The aim of this study is to explore these links.
Methods
We used data from three cycles of the Canadian Community Health Survey (n = 28,871 youth, 74,416 adults) to identify shielded children (those who reported not being food insecure but lived in food-insecure households). Using Poisson regression, we examined youth and adult mental health and well-being (mood disorder, anxiety disorder, fair/poor mental health, fair/poor health, and low life satisfaction) in shielding households compared to food-secure households and food-insecure households where children were not shielded.
Results
About one in six (15.3%) households with children was food insecure. One third of these (6.3%) included children who were shielded from experiencing food insecurity. Shielded youth did not differ significantly from food-secure youth in three of the five outcomes examined. However, unshielded youth, compared to food-secure youth, showed increased risks of every health outcome we investigated. Adults in food-insecure households also reported worse mental health than food-secure adults but better mental health if children were shielded.
Conclusion
Shielding is associated with reduced risk of common psychiatric outcomes and poor mental health in youth and adults, possibly because it is associated with milder forms of food insecurity. The inability to protect children from having inadequate access to food may compound the psychological strain of food insecurity on mental health and well-being among adults.
Supplementary Information
The online version contains supplementary material available at 10.17269/s41997-021-00597-2.
Keywords: Food insecurity, Mental health, Shielding, Anxiety, Mood disorders, Hunger
Résumé
Objectif
Les adultes d’un ménage en insécurité alimentaire sacrifient souvent leurs propres besoins nutritionnels afin que les enfants soient nourris en priorité. Cette protection peut préserver les enfants de la malnutrition, mais ses liens avec la santé mentale et le bien-être n’ont pas été spécifiquement examinés. L’objectif de cette étude est d’explorer ces liens.
Méthode
Nous avons utilisé les données de trois cycles de l’Enquête sur la santé dans les collectivités canadiennes (n = 28 871 jeunes, 74 416 adultes) dans le but d’identifier les ménages en insécurité alimentaire dans lesquels les enfants ne se trouvaient pas en insécurité alimentaire ( « protégés »). Afin de comparer la santé mentale et le bien-être des jeunes et adultes vivant au sein d’un ménage en insécurité alimentaire « protégé » par rapport aux individus vivant au sein d’un ménage en sécurité alimentaire et d’un ménage en insécurité alimentaire où les enfants n’étaient pas protégés de cette insécurité, nous avons utilisé la régression de Poisson.
Résultats
Environ un ménage avec des enfants sur six (15,3 %) était en insécurité alimentaire. Un tiers de ces enfants (6,3 %) étaient protégés de l’insécurité alimentaire. Les enfants « protégés » ne différaient pas significativement des enfants vivant au sein d’un ménage en sécurité alimentaire pour la plupart des résultats concernant la santé mentale. Les enfants « non protégés » ont montré des risques accrus pour chaque indicateur étudié (trouble de l’humeur, trouble de l’anxiété, santé mentale moyenne/ mauvaise, santé moyenne/ mauvaise, faible satisfaction de la vie). Les adultes vivant dans un ménage en insécurité alimentaire ont également déclaré une plus mauvaise santé mentale que les adultes vivant dans un ménage en sécurité alimentaire, mais une meilleure santé mentale lorsque les enfants du ménage étaient protégés de l’insécurité alimentaire.
Conclusion
La protection des enfants au sein d’un ménage en insécurité alimentaire est associé à une réduction du risque de problèmes psychiatriques communs et de mauvaise santé mentale chez les jeunes et les adultes, possiblement parce que les ménages dans lesquels les enfants sont protégés font face à des formes plus légères d’insécurité alimentaire. L’incapacité de protéger les enfants et l’accès inadéquat à la nourriture peut aggraver la pression psychologique de l’insécurité alimentaire sur la santé mentale et le bien-être des adultes.
Mots-clés: Insécurité alimentaire, santé mentale, protection, anxiété, trouble de l’humeur, faim
Introduction
Poor access to safe, sufficient, and nutritious food is a global public health concern (Food and Agricultural Organisation, 2020). In Canada, the problem of food insecurity affects one in every eight households and disproportionately affects the poor (Tarasuk et al., 2019), Indigenous and Black communities, and families with children (Dhunna & Tarasuk, 2021; Tarasuk & Mitchell, 2020). Food insecurity is associated with poor physical and mental health in all age groups, independently of income poverty (Kirkpatrick et al., 2015; Men et al., 2021; Maynard et al., 2019). Its resulting malnutrition can affect gut microbiota and deficiencies in sialic acid, tryptophan, and vitamin D which are important for healthy brain development in childhood (Jenkins et al., 2016). Additionally, the many adversities that accompany food insecurity, including chronic hunger, having to cut or skip meals, and the stigma of relying on donated or discarded food, elicit chronic psychological stress and increase the risks of developing mood and anxiety disorders and other stress-related health problems (Firth et al., 2020; Owen & Corfe, 2017; Nagata et al., 2019; McLaughlin et al., 2012; Pryor et al., 2016).
To date, few quantitative studies have examined attempts by adults to protect children from food insecurity. “Shielding” occurs when adults sacrifice their own nutritional needs during times of scarcity so that children can be fed first (Coleman-Jensen et al., 2013; Hamelin et al., 2002). This nurturing response may protect children from the physiological consequences of food scarcity, but whether shielding also protects children and youth from negative psychological outcomes is unclear (Coleman-Jensen et al., 2013; Fram et al., 2011; Ashiabi & O’Neal, 2007). The lack of research about this question is due, in part, to a reliance on singular household measures of food insecurity that fail to distinguish the experiences of children from those of adults. An exception is the US Department of Agriculture’s Household Food Security Survey Module (HFSSM), an 18-item scale that was adapted for three recent survey cycles of Canadian Community Health Survey (CCHS) (Bickel et al., 2000). This tool measures child food security separately from adult food security, and thus allows researchers to identify households where children report being food secure despite living in a household that is not.
