Abstract
Adoptive transfer of cytomegalovirus (CMV)-specific cytotoxic T lymphocytes (CMV-CTLs) from original transplant donors or third-party donors was effective for the treatment of CMV infection after allogenic stem cell transplantation (allo-SCT), but the antiviral activity of CMV-CTL types has not been compared. To determine whether third-party CMV-CTLs provide comparable long-term antiviral efficacy to transplant donor CMV-CTLs, we first compared the antiviral abilities of transplant donors and third-party CMV-CTLs for treatment of CMV infection in two mouse models, compared the in vivo recovery of CMV-specific immunity, and analyzed the underlying mechanisms driving sustained antiviral immunity. The results showed that both donor and third-party CMV-CTLs effectively combated systemic CMV infection by reducing CMV pathology and tumor burden 28 days postinfusion. The in vivo recovery of CMV-specific immunity after CMV-CTL infusion was comparable in both groups. A detailed analysis of the source of recovered CMV-CTLs showed the proliferation and expansion of graft-derived endogenous CMV-CTLs in both groups. Our clinical study, which enrolled 31 patients who received third-party CMV-CTLs and 62 matched pairs of individuals who received transplant donor CMV-CTLs for refractory CMV infection, further showed that adoptive therapy with donor or third-party CMV-CTLs had comparable clinical responses without significant therapy-related toxicity. We observed strong expansion of CD8+ tetramer+ T cells and proliferation of recipient endogenous CMV-CTLs after CMV-CTL infusion, which were associated with a reduced or cleared viral load. Our data confirmed that adoptive therapy with third-party or transplant donor CMV-CTLs triggered comparable antiviral responses to CMV infection that might be mediated by restoration of endogenous CMV-specific immunity.
Keywords: Allogeneic stem cell transplantation, CMV-specific cytotoxic T lymphocytes, Transplant donor, Third party donor, Immunotherapy
Subject terms: Bone marrow transplantation, Infection
Introduction
Allogeneic stem cell transplantation (allo-SCT) is a potentially curative treatment for patients with high-risk hematologic malignancies [1–3]. However, due to profound and prolonged T cell deficiency following conditions such as graft-versus-host disease (GVHD) and immunosuppression early after allo-SCT, viral illness, especially cytomegalovirus (CMV) infection, remains a major and potentially life-threatening complication following allo-SCT [4–7].
Adoptive therapy with CMV-specific cytotoxic T lymphocytes (CMV-CTLs) has been proposed as a feasible treatment option for CMV infection [8, 9]. Riddell et al. first established a proof-of-concept for adoptive transfer of donor-derived CMV-CTLs for treatment of CMV infection in allo-SCT recipients [10, 11]. Subsequent studies have confirmed the safety and efficacy of donor-derived CMV-CTLs prophylactically or therapeutically administered for CMV infection, with the efficacy reportedly ranging from 70–90% [12–19]. Unfortunately, the need to generate specific T cell lines for each patient makes this approach impractical for widespread or urgent use, and it is not an option when the donor lacks viral immunity.
HLA partially matched related or unrelated donors can serve as third-party donors and represent an appropriate alternative T cell source [20, 21]. As reported by Leen et al. [22], banked third-party CMV-CTLs could be used to safely and rapidly treat severe or intractable viral infections after allo-SCT, with a cumulative rate of complete or partial response at 6 weeks postinfusion of 73.9%. In a more recent study, Withers et al. [23], reported that third-party CMV-CTLs showed prolonged benefits, with a cumulative incidence of overall response at 12 months of 93%. As the in vivo expansion and persistence of transfused third-party CMV-CTLs have been lower and of shorter duration than those of donor CMV-CTLs [12], it is unclear whether third-party CMV-CTLs provide comparable long-term antiviral efficacy to transplant donor CMV-CTLs. In fact, the safety and efficacy of these two kinds of CMV-CTLs still need to be established and compared.
The reconstitution of CMV-CTLs is essential for the control of CMV reactivation [24–28]. In murine models, it has been well established that CMV-CTLs evolved to eliminate active infection and prevent recurrent viral infection [29]. Subsequently, data from clinical patients demonstrated that there was a correlation between CMV-CTL recovery and the control of CMV infection and disease, which showed that CMV-CTL counts above 10 × 106/L were associated with protection from CMV disease [30]. Further direct evidence for the critical role of CMV-CTL recovery in protective immunity to CMV was obtained from the transfer of CMV-CTLs as an adoptive therapy. As suggested by preclinical research in murine models, adoptive CMV-CTL transfer accelerates CMV-specific immune reconstitution, resulting in diminished CMV-mediated histopathology [31, 32]. In clinical studies, patients who received donor or third-party CMV-CTL transfer were protected from CMV-associated complications due to the effective reconstitution of cellular immunity against CMV, suggesting the critical role of CMV-specific immune reconstitution as an indicator of CMV control [23, 33–35].
The mechanisms driving sustained antiviral immunity induced by the donor or third-party CMV-CTLs remain largely unknown. In our previous study, we demonstrated that adoptive transfer of donor CMV-CTLs may have restored long-term CMV-specific immunity by stimulating the recovery of graft-derived endogenous T cells but not by expanding transferred cells [35]. Whether this recovery of antiviral immunity after third-party CMV-CTL infusion as a result of adoptively infused T cells, recipient endogenous immune recovery, or both remains to be established and compared with donor CMV-CTLs.
In the present study, (i) we explored the antiviral ability of donor and third-party CMV-CTLs for treatment of CMV infection in two mouse models of CMV infection, compared the in vivo recovery of CMV-specific immunity, and analyzed the underlying mechanisms driving the sustained antiviral immunity induced by these two types of CMV-CTL therapy. (ii) We also retrospectively compared the therapeutic application of donor CMV-CTLs and third-party CMV-CTLs in patients with refractory CMV infection after allo-SCT. We tracked the infused CMV-CTL populations and compared the recovery of virus-specific immunity in patients.
Materials and methods
CMV-CTL generation
Peripheral blood mononuclear cells (PBMCs) from healthy transplant donors or third-party donors were cocultured with irradiated monocyte-derived dendritic cells (moDCs) pulsed with HLA-A*0201-, HLA-A*2402-, and HLA-A*1101-restricted CMV pp65 peptide or with a pool of 138 synthetic pentadecapeptides (15-mers) covering CMV pp65, as previously described [34]. We expanded cells with weekly restimulation with pp65 peptide in the presence of recombinant human interleukin (rhIL)-2 for up to 14–21 days. The HLA-A-restricted peptide was used from 2012 to 2015, during which time the study was limited to donors who were HLA-A*0201-, HLA-A*2402-, and HLA-A*1101-positive. From 2015 onward, 138 overlapping peptides were used to allow for the recruitment of donor-recipient pairs with all HLA types. Third-party CMV-CTLs were selected on the basis of HLA matching at a minimum of 2/6 recipient HLA alleles. A total of 25 distinct CMV-CTL lines were used. The HLA restriction of the CMV-CTLs was at two alleles (n = 5), at three alleles (n = 20), at four alleles (n = 5) and at five alleles (n = 1). The detailed HLA allele information of the third-party CMV-CTLs is shown in Table S1.
