Abstract
OBJECTIVES:
To examine whether greater frequency of depressive symptoms associates with increased risk of incident HF.
BACKGROUND:
Depressive symptoms associate with adverse prognosis in patients with prevalent heart failure (HF). Their association with incident HF is less studied, particularly in low-income and minority individuals.
METHODS:
We studied 23,937 Black or White Southern Community Cohort Study (SCCS) participants (median age 53 years, 70% Black, 64% women) enrolled between 2002 and 2009, without prevalent HF, receiving Centers for Medicare and Medicaid Services (CMS). Cox models adjusted for traditional HF risk factors, socioeconomic and behavioral factors, social support, and anti-depressant medication were used to quantify the association between depressive symptoms assessed at enrollment via the Center for Epidemiologic Studies Depression Scale (CESD-10) and incident HF ascertained from CMS ICD-9 (428.x) and −10 (I50, I110) codes through December 31, 2016.
RESULTS:
The median CESD-10 score was 9 (IQR: 5, 13). Over a median 11-year follow-up, 6081 (25%) participants developed HF. The strongest correlates of CESD-10 score were anti-depressant medication use, age, and socioeconomic factors, rather than traditional HF risk factors. Greater frequency of depressive symptoms associated with increased incident HF risk (per 8-unit higher CESD-10 HR 1.04, 95% CI: 1.00, 1.09; p = 0.038) without variation by race or sex. The association between depressive symptoms and incident HF varied by anti-depressant use (interaction-p = 0.03) with increased risk among individuals not taking anti-depressants.
CONCLUSION:
In this high-risk, low-income, predominantly Black cohort, greater frequency of depressive symptoms significantly associates with higher risk of incident HF.
Keywords: Heart failure, depression, Center for Epidemiologic Studies Depression Scale
Tweet:
In a high-risk low-income cohort, depressive symptoms associate with greater risk of incident heart failure independent of traditional risk factors.
INTRODUCTION
Heart failure (HF) affects between 6–7 million adults in the United States and is particularly common in the southeast.(1) While traditional cardiovascular risk factors, such as hypertension (HTN), diabetes (DM), and obesity account for a substantial portion of HF risk, the contribution of social determinants of health is garnering increased attention.(2–5) Psychosocial factors, such as depression, can modulate relationships between social determinants and disease.(4) Among patients with prevalent coronary artery disease (CAD) and HF, depressive symptoms associate with adverse prognosis.(6–11) Whether depressive symptoms associate with increased risk for incident HF, independent of traditional risk factors and social factors is less characterized.
The lifetime prevalence of depression in the general population is estimated at 16%, corresponding to 35 million U.S. adults.(12) Despite this high prevalence, the relationship of depression with new-onset HF has received relatively little attention.(13–16) The few studies were limited by low rates of incident HF or included predominantly white or male individuals. Low-income and minority populations often face challenges with respect to social determinants of health, which may increase risk for adverse outcomes. Investigating the role of depressive symptoms in HF development among high-risk individuals could provide novel insights for prevention. Therefore, in the Southern Community Cohort Study (SCCS), a predominantly low-income Black population, we tested the hypothesis that depressive symptoms associate with increased risk of HF, independent of traditional risk factors and social factors.
METHODS
Study population
The SCCS is a prospective cohort composed of low-income predominantly Black adults living in 12 southeastern states. A detailed description of the study methods has been previously published.(17) Briefly, the SCCS was designed to investigate incidence of cancer and other chronic diseases in a population often underrepresented in other cohort studies. Between 2002 and 2009, adults aged 40 to 79 years (n = 84,797) were enrolled, primarily (86%) from community health centers (CHC). All participants provided written informed consent. Protocols were approved by the Institutional Review Boards of Vanderbilt University Medical Center and Meharry Medical College.
This analysis included 23,937 participants meeting the following criteria at enrollment: 1) either aged ≥65 years or aged <65 years who either reported coverage by Centers for Medicare and Medicaid Services (CMS) at enrollment or had a CMS claim within 90 days of SCCS enrollment, as previously described (18,19); 2) free from prevalent HF; 3) completed the Center for Epidemiologic Studies Depression questionnaire (CESD-10); and 4) without a history of myocardial infarction (MI) or coronary artery bypass, given that depression associates with HF risk in the setting of prevalent CAD.(20) The analysis was restricted to self-reported Black and non-Hispanic White participants, as low numbers in other racial groups precluded stable statistical analysis.
Depressive symptoms and medications
Depressive symptoms were ascertained using the 10-item version of the CESD Scale; a widely used, reliable, and validated tool for determining the frequency of depressive symptoms over a one-week period.(21–24) A score ≥10 (max 30) indicates clinically relevant depressive symptoms.(23,24) At enrollment, participants reported current prescriptions for anti-depressant/anxiolytic medications and history of physician diagnosed depression.
Additional details regarding the study population, depressive symptoms and medications, cardiovascular and behavioral risk factors, and social determinants of health are provided in the Supplemental Appendix.
Outcome
Incident HF was determined via linkage with CMS Research Identifiable Files and was defined as the first occurrence of a medical claim with an International Classification of Diseases, 9th revision (ICD-9), discharge code of 428.x (428.0–428.9) or 10th revision (ICD-10) code of I50 or I110 within the Medicare institutional, Part B carrier, outpatient-based claims files, or Medicaid Analytic Extract Inpatient and Other Services claims files, as previously described.(19) Vital status was determined via National Death Index linkage. Censoring occurred at date of HF event, death, or December 31, 2016, whichever occurred first.(19)
Statistical Analysis
For descriptive statistics, participants were categorized according to CESD-10 score <10, 10–19, or ≥20. Continuous data was summarized as median (25th, 75th percentiles) and categorical data as percentage, unless otherwise specified. Comparisons were made using Kruskal-Wallis or Pearson chi-squared tests.