The objective of this study was to investigate the cross-sectional association of shielding and mental health and well-being in a community sample of youth and adults who participated in the CCHS. We expected to find poorer psychological outcomes in youth (12–17 years) and adults in food-insecure households as compared with those in food-secure households (Men et al., 2021). We also expected to find better psychological outcomes as a function of shielding children from experiencing food insecurity.
Methods
Sample
We used public use microdata files from three recent cycles of the CCHS (2007–2008, 2011–2012, and 2017–2018). The CCHS is a biennial cross-sectional survey that represents 98% of the non-institutionalized population of Canada aged 12 years and older. Individuals living on Indian Reserves and Crown lands, Canadian residents of institutions, full-time members of the Canadian Forces, and residents of certain remote regions are not included. Random samples of households were identified based on geographic areas, phone numbers, and Canadian Child Benefit frames and the data were weighted according to geographic location, sex, and age (Brisebois & Thivierge, 2001). Approximately 130,000 households per survey cycle were interviewed by phone or in person using computer-assisted standardized assessments. For this analysis, we selected three survey cycles that fielded the HFSSM in all Canadian provinces and territories and a subset of data that contained information on child and adult food insecurity.
CCHS surveyors obtained formal informed consent from parents or adult guardians before interviewing a selected adolescent below age 16. One member per household was randomly selected to answer questions about themselves. Questions about food insecurity and household income were answered by an adult when the selected interviewee was younger than 18 years (or younger than 16 years in 2007–2008). Therefore, data on child and household food insecurity were mostly provided by adults, except for 16- to 17-year-olds in 2007–2008. All other questions about adult and child mental health and well-being were self-reported.
Measures
We determined the food insecurity status of the household using data collected with the HFSSM (Bickel et al., 2000). This scale was developed and validated by United States Department of Agriculture and later adapted for the CCHS by Health Canada. It contains 18 questions about a household’s access to food over the past 12 months ranked by increasing severity. Eight items describe the child(ren)’s experiences, ranging from “You or other adults in your household relied on only a few kinds of low-cost food to feed child(ren)” to “Any of the child(ren) ever did not eat for whole day.” Ten items describe the adults’ experiences, ranging from “You and other household members worried food would run out before you got money to buy more” to “You or other adults in your household ever did not eat for whole day.” According to Health Canada guidelines (Health Canada, n.d.), negative answers to all questions would identify a household as food secure. A summation of affirmative answers to the eight child items would identify children as either marginally food insecure (1 item), moderately food insecure (2 to 4 items), or severely food insecure (5 to 8 items). A summation of affirmative answers to the ten adult items would identify adults as either marginally food insecure (1 item), moderately food insecure (2 to 5 items), or severely food insecure (6 to 10 items).
Health and well-being measures included five dichotomous outcomes: previously diagnosed mood disorders (depression, bipolar disorder, mania, or dysthymia), previously measured anxiety disorders (phobia, obsessive-compulsive disorder, or panic disorder), fair or poor mental health (versus good, very good, or excellent), fair or poor health (versus good, very good, or excellent), and low life satisfaction (dissatisfied or very dissatisfied, versus neither satisfied nor dissatisfied, satisfied, or very satisfied). The questions were asked directly to respondents of all age groups. Although these items are brief and not validated at an individual level using clinical diagnostic information, previous research found similar prevalence of mood and anxiety disorders in CCHS and health administrative data captured in the Canadian Chronic Disease Surveillance System (i.e., ICD-9/-10-CA codes from physician billing claims and hospital discharge records) (O’Donnell et al., 2016).
We adjusted for potential confounders in associations with food insecurity by including individual demographic characteristics (sex [male/female], race/ethnicity [white vs. Black, Indigenous and other groups combined]), household size, household income quintile, highest education in the household (no secondary, secondary, or postsecondary), high body mass index (BMI ≥ 25 calculated using self-reported height and weight), and survey cycle (Tarasuk et al., 2019; Dhunna & Tarasuk, 2021; Men et al., 2021; Bøe et al., 2012; Sentenac et al., 2016; Vanzella-Yang & Veenstra, 2021). The public use datafiles of the CCHS did not identify specific race/ethnicity groups. Unfortunately, we could not control for the intensity or severity of food insecurity due to its high degree of overlap with shielding status. Shielding was identified in 64.8% (95% CI: 62.6–66.9) of households in marginal food insecurity, 33.9% (95% CI: 33.0–35.8) of households in moderate food insecurity, and 11.1% (95% CI: 6.0–6.5) of households in severe food insecurity, Wald χ2 = 7659.20, p < 0.001.
Data cleaning and analysis
The three cross-sectional surveys were treated as independent samples. We could not rule out the possibility that some cases participated in more than one cycle due to the anonymous nature of the data. Of 339,121 cases in the three cycles combined, we excluded 9843 cases (2.9%) due to non-response to all HFSSM items, 256,149 cases (75.5%) for missing data on child food security, and one case with a household size of 1 person (see sample flow chart in supplementary Fig. 1). The analyses of mental health and well-being were stratified by age group, 12 to 17 years (n = 28,871), and 18+ years (n = 74,416). We operationalized shielding as households with food-secure children living with adults experiencing marginal, moderate, or severe food insecurity. This group was compared to non-shielding households that included children experiencing marginal, moderate, or severe food insecurity and to a group of food-secure households where no members experienced food insecurity.