CMV infection and tumor infiltration humanized mouse models
A humanized mouse model (Fig. 1A, D) was established as previously described [35]. NOD-Prkdcscid IL2rgnull (NPG) mice (6 to 8 weeks old) were sublethally irradiated (1.5 Gy) and intravenously injected with 1 × 106 granulocyte colony-stimulating factor (G-CSF)-mobilized peripheral blood stem cells (PBSCs) obtained from CMV-seropositive donors. A total of 2 weeks later, after the reconstituted human CD45 cells accounted for more than 2% of the total lymphocytes (which is a sign of successful humanization), mice in the CMV infection mouse model (Fig. 1A) received 1 × 106 AD169-infected MRC5 cells (MRC-5 cells were cultured in 25 T flasks until 95% confluence. CMV AD169 was added to MRC-5 cells at MOI 3. The infected cells were incubated until 95% of the cells showed a cytopathic effect). Mice in the tumor infiltration mouse model (Fig. 1D) received 8 × 104 RAJI-HLA-A*0201-pp65-luciferase cells (kindly provided by Professor Lin Xin from Tsinghua University).
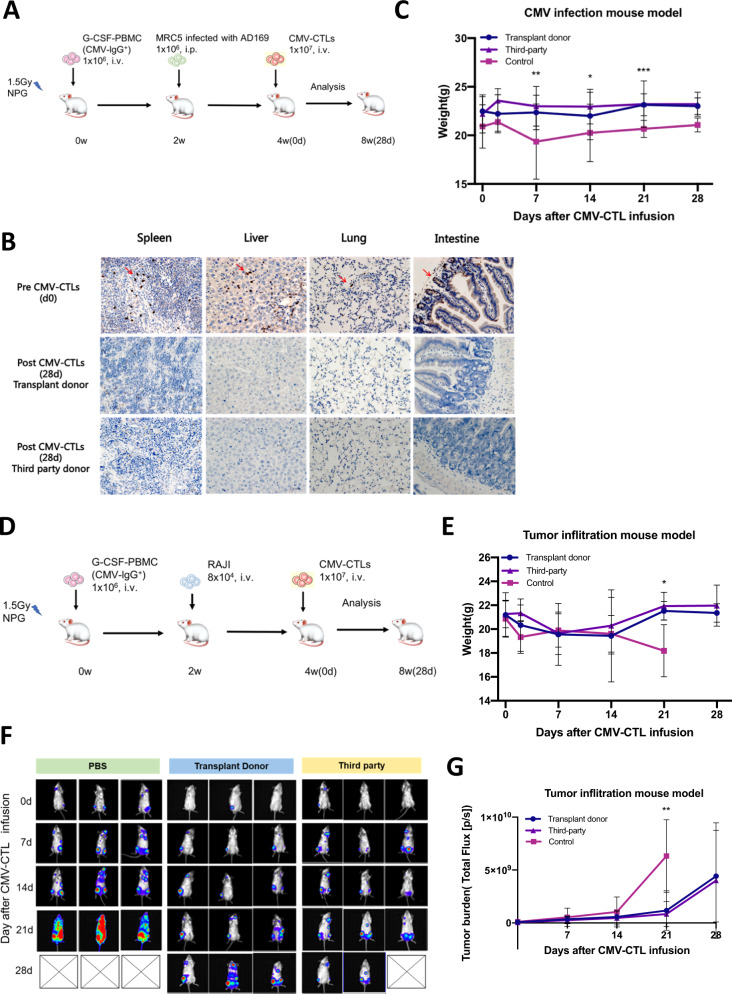
Fig. 1.
Humanized CMV infection and tumor infiltration NPG mouse models and in vivo anti-CMV efficacy. A The humanized CMV infection NPG mouse model and experimental strategy. B CMV pathology in the spleen, liver, lung, and intestine of mice pre-CMV-CTL infusion and 28 days post-donor and -third-party CMV-CTL infusion. Both donor and third-party CMV-CTLs effectively combated systemic CMV infection by diminishing CMV pathology in target organs within 28 days after CMV-CTL infusion. C Mouse weight change post-CMV-CTL infusion in the CMV infection NPG mouse model. D The humanized tumor infiltration NPG mouse model and experimental strategy. E Mouse weight change post-CMV-CTL infusion in the tumor infiltration NPG mouse model. F Photon emission and (G) tumor burden (total flux) change pre- and post-CMV-CTL infusion in the tumor infiltration NPG mouse model. No fewer than three mice were evaluated at each time point. Transplant donor and third-party CMV-CTL group vs. control group, *P < 0.05, **P < 0.01, ***P < 0.001
In CMV-infected mice, mice were sacrificed weekly, and the spleen, liver, lung and intestine were harvested for CMV DNA evaluation by in situ hybridization using a CMV probe (Leica Biosystems). In tumor infiltration mice, the mice were intraperitoneally injected with D-luciferin (15 ng/ml) and imaged with a Lumia II system at the indicated time points.
CMV-CTL transfusion into humanized mice
To examine the antiviral effect of donor and third-party CMV-CTLs against CMV in vivo and to monitor T cell proliferation and survival, we labeled CMV-CTLs with carboxyfluorescein succinimidyl ester (CFSE) and infused CMV-CTLs into both CMV infection and tumor infiltration humanized mice. Briefly, mice in the CMV-CTL group received 1 × 107 CFSE-labeled CMV-CTLs once CMV infection was diagnosed (approximately 2 weeks after MRC5 or tumor cell injection) based on the positivity of CMV DNA in harvested organs in CMV-infected mice or progressive bioluminescence imaging in tumor infiltration mice. In the control group, mice received equivalent volumes of PBS without T cells. The mice in the donor CMV-CTL, third-party CMV-CTL, and control groups were evaluated for recovery of CMV-CTLs at 0, 2, 4, 7, 14, and 28 days after adoptive therapy. The expansion of infused CFSE-positive CMV-CTLs and the recovery of endogenous CFSE-negative CMV-CTLs were analyzed.
Patients and study design
From 2012 to 2019, a total of 177 patients who received CMV-CTLs for refractory CMV infection after allo-SCT were enrolled. We collected data from 31 patients who received third-party CMV-CTLs and selected matched pairs of individuals (62 patients total) who received donor CMV-CTLs from contemporaneous subsets and who were closely matched with the third-party CMV-CTL group based on 1:2 case-control matching (Supplementary Fig. S1). The main endpoint of our study was the control of CMV-DNA viremia. Written informed consent was obtained from all patients and donors, and this study was approved by the ethics committee of Peking University People’s Hospital and was performed in accordance with the Declaration of Helsinki.
Transplant protocol and antiviral treatment
Allogeneic transplant protocols, including conditioning, mobilization, collection of stem cells, and GVHD prophylaxis, were performed as described previously [1, 36]. Briefly, pretransplant conditioning consisted of cytarabine (4 g/m2/day, days −10 to −9), busulfan (3.2 mg/kg/day intravenously, days −8 to −6), cyclophosphamide (1.8 g/m2/day, days −5 to −4), semustine (250 mg/m2, day −3) and rabbit antithymocyte globulin (thymoglobulin; Imtix Sangstat, Lyon, France; 2.5 mg/kg/day, days −5 to −2). All transplant recipients received cyclosporine A (CsA), mycophenolate mofetil (MMF), and short-term methotrexate for GVHD prophylaxis. Patients who developed acute GVHD received 1 to 2 mg/kg/d prednisolone equivalents and resumption of full-dose CsA administration. Nonresponders received second-line immunosuppressive therapy, such as tacrolimus (FK506), MMF, and CD25 monoclonal antibody (Novartis, Basel, Switzerland).