Multivariable ordinal logistic regression was performed to identify correlates of CESD-10 score. Multivariable Cox models were used to test whether depressive symptoms associate with increased risk of incident HF and a composite of death or HF. A test for a non-linear association between CESD-10 and HF was not significant; therefore, CESD-10 was modeled as a linear variable. A sensitivity analysis was performed in which CESD-10 score was replaced with a binary variable for whether a clinical diagnosis of depression was present at enrollment or not, defined as self-report of a physician diagnosis of depression or use of anti-depressant/anxiolytic medication. Models were adjusted for demographics (age, sex, and race), comorbidities (HTN, HLD, DM, BMI, stroke or TIA, and smoking), socioeconomic (income, education, employment, and enrollment source [CHC vs. general population]), behavioral (alcohol intake, sedentary activity, and physical activity), social support factors (marital status, the number of people providing emotional support or help in an emergency), and anti-depressant/anxiolytic use. Continuous variables were modeled using restricted cubic spline terms with 4 knots.
To address reverse causation; namely, the possibility undiagnosed HF contributed to depressive symptoms at enrollment, we performed a sensitivity analysis excluding individuals who developed HF within 3 months of enrollment. Additional exploratory analyses included examining the interaction of CESD-10 with race, sex, race-sex groups, and anti-depressant medications. Analyses were performed using R (The R project, Vienna, Austria).
RESULTS
Baseline characteristics
In the 23,937 participants, CESD-10 scores <10, 10–19, and ≥ 20 were present in 55%, 37%, and 8%, respectively. The median (25th, 75th percentile) CESD-10 score was 9 (5, 13). Table 1 displays baseline characteristics by CESD-10 score. Individuals with higher CESD-10 scores were younger and more often female and white. CESD-10 score inversely associated with education, income, and employment. HTN and DM were common and present with similar prevalence across CESD-10 score. BMI was greater among participants with higher CESD-10 scores.
Table 1.
Baseline Characteristics of 23,937 Southern Community Cohort Study Participants by CESD-10 Score
| CESD-10 Score | ||||
|---|---|---|---|---|
| Characteristic | <10 (N=13176) | 10–19 (N=8837) | ≥ 20 (N=1924) | p |
| Age, years | 57 (48, 67) | 51 (45, 58) | 49 (45, 54) | <0.001 |
| Female, % | 60 | 66 | 78 | <0.001 |
| Black, % | 71 | 72 | 59 | <0.001 |
| Education, % | <0.001 | |||
| <High school | 34 | 43 | 43 | |
| HS/vocational/junior college | 55 | 52 | 53 | |
| ≥ College degree | 11 | 5 | 4 | |
| Annual income < $15,000, % | 63 | 78 | 83 | <0.001 |
| Employed, % | 19 | 12 | 8 | <0.001 |
| Comorbidities, % | ||||
| Hypertension | 61 | 61 | 60 | 0.79 |
| Diabetes | 25 | 26 | 25 | 0.23 |
| Hyperlipidemia | 38 | 35 | 38 | <0.001 |
| Cerebrovascular disease | 8 | 9 | 10 | <0.001 |
| BMI | 28.9 (24.8, 34.0) | 29.3 (24.7, 35.3) | 29.9 (25.0, 36.3) | <0.001 |
| Smoking, % | <0.001 | |||
| Current | 34 | 48 | 55 | |
| Former | 28 | 20 | 16 | |
| Never | 38 | 33 | 29 | |
| Physical activity | ||||
| Sitting, hrs/day | 8.0 (5.4,11.0) | 8.2 (5.5,12.0) | 9.0 (6.0, 13.0) | <0.001 |
| Total activity, met-hrs/day | 13.9 (7.4, 23.6) | 12.6 (6.3, 22.9) | 11.5(4.8, 22.2) | <0.001 |
| Alcohol per daya | 0.96±3.3 | 1.4±4.2 | 1.3±4.2 | <0.001 |
| Marital Status, % | <0.001 | |||
| Married | 33 | 24 | 21 | |
| Divorced or separated | 31 | 36 | 46 | |
| Widowed | 16 | 12 | 10 | |
| Never married | 20 | 27 | 22 | |
| Close friends/relatives, n | 4 (2, 8) | 3 (1, 5) | 2 (1, 3) | <0.001 |
| Help in emergency, n | 3 (2, 5) | 2 (1, 4) | 2 (1, 3) | <0.001 |
| Anti-depressants/anxiolytics, % | 16 | 36 | 59 | <0.001 |
| History of Depression, % | 18 | 44 | 71 | <0.001 |
All continuous variables are displayed as median (25th, 75th percentile) except where indicated by (a) for which mean ± SD is displayed. BMI = body mass index, hrs= hours, HS= high school
Behavioral differences were apparent across CESD-10 scores. Participants reporting more frequent depressive symptoms were more often current smokers and more sedentary. Alcohol intake positively correlated with CESD-10 score. Additionally, lack of social support associated with increased frequency of depressive symptoms. Participants with higher CESD-10 scores had fewer social connections as demonstrated by marital status and fewer emotionally or financially supportive relationships. Anti-depressant/anxiolytic use and prior diagnosis of depression was more common among participants with higher CESD-10 scores.
Correlates of CESD-10 score were examined in a multivariable ordinal logistic regression with results shown in Supplemental Figures 1 A and B and Supplemental Table 1. Anti-depressant use and socioeconomic factors most strongly associated with CESD-10 score. In contrast, traditional cardiovascular risk factors, such as DM, HLD, BMI, history of stroke or TIA, and HTN contributed little to the overall variance in CESD-10 score despite significant associations.