Although missing data were few, we imputed missing observations on mood disorder (0.2%), anxiety disorder (0.2%), high body mass (8.3%), and household income quintile (7.7%) to ensure the most reliable estimations possible in our analysis. There were no missing data on the other variables. This step involved multiple imputations using the mi impute chained procedure in Stata version 16.1 (StataCorp. LP, College Station, Texas, USA), which uses iterative multivariable regression procedure to generate distributions for each variable with missing data that are conditional on all other variables in the imputation models (StataCorp, 2011). Variables with missing data were imputed using logistic (mood disorder, anxiety disorder, excess body mass) or ordered logistic (household income quintile, education) link functions and model estimates were pooled across ten imputed data sets using Stata’s mi estimate procedures.
Within Stata’s mi toolkit, we estimated the weighted relative risk (RR) of each mental health and well-being outcome using Poisson regression with robust variance estimators and adjustment for covariates. These analyses compared food-secure households (reference category) to food-insecure households with and without shielding. In subsequent analysis, we tested differences in mental health and well-being between shielding and non-shielding households by changing the reference category. Adjusted RRs are shown in tables and charts. We also estimated the predicted prevalence of each mental health and well-being outcome to graphically show differences between age groups by shielding status. In other analyses (not shown), we tested for moderating effects of sex but found none. Therefore, the results of more parsimonious models that exclude interactions of shielding status and sex are shown below.
Ethics approval
We accessed the data through the Data Liberation Initiative, a partnership between post-secondary institutions and Statistics Canada. The research was approved by the Institutional Review Board of the Faculty of Medicine at McGill University (A03-M13-19A). All data were deidentified to ensure confidentiality and protection of the respondents.
Results
This sample of households with children included 28,871 youth and 74,416 adult respondents. An estimated 84.7% of the sample were in food-secure households, 6.3% were food insecure but shielding children and youth, and 9.1% were food insecure and not shielding. A majority (70.7%) lived in households of four or more persons and 71.0% of the sample were white. Other characteristics of the sample are shown in Table 1.
Table 1.
Descriptive characteristics of the sample (n = 103,287)
| Variable | Unweighted | Weighted | ||
|---|---|---|---|---|
| n | % | n | % | |
| Age group | ||||
| Youth, 12–17 years | 28,871 | 28.0 | 22,337 | 21.6 |
| Adults, 18+ years | 74,416 | 72.0 | 80,950 | 78.4 |
| Gender | ||||
| Male | 45,899 | 44.4 | 49,939 | 48.3 |
| Female | 57,388 | 55.6 | 53,348 | 51.7 |
| Household size | ||||
| 2 persons | 7167 | 6.9 | 4401 | 4.3 |
| 3 persons | 28,896 | 28.0 | 25,817 | 25.0 |
| 4 persons | 67,224 | 65.1 | 73,069 | 70.7 |
| Household income (quintile group) | ||||
| 1 (lowest) | 18,476 | 19.4 | 21,508 | 20.8 |
| 2 | 18,614 | 19.5 | 21,705 | 21.0 |
| 3 | 20,697 | 21.7 | 23,087 | 22.4 |
| 4 | 20,324 | 21.7 | 20,521 | 19.9 |
| 5 (highest) | 17,216 | 18.1 | 16,466 | 15.9 |
| Education | ||||
|
Less than secondary Secondary Post-secondary |
7541 11,444 84,302 |
7.3 11.1 81.6 |
5706 10,706 86,876 |
5.5 10.4 84.1 |
| High body mass | ||||
| No (BMI < 25) | 47,177 | 49.8 | 52,408 | 50.7 |
| Yes (BMI ≥ 25) | 47,529 | 50.2 | 50,879 | 49.3 |
| Race/ethnicity | ||||
| White | 77,796 | 78.6 | 73,294 | 71.0 |
| Non-white | 21,183 | 21.4 | 29,993 | 29.0 |
| Shielding status of household | ||||
| Food secure | 86,343 | 83.6 | 87461 | 84.7 |
| Food insecure, youth are shielded | 6777 | 6.6 | 6457 | 6.3 |
| Food insecure, youth are not shielded | 10,167 | 9.8 | 9369 | 9.1 |
Note: The CCHS uses two sampling frames for its sample selection: an area frame for the Canadian population aged 18 and over, and a frame of telephone numbers from Canada Child Benefit (CCB) records for the 12–17 population. Sample weights take this stratified, multistage sampling design into account and were applied to an ensure accurate representation of the Canadian population (Statistics Canada, n.d.).
Our analytic sample differed from excluded cases in some respects. Compared to the 265,993 cases that were removed, our sample included more youth (21.6% vs. 0.6%) and represented households that were more likely to have four or more persons (70.7% vs. 12.5%), children under age 12 (62.6% vs. 0.1%), and a member with post-secondary education (84.1% vs. 73.8%). Our sample was also more likely to represent a racialized minority (29.5% vs. 17.8%). As shown in Table 2, the weighted prevalence of our mental health and well-being outcomes was lower in youth (0.7–1.8%) than in adults (5.3–6.3%).
Table 2.
Mental health outcomes in youth and adults (n = 103,287)
| Unweighted | Weighted | |||
|---|---|---|---|---|
| n | % | n | % | |
| Youth, 12–17 years | ||||
| Mood disorder | 1005 | 1.0 | 714 | 0.7 |
| Anxiety disorder | 1744 | 1.7 | 1312 | 1.3 |
| Fair or poor mental health | 2310 | 2.2 | 1812 | 1.8 |
| Fair or poor health | 1256 | 1.2 | 931 | 0.9 |
| Low life satisfaction | 2173 | 2.1 | 1620 | 1.6 |
| Adults, 18+ years | ||||
| Mood disorder | 5852 | 5.7 | 5578 | 5.4 |
| Anxiety disorder | 5551 | 5.4 | 5482 | 5.3 |
| Fair or poor mental health | 4902 | 4.8 | 5483 | 5.3 |
| Fair or poor health | 5408 | 5.2 | 6094 | 5.9 |
| Low life satisfaction | 5384 | 5.2 | 6499 | 6.3 |
Note: The CCHS uses two sampling frames for its sample selection: an area frame for the Canadian population aged 18 and over, and a frame of telephone numbers from Canada Child Benefit (CCB) records for the 12–17 population. Sample weights take this stratified, multistage sampling design into account and were applied to ensure an accurate representation of the Canadian population (Statistics Canada, n.d.).