CMV and EBV infection was monitored based on plasma DNA levels using a real-time PCR kit twice weekly for up to 3 months after the first infusion, and monitoring was continued thereafter if clinically indicated. Patients began therapy with ganciclovir (5 mg/kg intravenously, twice daily) when CMV infection was diagnosed (CMV DNA ≥ 1 × 103 copies/ml). Continued treatment consisted of a combination of foscarnet (60 mg/kg intravenously, twice daily) if patients were not complicated with renal function injury and immunoglobulin when CMV became refractory.
Definitions
CMV infection was diagnosed according to previously published criteria: CMV DNA ≥ 1 × 103 copies/ml in peripheral blood by CMV PCR assay [5, 34]. The definition of persistent viral infection was positive viral DNA for over 4 weeks despite treatment with a full dose of antiviral therapy [33]. Complete remission (CR) was specified by viremia clearance (negative CMV PCR) on two consecutive study dates [21].
TCR CDR3 sequencing
T cell receptor (TCR) CDR3 spectratyping was performed on the infused CMV-CTLs and CMV-CTLs isolated from patients’ PBMCs pre- and post-CMV-CTL infusion. RNA was extracted from tetramer-positive CMV-CTLs and converted to complementary DNA (cDNA). The cDNA was analyzed in parallel with clonotypic PCR using a modified switch mechanism at the 5′-end of RNA templates (SMART)-based method, and amplicons were subsequently sequenced to confirm CDR3 identity.
Statistical analyses
The chi-squared test or Fisher’s exact test was used for categorical variables. Two-tailed Student’s t test was used for normally distributed continuous variables, whereas the Mann–Whitney U test was used for skewed continuous variables. The overall survival (OS) rates were estimated with the Kaplan–Meier method. Cumulative incidence curves were used for treatment-related mortality (TRM) and CMV CR rates in a competing risk setting, with death considered a competing risk. P values ≤ 0.05 were considered statistically significant.
Results
Both donor and third-party CMV-CTLs effectively combated systemic CMV infection in humanized mice
To examine the in vivo activity of donor and third-party CMV-CTLs, we used two severe combined immunodeficient (SCID) mouse xenograft models. The CMV infection mouse model was infected with CMV by injecting AD169-infected MRC5 cells (Fig. 1A), and the tumor infiltration mouse model was generated by injecting RAJI-HLA-A*0201-pp65-luciferase cells (Fig. 1D).
In the CMV infection mouse model, all mice had CMV recurrence in human hematopoietic cells that had migrated to the tissue before CMV-CTL transfusion (Fig. 1B). As we expected, both donor and third-party CMV-CTLs effectively combated systemic CMV infection by diminishing CMV pathology in target organs (spleen, liver, lung, and intestine) within 28 days after infusion, in contrast to the mice in the control group, which remained positive for CMV DNA (Fig. 1B). Mice that received donor or third-party CMV-CTLs exhibited significantly higher weights than control mice, while mice that received donor or third-party CMV-CTLs had comparable weights at any indicated time point, which in some way might indicate the comparable antiviral ability of donor and third-party CMV-CTLs (Fig. 1C).
In the tumor infiltration mouse model, in contrast to control mice, in which photon emission and tumor size were increased, we observed a reduction in bioluminescence over 2 weeks in mice treated with donor or third-party CMV-CTLs (Fig. 1F), indicating that tumor growth was inhibited (Fig. 1F). Importantly, we observed that donor and third-party CMV-CTLs had comparable antitumor activity, as measured by tumor burden and mouse weight (Fig. 1E, G).
Donor and third-party CMV-CTLs had an equal ability to promote CMV-specific immunity in humanized mice
CMV-CTL quantities were determined pre-CMV-CTL transfusion and at the indicated time points post-CMV-CTL transfusion in peripheral blood (PB), bone marrow (BM), and organs. We found that both donor and third-party CMV-CTLs not only persisted in PB but also migrated to the virus-infected or tumor-infiltrated organs (liver, spleen, and lung) and persisted in the BM and those organs for at least 28 days after the infusion (Fig. 2D and Supplementary S2).
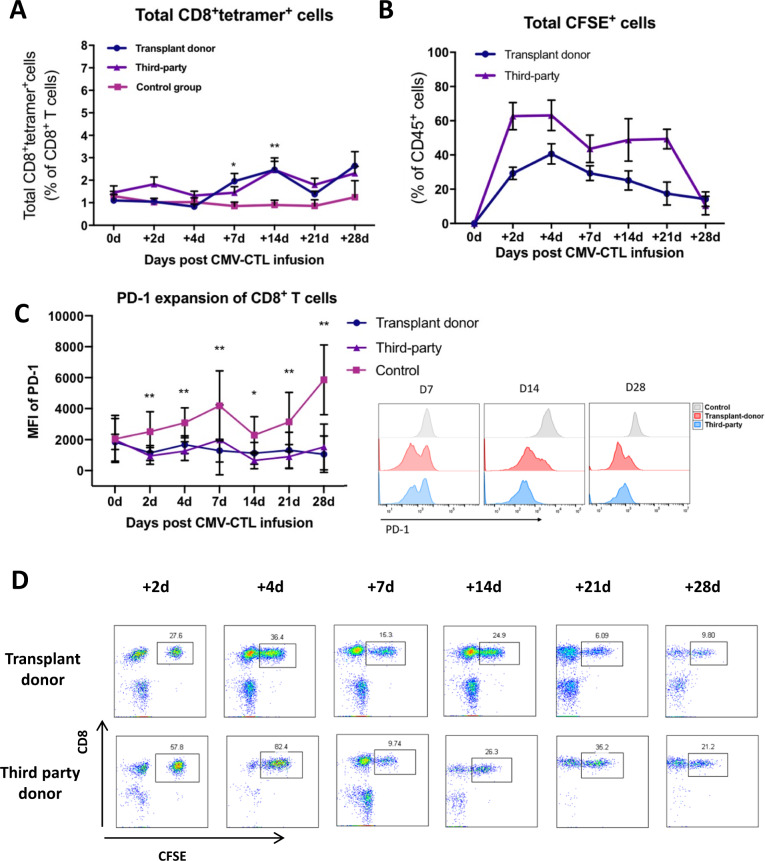
Fig. 2.
In vivo recovery of CMV-specific immunity in humanized mice after CMV-CTL therapy. A Recovery of CMV-CTLs in donor and third-party CMV-CTL-infused mice and control mice. B Persistence and expansion of CFSE+ CD8+ T cells (adoptively transferred CMV-CTLs) in PB after CMV-CTL infusion. C Change in PD-1 expression of CD8+ T cells in donor and third-party CMV-CTL-infused mice and control mice. D CFSE+ CD8+ T cells (adoptively transferred CMV-CTLs) in the PB of transplant donor and third-party CMV-CTL-infused mice from Day 2 to Day 28. No fewer than five mice were evaluated at each time point. Transplant donor and third-party CMV-CTL group vs. control group, *P < 0.05, **P < 0.01
Similar to our previous data, the proportion of CMV-CTLs in the donor CMV-CTL group increased after infusion, with a significant difference in the proportion at 7 days and 14 days compared with that in the control group (Fig. 2A). The same trend was also observed in the third-party CMV-CTL group (Fig. 2A). Importantly, our results showed that there was no significant difference between the donor and third-party CMV-CTL groups, indicating that these two types of CMV-CTLs had an equal ability to promote CMV-specific immunity (Fig. 2A).