Incident HF and Survival
Over a median 11 years (25th, 75th percentile: 8.6, 12.8) of follow-up, 6081 participants (25%) developed HF. Higher CESD-10 consistently associated with increased risk for incident HF (Table 2). In an age-, sex-, and race-adjusted model, each 8 point higher CESD-10, corresponding to the difference between the 25th to 75th percentiles of CESD-10 scores (5, 13), significantly associated with increased risk for incident HF (HR 1.17, 95% CI: 1.13–1.21; p <0.001). The association between CESD-10 and HF risk was attenuated but still significant after adjustment for traditional clinical HF risk factors (HR 1.11, 95% CI: 1.07–1.15; p <0.001). With further adjustment for socioeconomic and behavioral factors, social support and anti-depressant/anxiolytic use, higher CESD-10 score remained significantly associated with increased risk for incident HF (HR 1.04, 95% CI: 1.00–1.09; p = 0.038); Table 2, Supplemental Table 2, and Supplemental Figure 2. Central Illustration illustrates the predicted probability of incident HF at 5 years according to CESD-10 score. Results for the composite outcome of time to incident HF or death were similar (HR 1.04, 95% CI: 1.00–1.07; p = 0.032).
Table 2.
Risk of incident HF associated with CESD-10 score in the Southern Community Cohort Study
| Model | Covariates | Hazard Ratio per 8 unit increase in CESD-10 score | 95% CI | p |
|---|---|---|---|---|
| 1 | Age, sex, race | 1.17 | 1.13, 1.21 | <0.0001 |
| 2 | Model 1 + HTN, HLD, DM, BMI, Stroke/TIA, smoking | 1.11 | 1.07, 1.15 | <0.0001 |
| 3 | Model 2 + income, education, employment, alcohol, physical activity, marital status, close friends, help in emergency, anti-depressants | 1.04 | 1.00, 1.09 | 0.038 |
BMI= body mass index, DM= diabetes, HLD= hyperlipidemia, HTN= hypertension, TIA= transient ischemic attack
Central Illustration. Five-year risk of incident HF according to CESD-10 score in the Southern Community Cohort Study.
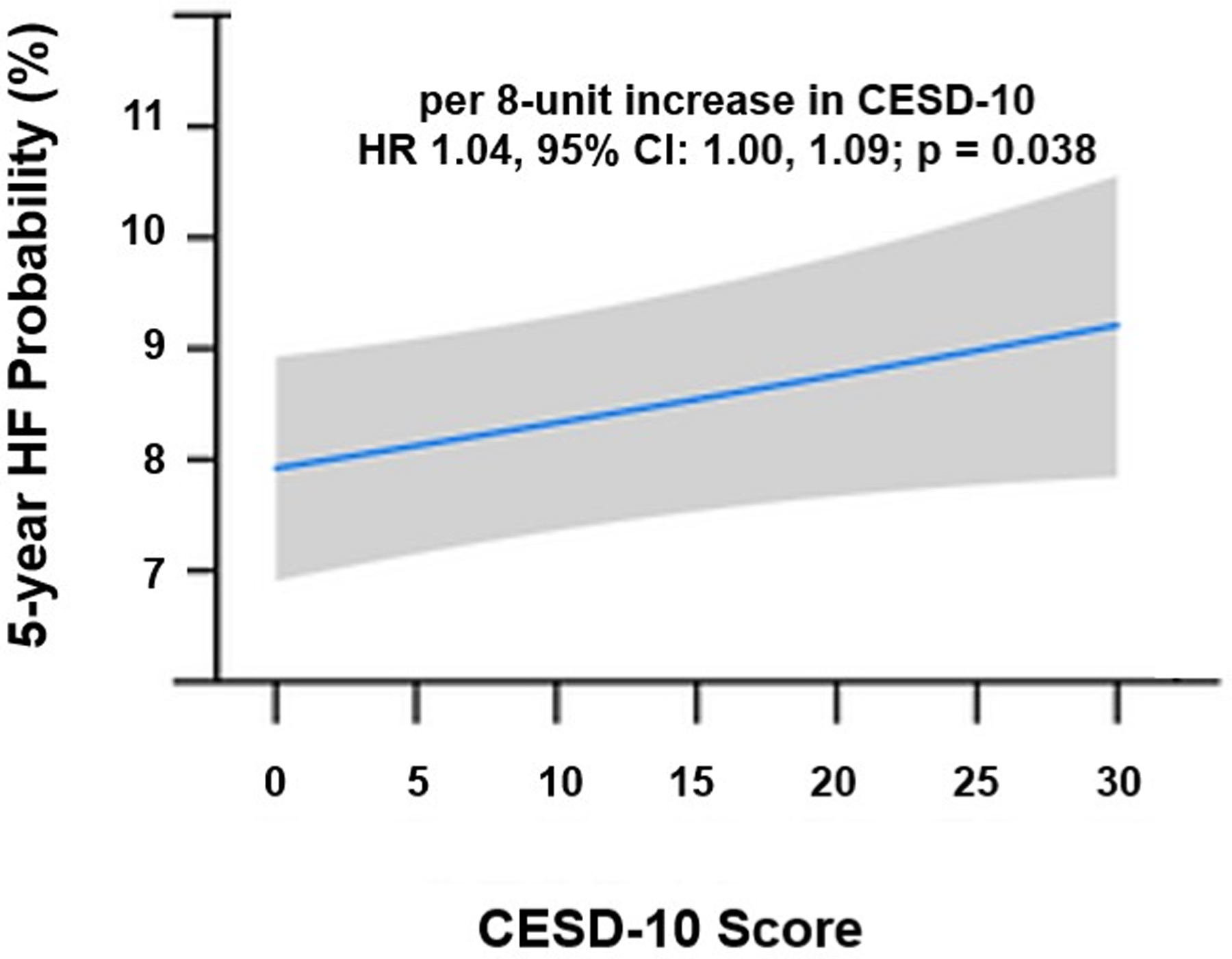
Greater frequency of depressive symptoms associated with increased risk of incident HF, including at levels considered to represent sub-clinical depression. Results shown are from the multivariable-adjusted Cox model including all variables shown in Table 2, Model 3.