Regression analyses showed that the relative risk of each mental health and well-being outcome was significantly higher in food-insecure households than in food-secure households, in both youth (Table 3) and adults (Table 4). However, there were differences in risk depending on whether children and youth were shielded. The youth in households where children and youth were not shielded showed, as for adults, elevated risks of mood disorder (RR = 1.92, 95% CI 1.41–2.62), anxiety disorder (RR = 1.44, 95% CI 1.11–1.87), fair or poor mental health (RR = 1.45, 95% CI 1.06–1.99), fair or poor general health (RR = 1.48, 95% CI 1.11–1.97), and low life satisfaction (RR = 1.64, 95% CI 1.15–2.35) compared to youth from food-secure households. However, the youth in households where youth were shielded showed an elevated risk of only anxiety disorder (RR = 1.44, 95% CI 1.02–2.03), and fair or poor mental health (RR = 1.56, 95% CI 1.07–2.29) and did not differ significantly from youth in food-secure households with respect to other mental health and well-being outcomes. The adults in food-insecure households showed consistently greater relative risks of poor mental health and well-being compared to adults in food-secure households, and these risks were mostly greater in non-shielding households compared to shielding households (Table 4).
Table 3.
Associations between shielding and mental health problems in youth (n = 28,871)
| Variables | Mood disorder | Anxiety disorder | Fair or poor mental health | Fair or poor health | Low life satisfaction | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Sex | ||||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Female | 1.71 | 1.34,2.18 | 2.07 | 1.71,2.51 | 1.65 | 1.34,2.03 | 0.98 | 0.79,1.22 | 1.56 | 1.23,1.97 |
| Household size | ||||||||||
| 2 persons | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 3 persons | 0.77 | 0.50,1.18 | 0.72 | 0.52,1.00 | 0.65 | 0.43,0.96 | 0.81 | 0.55,1.21 | 0.85 | 0.55,1.31 |
| 4+ persons | 0.47 | 0.31,0.72 | 0.51 | 0.37,0.70 | 0.53 | 0.36,0.77 | 0.83 | 0.58,1.20 | 0.77 | 0.50,1.17 |
| Race/ethnicity | ||||||||||
| White | ||||||||||
| Non-white | 0.58 | 0.42,0.79 | 0.58 | 0.44,0.76 | 1.19 | 0.92,1.52 | 1.10 | 0.84,1.45 | 1.23 | 0.93,1.64 |
| Household income | ||||||||||
| 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 4 | 1.31 | 0.90,1.90 | 0.91 | 0.67,1.22 | 1.42 | 1.00,2.02 | 1.37 | 0.91,2.07 | 1.28 | 0.87,1.90 |
| 3 | 1.06 | 0.71,1.56 | 1.10 | 0.83,1.47 | 1.35 | 0.95,1.92 | 1.42 | 0.96,2.10 | 1.56 | 1.08,2.25 |
| 2 | 1.20 | 0.81,1.77 | 1.00 | 0.74,1.35 | 1.24 | 0.85,1.80 | 1.40 | 0.92,2.13 | 1.43 | 0.99,2.07 |
| 1 (lowest) | 1.09 | 0.73,1.65 | 1.06 | 0.77,1.46 | 1.83 | 1.27,2.64 | 1.54 | 1.03,2.30 | 1.90 | 1.26,2.88 |
| Highest household education | ||||||||||
| Post-secondary | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Secondary | 1.17 | 0.85,1.62 | 0.74 | 0.55,0.99 | 0.66 | 0.47,0.92 | 1.11 | 0.79,1.58 | 0.99 | 0.70,1.41 |
| Below secondary | 1.26 | 0.78,2.02 | 1.16 | 0.84,1.59 | 1.01 | 0.68,1.49 | 1.68 | 1.20,2.36 | 0.99 | 0.71,1.38 |
| BMI | ||||||||||
| < 25 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| ≥ 25 | 1.01 | 0.74,1.38 | 0.97 | 0.75,1.24 | 1.16 | 0.91,1.47 | 1.65 | 1.23,2.20 | 1.48 | 1.11,1.98 |
| Survey cycle | ||||||||||
| 2007–2008 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 2011–2012 | 1.25 | 0.93,1.69 | 1.29 | 1.02,1.63 | 1.04 | 0.79,1.37 | 1.05 | 0.82,1.34 | 0.63 | 0.48,0.83 |
| 2017–2018 | 2.03 | 1.38,3.00 | 2.51 | 1.88,3.35 | 1.78 | 1.30,2.43 | 0.69 | 0.47,1.00 | 0.38 | 0.27,0.54 |
| Shielding status | ||||||||||
| Food secure | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Shielded | 1.15 | 0.78,1.69 | 1.44 | 1.02,2.03 | 1.56 | 1.07,2.29 | 1.27 | 0.79,2.07 | 1.54 | 0.94,2.52 |
| Not shielded | 1.92 | 1.41,2.62 | 1.44 | 1.11,1.87 | 1.45 | 1.06,1.99 | 1.48 | 1.11,1.97 | 1.64 | 1.15,2.35 |
Note: Shown are relative risk (RR) and 95% confidence intervals (CI). Statistically significant (p<0.05) RRs are bolded
Table 4.