Moreover, the mean fluorescence intensity of PD-1 on CD8+ T cells was significantly lower in the donor CMV-CTL group than in the control group and was comparable to that in the third-party CMV-CTL group (Fig. 2C). Consistent with our previous finding [34], both donor and third-party CMV-CTL transfer might result in an equivalent reversal of T cell impairment caused by CMV infection.
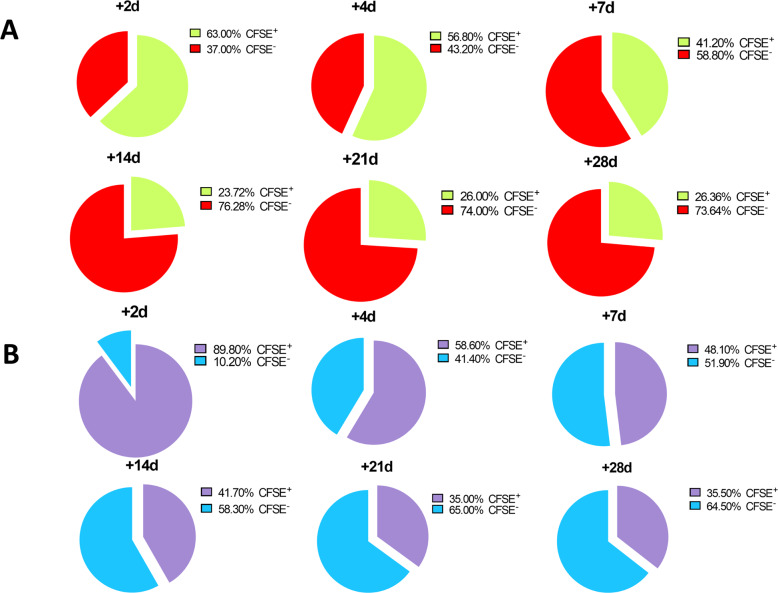
Donor and third-party CMV-CTL adoptive transfer stimulated the recovery of endogenous CMV-specific immunity
We also performed a detailed analysis of the source of the recovered CMV-CTLs. We found that the initial phase, within the first 4 days following the infusion, was characterized by the general activation and proliferation of adoptively transferred T cells in both donor and third-party groups. After 4 days, the proportion of total CFSE-positive cells began to slowly decrease (Fig. 2B). In CD8+tetramer+ cells, there was a reduction in the transferred CFSE+ CMV-CTLs and a preferential proliferation and expansion of graft-derived endogenous CFSE-negative CMV-CTLs in both the donor and third-party groups (Fig. 3). Our findings suggested that transferred donor or third-party CMV-CTLs transiently increased in vivo and performed long-term antiviral functions mainly by stimulating the recovery of endogenous CMV-specific immunity.
Fig. 3.
Source of the recovered CMV-CTLs in donor and third-party CMV-CTL-infused mice. CFSE+ CMV-CTLs indicate adoptively transferred CMV-CTLs, and CFSE- CMV-CTLs indicate endogenously recovered CMV-CTLs from engrafted stem cells. A Transplant donor CMV-CTL infusion group. B Third-party CMV-CTL infusion group
Donor and third-party CMV-CTLs had comparable antiviral ability in patients
The patient characteristics are summarized in Table 1. Sixty-two patients in the donor group received a total of 77 infusions, and 31 patients in the third-party group received a total of 64 infusions. In general, no immediate infusion-related side effects, including cytokine release syndrome, were observed in the donor or third-party group. No patients developed grade 3 to 4 acute GVHD after CMV-CTL infusion, although seven patients in the donor group and three patients in the third-party group developed grade 1 to 2 acute GVHD within 2 weeks after CMV-CTL transfer.
Table 1.
Patients’ characteristics
| Characteristics | Transplant donor CMV-CTLs (n = 62) | Third-party CMV-CTLs (n = 31) | P value |
|---|---|---|---|
| Follow-up (median, d) | 1000 (146–2210) | 910 (154–2415) | 0.65 |
| Age (median, y, range) | 31.50 (7–59) | 37 (7–55) | 0.19 |
| Sex (M/F) | 32/30 | 21/10 | 0.18 |
| Disease type, n (%) | 0.89 | ||
| AML | 25 (40.32) | 13 (41.94) | |
| ALL | 22 (35.48) | 9 (29.03) | |
| MDS | 8 (12.90) | 4 (12.90) | |
| Others | 7 (11.29) | 5 (16.13) | |
| Transplant type (n, %) | <0.01 | ||
| HLA-matched SCT | 2 (3.22) | 2 (6.45) | |
| HLA-mismatched SCT | 60 (96.78) | 22 (70.97) | |
| Unrelated SCT | 0 (0.00) | 7 (22.58) | |
| Maximal acute GVHD before infusions (n, %) | 0.82 | ||
| 0-I | 37 (59.67) | 16 (51.61) | |
| II-IV | 25 (40.33) | 12 (38.71) | |
| CMV serological status of transplant donor (n, %) | <0.01 | ||
| Positive | 62 (100.00) | 18 (58.06) | |
| Negative | 0 (0.00) | 8 (25.80) | |
| Unkonwn | 0 (0.00) | 5 (16.12) | |
| CMV reactivation day post SCT (d, median) | 33 (17–49) | 29 (15–67) | 0.26 |
| CMV-CTLs infusion day post SCT (d, median) | 71 (51–158) | 59 (44–198) | 0.09 |
| CMV persistent time before infusion (d, median) | 26 (15–119) | 20 (15–134) | 0.23 |
| Median CMV titer before infusion (103/ml) | 7.00 (1.60–103.20) | 4.20 (1.10–77.00) | 0.08 |
| Peak CMV titer before infusion (103/ml) | 36.60 (4.70–1030) | 22.60 (2.70–680) | 0.20 |
| CMV disease before infusion (n, %) | 10 (16.10) | 3 (9.70) | 0.40 |
Abbreviations: M Male; F Female; AML Acute myeloid leukemia; ALL Acute lymphoblastic leukemia; MDS Myelodysplastic syndrome; SCT Stem cell transplantation; GVHD graft-versus-host disease; CMV Cytomegalovirus; CMV-CTLs, Cytomegalovirus-specific cytotoxic T lymphocytes
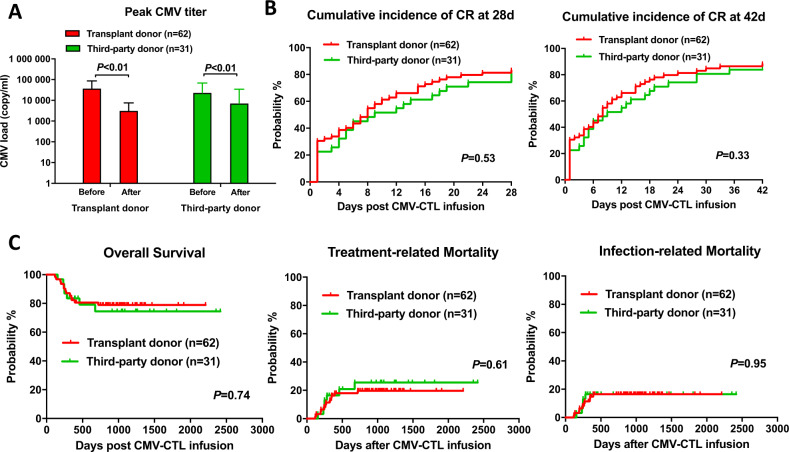
As shown in Fig. 4A, the CMV peak titer significantly decreased from 3.7 (range, 4.7–103) × 10E4 to 3.1 (range, 0–822) × 10E3 copies/ml in the donor group and from 2.3 (range, 2.7–680) × 10E4 to 7.0 (range, 0–780) × 10E3 copies/ml in the third-party group. The cumulative CR rates 4 weeks after the first CMV-CTL infusion were 83.1% (95% CI 66.7%–94.5%) in the donor group and 80.6% (95% CI 73.7%–92.5%) in the third-party group (Fig. 4B). The cumulative CR rates 6 weeks after the first CMV-CTL infusion were 88.1% (95% CI 79.8%–96.3%) in the donor group and 83.9% (95% CI 71.0%–96.8%) in the third-party group. The CR rates at the 4th week (P = 0.53) and 6th week (P = 0.33) were comparable in the donor and third-party groups (Fig. 4B).