To address the potential for reverse causation, we repeated the analysis after excluding 189 participants who developed HF within 3 months of enrollment. Our results did not substantially differ (HR 1.04, 95% CI: 1.00–1.09, p = 0.045). In another sensitivity analysis, we examined whether a diagnosis of depression, defined as a composite of self-reported history of depression or anti-depressant/anxiolytic medication use, associates with incident HF, with similar findings (HR 1.06, 95% CI:1.00–1.13, p = 0.045). Additionally, enrollment characteristics of participants who did and did not develop HF over the follow-up period are shown in Supplemental Table 3.
For the primary outcome of incident HF, we tested whether the association between depressive symptoms and HF risk varied by anti-depressant/anxiolytic medication use or by race, sex, or race-sex groups. The CESD-10 by anti-depressant/anxiolytic medication interaction term was significant (p = 0.03). Figure 1 demonstrates CESD-10 score associated with increased HF risk among participants without anti-depressant/anxiolytic use (HR 1.07, 95% CI: 1.02–1.12; p = 0.006), but not among participants using these medications (HR 1.00, 95% CI: 0.94–1.07; p = 0.91). We did not find evidence for significant variation in the risk of incident HF according to CESD-10 score by race, sex, or race-sex groups (interaction-p > 0.25 for all).
Figure 1. Differential association between CESD-10 score and HF risk according to anti-depressant/anxiolytic use in the Southern Community Cohort Study.
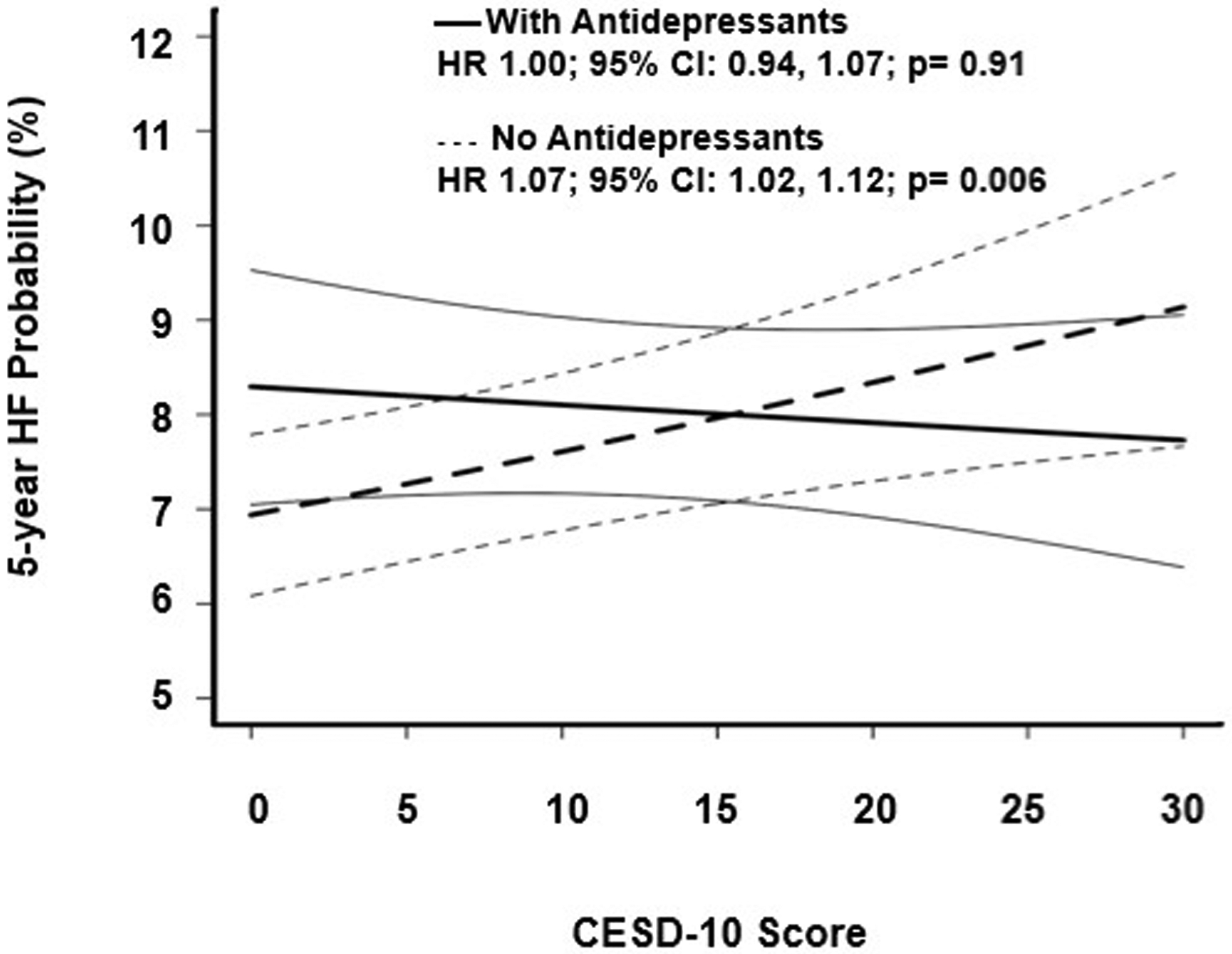
Risk of incident HF varies by anti-depressant/anxiolytic use. In participants taking anti-depressants/anxiolytics, greater frequency of depressive symptoms did not associate with increased HF risk in a multivariable adjusted analysis.