Associations between food insecurity shielding and mental health problems in adults (n = 74,416)
| Variables | Mood disorder | Anxiety disorder | Fair or poor mental health | Fair or poor health | Low life satisfaction | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Sex | ||||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Female | 2.44 | 2.19,2.72 | 2.15 | 1.92,2.40 | 1.46 | 1.29,1.64 | 1.23 | 1.10,1.36 | 0.97 | 0.87,1.08 |
| Household size | ||||||||||
| 2 persons | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 3 persons | 0.74 | 0.64,0.87 | 0.79 | 0.68,0.91 | 0.78 | 0.64,0.95 | 0.86 | 0.72,1.02 | 0.68 | 0.58,0.80 |
| 4+ persons | 0.60 | 0.52,0.69 | 0.70 | 0.61,0.80 | 0.74 | 0.61,0.89 | 0.78 | 0.66,0.91 | 0.54 | 0.46,0.62 |
| Race/ethnicity | ||||||||||
| White | ||||||||||
| Non-white | 0.52 | 0.46,0.60 | 0.43 | 0.37,0.49 | 0.84 | 0.73,0.97 | 1.14 | 1.02,1.28 | 1.39 | 1.24,1.56 |
| Household income | ||||||||||
| 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 4 | 1.29 | 1.09,1.52 | 1.28 | 1.08,1.53 | 1.39 | 1.12,1.74 | 1.31 | 1.07,1.61 | 1.33 | 1.05,1.69 |
| 3 | 1.36 | 1.15,1.60 | 1.35 | 1.14,1.59 | 1.42 | 1.15,1.76 | 1.62 | 1.34,1.98 | 1.86 | 1.48,2.34 |
| 2 | 1.40 | 1.18,1.66 | 1.48 | 1.25,1.75 | 1.68 | 1.35,2.08 | 1.76 | 1.45,2.15 | 2.13 | 1.70,2.68 |
| 1 (lowest) | 1.60 | 1.35,1.91 | 1.80 | 1.51,2.15 | 1.94 | 1.55,2.42 | 2.60 | 2.12,3.17 | 2.60 | 2.06,3.27 |
| Highest household education | ||||||||||
| Post-secondary | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Secondary | 1.15 | 1.00,1.32 | 1.08 | 0.94,1.23 | 1.12 | 0.96,1.31 | 1.38 | 1.20,1.58 | 1.08 | 0.94,1.25 |
| Below secondary | 1.24 | 1.02,1.50 | 1.08 | 0.89,1.32 | 1.13 | 0.91,1.41 | 1.63 | 1.34,1.97 | 1.53 | 1.25,1.88 |
| BMI | ||||||||||
| < 25 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| ≥ 25 | 1.45 | 1.32,1.59 | 1.21 | 1.10,1.33 | 1.15 | 1.03,1.30 | 1.71 | 1.54,1.90 | 1.19 | 1.07,1.32 |
| Survey cycle | ||||||||||
| 2007–2008 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 2011–2012 | 1.10 | 0.98,1.24 | 1.23 | 1.08,1.39 | 1.20 | 1.03,1.39 | 1.01 | 0.89,1.15 | 0.83 | 0.73,0.94 |
| 2017–2018 | 1.23 | 1.11,1.37 | 1.63 | 1.46,1.81 | 1.49 | 1.30,1.71 | 0.89 | 0.79,1.00 | 0.71 | 0.63,0.80 |
| Shielding status | ||||||||||
| Food secure | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Shielded | 1.84 | 1.59,2.12 | 1.75 | 1.51,2.02 | 2.14 | 1.77,2.57 | 1.71 | 1.47,1.99 | 2.38 | 2.02,2.80 |
| Not shielded | 2.41 | 2.13,2.73 | 2.07 | 1.80,2.37 | 2.71 | 2.33,3.15 | 2.21 | 1.93,2.53 | 2.94 | 2.57,3.36 |
Note: Shown are relative risk (RR) and 95% confidence intervals (CI). Statistically significant (p<0.05) RRs are bolded
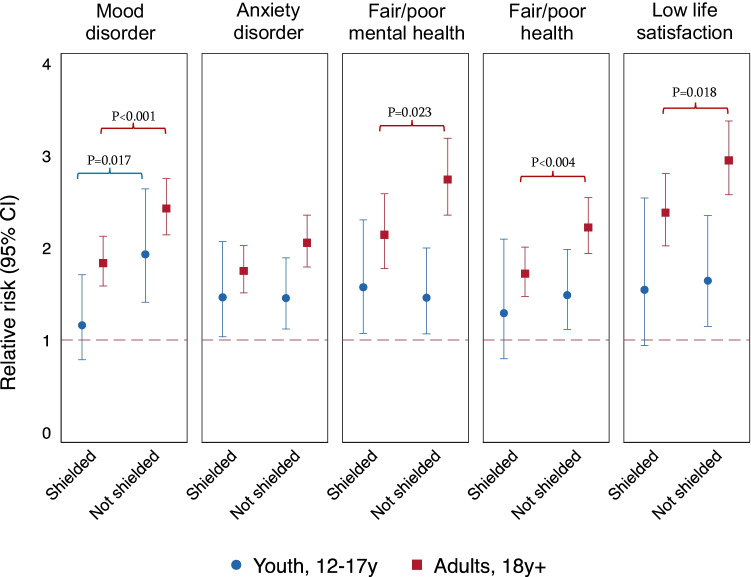
Figure 1 shows the differences in adjusted RR between shielding and non-shielding households. Apart from mood disorder, youth in non-shielding households showed similar relative risks of mental health and well-being outcomes as youth in shielding households. Only with respect to mood disorder did we observe that shielding was associated with reduced risk compared to households where children and youth were not shielded (RR = 0.60, p = 0.015). In all other outcomes, the youth in shielding and non-shielding households showed similar risks of experiencing mental health problems and low well-being.