Fig. 4.
Virologic response and clinical outcomes in patients who received donor CMV-CTL and third-party CMV-CTL therapy. A Peak CMV titer change after donor and third-party CMV-CTL therapy. B Cumulative incidence of CR at 28 days and 42 days after donor and third-party CMV-CTL therapy. C Overall survival, treatment-related mortality, and infection-related mortality after donor and third-party CMV-CTL therapy. A total of 31 patients were enrolled in the third-party CMV-CTL group and matched pairs of patients (62 total) were enrolled in the donor CMV-CTL group
We further analyzed the effects of HLA allele matching between transferred CMV-CTLs and recipients on clinical outcomes in the third-party group. We found that patients with 4, 3, and ≤ 2 mismatched HLA alleles had no difference in acute GVHD incidence (P = 0.401) or CMV CR rate (P = 0.983 for the CR rate at the 4th week, P = 0.963 for the CR rate at the 6th week).
A total of 12 deaths occurred during the follow-up period in the donor CMV-CTL group; 11 patients died from treatment-related events, and four patients had uncontrolled CMV at the time of death (Table 2). In the third-party CMV-CTL group, a total of seven deaths occurred; all patients died from treatment-related events, and two patients had an uncontrolled CMV infection at the time of death. The OS at 5 years was 80.5% (95% CI 70.7%–90.3%) in the donor group and 74.5% (95% CI 57.8%–91.2%) in the third-party group, which was comparable (P = 0.74) (Fig. 4C). The 5 years all-cause TRM (18.1% vs. 25.5%, P = 0.61) and particular infection-related mortality (16.4% vs. 16.5%, P = 0.95) were comparable between the donor and third-party groups (Fig. 4C). These data further suggested that donor and third-party CMV-CTLs had the comparable antiviral ability, which either directly targeted CMV or indirectly targeted other infections that are known to be common with uncontrolled CMV infections.
Table 2.
Safety of CMV-CTLs infusion
| Characteristics | Transplant donor CMV-CTLs (n = 62) | Third-party CMV-CTLs (n = 31) | P value |
|---|---|---|---|
| Number of infusions (n, %) | |||
| 1 | 51 (82.30) | 13 (41.90) | <0.01 |
| 2 | 7 (11.29) | 6 (19.35) | |
| ≥3 | 4 (6.45) | 12 (38.70) | |
| Immediate infusion-related toxicities (n, %) | 2 (3.22) | 2 (6.45) | 0.60 |
| Cytokine release syndrome (n, %) | 0 (0.00) | 0 (0.00) | 1 |
| Maximal acute GVHD after infusions (n, %) | 0.81 | ||
| I-II | 7 (11.29) | 3 (9.68) | |
| III-IV | 0 (0.00) | 0 (0.00) | |
| Death | |||
| Total causes | 12 (19.35) | 7 (22.58) | 0.79 |
| Treatment-ralated events | 11 (17.74) | 7 (22.58) | 0.59 |
Abbreviations: GVHD graft-versus-host disease; CMV-CTLs Cytomegalovirus-specific cytotoxic T lymphocytes
CMV-CTL infusion promotes the in vivo recovery of CMV-specific immunity in patients
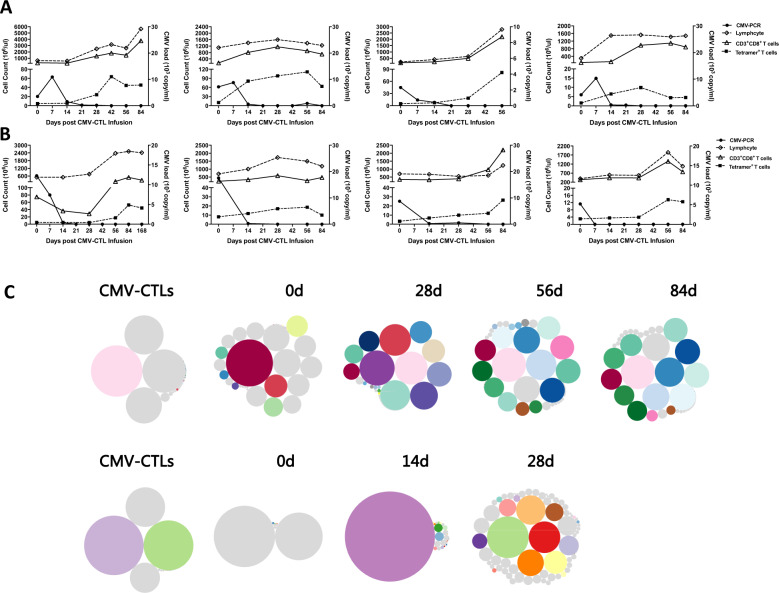
T cell response was monitored pre- and post-CMV-CTL infusion in eight patients whose samples were available. CMV-specific immunity was determined using CMV epitope-specific MHC multimers. As shown in Fig. 5A, B, we detected CMV-specific immune responses after both donor and third-party CMV-CTL infusions, and these responses were characterized by a strong expansion of CD8+ tetramer+ T cells. The proliferation of CMV-specific T cells was associated with a reduced or cleared viral load and permanent viral clearance. A total of 6/8 patients in Fig. 5 developed aucte GVHD and received 1 mg/kg/d bodyweight of prednisolone equivalents and resumption of full-dose CsA administration before CMV-CTL infusion. Although none of them received steroid treatment of > 0.5 mg/kg/d prednisolone equivalents within 1 week of CMV-CTL infusion, all of the patients received CsA during CMV-CTL infusion.
Fig. 5.