DISCUSSION
In a large, low-income, predominantly Black cohort of individuals residing in the southeastern United States at high risk for HF, individuals reporting a greater frequency of depressive symptoms at enrollment had significantly higher risk of incident HF independent of traditional cardiovascular risk factors, or socioeconomic and behavioral characteristics. Although the effect size was relatively small, the clinical significance of the increased risk of HF associated with higher CESD-10 scores may be substantial. CESD-10 score ≥10, an accepted threshold indicative of clinically relevant depressive symptoms, was common in our cohort, present in 45% of individuals; a prevalence exceeding DM (25%) and HLD (37%). Collectively, our findings suggest attention to depressive symptoms assessed using the clinically available CESD-10 score may help identify individuals at greater risk for the development of incident HF.
Distinct from other U.S. based community cohort studies (Cardiovascular Health Study [CHS], Multi-Ethnic Study of Atherosclerosis [MESA], and Yale Health and Aging Project [YHAP]), we demonstrate a significant association between greater depressive symptoms and incident HF (Table 3). Although a significant positive association between depressive symptoms or clinical diagnosis of depression has been demonstrated in a clinical cohort, an ancillary study of a hypertension clinical trial, and 2 European cohorts, compared with those studies, our SCCS cohort included the greatest proportion of Black individuals, was of substantially lower SES, had 2–15 times greater prevalence of depression, and had the highest incidence of HF (Table 3). Moreover, our analysis included adjustment for a greater number of social determinants of health compared with other studies. Insofar as the SCCS includes individuals not represented in most other cohorts, our findings are not only novel, but of potential clinical relevance as nearly one in two individuals in this population reported substantial depressive symptoms.
Table 3.
Novel characteristics of the SCCS compared with prior cohort studies investigating the association of depression with incident heart failure
| Cohort | N | Age | Race (%) | Female (%) | SES Descriptorsa | Depression Tool | Prevalence of Depression, % (n) | Incidence of HF, % (n) | Association with HF | Follow-up (years) |
|---|---|---|---|---|---|---|---|---|---|---|
| Community-based Cohort | ||||||||||
| SCCS | 23,937 | 40–79 | Black: 70 | 64 |
Income < 15k: 70%
< High school: 38% Employed: 16% |
CESD-10 | 45% (10,761) | 25% (6,081) | HR 1.04 (1.00–1.09) p = 0.038 | Median 11 |
| CHS (39) | 4,114 | ≥ 65 | Black: 14.2 | 59.2 |
Income < 25k: 61% (40) Education (y): 13.9 (41) Employed: NR/NC |
CESD-10 | 20.4% (840) | 24% (970) | HR 1.08 (0.92–1.26) p = NS | Median 10.7 |
| MESA (16) | 6,782 | 45–84 | Black: 27.9 | 52.9 |
Income < 25k: 31% (42) < High school: 18% Employed: 49% (43) |
CES-D | 12.9% (872) | 3.6% (242) | HR 1.19 (0.76–1.85) p = NS | Mean 9.3 |
| YHAP (13) | 2,501 | >65 | Non-white: 19.1 | 58.1 | Income: NR Education (y): ~9 Employment: NR |
CES-D | 7.5% (188) | 12.5 % (313) | HR 1.52 (0.94–2.43) p = 0.09 | Up to 14 |
| Clinical Cohort | ||||||||||
| VA (15) | 236,079 | 50–80 | Non-white: 17.4 | 6.6 | Income: NR Education: NR Employed: NR |
ICD-9 | 22.9% (54,062) | 4.7% (10,994) | HR 1.21 (1.13–1.28) | Up to 6 |
| Clinical-trial ancillary cohort | ||||||||||
| SHEP (14) | 4,538 | >60 | Non-white: 13.9 | 56.7 | Income: NR Education (y): 11.7 (44) Employment: NR |
CES-D | 4.9% (221) | 3.4% (156) | HR 2.59 (1.57–4.27) p < 0.001 | Median 4.5 |
| International Studies | ||||||||||
| HUNT (45) | 62,567 | ≥ 20 | No race reported (Norway) | 52.1 | Income: NR/NC Education: Up to 12 years: 77% Employed: NR |
Hospital Anxiety and Depression Scale | 3.2% (2,002) | 2.4% (1,499) | HR 1.41 (1.07–1.87)b | Mean 11.3 |
| UK (46) | ~1.3c million | >30 | Black: 1.6 | 46.4 | Lowest SES: 18.6% | Diagnosis or medication | 2.9% (39,747) | 0.7% (9,397) | HR 1.17 (1.03–1.32) | Median 6.9 |
CES-D = Center for Epidemiologic Studies Depression Scale, CHS = Cardiovascular Health Study, HF = heart failure, HUNT = Nord-Trøndelag Health Study, ICD-9 = International Classification of Diseases -9th revision, MESA = Multi-Ethnic Study of Atherosclerosis, NR/NC = not reported, not calculable, SCCS = Southern Community Cohort Study, SES = socioeconomic status, SHEP = Systolic Hypertension in the Elderly, UK = United Kingdom, VA= Veterans Affairs, YHAP = Yale Health and Aging Project.
SES descriptors: bolded if adjusted for in analysis, italicized if based on whole cohort statistics.
HR reported for severe symptoms.
Cohort 2.