Fig. 1.
Relative risk of mental health problems in youth and adults in food-insecure households where youth are shielded and not shielded, adjusted for sex, household size, race/ethnicity, household income, highest household education, BMI, and survey cycle. Reference groups are food-secure youth and adults respectively. p-values are shown where significant differences were found between shielded and unshielded groups.
A different risk profile was observed in adults, who showed a 22–37% greater risk of most mental health and well-being outcomes where children and youth were not shielded compared to adults in households where children and youth were shielded. Mood disorder showed the greatest increase in risk between these groups, from RR = 1.84 (95% CI 1.59–2.12) to 2.41 (95% CI 2.13–2.73), p < 0.001. Anxiety disorder in adults showed no significant difference in risk between shielding households (RR = 1.75, 95% CI 1.51–2.02) and non-shielding households (RR = 2.07, 95% CI 1.80–2.37; Fig. 1).
The other covariates in our regression analysis revealed social patterns in mental health and well-being (Tables 3 and 4). Female youth and adults had greater risks of mood disorder, anxiety disorders, and fair or poor mental health compared with their male counterparts. Household size was negatively associated with mood and anxiety disorder and fair or poor mental health in youth and with all five outcomes in adults. Furthermore, associations with household income, education, and high BMI were more apparent in adults than in youth.
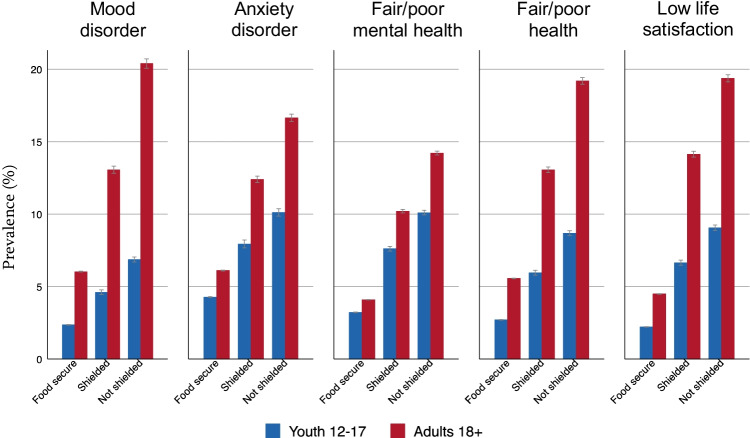
Figure 2 displays age group differences in adjusted predicted prevalence of each mental health and well-being outcome by shielding status. This figure demonstrates greater prevalence of poor mental health or reduced well-being among food-insecure households compared to food-secure households. These differences tended to increase if children and youth in the household were not shielded from food insecurity.
Fig. 2.
Predicted prevalence of mental health problems in youth and adults in food-secure households and food-insecure households where youth are shielded and not shielded. Error bars indicate 95% confidence intervals.
Discussion
This cross-sectional study examined the association of shielding children from food insecurity with the mental health and well-being of youth and adults. Approximately one in six (15.3%) households with children was found to be food insecure. Of these, about one in three (6.3% of the sample) included children who were not food insecure. Youth respondents in “shielding” households showed a reduced risk of mood disorder compared to youth in non-shielding households, but in all other outcomes showed similar risks of poor mental health and reduced well-being as a function of food insecurity. In adults, shielding children was associated with a reduced risk in four mental health and well-being outcomes compared to adults in non-shielding households. In all, our results show different mental health profiles in food-insecure households that depended on whether children and adults both experienced food insecurity.
The findings are consistent with prior research and suggest that shielding children from undernourishment (e.g., skipping or cutting meals by adults so that children have enough to eat) does not protect youth from the harmful psychological effects of food insecurity (Coleman-Jensen et al., 2013; Hamelin et al., 2002). Worrying about food supplies and having to rely on donated food, for instance, are intensely stressful experiences that disrupt parenting behaviours and family functioning (Coleman-Jensen et al., 2013). All members of a household will experience this strain regardless of how food is distributed. Moreover, some youths may conserve food or eat less than they wish to without their parent’s awareness, meaning that they may be less shielded from food insecurity than their parents believe (Bernard et al., 2018), and others may themselves be shielding younger children (Coleman-Jensen et al., 2013). We found no evidence to suggest that shielding was associated with reduced risks of anxiety disorder, having fair or poor health or mental health, or low life satisfaction in youth.
We did observe significantly reduced risks of mood disorder in youth and adults as a function of shielding. However, there were uncontrolled third variables and other study limitations that may account for these associations and should be noted. First, the presence of a mood disorder in parents is itself a robust risk factor for emotional problems in children and youth, and we could not control for this indirect pathway to youth mental health because of the survey design (one respondent per household) (Madigan et al., 2018). Second, adults might be better able to shield children from milder forms of food insecurity. An increased risk in mental health problems could have resulted from more severe food insecurity, and we could not control for the intensity or severity of food insecurity in the associations due to a high degree of overlap with shielding. Another possibility is that adults with better mental health and well-being are in a better position to shield. Third, because the HFSSM is a household assessment, we were unable to determine whether youth respondents in our sample were shielded by adults or whether the adult respondents were, in fact, parents shielding their children. Fourth, we were unable to explore important differences between Indigenous and other ethnic and racial groups that are known to underlie wide disparities in food access and mental well-being in the Canadian population (Chiu et al., 2018).
Despite these limitations, the study benefited from a large, representative community sample of youth and adults and assessments of various facets of mental health. The HFSSM provided unique information on adult and child food security, and the study included crucial statistical controls, including education and household income. Furthermore, a common set of mental health and well-being self-assessments allowed us to compare the psychological consequences of food insecurity in youth and adults, thus replicating prior studies in Canada (Men et al., 2021) and elsewhere (Melchior et al., 2012; Martin et al., 2016).