In vivo recovery of CMV-specific immunity in patients after CMV-CTL therapy. A Patients received donor CMV-CTLs, and B patients received third-party CMV-CTLs. Lines represent counts of lymphocytes, CD3+CD8+ T cells, tetramer+ T cells and CMV viral load. C TCR CDR3 spectratyping of CMV-CTLs sorted from the infusion lines and PBMC samples from two third-party CMV-CTL-infused patients. The TCR clonotype was defined based on clonotypes with the same CDR3 amino acid (CDR3aa) sequence plus the Vβ and Jβ genes. Each circle represents a clonotype. The diameter of the circle indicates the concentration of the clonotype. Clonotypes that persisted in the infused CMV-CTL lines or in PBMCs pre-CMV-CTL infusion (at Day 0) are marked as colorful and bright circles, and a single color represents one clonotype. Emerging clonotypes are uniformly marked as gray circles. Patients in Fig. 5 all received CMV-seropositive allografts
In our previous study, we confirmed that transplant donor-derived CMV-CTLs stimulated the recovery of endogenous CMV-specific immunity. Here, to test whether the expansion of CMV-specific T cells in response to third-party CMV-CTLs was driven by adoptively infused T cells, recipient endogenous T cells, or both, we performed TCR CDR3 spectratyping of CMV-CTLs sorted from the infusion lines and PBMC samples. As shown in Fig. 5C, although we found CDR3 sequences from PBMC samples identical to those from the infused CMV-CTL lines, we observed the absence of transferred CMV-CTLs among the expanding CMV-specific T cells. Interestingly, CDR3 sequences missing in the infused CMV-CTL lines were found in the PBMC pre-CMV-CTL infusion, supporting the recovery of graft-derived CMV-CTLs.
We should note that all eight patients in Fig. 5 received CMV-seropositive allografts. As we did not have samples to further compare the in vivo recovery of immunity between donor + (CMV-seropositive allografts) and donor- (CMV-seronegative allografts) subgroup recipients, we compared the CMV CR rates between donor+ and donor- recipients and found that they were comparable (P = 0.169 for the CR rate at the 4th week, P = 0.269 for the CR rate at the 6th week), which might suggest comparable immune recovery.
Discussion
In the current study, we used two humanized mouse models to compare the in vivo antiviral ability of transplant donor and third-party CMV-CTLs. Our results showed that adoptively infused donor and third-party CMV-CTLs both migrated to the virus-infected or tumor-infiltrated organs, persisted for at least 28 days, and contributed to the comparable diminishment of CMV pathology and viral burden in target organs. Moreover, our clinical data, derived from 31 patients who received third-party CMV-CTLs and 62 matched patients who received transplant donor CMV-CTLs, provided further evidence of the comparable antiviral responses induced by these two kinds of CMV-CTLs. To the best of our knowledge, this is the first report comparing the therapeutic application of donor and third-party CMV-CTLs in humanized mice and patients.
The potential advantages of third-party CMV-CTLs versus transplant donor CMV-CTLs include that they are not limited by donor viral immunity and can be banked in advance for clinical use [12]. Although experience with third-party CMV-CTLs is still limited, the results accumulated to date are quite promising, with the overall response rate reported to range from 50–93% [17, 20–22]. As reported by Tzannou et al. [20], 7 of 10 patients with persistent CMV infections or disease achieved CR after a single third-party CMV-CTL infusion, with a cumulative response rate of 100%. In a multicenter trial reported by Leen et al. [22], banked third-party CMV-CTLs were used to safely and rapidly treat severe and refractory CMV infection, with a response rate of 73.9% at 6 weeks postinfusion. In our study, we demonstrated that the cumulative CR rate at 4 weeks after CMV-CTLs infusion was 80.6% in patients who received third-party CMV-CTLs. Our study confirms the safety and efficacy of adoptive CMV-CTL therapy, as was suggested in earlier studies.
Studies directly comparing donor and third-party CMV-CTLs have not yet been reported. While single-arm trials have reported the feasibility of adoptive therapy with donor or third-party CMV-CTLs for treatment of CMV infection, due to the different strategies used to generate CMV-CTLs and the different strategies used for CMV-CTL infusion, the efficacy cannot be directly compared between different studies. One study from Neuenhahn et al. [21], assessed the safety and efficacy of the donor or third-party CMV-CTLs for the treatment of persistent CMV infections after allo-SCT. However, only 17 patients were enrolled, and the study did not focus on efficacy comparison. Our study provides the first data directly comparing donor and third-party CMV-CTL adoptive therapy for CMV infection; however, prospective clinical trials are needed to confirm our results.
The recovery of CMV-specific immunity is essential for the control of CMV. Previous studies, including both preclinical research in murine models and clinical research in patients, have demonstrated the correlation between CMV-CTL recovery and protection against CMV after adoptive CMV-CTL therapy [14, 24, 31, 32, 35, 37]. In line with a previous study, we observed the in vivo recovery of CMV-specific immunity after donor and third-party CMV-CTL infusion in humanized mouse models. Importantly, our results showed that the kinetics of the CMV-specific immune recovery were comparable in the donor and third-party CMV-CTL groups, which supported that these two kinds of CMV-CTLs generate comparable antiviral responses to treat CMV infection. For patients, we also observed a strong expansion of CD8+ tetramer+ T cells, after both donor and third-party CMV-CTL infusion; these expansions were associated with a reduced or cleared viral load, indicating the comparable antiviral ability of donor and third-party CMV-CTLs.
The mechanisms driving the sustained antiviral immunity induced by donor or third-party CMV-CTLs have rarely been reported. In the current study, with humanized mouse models, we observed that there was a reduction in the transferred CFSE+ CMV-CTLs and preferential proliferation and expansion of graft-derived endogenous CFSE-negative CMV-CTLs in both the donor and third-party groups, suggesting that graft-derived endogenous CMV-specific immunity recovered after stimulation by CMV-CTL infusion or due to the reduction in the CMV viral burden. These results were in accordance with our previous study [35], which demonstrated that the adoptive transfer of donor CMV-CTLs restored long-term CMV-specific immunity, potentially by stimulating the recovery of graft-derived endogenous T cells but not by expanding transferred cells. In patients, TCR CDR3 spectratyping analysis was performed, and we observed the absence of transferred CMV-CTLs among the expanding CMV-specific T cells, suggesting that endogenous graft-derived CMV-CTLs had recovered. These data support the hypothesis that both donor and third-party CMV-CTLs contribute to endogenous CMV-specific CMV-CTL reconstitution, suggesting that both CMV-CTLs have comparable antiviral efficacy. We should note that as T cell recovery was only analyzed in limited patients in our retrospective cohorts, prospective clinical trials with large samples monitoring immune reconstitution are needed to further confirm our results.