We examined depressive symptoms assessed by CESD-10 on a continuous scale and found a linear increase in incident HF risk with greater frequency of depressive symptoms. This finding suggests the presence of risk for HF among individuals with even sub-clinical depressive symptoms. Our approach contrasts with prior studies examining the association between depression and incident HF using categorical scales. For example, in the Systolic Hypertension in the Elderly Program (n = 4,538), participants with depression defined as a CES-D score ≥ 16 had a 2-fold greater risk of incident HF compared with individuals with CES-D scores <16.(14) A similar risk estimate for the association between depression, defined at a threshold CES-D score ≥ 21, and incident HF was found in the YHAP (n = 2501) for women (HR 1.96, 95% CI: 1.11–3.46) but not men (HR 0.62, 95% CI: 0.23–1.71).(13) In contrast, among a predominantly male (93.4%) veteran population with no baseline cardiovascular disease (CVD) (n = 236,079) a clinical diagnosis of major depressive disorder was associated with incident HF (HR 1.21, 95% CI:1.13–1.28) after adjustment for demographic, behavioral, CVD risk factors and psychotropic medications.(15) In our study, a sensitivity analysis demonstrated a clinical diagnosis of depression significantly associated with incident HF, HR 1.06 (95% CI:1.00–1.13, p = 0.045). Prior studies demonstrated the incidence and prevalence of depression is higher in women and concordantly we found higher CESD-10 scores among women.(25) We did not, however, observe sex-based variation in the association between depressive symptoms and risk of incident HF. Moreover, we did not observe effect modification by race, addressing a gap rarely examined in prior studies which included predominantly white individuals.
In contrast to the aforementioned studies, in MESA, psychosocial factors, including depressive symptoms, were not associated with incident HF overall, although participants reporting poor health at baseline and high depressive symptoms had a trend toward 2-fold higher risk of incident HF.(16) The contrasting results between SCCS and the other U.S. based community cohort studies (MESA, CHS, YHAP) may be due to differences in cohort characteristics with fewer risk factors and a wider range of socioeconomic status compared with SCCS participants (Table 3). A recent study found a significant association between depressive symptoms and incident CVD, defined as coronary heart disease (CHD) or stroke.(26) Using the CES-D, the effect size was of a similar magnitude to our study with a hazard ratio per 1 standard deviation increase in depression score of 1.06 (95% CI 1.04–1.08) for the composite endpoint of CHD or stroke, while adjusting for age, sex, smoking status, and history of diabetes. The authors noted that the association persisted even at levels that would be considered sub-clinical depressive symptoms, consistent with our findings.
We found psychosocial and behavioral factors, rather than traditional clinical cardiovascular risk factors, most strongly correlated with frequency of depressive symptoms. Participants with higher CESD-10 scores were more likely to have lower socioeconomic status, poor lifestyle behaviors, and less social support, but had similar rates of HTN and DM compared with individuals with lower CESD-10 scores. These findings may help providers identify individuals with greater likelihood of having depressive symptoms for whom evaluation may be indicated. Moreover, these findings suggest the association between depressive symptoms and risk for HF is unlikely to be fully explained by either traditional cardiovascular risk factors leading to depressive symptoms or conversely depressive symptoms augmenting susceptibility to traditional cardiovascular risk factors.
The mechanisms by which depressive symptoms may associate with the risk of incident HF independent of traditional CV risk factors are not well understood. A comprehensive review of potential mechanisms has been summarized by others.(27–31) Briefly, the available evidence suggests individuals with depression have abnormalities in the hypothalamic-pituitary axis, neurohormonal and autonomic nervous system, immune and vascular systems, which have been implicated in the pathogenesis of HF. For example, individuals with depression display excess catecholamine and cortisol secretion, increased sympathetic tone and autonomic nervous system dysregulation, increased pro-inflammatory cytokines, dysregulation of platelet and endothelial function, and behavioral changes in diet, physical activity, and medical adherence. Additional studies are needed to further elucidate the pathophysiologic and behavioral mechanisms underlying the association between depressive symptoms and risk of HF.
Whether treatment of depression improves HF outcomes may warrant further investigation. Among patients with prevalent HF, depression is associated with worse outcomes and increased mortality rate.(8–10) To date, two trials have reported the effect of drug-based treatment of depression on cardiovascular outcomes among patients with prevalent HF. The primary result in both trials was neutral, however, a post-hoc analysis of the Sertraline Against Depression and Heart Disease in Chronic Heart Failure (SADHART-CHF) trial found improved outcomes in the subset of patients who achieved remission of depression.(32–34) Other clinical trials have investigated the effects of interventions targeting depression on outcomes in patients with prevalent HF (Supplemental Table 4). Although not a randomized trial, in the previously mentioned study of veterans without prevalent HF, all anti-depressant classes, except tricyclics, significantly associated with lower risk of incident HF.(15) Similarly, we found the risk of incident HF in relation to depressive symptoms varied according to anti-depressant use. Higher CESD-10 scores only associated with higher HF risk in individuals who were not receiving anti-depressant medications. A prior study in the SCCS demonstrated racial disparities in the treatment of depression with less anti-depressant use in Black participants at all levels of depressive symptoms.(35) Although fewer Black participants reported anti-depressant use in our analysis (White 40%, Black 21%), we did not find evidence for a differential association between CESD-10 score and risk of incident HF according to race or sex, even when accounting for anti-depressant use. While we recognize our study was not a clinical trial specifically designed to test whether treatment of depressive symptoms reduces the risk of incident HF, our findings in the context of the existing literature suggest HF risk associated with depressive symptoms may be modifiable. The role for and mechanisms by which anti-depressant therapy may reduce the risk of incident HF could not be elucidated from this study design but are questions for future investigation.