Shielding aside, the results clearly show that food insecurity is associated with poor mental health and low well-being in adults and youth. The pathways that underlie these links include chronic hypothalamic activation due to stress and social deprivation from various positive interactions that accompany family meals and food preparation at home (Porter & Gallagher, 2006; Elgar et al., 2013). Food insecurity affects youth in schools as well. A study of low-income households in Quebec found that parents will go to great lengths to ensure their children have “fashion foods” (p. 126) in their lunch boxes to protect the “social image of their children at school” (p. 126) (Hamelin et al., 2002). Food insecurity is therefore socially disruptive to youth well-being during a formative stage of the life course, and we saw no evidence to suggest that adults’ efforts to shield youth from food insecurity might improve psychological outcomes.
Conclusion
Evidence on the family dynamics of food insecurity can support policy interventions that support mental health and well-being in vulnerable groups. This study found that shielding children and youth from experiencing food insecurity is associated with better psychological outcomes in adults and youth; however, further analysis is needed to isolate the costs and benefits of this protective behaviour from the severity of food insecurity. Such research is increasingly relevant to public health policy in Canada and globally as current trends in food insecurity reveal growing disparities in this foundational social determinant of health.
Contributions to knowledge
What does this study add to existing knowledge?
Food insecurity is associated with poor mental health and well-being in youth and adults.
In food-insecure households, shielding children is associated with lower risks of mood disorder in youth and various mental health problems in adults.
What are the key implications for public health interventions, practice, or policy?
Food insecurity is a robust social determinant of mental health and is distinct from income poverty.
Adults who can shield children from experiencing food insecurity may experience better mental health and well-being than adults who cannot.
Providing support and resources to families who experience food insecurity, including mental health screening and interventions, is important to more effective food policy.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
All the authors contributed to the study conception and design. Literature review and data cleaning and analysis were performed by MO and FE. The first draft of the manuscript was written by MO. MADS assisted with data analysis and editing of the manuscript. All the authors commented on previous versions of the manuscript and read and approved the final manuscript.
Funding
Supported by grants from the Canadian Institutes of Health Research (PJT-162463, PJT-165971), Social Sciences and Humanities Research Council (435-2019-1083), and Canada Research Chairs Program.
Availability of data and material
Public Use Microdata Files for the Canadian Community Health Survey are publicly available through the Data Liberation Initiative of Statistics Canada.
Code availability
Available upon request.
Declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
The project received ethics clearance by the Institutional Research Board, Faculty of Medicine, McGill University.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ashiabi, G. S., & O’Neal, K. K. (2007). Food insecurity and adjustment problems in a national sample of adolescents. Journal of Children and Poverty,13(2), 111–132. 10.1080/10796120701520226
- Bernard, R., Hammarlund, R., Bouquet, M., et al. (2018). Parent and child reports of food insecurity and mental health: Divergent perspectives. The Ochsner Journal,18(4), 318–325. 10.31486/toj.18.0037 [DOI] [PMC free article] [PubMed]
- Bickel, G., Nord, M., Price, C., et al. (2000). Guide to measuring household food security. United States Department of Agriculture. https://naldc.nal.usda.gov/download/38369/PDF. Accessed July 29, 2021.
- Bøe, T., Øverland, S., Lundervold, A. J., & Hysing, M. (2012). Socioeconomic status and children’s mental health: Results from the Bergen Child Study. Social Psychiatry and Psychiatric Epidemiology,47(10), 1557–1566. 10.1007/s00127-011-0462-9 [DOI] [PubMed]
- Brisebois, F., & Thivierge, S. (2001). The weighting strategy of the Canadian Community Health Survey. American Statistical Association.
- Chiu, M., Amartey, A., Wang, X., & Kurdyak, P. (2018). Ethnic differences in mental health status and service utilization: A population-based study in Ontario, Canada. Canadian Journal of Psychiatry,63(7), 481–491. 10.1177/0706743717741061 [DOI] [PMC free article] [PubMed]
- Coleman-Jensen, A., McFall, W., & Nord, M. (2013). Food insecurity in households with children: Prevalence, severity, and household characteristics, 2010-11, EIB-113, U.S. Department of Agriculture, Economic Research Service. https://www.ers.usda.gov/webdocs/publications/43763/37672_eib-113.pdf.
- Dhunna, S., & Tarasuk, V. (2021). Black–white racial disparities in household food insecurity from 2005 to 2014, Canada. Canadian Journal of Public Health,112, 888–902. 10.17269/s41997-021-00539-y. [DOI] [PMC free article] [PubMed]
- Elgar, F. J., Craig, W., & Trites, S. J. (2013). Family dinners, communication, and mental health in Canadian adolescents. Journal of Adolescent Health,52(4), 433–438. 10.1016/j.jadohealth.2012.07.012 [DOI] [PubMed]
- Firth, J., Gangwisch, J. E., Borisini, A., et al. (2020). Food and mood: How do diet and nutrition affect mental wellbeing? BMJ,369, m2382. 10.1136/bmj.m2382 [DOI] [PMC free article] [PubMed]
- Food and Agricultural Organisation. (2020). The state of food security and nutrition in the world 2019: Transforming food systems for affordable healthy diets. Safeguarding against economic slowdowns and downturns. FAO, Rome. 10.4060/ca9692en. Accessed 20 Nov 2021. [DOI]
- Fram, M. S., Frongillo, E. A., Jones, S. J., et al. (2011). Children are aware of food insecurity and take responsibility for managing food resources. Journal of Nutrition,141(6), 1114–1119. 10.3945/jn.110.135988 [DOI] [PubMed]
- Hamelin, A. M., Beaudry, M., & Habicht, J. P. (2002). Characterization of household food insecurity in Québec: Food and feelings. Social Science and Medicine,54(1), 119–132. 10.1016/s0277-9536(01)00013-2 [DOI] [PubMed]
- Health Canada. (n.d.). Determining food security status. https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/household-food-insecurity-canada-overview/determining-food-security-status-food-nutrition-surveillance-health-canada.html. Accessed July 29, 2021.