The strict species specificity of CMV results in the lack of a suitable animal model system for the study of human CMV [38, 39]. To mimic human CMV infection in the clinic, we established a humanized CMV infection mouse model by injecting G-CSF-mobilized PBSCs and AD169-infected MRC5 cells into NPG mice. In fact, the human hematopoietic cells that had infiltrated the organs were the ones that became infected with human CMV. With a focus on T cell-based immunotherapy, this humanized CMV infection model could be used to directly investigate CMV-mediated histopathology and evaluate in vivo CMV-specific immune reconstitution. However, as only a limited volume of PB could be collected for testing CMV-DNA by PCR in mouse plasma, mice had to be sacrificed weekly to harvest organs, and CMV DNA was hard to quantify by in situ hybridization using a CMV probe. To overcome this shortcoming, we further established a tumor infiltration mouse model by injecting NPG mice with RAJI-HLA-A*0201-pp65-luciferase cells. Although only the CMV pp65 peptide was carried by the mice, we quantitatively tested the tumor burden based on bioluminescence, which represented the viral burden in vivo. These two mouse models complemented each other, simulated clinical CMV infection to the greatest extent, and provided a suitable platform to examine viral clearance and immune reconstitution in vivo.
In conclusion, our data demonstrated that adoptive therapy with donor or third-party CMV-CTLs led to a comparable antiviral response to CMV infection by promoting the restoration of CMV-specific immunity. Both donor and third-party CMV-CTLs may stimulate the recovery of graft-derived endogenous CMV-specific immunity, which might contribute to the comparable antiviral efficacy.
Supplementary information
Acknowledgements
We thank Immunotech Biopharm Ltd. and iCELL Co. Ltd. for their aid in the organization of the clinical-grade expansion of CMV-CTLs. The authors thank every patient involved in the study and every faculty member of Peking University People’s Hospital who participated in this study. This work was supported by the National Key Research and Development Program of China (grant number 2017YFA0104500), the National Natural Science Foundation of China (grant numbers 81900137, 81530046 81930004, and 82070184), the Innovative Research Groups of the National Natural Science Foundation of China (grant number 81621001), and Peking University People’s Hospital Research and Development Funds (grant number RDY2019-34, RS2021-01).
Author contributions
HXJ and ZXY conceived and designed the study; PXY and LXF performed the experiments and collected and analyzed the data; SQN participated in the animal experiments; LM, MXD, SYQ, CYH, XLP, and YW performed the clinical study; CYJ, LKY, and ZXH helped design the study; HXJ and PXY wrote the manuscript. All authors approved the final manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Xu-Ying Pei, Xue-Fei Liu.
Supplementary information
The online version contains supplementary material available at 10.1038/s41423-021-00829-y.
References
- 1.Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W, et al. Haploidentical hematopoietic stem cell transplantation without in vitro T-cell depletion for the treatment of hematological malignancies. Bone Marrow Transplant. 2006;38:291–7. doi: 10.1038/sj.bmt.1705445. [DOI] [PubMed] [Google Scholar]
- 2.Singh AK, McGuirk JP. Allogeneic stem cell transplantation: a historical and scientific overview. Cancer Res. 2016;76:6445–51. doi: 10.1158/0008-5472.CAN-16-1311. [DOI] [PubMed] [Google Scholar]
- 3.Appelbaum FR. Hematopoietic-cell transplantation at 50. N. Engl J Med. 2007;357:1472–5. doi: 10.1056/NEJMp078166. [DOI] [PubMed] [Google Scholar]
- 4.Ljungman P, de la Camara R, Robin C, Crocchiolo R, Einsele H, Hill JA, et al. Guidelines for the management of cytomegalovirus infection in patients with haematological malignancies and after stem cell transplantation from the 2017 European Conference on Infections in Leukaemia (ECIL 7) Lancet Infect Dis. 2019;19:e260–e72. doi: 10.1016/S1473-3099(19)30107-0. [DOI] [PubMed] [Google Scholar]
- 5.Ljungman P, Boeckh M, Hirsch HH, Josephson F, Lundgren J, Nichols G, et al. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis: Off Publ Infect Dis Soc Am. 2017;64:87–91. doi: 10.1093/cid/ciw668. [DOI] [PubMed] [Google Scholar]
- 6.Afessa B, Peters SG. Major complications following hematopoietic stem cell transplantation. Semin Respir Crit Care Med. 2006;27:297–309. doi: 10.1055/s-2006-945530. [DOI] [PubMed] [Google Scholar]
- 7.Einsele H, Ljungman P, Boeckh M. How I treat CMV reactivation after allogeneic hematopoietic stem cell transplantation. Blood. 2020;135:1619–29. doi: 10.1182/blood.2019000956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tzannou I, Leen AM. Preventing stem cell transplantation-associated viral infections using T-cell therapy. Immunotherapy. 2015;7:793–810. doi: 10.2217/imt.15.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith CJ, Quinn M, Snyder CM. CMV-specific CD8 T cell differentiation and localization: implications for adoptive therapies. Front Immunol. 2016;7:352. doi: 10.3389/fimmu.2016.00352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riddell SR, Watanabe KS, Goodrich JM, Li CR, Agha ME, Greenberg PD. Restoration of viral immunity in immunodeficient humans by the adoptive transfer of T cell clones. Science. 1992;257:238–41. doi: 10.1126/science.1352912. [DOI] [PubMed] [Google Scholar]
- 11.Walter EA, Greenberg PD, Gilbert MJ, Finch RJ, Watanabe KS, Thomas ED, et al. Reconstitution of cellular immunity against cytomegalovirus in recipients of allogeneic bone marrow by transfer of T-cell clones from the donor. N. Engl J Med. 2012;333:1038–44.. doi: 10.1056/NEJM199510193331603. [DOI] [PubMed] [Google Scholar]
- 12.O’Reilly RJ, Prockop S, Hasan AN, Koehne G, Doubrovina E. Virus-specific T-cell banks for ‘off the shelf’ adoptive therapy of refractory infections. Bone Marrow Transplant. 2016;51:1163–72. doi: 10.1038/bmt.2016.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peggs KS, Verfuerth S, Pizzey A, Khan N, Guiver M, Moss PA, et al. Adoptive cellular therapy for early cytomegalovirus infection after allogeneic stem-cell transplantation with virus-specific T-cell lines. Lancet. 2003;362:1375–7. doi: 10.1016/S0140-6736(03)14634-X. [DOI] [PubMed] [Google Scholar]
- 14.Feuchtinger T, Opherk K, Bethge WA, Topp MS, Schuster FR, Weissinger EM, et al. Adoptive transfer of pp65-specific T cells for the treatment of chemorefractory cytomegalovirus disease or reactivation after haploidentical and matched unrelated stem cell transplantation. Blood. 2010;116:4360–7. doi: 10.1182/blood-2010-01-262089. [DOI] [PubMed] [Google Scholar]
- 15.Cobbold M, Khan N, Pourgheysari B, Tauro S, McDonald D, Osman H, et al. Adoptive transfer of cytomegalovirus-specific CTL to stem cell transplant patients after selection by HLA-peptide tetramers. J Exp Med. 2005;202:379–86. doi: 10.1084/jem.20040613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blyth E, Clancy L, Simms R, Ma CK, Burgess J, Deo S, et al. Donor-derived CMV-specific T cells reduce the requirement for CMV-directed pharmacotherapy after allogeneic stem cell transplantation. Blood. 2013;121:3745–58. doi: 10.1182/blood-2012-08-448977. [DOI] [PubMed] [Google Scholar]