Though our study is the largest U.S. community-based cohort to examine incident HF risk associated with depressive symptoms and included a relatively younger population with a greater proportion of Black and female individuals of low socioeconomic status compared with prior studies, limitations should be noted.(13–15) First, our results may not be generalizable to other populations as we specifically investigated the impact of depressive symptoms in a low-income and minority population. Second, we used CESD-10 to determine presence and severity of depressive symptoms. Although CESD-10 is not designed to diagnose depression, CESD-10 is a validated tool for assessing depressive symptoms, with a score ≥10 correlated with clinically relevant depressive symptoms.(24,36) Third, depressive symptoms and covariates were assessed at a single point at study enrollment. This approach, however, not only aligns with prior studies of depression and cardiovascular risk, but also clinical practice in which prognostication is based on data available at the time of assessment, rather than accounting for future occurrence of comorbidities or lifestyle changes.(6,14) We appreciate, however, that CESD-10 scores, comorbidities, and other health determinants may vary over time, such that their consideration over the life course should be an aim of future analyses.(37) While we excluded individuals with a history of myocardial infarction or coronary artery bypass grafting at enrollment, we were unable to account for interim CAD events after enrollment. Prior data from MESA, however, indicates interim myocardial infarction was less likely to contribute to incident HF, particularly in Blacks.(38) Fourth, we could not account for unmeasured clinical factors, such as left ventricular ejection fraction and/or circulating markers of myocardial injury or stress, which may be on the causal pathway associating depressive symptoms and HF risk. Understanding these relationships is a future direction. Fifth, medical history and health behaviors were ascertained via self-report, which could introduce misclassification bias; although prior studies in SCCS demonstrate the validity of this approach.(17)
CONCLUSION
In a large, high risk, low-income, and predominantly Black cohort from the southeastern United States, depressive symptoms significantly associate with greater risk of incident HF. In this cohort, depression is very common and a potentially modifiable mechanism contributing to the increased risk of HF, particularly in populations with less favorable social determinants of health.
Supplementary Material
Clinical Perspectives:
Competency in Medical Knowledge:
Depressive symptoms are common in low-income populations and represent a potentially modifiable risk factor for incident heart failure.
Translational Outlook:
Future research should examine the role of anti-depressant therapies in reducing risk for incident heart failure.
Acknowledgments:
The authors thank all SCCS participants and research team.
Funding Sources:
DD was supported by the Training in Cardiovascular Research T32 HL007411, Nashville, TN.
Agency for Healthcare Research and Quality/Patient Centered Outcomes Research Institute Learning Health Systems K12HS026395 to DN, Nashville, TN.
The Southern Community Cohort Study was supported by the National Cancer Institute (R01 CA092447, U01 CA202979). Data collection performed by the Survey and Biospecimen Shared Resource which is supported in part by the Vanderbilt-Ingram Cancer Center (P30 CA068485), Nashville, TN.
LIST OF ABBREVIATIONS
- HF
heart failure
- SCCS
Southern Community Cohort Study
- CES-D
Center for Epidemiologic Studies Depression Scale
- MI
myocardial infarction
- CAD
coronary heart disease
- CVD
cardiovascular disease
- HTN
hypertension
- DM
diabetes mellitus
- HLD
hyperlipidemia
- BMI
body mass index
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: No disclosures. No relationship with industry.
REFERENCES
- 1.Benjamin EJ, Virani SS, Callaway CW et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 2.Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol 1993;22:6a–13a. [DOI] [PubMed] [Google Scholar]
- 3.Dunlay SM, Weston SA, Jacobsen SJ, Roger VL. Risk factors for heart failure: a population-based case-control study. Am J Med 2009;122:1023–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Havranek EP, Mujahid MS, Barr DA et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2015;132:873–98. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation 1993;88:1973–98. [DOI] [PubMed] [Google Scholar]
- 6.Brown JM, Stewart JC, Stump TE, Callahan CM. Risk of coronary heart disease events over 15 years among older adults with depressive symptoms. Am J Geriatr Psychiatry 2011;19:721–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Neil A, Fisher AJ, Kibbey KJ et al. Depression is a risk factor for incident coronary heart disease in women: An 18-year longitudinal study. J Affect Disord 2016;196:117–24. [DOI] [PubMed] [Google Scholar]
- 8.Albert NM, Fonarow GC, Abraham WT et al. Depression and clinical outcomes in heart failure: an OPTIMIZE-HF analysis. Am J Med 2009;122:366–73. [DOI] [PubMed] [Google Scholar]
- 9.Johnson TJ, Basu S, Pisani BA et al. Depression predicts repeated heart failure hospitalizations. J Card Fail 2012;18:246–52. [DOI] [PubMed] [Google Scholar]
- 10.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006;48:1527–37. [DOI] [PubMed] [Google Scholar]
- 11.Lichtman JH, Froelicher ES, Blumenthal JA et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation 2014;129:1350–69. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Berglund P, Demler O et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003;289:3095–105. [DOI] [PubMed] [Google Scholar]
- 13.Williams SA, Kasl SV, Heiat A, Abramson JL, Krumholz HM, Vaccarino V. Depression and risk of heart failure among the elderly: a prospective community-based study. Psychosom Med 2002;64:6–12. [DOI] [PubMed] [Google Scholar]
- 14.Abramson J, Berger A, Krumholz HM, Vaccarino V. Depression and risk of heart failure among older persons with isolated systolic hypertension. Arch Intern Med 2001;161:1725–30. [DOI] [PubMed] [Google Scholar]