- Jenkins, T. A., Nguyen, J. C., Polglaze, K. E., & Bertrand, P. P. (2016). Influence of tryptophan and serotonin on mood and cognition with a possible role of the gut-brain axis. Nutrients,8(1), 56. 10.3390/nu8010056 [DOI] [PMC free article] [PubMed]
- Kirkpatrick SI, Dodd KW, Parsons R, et al. Household food insecurity is a stronger marker of adequacy of nutrient intakes among Canadian compared to American youth and adults. Journal of Nutrition. 2015;145:1596–1603. doi: 10.3945/jn.114.208579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan, S., Oatley, H., Racine, N., et al. (2018). A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. Journal of the American Academy of Child and Adolescent Psychiatry,57(9), 645–657.e8. 10.1016/j.jaac.2018.06.012 [DOI] [PubMed]
- Martin MS, Maddocks E, Chen Y, Gilman SE, Colman I. Food insecurity and mental illness: Disproportionate impacts in the context of perceived stress and social isolation. Public Health. 2016;132:86–91. doi: 10.1016/j.puhe.2015.11.014. [DOI] [PubMed] [Google Scholar]
- Maynard, M. S., Perlman, C. M., & Kirkpatrick, S. I. (2019). Food insecurity and perceived anxiety among adolescents: An analysis of data from the 2009–2010 National Health and Nutrition Examination Survey (NHANES). Journal of Hunger & Environmental Nutrition,14, 339–351. 10.1080/19320248.2017.1393363
- McLaughlin, K. A., Green, J. G., Alegría, M., et al. (2012). Food insecurity and mental disorders in a national sample of U.S. adolescents. Journal of the American Academy of Child and Adolescent Psychiatry,51(12), 1293–1303. 10.1016/j.jaac.2012.09.009 [DOI] [PMC free article] [PubMed]
- Melchior, M., Chastang, J. F., Falissard, B., et al. (2012). Food insecurity and children’s mental health: A prospective birth cohort study. PLoS ONE,7(12), e52615. 10.1371/journal.pone.0052615 [DOI] [PMC free article] [PubMed]
- Men, F., Elgar, F. J., & Tarasuk, V. (2021). Food insecurity is associated with mental health problems among Canadian youth. Journal of Epidemiology and Community Health, 75(8), 741–748. 10.1136/jech-2020-216149 [DOI] [PubMed]
- Nagata, J. M., Palar, K., Gooding, H. C., et al. (2019). Food insecurity is associated with poorer mental health and sleep outcomes in young adults. Journal of Adolescent Health,65(6), 805–811. 10.1016/j.jadohealth.2019.08.010 [DOI] [PMC free article] [PubMed]
- O’Donnell, S., Vanderloo, S., McRae, L., et al. (2016). Comparison of the estimated prevalence of mood and/or anxiety disorders in Canada between self-report and administrative data. Epidemiology and Psychiatric Sciences,25, 360–369. 10.1017/S2045796015000463 [DOI] [PMC free article] [PubMed]
- Owen, L., & Corfe, B. (2017). The role of diet and nutrition on mental health and wellbeing. The Proceedings of the Nutrition Society,76, 425–426. 10.1017/S0029665117001057 [DOI] [PubMed]
- Porter, R. J., & Gallagher, P. (2006). Abnormalities of the HPA axis in affective disorders: Clinical subtypes and potential treatments. Acta Neuropsychiatrica,18(5), 193–209. 10.1111/j.1601-5215.2006.00152.x [DOI] [PubMed]
- Pryor, L., Lioret, S., van der Waerden, J., Fombonne, É., Falissard, B., & Melchior, M. (2016). Food insecurity and mental health problems among a community sample of young adults. Social Psychiatry and Psychiatric Epidemiology,51(8), 1073–1081. 10.1007/s00127-016-1249-9 [DOI] [PubMed]
- Sentenac, M., Gariepy, G., McKinnon, B., & Elgar, F. J. (2016). Hunger and overweight in Canadian school-aged children: A propensity score matching analysis. Canadian Journal of Public Health,107(4–5), e447–e452. 10.17269/cjph.107.5526 [DOI] [PMC free article] [PubMed]
- StataCorp. (2011). Multiple-imputation reference manual. Stata Press.
- Statistics Canada. (n.d.) Canadian Community Health Survey - Annual Component (CCHS). Available online at: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=1314175. Accessed 10 Nov 2021.
- Tarasuk, V., Li, N., Dachner, N., & Mitchell, A. (2019). Household food insecurity in Ontario during a period of poverty reduction, 2005–2014. Canadian Public Policy,45(1), 93–104. 10.3138/cpp.2018-054
- Tarasuk, V., & Mitchell, A. (2020). Household food insecurity in Canada, 2017-18. Toronto ON. https://proof.utoronto.ca/resources/proof-annual-reports/household-food-insecurity-in-canada-2017-2018/. Accessed 20 Nov 2021.
- Vanzella-Yang, A, & Veenstra, G. (2021). Socio-economic resources and adult mental health in Canada: Controlling for time-invariant confounders and investigating causal directionality. Canadian Journal of Public Health, 112, 1042–1049. 10.17269/s41997-021-00547-y [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Public Use Microdata Files for the Canadian Community Health Survey are publicly available through the Data Liberation Initiative of Statistics Canada.
Available upon request.