- 17.Bollard CM, Heslop HE. T cells for viral infections after allogeneic hematopoietic stem cell transplant. Blood. 2016;127:3331–40. doi: 10.1182/blood-2016-01-628982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koehne G, Hasan A, Doubrovina E, Prockop S, Tyler E, Wasilewski G, et al. Immunotherapy with donor T cells sensitized with overlapping pentadecapeptides for treatment of persistent cytomegalovirus infection or viremia. Biol Blood Marrow Transpl. 2015;21:1663–78. doi: 10.1016/j.bbmt.2015.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rauser G, Einsele H, Sinzger C, Wernet D, Kuntz G, Assenmacher M, et al. Rapid generation of combined CMV-specific CD4(+) and CD8(+) T-cell lines for adoptive transfer into recipients of allogeneic stem cell transplants. Blood. 2004;103:3565–72. doi: 10.1182/blood-2003-09-3056. [DOI] [PubMed] [Google Scholar]
- 20.Tzannou I, Watanabe A, Naik S, Daum R, Kuvalekar M, Leung KS, et al. “Mini” bank of only 8 donors supplies CMV-directed T cells to diverse recipients. Blood Adv. 2019;3:2571–80.. doi: 10.1182/bloodadvances.2019000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neuenhahn M, Albrecht J, Odendahl M, Schlott F, Dössinger G, Schiemann M, et al. Transfer of minimally manipulated CMV-specific T cells from stem cell or third-party donors to treat CMV infection after allo-HSCT. Leukemia. 2017;31:2161–71.. doi: 10.1038/leu.2017.16. [DOI] [PubMed] [Google Scholar]
- 22.Leen AM, Bollard CM, Mendizabal AM, Shpall EJ, Szabolcs P, Antin JH, et al. Multicenter study of banked third-party virus-specific T cells to treat severe viral infections after hematopoietic stem cell transplantation. Blood. 2013;121:5113–23. doi: 10.1182/blood-2013-02-486324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Withers B, Blyth E, Clancy LE, Yong A, Gottlieb DJ. Long-term control of recurrent or refractory viral infections after allogeneic HSCT with third-party virus-specific T cells. Blood Adv. 2017;1:2193–205. doi: 10.1182/bloodadvances.2017010223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holtappels R, Böhm V, Podlech J, Reddehase MJ. CD8 T-cell-based immunotherapy of cytomegalovirus infection: “proof of concept” provided by the murine model. Med Microbiol Immunol. 2008;197:125–34. doi: 10.1007/s00430-008-0093-2. [DOI] [PubMed] [Google Scholar]
- 25.Blyth E, Withers B, Clancy L, Gottlieb D. CMV-specific immune reconstitution following allogeneic stem cell transplantation. Virulence. 2016;7:967–80. doi: 10.1080/21505594.2016.1221022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klenerman P, Oxenius A. T cell responses to cytomegalovirus. Nat Rev Immunol. 2016;16:367–77. doi: 10.1038/nri.2016.38. [DOI] [PubMed] [Google Scholar]
- 27.Gratama JW, van Esser JW, Lamers CH, Tournay C, Löwenberg B, Bolhuis RL, et al. Tetramer-based quantification of cytomegalovirus (CMV)-specific CD8+ T lymphocytes in T-cell-depleted stem cell grafts and after transplantation may identify patients at risk for progressive CMV infection. Blood. 2001;98:1358–64. doi: 10.1182/blood.V98.5.1358. [DOI] [PubMed] [Google Scholar]
- 28.Wills MR, Poole E, Lau B, Krishna B, Sinclair JH. The immunology of human cytomegalovirus latency: could latent infection be cleared by novel immunotherapeutic strategies? Cell Mol Immunol. 2015;12:128–38. doi: 10.1038/cmi.2014.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reddehase MJ, Mutter W, Münch K, Bühring HJ, Koszinowski UH. CD8-positive T lymphocytes specific for murine cytomegalovirus immediate-early antigens mediate protective immunity. J Virol. 1987;61:3102–8. doi: 10.1128/jvi.61.10.3102-3108.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cwynarski K, Ainsworth J, Cobbold M, Wagner S, Mahendra P, Apperley J, et al. Direct visualization of cytomegalovirus-specific T-cell reconstitution after allogeneic stem cell transplantation. Blood. 2001;97:1232–40. doi: 10.1182/blood.V97.5.1232. [DOI] [PubMed] [Google Scholar]
- 31.Reddehase MJ, Mutter W, Koszinowski UH. In vivo application of recombinant interleukin 2 in the immunotherapy of established cytomegalovirus infection. J Exp Med. 1987;165:650–6. doi: 10.1084/jem.165.3.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reddehase MJ, Jonjić S, Weiland F, Mutter W, Koszinowski UH. Adoptive immunotherapy of murine cytomegalovirus adrenalitis in the immunocompromised host: CD4-helper-independent antiviral function of CD8-positive memory T lymphocytes derived from latently infected donors. J Virol. 1988;62:1061–5. doi: 10.1128/jvi.62.3.1061-1065.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Einsele H, Roosnek E, Rufer N, Sinzger C, Riegler S, Löffler J, et al. Infusion of cytomegalovirus (CMV)–specific T cells for the treatment of CMV infection not responding to antiviral chemotherapy. Blood. 2002;99:3916–22. doi: 10.1182/blood.V99.11.3916. [DOI] [PubMed] [Google Scholar]
- 34.Pei XY, Zhao XY, Chang YJ, Liu J, Xu LP, Wang Y, et al. Cytomegalovirus-specific T-cell transfer for refractory cytomegalovirus infection after haploidentical stem cell transplantation: the quantitative and qualitative immune recovery for cytomegalovirus. J Infect Dis. 2017;216:945–56. doi: 10.1093/infdis/jix357. [DOI] [PubMed] [Google Scholar]
- 35.Zhao XY, Pei XY, Chang YJ, Yu XX, Xu LP, Wang Y, et al. First-line therapy with donor-derived human cytomegalovirus (HCMV)-specific T cells reduces persistent HCMV infection by promoting antiviral immunity after allogenic stem cell transplantation. Clin Infect Dis. 2020;70:1429–37. doi: 10.1093/cid/ciz368. [DOI] [PubMed] [Google Scholar]
- 36.Xu L, Chen H, Chen J, Han M, Huang H, Lai Y, et al. The consensus on indications, conditioning regimen, and donor selection of allogeneic hematopoietic cell transplantation for hematological diseases in China-recommendations from the Chinese Society of Hematology. J Hematol Oncol. 2018;11:33. doi: 10.1186/s13045-018-0564-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fabrizio VA, Rodriguez-Sanchez MI, Mauguen A, Dahi PB, Doubrovina E, O’Reilly RJ, et al. Adoptive therapy with CMV-specific cytotoxic T lymphocytes depends on baseline CD4+ immunity to mediate durable responses. Blood Adv. 2021;5:496–503. doi: 10.1182/bloodadvances.2020002735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yaguchi T, Kobayashi A, Inozume T, Morii K, Nagumo H, Nishio H, et al. Human PBMC-transferred murine MHC class I/II-deficient NOG mice enable long-term evaluation of human immune responses. Cell Mol Immunol. 2018;15:953–62. doi: 10.1038/cmi.2017.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thomas S, Klobuch S, Podlech J, Plachter B, Hoffmann P, Renzaho A, et al. Evaluating human T-Cell therapy of cytomegalovirus organ disease in HLA-transgenic mice. PLoS Pathog 2015;11:e1005049. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.