- 15.Garfield LD, Scherrer JF, Hauptman PJ et al. Association of anxiety disorders and depression with incident heart failure. Psychosom Med 2014;76:128–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ogilvie RP, Everson-Rose SA, Longstreth WT Jr., Rodriguez CJ, Diez-Roux AV, Lutsey PL. Psychosocial Factors and Risk of Incident Heart Failure: The Multi-Ethnic Study of Atherosclerosis. Circ Heart Fail 2016;9:e002243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved 2010;21:26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kubicki DM, Xu M, Akwo EA et al. Race and Sex Differences in Modifiable Risk Factors and Incident Heart Failure. JACC Heart failure 2020;8:122–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akwo EA, Kabagambe EK, Wang TJ et al. Heart Failure Incidence and Mortality in the Southern Community Cohort Study. Circ Heart Fail 2017;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.May HT, Horne BD, Carlquist JF, Sheng X, Joy E, Catinella AP. Depression after coronary artery disease is associated with heart failure. J Am Coll Cardiol 2009;53:1440–7. [DOI] [PubMed] [Google Scholar]
- 21.Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale: its use in a community sample. Am J Psychiatry 1983;140:41–6. [DOI] [PubMed] [Google Scholar]
- 22.Radloff LS. The CES-D Scale:A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 23.Bjorgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment 2013;20:429–36. [DOI] [PubMed] [Google Scholar]
- 24.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 1994;10:77–84. [PubMed] [Google Scholar]
- 25.Eid RS, Gobinath AR, Galea LAM. Sex differences in depression: Insights from clinical and preclinical studies. Prog Neurobiol 2019;176:86–102. [DOI] [PubMed] [Google Scholar]
- 26.Harshfield EL, Pennells L, Schwartz JE et al. Association Between Depressive Symptoms and Incident Cardiovascular Diseases. JAMA 2020;324:2396–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grippo AJ, Johnson AK. Biological mechanisms in the relationship between depression and heart disease. Neurosci Biobehav Rev 2002;26:941–62. [DOI] [PubMed] [Google Scholar]
- 28.Huffman JC, Celano CM, Beach SR, Motiwala SR, Januzzi JL. Depression and cardiac disease: epidemiology, mechanisms, and diagnosis. Cardiovasc Psychiatry Neurol 2013;2013:695925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carney RM, Freedland KE, Veith RC. Depression, the autonomic nervous system, and coronary heart disease. Psychosom Med 2005;67 Suppl 1:S29–33. [DOI] [PubMed] [Google Scholar]
- 30.Pasic J, Levy WC, Sullivan MD. Cytokines in depression and heart failure. Psychosom Med 2003;65:181–93. [DOI] [PubMed] [Google Scholar]
- 31.Joynt KE, Whellan DJ, O’Connor CM. Depression and cardiovascular disease: mechanisms of interaction. Biol Psychiatry 2003;54:248–61. [DOI] [PubMed] [Google Scholar]
- 32.O’Connor CM, Jiang W, Kuchibhatla M et al. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol 2010;56:692–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jiang W, Krishnan R, Kuchibhatla M et al. Characteristics of depression remission and its relation with cardiovascular outcome among patients with chronic heart failure (from the SADHART-CHF Study). Am J Cardiol 2011;107:545–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Angermann CE, Gelbrich G, Stork S et al. Effect of Escitalopram on All-Cause Mortality and Hospitalization in Patients With Heart Failure and Depression: The MOOD-HF Randomized Clinical Trial. JAMA 2016;315:2683–93. [DOI] [PubMed] [Google Scholar]
- 35.Osborn CY, Trott HW, Buchowski MS et al. Racial disparities in the treatment of depression in low-income persons with diabetes. Diabetes Care 2010;33:1050–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Irwin M, Artin K, Oxman MN. Screening for depression in the older adult: Criterion validity of the 10-item center for epidemiological studies depression scale (ces-d). Arch Intern Med 1999;159:1701–1704. [DOI] [PubMed] [Google Scholar]
- 37.Malhi GS, Mann JJ. Depression. Lancet 2018;392:2299–2312. [DOI] [PubMed] [Google Scholar]
- 38.Bahrami H, Kronmal R, Bluemke DA et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med 2008;168:2138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van den Broek KC, Defilippi CR, Christenson RH, Seliger SL, Gottdiener JS, Kop WJ. Predictive value of depressive symptoms and B-type natriuretic peptide for new-onset heart failure and mortality. Am J Cardiol 2011;107:723–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gottdiener JS, Arnold AM, Aurigemma GP et al. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol 2000;35:1628–37. [DOI] [PubMed] [Google Scholar]
- 41.Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ. Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med 2000;160:1761–8. [DOI] [PubMed] [Google Scholar]
- 42.Bild DE, Detrano R, Peterson D et al. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2005;111:1313–20. [DOI] [PubMed] [Google Scholar]
- 43.Fujishiro K, Diez Roux AV, Landsbergis P et al. Associations of occupation, job control and job demands with intima-media thickness: the Multi-Ethnic Study of Atherosclerosis (MESA). Occup Environ Med 2011;68:319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Group SR. Prevention of Stroke by Antihypertensive Drug Treatment in Older Persons With Isolated Systolic Hypertension: Final Results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991;265:3255–3264. [PubMed] [Google Scholar]
- 45.Gustad LT, Laugsand LE, Janszky I, Dalen H, Bjerkeset O. Symptoms of anxiety and depression and risk of heart failure: the HUNT Study. Eur J Heart Fail 2014;16:861–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Daskalopoulou M, George J, Walters K et al. Depression as a Risk Factor for the Initial Presentation of Twelve Cardiac, Cerebrovascular, and Peripheral Arterial Diseases: Data Linkage Study of 1.9 Million Women and Men. PLoS One 2016;11:e0153838. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


